Abstract
Coronavirus is a family of ARN positive single-stranded belonging to the family of Coronaviridae. There are several families of coronavirus that transmit more or less serious diseases. However, the so-called coronavirus-19 (SARS-CoV2) is the one that is currently causing most of the problems; in fact, biological dysfunctions that this virus causes provoke damage in various organs, from the lung to the heart, the kidney, the circulatory system, and even the brain. The neurological manifestations caused by viral infection, as well as the hypercoagulopathy and systemic inflammation, have been reported in several studies. In this review, we update the neurological mechanisms by which coronavirus-19 causes neurological manifestation in patients such as encephalomyelitis, Guillain-Barré syndrome, lacunars infarcts, neuropsychiatry disorders such as anxiety and depression, and vascular alterations. This review explains (a) the possible pathways by which coronavirus-19 can induce the different neurological manifestations, (b) the strategies used by the virus to cross the barrier system, (c) how the immune system responds to the infection, and (d) the treatment than can be administered to the COVID-19 patients.
Keywords: SARS-CoV-2, COVID-19, Viral mechanisms, Neurological disorders, Viral traffic, Therapies used
Introduction
SARS-CoV2 was discovered in Wuhan city (China) on December 2019. When this virus appeared, the Chinese doctors realized that it was not a common coronavirus but that its infection gave rise to numerous dysfunctions not well known and that it was also very contagious to the point of causing a pandemic. This virus was called SARS-CoV2 due to that its ARN has 82% similarities to SARS-CoV1 [1]. Its transmission, similar to the other virus that transmits pneumonia, is through the respiratory route in humans. The disease they transmit is called COVID-19 and its symptoms are cough, fever, lymphopenia, hypoxia, loss of smell and taste, and several neurological symptoms such as difficulty of movements, disorientation, and other less characterized dysfunctions [2]. Although COVID-19 preferably affects the respiratory and cardiovascular system, several COVID-19 patients present neurological symptoms such as headache and neuralgia as well as other complications including encephalopathy [3], acute cerebrovascular diseases [4], and difficulty of movements. Based on recent studies of cognitive symptoms in COVID-19 patients, it also seems present increased risk of dementia [5–7]. All these pathologies have hypothesized that a possible neuroinvasive potential of coronavirus-19 might be responsible for these symptoms. It is known that the coronavirus-19 enters the cell through the ACE2 enzyme of the rennin system, so it is not surprising that the virus can infect cells that possess this enzyme, including the brain. ACE2 is found in various body tissues as kidney [8], lung [9] heart [10], and the central nervous system [11]. Inside of CNS microglia and neurons have ACE2; therefore, the brain is a good candidate for the virus to attack it; however, the brain presents a problem to all those substances that can attack it, including viruses. This difficulty of entry is due to the blood–brain barrier (BBB) and to the blood-cerebrospinal barrier (B-CSF) [12]. In addition to this, one must be taken into account that many of the neurological dysfunctions can be caused by the entry of the virus through the respiratory system and mediated by the coagulation and hypoxia processes that this entails. Brain cells are very sensitive to oxygen deprivation and die; this situation can lead to coma, seizures, and even brain death. Symptoms of brain hypoxia include inattention, blunders, memory loss, and decreased motor coordination. All these symptoms have been found in some patients with COVID-19 [13]. Data on the characteristics of the disease such as pathologies, transmission, prevention, and treatments strategies have been cited [14]. This review explains the mechanism by which coronavirus can induce these diseases as well as the possible routes that this virus can use to reach the brain and the therapies than can be administered.
Neurological manifestations of COVID-19
The neurological manifestations induced by the coronavirus-19 can be produced at two levels: (a) one due to hypoxia and coagulation due to the dysfunctions that the virus induces outside the CNS when it attacks pulmonary cells, and (b) the neuronal dysfunctions that the virus can develop if it is able to reach the brain.
Neurological dysfunctions that coronavirus-19 induced without entering the brain
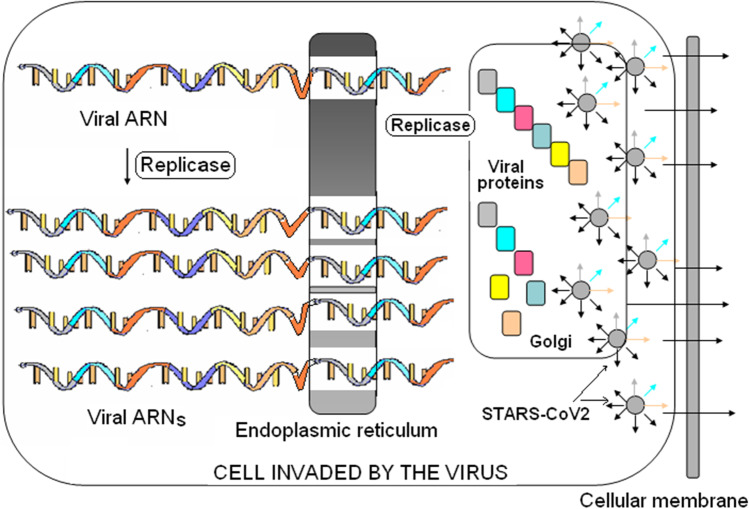
The leading cause of death for COVID-19 is the acute respiratory syndrome distress syndrome initiated by epithelial infection and alveolar macrophage activation in the lung. The virus enters into the alveolar cells through the angiotensin-convertin enzyme (ACE2) by a mechanism in which the virus, through its spiker protein, binds to the host cell membrane. Once it has entered the cell, the virus releases its + ARN and migrates to the endoplasmic reticulum to synthesize all their proteins (Fig. 1). The + ARN of SARS-CoV2 genome organization is arranged in a certain order. The gene for replicase, the protein which replicated the virus, is the first, followed by the synthesis of protein S, protein E, and protein M as well as nucleocapsid protein together another set of accessory proteins [15]. As the ARN viral is polycistronic, along its chain all its proteins are encoded, it is as if it were a long single mARN chain. The viral ARN, which encodes all viral proteins, migrates to the endoplasmic reticulum and begins by synthesizing the replicase protein, an enzyme capable of replicating the synthesis of several copies of viral ARN. These new viral ARNs migrate to the endoplasmic reticulum where they synthesize the rest of their proteins. Next, all the replicated viral ARNs, with their proteins, migrate to the Golgi apparatus. There, the viral ARNs are covered with their proteins giving rise to the formation of complete viruses, which leave the host cell by exocytose to infect other cells (Fig. 1).
Fig. 1.
Replication of the viral ARN
In this process, the host cell may (a) die, (b) to be phagocyted by macrophages, or (c) can be damaged. As a consequence, the loss of alveolar cells takes places, and as consequence dyspnoea and hypoxia can be induced. In addition, the infected cell alerts the immune system, releasing cytokines that alert macrophages, neutrophils, and antigen presenting cells; all these arrive where the infected cells and virus are. Macrophages phagocyte viruses and infected cells, and antigen-presenting cells recognize viruses and activate the adaptive immune system process. In this process, inflammation may take place. Inflammation is not always harmful, but when it occurs in an exaggerated way it can be dangerous. This inflammation is induced because when SARS-CoV2 enters in the cells, it produces an alteration in the expression of their genes counteracting the antiviral defences of the host cell [16].
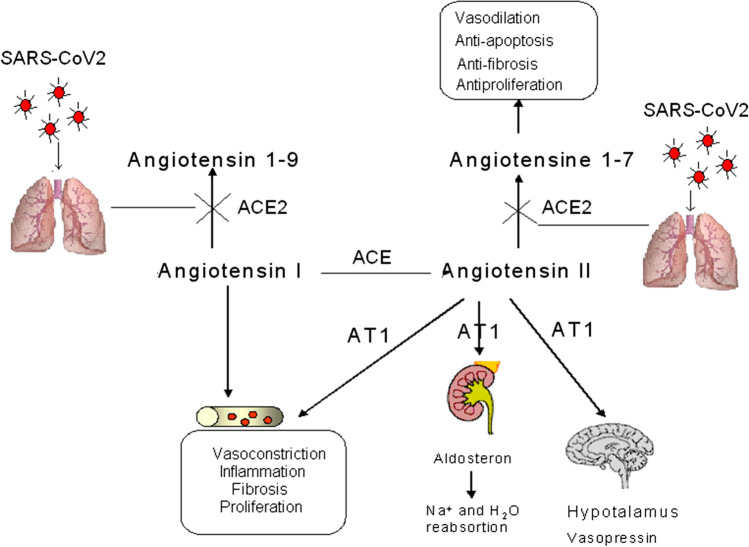
Coronavirus-19 can also cause blood coagulation and hypoxia because when the virus enters the cells through ACE2 this enzyme is inactivated. This enzyme is responsible for passing angiotensin I to angiotensin 1–9 and angiotensin II to angiotensin 1–7 (see Fig. 2). When this enzyme is inactivated, an excess of angiotensin I and angiotensin II can be produced. Under this circumstance, an excess of angiotensin I can cause vasoconstriction, inflammation, fibrosis, and proliferation and an excess of angiotensin II can bind to its AT1 receptor, giving also rise to vasoconstriction, inflammation, fibrosis, proliferation, and elevation of aldosterone and vasopressin. Then, ACE2 inhibition can be responsible for coagulation and as consequence to hypoxia. This hypoxia, mediated by coronavirus-19, may be responsible for the brain damage.
Fig. 2.
Possible mechanism of ACE2 in COVID-19
The first time that COVID-19 was found to induce harmful haemostatic disorder was reported by Guan et al. on 28 February 2020 [17]. These authors observed that out of the 46, 5% of the patients with COVID-19 presented a relevant increase in D-dimer levels. Now, it is suggested that patients with moderate and severe COVID-19 are likely to have reduced platelet number count and prothrombin time (PT), activated partial thromboplastin time (aPTT), and elevated D-dimer levels [18–20]. Several theories were performed to explain these haemostatic changes and high D-dimer levels [21–26]. Both, central and peripheral nervous systems, are affected by COVID-19. Most of the reports about neurological complications are currently developed in China but also in the USA and France among others. Neurological complications such as anosmia [27], stroke [28], paralysis [29], encephalopathy [30], neuropsychiatric alterations such as depression, stress, delirium [31], meningitis [32, 33], seizures [34], and metabolic imbalances were observed in COVID-19-infected patients. The long-term damage of COVID-19 is depression, insomnia, and cognitive problems, which could accelerate Parkinson’s or Alzheimer’s disease [35, 36]; however, more clinical studies are warranted to elucidate a possible impact of SARS-CoV2 in neurodegenerative studies, including Parkinson, Alzheimer, or multiple sclerosis [37].
Two to six percent of acute cerebrovascular disease was found in hospitalised patients with COVID-19 infection. Myalgia/fatigue is also another common post-traumatic stress disorder (PSTD), and anxiety, depression, insomnia, and behavioural alterations are spectrum of neuropsychiatric dysfunctions observed after the acute infection [38]. Many of these neurological dysfunctions can be caused as a consequence of the hypoxia that this virus induces in patients. Some evidence support that COVID-19 can also affect the cardiovascular system. A study in Wuhan observed arterial hypertension and cardiovascular dysfunctions in 15% of the studied patients [39], and stroke dysfunction mediated by coronavirus-19 has been further revised [40]. Some authors consider that the paucity of inflammatory changes in CSF of COVID-19 subject and lack of ARN of SARS-CoV2 do not support the possible dysfunctions of SARS-CoV2 on the neurological complications in COVID-19 [41].
The movement difficulties and even paralysis suffered by COVID-19 patients may be associated with an entry of this virus into peripheral neurons whose myelin is made up of Schwann cells. The death or damage of these cells leads to the demyelination of the peripheral nerves as a result to the difficulty of the conduction of the nerve impulse with the consequent paralysis or decreased mobility. Referent to this point, it has been found COVID-19 patients with typical experiential of acute inflammatory demyelinating polyneuropathy [42–44] and symptoms similar to those of the Guillain–Barre syndrome as weakness or paralysis that can spread to the muscles that control breathing, inducing respiratory dysfunctions to the point that patients need a breathing machine for treatment [45–53]. Other patient was reported with acute motor-sensory axonal neuropathy during the course of the infection but no samples from CSF were taken [54].
If SARS-CoV2 was able to enter to moto-neurons from spinal cord, the problem could be higher because it can produce similar symptoms of that in the amyotrophic lateral sclerosis (ALS) disease.
All these neurological pathologies discussed in this section referred to those in which the coronavirus-19 had not entered the brain.
How COVID-19 virus may enter in brain and infects neurons?
When a pathogen arrives, the CNS is necessary that passes through the blood–brain barrier (BBB). The BBB represents a protection system, which lead to the maintenance of homeostatic functions of the CNS. Its structure is not well known yet. However, endothelial cells take part of brain barrier cells together with pericytes, astrocytes, and microglia.
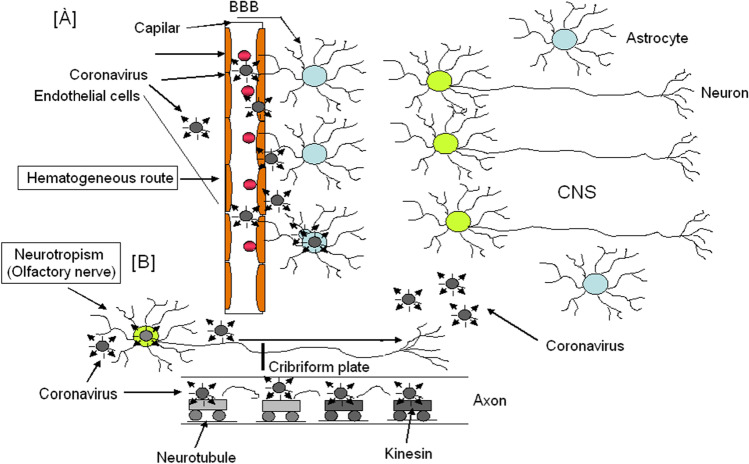
The inflammation could provoke vascular damage that can increase the BBB permeability [55–59]. Then, the virus can cross the BBB through several ways: (a) the hematogenous route through structures that contain less fortified barriers like the choroidal plexus (CP) and circumventricular organs. (b) Infecting peripheral nerves as olfactory nerves [56, 57, 59, 60] arriving to the brain by neurotropism (Fig. 3).
Fig. 3.
Possible mechanism by which SARS-CoV2 can reach the brain. A Haematogenous route. B Neurotropism route
Under this way, the virus can enter in periphery neurons (i.e. the olfactory nerve) by interacting with ACE2 receptor; SARS-CoV2 can move through axons of these cells towards the synapse by anterograde axonal transport, with the cooperation of motor protein called kinesin, which moves molecules along axon microtubules from neuronal soma to the synapse [61–63] (Fig. 3).
Paracellular migration takes place when the virus attacks the tight junctions in BBB [64, 65]. Recently, studies suggest the existence of axonal transport of SARS-CoV2 via the cribriform plate from the olfactory bulb nerves to brain [65]. The fact that the majority of COVID-19 patients present loss of smell (anosmia) [66–68] helps to think that the virus enters the brain through the olfactory nerve. Nevertheless, intranasal infection with SARS-CoV2 to transgenic mice that overexpressing ACE2 (ACE2-HB-01 mice) only caused mild symptoms with pulmonary inflammation but without brain involvement [69]. However, others have been postulated that SARS-CoV2 is reaching the CNS via systemic spread and even through the microcirculation capillary level near the endothelial cells [70].
The high neurotropism of SARS-CoV in animals has been demonstrated from years although symptomatology is not important [71]. These findings suggest a complex neuropathological mechanism of SARS-CoV2 infection in the brain, which seem to be associated with systemic inflammation and hypercoagulopathy states. The first indication that SARS-CoV2 induces meningoencephalitis was reported in a 24-year-old young man who presented altered consciousness, emesis, fever, and seizures and although the presence of the SARS-CoV2 virus was not detected in nasopharyngeal swab, it was detected in the cerebrospinal fluid (CSF) [72]. The presence of SARS-CoV2 in cerebrum spinal fluid has also been confirmed by gene sequencing, in a 56-year-old COVID-19-infected patient [73]. Besides that, a postmortem histological analysis of the brain from a 71-year-old man who died from COVID-19 revealed the presence of several types of lesions, among these was myelin loss [74] and Chu et al. [75] demonstrate that SARS-CoV2 is able to replicate in a human glioblastoma astrocytoma (U251). A review of Favas et al. (2021) give an extend references on the implications of SARS-CoV-2 on different neurological manifestation [76].
Moreover, SARS-CoV2 can infect neurons, given that it contains significant levels of ACE2, and can remain in some neurons without being neurotoxic [77].
The abnormal misfolding and aggregation of proteins in recovered patients from their acute SARS-CoV2 infection could contribute to neuronal loss in the future or promote behavioural alterations [78]. However, traces of SARS-Cov2 have not been detected by PCR in CSF samples from SARS-CoV2-infected patients, except in two cases of meningitis/encephalitis. This feature suggests that acute headache, seizure, and nuchal rigidity may be attributable to meningitis because higher levels of ACE2 are present in meninges [79].
In one study of 125 infected COVID-19 patients, neurological/psychiatric disease was evaluated over a 3-week period; there were 31% of patients whom had altered mental status, 13% showed encephalopathy, 8% had psychosis, 5% had minor cognitive impairment, and 3% had altered affective behaviour. Notably, 62% of patients had a cerebrovascular event, 7% showed an intracerebral haemorrhage, and less than 1% presented CNS vasculitis [80].
Recent studies have detected cerebrovascular problems by COVID-19 infection in patients. In fact, neuroimage studies have found haemorrhage and encephalopathy in a COVID-19-infected female from North America with cough, fever, and altered mental status [81]. Several neurological dysfunctions have been detected in SARS-CoV2-infected patients, who demonstrate that the viral attack is not only in the brain but also in the peripheral central nervous system (PNS) since ACE2 enzymes are present in both organs. All these examples help to consider that SARS-CoV2 could enter in the brain.
Once in the brain, SARS-CoV2 may infect neurons and glial cells because both cell types have ACE-2 enzyme. This can cause cellular death although the immune system could contribute to protect neurons against inflammation and oxidative stress that the virus can induce in the brain. However, it is well recognized that many pathogens can infect the brain causing several dysfunctions and that they also are able to produce immune response [82].
However, there is a problem for the immune cells to cross the BBB. The immune cells are in the blood and need to cross the BBB to arrive to the brain. The passage of T lymphocytes and other immune cells through the BBB does not seem to be an inconvenience because this process takes place in multiple sclerosis (MS) [83, 84]. Besides that, astrocytes and microglia may behave as the first defender of the immune system. Astrocytes are essential for brain homeostasis and for maintaining the BBB integrity and control and activate the immune cell traffic [85]. In addition, under an aggression, astrocytes secrete cytokines and chemokines that activated the immune defences [86] and microglia are the resident monoclonal phagocytes of the brain [87].
The viral infection could alter the immune-mediated responses as a consequence of a systemic propagation. It remains to establish the possible relationship between neurological abnormalities and the cytokine storm observed in some critical patients; the hypercoagulopathy provokes the formation of blood clots in brain vessels [88]. These proinflammatory cytokines associated with storm cytokines could contribute to microglia overactivation and also contribute to blood–brain barrier disruption, leading to neuronal loss and specific neuropsychiatry manifestations such as confusion, disorientation, and headache. In severe cases, encephalitis and vascular damage could lead to ischemia events in patients. The neuroimage analysis evidenced brain-induced dysfunctions and neuropathological manifestations by COVID-19.
Neurological manifestations of COVID-19 in the brain
Liu et al. [89] provided evidence for brain infection with SARS-CoV-2 and presented a neurological mechanism underlying the lethality of this virus infection. The long-term sequels of COVID-19 are depression, insomnia, and cognitive and behavioural problems. It has been observed that between 2 and 6% of patients hospitalized with COVID-19 presented cardiovascular diseases, myalgias, and fatigue.
It is also being observed that 31–50 months after the acute infection by SARS-CoV2, these people presented an extended spectrum of neuropsychiatry sequel such as anxiety, depression, insomnia, and behavioural alterations and even, some small number of patients, developed encephalitis and acute neuropathies such as Guillain-Barré syndrome [90]. Non-specific headache is also common in patients. Many COVID-19 patients show post-sepsis syndrome and pro-inflammatory hypercoagulable state by increasing C-reactive protein, D-dimer, and ferritin markers in those patients with cerebrovascular events. Characteristic cytokine storm incites severe metabolic changes and can provoke multiple organ failure. However, the cytokine storm in COVID-19 can cause a series of small punctuate strokes without inducing neurological alterations [81]. The presence of comorbidities like diabetes, hypertension, and obesity can aggravate pathological manifestations of COVID-19 [91]. However, it is not clear if these neurological abnormalities are caused by COVID-19 itself, or by a cytokine storm, resulting in hypercoagulopathy and formation of blood clots in brain vessels. Ramlall et al. [92] found that the age and coagulation dysfunctions predispose patients to poor clinical outmodes following SARS-CoV2 infections. Coagulopathies may manifest with ischemic or haemorrhagic stroke. In addition, the proinflammatory cytokine storm promotes dysfunction over-activation and also contributes to blood–brain barrier disruption, leading to neuronal loss and consequently to neuropsychiatric manifestations. SARS-CoV2 also could induce demyelization lesions in neurons of the spinal cord which could lead to movement dysfunction [93].
Several neuroimage studies in patients with COVID-19 have demonstrated encephalitis/meningitis [94, 95], haemorrhagic posterior reversible [96], cerebral venous thrombosis [74], and acute ischemic stroke [97] and encephalopathy in a North American COVID-19-infected female that had cough, fever, and altered mental status [83].
Several neurological manifestations were observed in 49 SARS-CoV-2 PCR positive patients (nasopharyngeal samples) [81]. All patients required treatment on ICU for severe COVID-19; 45 had been discharged from ICU at the time of this publication, 26 of 40 patients had confusion, 39 had corticospinal tract signs, and 15 presented transient ischemic attack, partial epilepsy, and mild cognitive impairment [98]. None of them had pleiocytosis in the CSF; in 13 patients who had brain MRI analysis, eight had enhancement in leptomeningeal spaces; finally, two patients had acute ischemic stroke, and one had subacute ischemic stroke. Another study has shown that 13 of the 221 SARS-CoV2-infected patients had imaging-confirmed evidence of cerebrovascular disease [99]. The increased risk of hypercoagulopathy [100] is consistent with cerebral angiography and venography images in patients since blood clots can lead to myocardial infarctions, pulmonary embolisms, and renal failure [101].
Zhao et al. [102] reported a male of 66 years old admitted with fever, dyspnoea, and asthma; 5 days after respiratory symptom onset, this patient developed acute flaccid paralysis of lower limbs and urinary and faecal incontinence. The MRI analysis reported lacunars infarcts. This patient was treated with moxifloxacin, oseltamivir, lopinavir–ritonavir, ganciclovir, and meropenem, followed by dexamethasone and intravenous immunoglobulin for neurological symptoms, in addition, required oxygen and still unable to walk after rehabilitation.
Mao et al. [103] have reported lower lymphocyte levels and platelet in conjunction with higher blood urea nitrogen levels in patients with severe COVID-19 symptomatology than in those without brain symptoms; these patients had impaired consciousness and severe respiratory disease. These also reported five patients who had ischemic strokes and one patient who had intracranial haemorrhage and cases of encephalomyelitis, and multiple sclerosis has been also reported in SARS-CoV2-infected patients [104, 105]. Wong et al. [106] have described a case of ataxia in a male from the UK (40 years old) with diploid oscillopsia, and bilateral facial weakness (rhom-bencephalitis), 13 days before he had fever and progressive shortness of breath on exertion. His white cell count was normal but lymphopenia and raised CRP were found in this patient; brain MRI analysis displayed a lesion in the right inferior cerebella peduncle and also micro-haemorrhage.
Long COVID-19 syndrome
Many patients who suffered from COVID-19, after having suffered from this disease, commented that they suffered from difficulties in walking and a very marked stage of fatigue to the point of not allowing them to continue with their normal life. This suggests that this disease leaves neurological sequels for a period still unknown.
After almost 2 years of the appearance of SARS-CoV2, it has been found that after suffering and healing the dysfunctions caused by this virus, about 94% of people have found a large number of squeal both at the level of dysfunctions in movement and neurological [107]. These dysfunctions are denominated long COVID-19 syndrome. It was found that the dysfunctions after COVID-19 were dependent of the severity of the disease [108]. Orru et al. [109] presented a study with 507 individuals after suffering from COVID-19. They observed a great persistence of neurological, psychological, and physiological symptoms. All these symptoms can cause a decrease of the quality of life, and further studies are necessary to know the “long COVID” conditions in order to better define the clinical treatments.
Possible treatments
Since SARS-CoV2 is a virus, the form to eradicate it, in addition to be attacked by the patient immune system, is the use of specific antiviral, antibody-based drugs and vaccines. However, in addition to this, it is necessary to have therapies that can alleviate the dysfunctions that the virus produces.
Antivirals
The most used antiviral is Remdesivir but, although this produces some positive effects against SARS-CoV2 squeal, is not entirely effective. This antiviral was created to combat Ebola and its mechanism of action consists in the inhibition of the viral ARN polymerase, preventing the virus division [110]. The Drug Agency recommends prioritizing the use of remdesivir for treatments with a maximum duration of 5 days in hospitalized COVID-19 patients who require supplemental oxygen, but not mechanical ventilation or extracorporeal membrane oxygenation (ECMO).
The cancer drug Aplidin could also be a remedy against COVID-19. Its active component is the “plitidepsin”, extracted from the sea squirt Aplidium albicans. This antiviral seems to be 27 times more effective that remdesivir. The mechanism of action of plitidepsin consists in blocking the protein (eEF1A), a protein elongation factor, which is present in human cells and is used by the virus to reproduce and infect other cells. This means that, if the treatment is effective in humans, a SARS-CoV2 virus mutant will not be able to become resistant to this drug. Actually, the Spanish biopharmaceutical PharmaMar is negotiating the start of the phase III trials and published the results of a preclinical study [111]. The study was carried out with 45 patients from 13 Spanish hospitals with good results and the company is working with the regulatory authorities of Spain and other countries to launch a phase III clinical trial.
Avifavir is an antiviral used against influenza that has been developed from the Japanese antiviral Favipiravir. It is a derivate of pirazinamide, which has been active against several ARN viruses [112]. It is an inhibitor of the RNA polymerase, an enzyme necessary for virus replication. Health authorities have confirmed the effectiveness of this treatment to combat SARS-CoV2 and assure that it will be administered in Russian hospitals. However, in Spain, the Ministry of Health does not recommend its use.
Monoclonal antibody–based drug
Monoclonal antibody–based drugs are an immunotherapy that used monoclonal antibodies to bind specifically to determined cell or proteins in order to be recognized by macrophages and be eliminated. Among the drug used to eradicate SARS-CoV2 is Bamlanivimab, which reduces the risk of developing COVID-19 up to 80%. This therapeutic agent has been developed by the pharmaceutical company Eli Lilly. It is a cocktail of monoclonal antibodies that are bound to the protein S of virus. The therapy is still under investigation and has been authorized in the USA under the heading of Emergency Use Authorization. It is indicated in patients with mild of moderate stage disease and with high risk of progressing to severe stage. Bamlanivimab is not licensed for patients who are hospitalized and require oxygen therapy because it has not been demonstrated efficiency in this patients.
Regeneron is an antibody cocktail of casirivimab and imdevimab devised by Regeneron Pharmaceuticals company to defend against SARS-CoV2. It seems that this drug reduces viral levels and improves symptoms in non-hospitalized COVID-19 patients. The US Food and Drug Administration (FDA) approved on 6/01/2021 the emergency authorization to use Regeneron as a drug against COVID-19. An exploratory analysis with 400 valuable people who were randomized to receive Regeneron was performed. The results showed that the administration of this therapy achieved 100% efficiency in the prevention of symptomatic infection.
Vaccines are important to eradicate SARS-CoV2 but there is a problem because this virus is mutating, and it has several strains, the English, first detected in England, the South African, and the Brazilian. Now, the English strain seems to be mutating into a new strain. This is of grand worry because it is not known whether the new vaccines designed for original SARS-CoV2 could work against mutant virus strains. For this reason, to reach a good treatment for COVID-19 would be a good solution.
Actually there are six vaccines against SARS-CoV2:
Pfizer/BioNTech, the name of this vaccine is BNT162b2. It has been designed by the USA (Pfizer) and Germany (BioNTech) and reports 95% effectiveness in preventing symptomatic infections. This vaccine uses ARNm as antigen; this is a mRNA against the Protein S of the virus.
Modern, designed by the USA, with 94% effective in preventing symptomatic infections, but it seems that it is not actually for people over 65 years. This vaccine also uses ARNm as antigen. The name of this vaccine is ARNm-1273. This vaccine is recommended for people 18 years old or older.
Sputnik V of Russia. This vaccine uses two common cold viruses, called adenovirus 5 and adenovirus 26, to transport the genetic material forms the virus protein to the body.
Novavax: uses virus-like nanoparticles as base, which coat them with genetically modified pieces of the coronavirus proteins. It is 89.3% effective on average: 95.6% against the original coronavirus-19 and 85.6% effective against the variant first identified in the UK. It appeared to be less effective against a variant first identified in South Africa. This vaccine is in phase III. Preliminary data from this phase are based on the results obtained in the UK with 15,000 volunteers and given an efficacy of 90% after the administration of two doses. Novavax is an American company that has reached an agreement with Biofabi, a subsidiary of the Zendal group, so that the Galician (Spain) company can produce its vaccines in Europe if it is accepted.
Oxford-Astrazeneca designed by England and Switzerland uses a viral vector and has an efficiency of about 70%. This vaccine will not be administered to people older than 65 years. According to the later studies, this vaccine reduces the transmission of SARS-CoV2 and it seems that distancing the supply of the second dose to 3 months increases its effectiveness. This vaccine has to be approved by the European Union (EU).
Johnson&Johnson: designed by USA, uses a viral vector and has 66% efficiency in global trial, but 85% effective against severe disease.
Sinopharm: designed in China, it uses the SARS-CoV2 inactive by chemicals. Data on vaccine efficiency has not been published.
All then, except the Russian vaccine, are approved by the European Medicines Agency (EMA). The Russian vaccine is being used by Russia and other subAmerican countries and has recently been accepted by Europe and is pending acceptance by the EMA. The Sputnik V is 91.6% of effective in preventing symptomatic COVID-19 and 100% effective in preventing severe coronavirus disease according to an interning analysis of data from phase III trial published in the medical journal The Lancet.
Other drugs
Lei et al. [113] generated a recombinant protein (ACE2-Ig) that contains an ACE2 mutant with low catalytic activity. When these authors checked the inhibitory activities of the ACE2 fusion proteins against SARS-CoV2 comparing with those against SARS-CoV, they found that both SARS-CoV and SARS-CoV2 were potentially neutralized by ACE2 and mACE2-Ig. In mouse models, the administration of rhACE2 shown inhibition of myocardial remodelling and also attenuates angiotensin II-induced cardiac hypertrophy as well as dysfunctions—provoked by viral infection [114] or renal oxidative stress, inflammation, and fibrosis. rhACE2 could be an emerging way in regulating the rennin-angiotensin system [115] as well as in SARS-CoV2 treatment [116]. However, in human and mice, rhACE2 exhibits a fast clearance, with a half-life of 1 h in human and mice [117]. From these results, some researches conclude that despite that ACE2 is a key functional receptor for coronavirus infection, practical use of the rhACE2 protein fusion may be impeded by the short half-life of rhACE2. However, there are other groups of research that consider that injection of human recombinant ACE2 (2hACE2) could be useful for treatment of acute respiratory distress syndrome (ARDS) as well as pulmonary arterial in human hypertension [118]. However, potential adverse effects as hypotension were reported in patients [119]. Recently, some authors reported that rhACE2 could significantly inhibit SARS-CoV2 infection in Vero-E6 cells and human capillary and kidney; these findings suggest that rhACE2 may not only reduce lung injury but also block entry of SARS-CoV2 in target cells. Taken together, these findings need to be confirmed in SARS-CoV2 clinical trials.
As the rhACE2 (recombinant ACE-2) treatment is not yet accurate, it would be necessary to explore new treatments. However, given the variety of symptoms, these treatments must be personalized. The asymptomatic patients do not need any medication since the immune system works properly and eradicates the virus. As inflammation is the most characteristic symptom of COVID-19, the use on anti-inflammatory drugs such as “curcumin” or non-steroidal anti-inflammatory drugs could be a good treatment. Dexamethasone (DEX), a steroid corticosteroid, could promote immunosuppressive effects and this is detrimental for the immune system to eradicate the virus. Therefore, corticoid treatment may have adverse secondary effects [120]. The use of antiviral would be efficient if a specific antiviral against SARS-CoV2 existed; however, it seems that “remdesivir” seems to work relatively well in the case of SARS-CoV2; therefore, its administration could be applied.
The use of anticoagulants as aspirin or low molecular weight heparin in patients with altered coagulation is important especially in those patients with severe breathing dysfunction that need a respiratory machine, since the coagulated blood decreases or even prevents the interchange between CO2/O2 [121]. Coagulation may be a consequence of the inhibition of ACE2 by SARS-CoV2 when it enters the cell. Inhibition of ACE2 would increase angiotensin II accumulation, which binds to its AT1 receptor, and promote vasoconstriction, fibrosis, and proliferation. The administration of losartan (an AT1 antagonist) could be also a good treatment because this can prevent the formation of blood clots due to vasoconstriction. Administration of tissue plasminogen activator (t-PA) is another alternative since a study has reported beneficial effects in three infected patients by SARS-CoV2 [122].
Finally, the use of either synthetic monoclonal antibodies or from people who have suffered from COVID-19 can be a good therapy, at least at the beginning of the disease, to avoid a serious stage of it.
Conclusion
The treatment that should be given to a patient must be personalized taking into account the symptoms that he presents. First, the patient’s condition must be checked and if he still does not have symptoms, it may be advisable to administer antivirals or antibodies to help the patient reduce his viral load.
If the patient has altered the coagulation parameters, the O2 levels, and the thoracic plate, anticoagulants, O2, and anti-inflammatories should be administered, because this would indicate that the virus is invading, at least, their lung cells. The used anticoagulants could be heparin, aspirin, or even plasminogen activator (t-PA) depending on the coagulation stage of the patient. This treatment would prevent the blood clot and allow the blood to carry O2/CO2 normally. Anti-inflammatories should be supplied because probably the patient can develop a cytokine storm, which leads to inflammatory responses. These treatments could be non-steroidal anti-inflammatory as dexamethasone (DEX); DEX is also an immunitary depressor, but other anti-inflammatory like curcumin could promote anti-inflammatory responses. The supplied oxygen and its application will depend on the condition of patient/s. Recent papers discuss the possible connection between Parkinson diseases and COVID-19.
Author contribution
JJ. Merino: Conceived and evaluated the study.
A. Macho González: Searched bibliography.
J. Benedi: Reviewed the study.
M.P. González: Wrote and evaluated the paper.
Data availability
This study has used reviews and scientific studies from doctors who have been in the forefront to fight the virus. This documentation has been performed using Pubmed references that obtained the terms of neurological COVID-19, SARS-CoV2 and icshemia, SARS-CoV-2 and stroke, SARS-CoV-2 and CNS, COVID 19, and neurological disease.
Taking into account the behaviour of this virus and available treatments, this review presents personal criteria on how this virus should be treated; although there are currently vaccines, it may not completely resolve the fact that there are infections by resurgent SARS-CoV2 strains that do not respond to the vaccines.
Declarations
Ethical approval
None.
Conflict of interest
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gorbalenya AE, Baker SC, Baric RS, de Groot RJ, Drosten Ch, Gulyaeva AA, et al. Severe acute respiratory syndrome-related coronavirus: the species and its viruses – a statement of the Coronavirus Study Group. Nat Microbiol. 2020;5(4):536–544. doi: 10.1101/2020.02.07.937862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chakraborty C, Sharma AR, Sharma G, Bhattacharya M. SARS-CoV-2 causing pneumonia-associated respiratory disorder (COVID-19): diagnostic and proposed therapeutic options. Eur Revi Med Pharmacol Sci. 2020;24(7):4016–4026. doi: 10.26355/eurrev_202004_20871. [DOI] [PubMed] [Google Scholar]
- 3.Kumar Garg R, Paliwal VK, Gupta A. Encephalopathy in patients with COVID-19: a review. J Med Virol. 2020;93:206–222. doi: 10.1002/jmv.26207. [DOI] [PubMed] [Google Scholar]
- 4.Reddy ST, Garg T, Shah C, Nascimento FA, Imran R, Kan P, Bowry R, González N, Barreto A, et al. Cerebrovascular disease in patients with COVID-19: a review of the literature and case series. Case Rep Neurol. 2020;12:199–209. doi: 10.1159/000508958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang H, Li T, Barbarino P, Gauthier S, Brodaty H, Molinuevo JL, Xie H, Sun Y, Yu E, et al. Dementia care during COVID-19. The Lancet. 2020;395(10231):1190–1191. doi: 10.1016/S0140-6736(20)30755-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cipriani G, Di Fiorin M. Access to care for dementia patients suffering from COVID-19. Am J Geriatric Psychiatry. 2020;28(7):796–797. doi: 10.1016/j.jagp.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bostancioglu M. Severe acute respiratory syndrome coronavirus 2 is penetrating to dementia research. Curr Neurovasc Res. 2020;17(4):342–342. doi: 10.2174/1567202617666200522220509. [DOI] [PubMed] [Google Scholar]
- 8.Ferrão FM, Lara LS, Lowe J. Renin-angiotensin system in the kidney: what is new? World J Nephrol. 2014;3(3):64–76. doi: 10.5527/wjn.v3.i3.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Catarata MJ, Ribeiro R, Oliveira MJ, Cordeiro CR, Medeiros R. Renin-angiotensin system in lung tumor and microenvironment interactions. Open Ophthalmol J. 2020;11:122–142. doi: 10.2174/1874364101711010122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ocaranza MP, Riquelme JA, García L, Jalil JE, Chiong M, Santos RAS, Lavandero S. Counter-regulatory renin–angiotensin system in cardiovascular disease. Nat Rev Cardiol. 2020;17(2):116–129. doi: 10.1038/s41569-019-0244-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cosarderelioglu C, Nidadavolu LS, George CJ, Oh ES, Bennett DA, Walston JD, Abadir PM. Brain renin–angiotensin system at the intersect of physical and cognitive frailty. Front Neurosci. 2018;14(586314):1–29. doi: 10.3389/fnins.2020.586314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abbott NJ, Patabendige AAK, Dolman DEM, Yusof SR, Begley DJ. Structure and function of the blood–brain barrier. Neurobiol Dis. 2010;37:13–25. doi: 10.1016/j.nbd.2009.07.030. [DOI] [PubMed] [Google Scholar]
- 13.Divani AA, Andalib S, Di Napoli M, Lattanzi S, Hussain MS, Biller J, McCullough LD, et al. Coronavirus disease 2019 and stroke: clinical manifestations and pathophysiological insights. J Stroke Cerebrovas Dis. 2020;29(8):1–12. doi: 10.1016/j.jstrokecerebrovasdis.2020.104941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tabata S, Imai K, Kawano S, Ikeda M, Kodama T, Myyoshi K, Obinata H, Mimura S, et al. Clinical characteristics of COVID-19 in 104 people with SARS-CoV-2 infection on the Diamond Princess cruise ship: a retrospective analysis. Lancet Infect Dis. 2020;20:1043–1050. doi: 10.1016/S1473-3099(20)30482-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fehr AR , Perlman S (2015) Coronaviruses: an overview of their replication and pathogenesis. Helena Jane Maier et al. (eds.), Coronaviruses: methods and protocols, methods in molecular biology, 1282. Springer Science Business Media New York. 10.1007/978-1-4939-2438-7_1 [DOI] [PMC free article] [PubMed]
- 16.Casas Rojo JM, Antón Santos JM, Millán Núñez-Cortés J, Lumbreras-Bemejo C, et al. Clinical characteristics of patients hospitalized with COVID-19 in Spain: results from the SEMI-COVID-19. Revista Clinica Española (English Edition) 2020;220(8):40–494. doi: 10.1101/2020.05.24.20111971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guan WJ, Ni ZY, Hu Y, Liang W, Ou Ch, He J-X, Liu L, Shan H, Lei Ch-L, Hui DSC, et al. China Medical Treatment Expert Group for Covid-19. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Wilde AH, Snijder EJ, Kikkert M, Van Hemert MJ. Host factors in coronavirus replication. Current Topics Microbiol Immunol. 2018;419:1–42. doi: 10.1007/82-2017-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395:1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chams N, Chams S, Badran R, Shams A, Araja A, Raad M, Mukhopadhyay S, Stroberg E, et al. (2020) COVID 19: a multidisciplinary review. Front Public Health. 2020;8(383):1–20. doi: 10.3389/fpubh.2020.00383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gando S, Levi M, Toh C-H. Disseminated intravascular coagulation. Nat Rev Dis Prim. 2016;2:1–16. doi: 10.1038/nrdp.2016.37. [DOI] [PubMed] [Google Scholar]
- 22.Iba T, Levy JH, Raj A, Warkentin TE. Advance in the management of sepsis-induced coagulopathy and disseminated intravascular coagulation. J Clin Med. 2019;8(5):728–744. doi: 10.3390/jcm8050728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gupta N, Zhao Y-Y, Evans CE. The stimulation of thrombosis by hypoxia. Thromb Res. 2019;181:77–83. doi: 10.1016/j.thromres.2019.07.013. [DOI] [PubMed] [Google Scholar]
- 24.Dolhniko M, Duarte-Neto NA, de Almeida Monteiro RA, Ferraz da Silva LF, de Oliveira EP, et al. Pathological evidence of pulmonary thrombotic phenomena in severe COVID-19. J Thromb Haemost. 2020;18(6):1517–1519. doi: 10.1111/jth.14844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marongiu F, Grandone E, Barcellona D. Pulmonary thrombosis in 2019-nCoV pneumonia? J Thromb Haemost. 2020;00:1–3. doi: 10.1111/jth.14818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marchandot B, Sattle L, Jesel L, Matssudhita K, Schini-Kerth V, grunebaum L, Morel O, COVID-19 related coagulopathy: a distinct entity? J Clin Med. 2020;9(6):1651–1668. doi: 10.3390/jcm9061651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lopez-Gros J, Iglesias Coma M, González Farré M, Serra Pujadas C. Alteraciones del olfato en la COVID-19, revisión de la evidencia e implicaciones en el manejo de la pandemia. Acta Otorrinolaringol Esp. 2020;71(6):379–385. doi: 10.1016/j.otorri.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhao J, Li H, Kung D, Fisher M, Shen Y, Liu R. Impact of the COVID-19 epidemic on stroke care and potential solutions. Stroke. 2020;51(7):1996–2001. doi: 10.1161/STROKEAHA.120.030225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sheraton M, Deo N, Kashyap R, Surani S. A review of neurological complications of COVID-19. Cureus. 2020;12(5):c8192. doi: 10.7759/cureus.8192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Saeeda S, Ghufran M, Abeer A, Ahmed M. COVID-19-associated encephalopathy: neurological manifestation of COVID-19. Radiol Case Rep. 2020;15(9):1646–1649. doi: 10.1016/j.radcr.2020.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ellul M, Benjamin L, Singh B, Lant S, Michael BD, Easto A, et al. Neurological associations of COVID-19. Lancet Neurol. 2020;19:767–783. doi: 10.1016/S1474-4422(20)30221-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, Ueno M, et al. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis. 2020;94:55–58. doi: 10.1016/j.ijid.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shin SY, Kwon KCh, Park JW, Kim JM, Shn SY, Koo SH. Evaluation of the Seeplex Meningitis ACE Detection kit for the detection of 12 common bacterial and viral pathogens of acute meningitis. Ann Lab Med. 2012;32(1):44–49. doi: 10.3343/alm.2012.32.1.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Asadi-Pooya AA. Seizures associated with coronavirus infections. Seizure. 2020;79:49–52. doi: 10.1016/j.seizure.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cohen ME, Eichel R, Steiner-Birmanns B, Janah A, Ioshpa M, Bar-Shalom R, Paul JJ, Gaber H, Skrahina V, Bornstein NM, Yahalom G. A case of probable Parkinson’s disease after SARS-CoV-2 infection. Lancet Neurol [Internet] 2020;19(10):804–805. doi: 10.1016/S1474-4422(20)30305-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Buccafusca M, Micali C, Autunno M, Versace AG, Nunnari G, Musumeci O. Favourable course in a cohort of Parkinson’s disease patients infected by SARS-CoV-2: a single-centre experience. Neurol Sci. 2021;42:811–816. doi: 10.1007/s10072-020-05001-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kumar M, Thakur AK. Neurological manifestations and comorbidity associated with COVID-19: an overview. Neurol Sci. 2020;41:3409–3418. doi: 10.1007/s10072-020-04823-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Varatharaj A, Thomas N, Ellul MA, Davies NWS, Pollak TA, Tenorio EL. Neurological and neuropsychiatric complications of COVID-19 in 153 patients: a UK-wide surveillance study. Lancet Psychiat. 2020;7(10):P875–882. doi: 10.1016/S2215-0366(20)30287-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Huang Ch, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet. 2020;395:497–506. doi: 10.1016/S0140-6736(20)30183-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Divani AA, Andalib S, Di Napoli M, Lattanc S, Hussain MS, Biller J, McCullough LD, et al. Coronavirus disease 2019 and stroke: clinical manifestations and pathophysiological insights. J Stroke Cerebrovasc Dis. 2020;29(8):1–12. doi: 10.1016/j.jstrokecerebrovasdis.2020.104941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Maria A. Garcia, Paula V. Barreras, Allie Lewis, Gabriel Pinilla, Lori J. Sokoll, Thomas Kickler, et al. (2021) Cerebrospinal fluid in COVID-19 neurological complications: no cytokine storm or neuroinflammation. medRxiv Preprint. 10.1101/2021.01.10.20249014 [DOI] [PMC free article] [PubMed]
- 42.Kiandokht Keyhanian, Raffaella Pizzolato Umeton, Babak Mohit, Vahid Davoudi, Fatemeh Hajighasemi, Mehdi Ghasemi (2021) SARS-CoV-2 and nervous system: from pathogenesis to clinical manifestation. J Neuroimmunol. 350: 577436. Published online 2020 Nov 7. 10.1016/j.jneuroim.2020.577436 [DOI] [PMC free article] [PubMed]
- 43.Rossella Talotta, Erle Robertson (2021) Autoimmunity as the comet tail of COVID-19 pandemic. World J. Clin. Cases. 8(17): 3621–3644. Published online 2020 Sep 6. 10.12998/wjcc.v8.i17.3621 [DOI] [PMC free article] [PubMed]
- 44.Parménides Guadarrama-Ortiz, José Alberto Choreño-Parra, Claudia Marisol Sánchez-Martínez, et al (2021) Neurological aspects of SARS-CoV-2 infection: mechanisms and manifestations. Front Neurol. 11: 1039. Published online 2020 Sep 4. 10.3389/fneur.2020.01039 [DOI] [PMC free article] [PubMed]
- 45.Alberti P, Beretta S, Piatti M, Karantzoulis A, Piatti ML, Santoro P, Viganò M, Giovannelli G, et al. Guillain-Barre syndrome related to COVID-19 infection. Neurol Neuroimmunol 20 Neuroinflamm. 2020;7(4):1–3. doi: 10.1212/NXI.0000000000000741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zhao H, Shen D, Zhou H, Liu J, Chen S. Guillain-Barre syndrome associated with sars-cov-2 infection: causality or coincidence? Lancet Neurol. 2020;19(5):383–384. doi: 10.1016/S1474-4422(20)30109-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ottaviani D, Boso F, Tranquillini E, Gapeni I, Pedrotti G, Cozzio S, Guarrera GM, Giometto B. Early Guillain-Barré syndrome in coronavirus disease 2019 (COVID-19): a case report from an Italian COVID-hospital. Neurol Sci. 2020;41(6):1351–1354. doi: 10.1007/s10072-020-04449-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Su XW, Palka SV, Rao RR, Chen FS, Cambi F. SARS-CoV-2 associated Guillain-Barre syndrome with dysautonomia. Muscle Nerve. 2020;62(2):E48–E51. doi: 10.1002/mus.26988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Padroni M, Mastrangelo V, Asioli GM, Pavolucci L, Abu-Rumeileh S, Piscaglia MG, et al. Guillain-Barre syndrome following COVID-19: new infection, old complication? J Neurol. 2020;267(7):1877–1879. doi: 10.1007/s00415-020-09849-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Camdessanche JP, Morel J, Pozzetto B, Paul S, Tholance Y, Bothelho-Nevers E. COVID-19 may induce Guillain-Barre syndrome. Rev Neurol. 2020;176(6):516–518. doi: 10.1016/j.neurol.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Arnaud S, Budowsk C, Wing Tin SN, Degos B. Post SARS-CoV-2 Guillain-Barré syndrome. Clin Neurophysiol. 2020;131(7):1652–1654. doi: 10.1016/j.clinph.2020.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Scheidl E, Canseco DD, Hadji-Naumov A, Bereznai B. Guillain-Barré syndrome during SARS-CoV-2 pandemic: a case report and review of recent literature. J Peripher Nerv Syst. 2020;25(2):204–207. doi: 10.1111/jns.12382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Gigli GL, Bax F, Marini A., Pelliteri G, Scalise A, Surcinelli A, Valente M (2020) Guillain-Barré syndrome in the COVID-19 era: just an occasional cluster? J Neurol 1–3. 10.1007/s00415-020-09911-3 [DOI] [PMC free article] [PubMed]
- 54.Jiang X, Andjelkovic AV, Zhu L, Yang T, Bennetti MVL, Chen J, Keep RF, Shi Y (2017) Blood-brain barrier dysfunction and recovery after ischemic stroke. Prog Neurobiol 163–164: 144–171. 10.1016/j.pneurobio.2017.10.001 [DOI] [PMC free article] [PubMed]
- 55.Sweeney MD, Zhao Z, Montagne A, Neloson AR, Zlokivic BV. Blood-brain barrier: from physiology to disease and back. Physiol Rev. 2018;99(1):21–78. doi: 10.1152/physrev.00050.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Abdullahi W, Tripathi D, Ronaldso PT. Blood-brain barrier dysfunction in ischemic stroke: targeting tight junctions and transporters for vascular protection. Am J Physiol Cell Physiol. 2018;315(3):C343–C356. doi: 10.1152/ajpcell.00095.2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Dahm T, Rudolph H, Schwerk C, Schroten H, Tenenbaum T (2016) Neuroinvasion and inflammation in viral central nervous system infections. Mediators Inflamm: 1-16. 10.1155/ 2016/ 8562805 [DOI] [PMC free article] [PubMed]
- 58.Swanson PA, McGavern DB. Portals of viral entry into the central nervous system. In: Dorovini-Zis K, ed. (2015). The blood-brain barrier in health and disease, volume two: pathophysiology and pathology, Cleveland, OH:CRC Press.
- 59.Azalea TP, Espiritu AI, Apor ADAO, Jamora RDG. Neuropathologic findings of patients with COVID-19: a systematic review. Neurol Sci. 2021;42:1255–1266. doi: 10.1007/s10072-021-05068-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Desai I, Manchanda R, Kumar N, Tiwari A, Kumar M. Neurological manifestations of coronavirus disease 2019: exploring past to understand present. Neurol Sci. 2021;42:773–785. doi: 10.1007/s10072-020-04964-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lahiri D, Mondal R, Deb S, Bandyopadhyay D, Shome G, Sarkar S, Biswas SC. Neuroinvasive potential of a primary respiratory pathogen SARS-CoV2: Summarizing the evidences. Diab Metabol Syndrome. 2020;14(5):1053–1060. doi: 10.1016/j.dsx.2020.06.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Marx A, Müller J, Mandelkow EM, Hoenger A, Mandelkow E. Interaction o kinesis motors, microtubules, and MAPs. J Muscle Res Cell Motil. 2006;27:125. doi: 10.1007/s10974-005-9051-4. [DOI] [PubMed] [Google Scholar]
- 63.Dodding MP, Way M. Coupling viruses to dynein and kinesin-1. EMBO J. 2011;30:3527–3539. doi: 10.1038/emboj.2011.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bohmwald K, Gálvez NMS, Ríos M, et al. Neurologic alterations due to respiratory virus infections. Front Cell Neurosci. 2018;12:1–15. doi: 10.3389/fncel.2018.00386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Swanson A, McGavern DB (2015) Portals of viral entry into the central nervous system. In: Dorovini-Zis K, ed. The blood-brain barrier in health and disease, volume two: pathophysiology and pathology, Cleveland, OH: CRC Press;. eBook ISBN 9780429075797
- 66.Eliezer M, Hautefort C, Hamel AL, et al (2020) Sudden and complete olfactory loss function as a possible symptom of COVID-19. JAMA Otolaryngol Head Neck Surg 146(7): 1–2. Letter. 10.1001/jamaoto.2020.0832 [DOI] [PubMed]
- 67.Solomon T (2009) Encephalitis, and infectious encephalopathies In: Donaghy M, ed. Brain’s diseases of the nervous system, 12th ed. Oxford: Oxford University Press, 10.1093/med/9780198569381.003.0989
- 68.Benezit F, Le Turnier P, Declerck C, Paillé C, Revest M, Dubée V, Tattevin P, et al. Utility of hyposmia and hypogeusia for the diagnosis of COVID-19. Lancet Infect Dis. 2020;20(9):1014–1015. doi: 10.1016/S1473-3099(20)30297-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bao L, Deng W, Huang B, Gao H, Liu J, Ren L, Wei Q, Yu P, Xu Y, Qi F, Qu Y, et al. The pathogenicity of SARS-CoV-2 in hACE2 transgenic mice. Nature. 2020;583:830–833. doi: 10.1038/s41586-020-2312-y. [DOI] [PubMed] [Google Scholar]
- 70.Deffner F, Scharr M, Klingenstein S, Klingenstein M, Milazzo A, Scherer S, Wagner A,et al (2020) Histological evidence for the enteric nervous system and the choroid plexus as alternative routes of neuroinvasion by SARS-CoV2. Front Neuroanat. 14: 596439. Published online 2020 Oct 6. 10.3389/fnana.2020.596439 [DOI] [PMC free article] [PubMed]
- 71.Conceicao C, Thakur N, Human S, Kelly JT, Logan L, Bialy D, Bhat S, Stevenson-Leggett P,et al. (2020) The SARS-CoV-2 Spike protein has a broad tropism for mammalian ACE2 proteins. PLoS Biol. 18(12): e3001016. Published online 2020 Dec 21. 10.1371/journal.pbio.3001016 [DOI] [PMC free article] [PubMed]
- 72.Moriguchi T, Harii N, Goto J, Harada D, Sugawara H, Takamino J, Ueno M, Sakata H, Kondo K, et al. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int J Infect Dis. 2020;94:55–58. doi: 10.1016/j.ijid.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhou L, Zhang M, Wang J, Gao J (2020) Sars-Cov-2: underestimated damage to nervous system. Travel Med Infect Dis 36, 2020, 101642. Letter. 10.1016/j.tmaid.2020.101642 [DOI] [PMC free article] [PubMed]
- 74.Reichard RR, Kashani KB, Boire NA, Constantopoulos E, Guo Y, Lucchinetti CF. Neuropathology of Covid-19: a spectrum of vascular and acute disseminated encephalomyelitis (ADEM)-like pathology. Acta Neuropathol. 2020;140(1):1–6. doi: 10.1007/s00401-020-02166-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Chu H, Chan JFW, Yuen TTT, Shuai H, Yuan S, Wang Y, Hu B, Yip CCY, Tsang JOL, Huang X, Chai Y. Comparative tropism, replication kinetics, and cell damage profiling of SARS-CoV-2 and SARS-CoV with implications for clinical manifestations, transmissibility, and laboratory studies of COVID-19: an observational study. The Lancet Microbe. 2020;1(1):e14–e23. doi: 10.1016/S2666-5247(20)30004-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Favas TT, Dev P, Chaurasia RN, Chakravarty K, Mishra R, Joshi D, Mishra VN, Kumar A, Singh VK, Pandey M, Pathak A (2021) Neurological manifestations of COVID-19: a systematic review and meta-analysis of proportions. Neurol Sci (2020) 41:3437–3470. 10.1007/ s10072-020-04801-y [DOI] [PMC free article] [PubMed]
- 77.Meinhardt J, Radke J, Dittmayer C, Mothes R, Franz J, Laue M, Schneider J, Brünink S, et al. Olfactory transmucosal SARS-CoV-2 invasion as port of Central Nervous System entry in COVID-19 patients. Nat Neurosci. 2020;24:168–175. doi: 10.1038/s41593-020-00758-5. [DOI] [PubMed] [Google Scholar]
- 78.Ye M, Ren Y, Lv T. Encephalitis as a clinical manifestation of COVID-19. Brain Behav, Immun. 2020;88:945–946. doi: 10.1016/j.bbi.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Mark AE, Benjamin L, Singh B, Lant S, Michael BD, Easton A, Kneen R, Defres S, et al (2020) Neurological associations of COVID-19. Lancet Neurol. 19(9): 767-783. 10.1016/S1474-4422 (20)30221-0. [DOI] [PMC free article] [PubMed]
- 80.Oxley TJ, Mocco J, Majidi S, Kellner Ch, Shoirah H, Shingh IP, De Leacy RA, et al. Large-vessel stroke as a presenting feature of Covid-19 in the young. N.Engl. J Med. 2020;382:1–3. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Helms J, Kremer S, Merdji H, Clere-Jehl R, Schenck M, Kummerlen CH, Collange O, et al. Neurologic features in severe SARS-CoV-2 infection. N Engl J Med. 2020;382:2268–2270. doi: 10.1056/NEJMc2008597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Dando SJ, Mackay-Sim A, Norton R, Currie BJ, St John JA, Ekberg JAK, Batzloff M, et al. Pathogens penetrating the central nervous system: infection pathways and the cellular and molecular mechanisms of invasion. Clin Microbiol Rev. 2014;27(4):691–726. doi: 10.1128/CMR.00118-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Sweeney MD, Zhao Z, Montagne A, Nelson AR, Zlokovic BV. blood-brain barrier: from physiology to disease and back. Physiol Rev. 2019;99(1):21–78. doi: 10.1152/physrev.00050.2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Wilson EH, Weninger W, Hunter ChA. Trafficking of immune cells in the central nervous system. J Clin Invest. 2010;120(5):1368–1379. doi: 10.1172/JCI41911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Abbott NJ, Ronnback L, Hansson E. Astrocyte-endothelial interactions at the blood-brain barrier. Nat Rev Neurosci. 2006;7:41–53. doi: 10.1038/nrn1824. [DOI] [PubMed] [Google Scholar]
- 86.Dong Y, Benveniste EN. Immune function of astrocytes. Glia. 2001;36:180–190. doi: 10.1002/glia.1107. [DOI] [PubMed] [Google Scholar]
- 87.Klein RS, Garber Ch, Funk KE, Salami H, Soung A, Kanmogne M, Manivasagam S, Agner S, Cain M. Neuroinflammation during RNA viral infections. Annu Rev Immunol. 2019;37:73–95. doi: 10.1146/annurev-immunol-042718-041417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Iadecola C, Anrather J, Kamel H. Effects of COVID-19 on the nervous system. Cell. 2020;183(1):16–27. doi: 10.1016/j.cell.2020.08.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Liu JM, Tan BH, Wu S, Gui Y, Suo JL, Li YC. Evidence of central nervous system infection and neuroinvasive routes, as well as neurological involvement in the lethality of SARS-CoV-2 infection. J Med Virol. 2021;93(3):1304–1313. doi: 10.1002/jmv.26570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Fotuhi M, Mian A, Meysami S, Raji CA. Neurobiology of COVID-19. J Alzheimers Dis. 2020;76(1):3–19. doi: 10.3233/JAD-200581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.McGavern DB, Kang SS. Illuminating viral infections in the nervous system. Nat Rev Immunol. 2011;11(5):318–329. doi: 10.1038/nri2971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ramlall V, Thangaraj PM, Meydan C, Foox J, Butler D, Kim J, May B, De Freitas JK, Glicksberg BS, et al. Immune complement and coagulation dysfunction in adverse outcomes of SARS-CoV-2 infection. Nat Med. 2020;26(10):1609–1615. doi: 10.1038/s41591-020-1021-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zanin L, Saraceno G, Panciani PP, Renisi G, Signorini L, Migliorati K, Fontanella, MM (2020) SARS-CoV-2 can induce brain and spine demyelinating lesions. Acta Neurochir (Wien) published online May 4. 10.1007/s00701-020-04374-x. [DOI] [PMC free article] [PubMed]
- 94.Zhou J, She Y, Wang XM. Venous thrombosis and arteriosclerosis obliterans of lower extremities in a very severe patient with 2019 novel coronavirus disease: a case report. J Thromb Thrombolysis. 2020;50(1):229–232. doi: 10.1007/s11239-020-02084-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Al-olama M, Rashid A, Garozzo D. COVID-19-associated meningoencephalitis complicated with intracranial hemorrhage: a case report. Acta Neurochir. 2020;162(7):1495–1499. doi: 10.1007/s00701-020-04402-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Franceschi AM, Ahmed O, Giliberto L, Castillo M. Hemorrhagic posterior reversible ncephalopathy syndrome as a manifestation of COVID-19 infection. AJNR Am J Neuroradiol. 2020;41(7):1173–1176. doi: 10.3174/ajnr.A6595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Zhou B, She J, Wang, Y, Ma X (2020) A case of coronavirus disease 2019 with concomitant acute cerebral infarction and deep vein thrombosis, Front Neurol 11. 10.3389/fneur.2020.00296 [DOI] [PMC free article] [PubMed]
- 98.Nepal G, Rehrig JH, Shrestha GS, Shing YK, Yadav JK, Ojha R, Pokhrel G, T ZL, Huang DY (2020) Neurological manifestations of COVID-19: a systematic review. Crit Care 24, 421-432. 10.1186/s13054-020-03121-z [DOI] [PMC free article] [PubMed]
- 99.Choi Y, Lee MK (2020) Neuroimaging findings of brain MRI and CT in patients with COVID-19: a systematic review and meta-analysis. Eur J Radiol. 2020 Dec; 133: 109393. Published online 2020 Nov 3. 10.1016/j.ejrad.2020.109393 [DOI] [PMC free article] [PubMed]
- 100.Spiezia L, Boscolo A, Poletto F, Cerruti L, Tiberio I, Campello E, Navalesi P, Simioni P. COVID-19-related severe hypercoagulability in patients admitted to intensive care unit for acute respiratory failure. Thromb Haemost. 2020;120(6):998–1000. doi: 10.1055/s-0040-1710018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Pasquarelli-do-Nascimento G, Braz-de-Melo HA, Faria SS, de Oliveira SI, Kobinger GP, Magalhaes G. Hypercoagulopathy and adipose tissue exacerbated inflammation may explain higher mortality in COVID-19 patients with obesity. Front Endocrinol (Lausanne) 2020;11:530–546. doi: 10.3389/fendo.2020.00530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhao K, Huang J, Dai D, Feng Y, Liu L, Nie S. Serum iron level as a potential predictor of coronavirus disease 2019 severity and mortality: a retrospective study. Open Forum Infect Dis. 2020;7(7):1–8. doi: 10.1093/ofid/ofaa250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Mao R, Qiu Y, He JS, Tan J-Y, Li X-H, Liang J. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2020;5(7):667–678. doi: 10.1016/S2468-1253(20)30126-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Zhang T, Rodricks MB, Hirsh E (2020) COVID-19-associated acute disseminated encephalomyelitis: a case report. medRxiv. 10.1101/2020.04.16.20068148
- 105.Zhao K, Li R, Wu X, Zhao Y, Wang T, Zheng Z, Zheng S, Ding X, Nie H. Clinical features in 52 patients with COVID-19 who have increased leukocyte count: a retrospective analysis. Eur J Clin Microbiol Infect Dis. 2020;10:2279–2287. doi: 10.1007/s10096-020-03976-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Wong PF, Craik S, Newman P, Makan A, Srinivasan K, Crawford E, Dev D, Moudgil H, Ahmad N (2020) l. Lessons of the month 1: a case of rhombencephalitis as a rare complication of acute COVID-19 infection. Clin Med (Lond) published online May 5. 20(3); 293–294. 10.7861/clinmed.2020 [DOI] [PMC free article] [PubMed]
- 107.Ayman Iqbal, Kinza Iqbal, Shajeea Arshad Ali, Dua Azim, Eisha Farid, Mirza D. Baig, Taha Bin Arif, Mohammad Raza The COVID-19 sequelae: a cross-sectional evaluation of post-recovery symptoms and the need for rehabilitation of COVID-19 survivors. 10.7759/cureus.13080 [DOI] [PMC free article] [PubMed]
- 108.Kamal M, Omirah MA, Hussein A, Saeed H. (2020) Assessment and characterisation of post-COVID-19 manifestations. Epub ahead of print. Int J Clin Pract E e13746. 10.1111/ijcp.13746 [DOI] [PMC free article] [PubMed]
- 109.Orrù G, Bertelloni D, Diolaiuti F, Mucci F, Di Giuseppe M, Biella M, Gemignani A, Ciacchini R, Conversano C (2021) Long-COVID syndrome? A study on the persistence of neurological, psychological and physiological symptoms. Healthcare 9: 575. 10.3390/healthcare9050575 [DOI] [PMC free article] [PubMed]
- 110.Tchesnokov EP, Feng JY, Porter DP, Götte M. Mechanism of inhibition of Ebola virus RNA-dependent RNA polymerase by remdesivir. Viruses. 2019;11(4):326–338. doi: 10.3390/v1104032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.White KM, Rosales R, Yildiz S, Kehrer T, Miorin L, Moreno E, Yangla S, uccellini MB, Rathnasinghe R. (2021) Plitidepsin has potent preclinical efficacy against SARS-CoV-2 by targeting the host protein eEF1A. Science 10.1126/science.Abf4058. https://www.http//cience.sciencemag.org/on Jaanuary 30,2021 [DOI] [PMC free article] [PubMed]
- 112.Premachandran KP, Nambi PS, Ramasubramanian V, Gopalakrishnan R (2020) Avifavir in treating patients with moderate covid 19. Clin Infect Dis. 27: ciaa1601. Published online 2020 Oct 27. 10.1093/cid/ciaa1601 [DOI] [PMC free article] [PubMed]
- 113.Lei Ch, Qian K, Li T, Zhang S, Fu W, Ding M, Hu S. Neutralization of SARS-CoV-2 spike pseudotyped virus by recombinant ACE2-Ig. Nat Commun. 2016;11(1):2070. doi: 10.1038/s41467-020-16048-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Chen L-J, Xu Z-Z, Song B, Yu H-M, Oudit GY, Xu R, Zhang Z-Z, Jin H-Y, Chang Q, et al. Angiotensin-converting enzyme 2 ameliorates renal fibrosis by blocking the activation of mTOR/ERK signaling in apolipoprotein E-deficient mice. Peptides. 2016;79:49–57. doi: 10.1016/j.peptides.2016.03.008. [DOI] [PubMed] [Google Scholar]
- 115.Kuba K, Imai Y, Rao S, Gao H, Guo F, Guan B, Huan Y, Yang P, Zhang Y, Deng W, Bao L, et al. A crucial role of angiotensin converting enzyme 2 (ACE2) in SARS coronavirus-induced lung injury. Nat Med. 2013;11:875–879. doi: 10.1038/nm1267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Guo J, Huang Z, Lin L, LCJ (2020) Coronavirus disease 2019 (COVID-19) and cardiovascular disease: a viewpoint on the potential influence of angiotensin-converting enzyme inhibitors/angiotensin receptor blockers on onset and severity of severe acute respiratory syndrome coronavirus 2 infection. J Amer Heart Association 9 (7): 1–5. 10.1161/JAHA.120.016219 [DOI] [PMC free article] [PubMed]
- 117.Haschke M, Schuster M, poglitsch M, Loibner H, Salzberg M, Bruggisser M, Penninger J, Krähenbühl S, Pharmacokinetics and pharmacodynamics of recombinant human angiotensin-converting enzyme 2 in healthy human subjects. Clin Pharmacokinet. 2013;52(9):783–792. doi: 10.1007/s40262-013-0072-7. [DOI] [PubMed] [Google Scholar]
- 118.Zhang H, Baker A (20017) Recombinant human ACE2: acing out angiotensin II in ARDS therapy. Crit Care 21(1): 305–308. 10.1186/s13054-017-1882-z [DOI] [PMC free article] [PubMed]
- 119.Patel VB, Lezutekong JN, Chen X, Oudit GY. Recombinant human ACE2 and the angiotensin 1–7 axis as potential new therapies for heart failure. Can J Cardiol. 2017;33(7):943–946. doi: 10.1016/j.cjca.2016.12.012. [DOI] [PubMed] [Google Scholar]
- 120.McKay LI, Cidlowski JA (2003) Physiologic and pharmacologic effects of corticosteroids [Efectos fisiológicos y farmacológicos de los corticosteroides. En Kufe, D. W.; Pollock, R. E.; Weichselbaum, R. R., eds. Holland-Frei Cancer Medicine (in english) (6 edition). Hamilton, Ontario: BC Decaer. Copyright 2003, BC Decker Inc.Bookshelf ID: NBK13780.
- 121.Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thrombos Haemostasis. 2020;18:1094–1099. doi: 10.1111/jth.14817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Wang J, Hajizadeh N, Moore EE, McIntyre RC, Moore PK, Veress LA, Yaffe MB, Moore HB, Barrett ChD. Tissue plasminogen activator (tPA) treatment for COVID-19 associated acute respiratory distress syndrome (ARDS): a case series. J Thromb Haemost. 2020;18(7):1752–1755. doi: 10.1111/jth.14828. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
This study has used reviews and scientific studies from doctors who have been in the forefront to fight the virus. This documentation has been performed using Pubmed references that obtained the terms of neurological COVID-19, SARS-CoV2 and icshemia, SARS-CoV-2 and stroke, SARS-CoV-2 and CNS, COVID 19, and neurological disease.
Taking into account the behaviour of this virus and available treatments, this review presents personal criteria on how this virus should be treated; although there are currently vaccines, it may not completely resolve the fact that there are infections by resurgent SARS-CoV2 strains that do not respond to the vaccines.