Abstract
Background
Trials of acupuncture in the West began before textbooks about acupuncture were generally available. This placed trials at risk of possible faulty assumptions about the practice of acupuncture and adoption of problematic research assumptions and methods. Further, this lack of information has had an influence on the theories of developing a valid and reliable sham control treatment in clinical trials of acupuncture. This commentary explores these issues.
Methods
Literature review focussing on the time line of developments in the field, developments of sham interventions and use thereof and knowledge of physiological effects of needling.
Results
Early trials demonstrated a lack of knowledge about acupuncture. As the methodology of trials improved, new sham treatment methods were developed and adopted; however, the sham treatment methods were implemented without physiological studies exploring their potential physiological effects and without examining the broader practice of acupuncture internationally.
Conclusions
Mistaken assumptions about the practice of acupuncture reinforced by paucity of physiological investigations are factors that led to use of inappropriate sham interventions for acupuncture trials. These not only lead to confusing or misleading trial results, they, as far as we can see underestimate the effects of acupuncture leading to bias against acupuncture. There are significant problems with sham interventions and how they are applied in trials of acupuncture. Further research is needed to explore the effects of this both for future trials and for interpreting existing evidence.
Keywords: Acupuncture, Sham interventions, History sham acupuncture
1. Introduction
Clinical trials of acupuncture began in Japan in the 1960s1 with a big increase in the number of studies in the last twenty years.2 When trials of acupuncture began outside Asia in the early 1970s, there were few publications about acupuncture available in English3 and little knowledge available about its practice.4, 5 Table 1 summarises general availability of clinical textbooks in the 1970s-1990s. Few detailed clinical texts were available before the mid-1980s, with little known about the international diversity of practice methods till the 1990s. Hence, many clinical trials may have been performed before a more detailed understanding had been established of what constitutes the study and practice of acupuncture.
Table 1.
Timeline of influential acupuncture publications in English.
| Published year | Category | Textbook / Details |
|---|---|---|
| 1974 | * C | The Treatment of Disease by Acupuncture, 3rd edition, by Felix Mann |
| Introduction to acupuncture, dismissive of traditional acupuncture, but some clinical content, especially for medical doctors seeking a simplified approach | ||
| 1975 | * C | An Outline of Chinese Acupuncture by Academy of Traditional Chinese Medicine |
| Introductory book on acupuncture for Doctors in China, translated to English – minimal clinical content | ||
| 1978 | * C | Acupuncture The ancient art of healing, 3rd edition, by Felix Mann |
| Introductory book on acupuncture – minimal clinical content | ||
| 1978 | * C | Current Acupuncture Therapy by Jane Lee and CS. Cheung |
| Introductory book on acupuncture – minimal clinical content | ||
| 1978 | * C | Principle and Practice of Scientific Acupuncture by Anton Jayasuriya and Felix Fernando |
| Introductory book on acupuncture – somewhat more clinical content | ||
| 1980 | * C | Essentials of Chinese Acupuncture by Beijing, Shanghai, Nanjing Colleges of TCM |
| More detailed book on acupuncture for doctors in China, translated to English – slightly more clinical content that the Outline of Acupuncture | ||
| 1983 | * C | Acupuncture: a Comprehensive Text by Shanghai College of TCM (translated by John O‘Connor & Dan Bensky) |
| First book on TCM in English – more clinical detail with some treatments | ||
| 1983 | * C | The Web that has no Weaver by Ted Kaptchuk |
| Popular book detailing TCM, but not a clinical text – theory with diagnosis but no treatment details | ||
| 1985 | ⁎⁎ C | Fundamentals of Chinese Medicine by Beijing, Nanjing, Shanghai Colleges of TCM (translated by Nigel Wiseman & Andy Ellis) |
| First detailed clinical text on Chinese medicine, including some text on acupuncture | ||
| First translation to apply a glossary based translation methodology | ||
| Level of clinical detail and more detailed language difficult for many Western practitioners to absorb and use | ||
| 1986 | ⁎⁎ C | Foundations of Chinese Medicine by Giovanni Maciocia |
| More details of clinical content, but almost no use of a glossary and often very simplistic approach to descriptions allowing more readers to use the content – but at expense of clinical details | ||
| 1987 | ⁎⁎ C | Chinese Acupuncture and Moxibustion by Xinnong Cheng |
| English translation from Chinese text with more details of clinical practice and techniques than the previous Outline and Essentials texts | ||
| 1988 | * J | Hara Diagnosis by Kiiko Matsumoto, Stephen Birch |
| Introduces Japanese acupuncture but minimal clinical content | ||
| 1988 | ⁎⁎ C | Fundamentals of Chinese Acupuncture by Andrew Ellis et al. |
| Glossary based translation and compilation with more details of clinical practice and techniques | ||
| 1989 | ⁎⁎ M | Acupuncture, Trigger Points and Musculoskeletal Pain by Peter Baldry |
| First detailed textbook for medical practitioners describing trigger point based system of acupuncture | ||
| 1990 | ⁎⁎ J | Introduction to Meridian Therapy by Denmei Shudo |
| First detailed clinical textbook of Japanese acupuncture detailing very shallow and light needling methods | ||
| 1994 | ⁎⁎ C | The Practice of Chinese Medicine by Giovanni Maciocia |
| More detailed clinical textbook of TCM practice | ||
| 1995 | ⁎⁎ M | Acupuncture Energetics: a Clinical Approach for Physicians by Joseph Helms |
| Detailed textbook on medical acupuncture clinical methods | ||
| 1995 | ⁎⁎ J | Chasing the Dragon's Tail by Yoshio Manaka et al. |
| Detailed clinical text describing Japanese acupuncture methods especially with shallow, light needling | ||
| 1998 | ⁎⁎ J | Japanese Acupuncture: a Clinical Guide by Stephen Birch, Junko Ida |
| Text detailing Japanese acupuncture treatment methods including non-inserted and shallow insertion acupuncture | ||
| 1998 | ⁎⁎ M | Medical Acupuncture a Western Scientific Approach by Jacqueline Filshie and Adrian White |
| Detailed textbook on medical acupuncture clinical methods | ||
| 1999 | ** C, J, M | Understanding Acupuncture by Stephen Birch & Robert Felt |
| First history clearly describing the variety of acupuncture methods of different countries. No clinical details |
, textbook introductory and basic with less clinical details;
, textbook has more clinical details; C, Chinese based needling; J, Japanese based shallow needling; M, medical acupuncture (including shallow needling).
This is a summary of influential publications in English that the authors (TA and SB) came across or contributed to during and after their initial studies in United Kingdom and in the United States, between 1979 and 1982, where there were almost no publications available in English that could be used as textbooks.
By the mid-1970s, varieties of the Chinese technique of inserted needling with sensory stimulation became a focus of study for clinical trial research published in English. Table 1 shows us that this focus developed before more detailed clinical textbooks were available. This lack of knowledge about acupuncture practice appears to have been problematic, as evidenced by the persistent lack of adequate treatments and often inappropriate treatments up through the 1990s with a paucity of literature citation to support treatment selection.6, 7, 8, 9, 10– To counter this, a way forward was the development and adoption of the STRICTA guidelines for reporting in clinical trials of acupuncture in the early 2000s.11, 12 During the period of the 1970s-1990s many different sham acupuncture methods were attempted13, 14 before much debate on the methodological requirements for such trials occurred and without a consensus on their description and adoption. The large number of different sham acupuncture methods are problematic for a number of reasons, chief among them the inability to draw conclusions across the studies.14 The range of sham interventions also heralds a lack of agreement on what might constitute a valid sham intervention among researchers.
A few papers in the 1980s discussed sham methods and requirements, but with little consensus on how to proceed.15, 16, 17, 18, 19, 20– After the establishment in 1992 of both the Office of Alternative Medicine (OAM) and the Society for Acupuncture Research (SAR), methodological discussions increased as critical analyses of methodological shortfalls and requirements emerged.10,21, 22, 23, 24, 25, 26– This increased discussion of the quality and methodology of acupuncture trials led, in the US first to an FDA workshop on acupuncture in 1994, followed two years later by the reclassification of acupuncture so that is no longer considered experimental.27 But there was still little detailed debate about the methodological needs for sham acupuncture clinical trials.
1.1. Purposes of control treatments
Placebo medications are used in controlled trials of a pharmacological substance in order to control for placebo effects and other non-specific effects of a therapy.28 For the control treatment to be considered as a placebo treatment it must be indistinguishable from the test treatment and be physiologically inert.29, 30 Sham treatment is used as a control treatment in clinical trials of a technique or device in order to control for the same effects.21 The placebo pill or sham technique/device should avoid the known pathways of action of the tested therapy.31 Since acupuncture is a treatment method, it needs to be subjected to the same testing as other interventions: it must demonstrate effectiveness beyond placebo. Hence, it must be tested in clinical trials that compare it to an inert fake or ‘sham acupuncture.’ Inducing a need for a detailed understanding of how acupuncture works so that we can be confident that a selected sham treatment avoid the mechanisms by which acupuncture works.32 Leading on to several questions we are aiming to answer: Is there a gap between the appearance and use of sham acupuncture control techniques and the appearance of a developed corpus of clinical acupuncture literature in English? Is there evidence of problems that may have resulted from this gap?
2. Methods
We will examine English language textbooks on the history and practice of acupuncture, papers on clinical trials of acupuncture, research methods and sham control interventions along with physiological studies of acupuncture. Furthermore, we will map out the time line of developments in the field, developments of sham interventions and knowledge of physiological effects of needling. In this brief review, we did not adopt a systematic searching strategy because of the narrative nature of this study. We made a potential list of literature on acupuncture based on recall from our own experiences and discussed it with each other to confirm whether or not to include them. Having previously written a number of papers about research publications on acupuncture,6,10,13 we drew from those and related papers to expose details of the history and nature of trials and their methods.
3. Development of sham acupuncture interventions
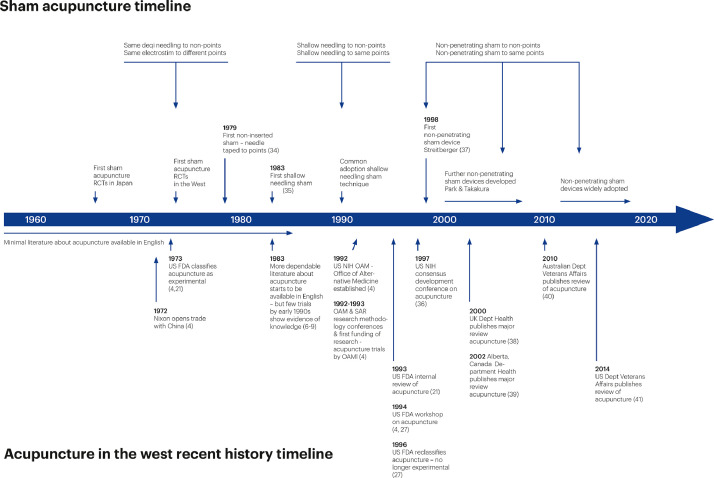
The first controlled trials of acupuncture were conducted in Japan in the 1960s and began in the West in the early 1970s,1, 33 but these were published in Japanese and remain virtually unknown outside Japan. Fig. 1 sketches the development of the main sham acupuncture methods published in English, contextualizing them against the background of other important developments in acupuncture34, 35, 36, 37, 38, 39, 40, 41; see also Table 1. The first trials of acupuncture began exploring two claims: that the sensory stimulation needling technique of deqi is effective and that it is more effective if applied to specific loci. There was no clear idea how to do sham acupuncture so early trialists designed their own approaches depending on what they thought to be important. Applying the same sensory stimulation techniques to loci not thought to be acupuncture points or not relevant to the symptom being treated in the trial42; apply some other form of needle stimulation than TCM's deqi sensory stimulation to the same acupuncture points34 or to other loci.35
Fig. 1.
Timeline for development acupuncture and sham acupuncture in English 1960–2020
Numbers in parentheses are to publications in the reference list.
By 1976, evidence began emerging that linked Chinese sensory stimulation needling with endorphins.1,4,5,43,44 This link was seen as very important as it increased the credibility of acupuncture.21 With acupuncture seen as a stimulation method to release endorphins this became the mechanism that acupuncture was thought to elicit, hence avoidance of this mechanism in the sham acupuncture treatment arm became more critical by the late 1970s. Efforts to avoid sensory stimulation with the needles led by the early 1980s to the regular adoption of the use of shallowly inserted needles with no manipulation – which became known as ‘minimal acupuncture.’35 It was thought that this technique should suffice as a sham35,45 and even as a placebo treatment45 control intervention for acupuncture trials, despite the fact that shallow sensationless needling was routinely used as a treatment method by many acupuncturists in Japan,1,4 Presumably this occurred because the research investigators involved were unaware of how Japanese acupuncture was practised. Additionally no physiological studies were conducted to test the hypothesis that shallow sensation-less needling is physiologically inert or to explore what physiological effects it might trigger and demonstrate that they are not relevant to the effectiveness of acupuncture. Hence the adoption of ‘minimal acupuncture’ as a sham control thought by some to be a placebo treatment was suppositional and not based on any evidence. In fact, a trial conducted in 1983 showing that shallow needling was effective appears to have been ignored by researchers,46 but not by clinicians.47 Reasons why emerging literature and evidence about shallow needling were ignored are not clear, but perhaps the absence of systematic debate allowed personal choices and preferences to dominate. The primary test of validity of these control interventions was to test and demonstrate the credibility of the sham intervention.48,49 We are not aware of pilot studies or physiological investigations50 being conducted to investigate whether this sham acupuncture technique is appropriate as a control treatment for acupuncture that can control for placebo effects.
Following use of ‘minimal acupuncture’ as a sham treatment for acupuncture, discussions began to emerge questioning whether this was a sufficient or appropriate sham control, with suggestions that non-penetrating sham would be better.25,26,50 Various non-penetrating sham techniques were starting to be used.51, 52, 53, 54– Then, in 1998, an innovative non-penetrating sham device was developed by Streitberger and colleagues,37 which was thought to both control for placebo effects and finally address the limitations of other sham techniques, especially once it was found to be a credible treatment. Park and colleagues55 and Takakura and colleagues56 developed novel components to this sham-acupuncture technology. In all cases validation was performed through credibility testing and ensuring that the treatments could be blinded. Physiological studies were not performed to demonstrate that the techniques were inert, or to explore what physiological mechanisms are stimulated or to demonstrate that they are unimportant for treatment effectiveness. Nor were pilot studies conducted.
4. Discussion
We found that assumptions underlying the selection of sham interventions for trials of acupuncture were mostly based on the notion of using a control treatment with minimal or no sensory stimulation to control for the sensory stimulation of deqi. While a broader knowledge of the practice of acupuncture including non-sensory stimulation (non-deqi based) needling techniques was emerging (see Table 1 and Fig. 1) it appears not to have influenced the thinking of clinical trialists. Perhaps this is because this knowledge had not yet emerged in medical databases like Pubmed, and because trialists tended to test what they knew or had studied which was not based upon extensive surveys or reviews of the field. Additionally, we have seen that little or no physiological research was conducted to validate these sham interventions as being physiologically inert or whether physiological effects that result from not being inert have clinically relevant effects. Instead, validation focused only on establishing blinding and credibility of the interventions. This is insufficient given the multiple physiological pathways and their potential effects of any form of sensory stimulation from touch to frank pain.
As we explored the sham interventions, we additionally uncovered another significant problem for the non-penetrating sham devices. The Streitberger and Takakura groups made several methodological mistakes in their development and testing of their sham devices. Given that sham acupuncture studies have varied the sites of needling and the techniques of needling there are three basic types of sham acupuncture, each of which investigates different questions.57 One of the three sham models applies the sham technique to the same acupoints as the test treatment while holding placebo equal between the two groups, this is a comparison of only the two techniques of treatment not a test of acupuncture.57,58 Streitberger59,60 and Takakura61 both used this model while thinking that they were answering the question of acupuncture's effectiveness (one of the other two sham models).57 These trials showed that the sham technique was as effective as the real technique. By their own efforts, the researchers that developed the sham devices have themselves demonstrated that the devices should not be used in clinical trials of acupuncture as a control treatment. The 2009 trial of So and colleagues investigating acupuncture to improve effectiveness of IVF procedures also used a non-penetrating sham device applied to the same points as the real treatment.63 This trial found the non-penetrating sham needling to be significantly more effective than the ‘real’ needling,62 which was viewed as demonstrating that acupuncture is not effective to assist IVF procedures rather than that milder sensory stimulation of the treatment points is more effective than heavier sensory stimulation of the treatment points for increasing IVF's effectiveness.62 Putting aside the trialists’ poor understanding of trial methodology, this trial is important because when we look to the probable mechanisms by which acupuncture might work to assist IVF procedures, it is likely due to the increased relaxation that acupuncture can produce.63 The milder stimulation of the non-penetrating device will stimulate structures and pathways at or just below the skin, which are probably more relaxing than the pathways triggered by deeper needling that is more stimulating.64 In this last example, we see probable physiological explanations for why the non-penetrating sham devices are not appropriate. From the above, serious questions emerge about the use of sham acupuncture with the findings from these studies. The non-inertness of sham acupuncture has been known for more than three decades,19,57,65, 66, 67 with no meaningful efforts to counter this or account for this in study design and interpretation of results except for the use of the no longer used non-comparative16 ‘mock TENS’ control.26 The use of non-inert sham introduces bias against acupuncture with risk of underestimating its’ effectiveness.57,66 Given the depth of problems we have exposed above with how sham studies have been conceived and conducted, it is important to examine these problems in more depth.
4.1. Conclusions
Since acupuncture related techniques and knowledge expanded in the 1970s in the western world, clinical trials have been conducted with a number of different types of sham acupuncture procedure, none of which can be accepted as proper sham controls in the sense of indistinguishability and physiological inertness. Current debates around the clinical evidence of acupuncture for various conditions appear to be derived from misunderstandings regarding the heterogeneous nature of acupuncture practice in different regional environments and the inappropriate selection of sham control techniques without clear consideration of research questions. We hope that this brief overview on the history of sham acupuncture techniques will be helpful for future researchers to understand the current problems about acupuncture studies. We suggest further analysis of the different sham procedures used in clinical trials of acupuncture is in order to better understand what purposes they can serve and what research questions they can answer. This will help to standardize how such trials are analysed and interpreted in systematic reviews, meta-analyses and to make the evidence base for acupuncture clearer.
Declaration of Competing Interest
The authors declare no conflict of interests.
Acknowledgments
Acknowledgement
Assistance provided by Merete Lindén Dahle with the design of Fig. 1, was greatly appreciated.
Author contribution
Conceptualization: SB, TA, MSL, and THK. Methodology: SB, TA, MSL, and THK. Resources: SB and TA. Writing – Original Draft: SB, TA, MSL, and THK. Writing – Review & Editing: SB, TA, MSL, and THK. Visualization: TA.
Funding
No specific funding was received for this study.
Ethical statement
Not applicable.
Data availability
The data used for this study are included in this manuscript.
References
- 1.Birch S., Lewith G., MacPherson H., Hammerschlag.R Lewith G, Schnyer R. Elsevier; London: 2007. Acupuncture Research: Strategies for Building an Evidence Base; pp. 15–35. Acupuncture research, the story so far. [Google Scholar]
- 2.Ma Y., Dong M., Zhou K., Mita C., Liu J., Wayne P.M. Publication trends in acupuncture research: a 20-year bibliometric analysis based on PubMed. PLoS ONE. 2016;11 doi: 10.1371/journal.pone.0168123. e0168123.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Birch S., Tsutani K. Survey of English-language publications on acupuncture. Complem Ther Med. 1996;4:172–177. [Google Scholar]
- 4.Birch S., Felt R. Churchill Livingstone; London: 1999. Understanding Acupuncture. [Google Scholar]
- 5.Lu G.D., Needham J. Cambridge University Press; Cambridge: 1980. Celestial Lancets, a History and Rationale of Acupuncture and Moxibustion. [Google Scholar]
- 6.Birch S.J. University of Exeter; 1997. An Exploration With Proposed Solutions of the Problems and Issues in Conducting Clinical Research in Acupuncture. [Google Scholar]
- 7.Ezzo J., Berman B., Hadhazy V.A., Jadad A.R., Lao L., Singh B.B. Is acupuncture effective for the treatment of chronic pain: a systematic review. Pain. 2000;86:217–225. doi: 10.1016/S0304-3959(99)00304-8. [DOI] [PubMed] [Google Scholar]
- 8.Birch S. Issues to consider in determining an adequate treatment in a clinical trial of acupuncture. Compl Ther Med. 1997;5:8–12. [Google Scholar]
- 9.Stux G., Birch S. Proposed standards of acupuncture treatment in clinical studies. In: G Stux, R. Hammerschlag., editors. Scientific Bases of Acupuncture in Basic and Clinical Research. Springer Verlag; Berlin: 2000. pp. 171–185. [Google Scholar]
- 10.Birch S. Proceedings of the Second Society for Acupuncture Research. 1994. Testing the clinical specificity of needle sites in controlled clinical trials of acupuncture: part one - the importance of validating the "relevance" of "true" or "active" points and "irrelevance" of "control" or "less-active" points - proposals for a justification method; Part two - the problem of "diffuse noxious inhibitory control", DNIC, and how to control for it; pp. 274–294. [Google Scholar]
- 11.MacPherson H., White A., Cummings M. Standards for Reporting Interventions in Controlled Trials of Acupuncture: the STRICTA recommendations. Compl Ther Med. 2001;9:246–249. doi: 10.1054/ctim.2001.0488. [DOI] [PubMed] [Google Scholar]
- 12.Macpherson H., Altman D.G., Hammerschlag R. on behalf of the STRICTA revision group. Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT Statement. Acupunct Med. 2010;28(2):83–93. doi: 10.1136/aim.2009.001370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Birch S. Controlling for non-specific effects of acupuncture in clinical trials. Clin Acup Orient Med. 2003;4(2–3):59–70. [Google Scholar]
- 14.Dincer F., Linde K. Sham interventions in randomized clinical trials of acupuncture—A review. Complement Ther Med. 2003;11(4):235–242. doi: 10.1016/s0965-2299(03)00124-9. [DOI] [PubMed] [Google Scholar]
- 15.ter Riet G., Kleijnen J., Knipschild P. Acupuncture and neck pain/back pain [in Dutch] Huisarts Wet. 1989;32:223–227. [Google Scholar]
- 16.ter Riet G., Kleijnen J., Knipschild P. Acupuncture and chronic pain: a criteriabased metaanalysis. J Clin Epidemiol. 1990;43(11) doi: 10.1016/0895-4356(90)90020-p. [DOI] [PubMed] [Google Scholar]
- 17.Vincent C.A., Richardson P.H. The evaluation of therapeutic acupuncture: concepts and methods. Pain; 1986;24:1–13. doi: 10.1016/0304-3959(86)90022-9. [DOI] [PubMed] [Google Scholar]
- 18.Vincent C.A. The methodology of controlled trials of acupuncture. Acupuncture Med. 1989;VI(14):9–13. [Google Scholar]
- 19.Lewith G.T., Machin D. On the evaluation of the clinical effects of acupuncture. Pain; 1983;16 doi: 10.1016/0304-3959(83)90202-6. [DOI] [PubMed] [Google Scholar]
- 20.Vincent C.A., Richardson P.H., Black J.J., Pither C.E. The significance of needle placement site in acupuncture. J Psychosomatic Res; 1989;33(4):489–496. doi: 10.1016/0022-3999(89)90010-x. [DOI] [PubMed] [Google Scholar]
- 21.Lytle C.D. An overview of acupuncture; U.S. Department of Health and Human Services, Public Health Service, Food and Drug Administration, Center For Devices and Radiological Health, 1993.
- 22.Vincent C., Lewith G. Placebo controls for acupuncture studies. J R Soc Med. 1995;88:199–202. [PMC free article] [PubMed] [Google Scholar]
- 23.Society for Acupuncture Research . Proceedings of the First Symposium of the Society for Acupuncture Research. 1993. held January 23-24. [Google Scholar]
- 24.Society for Acupuncture Research . Proceedings of the Second Symposium of the Society for Acupuncture Research. 1994. held September 17-18. [Google Scholar]
- 25.Society for Acupuncture Research . Proceedings of the third symposium of the Society for Acupuncture Research. 1995. held September 16-17. [Google Scholar]
- 26.Lewith G.T., Vincent C. On the evaluation of the clinical effects of acupuncture: a problem reassessed and a framework for future research. J Altern Compl Med. 1996;2:79–90. doi: 10.1089/acm.1996.2.79. [DOI] [PubMed] [Google Scholar]
- 27.Alpert S. Letter—Reclassification order, Docket No. 94P-0443, Acupuncture needles for the practice of acupuncture. Fed Regist. 1996:64616–64617. https://www.govinfo.gov/content/pkg/FR-1996-12-06/html/96-31047.htm Volume 61, Number 236 (Friday, December 6, [Google Scholar]
- 28.Ernst E., Resch K.L. Concept of true and perceived placebo effects. BMJ. 1995;311:551–553. doi: 10.1136/bmj.311.7004.551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gupta U., Verma M. Placebo in clinical trials. Perspect Clin Res. 2013;4(1):49–52. doi: 10.4103/2229-3485.106383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hernandez A., Banos J.-.E., Llop C., Farre M. The definition of placebo in the informed consent forms of clinical trials. PLoS ONE. 2014;9(11) doi: 10.1371/journal.pone.0113654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thomas K., Fitter M. Possible research strategies for evaluating CAM interventions. In: Lewith G, Jonas WB, Walach H, editors. Clinical Research in Complementary Therapies. Churchill Livingstone; Edinburgh: 2002. pp. 59–91. [Google Scholar]
- 32.Langevin H.M., Wayne P.M., Macpherson H. Paradoxes in acupuncture research: strategies for moving forward. eCAM. 2011;2011 doi: 10.1155/2011/180805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tsutani K., Shichido T., Sakuma K. When acupuncture met biostatistics. Proceedings of the Second World Conference of Acupuncture and Moxibustion; Paris; 1990. [Google Scholar]
- 34.Jensen L.B., Melsen B., Jensen S.B. Effect of acupuncture on headache measured by reduction in number of attacks and use of drugs. Scandinavian Journal of Dental Research; 1979;87:373–380. doi: 10.1111/j.1600-0722.1979.tb00696.x. [DOI] [PubMed] [Google Scholar]
- 35.Hansen P.E., Hansen J.H. Acupuncture treatment of chronic facial pain - a controlled cross-over trial. Headache; 1983;23:66–69. doi: 10.1111/j.1526-4610.1983.hed2302066.x. [DOI] [PubMed] [Google Scholar]
- 36.NIH consensus conference acupuncture. JAMA. 1998;280:1518–1524. [PubMed] [Google Scholar]
- 37.Streitberger K., Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet. 1998;352:364–365. doi: 10.1016/S0140-6736(97)10471-8. [DOI] [PubMed] [Google Scholar]
- 38.British Medical Association Board of Science and Education . Harwood Academic Publishers; London: 2000. Acupuncture: Efficacy, Safety and Practice. [Google Scholar]
- 39.Tait P.L., Brooks L., Harstall C. Alberta Heritage Foundation for Medical Research; Alberta, Canada: 2002. Acupuncture: Evidence from Systematic Reviews and Meta-Analyses. [Google Scholar]
- 40.Australian Government Department of Veterans' Affairs. Australian Government Department of Veterans' Affairs; 2010. Australian Government Department of Veterans' Affairs. Alternative therapies and Department of Veterans' Affairs Gold and White Card arrangements. [Google Scholar]
- 41.Hempel S., Taylor S.L., Solloway M.R., Miake-Lye I.M., Beroes J.M., Shanman R. Evidence Map of Acupuncture. Department of Veterans Affairs; WashingtonDC: 2014. VA evidence-based synthesis program reports. [PubMed] [Google Scholar]
- 42.Baust W., Strutzbecher H. Akupunkturbehandlung der migraine in doppelblindversuch. Med. Welt. 1978;29:669–673. [PubMed] [Google Scholar]
- 43.Pomeranz B., Chiu D. Naloxone blocks acupuncture analgesia and causes hyperalgesia. Life Sci. 1976;19:1757–1762. doi: 10.1016/0024-3205(76)90084-9. [DOI] [PubMed] [Google Scholar]
- 44.Pomeranz B., Berman B., Stux G., Berman B., Pomeranz B. Basics of Acupuncture. Springer; Berlin: 2003. Scientific basis of acupuncture; pp. 1–86. [Google Scholar]
- 45.Hansen P.E., Hansen J.H. Acupuncture treatment of chronic tension headache- a controlled cross-over trial. Cephalgia; 1985;5:137–142. doi: 10.1046/j.1468-2982.1985.0503137.x. [DOI] [PubMed] [Google Scholar]
- 46.MacDonald A.J.R., Macrae K.D., Master B.R., Rubin A.P. Superficial acupuncture in the relief of chronic low back pain. Ann R Coll Surg Engl. 1983;65:44–46. [PMC free article] [PubMed] [Google Scholar]
- 47.Baldry P.E. Churchill Livingstone; Edinburgh: 1989. Acupuncture Trigger points and Musculoskeletal Pain. [Google Scholar]
- 48.Vincent C.A. Credibility assessment in trials of acupuncture. Compl Med Res. 1990;4(1):8–11. [Google Scholar]
- 49.Petrie J., Hazelman B. Credibility of placebo transcutaneous nerve stimulation and acupuncture. Clin Exp Rheum. 1985;3:151–153. [PubMed] [Google Scholar]
- 50.Hammerschlag R. Methodological and ethical issues in clinical trials of acupuncture. J Altern Compl Med. 1998;4:159–171. doi: 10.1089/acm.1998.4.159. [DOI] [PubMed] [Google Scholar]
- 51.Lao L.X., Bergman S., Anderson R., Langenberg P., Wong R.H., Berman B. The effect of acupuncture on post-operative oral surgery pain: a pilot study. Acupunct Med. 1994;12(1):13–17. [Google Scholar]
- 52.Molsberger A., Hille E. The analgesic effect of acupuncture in chronic tennis elbow pain. Br J Rheumatol. 1994;33(12):1162–1165. doi: 10.1093/rheumatology/33.12.1162. [DOI] [PubMed] [Google Scholar]
- 53.Hesse J., Mogelvang B., Simonsen H. Acupuncture versus metoprolol in migraine prophylaxis: a randomized trial of trigger point inactivation. J Internal Med. 1994;235:451–456. doi: 10.1111/j.1365-2796.1994.tb01102.x. [DOI] [PubMed] [Google Scholar]
- 54.White A.R., Eddleston C., Hardie R., Resch K.L., Ernst E. A pilot study of acupuncture for tension headache, using a novel placebo. Acupunct Med. 1996;14(1):11–15. [Google Scholar]
- 55.Park J., White A., Lee H., Ernst E. Development of a new sham needle. Acupunct. Med. 1999;17:110–112. [Google Scholar]
- 56.Takakura N., Yajima H. A double-blind placebo needle for acupuncture research. BMC Compl Altern Med. 2007;7:31. doi: 10.1186/1472-6882-7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Birch S., Alraek T., Kim K.H., Lee M.S. Chapter 4 Placebo controlled trials in acupuncture: problems and solutions. In: S. Leung, H. Hu., editors. Evidence Based Chinese Medicine. Evidence-based Research Methods for Chinese Medicine; 2016. pp. 55–64. [DOI] [Google Scholar]
- 58.Birch S., Hammerschlag R., Trinh K., Zaslawski C. The non-specific effects of acupuncture treatment: when and how to control for them. Clin Acup Orien Med. 2002;3(1):20–25. [Google Scholar]
- 59.Kleinhenz J., Streitberger K., Windeler J., Güssbacher A., Mavridis G., Martin E. Randomised clinical trial comparing the effects of acupuncture and a newly designed placebo needle in rotator cuff tendinitis. Pain. 1999;83:235–241. doi: 10.1016/s0304-3959(99)00107-4. [DOI] [PubMed] [Google Scholar]
- 60.Streitberger K., Friedrich-Rust M., Bardenheuer H. Effect of acupuncture compared with placebo-acupuncture at P6 as additional antiemetic prophylaxis in high-dose chemotherapy and autologous peripheral blood stem cell transplantation: a randomized controlled single-blind trial. Clin. Cancer Res. 2003;9:2538–2544. [PubMed] [Google Scholar]
- 61.Takakura N., Yajima H. Analgesic effect of acupuncture needle penetration: a double-blind crossover study. Open Med. 2009;3:e54–e61. [PMC free article] [PubMed] [Google Scholar]
- 62.So E.W., Ng E.H., Wong Y.Y., Lau E.Y., Yeung W.S., Ho P.C. A randomized double blind comparison of real and placebo acupuncture in IVF treatment. Hum. Reprod. 2009;24:2–8. doi: 10.1093/humrep/den380. [DOI] [PubMed] [Google Scholar]
- 63.Manheimer E. Selecting a control for in vitro fertilization and acupuncture randomized controlled trials (RCTs): how sham controls may unnecessarily complicate the RCT evidence base. Fertil Steril. 2011;95(8):2456–2461. doi: 10.1016/j.fertnstert.2011.04.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhang Z.J., Wang X.M., McAlonan G.M. Neural acupuncture unit: a new concept for interpreting effects and mechanisms of acupuncture. Evid Based Compl Alternat Med. 2012;2012 doi: 10.1155/2012/429412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fregni F., Imamura M., Chien H.F. Challenges and recommendations for placebo controls in randomized trials in physical and rehabilitation medicine: a report of the international placebo symposium working group. Am J Phys Med Rehabil. 2010;89:160–172. doi: 10.1097/PHM.0b013e3181bc0bbd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Appleyard I., Lundeberg T., Robinson N. Should systematic reviews assess the risk of bias from sham–placebo acupuncture control procedures? Eur J Integr Med. 2014;6:234–243. [Google Scholar]
- 67.Lund I., Naslund J., Lundeberg T. Minimal acupuncture is not a valid placebo control in randomised controlled trials of acupuncture: a physiologist's perspective. Chin Med. 2009;4:1. doi: 10.1186/1749-8546-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used for this study are included in this manuscript.