Abstract
Evidence suggests that perceived stress and psychological resilience are related to the presence and severity of cardiometabolic disease. Despite increased stress and cardiometabolic disease burden among American Indian and Alaska Native (AI/AN) people, the relationships between these factors are not well established in these populations. The objective of this study was to evaluate the relationships of stress with five cardiometabolic health indicators and to assess whether psychological resilience mediates these relationships in AI/AN adults. Four hundred and ninety-six AI/AN attendees were surveyed at three powwows. The questionnaire included sociodemographic items, questions on self-reported obesity, prediabetes, diabetes, high blood pressure, and high cholesterol, the Perceived Stress Scale, and the Brief Resilience Scale. Multivariable logistic regression models were used to measure associations of health indicators with Perceived Stress Scale and Brief Resilience Scale scores while controlling for sociodemographic characteristics. Among respondents, obesity was the most common cardiometabolic health indicator reported (48%), followed by high blood pressure, prediabetes, diabetes, and high cholesterol. Mean Perceived Stress Scale and Brief Resilience Scale scores were 16.1 (6.4 SD) and 3.5 (0.7 SD), respectively. Higher Perceived Stress Scale scores were associated with greater odds of self-reported prediabetes and diabetes. Brief Resilience Scale scores did not serve as a mediator. These results suggest that perceived stress is associated with some self-reported indicators of cardiometabolic health among AI/AN adults, but findings are limited by the convenience sample, reliance on self-report, and cross-sectional design. Future work should capitalize on nationally representative data, longitudinal designs, and objective measures of cardiometabolic health.
Keywords: Native American, Indigenous, Chronic disease, Health disparities
1. Introduction
American Indian and Alaska Native (AI/AN) individuals experience excess stress and discrimination (American Psychological Association, 2016) and are more likely to live in poverty than non-Hispanic white Americans (Sarche and Spicer, 2008). Chronic stress can develop from a variety of sources, from daily hassles to major life events or latent sources, such as settler colonialism (Elm et al., 2019). Psychological resilience may limit the physiological effects of stress (Southwick et al., 2014, Karatsoreos and McEwen, 2013). Psychological resilience has been defined as an individual’s ability to cope positively with stress (Connor and Davidson, 2003) or to maintain a positive outlook on life, despite negative circumstances (Toukhsati et al., 2017). AI/AN communities are a diverse grouping, comprising more than 5.6 million people from more than 600 federal or state recognized tribes (Office of Minority Health, 2018), with a variety of histories, practices, and regional influences. Resilience is a commonly recognized value despite – and perhaps a result of – the shared and multi-generational experiences of adversity and trauma that AI/AN communities have experienced, both historically and today (Ore et al., 2016).
Research shows that chronic or severe stress may increase the risk of cardiometabolic diseases (Richardson et al., 2012, Felix et al., 2019, Lehrer et al., 2020). Similarly, a systematic review of descriptive studies supports the association of higher resilience scores with reduced chronic disease severity (Cal et al., 2015). AI/AN adults have a higher prevalence of cardiometabolic conditions, such as obesity (44% vs. 29%), diabetes (18% vs. 7%), and coronary heart disease (8% vs. 6%), compared with non-Hispanic White adults (Obesity and American Indians, 2017, Diabetes and American Indians, 2016, Office of Minority Health, 2017). The National Longitudinal Study of Adolescent to Adult Health (Add Health), a longitudinal study of a nationally representative sample of adolescents, found higher average perceived stress levels among AI/AN respondents compared with all study participants (Marley and Metzger, 2015). Higher stress levels among AI/AN adolescents were cross-sectionally associated with self-reported diagnoses of high blood glucose or diabetes (Marley and Metzger, 2015). Further, psychological resilience appears to mediate the relationship between stress and cardiometabolic health in a convenience sample of adults in the Southwestern U.S. (Lehrer et al., 2020).
The present study sought to evaluate the relationships of stress and psychological resilience with five self-reported cardiometabolic health indicators (obesity, prediabetes, diabetes, high blood pressure, high cholesterol) in a cross-sectional, multi-state survey of AI/AN respondents and to assess whether resilience mediates any observed associations between stress and cardiometabolic health. It was hypothesized that higher stress would be associated with poorer cardiometabolic health, and that greater resilience would be associated with better self-reported cardiometabolic health. Further, it was expected that resilience would mediate or disrupt the associations between stress and cardiometabolic health.
2. Materials and methods
2.1. Data collection
Cross-sectional surveys were distributed to AI/AN attendees at three large powwows. Powwows are public community events that celebrate the cultural traditions and practices of AI/AN tribes and communities. The number of attendees at a powwow varies; attendees range from predominantly local residents to international visitors. For this study, participants were recruited from powwows hosted in Oklahoma and Washington State between June and August 2018. Typical annual powwow attendance combined across these three events is estimated at 7500 attendees. Eligibility criteria to participate in the survey were self-identification as AI/AN (alone or with one or more additional races) and aged 18 years or older. The 45-item anonymous survey was completed onsite in paper-and-pencil format. This research was determined to be exempt by the Washington State University Institutional Review Board (Protocol #15144), and informed consent was not required. Participants received a $10.00 gift card as compensation for their time.
2.2. Measures
Sociodemographic characteristics. Participants self-reported their age in years. Gender was categorized as “female” and “male” or “other” for analysis. Race was not a mutually exclusive variable, in that respondents were asked to select all categories that applied to them from a list consisting of “American Indian,” “Alaska Native,” “Asian,” “Native Hawaiian or Pacific Islander,” “African American or Black,” “White,” and “Other.” Ethnicity was recorded dichotomously as either “Latino/Latina or Hispanic” or “Not Latino/Latina or Hispanic.” Self-reported highest level of education was classified as “no high school diploma or GED,” “high school graduate or GED,” “some college but no degree,” “technical/vocational degree or Associate’s degree,” or “bachelor’s or graduate degree.” Marital status was recorded as “married or living with partner,” “widowed, divorced, or separated,” and “never married.” Finally, residence was considered as “reservation or rural area,” “small town,” or “large metropolitan area.”
Health status. Respondents rated their health on a 5-point Likert scale from “Excellent” =5 to “Poor” =1. Self-reported height (inches) and weight (pounds) were used to calculate body mass index (BMI) as kilograms/meters2 and to categorize participants as obese (BMI ≥ 30) or not obese (BMI < 30). Participants self-reported prior diagnoses (“yes” or “no”) made by a health professional of prediabetes, diabetes, high blood pressure, and high cholesterol.
Perceived stress. Cohen’s 10-item Perceived Stress Scale evaluates experiences of stress in the prior month (Cohen et al., 1983). This questionnaire has been used in various countries and has demonstrated convergent and discriminant validity, internal reliability, and test–retest reliability in adult populations (Lee, 2012). In response to statements such as “how often have you been able to control things that bother you” or “how often have you felt things were piling up so high that you could not overcome them,” each item is rated on a 5-point Likert scale that ranges from “Never” =0 to “Very Often” =4 or from “Never” =4 to “Very Often” =0 (Cohen et al., 1983). The summary score, which can range from 0 to 40, was evaluated as a continuous measure, with higher values reflecting greater perceived stress (Cronbach’s α = 0.81).
Resilience. The Brief Resilience Scale was used to assess psychological resilience. This scale has demonstrated internal consistency, criterion validity, construct validity, and test–retest reliability among university students and with cardiac and chronic pain patients (Smith et al., 2008). Response choices range from “Strongly Disagree” =1 to “Strongly Agree” =5 on items such as “I tend to bounce back quickly after hard times.” The coding of responses is reversed for items such as “I tend to take a long time to get over set-backs in my life.” The average of all responses was used as a continuous measure of resilience that ranged from 1 to 5, with higher values reflecting greater psychological resilience (Cronbach’s α = 0.78).
2.3. Statistical analyses
Means and standard deviations were calculated for continuous variables and counts and percentages were calculated for categorical variables. Missing values ranged from n = 2 (0.4%) for Perceived Stress Scale to 68 (13.7%) for ethnicity. Independent sample T-tests were used to assess the bivariate relationship of self-reported cardiometabolic health indicators with Perceived Stress Scale and Brief Resilience Scale scores. Multivariable logistic regression models were used to measure the association of health indicators with Perceived Stress Scale scores while adjusting for sociodemographic variables (age, gender, ethnicity, education level, marital status, and residence type). A quasi-Bayesian causal mediation analysis was then used to test whether Brief Resilience Scale scores served as a mediator between Perceived Stress Scale scores and each health indicator (Hicks and Tingley, 2011, Imai et al., 2010). All regression models adjusted for powwow event attended and used listwise deletion for incomplete cases. Two models were used for each of the cardiometabolic health indicators. The first model included the health indicator as the dependent variable, with demographic characteristics and Perceived Stress Scale score as the independent variables. The second model added the Brief Resilience Scale score as a mediating feature. A comparison of the coefficient derived from each model provided indirect evidence for mediation by the Brief Resilience Scale score. All statistical analyses were conducted in Stata/MP (version 15.0, StataCorp, College Station, Texas, 2016), with a significance level set at alpha = 0.05.
3. Results
Characteristics of the 496 respondents are shown for the overall study sample and by powwow event in Table 1. To preserve anonymity, powwows are identified by a number and not by event name. The overall mean age was 45.8 years and 64% of the study sample identified as female. The majority (83%) of participants were AI or AN only, with the remaining 17% identifying as AI or AN as well as one or more other racial categories. Characteristics of respondents varied by powwow. Due to variation in sociodemographic characteristics across powwows, all regression models adjusted for powwow event attended. On average, respondents rated their health as 3.2 (±1.0), which corresponds to a rating slightly above “Good.” Among all respondents, obesity was the most common cardiometabolic health indicator reported (48%), followed by high blood pressure (33%), prediabetes (22%), diabetes (21%), and high cholesterol (20%).
Table 1.
Sociodemographic characteristics and health status of participants.
| Powwow | ||||
|---|---|---|---|---|
| Characteristic | All participants (n = 496) | Powwow 1 (n = 180) | Powwow 2 (n = 210) | Powwow 3 (n = 106) |
| Age, years, mean (SD) | 45.8 (17.1) | 49.5 (17.9) | 45.1 (17.0) | 41.0 (14.6) |
| Gender, % (n) | ||||
| Female | 63.9 (3 1 7) | 70.6 (1 2 7) | 61.4 (1 2 9) | 57.6 (61) |
| Male or other1 | 36.1 (1 7 9) | 29.5 (53) | 38.7 (81) | 42.5 (45) |
| Race, “check all that apply,” % (n)2 | ||||
| American Indian | 88.9 (4 4 1) | 98.9 (1 7 8) | 76.2 (1 6 0) | 97.2 (1 0 3) |
| Alaska Native | 13.3 (66) | 1.7 (3) | 27.6 (58) | 4.7 (5) |
| Asian | 0.4 (2) | 0.0 (0) | 1.0 (2) | 0.0 (0) |
| Native Hawaiian or Pacific Islander | 2.0 (10) | 0.0 (0) | 3.3 (7) | 2.8 (3) |
| African American or Black | 2.2 (11) | 0.0 (0) | 4.8 (10) | 0.9 (1) |
| White | 11.1 (55) | 9.4 (17) | 13.8 (29) | 8.5 (9) |
| Other | 1.4 (7) | 0.6 (1) | 1.9 (4) | 1.9 (2) |
| Ethnicity, % (n) | ||||
| Latino/Latina or Hispanic | 8.6 (37) | 4.0 (6) | 13.4 (24) | 7.1 (7) |
| Not Latino/Latina or Hispanic | 91.4 (3 9 1) | 96.0 (1 4 4) | 86.6 (1 5 5) | 92.9 (92) |
| Education, % (n) | ||||
| No high school diploma or GED | 8.4 (41) | 8.0 (14) | 6.7 (14) | 12.3 (13) |
| High school graduate/GED | 21.6 (1 0 6) | 22.6 (40) | 21.7 (45) | 19.8 (21) |
| Some college but no degree | 24.3 (1 1 9) | 22.0 (39) | 22.7 (47) | 31.1 (33) |
| Technical/vocational degree or Associate’s degree | 19.8 (97) | 20.3 (36) | 22.2 (46) | 14.2 (15) |
| Bachelor’s or Graduate degree | 25.9 (1 2 7) | 27.2 (48) | 26.6 (55) | 22.7 (24) |
| Marital status, % (n) | ||||
| Married or living with partner | 48.6 (2 3 7) | 50.0 (86) | 43.8 (92) | 55.7 (59) |
| Widowed, divorced, or separated | 21.2 (1 0 3) | 27.3 (47) | 18.6 (39) | 16.0 (17) |
| Never married | 30.3 (1 4 8) | 22.7 (39) | 37.6 (79) | 28.3 (30) |
| Residence, % (n) | ||||
| Reservation or rural area | 30.3 (1 4 8) | 22.9 (40) | 23.8 (50) | 55.8 (58) |
| Small town | 20.7 (1 0 1) | 29.7 (52) | 16.2 (34) | 14.4 (15) |
| Large metropolitan area | 49.1 (2 4 0) | 47.4 (83) | 60.0 (1 2 6) | 29.8 (31) |
| Health status | ||||
| Self-rated health, 5-point scale, mean (SD) | 3.2 (1.0) | 3.3 (0.9) | 3.2 (1.0) | 3.1 (1.1) |
| Body mass index, mean (SD) | 31.0 (7.0) | 31.3 (6.6) | 30.4 (7.2) | 31.6 (7.3) |
| Obesity, % (n) | 48.2 (2 3 3) | 51.7 (89) | 43.4 (89) | 51.6 (55) |
| Prediabetes, % (n) | 21.8 (1 0 1) | 23.8 (38) | 19.8 (40) | 22.6 (23) |
| Diabetes, % (n) | 21.4 (1 0 1) | 28.1 (47) | 16.4 (33) | 20.2 (21) |
| High blood pressure, % (n) | 32.5 (1 5 7) | 43.4 (75) | 27.2 (56) | 25.0 (26) |
| High cholesterol, % (n) | 19.8 (94) | 27.1 (46) | 17.2 (35) | 12.8 (13) |
| Perceived stress, mean (SD) | 16.1 (6.4) | 14.6 (6.3) | 16.7 (6.3) | 17.2 (6.4) |
| Resilience, mean (SD) | 3.5 (0.7) | 3.6 (0.7) | 3.5 (0.8) | 3.4 (0.7) |
Note. Missing values for age (n = 8), ethnicity (n = 68), education (n = 6), marital status (n = 8), residence (n = 7), self-rated health (n = 6), height or weight to calculate BMI (n = 13), obesity (n = 13), diabetes (n = 24), high blood pressure (n = 13), high cholesterol (n = 20), prediabetes (n = 32), perceived stress (n = 2), and resilience (n = 5). 1 Includes responses of Transgender (n = 4) and Other (n = 6). 2 Categories were not mutually exclusive, so will exceed 100%
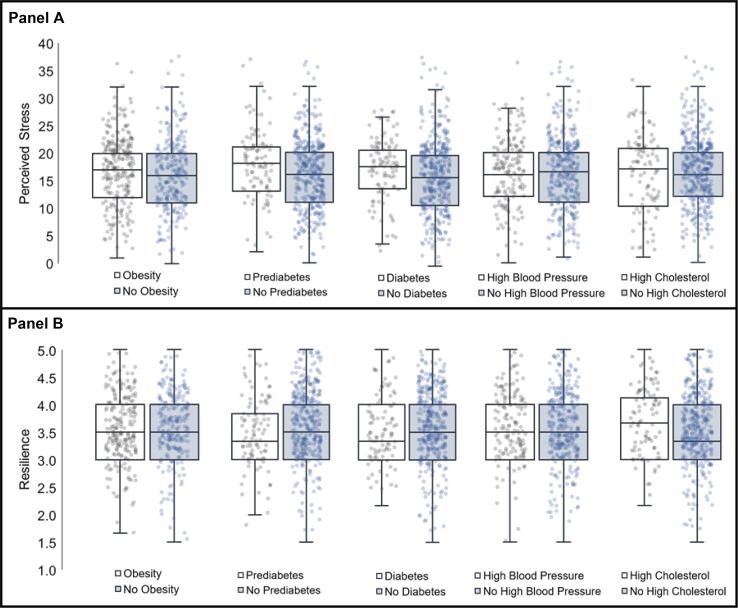
Mean Perceived Stress Scale scores were 16.1 (6.4 SD) among respondents, with scores ranging from 0 to 36. Average Perceived Stress Scale scores were significantly higher among respondents who self-reported prediabetes, compared to those without prediabetes (Fig. 1; Panel A; 17.6 vs. 15.6; P = 0.005). Perceived Stress Scale scores were not significantly associated with any other cardiometabolic health indicator. Mean Brief Resilience Scale scores were 3.5 (0.7 SD), with scores ranging from 1.5 to 5. Brief Resilience Scale scores were significantly lower among respondents who self-reported prediabetes compared to those without prediabetes (Fig. 1; Panel B; 3.4 vs. 3.6; P = 0.027). Brief Resilience Scale scores were not significantly related to any other cardiometabolic health indicator.
Fig. 1.
Association of Perceived Stress Scale and Brief Resilience Scale scores with self-reported cardiometabolic health indicators. Panel A: Dot and box plots comparing Perceived Stress Scale scores (Y-axes) for participants with (white) and without (blue) self-reported obesity, prediabetes, diabetes, high blood pressure, and high cholesterol in American Indian or Alaska Native participants. Independent group t-tests comparing Perceived Stress Scale scores between groups for obesity, prediabetes, diabetes, high blood pressure, and high cholesterol produced P-values of 0.205, 0.005, 0.128, 0.969, and 0.417, respectively. Panel B: Dot and box plots comparing Brief Resilience Scale scores (Y-axes) for participants with (white) and without (blue) self-reported obesity, prediabetes, diabetes, high blood pressure, and high cholesterol in American Indian or Alaska Native participants. Independent group t-tests comparing Brief Resilience Scale scores between groups for obesity, prediabetes, diabetes, high blood pressure, and high cholesterol produced P-values 0.722, 0.027, 0.742, 0.487, and 0.0647, respectively. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
In multivariable logistic regression models adjusting for powwow attended and sociodemographic characteristics (Table 2), greater Perceived Stress Scale scores were associated with increased likelihood of self-reported prediabetes (β = 0.07; 95% CI = 0.03, 0.11; P = 0.002) and diabetes (β = 0.05; 95% CI = 0.01, 0.10; P = 0.02). Models structured to test potential mediation by Brief Resilience Scale found that higher scores on the Perceived Stress Scale were significantly associated with lower scores on the Brief Resilience Scale (β = -0.07; 95% CI = -0.08, −0.06; P < 0.001), controlling for powwow attended and sociodemographic characteristics. In addition, higher Brief Resilience Scale scores were associated with high cholesterol (β = 0.68; 95% CI = 0.18, 1.18; P = 0.008), independent of Perceived Stress Scale scores or other model variables. The average mediation effect of Brief Resilience Scale scores on high cholesterol was −0.005 (95% CI = -0.010, −0.001). However, Brief Resilience Scale scores were not associated with any other cardiometabolic health indicators.
Table 2.
Association of Perceived Stress Scale and Brief Resilience Scale scores with cardiometabolic health indicators in multivariable logistic regression models.
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Coefficient | 95% CI | Coefficient | 95% CI | |
| Obesity | ||||
| Perceived stress | 0.02 | (−0.01, 0.06) | 0.04 | (−0.00, 0.08) |
| Resilience | – | – | 0.22 | (−0.13, 0.57) |
| Average mediation effect | – | – | −0.003 | (−0.009, 0.002) |
| Prediabetes | ||||
| Perceived stress | 0.07** | (0.03, 0.11) | 0.07** | (0.02, 0.12) |
| Resilience | – | – | −0.03 | (−0.47, 0.42) |
| Average mediation effect | – | – | 0.000 | (−0.002, 0.003) |
| Diabetes | ||||
| Perceived stress | 0.05* | (0.01, 0.10) | 0.07* | (0.01, 0.12) |
| Resilience | – | – | 0.23 | (−0.01, 0.12) |
| Average mediation effect | – | – | −0.001 | (−0.005, 0.001) |
| High blood pressure | ||||
| Perceived stress | 0.03 | (−0.01, 0.07) | 0.03 | (−0.02, 0.08) |
| Resilience | – | – | 0.09 | (−0.32, 0.50) |
| Average mediation effect | – | – | −0.001 | (−0.005, 0.003) |
| High cholesterol | ||||
| Perceived stress | 0.01 | (−0.04, 0.05) | 0.06 | (−0.00, 0.11) |
| Resilience | – | – | 0.68** | (0.18, 1.18) |
| Average mediation effect | – | – | −0.005 | (−0.010, −0.001) |
Note. Abbreviations include CI: Confidence Interval. Model 1 includes powwow attended, demographic characteristics (age, gender, ethnicity, education level, marital status, and residence type), and the Perceived Stress Scale. Model 2 includes all variables in Model 1 with the addition of score on the Brief Resilience Scale. P-values are denoted as * for < 0.05 and ** for < 0.01.
4. Discussion
The aim of this study was to evaluate the relationships of perceived stress with cardiometabolic health indicators, and to assess whether psychological resilience mediates these relationships. This line of research is important to understand mechanisms by which dramatic cardiometabolic health inequities among AI/AN people, including high prevalence of obesity, diabetes, and cardiovascular disease (Obesity and American Indians, 2017, Diabetes and American Indians, 2016, Office of Minority Health, 2017), continue to persist and inform the design of effective prevention efforts. In this convenience sample of AI/AN adults, greater perceived stress was associated only with prediabetes and diabetes. Resilience did not change or mediate this association. In addition, greater resilience was associated with high cholesterol, independent of stress, with a negligible estimated mediation effect. Which, may have been a chance finding.
The findings between stress and diabetes in the current study is consistent with results from Add Health (Marley and Metzger, 2015). Identifying latent drivers of diabetes among AI/AN adults, such as chronic stress and inflammation, may offer critical information towards novel public health and prevention opportunities. Diabetes is not only more prevalent among AI/AN adults than non-Hispanic white adults (Diabetes and American Indians, 2016), but treating diabetes consumes a substantial proportion of the IHS budget (O’Connell et al., 2012) and AI/AN adults with diabetes are more likely to experience comorbidities as well as die from diabetes (O'Connell et al., 2010). Perceived stress is associated with incidence of diabetes among Swedish men and Australian women in multi-year longitudinal studies (Novak et al., 2013, Harris et al., 2017). Results from this analysis suggest a cross-sectional relationship between perceived stress and both self-reported prediabetes and diabetes, but longitudinal studies will be needed to demonstrate the direction of this relationship among AI/AN adults. In contrast to prior literature suggesting relationships between perceived stress and BMI, blood pressure, or blood lipids in other population (Spruill et al., 2019, Tenk et al., 2018), no statistical relationships between perceived stress and these cardiometabolic health outcomes were identified in this analysis.
Several physiological or behavioral pathways may underpin the relationships of stress and resilience to prediabetes and diabetes, such as pro-inflammatory processes (Kivimäki and Steptoe, 2018) and overstimulation of the hypo-thalamic-pituitary adrenal axis (Farag et al., 2008). However, these constructs are often modeled as control variables (Richardson et al., 2012). One nascent area of study involves food insecurity (Nikolaus et al., 2019, Myers et al., 2020), namely, how insufficient access to nutritious food may be linked to stress, resilience, and health. Food insecurity likely both precipates stress and influences dietary patterns, but these relationships have not been explored in AI/AN adults. This avenue of research hold promise given that an estimated 25% of AI/AN-led households, nationwide, are food insecure (Jernigan et al., 2017).
Scores on the Perceived Stress Scale were greater than those reported for Non-Hispanic White respondents in three national probability surveys (Cohen and Janicki-Deverts, 2012), aligning with studies showing elevated Perceived Stress Scale scores among AI/AN young adults (Marley and Metzger, 2015). Scores on the Brief Resilience Scale were on average similar to those reported for undergraduate students from the general population (Smith et al., 2008). Prior studies of psychological resilience and health in AI/AN populations have been limited to AI/AN children and youth or small studies of AI adults (Cummins et al., 1999, Schure et al., 2013). Higher levels of resilience have been related to better self-reported physical health among AI/AN adolescents (Cummins et al., 1999) and older adults (Schure et al., 2013). In a small study of older AI/AN adults, greater resilience was associated with fewer symptoms of depression and lower levels of chronic pain (Schure et al., 2013). Among AI/AN adolescents, emotional health – which included components related to stress and resilience, such as optimism and worry – explained 16% of variation in self-reported physical health (Cummins et al., 1999). However, prior studies have not focused on the cardiometabolic health outcomes of interest in the current research. Thus, though present results support a relationship between Brief Resilience Scale scores and greater likelihood of high blood cholesterol, additional research on resilience and cardiometabolic health among AI/AN adults will be necessary to replicate these findings.
Of note, the Brief Resilience Scale may not capture a holistic impression of resilience in AI/AN populations. Qualitative investigations have suggested that resilience is conceptualized by some AI/AN adults at the community level (Shea et al., 2013, Grandbois and Sanders, 2012, Hobfoll et al., 2002) as well as the individual level, e.g., strong community resources and support in addition to a strong self-identity (Grandbois and Sanders, 2012). In a study with adolescents in California, resiliency was conceptualized based on family characteristics (Mistry et al., 2009). Assessing collective resilience (Teufel-Shone et al., 2018) at family or community levels, or with individual measures that include perceptions of social support (Albert, 2019), may be more informative in investigations of resiliency and health among AI/AN people. Though the Brief Resilience Scale had reasonable internal consistency in this study, this does not indicate content validity. Thus, future work with AI/AN adults in this area may be improved by re-envisioning the measurement of resiliency.
Unlike other investigations of stress and psychological resilience (Felix et al., 2019, Rod et al., 2009), the present study did not find an association of stress with obesity, high blood pressure, or high cholesterol. Psychological resilience did not mediate the relationship between stress and cardiometabolic health, which contradicts previous evidence (Lehrer et al., 2020), possibly due to the current study’s reliance on dichotomized, self-reported health measures. There also was no measure of physical activity included in this study, which has been postulated to mediate the link between stress and health among AI/AN people in some (Bersamin et al., 2014) but not all studies (Grant et al., 2018). Further, use of a modest size convenience sample may have increased Type II error and reduced power to detect existing relationships. The sampling strategy also limits generalizability of the results. Finally, cross-sectional designs cannot elucidate temporality of associations and may have resulted in biased estimates of mediation effects (Fairchild and McDaniel, 2017). Longitudinal analyses would provide a natural advantage for this line of inquiry.
4.1. Conclusion
Future studies of stress and resilience among AI/AN people may yield more robust results by characterizing health conditions using continuous and proximal biological measures, applying longitudinal study designs, as well as more detailed, and culturally informed measures of stress and resilience. Such investigations will provide valuable information as to how the constructs of stress and resilience might be integrated into efforts to prevent or improve cardiometabolic health in AI/AN households and communities. Though there is need for additional research, the high prevalence of cardiometabolic health concerns and elevated average stress levels among respondents in the current study mirrors what has been reported for the larger AI/AN adult population. Therefore, continued efforts by community and clinical organizations to prevent and treat diet-related cardiometabolic conditions among AI/AN people are well warranted.
CRediT authorship contribution statement
Cassandra Nikolaus: Conceptualization, Methodology, Formal analysis, Writing – original draft. Ka’imi Sinclair: Investigation, Resources, Project administration. Dedra Buchwald: Writing - review & editing, Funding acquisition. Astrid Suchy-Dicey: Conceptualization, Methodology, Writing - review & editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Albert M.A. Ignored in Plain Sight. Circ Cardiovasc Qual Outcomes. 2019;12(4) doi: 10.1161/CIRCOUTCOMES.119.005647. [DOI] [PubMed] [Google Scholar]
- American Psychological Association Stress in America: The impact of discrimination. Stress Am.TM Survey. 2016 [Google Scholar]
- Bersamin A., Wolsko C., Luick B.R., Boyer B.B., Lardon C., Hopkins S.E., Stern J.S., Zidenberg-Cherr S. Enculturation, perceived stress, and physical activity: implications for metabolic risk among the Yup’ik–the Center for Alaska Native Health Research Study. Ethn Health. 2014;19(3):255–269. doi: 10.1080/13557858.2012.758691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cal SF, S LRd, Glustak ME, Santiago MB, Walla P. Resilience in chronic diseases: A systematic review. Cogent Psychology. 2015;2(1).
- Cohen S., Janicki-Deverts D. Who's Stressed? Distributions of Psychological Stress in the United States in Probability Samples from 1983, 2006, and 20091. J. Appl. Soc. Psychol. 2012;42(6):1320–1334. [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A Global Measure of Perceived Stress. J. Health Soc. Behav. 1983;24(4) [PubMed] [Google Scholar]
- Connor K.M., Davidson J.R.T. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- Cummins J.R., Ireland M., Resnick M.D., Blum R.W. Correlates of physical and emotional health among Native American adolescents. J. Adolesc. Health. 1999;24(1):38–44. doi: 10.1016/s1054-139x(98)00063-9. [DOI] [PubMed] [Google Scholar]
- Diabetes and American Indians/Alaska Natives. 2016 https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlID=33 [Google Scholar]
- Elm JHL, Walls ML, Aronson BD. Sources of Stress Among Midwest American Indian Adults with Type 2 Diabetes. Am. Indian Alsk Native Ment. Health Res. 2019, 26(1):33-62. [DOI] [PMC free article] [PubMed]
- Fairchild A.J., McDaniel H.L. Best (but oft-forgotten) practices: mediation analysis. The American Journal of Clinical Nutrition. 2017 doi: 10.3945/ajcn.117.152546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farag N.H., Moore W.E., Lovallo W.R., Mills P.J., Khandrika S., Eichner J.E. Hypothalamic-pituitary-adrenal axis function: relative contributions of perceived stress and obesity in women. J Womens Health (Larchmt). 2008;17(10):1647–1655. doi: 10.1089/jwh.2008.0866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Felix A.S., Lehman A., Nolan T.S. Stress, Resilience, and Cardiovascular Disease Risk Among Black Women. Circ Cardiovasc Qual Outcomes. 2019;12(4) doi: 10.1161/CIRCOUTCOMES.118.005284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandbois D.M., Sanders G.F. Resilience and stereotyping: the experiences of Native American elders. J. Transcult. Nurs. 2012;23(4):389–396. doi: 10.1177/1043659612451614. [DOI] [PubMed] [Google Scholar]
- Grant V.M., Tomayko E.J., Prince R.J., Cronin K., Adams A. Understanding Correlates of Physical Activity in American Indian Families: The Healthy Children Strong Families-2 Study. J Phys Act Health. 2018;15(11):866–873. doi: 10.1123/jpah.2017-0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris M.L., Oldmeadow C., Hure A., Luu J., Loxton D., Attia J. Stress increases the risk of type 2 diabetes onset in women: A 12-year longitudinal study using causal modelling. PLoS ONE. 2017;12(2) doi: 10.1371/journal.pone.0172126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks R., Tingley D. Causal Mediation Analysis. Stata J. Promoting Commun. Statist. Stata. 2011;11(4):605–619. [Google Scholar]
- Hobfoll S.E., Jackson A., Hobfoll I., Pierce C.A., Young S. The impact of communal-mastery versus self-mastery on emotional outcomes during stressful conditions: a prospective study of Native American women. Am. J. Community Psychol. 2002;30(6):853–871. doi: 10.1023/A:1020209220214. [DOI] [PubMed] [Google Scholar]
- Imai K., Keele L., Tingley D. A general approach to causal mediation analysis. Psychol. Methods. 2010;15(4):309–334. doi: 10.1037/a0020761. [DOI] [PubMed] [Google Scholar]
- Jernigan V.B.B., Huyser K.R., Valdes J., Simonds V.W. Food Insecurity among American Indians and Alaska Natives: A National Profile using the Current Population Survey-Food Security Supplement. J Hunger Environ Nutr. 2017;12(1):1–10. doi: 10.1080/19320248.2016.1227750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karatsoreos I.N., McEwen B.S. Annual Research Review: The neurobiology and physiology of resilience and adaptation across the life course. J. Child Psychol. Psychiatry. 2013;54(4):337–347. doi: 10.1111/jcpp.12054. [DOI] [PubMed] [Google Scholar]
- Kivimäki M., Steptoe A. Effects of stress on the development and progression of cardiovascular disease. Nat. Rev. Cardiol. 2018;15(4):215–229. doi: 10.1038/nrcardio.2017.189. [DOI] [PubMed] [Google Scholar]
- Lee E.-H. Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res (Korean Soc Nurs Sci). 2012;6(4):121–127. doi: 10.1016/j.anr.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Lehrer H.M., Steinhardt M.A., Dubois S.K., Laudenslager M.L. Perceived stress, psychological resilience, hair cortisol concentration, and metabolic syndrome severity: A moderated mediation model. Psychoneuroendocrinology. 2020;113:104510. doi: 10.1016/j.psyneuen.2019.104510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marley T.L., Metzger M.W. A longitudinal study of structural risk factors for obesity and diabetes among American Indian young adults, 1994–2008. Prev Chronic Dis. 2015;12:E69. doi: 10.5888/pcd12.140469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mistry R., McCarthy W.J., Yancey A.K., Lu Y., Patel M. Resilience and patterns of health risk behaviors in California adolescents. Prev. Med. 2009;48(3):291–297. doi: 10.1016/j.ypmed.2008.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers C.A., Beyl R.A., Martin C.K., Broyles S.T., Katzmarzyk P.T. Psychological mechanisms associated with food security status and BMI in adults: a mixed methods study. Public Health Nutr. 2020;23(14):2501–2511. doi: 10.1017/S1368980020000889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikolaus C.J., Schierer M., Ellison B., Eicher-Miller H.A., Gundersen C., Nickols-Richardson S.M. Grit is Associated with Food Security among US Parents and Adolescents. Am J Health Behav. 2019;43(1):207–218. doi: 10.5993/AJHB.43.1.17. [DOI] [PubMed] [Google Scholar]
- Novak M., Bjorck L., Giang K.W., Heden-Stahl C., Wilhelmsen L., Rosengren A. Perceived stress and incidence of Type 2 diabetes: a 35-year follow-up study of middle-aged Swedish men. Diabet. Med. 2013;30(1):e8–16. doi: 10.1111/dme.12037. [DOI] [PubMed] [Google Scholar]
- Obesity and American Indians/Alaska Natives. 2017 https://minorityhealth.hhs.gov/omh/content.aspx?lvl=3&lvlID=62&ID=6457 [Google Scholar]
- O’Connell J.M., Wilson C., Manson S.M., Acton K.J. The costs of treating American Indian adults with diabetes within the Indian Health Service. Am. J. Public Health. 2012;102(2):301–308. doi: 10.2105/AJPH.2011.300332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Connell J., Yi R., Wilson C., Manson S.M., Acton K.J. Racial disparities in health status: a comparison of the morbidity among American Indian and U.S. adults with diabetes. Diabetes Care. 2010;33(7):1463–1470. doi: 10.2337/dc09-1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Office of Minority Health. Heart Disease and American Indians/Alaska Natives. 2017; https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=34.
- Office of Minority Health. Profile: American Indian/Alaska Native. 2018; https://www.minorityhealth.hhs.gov/omh/browse.aspx?lvl=3&lvlid=62.
- Ore C.E., Teufel-Shone N.I., Chico-Jarillo T.M. American Indian and Alaska Native resilience along the life course and across generations: A literature review. Am. Indian Alsk. Native Ment. Health Res. 2016;23(3):134–157. doi: 10.5820/aian.2303.2016.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richardson S., Shaffer J.A., Falzon L., Krupka D., Davidson K.W., Edmondson D. Meta-analysis of perceived stress and its association with incident coronary heart disease. Am. J. Cardiol. 2012;110(12):1711–1716. doi: 10.1016/j.amjcard.2012.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rod N.H., Gronbaek M., Schnohr P., Prescott E., Kristensen T.S. Perceived stress as a risk factor for changes in health behaviour and cardiac risk profile: a longitudinal study. J. Intern. Med. 2009;266(5):467–475. doi: 10.1111/j.1365-2796.2009.02124.x. [DOI] [PubMed] [Google Scholar]
- Sarche M, Spicer P. Poverty and health disparities for American Indian and Alaska Native children: current knowledge and future prospects. Ann. N Y Acad. Sci. 2008, 1136, 126-136. [DOI] [PMC free article] [PubMed]
- Schure M.B., Odden M., Goins R.T. The association of resilience with mental and physical health among older American Indians: the Native Elder Care Study. Am. Indian Alsk. Native Ment. Health Res. 2013;20(2):27–41. doi: 10.5820/aian.2002.2013.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shea J.M., Poudrier J., Chad K., Jeffery B., Thomas R., Burnouf K. In their own words: First Nations girls' resilience as reflected through their understandings of health. Pimatisiwin: A Journal of Aboriginal & Indigenous. Community Health. 2013;11(1) [Google Scholar]
- Smith B.W., Dalen J., Wiggins K., Tooley E., Christopher P., Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- Southwick S.M., Bonanno G.A., Masten A.S., Panter-Brick C., Yehuda R. Resilience definitions, theory, and challenges: interdisciplinary perspectives. Eur J Psychotraumatol. 2014;5 doi: 10.3402/ejpt.v5.25338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spruill T.M., Butler M.J., Thomas S.J. Association Between High Perceived Stress Over Time and Incident Hypertension in Black Adults: Findings From the Jackson Heart Study. J Am Heart Assoc. 2019;8(21) doi: 10.1161/JAHA.119.012139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tenk J., Mátrai P., Hegyi P., Rostás I., Garami A., Szabó I., Hartmann P., Pétervári E., Czopf L., Hussain A., Simon M., Szujó S., Balaskó M. Perceived stress correlates with visceral obesity and lipid parameters of the metabolic syndrome: A systematic review and meta-analysis. Psychoneuroendocrinology. 2018;95:63–73. doi: 10.1016/j.psyneuen.2018.05.014. [DOI] [PubMed] [Google Scholar]
- Teufel-Shone N.I., Tippens J.A., McCrary H.C., Ehiri J.E., Sanderson P.R. Resilience in American Indian and Alaska Native Public Health: An Underexplored Framework. Am J Health Promot. 2018;32(2):274–281. doi: 10.1177/0890117116664708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toukhsati S.R., Jovanovic A., Dehghani S., Tran T., Tran A., Hare D.L. Low psychological resilience is associated with depression in patients with cardiovascular disease. Eur J Cardiovasc Nurs. 2017;16(1):64–69. doi: 10.1177/1474515116640412. [DOI] [PubMed] [Google Scholar]