Abstract
Most of the existing literature concerning the links between built environment and COVID-19 outcomes is based on aggregate spatial data averaged across entire cities or counties. We present neighborhood level results linking census tract-level built environment and active/sedentary travel measures with COVID-19 hospitalization and mortality rates in King County Washington. Substantial variations in COVID-19 outcomes and built environment features existed across neighborhoods. Using rigorous simulation-assisted discrete outcome random parameter models, the results shed new lights on the direct and indirect connections between built environment, travel behavior, positivity, hospitalization, and mortality rates. More mixed land use and greater pedestrian-oriented street connectivity is correlated with lower COVID-19 hospitalization/fatality rates. Greater participation in sedentary travel correlates with higher COVID-19 hospitalization and mortality whereas the reverse is true for greater participation in active travel. COVID-19 hospitalizations strongly mediate the relationships between built environment, active travel, and COVID-19 survival. Ignoring unobserved heterogeneity even when higher resolution smaller area spatial data are harnessed leads to inaccurate conclusions.
Keywords: Transportation, Built environment, Active travel, COVID-19 mortality, COVID-19 hospitalizations, Poisson model, Random parameters, Path analysis
1. Introduction & background
Built environment design significantly impacts public health. The importance of built environment design was well realized in the latter 1800s and early 1900s when infectious diseases (such as Influenza) were the primary public health threat faced by humanity (Frumkin et al., 2004). Over decades, compact built environment design also proved to be effective in combatting noncommunicable chronic diseases, including obesity, diabetes, asthma, and heart diseases (Lopez-Zetina et al., 2006; Xu and Wang, 2015; Ewing et al., 2003; Cerin et al., 2020; Sallis et al., 2020; Sallis et al., 2012; Frank et al., 2006). Recent evidence also suggests that the design of built environment has simultaneous implications for chronic as well as infectious diseases (such as COVID-19) (Megahed and Ghoneim, 2020; Frank and Wali, 2021; Frumkin, 2021). A broad spectrum of studies has documented the multiple mechanisms through which the built environment can influence health (Berrigan and McKinno, 2008; Frank et al., 2019; Jackson, 2003; Rao et al., 2007). Compact and dense (more walkable) environments support active travel and physical activity (Handy et al., 2002; Khattak and Rodriguez, 2005; Saelens and Handy, 2008; Rodríguez et al., 2006; Brownson et al., 2009). Additionally, the features of a “walkable” built environment exhibit an inverse relationship with time spent in cars (sedentary travel) (Frank et al., 2004; Carlson et al., 2015). Causal evidence also suggests that the gains in physical activity and active travel due to being exposed to compact and more walkable environments over time are effective in protecting and prescriptively reducing mortality and morbidity from the chronic disease epidemic (Schmid et al., 2015). For example, more walkable neighborhoods are associated with lower incidence of diabetes (Creatore et al., 2016), obesity and body mass index (Frank et al., 2004; Sallis et al., 2020; Creatore et al., 2016), systolic (SBP in mmHg) and diastolic (DBP in mmHg) blood pressure (Sarkar et al., 2018). Serving as a key foundation for lasting population-level interventions, designing walkable, compact, and activity-supportive built environments has been effective in combating noncommunicable diseases and accomplishing sustainable development goals (WHO, 2018; United Nations, 2020).
The emergence of the highly contagious COVID-19 virus led to discussions about the role of built environment in facilitating COVID-19 spread. The focus has been largely on density as one measure describing the built environment. The discussion started originally with media reports that held (population) density and transit use (features of “Big Cities”) responsible for mortalities from COVID-19 (Shoichet and Jones, 2020). As the COVID-19 pandemic evolved, several studies examined the links between population density and COVID-19 related infection and mortality rates – revealing contradictory results (Li et al., 2021b; Nguyen et al., 2020; Bray et al., 2020; Hamidi et al., 2020a; Hamidi et al., 2020b; Carozzi, 2020; Li et al., 2021a). Greater population density was linked with higher infection rates (Kulu and Dorey, 2021; Nguyen et al., 2020). Other earlier studies on the topic reported negative or no statistically significant correlations between population density and infection rate (Hamidi et al., 2020a; Hamidi et al., 2020b; Carozzi, 2020; Kim et al., 2021). Since denser environments facilitate more interactions and greater proximity among people, one would logically expect a positive correlation between density and COVID-19 infection rate. Regarding mortality rates, Bray et al. (2020) and Kodera et al., (2020) found a positive correlation between mortality and population density, whereas a negative relationship between the two was reported elsewhere (Hamidi et al., 2020a; Hamidi et al., 2020b). Carozzi (2020) reported no statistically significant correlation between COVID-19 mortality and population density. Frank and Wali, 2021 argued that the mechanisms through which the built and natural environment influences COVID-19 infection and severity of illness are quite different. Individuals living in more walkable environments are more likely to survive the illness from COVID-19 due to the health benefits offered by compact and more walkable environments (such as support for greater physical activity and lower chronic disease prevalence). Along these lines, by using a broader range of built and natural environment features, the study assessed the role of chronic disease prevalence in mediating the relationship between built environment and COVID-19 mortality using U.S. county-level data. Statistically significant negative relationships between built and natural environment features and COVID-19 mortality were found when accounting for the mediating effect of chronic disease prevalence (Frank and Wali, 2021). Besides built environment factors, the disparate sociodemographic related impacts of COVID-19 are also documented – with studies showing more severe impacts of COVID-19 in areas with higher deprivation and greater proportion of racial and ethnic minorities (Yang et al., 2021; Kim et al., 2021; Pierce et al., 2021; Gibertoni et al., 2021; Kulu and Dorey, 2021; Harris, 2020).
1.1. Research gaps & objective
Previous studies made important contributions by shedding new light on the role of density as the pandemic evolved. However, several major gaps remain. First, population density has been largely used as a proxy measure to capture the overall level of walkability, yet it is well understood that density alone does not make a place walkable and less car dependent (Cervero and Kockelman, 1997b). There are several other aspects of community design that constitutes a walkable environment including heterogeneity of land uses, and connected street networks along with a supportive pedestrian environment1 (Saelens and Handy, 2008) (Sallis et al., 2018; Khattak and Rodriguez, 2005). Second, reliable estimates of COVID-19 incidence and severity were arguably impossible to gauge early on in the pandemic when several studies focused on this outcome were published. Testing regimes varied considerably and likely also systematically across urban form further confounding the ability to assess how built environments correlate with COVID-19. Denser urban areas may have been more rigorous in their testing procedures early on relative to sprawling lower density suburban areas. Likewise, earlier data on COVID-19 mortality rates were extremely dynamic and changed rapidly by location making it a difficult outcome to pin down. In addition to the focus of previous studies on density as a key built environment measure discussed earlier, this may explain the inconsistent and contradictory statistical links reported between density and infection/mortality rates early on the pandemic (discussed earlier). In fact, statistically significant negative correlations between broader measures of the built environment and COVID-19 mortality rates at a US county level were observed only after November 2020 when the data became relatively more stable (Frank and Wali, 2021). Third, most previous studies did not explicitly account for the important methodological concern of unobserved heterogeneity. It is unlikely that data on all other relevant factors likely correlated with COVID-19 outcomes (positive cases, hospitalizations, mortality) could be available for analysis. Such factors can include attitudinal predispositions, lifestyle factors, residential preferences, and environmental determinants2 (to name a few). In the absence of such potentially important omitted factors, it is impossible to estimate reliable relationships between observed factors (such as built environment) and COVID-19 outcomes. Additionally, the “latent” effects of such unobserved factors could be manifested through observed variables (such as built environment) leading to heterogeneity in the associations between key built environment features and COVID-19 outcomes. In fact, when unobserved heterogeneity was adequately accounted for, Frank and Wali, 2021 found a positive relationship (at the county level) between population density and COVID-19 infection rate – as opposed to a statistically significant negative relationship between the two when unobserved heterogeneity was ignored. Fourth, evidence on how active and sedentary travel correlate with COVID-19 severity (hospitalizations and mortality) does not exist. As discussed earlier, this is important since individuals with more healthier travel lifestyles (greater active travel and less time spent in cars) have lower risk of chronic disease (Frank and Wali, 2021; Chidambaram et al., 2020) and can be relatively more likely to survive illness due to COVID-19. Finally, and most importantly, most of the previous studies (including US level national studies) used aggregate data at an extremely coarse geographic scale (Chidambaram et al., 2020). This required averaging density or built environment measures across large geographies (such as cities and counties). This is problematic because built environment features and COVID-19 outcomes substantially vary within cities and counties.
Keeping in view the above gaps, the present study contributes by conducting a neighborhood-level analysis of the associations between built environment, COVID-19 hospitalization and mortality rate using fine-grained census-tract level data from King County, Washington. Findings can help to inform how policy makers respond to the threat of not only COVID-19 but future infectious disease threats. By including neighborhood-level data on COVID-19 hospitalizations (in addition to mortality data), we examine the role of hospitalization rates in mediating the relationships between built environment measures and COVID-19 mortality. In addition to the built environment, the present study sheds light on the effects of neighborhood-level active (sedentary) travel on COVID-19 hospitalizations and mortality. While the focus is on hospitalization rates as a key mediator, we also test and include COVID-19 positivity rate as an additional mediator linking built environment and active/sedentary travel with COVID-19 mortality outcomes. Methodologically, rigorous simulation-assisted random parameter discrete outcome models are developed for COVID-19 positivity, hospitalization and mortality rates to account for the methodological issues related to unobserved heterogeneity and omitted variable bias. Using the results from the heterogeneous discrete outcome models, path analysis is then performed to quantify the direct and indirect correlations between built environment, active travel, COVID-19 hospitalization and mortality rate. From this point onward, the terms fatality rate and mortality rate are interchangeably used.
2. Methods
2.1. Conceptual framework
The conceptual framework shown in Fig. 1 conveys different pathways between upstream predictors and downstream COVID-19 hospitalization and mortality. The inclusion of hospitalization rates provides a broader picture of the actual neighborhood-level harm imposed by COVID-19 since not all hospitalizations (indicating severe illness) lead to deaths. In fact, compared to the early days of the pandemic, patients hospitalized due to COVID-19 infection were reported to be surviving at higher rates. Thus, to paint a broader picture of the actual COVID-19 associated harm, hospitalization rates should also be considered in addition to eventual mortality outcomes. In addition, evidence suggests that pre-existing conditions (such as obesity) may triple the risk of severe illness and hospitalization due to COVID-19 infection (CDC, 2020). Chronic disease serves as a mechanism in the causal pathway mediating upstream environmental factors with downstream COVID-19 outcomes (Frank and Wali, 2021) which further points to the critical importance of demographics and social inequality. Reliable data on chronic disease are not typically available at a census-tract/neighborhood level. To this end, the inclusion of hospitalization rates can serve as a proxy for preexisting conditions as well. While the focus is on hospitalization rate as a key mediator, thanks to the suggestion by anonymous reviewers, we also include positivity rate as an additional mediator in the conceptual pathway linking built environment and active/sedentary travel with COVID-19 mortality outcomes.
Fig. 1.
Simulation-Assisted Heterogeneity Framework
(Notes: Subscript “i” indicates individual neighborhood-level parameter estimates; The dashed lines show the latent effects of unobserved factors which are manifested through observed exogenous variables; Figure shows a simplified version of the multiple pathways between upstream factors and COVID-19 outcomes. For brevity, all possible pathways between built environment, sedentary/active travel and COVID-19 outcomes are not shown).
A more compact and walkable environment is hypothesized to be correlated with lower COVID-19 hospitalization rates due to the health benefits of increased overall activity levels (Fig. 1). To this end, the key hypothesis is that compared to less compact and less walkable neighborhoods, individuals in more compact neighborhoods are more likely (on-average) to survive the illness. Since the hospitalization rate outcome directly influences the downstream COVID-19 fatality rate, the built environment related variables are also indirectly related with COVID-19 mortality rate through their associations with hospitalization rates. With regards to activity patterns, we examine the role of active and sedentary travel behavior by capturing the commuting travel modes in a neighborhood. Active commuting is defined as the use of walk and/or bike mode for commute travel, whereas sedentary commuting is defined as the use of automobile for travel purposes. Active travel modes (walk, bike) offer an opportunity to engage in physical activity and are known to be correlated with better health outcomes (Bassett et al., 2008; Frank et al., 2008; Raza et al., 2021; Sallis et al., 2020). Contrarily, sedentary (automobile) travel is positively correlated with obesity which predicts several other chronic health outcomes (Frank et al., 2004). Independent of each other, enhancing active travel and reducing sedentary travel behaviors have been effective measures to improve population health and are recommended by the World Health Organization for combating noncommunicable diseases. In the context of the present study, we hypothesize that active travel behaviors (walking, biking) are inversely correlated with mortality and hospitalizations from COVID-19, whereas sedentary travel is positively related to COVID-19 hospitalization and mortality outcomes. Given the framework shown in Fig. 1, the built environment and active/sedentary travel behavior factors can possess direct associations with COVID-19 mortality rate and/or indirect associations through hospitalization rates.
From a methodological standpoint, it is obvious that not all factors correlated with COVID-19 outcomes are observed in the data. These unobserved factors (such as attitudinal predispositions, residential preferences, etc.) exhibit direct “latent” effects on COVID-19 hospitalization and fatality rates (Fig. 1). Such (potentially important) latent effects cannot be explicitly quantified since the relevant factors are unobserved in the data (Wali et al., 2020; Mannering et al., 2020; Mannering et al., 2016). However, the latent effects of these unobserved factors could manifest through the observed exogenous factors (indicated by dashed lines in Fig. 1) – ultimately leading to heterogeneity in the coefficients associated with specific observed independent variables (Wali et al., 2020; Mannering et al., 2020). Fixed parameter models ignore this important methodological concern which can lead to erroneous findings when significant heterogeneity exists in the underlying data which is then masked through aggregation.
This results in the inability to accurately attribute a given coefficient to a large proportion of the sample. Likewise, due to inherent differences (Salon, 2015), it is unrealistic to posit that each individual respond in a same fashion to a potential change in built environment. In other words, different individuals interact differently even with a similar built environment fabric due to variations in their sociodemographic profiles, attitudinal predispositions and preferences. To this end, the methodological framework allows estimation of individual neighborhood-level parameter estimates by harnessing advances in simulation-assisted estimation.
2.2. Data
Census-tracts in King County, WA, serve as the unit of analysis in this study. The terms census-tracts and neighborhoods are interchangeably used throughout the paper. Containing around 35 cities (including Seattle), King County is the twelfth most populous county in United States with over 2.2 million inhabitants and a land area of 2307 sq mi. King County is comprised of 397 census tracts. In the US, census tracts are statistical subdivisions of a county that roughly have around 4000 inhabitants – serving as a geographical unit with highest spatial resolution for which demographic and built environment data are publicly available (beside census block groups).
To achieve the study objectives, multiple data streams are spatially joined at the census tract level. Census-tract level data on COVID-19 (including positive cases, hospitalizations and fatalities as of March 17th, 2021) for King County, Washington are obtained from the county's COVID-19 data dashboard (https://kingcounty.gov/depts/health/covid-19/data.aspx). Data on community design and built environment features are obtained from the Smart Location Database (SLD) by US Environmental Protection Agency. SLD provides comprehensive block group level-built environment data that was aggregated to a census-tract level (Ramsey and Bell, 2014). The built-environment measures included in SLD are mostly indicators of the “5D” variables (design, diversity, design, destination accessibility, and transit access) used in the transportation, planning, and health literature to examine environmental correlates of travel behavior and health outcomes3 (Ramsey and Bell, 2014). Data on census-tract level sociodemographic (race, gender, age, education, income, unemployment) and active/sedentary travel outcomes are obtained from the American Community Survey (ACS). In particular, “Detailed Tables” from the ACS are used providing population counts for each category of relevant variables. To increase statistical reliability of the data (especially for less populated areas), most recent 5-year estimates from the ACS are used. ACS includes journey to work questions to assess each neighborhood's commuting patterns. A primary factor is mode choice including car, truck, van, taxicab, bus, motorcycle, subway/elevated rail, bicycle, and walk. Proportions of those who walked, biked, and drove alone to work were calculated for each census tract in King County.
Regarding the built environment variables, the first one relates to street connectivity measuring pedestrian-oriented intersection density per unit area (D3B in SLD database). This measure is included since it is a leading design/connectivity measure used extensively in the travel behavior and planning literature (Cho et al., 2009; Ewing and Cervero, 2010). However, a modified intersection density measure is used in this study created from a weighted sum of component intersection density metrics. For instance, auto-oriented intersections typically are barriers to pedestrian and bicyclist mobility. Thus, it was given a zero weight. Likewise, four-way intersections were given more weight since it promotes street connectivity more effectively than three-way intersections. To capture regional auto-oriented accessibility, a regional auto centrality index ranging between 0 and 100 is used (D5CEI). This measure reflects the proportional accessibility to regional destinations by automobile and capture working age population accessibility (via automobile) relative to the maximum auto accessibility in a core-based statistical area (CBSA). A time-decay network travel time is used to place more weight on jobs and population closer to the origin block group. The auto accessibility measures are generated based on data from a commercial Application Programming Interface (API). For details on the decay function, geoprocessing model to tabulate automobile accessibility, and equations, see (Ramsey and Bell, 2014). Higher values for a census tract indicate greater auto oriented accessibility. The auto centrality index is included in the built environment variables because regional destination accessibility is one of the “D” variables measuring the built environment (Ewing and Cervero, 2010). We do note that the “3D” (Cervero and Kockelman, 1997a) and “5D” built environment classification (Ewing and Cervero, 2010) could have some overlapping dimensions (e.g., between destination accessibility and land-use/diversity). Finally, regarding diversity and land use configuration, a five-tier employment and residential entropy measure is used. Developed originally by Cervero (1989) (Cervero, 1989), this measure was first applied to predict active travel by Frank and Pivo in 1994 in a study also based in King County Washington and used parcel data to determine the evenness of floor space across residential, retail, employment, and commercial land uses at the census tract level. Land use mix in the current study is derived using the evenness of the distribution of residential areas and the following job classifications: retail, office, industrial, service, and entertainment jobs. The measure is based on trip production and attractions including residential and five employment categories. The productions and attractions are derived by multiplying average trip generation rates published by the Institute of Transportation Engineers by employment types and households. Higher values for this variable indicate a more even distribution of residential and commercial activities. For details and formulae, see (Ramsey and Bell, 2014). This proxies for the original land use based measure where more mixed land-use (live, work, play) environments were positively correlated with active travel and inversely correlated with driving (Frank and Pivo, 1994). As a limitation, we acknowledge that while the land-use measure includes different land-use proportions, occupation mix could not be included due to data unavailability. Also, while the land-use mix incorporates concentrations of households, type of households (single vs. multi-family) could not be incorporated due to data unavailability. Future research can also extend the present study by harnessing land use and points of interest (POI) data derived from social network APIs and digital map service providers (Gong et al., 2011). For the present study, such data are not publicly available at the neighborhood/census-tract level to our knowledge.
2.3. Random parameter discrete outcome models
The three dependent variables (COVID-19 positive cases, hospitalizations and fatalities) in this study are non-negative, discrete and count in nature. Thus, Poisson or Negative Binomial Generalized Linear Modeling framework can be used at a basic level to model the three dependent variables. For a Poisson regression, the likelihood/probability of having a specific number of positive cases , hospitalizations and number of fatalities in census-tract can be expressed as:
| (1) |
| (2) |
| (3) |
where: , and represent the probability of a positive case, hospitalization, and fatality in census tract ; , and are Poisson-distributed parameters for census tract equivalent to the predicted COVID-19 positive cases, hospitalization and fatality counts, respectively. Precisely, , and can be modeled as log link functions consisting of a set of independent variables as:
| (4) |
| (5) |
| (6) |
where: is a vector of census-tract specific independent variables (indexed by K); , and are vectors of estimable parameter estimates for corresponding variables in in the equation for positive cases (Eq. (4)), hospitalizations (Eq. (5)) and fatalities (Eq. (6)), respectively. The functions in Eq. (4) through Eq. (6) can be maximized with maximum likelihood estimation procedures. The above exposition can be algebraically manipulated to model rates (instead of counts) within the Poisson framework. A natural logarithm of census-tract population is included as an exposure term to model the outcomes as rates and to account for the varying level of exposure (population) across neighborhoods. The coefficients on the exposure terms are constrained to be 1 – which allows modeling the dependent variables as rates per capita (instead of counts). With this, the models in Equation (4), (5), (6) become models of per capita positivity, hospitalization, and fatality rates: , , and – where is the number of independent variables. As is evident, the coefficients on exposure must be fixed at 1 to be able to model rates per capita (instead of counts). For details, see (Osgood, 2017).
The fixed parameter Poisson models (Equation (1), (2), (3), (4), (5), (6)) unrealistically assumes that the coefficients associated with each of the explanatory factors are fixed/constant across all the census-tracts. Given the methodological concern of unobserved heterogeneity (explained in section 2.1), random parameters can be incorporated as (subscript “” for variables dropped for brevity):
| (7) |
| (8) |
| (9) |
where:, and are vectors containing the fixed coefficients corresponding to exogenous variable ; , and are random deviation terms distributed over the sample of census-tracts following a pre-specified distribution with zero mean and variance . With this, the exposition in Equation (4), (5), (6) is extended as:
| (10) |
| (11) |
| (12) |
Finally, the likelihood for the random parameter Poisson models for positive cases, hospitalizations and fatalities become:
| (13) |
| (14) |
| (15) |
Since the likelihood functions in Eq. (13), (14), (15) involve integration over densities for unobserved factors, maximum simulation likelihood procedures are used. To perform the simulation, Halton draws (as opposed to random Monte Carlo sequences) are used to achieve better coverage and covariance. 200 Halton draws are used for each of the random-held parameter shown in the literature to yield satisfactory simulation results (Train, 2009). Following relevant literature (Mannering et al., 2016; Train, 2009; Wali et al., 2020), several distributions such as normal, log-normal, triangular, Weibull, logistic, and Erlang distributions are tested regarding the functional specification of the unobserved factors in Equation (13), (14), (15).
2.3.1. Heterogenous direct and indirect effects
COVID-19 positive cases are used as a chaining variable in the hospitalization model, whereas hospitalizations are used as a chaining variable in the COVID-19 mortality models. For convenience, the hospitalization rate and mortality rate models are referred to as upstream and downstream models, respectively (Fig. 1). The direct associations between independent variables and each of the three outcomes are captured in (heterogeneous) census-tract level , β and estimates, respectively. In particular, the direct effects of hospitalization rate, built environment, active travel, and sociodemographic controls on COVID-19 fatality rate are captured in a heterogeneous matrix, namely [. Likewise, the (heterogeneous) direct effects of exogenous variables on positive cases and hospitalizations are stored in [ and [. Two sets of indirect effects are relevant. To calculate the indirect effects of exogenous variables on COVID-19 hospitalizations through positivity rate, the corresponding elements in [ can be multiplied with the estimate in the hospitalization model (assuming the direct effect of positive cases on hospitalizations is stored in . Likewise, the indirect effects of exogenous variables on COVID-19 fatalities through hospitalizations can be calculated by multiplying the corresponding elements in [ with (assuming the direct effect of hospitalization on fatality rate is stored in ).
2.3.2. Spatial correlation analysis
The methodological framework presented above can track unobserved heterogeneity in the determinants of COVID-19 outcomes due to systematic variations in unobserved factors. Since the COVID-19 outcomes in this study are correlated (discussed later), it is important to determine that there is no spatial autocorrelation in the regression residuals (Wali et al., 2018). The hypothesis is that after conditioning on exogeneous factors and unobserved heterogeneity, the resulting regression residuals do not exhibit spatial autocorrelation. Precisely, spatial autocorrelation can be considered as a second order variation that could not be accurately captured even after controlling for exogenous factors and unobserved heterogeneity (Wali et al., 2018). To examine spatial autocorrelation, we conduct Moran's I tests on the errors of the random parameter models for the three COVID-19 outcomes: positivity, hospitalization, and fatality rates (Quddus, 2013; Banerjee et al., 2003; Black and Thomas, 1998).
| (16) |
where: and represent the indices of surrounding census-tracts; and are the average magnitude of COVID-19 outcomes in census-tracts and ; is the global average of COVID-19 outcomes across all census-tracts; is the spatial proximity matrix that captures the spatial correlations across census-tracts and ; and is the total number of census-tracts in the sample. Compared to a binary spatial contiguity matrix (1 if two census-tracts are neighbors, 0 otherwise), we use a distance decay function for assigning weights to surrounding census-tracts that can more accurately reflect the spatial drift in COVID-19 outcomes across the census-tracts in King county. In particular, if , and 0 if otherwise, where is an inverse decreasing function of the distances between the centroids of census-tracts – implying that nearby census-tracts are more similar than the distant ones (Quddus, 2013; Banerjee et al., 2003; Black and Thomas, 1998). In terms of interpretation, a positive (negative) statistically significant spatial statistic will indicate that the COVID-19 outcomes are positively (negatively) correlated across the sampled census-tracts.
3. Results
3.1. Descriptive statistics
Descriptive statistics for key variables at the census-tract level are shown in Table 1 . Complete data on COVID-19 outcomes, built environment and active travel measures, and sociodemographic variables are available for the 397 census tracts in King County, WA. The average hospitalizations and fatalities across census-tracts in King County are 12.65 and 3.57, respectively. Referring to the standard deviation estimates, substantial heterogeneity exists in COVID-19 hospitalizations and fatalities within a county (Fig. 2 ). In terms of built environment, the census tracts in King County exhibit a wide range of pedestrian-oriented street intersection density (as a measure of connectivity), regional auto centrality index (accessibility), and 5-tier employment and household entropy (as a measure of diversity). With a mean of 100.76, the range of pedestrian-oriented intersection density ranges between 4.01 and 600.76 (Table 1). Likewise, the sampled census tracts vary significantly in terms of auto-oriented development (auto centrality index) and 5-tier employment and household entropy (diversity).
Table 1.
Descriptive statistics of key variables.
| Variables | Mean | SD | Min | Max | Data Source & Description |
|---|---|---|---|---|---|
| COVID-19 Outcomes | |||||
| Positive cases | 205.54 | 135.71 | 32 | 953 | King County COVID-19 data dashboard (https://kingcounty.gov/depts/health/covid-19/data.aspx) |
| Hospitalizations | 12.65 | 10.86 | 0 | 69 | |
| Mortalities/fatalities | 3.57 | 4.94 | 0 | 42 | |
| Exposure | |||||
| Population | 5607.81 | 1896.98 | 1547.29 | 14849.2 | |
| Exogenous Variables | |||||
| Built Environment | |||||
| Design: Street intersection density (weighted, auto-oriented intersections eliminated) (in 10s) | 10.76 | 7.46 | 0.04 | 60.79 | 2013 US Environmental Protection Agency's (EPA) Smart Location Database (SLD) (variable name: D3B) |
|
Destination Accessibility: Regional auto centrality index |
60.01 | 17.58 | 5.75 | 97.67 | 2013 US EPA's SLD (variable name: D4CEI) |
|
Diversity: Employment and household entropy |
48.79 | 11.93 | 12.08 | 77.58 | 2013 US EPA's SLD (variable name: D2C_TRPMX1) |
| Sedentary and Active Travel (workers' transportation mode to work) (% of workers) | |||||
| Drive alone | 63.14 | 14.71 | 11.09 | 89.06 | 2019 American Community Survey “Detailed Tables”: 5-year estimates (2015–2019) (https://www.census.gov/acs/www/data/data-tables-and-tools/american-factfinder/) |
| Biking | 1.51 | 2.14 | 0 | 14.89 | |
| Walking | 4.64 | 8.84 | 0 | 57.45 | |
| Carpool | 9.62 | 4.20 | 0 | 23.85 | |
| Teleworking | 6.97 | 3.55 | 0 | 25.16 | |
| Controls (% of population/total households) | |||||
| Race: Black | 6.42 | 7.70 | 0 | 40.47 | 2019 American Community Survey “Detailed Tables”: 5-year estimates (2015–2019) (https://www.census.gov/acs/www/data/data-tables-and-tools/american-factfinder/) |
| Race: White | 64.67 | 17.62 | 10.18 | 96.79 | |
| Race: Asian | 17.06 | 11.68 | 0.17 | 62.04 | |
| Gender: Female | 49.84 | 3.42 | 32.21 | 61.00 | |
| Graduate degree holders | 20.54 | 11.81 | 1.70 | 48.23 | |
| High income (USD >100,000 per annum) | 47.76 | 16.84 | 0 | 85.43 | |
| No-vehicle households | 8.89 | 10.91 | 0 | 68.51 | |
| Old age (65 years +) | 13.41 | 5.15 | 0 | 51.66 | |
| Old age (65 years +) with disability | 4.18 | 2.36 | 0 | 17.60 | |
| Unemployed | 2.94 | 1.50 | 0 | 9.31 | |
Notes: N = 397 census tracts; SD is standard deviation; For details on SLD database, see (Ramsey and Bell, 2014).
Fig. 2.
Spatial Distribution of COVID-19 Positivity, Hospitalization and Fatality Rates Across Census Tracts in King County, WA.
(Note: Please zoom in for better legibility. The mapping scheme is based on linear mapping from continuous numeric data to an interpolated plasma color palette.)
Regarding sedentary and active travel, on-average 63% of the workers across the census-tracts drove alone to their work, whereas around 1.5% and 4.6% of the workers biked and walked for their commute trips, respectively. Another 9.6% of the workers in the King County had carpooling as their main commute travel mode. Interestingly, around 7% of the individuals participated in teleworking. Descriptive statistics for other variables are shown in Table 1. Overall, substantial heterogeneity in COVID-19 outcomes, built environment and active travel, and sociodemographic factors exists across the census-tracts. A county or city-level analysis, on the other hand, discards such heterogeneous patterns.
3.2. Modeling results
The results of random parameter Poisson models for COVID-19 positivity, hospitalization, and fatality rates are discussed next. Fixed parameter Poisson counterparts are also briefly discussed to highlight the implications of ignoring issues related to unobserved heterogeneity and omitted variable bias. Initially, a series of fixed parameter Poisson models were developed – modeling positivity, hospitalization, and fatality rates as a function of built environment, active and sedentary commute travel, and sociodemographic factors.
In these models, the parameter estimates were assumed to be fixed/constant across the census-tracts. Owing to the issue of unobserved heterogeneity, random parameter Poisson models were developed next where the parameter estimates were allowed to vary across census tracts. Potential heterogeneity in parameter estimates was tested for all the explanatory variables. Variables were treated as random parameters in the following two cases: (1) if heterogeneous parameters exhibited statistically significant mean and standard deviation terms, or (2) if the parameters exhibited only statistically significant variance (standard deviation) terms. In the latter case, the variable was treated as a random parameter only if the Akaike Information Criterion (AIC) of the model was better (lower) than the AIC of corresponding model treating the particular explanatory factor as fixed. Regarding the distributions tested for densities of unobserved factors, normal distribution provided the best-fit. To derive the final specifications based on variables shown in Table 1, a systematic process was followed considering specification parsimony, bivariate (unadjusted) correlations, and statistical significance. Exogenous variables were retained if they were statistically significant at a 90% confidence level and led to an improvement in model goodness of fit in terms of log-likelihood at convergence and AIC. Variables that appeared statistically insignificant in the fixed parameter models but later emerged significant in the random parameter counterparts were also retained. The models presented next were found relatively best in terms of predictive fit, specification parsimony, and providing key inferential insights. Variance Inflation Factors (VIFs) were computed and examined to ensure that the final specifications do not exhibit problematic multicollinearity (Washington et al., 2010). As a conservative benchmark, a VIF of greater than 10 is considered large enough indicating potential problems (Chatterjee and Price, 1991). The VIFs of all the variables included in the final models were less than 3 – with a maximum VIF of 2.83, indicating the absence of problematic multicollinearity.
Table 2 shows the goodness-of-fit comparison for fixed and random parameter Poisson models for the three COVID-19 outcomes. For hospitalization rate outcome, three variables were found to be random parameters suggesting that the effects of these variables are heterogeneous across census tracts. Compared to the fixed parameter model, explicitly accounting for unobserved heterogeneity led to a marked improvement in log-likelihood and a substantial reduction of 440 points in AIC. As a general rule, a difference of more than ten points between AICs of two competing models implies significant support in favor of the model with lowest AIC (Burnham and Anderson, 2004). Note that AIC simultaneously considers both model complexity (degrees of freedom) and predictive ability in assessing a set of models. Likewise, compared to the mean absolute predictive error (MAPE) of 4.71 for fixed parameter model, the MAPE for random parameter model reduced to 1.46 – a 69% reduction in predictive errors. In addition to the predictive and inferential gains (discussed later), compared to nine variables in the random parameter model, only seven variables were statistically significant at 90% level of confidence in fixed parameter model.
Table 2.
Comparison of fixed and random parameter Poisson models for COVID-19 positive cases, hospitalizations and mortalities/fatalities.
| Summary Statistics | COVID-19 Positivity |
COVID-19 Hospitalizations |
COVID-19 Fatalities |
|||
|---|---|---|---|---|---|---|
| FP Poisson Model | RP Poisson Model | FP Poisson Model | RP Poisson Model | FP Poisson Model | RP Poisson Model | |
| N (# of census tracts) | 397 | 397 | 397 | 397 | 397 | 397 |
| No. of Halton draws |
– |
200 |
– |
200 |
– |
200 |
| No. of significant variables at 90% level (excluding constant)* | 6 | 6 | 7 | 9 | 2 | 7 |
| No. of parameters (excluding constant) | 6 | 7 | 9 | 12 | 7 | 9 |
| No. of random parameters |
0 |
1 |
0 |
3 |
0 |
2 |
| Log-likelihood (constant-only) | −13767.68 | −13767.68 | −2330.37 | −2330.37 | −1417.58 | −1417.58 |
| Log-likelihood at convergence |
−5453.54 |
−2379.1 |
−1425.6 |
−1202.61 |
−934.46 |
−811.12 |
| McFadden Pseudo R2 | 0.604 | 0.827 | 0.388 | 0.484 | 0.340 | 0.428 |
| AIC | 10921.1 | 4774.2 | 2871.2 | 2431.2 | 1884.9 | 1642.2 |
| ΔAIC [AICRANDOM-PARAMETER - AICFIXED-PARAMETER] |
−6146.9 |
−440 |
−242.7 |
|||
| Mean Absolute Prediction Error (MAPE) | 50.95 | 3.49 | 4.71 | 1.46 | 2.19 | 0.88 |
Notes: AIC is Akaike Information Criterion; (---) indicates Not Applicable; (*) This indicates the number of statistically significant exogenous variables at 90% level excluding constant terms and the scale parameters for randomly distributed parameter estimates; FP is fixed parameter; RP is random parameter.
Similar insights were obtained for COVID-19 fatality rate outcome (Table 2). Compared to the fixed parameter Poisson model, the AIC of the random parameter Poisson model reduced by 242.7 points. Likewise, random parameter Poisson model led to a substantial improvement in predictive fit (see Fig. 3 ). From an inferential standpoint, only two variables were statistically significant in the fixed parameter model (compared to seven (7) statistically significant variables in the random parameter counterpart). Finally, the random parameter Poisson model for positivity rate substantially outperformed the fixed parameter counterpart – with a reduction of 6146.9 points in the AIC and a reduction in MAPE from 50.95 to 3.49 for random parameter model (Table 2). Overall, these findings provide compelling evidence related to the importance of accounting for unobserved heterogeneity. Importantly, the results suggest that the associations between built environment and COVID-19 outcomes even vary significantly within a county (as opposed to inter-county heterogeneity reported elsewhere (Frank and Wali, 2021). This finding is intuitive given the personalized nature of behavioral interactions between users and the environment.4
Fig. 3.
Predictive comparison of fixed and random parameter discrete outcome models for COVID-19 positivity, hospitalization and fatality/mortality outcomes.
Table 3 shows the estimation results for COVID-19 positivity, hospitalization and fatality rate outcomes. The direct and indirect effects of exogenous variables are shown in Table 4 . Since the raw parameter estimates from non-linear models (such as Poisson) are not meaningful, the direct and indirect effects are based on relative risks. With a log-linear link, Poisson distributed error terms, and the addition of the natural logarithm of population as an offset, the exponent of the parameter estimates from the multiplicative Poisson models provides relative risk estimates or incidence rate ratio. Computed as (Eq. 6.9 in (Wooldridge, 2015)), the relative risks show the percent increase/decrease in positivity/hospitalization/fatality rates per capita with a unit increase in the exogenous variable. For random parameters, unconditional individual census-tract level parameter estimates are first estimated which are then used to estimate individual census-tract level relative risks.
Table 3.
Estimation results of fixed and random parameter models for COVID-19 positive cases, hospitalizations and fatalities.
| Variables | COVID-19 Positive Cases |
COVID-19 Hospitalizations |
COVID-19 Fatalities |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| FP Poisson Model |
RP Poisson Model |
FP Poisson Model |
RP Poisson Model |
FP Poisson Model |
RP Poisson Model |
|||||||
| β | z-score | β | z-score | β | z-score | β | z-score | β | z-score | β | z-score | |
| Intercept | −2.022 | −75.95 | −2.443 | −92.7 | −6.546 | −45.07 | −6.485 | −43.83 | −9.733 | −18.24 | −10.57 | −19.79 |
| Exposure (log of population) | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||
| Chaining Variable | ||||||||||||
| Positive cases | – | – | – | – | 0.001 | 14.62 | 0.002 | 16.27 | – | – | – | – |
| Hospitalizations | – | – | – | – | – | – | – | – | 0.05 | 27.50 | 0.057 | 28.96 |
| Built Environment | ||||||||||||
| Street intersection density (weighted, auto-oriented intersections eliminated) (in 10s)* | −0.024 | −44.37 | −0.014 | −30.54 | 0.003 | 0.94 | −0.011 | −2.97 | – | – | – | – |
| standard deviation of random parameter | – | – | 0.064 | 112.23 | – | – | – | – | – | – | – | – |
| Regional auto centrality index | – | – | – | – | 0.003 | 2.56 | 0.009 | 7.62 | 0.0006 | 0.26 | 0.008 | 3.51 |
| Employment and household entropy* | – | – | – | – | 0.001 | 0.88 | −0.002 | −1.73 | 0.002 | 0.79 | −0.003 | −1.57 |
| standard deviation of random parameter | – | – | – | – | – | – | 0.008 | 33.1 | – | – | 0.007 | 14.23 |
| Sedentary and Active Travel (workers' transportation mode to work) (% of workers) | ||||||||||||
| Drive alone | – | – | – | – | – | – | – | – | 0.002 | 1.06 | 0.006 | 2.02 |
| Walking* | – | – | – | – | −0.009 | −4.060 | −0.015 | −6.510 | – | – | – | – |
| standard deviation of random parameter | – | – | – | – | – | – | 0.023 | 11.38 | – | – | – | – |
| Biking* | – | – | – | – | −0.110 | −9.22 | −0.112 | −9.33 | – | – | – | – |
| standard deviation of random parameter | – | – | – | – | – | – | 0.048 | 5.71 | – | – | – | – |
| Telecommuting | −0.019 | −13.71 | −0.034 | −42.11 | – | – | – | – | – | – | – | – |
| Controls | ||||||||||||
| Race: Black | 0.007 | 13.09 | 0.011 | 19.21 | 0.008 | 4.21 | 0.004 | 2.28 | – | – | – | – |
| Race: White | −0.003 | −12.45 | −0.002 | −7.56 | – | – | – | – | – | – | – | – |
| Gender: Female | – | – | – | – | – | – | – | – | 0.0133 | 1.6 | 0.014 | 1.75 |
| High income (USD >100,000 per annum)* | −0.017 | −60.63 | −0.014 | −68.2 | −0.014 | −11.78 | −0.017 | −14.38 | −0.003 | −1.64 | −0.003 | −1.75 |
| standard deviation of random parameter | – | – | – | – | – | – | – | – | – | – | 0.011 | 17.89 |
| Old age (65 years +)* | – | – | – | – | 0.033 | 12.06 | 0.028 | 9.86 | 0.049 | 10.72 | 0.054 | 11.02 |
| standard deviation of random parameter | – | – | – | – | – | – | – | – | – | – | – | – |
| Unemployed | 0.015 | 6.47 | 0.065 | 29.89 | – | – | – | – | – | – | – | – |
Notes: (*) indicates random parameters; (---) indicates when a given variable is dropped from a model due to statistical insignificance, lack of improvement in goodness-of-fit, and/or to retain the most important variables in line with study objectives.
Table 4.
Direct and Indirect Associations (in percentage) of Exogenous Variables with COVID-19 Positive Cases, Hospitalizations and Fatalities.
| Variables | Direct Effect on COVID-19 Positive Cases |
Direct Effect on Hospitalizations |
Direct Effects on COVID-19 Fatalities |
Indirect Effects on COVID-19 Hospitalizations Through Positive Cases |
Indirect Effects on COVID-19 Fatalities Through Hospitalizations |
|---|---|---|---|---|---|
| μ | μ | μ | μ | μ | |
| Chaining Variable | |||||
| Positive cases | – | 0.195 | – | – | 1.157 |
| Hospitalizations | – | – | 5.928 | – | – |
| Built Environment | |||||
| Street intersection density (weighted, auto-oriented intersections eliminated) (in 10s) | −1.586* | −1.039 | – | −0.309* | −6.162 |
| Regional auto centrality index | – | 0.986 | 0.831 | – | 5.851 |
| Employment and household entropy | – | −0.241* | −0.381* | – | −1.428* |
| Sedentary and Active Travel (workers' transportation mode to work) (% of workers) | |||||
| Drive alone | – | – | 0.606 | – | – |
| Walking | – | −1.562* | – | – | −9.259* |
| Biking | – | −10.611* | – | – | −62.902* |
| Telecommuting | −3.369 | – | – | −0.657 | – |
| Controls | – | – | – | ||
| Race: Black | 1.166 | 0.431 | – | 0.227 | 2.554 |
| Race: White | −0.205 | – | – | −0.041 | – |
| Gender: Female | – | – | 1.461 | – | – |
| High income (USD >100,000 per annum) | −1.461 | −1.726 | −0.361* | −0.285 | −10.237 |
| Old age (65 years +) | 1.741 | 2.897 | 5.603 | 0.339 | 17.174 |
| Unemployed | 6.721 | – | – | 1.311 | – |
Notes: (---) indicates Not Applicable; (*) indicates heterogeneous direct and indirect effects; μ indicates direct and indirect effects (including “average” effects for random-held parameters).
4. Discussion and synthesis
This discussion of key findings is based on the results of the best-fit random parameter models. The key findings with regards to the direct and indirect effects (see Fig. 1) are presented. Higher levels of street connectivity and more mixed-use correlate with less sedentary and more active travel. The opposite is true for the regional auto centrality index. Results suggest that neighborhoods with more pedestrian-oriented street connectivity, more mixed use (in terms of residential and employment mix), and lower auto accessibility will on-average have lower COVID-19 hospitalizations and fatalities. We postulate this relationship with COVID-19 is largely the result of increase in physical activity and lower levels of obesity and chronic disease associated with these built environment characteristics.
4.1. Correlations of built environment and travel behavior with COVID-19 hospitalizations
After controlling for sociodemographic and other unobserved factors, pedestrian-oriented street density (indicating higher connectivity) and 5-tier employment and household entropy (proxy for land-use mix) are negatively correlated with COVID-19 hospitalizations. A ten-unit increase in pedestrian-oriented street intersection density correlates with a 1.039% reduction in COVID-19 hospitalizations per capita. Likewise, a one percent increase in employment and household mix is associated with a 0.241% reduction in COVID-19 hospitalizations per capita. As expected, a percent increase in auto centrality index associates with a 0.986% increase in hospitalizations (Table 3, Table 4). However, the associations between employment and household mix and hospitalizations exhibit substantial heterogeneity in varying degrees. For example, with a mean structural parameter estimate of −0.002 and standard deviation of 0.008 (Table 3), the associations between land-use mix and hospitalizations are negative for around 60% of the population and positive for the rest. The positive association for 40% of the population does not imply causation. Instead, it suggests that there are other unobserved census-tract specific factors which when combined with employment and household mix correlate with higher hospitalizations. Noteworthy is the fact that none of the street connectivity and employment/household mix variables were statistically significant in the fixed parameter model (see Table 3). The application of more advanced random parameter methods found that designing more walkable neighborhoods could be an effective strategy to combat COVID-19 severity while sedentary auto-oriented development may be further discouraged.
Regarding active travel, a one percent increase in the proportion of workers using bike for work commute is associated with a 10.611% reduction in COVID-19 hospitalizations. Likewise, a percent increase in workers walking for commute is correlated with a 1.562% reduction in COVID-19 related hospitalizations. The significant reductions in hospitalizations highlight the importance of active travel since individuals with greater participation in active travel activities are more likely to have lower prevalence of chronic disease (Dietz and Santos-Burgoa, 2020) – an independent and key predictor of COVID-19 severity (Busetto et al., 2020; Cai et al., 2020; Frank and Wali, 2021). Also, more active individuals may likely have stronger immune systems. In addition to the health benefits discussed above, active travel may also improve mental health during the pandemic (Hino and Asami, 2021; Yang and Xiang, 2021). Both variables were also found to be random parameters suggesting that the associations of these variables with COVID-19 hospitalizations vary across neighborhoods. Regarding sociodemographic factors, neighborhoods with greater proportion of Black and old individuals (65 years +) have higher hospitalization rates, whereas the reverse is true for neighborhoods with more high-income individuals (Table 3, Table 4). These findings are in line with previous studies documenting disparate and more severe impacts of COVID-19 on vulnerable populations (Pierce et al., 2021; Gibertoni et al., 2021). Likewise, capturing exposure, neighborhoods with greater COVID-19 positive cases have on-average greater hospitalization rates per cases.
4.2. Correlations of built environment and travel behavior with COVID-19 fatalities
Referring to the results of random parameter Poisson model for COVID-19 fatalities, greater auto accessibility is positively correlated with neighborhood fatality rates. A one percent increase in auto centrality index correlates with a 0.831% increase in COVID-19 fatality rates. Contrarily, more mixed land use (employment and household entropy) is associated with lower COVID-19 fatalities. However, the associations between employment/household entropy and COVID-19 fatalities are heterogeneous across the neighborhoods (see the structural mean and standard deviation parameters in Table 3). Again, both variables were statistically insignificant in the fixed parameter model. These findings suggest that if unobserved heterogeneity is ignored, one may incorrectly conclude that greater walkability is not associated with mortality. Regarding commute travel, neighborhoods with greater proportion of workers driving alone had on-average a higher COVID-19 mortality rate. A one percent increase in workers driving alone to work is associated with a 0.606% increase in COVID-19 fatalities. As expected, a one unit increase in COVID-19 hospitalization correlates with a 5.928% increase in COVID-19 mortality. The relationships between sociodemographic factors and COVID-19 mortality are shown in Table 3, Table 4 and are intuitive. Overall, female and elder populations are more vulnerable to develop serious illness (hospitalizations) and die from COVID-19. Due to space constraints, the results of COVID-19 positivity rate model are not discussed in detail but largely follow intuition. For example, in line with Yang et al. (2021), greater percentage of telecommuting workers in a neighborhood is correlated with lower positivity rate (Yang et al., 2021). Neighborhoods with greater percentage of Black, old age, unemployed individuals have higher positivity rates whereas the reverse is true for neighborhoods with greater percentage of white individuals. Noteworthy is the heterogeneity in the associations of pedestrian-oriented street connectivity with COVID-19 positivity rate. Distributed as a normally distributed random parameter with a mean of −0.014 and a relatively greater standard deviation of 0.064, the associations are negative for around 58% of the population and positive for the rest. We note that the negative associations observed between pedestrian-oriented street connectivity and infection rate for 58% of the population may not be attributed to greater street connectivity itself. Instead, it could reflect other place-based characteristics that neighborhoods with better street connectivity could exhibit, and which may lower infection rates. For example, areas that are more connected and exhibit more walkable infrastructure could be more capable of timely implementing social distancing and stay-at-home orders due to their better socioeconomic status – thus reducing the spread of the virus. As discussed earlier (footnote 1), street connectivity is strongly correlated with population density in the U.S. context – and would be logically expected to correlate with higher infection risk. The random parameter framework better captures the underlying complex mechanisms. A fixed parameter model, on the other hand, missed the heterogeneous patterns, implying that the associations are negative throughout the population. While not the focus of the present study, similar heterogeneous associations were found for other built environment features including employment and household entropy and auto centrality index as it related to COVID-19 positivity rate (results not shown). To have a more parsimonious model structure, these variables were not included in the final model for positivity rate. For insights regarding the role of built environment in COVID-19 spread, please see (Ma et al., 2021; Lak et al., 2021; Li et al., 2021b; Li et al., 2021a). Regarding travel behavior, active and sedentary travel outcomes (except telecommuting) were not included in the COVID-19 positivity rate model. This is because it is unclear how sedentary and active travel behaviors may correlate with COVID-19 infection rate. Contrarily, the pathways between sedentary/active travel and COVID-19 hospitalizations and fatalities are conceptually clearer (and which are captured in this study). To this end, future research can further build upon the present results by conceptualizing and testing the relationships between active/sedentary travel and COVID-19 positivity rate.
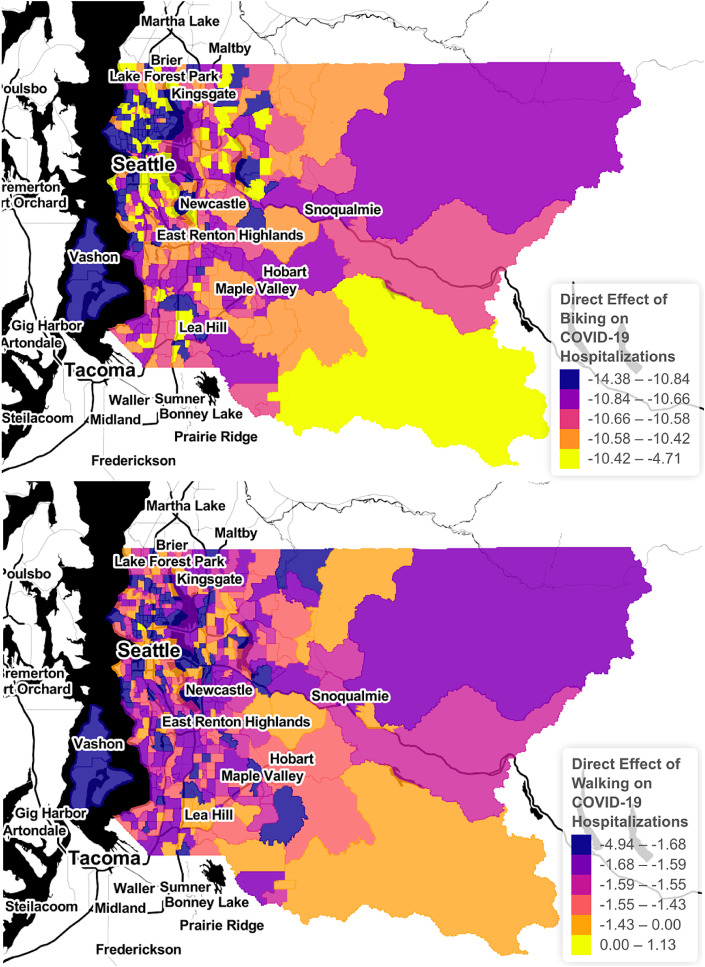
4.3. Direct and indirect effects – built environment, travel behavior, COVID-19 hospitalizations and fatalities
Table 4 provides the direct and indirect effects of exogenous variables on COVID-19 positive cases, hospitalizations, and fatalities. Related to the direct effect, a one percent increase in employment and household mix (more mixed land use) is correlated with a 0.241% and 0.381% reduction in hospitalizations and fatalities, respectively. In addition, more mixed land use indirectly correlates with COVID-19 fatalities through its relationship with hospitalizations rates. In particular, a one percent increase in employment and household mix is associated with a 1.428% reduction in COVID-19 fatalities per capita (Table 4). The relationships of employment and household mix with COVID-19 mortality is based on a random parameter model resulting in neighborhood-level parameter estimates. Fig. 4 shows the heterogeneity in the direct and indirect effects of household and employment mix where quantile based distributional splits of the relevant direct and indirect effects are used. Such local inferential insights cannot be obtained from traditional fixed parameter Poisson models. Regarding auto-oriented development, a one percent increase in auto centrality index is associated with a 0.986% increase in COVID-19 hospitalizations which in turn is correlated with around 5.928% increase in COVID-19 deaths per capita. Thus, the indirect effect of auto centrality index on COVID-19 fatalities is 5.851% (0.986 × 5.928). The heterogeneous direct effects of active travel on hospitalizations per capita are shown in Fig. 5 . Both walking and biking for commute also exhibited profound indirect effects on fatalities through hospitalizations (Table 4). For instance, a one percent increase in walking for commute was indirectly associated with a 9.259% reduction in COVID-19 fatalities per capita through its associations with hospitalizations (Table 4). Regarding vulnerable populations, both Black and old age variables exhibit substantial indirect correlations with COVID-19 fatalities (see estimates in last column of Table 4 for these variables). The most important point of our fatality model through hospitalization is the finding that the indirect effects of exogenous variable on COVID-19 fatality/mortality are significantly more profound compared to the direct effects of exogenous factors on COVID-19 fatality. This highlights the significant role of hospitalizations in mediating the relationships between built environment, active/sedentary travel, and COVID-19 mortality. Ignoring hospitalizations as a mediator masks these significant indirect effects of built environment and active/sedentary travel factors.
Fig. 4.
Heterogeneous Direct and Indirect Effects (in percentage) of Mixed-Use Developments (Household and Employment Mix) (Note: The mapping scheme is based on binning with cut-off points derived from the quantiles of the respective distribution of direct and indirect effects).
Fig. 5.
Heterogeneous Direct Effects (in percentage) of Biking and Walking for Commute
(Note: The mapping scheme is based on binning with cut-off points derived from the quantiles of the respective distribution of direct and indirect effects).
5. Limitations & strengths
Despite the higher-resolution spatial data and rigorous methodological framework, the study is correlational in nature and causal insights cannot be made. This study is based on neighborhood-level data from King County, WA. Thus, caution must be exercised in generalizing the findings. However, the neighborhood-level built environment features harnessed in this study appear to be similar to what is found nationally. In terms of housing and household size, the owner-occupied housing rate and household occupancy (persons per household) is 56.9% in King County versus 64% nationally and 2.45 in King County versus 2.62 nationally. The proportion of high school graduates (93.1%) in King County is a bit greater than the national average (88%). Regarding accessibility, the mean travel time to work is 29.6 min (compared to 26.9 min nationwide). Poverty in King County (7.7%) is lower than the national average (10.5%). These statistics may allow readers to infer broader similarity patterns between King County and counties in other states. The findings from this study highlight several promising avenues for future research. As discussed, chronic disease was not considered due to the unavailability of reliable neighborhood-level data. Due to data unavailability, the active/sedentary travel measures considered in this study only relate to work-commute and does not capture other forms of travel activity for leisure/non-utilitarian purposes. Thus, our findings capturing the impacts of active/sedentary travel are likely conservative. Likewise, the conceptual framework presented in this study could be further expanded by capturing the pathway between built environment and active/sedentary travel. In other words, active/sedentary travel can be considered as an up-stream mediator between built environment and COVID-19 outcomes. The study did not focus on examining the changes in COVID-19 outcomes over time. In line with the study objective, pre-pandemic travel patterns and built environment features are used to explain variations in COVID-19 outcomes. However, resident behaviors and travel patterns are significantly different before and during the pandemic. Likewise, population dynamics in and out of neighborhoods may have changed during the pandemic. To this end, the study presents a static cross-sectional snapshot of the associations and insights about changes over time cannot be made. Future studies can further extend the framework presented in this study by analyzing COVID-19 outcomes in a joint econometric framework to account for spatial heterogeneity and (spatial) correlations among the unobserved factors determining COVID-19 positivity, hospitalization, and mortality rate (Wali et al., 2021; Barua et al., 2016; Buddhavarapu et al., 2016). Along this line, to capitalize on the potential efficiency gains from the joint econometric framework (especially in the presence of dynamic stochastic dependencies), more advanced copula-based methods could be explored (Bhat and Eluru, 2009; Wali et al., 2018; Yasmin et al., 2014). The availability of more data at the neighborhood level in the future can enable development of joint heterogeneity-based models with sufficiently larger sample sizes so to efficiently estimate the significantly expanded set of estimable parameters in more advanced joint models.
This study makes several novel contributions. To our knowledge, it is the first study that jointly considers built environment, active travel, COVID-19 hospitalizations, and mortalities at the neighborhood level. As discussed, county-level analyses require aggregation of COVID-19 outcomes and built environment measures across large geographies – which is problematic given the substantial within-county variations. Second, the results demonstrate that hospitalization rate is an important mediator and should be considered together with fatalities to paint a broader picture of the actual harm imposed by COVID-19. Previous studies have not examined/reported the significant neighborhood-level correlations between active/sedentary travel and COVID-19 hospitalizations/mortalities reported in this study. Third, methodologically, the application of simulation-assisted discrete outcome random parameter approach is novel to modeling COVID-19 mortality and hospitalizations. The results highlight the importance of accounting for unobserved heterogeneity in arriving at more accurate conclusions at a neighborhood-level. Thus, great caution must be exercised in arriving at conclusions derived from fixed parameter modeling methods especially where highly aggregate data is applied. The study provides a conceptual pathway from the built environment to examine systematic disparities across sociodemographic cohorts in the spatiotemporal distribution of COVID-19 hospitalization and mortality rates.
6. Conclusions
This study contributes by presenting a neighborhood-level conceptual model linking built environment and active/sedentary travel measures with COVID-19 positivity, hospitalization and mortality rates. Integrated census-tract level data on COVID-19 mortality, hospitalization, and positive cases, built environment, travel behavior, and sociodemographic factors were harnessed. Informed by rigorous simulation-assisted discrete outcome random parameter models, the results shed new lights on the direct and indirect connections between built environment, active/sedentary travel behavior, hospitalization, and mortality rates. The key conclusions are:
-
1.
Auto-oriented built environment design (greater auto accessibility) is positively correlated with COVID-19 fatality rate. Conversely, more mixed land use and greater pedestrian-oriented street connectivity is associated with lower fatality and/or hospitalization rates.
-
2.
Sedentary (auto) travel is associated with greater COVID-19 fatality rate. Conversely, active travel (biking and walking) is correlated with lower COVID-19 hospitalization/fatality rates.
-
3.
COVID-19 hospitalizations strongly mediate the relationships between built environment, active travel, and COVID-19 fatality rate. Given the strong mediation role of hospitalizations, the indirect effects of built environment and active travel on COVID-19 fatalities are relatively more profound.
-
4.
Black and elder populations are more vulnerable to develop serious illness (hospitalizations) and die from COVID-19.
Methodologically, the associations explored in this study exhibited remarkable heterogeneity across neighborhoods. Accounting for unobserved heterogeneity not only led to remarkable improvement in predictive fit but provided more accurate insights as well. Importantly, ignoring unobserved heterogeneity leads to incorrect conclusions – such as concluding that built environment is not related to COVID-19 hospitalization/fatality rates. The findings have important implications. Healthier (active) transportation infrastructure can be effective in combating the severity of COVID-19 and perhaps other highly contagious infectious diseases. Population-level health and well-being of residents can be improved by continuing to advocate for active-travel supportive transport infrastructure with more mixed land-use and greater pedestrian-oriented street connectivity. Independent of mixed land use, the negative associations between street connectivity and COVID-19 hospitalizations assert the independent role of pedestrian-oriented street design in promoting walkability and combating COVID-19. Likewise, the results suggest that developments with greater auto-oriented accessibility may be further discouraged. Neighborhoods with more mixed land-use, greater street connectivity, and lower auto-oriented accessibility promote active (walk, bike) and discourage sedentary travel. Related to population health, the importance of walkable built environment in combatting COVID-19 is further highlighted by our findings related to active and sedentary travel behaviors – suggesting that greater participation in active travel and lower participation in automobile travel significantly reduces COVID-19 hospitalization and/or mortality rates. In assessing the relationships between built environment and COVID-19 outcomes, broader built environment measures should be considered to paint a more accurate and informed picture of the underlying mechanisms and pathways connecting transportation infrastructure and built environment with infectious diseases.
Acknowledgement
We would like to acknowledge the support of Department of Urban Studies and Planning at UC San Diego and US Environmental Protection Agency’s Office of Research and Development and Smart Growth Office. We would also like to thank two anonymous reviewers for providing useful feedback on earlier versions of the paper.
Footnotes
With regards to the built environment measures, the use of population density as a key surrogate measure of the built environment in understanding COVID-19 outcomes is problematic. While healthier and more walkable neighborhoods are denser, dense environments are not necessarily walkable (especially in developing countries). Consider the city of Karachi which is among the most populous cities in the world, with a population density of around 25,229 individuals/km2 – over three times that of Vancouver (5400 individuals/km2). However, the two cities are on completely opposite ends of the livability spectrum – with Karachi rated as one of the least livable cities globally with poor levels of pedestrian-oriented infrastructure and connectivity, residential allotment, public services, and transportation. As discussed elsewhere (Frank and Wali, 2021), greater density brings people closer and is a completely opposed spatial concept to distancing. It is not logically possible that greater population density would be unrelated or negatively correlated with COVID-19 infection rate. In addition, given the strong positive correlations between density and measures of walkable environments (especially in developed countries), it is not possible to disentangle the effect of density from the effects of walkable built environment features. When density is used as a key built environment predictor, the effects of other measures of walkable environments are manifested through density. In addition to the methodological issue of unobserved heterogeneity (discussed next), this mechanism could be a key factor behind previous findings concluding that population density is unrelated or negatively related with COVID-19 spread.
As one example, thanks to advancements in objective-built environment assessment methods, measures of walkability/built environment provide influential data about key elements of the physical environment known to support active travel. However, these data still do not approach the level of detail needed to fully capture the entire fabric of built environment. It is impractical to expect that information on all the relevant environmental factors can be collected and/or observed in the data typically available for analysis.
A newer version of SLD has been released by U.S. EPA recently – enhancing the methodology to quantify built environment features along with inclusion of more built environment features. For details, see (Chapman et al., 2021).
Following the discussion in section 2.3.2, we examined potential spatial autocorrelations in the residuals of the best-fit random parameter models for COVID-19 positivity, hospitalization, and fatality rates. For the three COVID-19 outcomes including positivity, hospitalization, and fatality rates, the calculated Moran's I statistics are 0.009 (p-value: 0.0007), −0.001 (p-value: 0.70), and −0.004 (p-value: 0.62) respectively. Given the statistical insignificance of the spatial statistic values for COVID-19 hospitalization and fatality rates, a lack of significant spatial autocorrelation in the regression residuals is concluded at a 99% confidence level. While the Moran's I statistic for COVID-19 positivity rate is statistically significant, we consider it unproblematic given its very small magnitude (0.0007).
References
- Banerjee S., Carlin B.P., Gelfand A.E. Chapman and Hall/CRC; 2003. Hierarchical Modeling and Analysis for Spatial Data. [Google Scholar]
- Barua S., El-Basyouny K., Islam M.T. Multivariate random parameters collision count data models with spatial heterogeneity. Analytic methods in accident research. 2016;9:1–15. [Google Scholar]
- Bassett D.R., Pucher J., Buehler R., et al. Walking, cycling, and obesity rates in Europe, North America, and Australia. J. Phys. Activ. Health. 2008;5:795–814. doi: 10.1123/jpah.5.6.795. [DOI] [PubMed] [Google Scholar]
- Berrigan D., McKinno R.A. Built environment and health. Prev. Med. 2008;47:239. doi: 10.1016/j.ypmed.2008.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhat C.R., Eluru N. A copula-based approach to accommodate residential self-selection effects in travel behavior modeling. Transp. Res. Part B Methodol. 2009;43:749–765. [Google Scholar]
- Black W.R., Thomas I. Accidents on Belgium's motorways: a network autocorrelation analysis. J. Transport Geogr. 1998;6:23–31. [Google Scholar]
- Bray I., Gibson A., White J. Coronavirus disease 2019 mortality: a multivariate ecological analysis in relation to ethnicity, population density, obesity, deprivation and pollution. Publ. Health. 2020;185:261–263. doi: 10.1016/j.puhe.2020.06.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brownson R.C., Hoehner C.M., Day K., et al. Measuring the built environment for physical activity: state of the science. Am. J. Prev. Med. 2009;36:S99–S123. doi: 10.1016/j.amepre.2009.01.005. e112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buddhavarapu P., Scott J.G., Prozzi J.A. Modeling unobserved heterogeneity using finite mixture random parameters for spatially correlated discrete count data. Transp. Res. Part B Methodol. 2016;91:492–510. [Google Scholar]
- Burnham K.P., Anderson D.R. Multimodel inference: understanding AIC and BIC in model selection. Socio. Methods Res. 2004;33:261–304. [Google Scholar]
- Busetto L., Bettini S., Fabris R., et al. Obesity and COVID‐19: an Italian snapshot. Obesity. 2020;28:1600–1605. doi: 10.1002/oby.22918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Q., Chen F., Wang T., et al. Obesity and COVID-19 severity in a designated hospital in Shenzhen, China. Diabetes Care. 2020;43:1392–1398. doi: 10.2337/dc20-0576. [DOI] [PubMed] [Google Scholar]
- Carlson J.A., Saelens B.E., Kerr J., et al. Association between neighborhood walkability and GPS-measured walking, bicycling and vehicle time in adolescents. Health Place. 2015;32:1–7. doi: 10.1016/j.healthplace.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carozzi F. Urban density and COVID-19. 2020. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3643204 URL: [DOI] [PMC free article] [PubMed]
- CDC Obesity, race/ethnicity, and COVID-19. Centers for disease control and prevention. 2020. https://www.cdc.gov/obesity/data/obesity-and-covid-19.html#:~:text=Obesity%20Worsens%20Outcomes%20from%20COVID%2D19&text=People%20who%20are%20overweight%20may,linked%20to%20impaired%20immune%20function.&text=Obesity%20decreases%20lung%20capacity%20and%20reserve%20and%20can%20make%20ventilation%20more%20difficult URL:
- Cerin E., Van Dyck D., Zhang C.J., et al. Urban environments and objectively-assessed physical activity and sedentary time in older Belgian and Chinese community dwellers: potential pathways of influence and the moderating role of physical function. Int. J. Behav. Nutr. Phys. Activ. 2020;17:1–15. doi: 10.1186/s12966-020-00979-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cervero R. Land-use mixing and suburban mobility. 1989. https://escholarship.org/uc/item/4nf7k1v9 URL:
- Cervero R., Kockelman K. Travel demand and the 3Ds: density, diversity, and design. Transport. Res. Transport Environ. 1997;2:199–219. [Google Scholar]
- Cervero R., Kockelman K. Travel demand and the 3Ds: density, diversity, and design. Transport. Res. Transport Environ. 1997;2:199–219. [Google Scholar]
- Chapman J., Fox E., Bachman W., et al. 2021. Smart Location Database. Technical Documentation and User Guide.https://www.epa.gov/sites/production/files/2021-06/documents/epa_sld_3.0_technicaldocumentationuserguide_may2021.pdf URL: [Google Scholar]
- Chatterjee S., Price B. 1991. Regression Diagnostics. New York. [Google Scholar]
- Chidambaram V., Tun N.L., Haque W.Z., et al. Factors associated with disease severity and mortality among patients with COVID-19: a systematic review and meta-analysis. PloS One. 2020;15 doi: 10.1371/journal.pone.0241541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cho G., Rodríguez D.A., Khattak A.J. The role of the built environment in explaining relationships between perceived and actual pedestrian and bicyclist safety. Accid. Anal. Prev. 2009;41:692–702. doi: 10.1016/j.aap.2009.03.008. [DOI] [PubMed] [Google Scholar]
- Creatore M.I., Glazier R.H., Moineddin R., et al. Association of neighborhood walkability with change in overweight, obesity, and diabetes. Jama. 2016;315:2211–2220. doi: 10.1001/jama.2016.5898. [DOI] [PubMed] [Google Scholar]
- Dietz W., Santos‐Burgoa C. Obesity and its implications for COVID‐19 mortality. Obesity. 2020;28 doi: 10.1002/oby.22818. 1005-1005. [DOI] [PubMed] [Google Scholar]
- Ewing R., Cervero R. Travel and the built environment: a meta-analysis. J. Am. Plann. Assoc. 2010;76:265–294. [Google Scholar]
- Ewing R., Schmid T., Killingsworth R., et al. Relationship between urban sprawl and physical activity, obesity, and morbidity. Am. J. Health Promot. 2003;18:47–57. doi: 10.4278/0890-1171-18.1.47. [DOI] [PubMed] [Google Scholar]
- Frank LD., Andresen MA., Schmid TL. Obesity relationships with community design, physical activity, and time spent in cars. American journal of preventive medicine. 2004;27:87–96. doi: 10.1016/j.amepre.2004.04.011. [DOI] [PubMed] [Google Scholar]
- Frank LD., Iroz-Elardo N., Macleod KE., Hong A. Pathways from built environment to health: a conceptual framework linking behavior and exposure-based impacts. Journal of Transport & Health. 2019;12:319–335. [Google Scholar]
- Frank LD., Kerr J., Sallis J., Miles R., Chapman J. A hierarchy of sociodemographic and environmental correlates of walking and obesity. Preventive medicine. 2008;47:172–178. doi: 10.1016/j.ypmed.2008.04.004. [DOI] [PubMed] [Google Scholar]
- Frank, Lawrence D., Sallis, James F., Conway, Terry L., Chapman James., Saelens, Brian E., Bachman William. Many pathways from land use to health: associations between neighborhood walkability and active transportation, body mass index, and air quality. Journal of the American planning Association. 2006;72:75–87. [Google Scholar]
- Frank LD., Pivo G. Impacts of mixed use and density on utilization of three modes of travel: single-occupant vehicle, transit, and walking. Transportation research record. 1994;1466:44–52. [Google Scholar]
- Frank LD., Wali B. Treating two pandemics for the price of one: Chronic and infectious disease impacts of the built and natural environment. Sustain. Cities Soc. 2021:103089. doi: 10.1016/j.scs.2021.103089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frumkin H. COVID-19, the built environment, and health. Environ. Health Perspect. 2021;129 doi: 10.1289/EHP8888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frumkin H., Frank L., Frank L.D., et al. Island Press; 2004. Urban Sprawl and Public Health: Designing, Planning, and Building for Healthy Communities. [Google Scholar]
- Gibertoni D., Adja K.Y.C., Golinelli D., et al. Patterns of COVID-19 related excess mortality in the municipalities of Northern Italy during the first wave of the pandemic. Health Place. 2021;67:102508. doi: 10.1016/j.healthplace.2021.102508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong B., Im J., Mountrakis G. An artificial immune network approach to multi-sensor land use/land cover classification. Rem. Sens. Environ. 2011;115:600–614. [Google Scholar]
- Hamidi S., Ewing R., Sabouri S. Longitudinal analyses of the relationship between development density and the COVID-19 morbidity and mortality rates: early evidence from 1,165 metropolitan counties in the United States. Health Place. 2020;64:102378. doi: 10.1016/j.healthplace.2020.102378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamidi S., Sabouri S., Ewing R. Does density aggravate the COVID-19 pandemic? Early findings and lessons for planners. J. Am. Plann. Assoc. 2020;86:495–509. [Google Scholar]
- Handy S.L., Boarnet M.G., Ewing R., et al. How the built environment affects physical activity: views from urban planning. Am. J. Prev. Med. 2002;23:64–73. doi: 10.1016/s0749-3797(02)00475-0. [DOI] [PubMed] [Google Scholar]
- Harris R. Exploring the neighbourhood-level correlates of Covid-19 deaths in London using a difference across spatial boundaries method. Health Place. 2020;66:102446. doi: 10.1016/j.healthplace.2020.102446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hino K., Asami Y. Vol. 69. Health & place; 2021. Change in walking steps and association with built environments during the COVID-19 state of emergency: a longitudinal comparison with the first half of 2019 in Yokohama, Japan; p. 102544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson R.J. American Public Health Association; 2003. The Impact of the Built Environment on Health: an Emerging Field. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khattak A.J., Rodriguez D. Travel behavior in neo-traditional neighborhood developments: a case study in USA. Transport. Res. Pol. Pract. 2005;39:481–500. [Google Scholar]
- Kim B., Rundle A.G., Goodwin A.T.S., et al. COVID-19 testing, case, and death rates and spatial socio-demographics in New York City: an ecological analysis as of June 2020. Health Place. 2021;68:102539. doi: 10.1016/j.healthplace.2021.102539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kodera S, Rashed EA, Hirata A. Correlation between COVID-19 morbidity and mortality rates in Japan and local population density, temperature, and absolute humidity. Int. Res. J. Publ. Environ. Health. 2020;17:5477. doi: 10.3390/ijerph17155477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulu H., Dorey P. Infection rates from Covid-19 in Great Britain by geographical units: a model-based estimation from mortality data. Health Place. 2021;67:102460. doi: 10.1016/j.healthplace.2020.102460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lak A., Sharifi A., Badr S., et al. Sustainable cities and society; 2021. Spatio-temporal Patterns of the COVID-19 Pandemic, and Place-Based Influential Factors at the Neighborhood Scale in Tehran; p. 103034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li B., Peng Y., He H., et al. Built environment and early infection of COVID-19 in urban districts: a case study of Huangzhou. Sustainable cities and society. 2021;66:102685. doi: 10.1016/j.scs.2020.102685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S., Ma S., Zhang J. Association of built environment attributes with the spread of COVID-19 at its initial stage in China. Sustainable cities and society. 2021;67:102752. doi: 10.1016/j.scs.2021.102752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez-Zetina J., Lee H., Friis R. The link between obesity and the built environment. Evidence from an ecological analysis of obesity and vehicle miles of travel in California. Health Place. 2006;12:656–664. doi: 10.1016/j.healthplace.2005.09.001. [DOI] [PubMed] [Google Scholar]
- Ma S., Li S., Zhang J. Diverse and nonlinear influences of built environment factors on COVID-19 spread across townships in China at its initial stage. Sci. Rep. 2021;11:1–13. doi: 10.1038/s41598-021-91849-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mannering F.L., Shankar V., Bhat C.R. Unobserved heterogeneity and the statistical analysis of highway accident data. Analytic methods in accident research. 2016;11:1–16. [Google Scholar]
- Mannering F., Bhat C.R., Shankar V., et al. Big data, traditional data and the tradeoffs between prediction and causality in highway-safety analysis. Analytic methods in accident research. 2020;25:100113. [Google Scholar]
- Megahed N.A., Ghoneim E.M. Antivirus-built environment: lessons learned from Covid-19 pandemic. Sustainable cities and society. 2020;61:102350. doi: 10.1016/j.scs.2020.102350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen Q.C., Huang Y., Kumar A., et al. Using 164 million google street view images to derive built environment predictors of COVID-19 cases. Int. J. Environ. Res. Publ. Health. 2020;17:6359. doi: 10.3390/ijerph17176359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osgood D.W. Routledge; 2017. Poisson-based Regression Analysis of Aggregate Crime Rates. Quantitative Methods in Criminology; pp. 577–599. [Google Scholar]
- Pierce J.B., Harrington K., McCabe M.E., et al. Racial/ethnic minority and neighborhood disadvantage leads to disproportionate mortality burden and years of potential life lost due to COVID-19 in Chicago, Illinois. Health & place. 2021;68:102540. doi: 10.1016/j.healthplace.2021.102540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quddus M. Exploring the relationship between average speed, speed variation, and accident rates using spatial statistical models and GIS. J. Transport. Saf. Secur. 2013;5:27–45. [Google Scholar]
- Ramsey K., Bell A. Smart location database. 2014. https://www.epa.gov/sites/production/files/2014-03/documents/sld_userguide.pdf URL: Washington, DC.
- Rao M., Prasad S., Adshead F., et al. The built environment and health. The lancet. 2007;370:1111–1113. doi: 10.1016/S0140-6736(07)61260-4. [DOI] [PubMed] [Google Scholar]
- Raza W., Krachler B., Forsberg B., et al. Air pollution, physical activity and ischaemic heart disease: a prospective cohort study of interaction effects. BMJ open. 2021;11 doi: 10.1136/bmjopen-2020-040912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez D.A., Khattak A.J., Evenson K.R. Can new urbanism encourage physical activity?: comparing a new Urbanist neighborhood with conventional suburbs. J. Am. Plann. Assoc. 2006;72:43–54. [Google Scholar]
- Saelens B.E., Handy S.L. Built environment correlates of walking: a review. Med. Sci. Sports Exerc. 2008;40:S550. doi: 10.1249/MSS.0b013e31817c67a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis J.F., Floyd M.F., Rodríguez D.A., et al. Role of built environments in physical activity, obesity, and cardiovascular disease. Circulation. 2012;125:729–737. doi: 10.1161/CIRCULATIONAHA.110.969022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis J.F., Conway T.L., Cain K.L., et al. Neighborhood built environment and socioeconomic status in relation to physical activity, sedentary behavior, and weight status of adolescents. Prev. Med. 2018;110:47–54. doi: 10.1016/j.ypmed.2018.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis J.F., Cerin E., Kerr J., et al. Built environment, physical activity, and obesity: findings from the international physical activity and environment network (IPEN) adult study. Annu. Rev. Publ. Health. 2020;41:119–139. doi: 10.1146/annurev-publhealth-040218-043657. [DOI] [PubMed] [Google Scholar]
- Salon D. Heterogeneity in the relationship between the built environment and driving: focus on neighborhood type and travel purpose. Res. Transport. Econ. 2015;52:34–45. [Google Scholar]
- Sarkar C., Webster C., Gallacher J. Neighbourhood walkability and incidence of hypertension: findings from the study of 429,334 UK Biobank participants. Int. J. Hyg Environ. Health. 2018;221:458–468. doi: 10.1016/j.ijheh.2018.01.009. [DOI] [PubMed] [Google Scholar]
- Schmid D., Behrens G., Keimling M., et al. A systematic review and meta-analysis of physical activity and endometrial cancer risk. Eur. J. Epidemiol. 2015;30:397–412. doi: 10.1007/s10654-015-0017-6. [DOI] [PubMed] [Google Scholar]
- Shoichet C., Jones A. CNN; 2020. Coronavirus is making some people rethink where they want to live.https://www.cnn.com/2020/05/02/us/cities-population-coronavirus/index.html [Google Scholar]
- Train K.E. Cambridge university press; 2009. Discrete Choice Methods with Simulation. [Google Scholar]
- United Nations . Department of Economic and Social Affairs; 2020. The 17 Goals. Sustainable Development.https://sdgs.un.org/goals URL: [Google Scholar]
- Wali B., Greene D.L., Khattak A.J., Liu J. Analyzing within garage fuel economy gaps to support vehicle purchasing decisions–A copula-based modeling & forecasting approach. Transp. Res. D: Transp. Environ. 2018;63:186–208. [Google Scholar]
- Wali B., Khattak A.J., Bozdogan H., Kamrani M. How is driving volatility related to intersection safety? A Bayesian heterogeneity-based analysis of instrumented vehicles data. Transport. Res. C Emerg. Technol. 2018;92:504–524. [Google Scholar]
- Wali B., Khattak AJ., Karnowski T. The relationship between driving volatility in time to collision and crash-injury severity in a naturalistic driving environment. Anal. Methods Accid. Res. 2020;28:100136. [Google Scholar]
- Wali B., Santi P., Ratti C. Modeling consumer affinity towards adopting partially and fully automated vehicles–The role of preference heterogeneity at different geographic levels. Transport. Res. C Emerg. Technol. 2021;129:103276. [Google Scholar]
- Washington SP., Karlaftis MG., Mannering F. Statistical and econometric methods for transportation data analysis. Chapman and Hall/CRC; 2010. [Google Scholar]
- WHO Physical inactivity: a global public health problem. 2018. https://www.who.int/dietphysicalactivity/factsheet_inactivity/en/ Available at:
- Wooldridge J.M. 2015. Introductory Econometrics: A Modern Approach: Cengage Learning. [Google Scholar]
- Xu Y., Wang F. Built environment and obesity by urbanicity in the US. Health Place. 2015;34:19–29. doi: 10.1016/j.healthplace.2015.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Y., Xiang X. Examine the associations between perceived neighborhood conditions, physical activity, and mental health during the COVID-19 pandemic. Health Place. 2021;67:102505. doi: 10.1016/j.healthplace.2021.102505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang T.-C., Kim S., Zhao Y., et al. Examining spatial inequality in COVID-19 positivity rates across New York City ZIP codes. Health Place. 2021;69:102574. doi: 10.1016/j.healthplace.2021.102574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yasmin S., Eluru N., Pinjari A.R., et al. Examining driver injury severity in two vehicle crashes–A copula based approach. Accid. Anal. Prev. 2014;66:120–135. doi: 10.1016/j.aap.2014.01.018. [DOI] [PubMed] [Google Scholar]