Abstract
Introduction:
Alternate nostril breathing (ANB) is an effective breathing exercise with therapeutic benefits on cardiorespiratory functions for healthy and diseased individuals. This study was conducted to assess the effects of ANB exercise on cardiorespiratory tasks in healthy adults.
Materials and Methods:
This randomized experimental study was conducted in the Department of Physiology, Chittagong Medical College, Chattogram, from July 2017 to June 2018. A total of 100 1st-year students, aged between 18 and 20 years, were included by a random sampling method. Fifty participants (25 males and 25 females) were enrolled in the experimental group, while age- and body mass index-matched another 50 participants (25 males and 25 females) served as the control group. Experimental group participants performed ANB exercise for 4 weeks. Cardiorespiratory parameters (pulse rate, blood pressure, forced vital capacity, forced expiratory volume in 1st s [FEV1], and peak expiratory flow rate [PEFR] were measured. Data were taken at the start and after 4 weeks in both groups.
Results:
Independent t-test showed no significant differences in the cardiorespiratory functions between the experimental and control groups among the male and female participants, except for the females’ PEFR which showed small differences. On the other hand, repeated measure ANOVA shows significant improvement in the experimental groups among males (P < 0.001–0.028) and females (P < 0.001–0.001) in all the cardiorespiratory functions measured, except for the FEV1 and PEFR among males.
Conclusion:
The results of this study suggest that cardiorespiratory functions were improved after breathing exercise, and therefore, ANB can be recommended for increasing cardiorespiratory efficiency.
Keywords: Alternate nostril breathing exercise, alternate nostril breathing, cardiorespiratory functions, Chittagong Medical College, healthy young adults, Exercice de respiration nasale alternée, respiration nasale alternée, fonctions cardiorespiratoires, Chittagong Medical College, jeunes adultes en bonne santé
Résumé
Introduction:
La respiration nasale alternée (ANB) est un exercice de respiration efficace avec des avantages thérapeutiques sur les fonctions cardiorespiratoires pour les individus sains et malades. Cette étude a été menée pour évaluer les effets de l’exercice ANB sur les tâches cardiorespiratoires chez des adultes en bonne santé.
Matériels et méthodes:
Cette étude expérimentale randomisée a été menée au Département de physiologie, Chittagong Medical College, Chattogram, de juillet 2017 à juin 2018. Un total de 100 étudiants de 1ère année, âgés de 18 à 20 ans, ont été inclus par un échantillonnage aléatoire. méthode. Cinquante participants (25 hommes et 25 femmes) ont été inscrits dans le groupe expérimental, tandis que l’âge et l’indice de masse corporelle correspondaient à 50 autres participants (25 hommes et 25 femmes) servant de groupe témoin. Les participants du groupe expérimental ont effectué des exercices ANB pendant 4 semaines. Les paramètres cardiorespiratoires (fréquence du pouls, pression artérielle, capacité vitale forcée, volume expiratoire forcé en 1ère s [VEMS] et débit expiratoire de pointe [PEFR] ont été mesurés. Les données ont été recueillies au début et après 4 semaines dans les deux groupes.
Résultats:
Le test t indépendant n’a montré aucune différence significative dans les fonctions cardiorespiratoires entre les groupes expérimentaux et témoins parmi les participants masculins et féminins, à l’exception du PEFR des femmes qui présentait de petites différences. D’autre part, l’ANOVA à mesures répétées montre une amélioration significative dans les groupes expérimentaux chez les hommes (P < 0,001 à 0,028) et les femmes (P < 0,001 à 0,001) dans toutes les fonctions cardiorespiratoires mesurées, à l’exception du VEMS et du DEP chez les hommes
Conclusion:
Les résultats de cette étude suggèrent que les fonctions cardiorespiratoires ont été améliorées après un exercice respiratoire, et par conséquent, l’ANB peut être recommandé pour augmenter l’efficacité cardiorespiratoire.
INTRODUCTION
Proper diet, adequate exercise, and a stress-free life are vital components of maintaining physical and mental well-being.[1] Rapid industrialization, environmental pollution, overcrowding, and sedentary lifestyle are responsible for the deterioration of an individual health status.[2] The WHO predicts that physical or mental stress will become the second leading cause of disability and cardiovascular morbidity by 2020.[3] Currently, obesity and various stress-related factors are responsible for ill health.[2] Due to abrupt changes in professional, personal, social, and educational lifestyles, the prevalence of stress-related diseases such as obesity, diabetes, hypertension (HTN), ischemic heart disease, angina, and myocardial infarction have also become prevalent.[4] Atmospheric pollution is also responsible for various types of respiratory diseases.[1] Dust allergy, common cold with cough, chronic obstructive pulmonary disease (COPD), bronchial asthma, and status asthmaticus are common diseases in recent times, especially in urban areas.[1] In Bangladesh, approximately 20% of the adult population are suffering from HTN, 11.4% from COPD residing in urban areas for 35 years or more, and 6.8% from bronchial asthma in the coastal region.[5,6,7]
Both physical health and mental health depend on cardiorespiratory endurance.[8] Some unique and specific techniques are required to improve our physical and mental abilities in everyday life.[2] Preventive and curative health in medical science is essential to achieve optimum physical and psychological fitness.[7] Among all the autonomic functions of our body, the breathing function that can be consciously controlled[8] is widely admired as a useful technique to enhance the human body's mental and physical strength.[9] It also provides oxygen and expires out carbon dioxide and other toxic gaseous substances from the body.[9] Controlled breathing can help turn the sympathetic and parasympathetic functions into a harmonic state.[10]
In earlier studies, it was found that alternate nostril breathing (ANB) modulated sympathovagal balance with improved respiratory function.[4,10,11,12] It also relieved stress and refined metabolism.[13,14,15,16,17,18,19,20,21,22] It also enhanced cognitive function[13,23,24,25] and attenuation of the physiological aging process.[26,27] Breathing exercises (Pranayama) are a common term used in Yoga.[12] Yoga is a psycho–somatic–spiritual discipline for achieving union and harmony between the mind, body, and soul.[2] Regular Yoga practice is a perfect exercise for maintaining proper health of all ages.[28] It is beneficial for the prevention, control, and rehabilitation of many diseases.[28] Yoga consists of prayer, Asanas, Pranayama, and meditation.[8,9,29,30] It is widely practiced in the Indian subcontinent over thousands of years.[12] It is gaining importance and becoming increasingly acceptable in the Western society.[31,32] June 21 was declared as “International Yoga Day” by the United Nations General Assembly in 2015.[33] Different types of breathing exercises are practiced in Yoga.[9] Deep breathing, inhalation–retention–exhalation at fixed intervals, abdominal/diaphragmatic breathing, and ANB/anuloma viloma were practiced in different studies.[9] Among these breathing exercises, ANB is one of the most comfortable and cost-effective breathing exercises that does not require any special equipment or extra time investment.[11] It refreshes the body as well as mind and promotes health and fitness.[2,11]
ANB produces consistent positive physiological changes and has a sound scientific basis for their beneficial human body outcomes.[8] In ANB exercise, slow inhalation followed by slow exhalation of air through one nostril is practiced. Individual need to close alternate nose, and holds breathing for a brief period between inhalation and exhalation.[34] Different studies observed that beneficial effects of breathing exercise are diseased as well as normal healthy subjects.[9,10,35,36,37,38,39,40] Eighteen percent improvement of O2 consumption was observed after a 1-month ANB exercise.[16] Significantly increased VO2 max (maximal oxygen uptake) and basal metabolic rate were found after deep breathing exercise in healthy participants and medical students.[8,17]
The burden of the medical curriculum imposes extreme study stress on medical students.[4,40] Continuous stress can cause irritability, insomnia, anxiety, and depression.[4] Stress also changes the sympathovagal balance due to change in the hypothalamic–pituitary axis set point.[10] It causes harmful effects on heart rate (HR), blood pressure (BP), and respiratory rate (RR), leading to cardiorespiratory disease formation.[10] Several studies revealed that deep breathing exercise significantly decreased salivary cortisol concentration and decreased BP, necessary for a stress-free life.[13,14] Deep breathing exercise is neuroprotective that increases skills, and memory decreases anxiety and improves cognitive functions.[23,24,25] Blood glucose level was significantly reduced after practicing Pranayama for days to weeks in medical students and diabetic patients.[14,18,19] It might be due to increased sensitivity of β-cells of the pancreas to glucose, increased insulin sensitivity to tissue, or decreased insulin resistance with increasing peripheral utilization of glucose.[14,18,19]
Significant improvement in the lipid profile was observed after Pranayama in healthy volunteers and Type 2 diabetic patients with dyslipidemia.[20,21,22] It might be due to the hydrolysis of triglyceride by relieving stress.[20,21,22] Breathing exercise has beneficial effects on aging, cell death, and stress regulation through transcriptional regulation.[27] In some previous studies, it was found that antioxidants such as glutathione, glutathione peroxidase, and superoxide dismutase were higher in the breathing exercise group.[27]
Central and peripheral chemoreceptors become adapted to anoxia and acclimatized to hypercapnia by practicing breath-holding exercises.[41] Significant improvements were found in breath holding time (BHT), forced expiratory volume in 1st s (FEV1)/forced vital capacity (FVC)%, and tidal volume among medical students after breathing exercise.[41,42] It was supposed that increased BHT was due to the predominance of parasympathetic over sympathetic tone.[41,42] RR was found unaltered or decreased in some studies.[12,39] Respiratory muscles undergo work hypertrophy with maximum functioning during the breathing exercise.[9,42] A statistically significant improvement was observed in FVC, FEV1, maximum expiratory pressure, maximum inspiratory pressure, peak expiratory flow rate (PEFR), and expiratory reserve volume (ERV) among healthy young subjects and also in healthy medical students.[9,12,39,41] In one study, on status asthmaticus, breathing exercise relieved bronchoconstriction.[1] It improved lung capacity.[1] FVC, FEV1, inspiratory reserve volume, and maximum voluntary ventilation were significantly improved. Although low vital capacity (SVC) and ERV were improved, it was nonsignificant.[1]
Marked improvement in the lung functions after ANB was observed among asthmatic and COPD patients.[37,38] Several studies showed the decreased frequency of attacks, less use of drugs, and improvement in diffusing capacity indicated by the transfer factor of the lung for carbon monoxide.[29,43] COPD assessment test score was increased in COPD patients after breathing exercise.[44] Breathing exercise reduced HR and BP significantly in healthy subjects and hypertensive and ischemic heart disease in patients.[4,10,40,45] During breathing exercise, full attention on the breathing helped to feel relaxed from stress.[10,30,35,45] It resets the autonomic nervous system with decreased adrenalin-mediated sympathetic activity and peripheral resistance.[10,30,35,36,45] Due to vasodilation, HR and BP might be reduced in those cases.[10,30,35,45] ANB can be used effectively for preventive and therapeutic purposes, either alone or in addition to therapy.[2] Considering ANB practice as an integral part of our daily routine may help in conditioning the cardiorespiratory system in life.[2] Therefore, onset and progression of diseases, such as asthma, COPD, and HTN, may be prevented in later life stages.[2] This study aimed to assess the physiological effects of short-term ANB exercise on cardiorespiratory function in healthy adult individuals in stressful conditions. As medical students lead a stressful study life, this study mainly focused on medical students to observe the effects of breathing exercises on the cardiorespiratory system.
MATERIALS AND METHODS
Study design
This research work was a randomized experimental study. It was conducted in the Department of Physiology, Chittagong Medical College (CMC), Chattogram, Bangladesh, from July 2017 to June 2018.
Study sample
A total of 100 research participants (RPs) were recruited in this study, where 50 of them (25 males and 25 females) were allocated to be in the control group, and the other 50 participants (25 males and 25 females) belonged to the experimental group by the lottery method. RPs were the 1st-year medical students of CMC, aged between 18 and 20 years, having the body mass index (BMI) of 18.5–22.9 kg/m2, fulfilling the inclusion and exclusion criteria. They enrolled in the study with informed consent.
Sampling method
Simple random sampling by lottery method was adopted to select all the RPs.
Study period
The study period was from July 2017 to June 2018.
Study area
The study was conducted at the Department of Physiology, CMC, Chattogram, Bangladesh.
Inclusion criteria
The 1st-year medical students aged between 18 and 20 years, having a BMI of 18.5–22.9 kg/m2 of CMC, Chattogram, were enrolled in the study with their informed consent. Detailed personal information, medical and family history, and physical activity status history were recorded in a prefixed questionnaire from all the RPs who participated voluntarily. The RPs who never performed breathing exercises before were randomly selected.
Exclusion criteria
The previous history of cardiovascular, respiratory illness, having any nasal pathology, smokers, receiving respiratory depressant drugs, and vertebral deformities were excluded from the study.
Project details
Age, height, and body weight of the RPs were recorded in a predesigned case record form. BMI was calculated by the formula, BMI = weight in kg/height in m2. Cardiorespiratory parameters (pulse, systolic blood pressure [SBP], diastolic blood pressure [DBP], FVC, FEV1, and PEFR) of the RPs were recorded in an upright sitting posture before commencing breathing exercises to note the baseline parameters in both the control and experimental groups. Radial pulse was counted for a minute keeping the RP's forearm slightly pronated. SBP and DBP were measured in the sitting position by a palpatory and auscultatory method with the help of a stethoscope and aneroid sphygmomanometer after proper exposure (ALPK2 aneroid sphygmomanometer, Japan). RPs were asked to remain in sitting posture for 15 min to become mentally and physically relaxed and free from excitation and anticipation. Three consecutive readings for a pulse and BP measurement procedures were taken, and the best value was recorded. The measured predicted and percentage of predicted values of FVC, FEV1, and PEFR were recorded from the digital spirometer monitor (Chest graph, HI-101, Japan). Three consecutive readings were taken, and the best value was noted on tracing paper. Then, the experimental group practiced ANB exercise [Figure 1] daily for 10 min for 4 weeks. After 4 weeks, the cardiorespiratory parameters were again measured in both the control and experimental groups.
Figure 1.
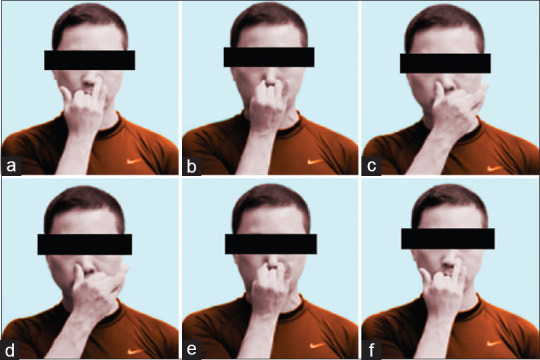
Steps of alternate nostril breathing exercise (a) The subjects were asked to close the left nostril with the left hand's finger and inhale through the right nose for 6 s. (b) Then, they closed the right nostril by the index finger and held the breath for 6 s. (c) Then, they exhaled through the left nostril slowly for 6 s. (d) Then, they inhaled through the left nose, keeping the right nostril closed for 6 s. (e) Then, the subjects hold the breath, closing both nostrils for 6 s. (f) Then, they exhaled through the right nose, keeping the left closed for 6 s
Data collection details
Detailed personal information, medical and family history, and the history of physical activity status were recorded in a prefixed questionnaire from all the RPs who participated voluntarily.
Statistical analysis
The data were entered into an Excel file, which then transferred into SPSS software (IBM SPSS Statistics for Windows, Version 23.0. Armonk, NY, USA: IBM Corp.) for further analysis. All the data were in the numerical form. Hence, the mean and standard deviation were used to describe the variables. The interaction term of the repeated measure (RM) ANOVA was used to assess the effectiveness of ANB, i.e., in comparing the changes in the cardiorespiratory functions before and after the intervention between the experimental and the control groups. The analysis was carried out separately for male and female participants after comparing the baseline measures between the experimental and control groups using an independent t-test to ensure their comparability. The statistical tests’ assumptions were checked to confirm the test results’ validity, such as the normality and homogeneity of variances assumptions. The significance level was set at 0.05 for all the statistical tests used.
Ethical approval
The protocol of this study was approved by the members of the ethical review board (ERB) of CMC, Chattogram, and received a certificate of ethical clearance of ERB (Reference No.: CMC/PG/2018/403 dated May 10, 2018).
RESULTS
An independent t-test was used to compare the baseline measured cardiorespiratory functions between the experimental and control groups. There were 25 males and 25 females in each control and experimental group. The results are illustrated in Table 1, where it can be seen that there are no significant differences in all the baseline measures between the experimental and control groups of male and female participants, except for PEFR in female participants. However, the difference observed was quite small, and this will be taken care of in the RM ANOVA in comparing the changes between the before and after intervention measurements later.
Table 1.
Comparing the baseline cardio-respiratory functions between the experimental and control groups among the male and female participants using an independent t-test
| Variables (unit of measurement) | Mean (SD) | t-statistics (df) | P | |
|---|---|---|---|---|
|
| ||||
| Experimental group (n=25) | Control group (n=25) | |||
| Male | ||||
| Age (years) | 19.1 (0.73) | 19.1 (0.67) | <0.001 (48) | 1.000 |
| BMI (kg/m2) | 21.14 (1.475) | 20.85 (1.224) | 0.772 (48) | 0.444 |
| Pulsea (beat/min) | 79.1 (1.54) | 78.3 (1.38) | 1.940 (48) | 0.058 |
| SBP (mmHg) | 116.4 (4.90) | 116.4 (4.90) | <0.001 (48) | 1.000 |
| DBP (mmHg) | 74.4 (5.07) | 75.6 (5.83) | −0.777 (48) | 0.441 |
| FVC (L) | 3.365 (0.5003) | 3.456 (0.4997) | −0.648 (48) | 0.520 |
| FEV1 (L) | 3.231 (0.4675) | 3.313 (0.4069) | −0.665 (48) | 0.509 |
| PEFR (L/s) | 7.229 (1.4221) | 7.004 (1.4357) | 0.557 (48) | 0.580 |
| Female | ||||
| Age (years) | 18.6 (0.70) | 19.0 (0.68) | −1.644 (48) | 0.107 |
| BMI (kg/m2) | 20.71 (1.654) | 20.92 (1.561) | −0.457 (48) | 0.650 |
| Pulsea (beat/min) | 78.7 (2.23) | 78.7 (2.30) | <0.001 (48) | 1.000 |
| SBP (mmHg) | 115.2 (5.10) | 115.2 (5.10) | <0.001 (48) | 1.000 |
| DBPb (mmHg) | 74.0 (7.07) | 74.4 (5.07) | −0.230 (43.5) | 0.819 |
| FVC (L) | 2.387 (0.2512) | 2.543 (0.3667) | −1.760 (48) | 0.085 |
| FEV1 (L) | 2.369 (0.2591) | 2.528 (0.3611) | −0.786 (48) | 0.080 |
| PEFR (L/s) | 5.628 (0.6496) | 6.126 (0.7998) | −2.419 (48) | 0.019 |
aHR, bHomegeneity of variances was not assumed. SD=Standard deviation, df=Degree of freedom, BMI=Body mass index, SBP=Systolic blood pressure, DBP=Diastolic blood pressure, FVC=Forced vital capacity, FEV1=Forced expiratory volume in 1 s, PEFR=Peak expiratory flow rate, HR=Heart rate
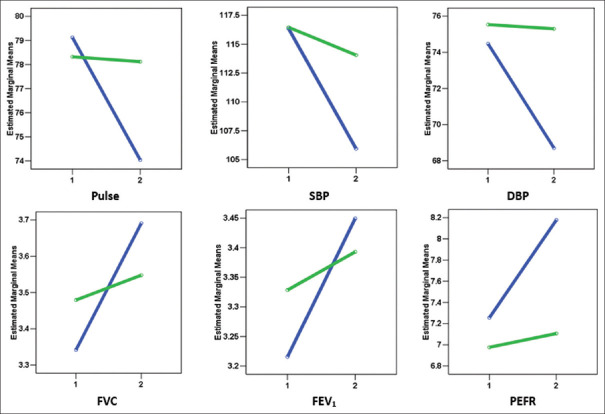
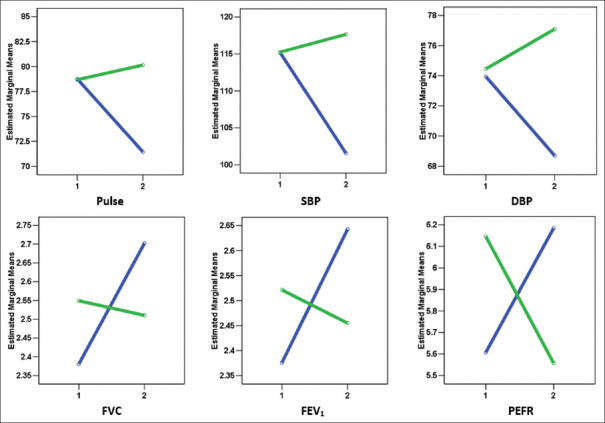
RM ANOVA was used to assess the effectiveness of ANB on the cardiorespiratory functions among male and female healthy adults in this study. The multivariate interaction terms of RM ANOVA showed that there were significant changes on at least one of the cardiorespiratory functions of before and after intervention in comparing between the experimental and control groups among males [F (6, 41) = 7.179, P < 0.001] and among females [F (6, 41) =25.455, P < 0.001] after adjusting for the effect of age and BMI. The results of univariate RM ANOVA post hoc tests summarized in Table 2 show that the significant changes were observed in all the cardiorespiratory functions among males (P < 0.001–0.028) and females (P < 0.001–0.001), except for FEV1 (P = 0.094) and PEFR (P = 0.082) among males. It can further be seen from Figure 2 for males and Figure 3 for females that there was more reduction in all the cardiac functions (pulse, SBP, and DBP) and more increment in all the respiratory functions (FVC, FEV1, and PEFR) of the experimental group as compared to the control group, though as mentioned above, the differences were not statistically significant for FEV1 and PEFR among males which could be due to the low power of the study in those comparisons.
Table 2.
The univariate repeated measures ANOVA in comparing the changes in the cardiorespiratory functions postalternate nostril breathing exercise between the experimental and control groups among male and female participants
| Variables | Estimated marginal meana (95% CI) | P | |||
|---|---|---|---|---|---|
|
| |||||
| The experimental group (n=25) | Control group (n=25) | ||||
|
|
|
||||
| Before | After | Before | After | ||
| Males | |||||
| Pulseb (beat/min) | 79.1 (78.5, 79.7) | 74.0 (72.5, 75.6) | 78.3 (77.7, 78.9) | 78.1 (76.6, 79.7) | <0.001 |
| SBP (mmHg) | 116.3 (114.3, 118.3) | 105.9 (103.4, 108.5) | 116.6 (114.5, 118.3) | 114.1 (111.5, 116.6) | <0.001 |
| DBP (mmHg) | 74.5 (72.3, 76.7) | 68.7 (65.9, 71.5) | 75.5 (73.3, 77.7) | 75.3 (72.5, 78.1) | 0.028 |
| FVC (L) | 3.342 (3.156, 3.528) | 3.691 (3.526, 3.856) | 3.479 (3.293, 3.665) | 3.548 (3.383, 3.712) | 0.008 |
| FEV1 (L) | 3.216 (3.050, 3.381) | 3.449 (3.297, 3.602) | 3.328 (3.163, 3.494) | 3.393 (3.241, 3.545) | 0.094 |
| PEFR (L/s) | 7.256 (6.675, 7.837) | 8.178 (7.559, 8.796) | 6.976 (6.396, 7.557) | 7.106 (6.488, 7.725) | 0.082 |
| Females | |||||
| Pulseb (beat/min) | 78.8 (77.8, 79.7) | 71.5 (70.0, 72.9) | 78.7 (77.7, 79.6) | 80.1 (78.7, 81.6) | <0.001 |
| SBP (mmHg) | 115.1 (113.1, 117.2) | 101.6 (98.7. 104.4) | 115.2 (113.2, 117.3) | 117.6 (114.8, 120.5) | <0.001 |
| DBP (mmHg) | 73.9 (71.4, 76.4) | 68.7 (66.5, 70.9) | 74.5 (72.0, 77.0) | 77.1 (74.9, 79.3) | <0.001 |
| FVC (L) | 2.381 (2.252, 2.509) | 2,702 (2.566, 2.838) | 2.549 (2.421, 2.678) | 2.510 (2.374, 2.647) | 0.001 |
| FEV1 (L) | 2.376 (2.246, 2.505) | 2.643 (2.513, 2.772) | 2.521 (2.392, 2.651) | 2.455 (2.326, 2.585) | 0.001 |
| PEFR (L/s) | 5.607 (5.308, 5.906) | 6.185 (5.932, 6.438) | 6.147 (5.848, 6.446) | 5.557 (5.304, 5.810) | <0.001 |
aAdjusted for age and BMI, bHR. SBP=Systolic blood pressure, DBP=Diastolic blood pressure, FVC=Forced vital capacity, FEV1=Forced expiratory volume in 1 s, PEFR=Peak expiratory flow rate, CI=Confidence interval, HR=Heart rate, BMI=Body mass index
Figure 2.
Comparing the changes in cardiorespiratory functions* before (1) and after (2) alternate nostril breathing exercise between the experimental (blue lines) and control (green lines) groups among male participants (n = 25 in each group). *(Pulse [beat per minute], systolic blood pressure [mmHg], diastolic blood pressure [mmHg], forced vital capacity [L], forced expiratory volume in 1st s [L], peak expiratory flow rate [L/s])
Figure 3.
Comparing the changes in cardiorespiratory functions* before (1) and after (2) alternate nostril breathing exercise between the experimental (blue lines) and control (green lines) groups among female participants (n = 25 in each group). *(Pulse [beat per minute], systolic blood pressure [mmHg], diastolic blood pressure [mmHg], forced vital capacity [L], forced expiratory volume in 1st s [L], peak expiratory flow rate [L/s])
DISCUSSION
A comparison between male and female study groups was made in this study. It was observed that there was a significant reduction in cardiac parameters and increment of respiratory parameters in the case of males and females at the end of 1 month of breathing exercise. This research assessed by comparing cardiorespiratory functions in the experimental group before and after adopting ANB exercises for 4 weeks. Additionally, pulse, SBP, DBP, FVC, FEV1, and PEFR value where compared with control group.
The control group of the current study did not practice breathing exercises. The baseline values in males and females regarding pulse, SBP, DBP, FVC, FEV1, and PEFR did not significantly change the experimental group. This finding is consistent with some previous studies where a significant change in cardiorespiratory parameters in both sexes’ control groups was not evident.[9,37,38]
In the experimental group, cardiac parameters (pulse rate, SBP, and DBP) before and after ANB for 1 month were significantly decreased among males and females. Previous investigators also reported similar findings.[2,4,10,30,34,40,45,46,47,48,49,50] Findings of this study were identical with the conclusions from Biswas et al. in 2014, Pal et al. in 2014, and other investigators.[2,4,10,30,34,40,45,46,47,48,49,50] They supposed that breathing exercise might activate the vasomotor center which ultimately increase parasympathetic activity and decrease the sympathetic activity.[2,4] This might cause a decrease in pulse rate and BP.[2,4]
During breathing exercises, attention to breathing removes attention from worldly worries and de-stress a person.[44,51] This may decrease adrenaline release and decrease BP, which was explained by Gupta et al. in 2014 and Upadhyay-Dhungel et al. in 2013.[44,51] Breathing exercise alters the hypothalamic discharge, leading to a decrease in sympathetic tone and peripheral resistance and an increase in venous return. Hence, the DBP was decreased. Increase vagal tone reduces the workload on the heart and thus decreases cardiac output (CO) and hence SBP.[44] Regular practice of slow rhythmic breathing has increased baroreflex sensitivity activation with reduction of chemoreflex activation and thus reduces SBP and DBP in hypertensive patients.[52] Possibly, the above mechanisms were also responsible for loosening the cardiac parameters in this study. Some investigators found no significant SBP and DBP changes after breathing exercise, unlike the current research.[53] It was supposed that their study subjects were normotensive and due to the short period of study.[53]
In the experimental group, who practiced ANB exercise for 1 month, the mean values of FVC, FEV1, and PEFR significantly increased from their baseline values supporting other study results.[2,9,11,12,28,39,40,41,42,44,46,47,48,49,54,55,56,57,58,59,60,61] They found that FVC might be increased due to the strengthening of respiratory muscles by regular practicing breathing exercises.[2,54,55,56] This act trains the respiratory apparatus to get emptied and filled more completely and efficiently.[62] FEV1 might be increased due to removing secretions from the bronchial tree, which made room in the alveoli for more air after breathing exercise.[63] Increased PEFR was due to more lung alveoli involvement during breathing exercise, dormant before the workout.[44,47,64] According to Joshi et al. in 1992 and Ankad et al. in 2011, PEFR was supposed to increase by increased release of lung surfactant and prostaglandins, which reflexively relaxes the smooth muscle of the larynx and tracheobronchial tree. Thus, modulating the airways’ caliber and reduced airway resistance were the causal factors for increased PEFR in their study.[54,65] Stimulation of pulmonary stretch receptors due to maximum inflation of the lungs reflexly relaxes smooth muscles of larynx and tracheobronchial tree, and hence, PEFR was increased.[65] Surfactant reduces the surface tension, thereby, promotes exchange of gases in the alveolar membrane, and enhances the oxygen carrying capacity of the red blood cells.[66] Multiple studies reported that increment in thoracopulmonary compliance and bronchodilatation by breathing exercise might be responsible for increased PEFR in previous studies.[32,46,48] In this study, respiratory functions improved after 1 month might be due to the causes, as mentioned earlier. Some investigators found only marginal improvement in FVC and FEV1 after Pranayama training, unlike our study findings.[61,67] They explained that it might be due to short research conducted on normal healthy subjects.[61,67]
ANB exercise manifested a significant decrement in cardiac parameters (pulse, SBP, and DBP) while substantial improvement in respiratory parameters (FVC, FEV1, and PEFR) in the experimental group of medical students. Therefore, ANB tends to play a significant role in improving cardiorespiratory function and preventing different cardiorespiratory complications.
CONCLUSION
In the present study, Yoga-based ANB exercise for 1 month brought significant improvement in cardiorespiratory parameters (pulse, SBP, DBP, FVC, FEV1, and PEFR) in the study subjects. Although it is difficult to explain the underlying mechanism involved for such improvements, the shifting of sympathovagal balance toward parasympathetic predominance may play a role. From the results of this study, it appears likely that the regular performance of ANB can be a useful measure for the improvement of cardiorespiratory endurance and functions. Such breathing practices may help in reducing the evolvement of cardiopulmonary complications. Since no instrument is necessary, and it is a straightforward and cost-effective practice to adopt, promoting this maneuver will improve health and well-being.
Limitations of the study
The comparatively shorter period for conducting this prospective intervention study and smaller sample size based on medical students of a specific age group enrolled first limit the findings’ representative criteria. Sociodemographic factors were not assessed in the study. Furthermore, appropriate sitting posture on the floor mat might not be maintained in all cases. Moreover, the catecholamine level in blood and urinary excretion was not measured to examine stress patterns.
Financial support and sponsorship
This study obtain no financial support.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors acknowledge the support of the Department of Physiology, CMC, Chattogram during sample collection and laboratory instrument uses. The authors are also thankful to the study subjects for their active, sincere, and voluntary participation.
REFERENCES
- 1.Sharma KK, Udayakumara K, Thirmaleshwara PH, Ajithesha NH. Effect of yoga therapy on lung functions in respiratory disorder subjects. Eur Sci J. 2014;10:102–8. [Google Scholar]
- 2.Biswas S, Biswas P, Sayyad R, Eliyaraju A, Yadav PK, Kar SK. Effect of forty days of pranayama training on cardiorespiratory parameters. Indian J Basic Appl Med Res. 2014;3:196–202. [Google Scholar]
- 3.Murray, Christopher J. L, Lopez, Alan D. Christopher J. L, Murray, Alan D, Lopez, editors. World Health Organization, World Bank & Harvard School of Public Health. (1996). The Global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020: summary. World Health Organization. https://apps.who.int/iris/handle/10665/41864 .
- 4.Pal GK, Agarwal A, Karthik S, Pal P, Nanda N. Slow yogic breathing through right and left nostril influences sympathovagal balance, heart rate variability, and cardiovascular risks in young adults. N Am J Med Sci. 2014;6:145–51. doi: 10.4103/1947-2714.128477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koly KN, Biswas T, Islam A. Increasing prevalence of hypertension in Bangladesh: A review. Cardiovasc J. 2015;8:59–64. [Google Scholar]
- 6.Alam DS, Chowdhury MA, Siddiquee AT, Ahmed S, Clemens JD. Prevalence and determinants of Chronic Obstructive Pulmonary Disease (COPD) in Bangladesh. COPD. 2015;2:1–11. doi: 10.3109/15412555.2015.1041101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hassan MR, Bennoor KS, Rahman F, Kabir AR, Mahmud AM, Haque ME, et al. Prevalence of asthma in highly polluted Dhaka city and low polluted coastal area of Bangladesh. Indian J Allergy Asthma Immun. 2005;19:85–92. [Google Scholar]
- 8.Doijad VP, Kamble P, Surdi AD. Effect of yogic exercises on aerobic capacity. Int J Recent Trend Tech. 2013;6:119–21. [Google Scholar]
- 9.Yadav RK, Das S. Effect of yogic practice on pulmonary functions in young females. Indian J Physiol Pharmacol. 2001;45:493–6. [PubMed] [Google Scholar]
- 10.Chethan K, Devaraju MR. A study on the effect of Nadi-Shodhana Pranayama on cardiac parameters. Indian J Basic Appl Med Res. 2016;6:484–7. [Google Scholar]
- 11.Bal BS. Impact of short-term training of Anulom Vilom (Alternate nostril breathing) on respiratory parameters. Am J Sports Sci Med. 2015;3:9–14. [Google Scholar]
- 12.Chakraborti T, Das K, Samajdar K. Effect of yogic exercise on selected pulmonary function tests in apparently healthy elderly subjects. IOSR J Dent Med Sci. 2013;9:1–5. [Google Scholar]
- 13.Ma X, Yue ZQ, Gong ZQ, Zhang H, Duan NY, Shi YT, et al. The effect of diaphragmatic breathing on attention, negative affect and stress in healthy adults. Front Psychol. 2017;8:874. doi: 10.3389/fpsyg.2017.00874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Singh S, Katwal B, Panta PP. Slow and deep breathing exercise (Pranayama) for a stress-free life amongst medical students. Int J Res Rev. 2017;4:67–72. [Google Scholar]
- 15.Naik GS, Gaur GS, Pal GK. Effect of modified slow breathing exercise on perceived stress and basal cardiovascular parameters. Int J Yoga. 2018;11:1–4. doi: 10.4103/ijoy.IJOY_41_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Telles S, Nagarathna R, Nagendra HR. Breathing through a particular nostril can alter metabolism and autonomic activities. Indian J Physiol Pharmacol. 1994;38:133–7. [PubMed] [Google Scholar]
- 17.Yong MS, Lee YS, Lee HY. Effects of breathing exercises on resting metabolic rate and maximal oxygen uptake. J Phys Ther Sci. 2018;30:1173–5. doi: 10.1589/jpts.30.1173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shende V, Waghmore S, Pawar S, Kashalikar S. Effect of pranayama on blood glucose level in medical students: A case-control study. Int J Res Health Sci. 2013;1:209–12. [Google Scholar]
- 19.Manjunatha S, Vempati RP, Ghosh D, Bijlani RL. An investigation into the acute and long-term effects of selected yogic postures on fasting and postprandial glycemia and insulinemia in healthy young subjects. Indian J Physiol Pharmacol. 2005;49:319–24. [PubMed] [Google Scholar]
- 20.Surendra BV, Hariprasad T. Effect of pranayama and yogasanas on lipid profile in normal healthy volunteers. Int J Clin Biomed Res. 2016;2:13–6. [Google Scholar]
- 21.Chanda R, Sanjjev R, Rahul V, Mahapatra SP. Biochemical modulation in regular practice of yoga in young healthy medical students. World J Pharm Pharma Sci. 2017;6:617–28. [Google Scholar]
- 22.Shantakumari N, Sequeira S, El Deeb R. Effects of a yoga intervention on lipid profiles of diabetes patients with dyslipidemia. Indian Heart J. 2013;65:127–31. doi: 10.1016/j.ihj.2013.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Villemure C, Čeko M, Cotton VA, Bushnell MC. Neuroprotective effects of yoga practice: Age-, experience-, and frequency-dependent plasticity. Front Hum Neurosci. 2015;9:1–2. doi: 10.3389/fnhum.2015.00281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Subramanya P, Telles S. Effect of two yoga-based relaxation techniques on memory scores and state anxiety. Biopsychosoc Med. 2009;1:1–5. doi: 10.1186/1751-0759-3-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yadav G, Mutha PK. Deep breathing practice facilitates retention of newly learned motor skills. Sci Rep. 2016;1:1–8. doi: 10.1038/srep37069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Berri K. Breathing to younger skin: ‘Reversing the molecular mechanism of skin aging with yoga’. Future Sci OA. 2016;2:10–24. doi: 10.4155/fsoa-2016-0015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sharma H, Datta P, Singh A, Sen S, Bhardwaj NK, Kochupillai V, et al. Gene expression profiling in practitioners of Sudarshan Kriya. J Psychosom Res. 2008;64:213–8. doi: 10.1016/j.jpsychores.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 28.Doijad VP, Surdi AD. Effect of short-term yoga practice on pulmonary function tests. Indian J Basic Appl Med Res. 2012;3:226–30. [Google Scholar]
- 29.Soni R, Munish K, Singh K, Singh S. Study of the effect of yoga training on diffusion capacity in chronic obstructive pulmonary disease patients: A controlled trial. Int J Yoga. 2012;5:123–7. doi: 10.4103/0973-6131.98230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chintamoni DB, Bhave SN, Jankar DS. Effects of short-term pranayama on certain cardiovascular risk factors. Int J Biomed Res. 2015;6:83–6. [Google Scholar]
- 31.Subhalakshmi NK, Saxena SK, Urmimala S, Urban JA. Immediate effect of nadishodhana pranayama on some selected parameters of cardiovascular, pulmonary, and higher functions of brain. Thai J Phys Sci. 2005;18:10–6. [Google Scholar]
- 32.Kurmur KA, Joshi VS, Maulik S, Padlia JL, Sarvaiya JL. Effect of ten weeks’ yoga practice on pulmonary function tests. Int J Biomed Adv Res. 2015;6:682–5. [Google Scholar]
- 33.Agarwal D, Gupta PP, Sood S. Assessment for efficacy of additional breathing exercises over improvement in health impairment due to asthma assessment using St.George's respiratory questionnaire. Int J Yoga. 2017;10:145–51. doi: 10.4103/0973-6131.213472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pal GK, Velkumary S, Madanmohan Effect of short-term practice of breathing exercises on autonomic functions in normal human volunteers. Indian J Med Res. 2004;120:115–21. [PubMed] [Google Scholar]
- 35.Yadav RC. Effects of twelve weeks selected pranayama practice on primary high blood pressure patients. Eur J Pharm Med Res. 2016;3:471–4. [Google Scholar]
- 36.Satayanand V, Reddy B, Lilly N, Mahaboobvali S, Mohan D, Salma S, et al. Effect of yoga on hypertension. Narayana Med J. 2016;5:4–11. [Google Scholar]
- 37.Satyanand V, Kumar GP, Ram NB, Mohanan D, Basha SA, Kumari BP. Study effect of two breathing techniques on pulmonary function in asthma. Int J Biomed Adv Res. 2014;5:510–12. [Google Scholar]
- 38.Candy S, Singh S, Dandona PK. Study of the effect of yoga training on pulmonary functions in patients with bronchial asthma. Indian J Physiol Pharmacol. 2009;53:169–74. [PubMed] [Google Scholar]
- 39.Thirupathi C, Ananda SK. Effect of yoga exercise on pulmonary function in young medical students. Int J Med Res Health Sci. 2016;5:341–3. [Google Scholar]
- 40.Dhanvijay AD, Dhokne N, Choudhary AK, Kishanrao SS, Chandan L. Effects of alternate nostril breathing on cardiorespiratory variable in healthy young adults. Int J Pharmacy Biol Sci. 2015;6:1352–60. [Google Scholar]
- 41.Karthik S, Chandrashekhar M, Ambareesha S, Nikhil C. Effect of pranayama and suryanamaskar on pulmonary functions in medical students. J Clin Diag Res. 2014;8:4–6. doi: 10.7860/JCDR/2014/10281.5344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Makwana K, Khirwadkar N, Gupta HC. Effect of short-term yoga practice on ventilator function tests. Indian J Physiol Pharmacol. 1988;32:202–8. [PubMed] [Google Scholar]
- 43.Mekonnen D, Mossie A. Clinical effects of yoga on asthmatic patients: A preliminary clinical trial. Ethiop J Health Sci. 2010;20:107–12. [PMC free article] [PubMed] [Google Scholar]
- 44.Gupta A, Gupta R, Sood S, Akram M. Pranayama for treatment of chronic obstructive pulmonary disease: Results from a randomized controlled trial. Integrat Med. 2014;13:26–31. [PMC free article] [PubMed] [Google Scholar]
- 45.Satayanand V, Reddy B, Lilly N, Mahaboobvali S, Shaik AB, Aditya M. Studying the role of yogic pranayama in the management of blood pressure. Int J Biomed Adv Res. 2014;5:609–11. [Google Scholar]
- 46.Upadhyay Dhungel K, Malhotra V, Sarkar D, Prajapati R. Effect of alternate nostril breathing exercise on cardiorespiratory functions. Nepal Med Coll J. 2008;10:25–7. [PubMed] [Google Scholar]
- 47.Gupta V, Singh Y, Vikramaditya B, Singh H. Immediate effect of “Nadi-Shodhana Pranayam” on some selected parameters of cardiorespiratory and mental efficiency. J Current Trends Clin Med Lab Biochem. 2014;2:12–5. [Google Scholar]
- 48.Shrivastava RD, Nidhi J, Singhal A. Influence of alternate nostril breathing on cardiorespiratory and autonomic functions in healthy young adults. Indian J Physiol Pharmacol. 2005;49:475–83. [PubMed] [Google Scholar]
- 49.Singh S, Gaurav V, Parkash V. Effects of a 6 week nadi-shodhana pranayama training on cardio-pulmonary parameters. J Phys Educ Sport Manag. 2011;2:44–7. [Google Scholar]
- 50.Telles S, Yadav A, Kumar N, Sharma S, Visweshwaraiah NK, Balkrishna A. Blood pressure and Purdue pegboard scores in individuals with hypertension after alternate nostril breathing, breath awareness, and no intervention. Med Sci Monit. 2013;19:61–6. doi: 10.12659/MSM.883743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Upadhyay-Dhungel K, Sohal A. Physiology of nostril breathing exercises and its probable relation with nostril and cerebral dominance: A theoretical research on literature. Janaki Med Coll J Med Sci. 2013;1:38–47. [Google Scholar]
- 52.Isac S, Indu KM. Effectiveness of breathing exercises on hypertension among patients with chronic renal failure. Int J Med Health Profession Res. 2016;3:25–30. [Google Scholar]
- 53.Turankar AV, Jain S, Patel SB, Sinha SR, Joshi AD, Vallish BN, et al. Effects of slow breathing exercise on cardiovascular functions, pulmonary functions & galvanic skin resistance in healthy human volunteers – A pilot study. Indian J Med Res. 2013;137:916–21. [PMC free article] [PubMed] [Google Scholar]
- 54.Joshi LN, Joshi VD, Gokhale LV. Effect of short term ’Pranayam’ practice on breathing rate and ventilator functions of lung. Indian J Physiol Pharmacol. 1992;36:105–8. [PubMed] [Google Scholar]
- 55.Garg S, Chandla S. Effect of Nadi Shodhan pranayama on pulmonary functions. Int J Health Sci Res. 2016;6:192–6. [Google Scholar]
- 56.Shankarappa V, Prashanth P, Annamalai N, Varunmalhotra S. The short term effect of pranayama on the lung parameters. J Clin Diagnos Res. 2012;6:27–30. [Google Scholar]
- 57.Kumar K. Significance of nadi Sodhan and kapalbhati on forced ventilation capacity (FVC), maximum voluntary ventilation (MVV), and peak expiratory flow rate (PEFR) Indian J Tradit Knowl. 2013;12:342–5. [Google Scholar]
- 58.Bal SB. Effect of Anulom Vilom and bhastrika pranayama on the vital capacity and maximal ventilatory volume. J Physical Edu Sport Manag. 2010;1:11–5. [Google Scholar]
- 59.Panwar S, Chourishi A, Makwana J. Effect of pranayama (Yoga) on pulmonary function test of young, healthy students. Int J Pharmacy Biol Sci. 2012;3:12–6. [Google Scholar]
- 60.Madanmohan S, Jatiya L, Udupa K, Bhavani AB. Effect of yoga training on handgrip, respiratory Pressure, and pulmonary function. Indian J Physiol Pharmacol. 2003;47:387–92. [PubMed] [Google Scholar]
- 61.Dullo P, Vedi N, Gupta U. Improvement in respiratory functions after Alternate Nostril Breathing in healthy young adults. Pakistan J Physiol. 2008;4:102–15. [Google Scholar]
- 62.Karmur KA, Jani HA, Vala NH, Bhanderi PC. Effect of yoga on pulmonary function tests. Int J Res Med Sci. 2015;3:2357–61. [Google Scholar]
- 63.Surendra BV, Chidri SV. Impact of short term yogic practice over ventilator functions in healthy individuals. Int J Healthc Biomed Res. 2014;2:140–6. [Google Scholar]
- 64.Sivapriya DV, Suba-Malani S, Thirumeni S. Effect of nadi shodhana pranayama on respiratory parameters in school students. Rec Res Sci Tech. 2010;2:32–9. [Google Scholar]
- 65.Ankad RB, Ankad BS, Anita H, Shailaja P, Surekharani C, Shashikala GV. Effect of short term pranayama and meditation on respiratory parameters in healthy individuals. Int J Collabor Res Int Med Public Health. 2011;3:10–4. [Google Scholar]
- 66.Hakked CS, Balakrishnan R, Krishnamurthy MN. Yogic breathing practices improve lung functions of competitive young swimmers. J Ayurveda Integr Med. 2017;8:99–104. doi: 10.1016/j.jaim.2016.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Dinesh T, Gaur G, Sharma V, Madanmohan T, Harichandra Kumar K, Bhavanani A. Comparative effect of 12 weeks of slow and fast pranayama training on pulmonary function in young, healthy volunteers: A randomized controlled trial. Int J Yoga. 2015;8:22–6. doi: 10.4103/0973-6131.146051. [DOI] [PMC free article] [PubMed] [Google Scholar]