Abstract
Evidence for proximal risk factors for suicide is based on case–control psychological autopsy studies, with these reports showing that mood and substance use disorders are the most prevalent mental disorders among suicide decedents worldwide and are associated with marked risk. However, moderators of risk and the degree of risk associated with (nonalcohol) drug use disorder are unknown. A comprehensive search was used to identify 35 case–control psychological autopsy studies published worldwide over a 30-year period that were metaanalyzed using random effects models. Major depression, odds ratio (95% confidence interval) = 9.14 (5.53, 15.09), and drug use disorder, OR (95% CI) = 7.18 (3.22, 16.01), had large effect sizes, among other results. Risk estimates associated with major depression were greater in studies with a larger proportion of women and those conducted in Asia compared with other regions. There was no evidence of publication bias or that any one study had a disproportionate impact on findings. Risk for suicide associated with major depression appears to be moderated by sex and/or world region. Drug use disorder is a potent risk factor, illustrating the importance of assessing drug use in clinical risk assessment.
Worldwide, there are more than 800,000 suicide deaths annually, accounting for 50% of all violent deaths in men and 71% in women (World Health Organization, 2014). Although cohort studies have generated much of the evidence for distal risk factors for suicide (Franklin et al., 2017), data on proximal risk factors (i.e., present near time of death) is based primarily on case–control psychological autopsy studies. With this design, researchers interview proxy respondents of suicide decedents, most often family members, and gather comparable information on nonsuicide control subjects along with additional information obtained from records when available (e.g., medical records) for the purpose of making systematic comparisons between study groups (Conner et al., 2011, 2012).
Psychological autopsy research shows that mood disorders are the most common category of mental disorders among suicide decedents worldwide (Cavanagh, Carson, Sharpe, & Lawrie, 2003). Illustrating their central importance in suicide, a metaanalysis concluded that 26.3% of suicides in males and 31.6% in females are “attributable” to a mood disorder, highest among mental disorders, based on a formula that considers both the high prevalence of mood disorders among suicide decedents and the substantially higher likelihood of a mood disorder in suicide cases compared to nonsuicide controls (Li, Page, Martin, & Taylor, 2011). Alcohol or other drug use disorders are the second most common category of mental disorder among suicide decedents (Cavanagh et al., 2003). Prior metaanalyses of case–control psychological autopsy studies have generated pooled estimates of risk for suicide associated with mood disorders and alcohol or drug use disorders (Arsenault-Lapierre, Kim, & Turecki, 2004; Cavanagh et al., 2003; Yoshimasu, Kiyohara, & Miyashita, 2008), but numerous studies with large sample sizes from different regions of the world have been conducted since these reports were published. A more recent metaanalysis by Cho, Na, Cho, Im, and Kang (2016) served to update the literature, but the inclusion criteria required an estimate of risk for any mental disorder, serving to exclude more targeted papers, with implications for results (see Discussion).
As well, prior metaanalyses did not determine whether mood disorders and alcohol or drug use disorders confer differing levels of risk across populations. Along these lines, it is well-established that there are age, sex, and regional differences in the prevalence of mood disorders and alcohol or drug use disorders among suicide decedents, with females generally more likely to have mood disorders compared to males, younger individuals more likely to have alcohol or drug use disorders compared to older individuals (Qin, 2011), and suicide decedents in China showing lower prevalence of depression and alcohol or drug use disorders compared to Western populations (Phillips et al., 2002). Furthermore, the metaanalysis by Cho et al. (2016) examined age, sex, and regional differences in the presence of any mental disorder (but not mood or substance use disorder per se) among suicide cases. Although these reports are useful, they are limited by the examination of suicide cases only, with the potential that results merely reflect underlying population distributions of these disorders as opposed to moderating influences of age and so forth in suicide risk. Addressing this topic will require analysis of case–control data and formal tests of moderating effects, yet, with rare exception (e.g., Conner, Beautrais, & Conwell, 2003), formal tests of moderation that produce statistically significant results in the case–control psychological autopsy research literature are rare, a limitation that can be overcome by combining the results of studies through metaanalysis. A metaanalysis by Li et al. (2011) examined risk for suicide associated with mood disorders and alcohol or drug use disorders using controlled reports that included a focus on moderating effects of sex, age, and region. However, the authors narrowed their search to studies that reported risk estimates for various diagnoses and one or more socio-economic variables (e.g., low occupational status), resulting in a restricted number of studies analyzed, with unclear generalizability to the broader case–control psychological autopsy literature.
A recent metaanalysis examined risk for suicide associated with alcohol use disorder, providing a pooled estimate, OR (95% CI) = 2.59 (1.95, 3.23) (Darvishi, Farhadi, Haghtalab, & Poorolajal, 2015). The authors also examined age and sex as moderators of the association between alcohol use disorder and suicide and did not find evidence of moderation. However, the analyses combined the results from studies using different study designs, including cohort studies that may assess mental disorders years prior to suicide, making the relevance of the findings to proximal risk for suicide unclear. The metaanalysis by Cho et al. (2016) narrowed the focus to psychological autopsy research studies and reported risk estimates for any substance use disorder (i.e., alcohol or drug) and alcohol use disorder broadly defined. However, neither metaanalysis disentangled subcategories of alcohol use disorder, including alcohol abuse and alcohol dependence, or examined nonalcohol drug use disorders. These are critical gaps because case–control psychological autopsy research has been dominated by reports of alcohol use disorder alone or summary substance use disorders variables that combine alcohol and other drug use disorders, making the contribution of (nonalcohol) drug use disorders to risk unclear. Disentangling categories of alcohol use disorder is also needed because some reports suggest that alcohol dependence but not alcohol abuse is greater in suicide decedents compared to nonsuicide controls (Cheng, 1995; Foster, Gillespie, McClelland, & Patterson, 1999; Kolves, Varnik, Tooding, & Wasserman, 2006), which may be attributable to greater alcohol-related severity associated with alcohol dependence.
We conducted a metaanalysis of case–control psychological autopsy studies of suicide to provide updated estimates of risk associated with mood disorders and alcohol or drug use disorders; test the moderating effects of age, sex, and region on these variables; disentangle risk in diagnostic subcategories based on the idea that risk may vary as a function of illness severity; and generate novel proximal risk estimates for nonalcohol drug use disorders.
METHODS
Literature Search
Inclusion criteria were as follows: (1) case–control study design that included a suicide decedent group and a nonsuicide control group, living or dead; (2) descriptive data provided on one or more mood disorder(s) and/or alcohol or drug use disorders in suicide cases and controls and/or the results of adjusted or unadjusted comparisons that were sufficient to calculate an effect size with respect to these disorders; (3) in-person research interviews using a diagnostic instrument with proxy respondents of suicide decedents and with nonsuicide controls and/or proxy respondents of controls; and (4) examinations of all suicides in a given population and/or subgroups defined by age, sex, and/or geographic location but no other criteria (e.g., a study comparing a general population sample of suicides and controls ages 60 and over would be eligible). Exclusion criteria were as follows: (1) non-English reports; (2) nonsuicide studies (e.g., examinations of non-lethal suicide attempt); (3) subpopulations of cases defined other than by age, sex, or geographic location (e.g., hospital patients, prisoners); (4) ineligible study design (e.g., record linkage study); (5) results were unavailable to calculate an effect size for a mood disorder and/or alcohol or drug use disorder and suicide or such results were duplicative of other reports of the same sample; (6) papers published before 1985; and (7) non-peer-reviewed studies (e.g., book chapters).
The identification of reports for the metaanalysis is described in Figure 1. First, electronic searches of PubMed using the terms “case-control” [All Fields] AND “suicide” [All Fields]) OR “psychological autopsy” [All Fields] were used to identify reports between January 1, 1985, and May 9, 2016 (n = 1,559). Second, review of the abstracts and, when necessary, the full reports of these studies were used to narrow the list to nonduplicative reports that met all eligibility criteria (n = 32). Third, the reference lists of the eligible papers, along with the reference sections of prior metaanalyses (Arsenault-Lapierre et al., 2004; Cavanagh et al., 2003; Darvishi et al., 2015; Yoshimasu et al., 2008) and comprehensive reviews (Conner et al., 2011, 2012), were used to identify three additional studies (N = 35).
Figure 1.
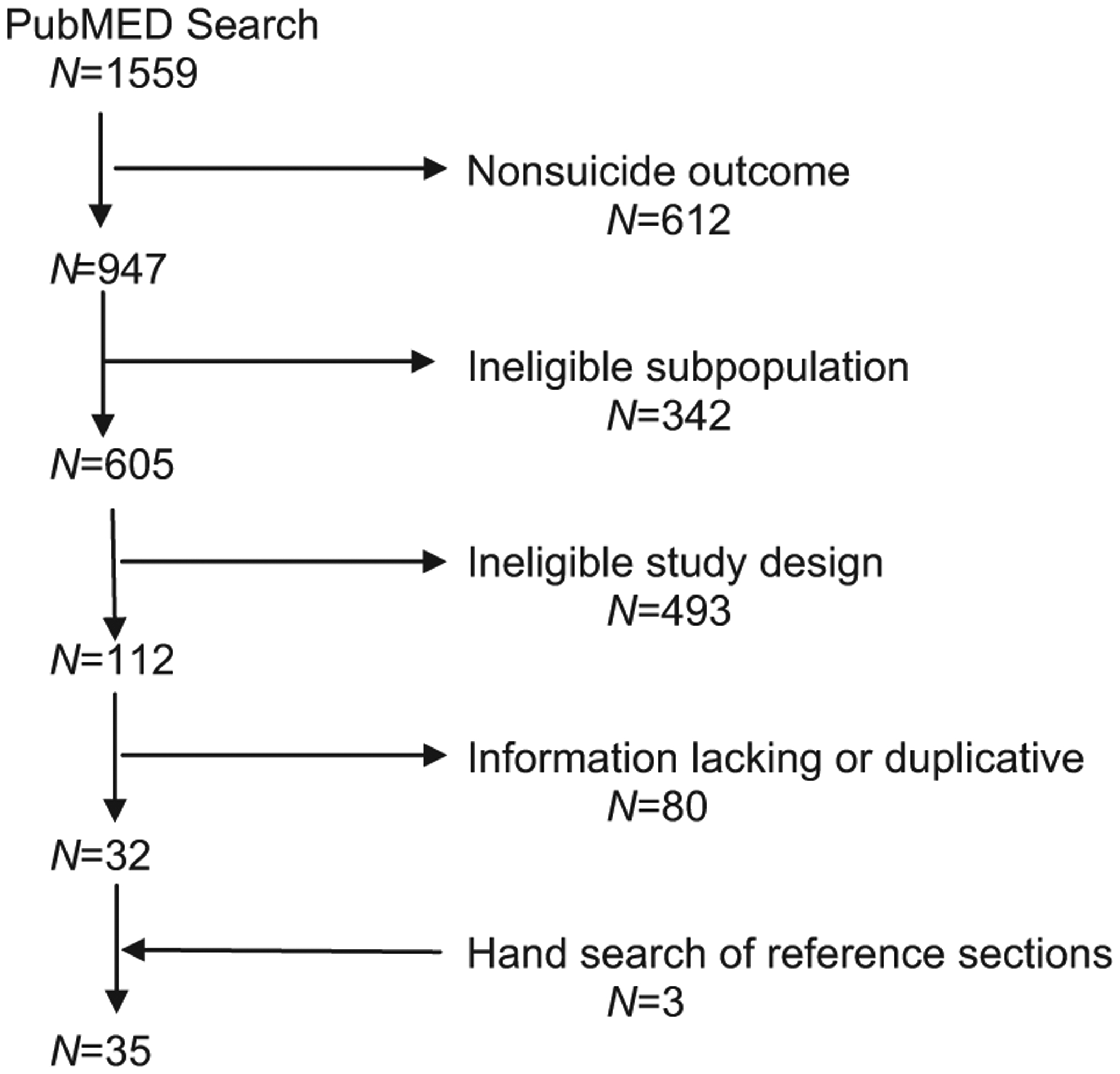
Selection of studies for metaanalysis.
Data Abstraction and Coding
Standardized data collection forms were developed for abstracting data (Lipsey & Wilson, 2001). The studies were coded by one of the authors (DJD) who reviewed the codes regularly with a second author (JAB) and, when there were questions, they consulted with a third author (KRC) to reach a consensus. The codes included: date of publication; region; country; sample size (cases, controls); participation rates (when available); age (mean, range); sex distribution; race/ethnic distribution when available; other demographic characteristics when available (e.g., education); nature of control group (e.g., community sample, injury decedents); instrument used to assess mental disorders; diagnostic system; and relevant results including descriptive, unadjusted, and adjusted findings.
Age, sex, and region were defined by mean age of cases (median age or age range used if mean age not available); proportion of male cases; and region of data collection including Asia, Australia or Oceania, Central America, Europe, and North America. Diagnoses of mood disorders and substance use disorders were used if they were based on one of the versions of the Diagnostic and Statistical Manual (e.g., American Psychiatric Association, 1994), International Classification of Diseases (e.g., World Health Organization, 1995), or if we determined that they were a reasonable proxy (e.g., substance misuse). Mood disorders included five categories: (1) mood disorder (broadest); (2) minor depression or dysthymic disorder; (3) major depression; (4) depression with psychosis; and (5) bipolar disorder. Alcohol and drug use disorders included five categories: (1) substance misuse or substance use disorder (substance use disorder) (broadest); (2) nonalcohol drug misuse or drug use disorder (drug use disorder); (3) alcohol abuse; (4) alcohol dependence; and (5) alcohol misuse or alcohol use disorder (alcohol use disorder). Data from separate reports of the same data set were included when they provided nonoverlapping results pertinent to the metaanalysis, including estimates for different diagnoses (e.g., Kolves, Sisask, et al., 2006; Kolves, Varnik, et al., 2006) or examinations of different age groups (e.g., Chan et al., 2009; Chiu et al., 2004). Methodological quality ratings were generated by one of the authors (KRC) using a 14-item rating scale (score range 0–18) that included 10 applicable items from a standard measure (Downs & Black, 1998) and four novel items created for the current study; for example, “What was the response rate for cases in the study?” ≥75% (scored 2), 50–74% (scored 1), ≤49% or unreported (scored 0).
Analyses
We obtained pooled estimates of the size of associations between mood disorders and alcohol or drug use disorders with suicide using random effects models (DerSimonian & Laird, 1986). We chose random effects models instead of fixed effects models in anticipation of heterogeneous effect sizes (Cooper, Hedges, & Valentine, 2009). Statistical analyses were performed using Comprehensive Metaanalyses version 2.2 (Biostat, Englewood, NJ) and SPSS version 24 (SPSS Inc, Chicago, IL). Odds ratios and 95% confidence intervals (OR, 95% CI) generated in these models provided measures of effect size. As data allowed, we examined world region, sex, age, and methodological quality as moderators of risk associated with mood disorders, major depression, minor depression or dysthymia, substance use disorder, and alcohol use disorder; there were too few reports to examine moderating influences on other disorders. World region and age were categorical moderators of outcome. For continuous moderators, mixed effects metaregression was used to explore whether proportion of male cases and methodological quality influenced outcome. Continuous moderators that showed an association with outcome were dichotomized by median split and reexamined as categorical moderators. Heterogeneity of effect sizes was examined using the Cochran Q chi-square statistic (p ≤ .10) and the I2 statistic, a transformation of Q that indicates the percentage of variation in the effect size estimate attributable to heterogeneity rather than sampling error (Higgins & Thompson, 2002). Publication bias was assessed visually using funnel plots and quantitatively using an adjusted rank correlation test (Begg & Mazumdar, 1994) and a regression procedure to measure funnel plot asymmetry (Egger, Davey Smith, Schneider, & Minder, 1997). We performed leave-oneout analyses by iteratively deleting each study and calculating the resulting effect to determine whether any study unduly influenced pooled effect size estimates.
RESULTS
Eligible Studies
Characteristics of the 35 studies analyzed are listed in Table 1. Region of studies include Asia (n = 11), Australia or Oceania (n = 5), Central America (n = 1), Europe (n = 12), and North America (6). Age categories include adolescent and/or young adult (n = 10), mixed age (n = 19), and older adult (n = 6). Across all studies, the average proportion of male cases was 0.71 (standard deviation [SD] = 0.14). Quality ratings ranged from 4 to 17, with mean (SD) = 12.7 (3.4). The studies reported the results for the disorders examined in this review.
TABLE 1.
Description of Reports Analyzed
| Report | N | Region | Age category | % Male (cases) | Quality rating | Diagnoses examined |
|---|---|---|---|---|---|---|
| 1. Almasi et al. (2009) | 194 | Europe | Mixed | 81 | 16 | Mood disorder, minor depression, SUD |
| 2. Appleby, Cooper, Amos, and Faragher (1999) | 84 | Europe | Adolescent/young adult | 81 | 8 | SUD |
| 3. Beautrais (2001) | 202 | Australia/Oceania | Mixed | 78 | 16 | Mood disorder, SUD |
| 4. Brent, Baugher, Bridge, Chen, and Chiappetta (1999) | 140 | North America | Adolescent/young adult | 85 | 16 | Mood disorder, SUD |
| 5. Brent et al. (1993) | 67 | North America | Adolescent/young adult | 85 | 13 | Major depression, drug use disorder, AUD |
| 6. Chan et al. (2009) | 150 | Asia | Mixed | 64 | 9 | Major depression |
| 7. Chen et al. (2006) | 150 | Asia | Mixed | 64 | 9 | Mood disorder |
| 8. Cheng (1995) | 117 | Asia | Mixed | 62 | 13 | Minor depression, alcohol abuse, alcohol dependence |
| 9. Cheng, Chen, Chen, and Jenkins (2000) | 117 | Asia | Mixed | 62 | 14 | Major depression, SUD |
| 10. Chiu et al. (2004) | 70 | Asia | Older adult | 46 | 8 | Mood disorder, minor depression, major depression, alcohol dependence |
| 11. Conner et al. (2003) | 193 | Australia/Oceania | Mixed | 77 | 16 | Drug use disorder, alcohol dependence |
| 12. Conwell et al. (2010) | 86 | North America | Older adult | 73 | 15 | Mood disorder, major depression, SUD, AUD |
| 13. De Leo, Draper, Snowdon, and Kõlves (2013a) | 84 | Australia/Oceania | Mixed | 85 | 13 | Mood disorder, SUD |
| 14. De Leo, Draper, Snowdon, and Kõlves (2013b) | 261 | Australia/Oceania | Mixed, Older adult | 75 | 14 | Major depression, bipolar disorder, AUD |
| 15. Foster et al. (1999) | 117 | Europe | Mixed | NR | 14 | Mood disorder, major depression, SUD, alcohol abuse, alcohol dependence, AUD |
| 16. Freuchen, Kjelsberg, Lundervold, and Groholt (2012) | 41 | Europe | Adolescent/young adult | 71 | 12 | Mood disorder, minor depression |
| 17. Harwood, Hawton, Hope, and Jacoby (2001) | 54 | Europe | Older adult | 41 | 6 | Mood disorder, SUD |
| 18. Khan, Mahmud, Karim, Zaman, and Prince (2008) | 100 | Asia | Mixed | 83 | 14 | SUD |
| 19. Kim et al. (2003) | 115 | Asia | Mixed | 100 | 11 | Major depression, bipolar disorder, drug use disorder, alcohol abuse, alcohol dependence |
| 20. Kolves, Varnik, et al. (2006) | 427 | Europe | Mixed | 80 | 15 | Alcohol abuse, alcohol dependence |
| 21. Kolves, Sisask, et al. (2006) | 419 | Europe | Mixed | 80 | 15 | SUD |
| 22. Manoranjitham et al. (2010) | 100 | Asia | Mixed | 59 | 14 | Minor depression, major depression, alcohol dependence |
| 23. Page et al. (2014) | 84 | Australia/Oceania | Adolescent/young adult | 85 | 12 | Mood disorder, major depression, SUD |
| 24. Palacio et al. (2007) | 108 | Central America | Mixed | 81 | 12 | Minor depression, major depression, SUD |
| 25. Préville, Hébert, Boyer, Bravo, and Seguin (2005) | 95 | Europe | Older adult | 75 | 13 | Major depression, alcohol abuse, alcohol dependence |
| 26. Renaud, Berlim, McGirr, Tousignant, and Turecki (2008) | 55 | North America | Adolescent/young adult | 78 | 8 | Mood disorder, minor depression, bipolar disorder, SUD, drug use disorder, AUD |
| 27. Schneider et al. (2006) | 163 | Europe | Mixed | 64 | 13 | Mood disorder, minor depression, major depression, bipolar disorder, SUD, AUD |
| 28. Shaffer et al. (1996) | 120 | North America | Adolescent/young adult | 79 | 16 | Mood disorder, major depression, bipolar disorder, SUD, drug use disorder, AUD |
| 29. Shafii, SteltzLenarsky, Derrick, and Beckner (1988) | 21 | North America | Adolescent/young adult | 91 | 8 | Mood disorder, minor depression, major depression, SUD |
| 30. Tong and Phillips (2010) | 895 | Asia | Mixed | 51 | 17 | Mood disorder, SUD |
| 31. Vijayakumar et al. (1999) | 100 | Asia | Mixed | 55 | 17 | Minor depression, major depression, bipolar disorder, drug use disorder, AUD |
| 32. Waern et al. (2002) | 85 | Europe | Older adult | 54 | 16 | Mood disorder, minor depression, major depression, bipolar disorder, SUD |
| 33. Waern (2003) | 88 | Europe | Adolescent/young adult | 56 | 16 | AUD |
| 34. Zhang, Xiao, and Zhou (2010) | 392 | Asia | Adolescent/young adult | 55 | 11 | Mood disorder, minor depression, major depression, bipolar disorder, SUD, drug use disorder, AUD |
| 35. Zonda (2006) | 100 | Europe | Mixed | 67 | 4 | Major depression, drug use disorder, AUD |
AUD, alcohol use disorder; SUD, substance use disorder; NR, not reported.
Main Effects
The primary results of the analyses are shown in Table 2. Mood disorder broadly defined and major depression showed the largest effect sizes in risk for suicide: mood disorder, OR (95% CI) = 14.34 (9.10, 22.57); major depression, OR (95% CI) = 9.14 (5.53, 15.09). The effect sizes for bipolar disorder, depression with psychosis, and minor depression or dysthymic disorder were statistically significant although smaller in magnitude, in the range of three- to fourfold risk. The results of the analyses of the various alcohol and drug use disorders are also shown in Table 2, with each disorder showing statistically significant results in the range of threefold risk for suicide and higher, with the highest risk estimate for drug use disorder, OR (95% CI) = 7.18 (3.22, 16.01). Significant heterogeneity across studies was noted for each disorder (I2 range, 39%–80%), with the exception of depression with psychosis and bipolar disorder.
TABLE 2.
Risk for Suicide Associated with Mood and Alcohol and Drug Use Disorders
| Disorder | N of studies | OR | 95% CI lower | 95% CI upper | p Value | Heterogeneity | ||
|---|---|---|---|---|---|---|---|---|
| Qdf Within | p Value | Variance explained, % | ||||||
| Mood disorder | 18 | 14.34 | 9.10 | 22.57 | <.001 | 77.917 | <.001 | 78 |
| Minor depression | 12 | 2.73 | 1.53 | 4.85 | .001 | 18.111 | .08 | 39 |
| Major depression | 19 | 9.14 | 5.53 | 15.09 | <.001 | 72.518 | <.001 | 75 |
| Depression with psychosis | 3 | 3.37 | 1.01 | 11.24 | .048 | 0.62 | .73 | 0 |
| Bipolar disorder | 8 | 3.70 | 1.59 | 8.61 | .002 | 9.67 | .22 | 27 |
| Substance use disorder | 20 | 4.09 | 3.10 | 5.40 | <.001 | 40.719 | .003 | 53 |
| Drug use disorder | 8 | 7.18 | 3.22 | 16.01 | <.001 | 13.67 | .06 | 49 |
| Alcohol abuse | 5 | 3.90 | 1.62 | 9.38 | .002 | 9.14 | .06 | 56 |
| Alcohol dependence | 8 | 4.40 | 2.55 | 7.59 | <.001 | 21.57 | .003 | 67 |
| Alcohol use disorder | 11 | 3.68 | 1.99 | 6.82 | <.001 | 49.410 | <.001 | 80 |
Note. All results based on random effects models.
OR, odds ratio; CI, confidence interval; df, degrees of freedom.
Moderator Analyses
There is evidence of a moderating effect of region on risk for suicide associated with mood disorder (Q3 = 9.60, p = .022) and major depression (Q2 = 7.63, p = .022), with studies conducted in Asia showing the highest pooled risk estimate for each of these disorders. However, the test for a moderating effect of region on risk for suicide associated with substance use disorder was nonsignificant (Q3 = 4.98, p = .173). Also, risk for suicide associated with major depression was higher in studies with larger proportions of females (β= 4.48, Q1 = 6.87, p = .009). Dichotomizing proportion of male cases by median split (≤ 0.70 vs. > .70) revealed significantly larger effect sizes (Q1 = 3.97, p = .046) in studies where the proportion of male cases was ≤ .70 (OR = 15.34, 95% CI = 7.17–32.83) compared to studies with > .70 proportion of male cases (OR = 5.37, 95% CI = 2.67–10.80). Studies with higher quality ratings generated higher risk estimates associated with alcohol use disorder (p = .003) and drug use disorder (p < .001). There was a lack of evidence of moderating effects of region or gender on risk associated with other disorders, and we found no evidence of moderating effects of age.
Publication Bias and Leave-One-Out Analysis
Separate analyses of publication bias were conducted for each pooled estimate of risk of suicide associated with mood disorders and alcohol or drug use disorders. We did not find evidence of publication bias in any of the models based on visual inspection of the funnel plots, the adjusted rank correlation tests, and the regression intercept approach (data available on request). Sensitivity analyses did not suggest that any individual study unduly influenced the pooled risk estimates reported in Table 2 (data available on request).
DISCUSSION
Mood Disorders
The current metaanalysis of case–control psychological autopsy studies conducted worldwide over a 30-year period provided estimates of proximal risk for suicide associated with various mood and substance use disorders and tested moderators of risk. The risk estimate for major depression was significantly lower than that provided by Cho et al. (2016) which may be presumed to be attributable to the differing search strategies, with the current search uncovering a greater number of relevant reports (n = 19 vs. n = 12). Nonetheless, the risk estimate that we obtained for major depression is on the order of ninefold risk, underscoring that it is a potent risk factor. In contrast, the estimate of proximal risk for suicide associated with minor depression or dysthymia OR (95%) CI = 2.7 (1.5., 4.9) was similar to that provided by Cho et al., with the implication that nonsevere depression confers increased risk for suicide.
Tests of moderation suggest that mood disorder broadly defined and major depression are more potent proximal risk factors in studies conducted in Asia than other world regions. Interestingly, psychological autopsy studies conducted in Asia have generally shown that the percentage of suicide decedents with depressive symptoms or disorders is lower compared to Western reports (e.g., Phillips et al., 2002; Vijayakumar et al., 1999). However, it is critical to consider the generally very low prevalence of depressive illness in nonsuicide control subjects in Asian studies and, as illustrated by the current analysis, when cases and controls from studies conducted in Asia are pooled and compared on major depression, it produces dramatic risk estimates. Tests of moderation also suggest that major depression is associated with greater increased risk for suicide in women than men (Table 3).
TABLE 3.
Region-Grouped Risk for Suicide Associated with Mood Disorder, Major Depression, and Substance Use Disorder
| Heterogeneity | Effect of Region | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Disorder | Regiona | N of studies | OR | 95% CI lower | 95% CI upper | p Value | Qdf Within | p Value | Variance explained, % | Qdf Between | p Value |
| Mood disorder | Asia | 4 | 28.61 | 14.91 | 54.92 | <.001 | 8.33 | .04 | 64 | 9.603 | .022b |
| Australia/Oceania | 3 | 6.90 | 3.50 | 13.61 | <.001 | 5.332 | .07 | 62 | |||
| Europe | 6 | 10.62 | 4.50 | 25.09 | <.001 | 25.135 | <.001 | 80 | |||
| North America | 5 | 17.32 | 9.42 | 31.85 | <.001 | 3.794 | .44 | 0 | |||
| Major depressionc | Asia | 6 | 26.87 | 15.58 | 46.36 | <.001 | 2.35 | .80 | 0 | 7.632 | .022d |
| Europe | 4 | 7.95 | 3.30 | 19.16 | <.001 | 14.53 | .002 | 79 | |||
| North America | 6 | 7.68 | 2.60 | 22.70 | <.001 | 21.05 | .001 | 76 | |||
| Substance use disorder | Asia | 4 | 3.35 | 2.00 | 5.61 | <.001 | 2.682 | .26 | 25 | 4.983 | .173 |
| Australia/Oceania | 3 | 2.64 | 1.35 | 5.14 | .004 | 6.762 | .03 | 70 | |||
| Europe | 7 | 6.54 | 3.76 | 11.39 | <.001 | 16.226 | .01 | 63 | |||
| North America | 5 | 3.97 | 1.99 | 7.90 | <.001 | 5.484 | .24 | 27 | |||
OR, odds ratio; CI, confidence interval; df, degrees of freedom.
Random effects model used to combine studies within each region.
Pairwise comparisons: Asia vs. Australia/Oceania, Q1 = 8.77, p = .003; Asia vs. Europe, Q1 = 3.24, p = .072; Asia vs. North America, Q1 = 1.22, p = .270; Australia/Oceania vs. Europe, Q1 = 0.60, p = .44; Australia/Oceania vs. North America, Q1 = 3.91, p = .048; Europe vs. North America, Q1 = 0.83, p = .36.
Australia/Oceania and Central America were excluded from analyses because there were <3 studies within each region.
Pairwise comparisons: Asia vs. Europe, Q1 = 5.32, p = .021; Asia vs. North America, Q1 = 4.09, p = .043; Europe vs. North America, Q1 = 0.00, p = .96.
Alcohol and Drug Use Disorders
The study provides a novel estimate for proximal risk for suicide associated with nonalcohol drug use disorder, and the high-risk estimate, OR (95% CI) = 7.2 (3.2, 16.0), illustrates the importance of targeting drug abuse in suicide prevention efforts. Drug use disorders are heterogeneous, and prior research suggests that nonmedical use of opiates, cocaine, amphetamine, and other stimulants is associated with suicide (Degenhardt, Roxburgh, & Barker, 2005; Wilcox, Conner, & Caine, 2004). Unfortunately, information on specific drug use disorders is generally lacking in case–control psychological autopsy studies, making it unclear whether similar results would be obtained using this methodology. The risk estimates for alcohol use disorder broadly defined, alcohol abuse, and alcohol dependence are similar to one another, in the area of three- to four-fold risk. These results suggest that it would not represent a significant loss of information to use a unitary measure of alcohol use disorder in case–control psychological autopsy research studies, for example, as defined using current nosology (American Psychiatric Association, 2013). Finally, risk estimates did not differ by region or sex, unlike the results for mood disorder and major depression.
Effect Sizes
The effect sizes in the current study were generally higher than in Franklin et al.’s (2017) landmark metaanalysis of suicidal behavior. However, it is difficult to make head-to-head comparisons of effect sizes of postmortem case–control studies and cohort studies. Cohort studies of suicide deaths have had long lengths of follow-up, with potential that an assessed exposure (e.g., alcohol use disorder) is no longer an active problem at the time of death, among other problems of interpretation. Indeed, the median length to follow-up in Franklin and colleagues’ metaanalysis was 6 years, with fewer than 1% of the effect sizes based on reassessments of 1 month or less, and approximately 29% based on follow-ups of 10 years or greater. The study also showed that effect sizes for suicide deaths were modestly reduced with length of follow-up, suggesting longer follow-ups may bias effect sizes downward. Recognizing the limitation of lengthy follow-ups, Franklin and colleagues called for the use of short follow-up periods in cohort studies moving forward. We agree, although the feasibility of such research for studies of suicide deaths is unclear given the low incidence rate. Case–control psychological autopsy studies are focused on the time period prior to death and a comparable exposure period in nonsuicide controls, increasing their capability to estimate risk associated with active symptoms. Accordingly, this study design seems better equipped to estimate proximal risk for suicide deaths associated with mental disorders (and other exposures). Finally, despite generally large effect sizes associated with mood and substance use disorders, suicide is a rare outcome that cannot be predicted with accuracy by clinicians, researchers, or other stakeholders, and the results of the current study do not change this bottom-line conclusion.
Limitations
There were limitations of the meta-analysis. Broad measures were used to create the moderators including age (mean age of study) and sex (proportion male in study). There were no data to allow for examination of several world regions. We examined proximal risk associated with alcohol and drug use disorders, but it was not possible to examine the role of acute use of alcohol (e.g., Branas, Richmond, Ten Have, & Wiebe, 2011) or acute use of various drugs in risk (e.g., Borges, Bagge, & Orozco, 2016) because such data are rarely available in case–control psychological autopsy studies. Females make up a greater percentage of suicide decedents in Asia, and in China in particular, compared to other regions (World Health Organization, 2014), complicating the interpretation of moderating effects of sex and region on risk for suicide associated with major depression that were identified in the current analyses. More specifically, in our metaanalysis, it was not possible to disentangle main or interactive effects of region and sex in the moderation analysis concerning major depression because all studies in Asia had a low proportion (≤ .70) of male cases. As well, the risk estimate for bipolar disorder, OR (95% CI) = 3.7 (1.6, 8.6), in the current study requires cautious interpretation in light of high risk associated with this disorder that has been reported in studies using prospective designs (Angst, Stassen, Clayton, & Angst, 2002; Chang, Chen, Yen, Chen, & Lee, 2012) and because of the potential for missing the diagnosis using retrospective methodology in individuals who killed themselves during the depressive (rather than manic) phase of the illness (Valtonen et al., 2008). Another limitation is that the available data did not make it feasible to estimate risk associated with mental disorder comorbidity (e.g., mood disorder plus substance use disorder). There are inherent limitations of case–control psychological autopsy research, including retrospective biases, primary reliance on proxy reports, and participation rates that vary widely (Conner et al., 2011, 2012). Future research on suicide, regardless of the methodology used, would be improved by examining acute use of alcohol, investigating social media content (e.g., to identify suicide-related communication before suicide), employing cutting-edge data analytic techniques, and gathering data on other domains of study (e.g., stressful life events, perceived belonging) with widely used and validated measures to allow for pooling such data for metaanalysis (Conner et al., 2011, 2012; Franklin et al., 2017; Luxton, June, & Fairall, 2012).
CONCLUSION
Merits of the current metaanalysis included the focus on a single study design (case–control) and outcome (suicide death) to aid interpretation; examination of the two most prevalent broad categories of mental disorders among suicide decedents worldwide (i.e., mood disorders, substance use disorders); use of several strategies to examine potential biases on results; and a focus on proximal risk for suicide that is uniquely suited for psychological autopsy research designs. In conclusion, the current metaanalysis provides new evidence that major depression and mood disorder may be an especially virulent proximal risk factor for suicide in Asian populations and that major depression may be a more potent risk factor in women. The pooled estimate concerning drug use disorders is novel and underscores the importance of targeting drug abuse in suicide prevention efforts. Results do not suggest differences in suicide risk associated with alcohol abuse and alcohol dependence, suggesting that the change to simplify substance use disorder nomenclature in DSM-V does not come at a cost to estimations of suicide risk.
Acknowledgments
This work was supported by a grant from the American Foundation for Suicide Prevention (Conner PI). An earlier version was presented in June, 2015, at the World Congress of the International Association of Suicide Prevention, Montreal, Canada.
REFERENCES
- Almasi K, Belso N, Kapur N, Webb R, Cooper J, Hadley S, et al. (2009). Risk factors for suicide in Hungary: A case-control study. BMC Psychiatry, 9, 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and statistical manual of mental disorders (4th ed.). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: Author. [Google Scholar]
- Angst F, Stassen HH, Clayton PJ, & Angst J (2002). Mortality of patients with mood disorders: Follow-up over 34–38 years. Journal of Affective Disorders, 68, 167–181. [DOI] [PubMed] [Google Scholar]
- Appleby L, Cooper J, Amos T, & Faragher B (1999). Psychological autopsy study of suicides by people aged under 35. British Journal of Psychiatry, 175, 168–174. [DOI] [PubMed] [Google Scholar]
- Arsenault-Lapierre G, Kim C, & Turecki G (2004). Psychiatric diagnoses in 3275 suicides: A meta-analysis. BMC Psychiatry, 4, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beautrais AL (2001). Suicides and serious suicide attempts: Two populations or one? Psychological Medicine, 31, 837–845. [DOI] [PubMed] [Google Scholar]
- Begg CB, & Mazumdar M (1994). Operating characteristics of a rank correlation test for publication bias. Biometrics, 50, 1088–1101. [PubMed] [Google Scholar]
- Borges G, Bagge CL, & Orozco R (2016). A literature review and meta-analyses of cannabis use and suicidality. Journal of Affective Disorders, 195, 63–74. [DOI] [PubMed] [Google Scholar]
- Branas CC, Richmond TS, Ten Have TR, & Wiebe DJ (2011). Acute alcohol consumption, alcohol outlets, and gun suicide. Substance Use and Misuse, 46, 1592–1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, Baugher M, Bridge J, Chen T, & Chiappetta L (1999). Age- and sex-related risk factors for adolescent suicide. Journal of the American Academy of Child and Adolescent Psychiatry, 38, 1497–1505. [DOI] [PubMed] [Google Scholar]
- Brent DA, Perper JA, Moritz G, Allman C, Friend A, Roth C, et al. (1993). Psychiatric risk factors for adolescent suicide: A case-control study. Journal of the American Academy of Child and Adolescent Psychiatry, 32, 521–529. [DOI] [PubMed] [Google Scholar]
- Cavanagh JTO, Carson AJ, Sharpe M, & Lawrie SM (2003). Psychological autopsy studies of suicide: A systematic review. Psychological Medicine, 33, 395–405. [DOI] [PubMed] [Google Scholar]
- Chan SS, Chiu HF, Chen EY, Chan WS, Wong PW, Chan CL, et al. (2009). Population-attributable risk of suicide conferred by axis I psychiatric diagnoses in a Hong Kong Chinese population. Psychiatric Services, 60, 1135–1138. [DOI] [PubMed] [Google Scholar]
- Chang JC, Chen HH, Yen AM, Chen SL, & Lee CS (2012). Survival of bipolar depression, other type of depression and comorbid ailments: Ten-year longitudinal follow-up of 10,922 Taiwanese patients with depressive disorders. Journal of Psychiatric Research, 46, 1442–1448. [DOI] [PubMed] [Google Scholar]
- Chen EYH, Chan WSC, Wong PWC, Chan SSM, Chan CLW, Law YW, et al. (2006). Suicide in Hong Kong: A case-control psychological autopsy study. Psychological Medicine, 36, 815–825. [DOI] [PubMed] [Google Scholar]
- Cheng AT (1995). Mental illness and suicide: A case-control study in east Taiwan. Archives of General Psychiatry, 52, 594–603. [DOI] [PubMed] [Google Scholar]
- Cheng AT, Chen TH, Chen CC, & Jenkins R (2000). Psychosocial and psychiatric risk factors for suicide: Case-control psychological autopsy study. British Journal of Psychiatry, 177, 360–365. [DOI] [PubMed] [Google Scholar]
- Chiu HF, Yip PS, Chi I, Chan S, Tsoh J, Kwan CW, et al. (2004). Elderly suicide in Hong Kong: A case-controlled psychological autopsy study. Acta Psychiatrica Scandinavica, 109, 299–305. [DOI] [PubMed] [Google Scholar]
- Cho S-E, Na K-S, Cho S-J, Im J-S, & Kang S-G (2016). Geographical and temporal variations in the prevalence of mental disorders in suicide: Systematic review and meta-analysis. Journal of Affective Disorders, 190, 704–713. [DOI] [PubMed] [Google Scholar]
- Conner KR, Beautrais AL, Brent DA, Conwell Y, Phillips MR, & Schneider B (2011). The next generation of psychological autopsy studies. Part I. Interview content. Suicide and Life-Threatening Behavior, 41, 594–613. [DOI] [PubMed] [Google Scholar]
- Conner KR, Beautrais AL, Brent DA, Conwell Y, Phillips MR, & Schneider B (2012). The next generation of psychological autopsy studies. Part 2. Interview procedures. Suicide and Life-Threatening Behavior, 42, 86–103. [DOI] [PubMed] [Google Scholar]
- Conner KR, Beautrais AL, & Conwell Y (2003). Moderators of the relationship between alcohol dependence and suicide and medically serious suicide attempts: Analyses of Canterbury Suicide Project data. Alcoholism, Clinical and Experimental Research, 27, 1156–1161. [DOI] [PubMed] [Google Scholar]
- Conwell Y, Duberstein PR, Hirsch JK, Conner KR, Eberly S, & Caine ED (2010). Health status and suicide in the second half of life. International Journal of Geriatric Psychiatry, 25, 371–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper HM, Hedges LV, & Valentine JC (2009). The handbook of research synthesis and meta-analysis (2nd ed.). New York: Russell Sage Foundation. [Google Scholar]
- Darvishi N, Farhadi M, Haghtalab T, & Poorolajal J (2015). Alcohol-related risk of suicidal ideation, suicide attempt, and completed suicide. PLoS ONE, 10, e0126870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Leo D, Draper BM, Snowdon J, & Kõlves K (2013a). Contacts with health professionals before suicide: Missed opportunities for prevention? Comprehensive Psychiatry, 54, 1117–1123. [DOI] [PubMed] [Google Scholar]
- De Leo D, Draper BM, Snowdon J, & Kõlves K (2013b). Suicides in older adults: A case-control psychological autopsy study in Australia. Journal of Psychiatric Research, 47, 980–988. [DOI] [PubMed] [Google Scholar]
- Degenhardt L, Roxburgh A, & Barker B (2005). Underlying causes of cocaine, amphetamine and opioid related deaths in Australia. Journal of Clinical Forensic Medicine, 12, 187–195. [DOI] [PubMed] [Google Scholar]
- DerSimonian R, & Laird N (1986). Meta-analysis in clinical trials. Controlled Clinical Trials, 7, 177–188. [DOI] [PubMed] [Google Scholar]
- Downs SH, & Black N (1998). The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. Journal of Epidemiology and Community Health, 52, 377–384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M, & Minder C (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ, 315, 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster T, Gillespie K, McClelland R, & Patterson R (1999). Risk factors for suicide independent of DSM-III-R Axis I disorder. British Journal of Psychiatry, 175, 175–179. [DOI] [PubMed] [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, et al. (2017). Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin, 143, 187–232 10.1037/bul0000084 [DOI] [PubMed] [Google Scholar]
- Freuchen A, Kjelsberg E, Lundervold AJ, & Groholt B (2012). Differences between children and adolescents who commit suicide and their peers: A psychological autopsy study of suicide victims compared to accident victims and a community sample. Child and Adolescent Psychiatry and Mental Health, 6, 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harwood D, Hawton K, Hope T, & Jacoby R (2001). Psychiatric disorder and personality factors associated with suicide in older people: A descriptive and case-control study. International Journal of Geriatric Psychiatry, 16, 155–165. [DOI] [PubMed] [Google Scholar]
- Higgins JPT, & Thompson SG (2002). Quantifying heterogeneity in a meta-analysis. Statistics in Medicine, 21, 1539–1558. [DOI] [PubMed] [Google Scholar]
- Khan MM, Mahmud S, Karim MS, Zaman M, & Prince M (2008). Case-control study of suicide in Karachi, Pakistan. British Journal of Psychiatry, 193, 402–405. [DOI] [PubMed] [Google Scholar]
- Kim CD, Lesage A, Seguin M, Chawky N, Vanier C, Lipp O, et al. (2003). Patterns of co-morbidity in male suicide completers. Psychological Medicine, 33, 1299–1309. [DOI] [PubMed] [Google Scholar]
- Kolves K, Sisask M, Anion L, Samm A, & Värnik A (2006). Factors predicting suicide among Russians in Estonia in comparison with Estonians: Case-control study. Croatian Medical Journal, 47, 869–877. [PMC free article] [PubMed] [Google Scholar]
- Kolves K, Varnik A, Tooding LM, & Wasserman D (2006). The role of alcohol in suicide: A case-control psychological autopsy study. Psychological Medicine, 36, 923–930. [DOI] [PubMed] [Google Scholar]
- Li Z, Page A, Martin G, & Taylor R (2011). Attributable risk of psychiatric and socio-economic factors for suicide from individual-level, population-based studies: A systematic review. Social Science & Medicine, 72, 608–616. [DOI] [PubMed] [Google Scholar]
- Lipsey MW, & Wilson DB (2001). Practical meta-analysis. Thousand Oaks, CA: Sage. [Google Scholar]
- Luxton DD, June JD, & Fairall JM (2012). Social media and suicide: A public health perspective. American Journal of Public Health, 102, S195–S200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manoranjitham SD, Rajkumar AP, Thangadurai P, Prasad J, Jayakaran R, & Jacob KS (2010). Risk factors for suicide in rural south India. British Journal of Psychiatry, 196, 26–30. [DOI] [PubMed] [Google Scholar]
- Page A, Morrell S, Hobbs C, Carter G, Dudley M, Duflou J, et al. (2014). Suicide in young adults: Psychiatric and socio-economic factors from a case-control study. BMC Psychiatry, 14, 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palacio C, García J, Diago J, Zapata C, Lopez G, Ortiz J, et al. (2007). Identification of suicide risk factors in Medellín, Colombia: A case-control study of psychological autopsy in a developing country. Archives of Suicide Research, 11, 297–308. [DOI] [PubMed] [Google Scholar]
- Phillips MR, Yang G, Zhang Y, Wang L, Ji H, & Zhou M (2002). Risk factors for suicide in China: A national case-control psychological autopsy study. The Lancet, 360, 1728–1736. [DOI] [PubMed] [Google Scholar]
- Préville M, Hébert R, Boyer R, Bravo G, & Seguin M (2005). Physical health and mental disorder in elderly suicide: A case-control study. Aging and Mental Health, 9, 576–584. [DOI] [PubMed] [Google Scholar]
- Qin P (2011). The impact of psychiatric illness on suicide: Differences by diagnosis of disorders and by sex and age of subjects. Journal of Psychiatric Research, 45, 1445–1452. [DOI] [PubMed] [Google Scholar]
- Renaud J, Berlim MT, McGirr A, Tousignant M, & Turecki G (2008). Current psychiatric morbidity, aggression/impulsivity, and personality dimensions in child and adolescent suicide: A case-control study. Journal of Affective Disorders, 105, 221–228. [DOI] [PubMed] [Google Scholar]
- Schneider B, Wetterling T, Sargk D, Schneider F, Schnabel A, Maurer K, et al. (2006). Axis I disorders and personality disorders as risk factors for suicide. European Archives of Psychiatry and Clinical Neuroscience, 256, 17–27. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Fisher P, Trautman P, Moreau D, Kleinman M, et al. (1996). Psychiatric diagnosis in child and adolescent suicide. Archives of General Psychiatry, 53, 339–348. [DOI] [PubMed] [Google Scholar]
- Shafii M, SteltzLenarsky J, Derrick AM, & Beckner C (1988). Comorbidity of mental disorders in the post-mortem diagnosis of completed suicide in children and adolescents. Journal of Affective Disorders, 15, 227–233. [DOI] [PubMed] [Google Scholar]
- Tong Y, & Phillips MR (2010). Cohort-specific risk of suicide for different mental disorders in China. British Journal of Psychiatry, 196, 467–473. [DOI] [PubMed] [Google Scholar]
- Valtonen HM, Suominen K, Haukka J, Mantere O, Leppamaki S, Arvilommi P, et al. (2008). Differences in incidence of suicide attempts during phases of bipolar I and bipolar II disorders. Bipolar Disorders, 10, 588–596. [DOI] [PubMed] [Google Scholar]
- Vijayakumar L, & Rajkumar S (1999). Are risk factors for suicide universal? A case-control study in India. Acta Pscyhiatrica Scandinavica, 99, 407–411. [DOI] [PubMed] [Google Scholar]
- Waern M (2003). Alcohol dependence and misuse in elderly suicides. Alcohol and Alcoholism, 38, 249–254. [DOI] [PubMed] [Google Scholar]
- Waern M, Runeson BS, Allebeck P, Beskow J, Rubenowitz E, Skoog I, et al. (2002). Mental disorder in elderly suicides: A case-control study. American Journal of Psychiatry, 159, 450–455. [DOI] [PubMed] [Google Scholar]
- Wilcox HC, Conner KR, & Caine ED (2004). Association of alcohol and drug use disorders and completed suicide: An empirical review of cohort studies. Drug and Alcohol Dependence, 76(Suppl), S11–S19. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (1995). International Classification of Diseases, ninth revision, clinical modification (ICD-9-CM). Los Angeles, CA: Practice Management Information Corporation and World Health Organization. [Google Scholar]
- World Health Organization. (2014). Preventing suicide: A global imperative. Geneva: Author. RetrievedOctober 29, 2016, from www.who.int/mental_health/suicide-prevention/exe_summary_english.pdf. [Google Scholar]
- Yoshimasu K, Kiyohara C, Miyashita K, & Stress Research Group of the Japanese Society for Hygiene. (2008). Suicidal risk factors and completed suicide: Meta-analyses based on psychological autopsy studies. Environmental Health and Preventive Medicine, 13, 243–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Xiao S, & Zhou L (2010). Mental disorders and suicide among young rural Chinese: A case-control psychological autopsy study. American Journal of Psychiatry, 167, 773–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zonda T (2006). One-hundred cases of suicide in Budapest: A case-controlled psychological autopsy study. Crisis, 27, 125–129. [DOI] [PubMed] [Google Scholar]


