Abstract
Background/Aim: Coronavirus is an ongoing pandemic challenging health systems worldwide. The aim of this report was to evaluate the effectiveness of lockdown in different countries, highlighting the performance of Greek society and authorities. Methods: We analyzed publicly available data from the “Worldometer”. We evaluated the efficacy of lockdown at one month after implementation. Delta Days (DD) referred to the difference in the days of reaching 1 case/million people to the adoption of lockdown. Results: Higher healthcare expenditure as % of the national GDP was not correlated with better 30-day mortality outcomes. DD index was significantly correlated to the incidence of COVID-19 per million people at 30 days (p-value=0.001). The correlation between DD and 30-day mortality was not statistically significant (p-value=0.087). Conclusion: Early lockdown was proven to be the appropriate policy to limit the spread of COVID-19. Greece was a success story in preventing spread despite limited resources.
Keywords: Coronavirus, COVID-19, quarantine, Greece
Coronavirus 2 is the cause of an ongoing international outbreak of a respiratory illness, known as coronavirus disease 2019 (COVID-19) (1). It consists of the largest epidemic since the swine flu outbreak in 2009, claiming more than 300,000 deaths until today (2). This pandemic is proved to be a major public health challenge for health systems internationally, exceeding the capacity of intensive care units and means of mechanical ventilation as expected from the available models (3). Since the outbreak of the disease, the major targets for its successful management were the deployment of massive, reliable testing methods, identification of successful treatments and prevention of health system oversaturation.
Greece reported its first confirmed case on February 26th (4). Greek Health authorities preemptively announced a series of measures to limit the spread of the disease. In the same frame, 13 reporting hospitals with expertise have been designated to manage these cases (4). Definitely, COVID-19 posed an unprecedented challenge to Greece’s healthcare system for many reasons. Besides the obvious concerns for the disease-related mortality (1) that mandates preparation for managing this pandemic at the level of individual and public health, a slowly recovering economy after a decade of financial regression seems vulnerable to its global and local effects (5). All measures are predicted to have disruptive effects on the economy, especially as far as the access to the supply of goods, services, and an increase in unemployment (6).
The aim of our analysis was to evaluate the effectiveness of the lockdown measures at an international scale, taking into consideration the mixture of policies, the healthcare-directed expenditure and the outcomes in terms of incidence and COVID-19-related mortality. Was Greece a success story?
Methods
To address this question, we analyzed publicly available data from the “Worldometer”, regarding the effectiveness of the implemented measures to prevent oversaturation of health systems, such as the adoption of early quarantine measures and the large-scale sampling of COVID-19 cases. We evaluated the efficacy of these measures at one month after their implementation, focusing on the 30-day number of confirmed COVID-19 cases and reported deaths per million of population. Since school shutdown was a universally adopted measure, it was selected to represent the starting point of the quarantine. Delta Days (DD) referred to the difference in days of reaching 1 case/million people to the adoption of quarantine. A linear regression analysis was performed to demonstrate the correlations between DD, confirmed cases and reported mortality (STATA 16, College Station, TX, USA). p-Value<0.05 was defined as statistically significant.
Results
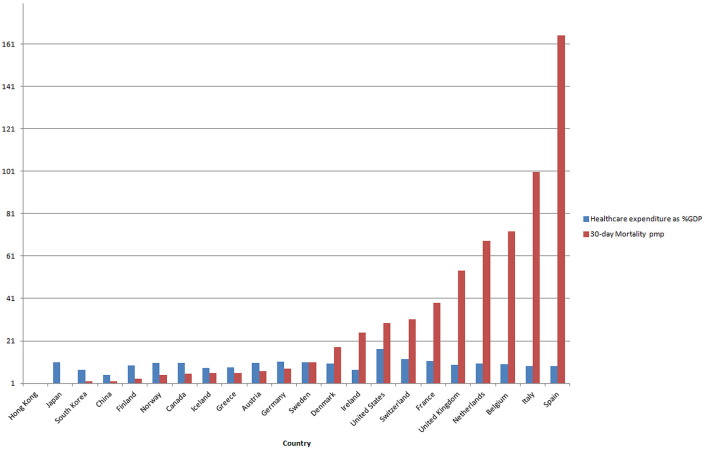
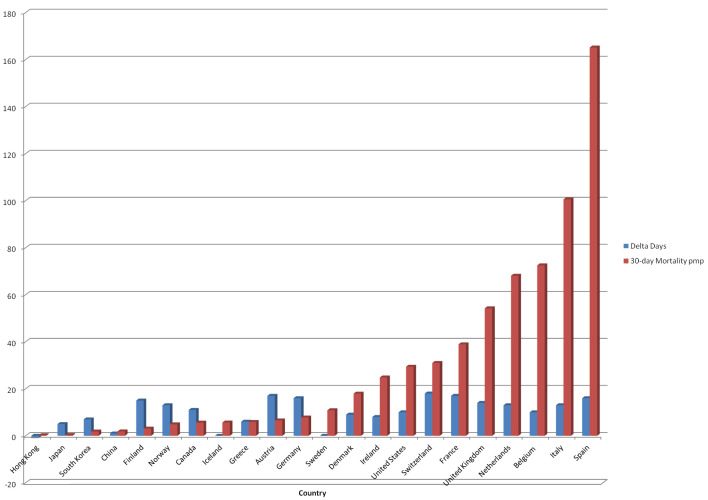
Iceland and Sweden were the most important examples of the large-scale sampling of the population. The rest of the affected countries implemented the quarantine (lockdown) policy. Table I summarizes the findings of our analysis. The first finding of our analysis was the high heterogeneity in terms of the time of implementation of the lockdown after the documentation of the first COVID-19 positive case. The timeframe, which varied from -1 day to 1 month (31 days), might reflect differences in policies and perception of the magnitude of the disease, with an average of 10.9 days and a median of 12 days. Another interesting finding of our analysis was the fact that higher healthcare expenditure, as % of the national GDP, was not correlated with better 30-day mortality outcomes (Figure 1). This suggests that the policies to prevent disease spread and related mortality are more effective than the policies to rescue, such as more resources directed to treatment and advanced critical care. DD index was significantly correlated to the incidence of COVID-19 per million people at 30 days (p-value=0.001). The correlation between the DD and the 30-day mortality rate per million people was not statistically significant (p-value=0.087) (Figure 2), indicating that other factors also have driven the COVID-19 attributed mortality.
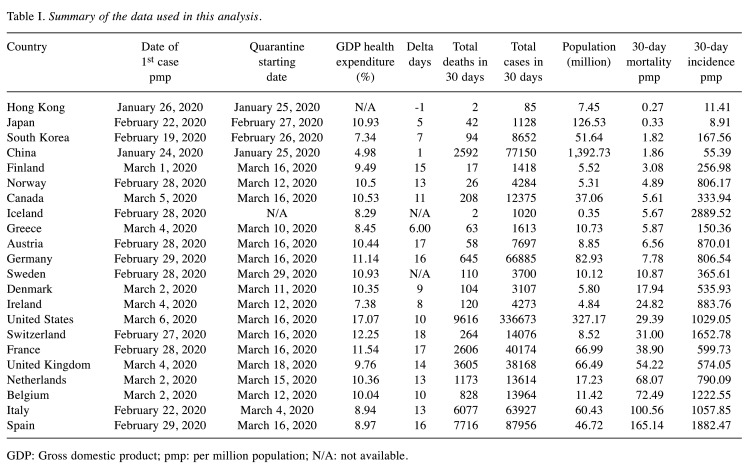
Table I. Summary of the data used in this analysis.
GDP: Gross domestic product; pmp: per million population; N/A: not available.
Figure 1. Illustration of the 30-day mortality per million people (pmp) and healthcare expenditure in millions as % of the national GDP.
Figure 2. Delta days and 30-day mortality per million people per country.
Discussion
Since most countries have now completed the first month since the beginning of the outbreak, the first conclusions can be drawn for the efficacy of the lockdown. It is clear, that East Asia countries did significantly better than Europe and North America since the beginning of this outbreak. A rapid adoption of quarantine measures as well as large-scale testing of the population contributed to this successful outcome.
In Europe, Greece was definitely one of the ‘’success stories’’, especially if we take into consideration that it had the lowest health expenditure in Europe and suffered significant shortages in the public health system as a result of the recent economic crisis (7-10). Another challenge that Greece had to face is the “explosive mixture’’ of this epidemiological threat with the persistent refugee crisis that is evolving since 2014, with millions of migrants entering Europe via the Mediterranean (11,12). This humanitarian (13) and social crises (14) generated challenges and struggles for the recovering Greek economy mostly in the field of healthcare and integration (11).
Despite being between a rock and a hard place as explained above, Greece was the country with the earliest adoption of the lockdown in response to COVID-19 outbreak, resulting in the lowest number of 30-day mortality per million population after Norway and Finland, which however had invested significantly in the development of their health system as demonstrated by the public health expenditure (15,16). In contrast, other Southern Europe countries with similar statistics to Greece in terms of Gross Domestic Health Expenditure (15) and aging population (17), but with delayed adoption of quarantine, suffered the highest losses from the pandemic.
Our analysis has many limitations that deserve mentioning. We based our analysis on strict and widely accepted data without analyzing in depth the peculiarities and differences among nations and populations. The truth is that the Greek population is rather homogeneous compared to the diversity that can be found in other European countries or in the USA (18). Also, we did not discuss the differences in the economics of policies behind the implementation of the lockdown, since in many circumstances, the countries decided to follow less restrictive protection measures to prevent the financial impact and regression a general lockdown could cause to the local economy (19,20). This decision might be financially justified but is not supported by data at the health and humanitarian level. Also, we did not assess the effect of lockdown on other aspects of social life, such as mental health (21), academic growth (22), education (23) and advanced healthcare services (24,25). These are important factors that should be taken into consideration when evaluating outcomes of specific policies.
In conclusion, early lockdown was proven to be the appropriate policy to limit the spread of COVID-19. As more qualitative quarantine metrics, such as the different bundle of measures and restrictions and the level of population compliance per country become available, more conclusions regarding its role will be drawn. Together with the lack of reliable metrics to assess the capacity of health systems to respond to public health crisis, this might be the most important lesson from the current crisis.
Conflicts of Interest
The Authors have no conflicts of interest to declare in relation to this study.
Authors’ Contributions
Dimitrios Moris performed the literature search and wrote the manuscript. Dimitrios Schizas revised the manuscript.
Acknowledgements
The Authors would like to thank Dr. Marinos Kosmopoulos for his contribution to the design of the study.
References
- 1.Wang C, Horby PW, Hayden FG, Gao GF. A novel coronavirus outbreak of global health concern. Lancet. 2020;395(10223):470–473. doi: 10.1016/S0140-6736(20)30185-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Worldometers. Available at: https://www.worldometers.info/coronavirus/ [Last accessed May 23, 2020]
- 3.Ajao A, Nystrom SV, Koonin LM, Patel A, Howell DR, Baccam P, Lant T, Malatino E, Chamberlin M, Meltzer MI. Assessing the capacity of the us health care system to use additional mechanical ventilators during a large-scale public health emergency. Disaster Med Public Health Prep. 2015;9(6):634–641. doi: 10.1017/dmp.2015.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Worldometers. Available at: https://www.worldometers.info/coronavirus/country/greece/ [Last accessed May 23, 2020]
- 5.Global Burden of Disease Greece Collaborators The burden of disease in Greece, health loss, risk factors, and health financing, 2000-16: An analysis of the global burden of disease study 2016. Lancet Public Health. 2018;3(8):e395–e406. doi: 10.1016/S2468-2667(18)30130-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.L’Angiocola PD, Monti M. Covid-19: The critical balance between appropriate governmental restrictions and expected economic, psychological and social consequences in italy. Are we going in the right direction. Acta Biomed. 2020;91(2):35–38. doi: 10.23750/abm.v91i2.9575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zilidis C, Stuckler D, McKee M. Use of amenable mortality indicators to evaluate the impact of financial crisis on health system performance in greece. Eur J Public Health. 2020 doi: 10.1093/eurpub/ckaa058. [DOI] [PubMed] [Google Scholar]
- 8.Schizas D, Michalinos A, Kanavidis P, Karaolanis G, Lidoriki I, Sioulas AD, Moris D. The profile of patients receiving public and private surgical services in greece during the economic crisis: A comparative study. Ann Transl Med. 2019;7(1):5. doi: 10.21037/atm.2018.12.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moris D, Zavos G, Menoudakou G, Karampinis A, Boletis J. Organ donation during the financial crisis in greece. Lancet. 2016;387(10027):1511–1512. doi: 10.1016/S0140-6736(16)30130-1. [DOI] [PubMed] [Google Scholar]
- 10.Moris D, Schizas D, Papalampros A, Felekouras E, Liakakos T. The struggle for intensive care coverage of patients with hepatobiliary malignancies in greece: Patients are not numbers. J BUON. 2017;22(5):1363–1364. [PubMed] [Google Scholar]
- 11.Moris D, Kousoulis A. Refugee crisis in greece: Healthcare and integration as current challenges. Perspect Public Health. 2017;137(6):309–310. doi: 10.1177/1757913917726019. [DOI] [PubMed] [Google Scholar]
- 12.Moris D, Felekouras E, Linos D. Global surgery initiative in greece: More than an essential initiative. Lancet. 2016;388(10048):957. doi: 10.1016/S0140-6736(16)31487-8. [DOI] [PubMed] [Google Scholar]
- 13.Kontos M, Moris D, Zografos N, Liakakos T. The greek financial crisis: Maintaining medical education against the odds. Postgrad Med J. 2015;91(1081):609–611. doi: 10.1136/postgradmedj-2015-133638. [DOI] [PubMed] [Google Scholar]
- 14.Moris D, Karamagioli E, Kontos M, Athanasiou A, Pikoulis E. Refugee crisis in greece: The forthcoming higher education challenge. Ann Transl Med. 2017;5(15):317. doi: 10.21037/atm.2017.05.05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Current health expenditure (% of GDP) | Data. Available at: https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS. [Last Accessed May 23, 2020]
- 16.Rechel B, Wright S, Barlow J, McKee M. Hospital capacity planning: From measuring stocks to modelling flows. Bull World Health Organ. 2010;88(8):632–636. doi: 10.2471/BLT.09.073361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Worldometers. Available at: https://www.worldometers.info/world-population/ [Last accessed May 23, 2020]
- 18.Schmidt HD, Scheil HG, Huckenbeck W, Scheffrahn W, Efremovska L. Genetic studies in south balkan populations. Coll Antropol. 2003;27(2):501–506. [PubMed] [Google Scholar]
- 19.Yamin M. Counting the cost of covid-19. Int J Inf. 2020;Technol:1–7. doi: 10.1007/s41870-020-00466-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Bausch DG. Precision physical distancing for COVID-19: An important tool in unlocking the lockdown. Am J Trop Med Hyg. 2020 doi: 10.4269/ajtmh.20-0359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Torjesen I. Covid-19: Mental health services must be boosted to deal with "tsunami" of cases after lockdown. BMJ. 2020;369:m1994. doi: 10.1136/bmj.m1994. [DOI] [PubMed] [Google Scholar]
- 22.Saini KS, de Las Heras B, de Castro J, Venkitaraman R, Poelman M, Srinivasan G, Saini ML, Verma S, Leone M, Aftimos P, Curigliano G. Effect of the COVID-19 pandemic on cancer treatment and research. , 2020. PMID: . DOI: . Lancet Haematol. 2020 doi: 10.1016/S2352-3026(20)30123-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sahu P. Closure of universities due to coronavirus disease 2019 (covid-19): Impact on education and mental health of students and academic staff. Cureus. 2020;12(4):e7541. doi: 10.7759/cureus.7541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al-Shamsi HO, Alhazzani W, Alhuraiji A, Coomes EA, Chemaly RF, Almuhanna M, Wolff RA, Ibrahim NK, Chua MLK, Hotte SJ, Meyers BM, Elfiki T, Curigliano G, Eng C, Grothey A, Xie C. A practical approach to the management of cancer patients during the novel coronavirus disease 2019 (covid-19) pandemic: An international collaborative group. Oncologist. 2020 doi: 10.1634/theoncologist.2020-0213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Moris D, Shaw BI, Dimitrokallis N, Barbas AS. Organ donation during the coronavirus pandemic: An evolving saga in uncharted waters. Transpl Int. 2020 doi: 10.1111/tri.13614. [DOI] [PMC free article] [PubMed] [Google Scholar]