Abstract
The Hierarchical Taxonomy of Psychopathology (HiTOP) is an empirical, dimensional model of psychological symptoms and functioning. Its goals are to augment the use and address the limitations of traditional diagnoses, such as arbitrary thresholds of severity, within-disorder heterogeneity, and low reliability. HiTOP has made inroads to addressing these problems, but its prognostic validity is uncertain. The present study sought to test the prediction of long-term outcomes in psychotic disorders was improved when the HiTOP dimensional approach was considered along with traditional (ie, DSM) diagnoses. We analyzed data from the Suffolk County Mental Health Project (N = 316), an epidemiologic study of a first-admission psychosis cohort followed for 20 years. We compared 5 diagnostic groups (schizophrenia/schizoaffective, bipolar disorder with psychosis, major depressive disorder with psychosis, substance-induced psychosis, and other psychoses) and 5 dimensions derived from the HiTOP thought disorder spectrum (reality distortion, disorganization, inexpressivity, avolition, and functional impairment). Both nosologies predicted a significant amount of variance in most outcomes. However, except for cognitive functioning, HiTOP showed consistently greater predictive power across outcomes—it explained 1.7-fold more variance than diagnoses in psychiatric and physical health outcomes, 2.1-fold more variance in community functioning, and 3.4-fold more variance in neural responses. Even when controlling for diagnosis, HiTOP dimensions incrementally predicted almost all outcomes. These findings support a shift away from the exclusive use of categorical diagnoses and toward the incorporation of HiTOP dimensions for better prognostication and linkage with neurobiology.
Keywords: nosology, DSM, schizophrenia, psychotic disorders, thought disorder, classification
Introduction
Traditional diagnostic taxonomies, such as those put forth in the Diagnostic and Statistical Manual (DSM)1 and International Classification of Diseases,2 have enabled advances in psychiatry, providing a common language for researchers, clinicians, and policymakers (eg, ref.3). However, diagnoses defined in these traditional taxonomies have some limitations. First, many are heterogeneous.4,5 For example, 2 individuals with a schizophrenia diagnosis can have completely non-overlapping symptom profiles. Associations with symptom dimensions are obscured in analyses of the diagnostic category.6,7 Second, data consistently indicate that psychotic disorders lie on a continuum from healthy cognitive processes to frank psychosis. Discrete boundaries of categorical diagnoses are arbitrary.8–10 Third, owing to arbitrary boundaries, the reliabilities of psychotic disorder diagnoses are only modest,11,12 limiting their informativeness.
The Hierarchical Taxonomy of Psychopathology (HiTOP) was developed to address these limitations.13 The aim of HiTOP is to systematize and facilitate clinical evaluation by taking what clinicians are doing already and helping to make it most effective. Drawing on the long history of efforts to identify symptom dimensions,14–16 HiTOP is a fully empirical, quantitative nosology. The model includes 6-dimensional spectra, identified through statistical modeling of associations among symptoms and traits. Psychotic disorders fall on the thought disorder spectrum, which is comprised of reality distortion (hallucinations and delusions), disorganization (formal thought disorder and bizarre behavior), inexpressivity (blunted facial expressions and alogia), and avolition (apathy and asociality).13,17–19 Functional impairment cuts across these symptom dimensions and is assessed separately.20
The HiTOP model of psychotic disorders offers a number of advantages. First, it decomposes heterogeneous diagnoses into the component dimensions listed above. Second, patients can be reliably rated along these dimensions.18,19 Third, this approach recognizes the continuum between normality, schizotypy, and psychotic disorders.21,22 Fourth, DSM diagnostic criteria conflate symptoms and their functional consequences, whereas HiTOP characterizes these separately. This allows for the characterization of symptoms independent of impairment, which is important in tracking illness course and treatment response.20,23,24
Nevertheless, a clinically useful nosology needs to demonstrate prognostic validity. Prognostic validity was a major benchmark in neo-Kraepelinian movement that led to DSM-III. In particular, Robin and Guze25 spotlight validation by follow-up studies, and Goodwin and Guze26 went as far as to say “diagnosis is prognosis.” Currently, the prognostic validity of HiTOP is unclear, as few investigations directly compared it to the DSM. In one study, symptom dimensions of people with psychotic experiences explained more variance than diagnoses in service use, behavior requiring arrest or involuntary hospitalization, and occupational and social functioning.27 HiTOP has also been shown to be more closely aligned with neurobiological characteristics. An investigation of patients with psychosis reported that neurobiological subtypes, derived from multiple indicators of brain functioning, align much more closely with symptom dimensions than with diagnoses.5 Although these studies suggest that HiTOP may provide a useful description of psychotic disorders, both were cross-sectional, and thus HiTOP’s prognostic validity remains unknown.
The current study attempted to test whether the addition of the HiTOP dimensions to DSM diagnoses aided in the predictive power in an epidemiologic sample of psychotic disorders ascertained at first admission and followed for 20 years. We sought to extend prior research by considering a wide range of outcomes, including illness remission and recovery, aspects of community functioning, physical health, cognitive performance, and neural functioning, all of which are important for evaluating the validity of a diagnostic system.28 We hypothesized that, as in prior research,5,27 HiTOP would have greater predictive power than DSM, indicating that dimensions can augment categorical diagnoses in the prediction of outcomes.
Methods
Participants
Data were drawn from the Suffolk County Mental Health Project, a longitudinal study of first-admission psychosis.11,29,30 Between 1989 and 1995, individuals were recruited from the 12 inpatient facilities in Suffolk County, New York (response rate 72%). The Stony Brook University Committee on Research Involving Human Subjects and review boards of participating hospitals approved the protocol annually. Written consent was obtained from all study participants. For those who were minors at baseline, child’s assent and parental permission were obtained. Eligibility criteria included residence in Suffolk County, age between 15 and 60, ability to speak English, IQ > 70, first admission within the past 6 months, current psychosis, and no apparent medical etiology for psychotic symptoms.
Altogether, 628 participants met inclusion criteria. Follow-up interviews were conducted at multiple points, including 6 months and 20 years after baseline admission. Predictors in these analyses are based on data obtained at the 6-month point, as diagnosis of schizophrenia requires 6 months of illness. Of the 469 patients who completed the 6-month follow-up, 316 were reassessed at Year 20 and constitute the analysis sample. Others were not assessed because 50 died, 47 were lost to follow-up, and 56 refused. Table 1 contains demographic information and descriptive statistics for all the measures used in the current study.
Table 1.
Descriptive Information on all Measures
| Year 20 Completers (n = 316) | Year 20 Non-completers (n = 153) | P-value for Mean Comparisons | |
|---|---|---|---|
| Mean (SD) or % | Mean (SD) or % | ||
| Demographics | |||
| Women | 39% | 45% | .20 |
| Age at 6-mo wave (y) | 28.80 (8.99) | 31.95 (9.99) | <.05 |
| White | 83% | 70% | .02 |
| Diagnostic measures at 6 mo | |||
| HiTOP dimensions | |||
| SAPS Reality Distortion | 2.77 (5.76) | 3.44 (6.91) | .26 |
| SAPS Disorganization | 2.13 (4.01) | 2.16 (3.41) | .95 |
| SANS Avolition | 8.74 (7.68) | 10.06 (7.69) | .08 |
| SANS Inexpressivity | 6.78 (8.11) | 6.90 (8.21) | .88 |
| QLS Global Functioning | 2.70 (1.21) | 2.47 (1.17) | .06 |
| DSM-IV Diagnoses | |||
| Schizophrenia | 35% | 36% | .91 |
| Bipolar disorder with psychotic features | 28% | 25% | .53 |
| Major depressive disorder with psychotic features | 18% | 20% | .71 |
| Substance-induced psychosis | 7% | 9% | .32 |
| Other psychoses | 12% | 10% | .56 |
| Outcomes at 20 years | Mean (SD) or % | ||
| Psychiatric outcomes | |||
| Recovery | 46% | ||
| Full Symptom Remission | 29% | ||
| Community functioning | |||
| Educational attainment (any college) | 40% | ||
| Employed | 55% | ||
| Public assistance | 63% | ||
| Role functioning | 2.55 (1.14) | ||
| Living independently over the interval | 0.95 (0.68) | ||
| Social functioning | 10.25 (4.49) | ||
| WHO-DAS Global Disability | 22.06 (8.70) | ||
| Physical health | |||
| Diabetes | 21% | ||
| Hypertension | 30% | ||
| Neural responses | |||
| MMN duration (μV) | −1.60 (1.85) | ||
| MMN frequency (μV) | −1.75 (1.43) | ||
| P3a amplitude (μV) | 8.54 (5.15) | ||
| P3a latency (ms) | 390.49 (61.33) | ||
| Cognitive functioning | |||
| Composite score | −11.55 (73.78) |
Note: SAPS, Scale for the Assessment of Positive Symptoms; SANS, Scale for the Assessment of Negative Symptoms; QLS, Quality of Life Scale; WHO-DAS, World Health Organization Disability Assessment Schedule; MMN, mismatched negativity.
Predictors
Diagnoses
DSM-IV diagnoses were made by the consensus of study psychiatrists at the 6-month follow-up using all information accumulated over time: Structured Clinical Interview Diagnostic (SCID)31 interviews with participants, interviews with participants’ significant others, medical records, and behavioral ratings by masters-level interviewers, as described in Bromet et al.11 Diagnoses were grouped into 5 categories to ensure adequate sizes within each category: schizophrenia/schizoaffective/schizophreniform disorders, bipolar disorder with psychotic features, major depressive disorder with psychotic features, substance-induced psychosis, and other psychoses (brief reactive psychosis, delusional disorder, and psychosis NOS) (Bipolar disorder with psychosis, major depressive disorder with psychosis, and substance-induced psychosis were each an individual DSM-IV diagnosis. The schizophrenia group was comprised of individuals with either a schizophrenia (N = 75), schizoaffective bipolar type (N = 14), schizoaffective depressed (N = 13), or schizophreniform diagnosis (N = 9). The former groups are small and challenging to analyze independently. Fortunately, previous research on this sample found that these groups are quite similar with regard to outcomes and combining them does not increase heterogeneity vis-à-vis prognosis.32 Finally, the other psychoses group has substantial heterogeneity. Subdivision of this group into individual diagnoses would render them unfit for analyses due to small sizes. However, previous work in this cohort found that these 5 categories offer an effective representation of psychotic disorder diagnoses.11,24).
HiTOP Dimensions
Consistent with the HiTOP model, symptoms and functional consequences were rated separately. For equivalence with diagnoses, we focused on 5 dimensions that comprise the thought disorder spectrum and its consequences. These HiTOP dimensions can be measured by widely available scales.13,33 In the current study, 4 dimensions—reality distortion, disorganization, inexpressivity, and avolition—were derived by a factor analysis of the Scale for the Assessment of Positive Symptoms (SAPS)34 and Scale for the Assessment of Negative Symptoms (SANS).35 As detailed in Kotov et al,18 rather than using global ratings scores from the SAPS and SANS, individual items were used as a pool of symptoms to derive these empirical dimensions from an exploratory factor analysis. We compared the reliability and validity of resulting factor solutions. A 4-factor model showed high reliability and validity, and more complex models did not improve on it. These 4 dimensions were replicable in 5 waves of data, internally consistent, stable across assessments, and showed strong discriminant validity. The fifth dimension, functional impairment, was assessed by the global rating of the Quality of Life scale (QLS), a semi-structured interview.36 This item summarizes all data gathered in the interview and captures adjustment in work and relationships based on participant’s education and social background. It is rated from 1 (markedly impaired) to 5 (very good).
Outcomes
Psychiatric Outcomes
These included recovery and full symptom remission. Recovery status at the 20-year follow-up was defined according to the criteria of Liberman and colleagues,37 which included ratings of 4 or less on multiple items from the Brief Psychiatric Rating Scale38 as well as ratings of 2 or more on items assessing occupational and social functioning from the QLS.36 Remission status at the 20-year follow-up was defined according to Andreasen and colleagues’ criteria,39 in which ratings of mild or less on all global items of the SAPS and SANS are considered evidence of remission.
Community Functioning
This category of outcomes included educational attainment, employment, role functioning, residential independence, use of public assistance, social functioning, and global disability at the 20-year follow-up. We operationalized educational attainment as any college, and employment as full- or part-time paid work or school. Role functioning was assessed with the QLS level of accomplishment item, which is a rating of participants’ performance in their roles during the past month. This rating is made on a scale from 0 (attempted no rule functioning) to 6 (very good functioning). Residential independence was rated for the 20-year interval as 0 = participant never lived independently (ie, lived with relatives or in institutional settings), 1 = sometime lived independently, and 2 = always lived independently (ie, in participant’s own household). Use of public assistance was coded from sources of income as 0 = no and 1 = yes (eg, SSI, SSD, welfare, rent supplements, and food stamps). Social functioning was quantified through a composite of 3 interpersonal relations items from the QLS: social activity, sociosexual relations, and relationships with friends. The composite score ranged from 1 (worst functioning) to 17 (best).40 Global disability was assessed with the 12-item self-report version of the World Health Organization Disability Assessment Schedule 2.0 (WHO-DAS) measuring basic physical, psychological, and social functions, with a total score ranging from 0 (no difficulty with any function assessed) to 100 (extreme difficulty/cannot do any function assessed).41
Physical Health
We focused on 2 conditions that are particularly prevalent in psychotic disorders: diabetes and hypertension.42,43 Participants were interviewed about diagnosis and treatment of these disorders. Self-report was corroborated by medical records where available.
Neural Functioning
Neural functioning was assessed using event-related potential components that show consistent, robust abnormalities in psychotic disorders: mismatch negativity (MMN)44 and auditory P3a.45 Both of these components are passive measures of neural functioning as oppose to more conscious, volitional measures related to task performance (eg, P3b).46 We focused on ERP outcomes because of the clear practical and methodological advantages over other neural measures (eg, less expensive than MRI; less invasive than PET47) as well as potential statistical benefits, such as increased statistical power and high reliability.48
To elicit duration and frequency MMN, participants heard tones while completing a picture-word matching task (see Donaldson et al49 for task and processing details). To elicit the auditory P3a, participants completed an auditory 3-stimulus oddball task, and amplitude and latency was calculated for each (see Perlman et al50 for task and processing details) (Although Perlman and colleagues used P3 amplitudes derived from temporal-spatial principal components analysis, we used standard amplitudes in the current analysis.).
Cognitive Functioning
The neuropsychological battery at the 20 year follow-up included the Controlled Oral Word Association Test,51 Verbal Paired Associates and Visual Reconstruction from the Wechsler Memory Scale-Revised (immediate and delay trials from both scales),52 Symbol-Digit Modalities, Letter-Number Sequencing, and Vocabulary from the Wechsler Adult Intelligence Scale-R,53 Trails A and B,54 and the Stroop Test.55 Given the strong relationship among several of these measures, we computed a composite score consistent with prior research56 using a similar procedure as reported in Jonas et al.57 We first removed redundancies and then conducted an exploratory factor analysis. Trait estimates from the first unrotated factor were used as a composite factor score.
Attrition
As can be seen in table 1, individuals with data at the 20-year follow-up were younger and more likely to identify as White. At the 20-year follow-up, some participants were interviewed in their homes or over the phone. For these individuals, data on neural and neuropsychological function were not obtained. As a result, sample sizes for these outcomes are smaller than those of psychiatric outcomes, community functioning, and physical health.
Data Analysis
First, we examined associations of the 5 DSM diagnostic categories and 5 HiTOP dimensions with outcomes. Next, we fit 2 hierarchical regression model for each outcome. The 5 HiTOP dimensions entered as a block in Step 1, and DSM diagnoses entered as a block in Step 2 (Four, instead of 5, dummy coded variables were entered into the regressions because the fifth was perfectly collinear with the rest.). Then, the order of blocks was reversed. Logistic regression was used for dichotomous outcomes, and linear regression was used for continuous outcomes. These analyses assessed the predictive power of each nosology (R2 of Step 1) and incremental validity over the other nosology (ΔR2 of Step 2).
Results
Associations Among Individual Dimensions, Diagnoses, and Outcomes
Table 2 reports the zero-order correlations for diagnoses and dimensions with outcomes (see supplementary table 1 for correlations among outcomes). Sixth-month diagnoses and dimensions were correlated, but not so strongly as to be redundant. Specifically, a diagnosis of schizophrenia was associated with elevations on all symptom scales, and low functioning. The bipolar group showed the opposite pattern, and the other diagnostic groups were near the sample mean on all dimensions. For the majority of outcomes, all 5 HiTOP dimensions showed significant effects in the same direction as diagnosis. In contrast, the associations of diagnoses were largely limited to schizophrenia and bipolar disorder, with worse outcomes in the former and better outcomes in the latter. Several 20-year outcomes showed a more specific pattern: hypertension was predicted only by reality distortion and disorganization, greater P3a amplitude by lower avolition and better functioning, and longer P3a latency by avolition.
Table 2.
Zero-Order Correlations Between HiTOP Measures, Diagnoses, and Outcome Measures
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. SAPS Reality Distortion | ||||||||||
| 2. SAPS Disorganization | 0.45*** | |||||||||
| 3. SANS Avolition | 0.25*** | 0.26*** | ||||||||
| 4. SANS Inexpressivity | 0.18** | 0.17** | 0.52*** | |||||||
| 5. QLS Global Functioning | −0.37*** | −0.29*** | −0.72*** | −0.49*** | ||||||
| 6. Schizophrenia | 0.27*** | 0.13* | 0.27*** | 0.38*** | −0.29*** | |||||
| 7. BD-P | −0.20*** | −0.02 | −0.26*** | −0.29*** | 0.32*** | −0.46*** | ||||
| 8. MDD-P | −0.09 | −0.13* | −0.05 | −0.10 | 0.03 | −0.35*** | −0.30*** | |||
| 9. SI psychosis | −0.01 | −0.05 | 0.02 | −0.01 | 0.01 | −0.20*** | −0.17** | −0.13* | ||
| 10. Other psychoses | −0.01 | 0.02 | 0.01 | −0.02 | −0.06 | −0.27*** | −0.23*** | −0.17** | -0.10 | |
| 11. Recovery | −0.23*** | −0.18** | −0.43*** | −0.26*** | 0.42*** | −0.27*** | 0.27*** | 0.09 | −0.09 | −0.02 |
| 12. Full symptom remission | −0.15* | −0.17** | −0.34*** | −0.38*** | 0.35*** | −0.37*** | 0.28*** | 0.20** | −0.07 | −0.01 |
| 13. Educational attainment | −0.10 | −0.08 | −0.24*** | −0.18** | 0.26*** | −0.05 | 0.19** | −0.04 | −0.07 | −0.09 |
| 14. Employed | −0.21*** | −0.15** | −0.30*** | −0.26*** | 0.34*** | −0.16** | 0.25*** | −0.05 | −0.01 | −0.03 |
| 15. Public assistance | 0.22*** | 0.15** | 0.33*** | 0.31*** | −0.37*** | 0.26*** | −0.25*** | −0.04 | −0.02 | 0.03 |
| 16. Role functioning | −0.22*** | −0.19** | −0.43*** | −0.32*** | 0.42*** | −0.26*** | 0.25*** | 0.14* | −0.05 | −0.08 |
| 17. Living independently | −0.18** | −0.12* | −0.20*** | −0.27*** | 0.28*** | −0.30*** | 0.20*** | 0.13* | 0.00 | 0.00 |
| 18. Social functioning | −0.14* | −0.17** | −0.47*** | −0.30*** | 0.41*** | −0.17** | 0.21*** | 0.06 | −0.08 | −0.06 |
| 19. WHO-DAS Global Disability | 0.21** | 0.15* | 0.37*** | 0.15* | −0.30*** | 0.08 | −0.24*** | 0.11 | 0.13* | 0.00 |
| 20. Diabetes | 0.14* | 0.06 | 0.23*** | 0.10** | −0.20*** | 0.11** | −0.16** | 0.01 | 0.05 | 0.00 |
| 21. Hypertension | 0.13* | 0.14* | 0.10 | 0.05 | −0.08 | 0.01 | −0.02 | 0.08 | −0.05 | −0.05 |
| 22. MMN duration | 0.21** | 0.12 | 0.15* | 0.15* | −0.11 | 0.13** | −0.03 | −0.01 | −0.01 | −0.14** |
| 23. MMN frequency | 0.04 | −0.04 | 0.01 | 0.10 | −0.02 | 0.00 | 0.01 | −0.01 | 0.06 | −0.05 |
| 24. P3a amplitude | −0.02 | −0.04 | −0.14** | 0.01 | 0.21** | −0.06 | −0.01 | 0.09 | 0.00 | 0.01 |
| 25. P3a latency | 0.03 | 0.04 | 0.14* | −0.04 | −0.01 | −0.09 | 0.08 | 0.06 | −0.08 | 0.02 |
| 26. Cognition composite | −0.19* | −0.15* | −0.24** | −0.34*** | 0.29*** | −0.23** | 0.37*** | −0.06 | 0.08 | −0.17* |
Note: SAPS, Scale for the Assessment of Positive Symptoms; SANS, Scale for the Assessment of Negative Symptoms; QLS, Quality of Life Scale; BD-P, Bipolar disorder with psychotic features; MDD-P, Major depressive disorder with psychotic features; SI psychosis, Substance-induced psychosis; WHO-DAS, World Health Organization Disability Assessment Schedule; MMN, Mismatched negativity.
*P < .05, **P < .01, *** P< .001.
Direct Comparison of Predictive Power Between HiTOP Dimensions and DSM Diagnoses
Table 3 (Step 1) shows predictive power of HiTOP dimensions together and DSM diagnoses together. Both HiTOP and DSM explained a significant amount of variance in most outcomes. However, only HiTOP predicted diabetes and neural responses. HiTOP showed consistently higher predictive power across outcomes, except for the prediction of cognitive functioning. It explained 1.7-fold more variance than DSM in psychiatric and physical health outcomes; 2.1-fold more variance in community functioning; and 3.4-fold more variance in neural responses.
Table 3.
Results of Regression Analyses
| First Set of Models | Second Set of Models | ||||||
|---|---|---|---|---|---|---|---|
| Step 1: HiTOP Dimensions | Step 2: Diagnoses | Step 1: Diagnoses | Step 2: HiTOP Dimensions | ||||
| R 2 | ΔR2 | F change | R 2 | ΔR2 | F Change | R2 Step 1 HiTOP/ R2 Step 1 Diagnosis | |
| Psychiatric outcomes | |||||||
| Recoverya | .27*** | .04* | .14*** | .17*** | 1.91 | ||
| Full symptom remissiona | .34*** | .09*** | .25*** | .18*** | 1.35 | ||
| Community functioning | |||||||
| Educational attainmenta | .10*** | .03 | .06* | .07** | 1.70 | ||
| Employeda | .18*** | .02 | .09*** | .12*** | 2.08 | ||
| Public assistancea | .24*** | .03 | .13*** | .14*** | 1.88 | ||
| Role functioning | .22*** | .03* | 2.81* | .11*** | .14*** | 9.85*** | 1.98 |
| Living independently | .11*** | .04* | 3.29* | .10*** | .05** | 3.46** | 1.12 |
| Social functioning | .23*** | .01 | 0.99 | .06** | .18*** | 12.02*** | 3.82 |
| WHO-DAS Global Disability | .15*** | .05* | 3.15* | .07** | .13*** | 7.05*** | 2.12 |
| Physical health | |||||||
| Diabetesa | .10** | .02 | .05 | .07* | 1.97 | ||
| Hypertensiona | .05 | .02 | .02 | .05 | -- | ||
| Neural responses | |||||||
| MMN duration | .06* | .02 | 0.73 | .03 | .05 | 1.87 | 2.28 |
| MMN frequency | .02 | .01 | 0.39 | .01 | .02 | 0.74 | -- |
| P3a amplitude | .07* | .01 | 0.60 | .01 | .07* | 2.73* | 7.34 |
| P3a latency | .05 | .02 | 1.09 | .02 | .06 | 2.14 | -- |
| Cognitive functioning | |||||||
| Cognition composite | .15*** | .09*** | 4.81*** | .17*** | .07*** | 2.53*** | 0.86 |
Note: WHO-DAS, World Health Organization Disability Assessment Schedule; MMN, Mismatched negativity; Ratio was not computed if none of the steps was significant.
aNagelkerke’s R2 estimated in logistic regression; F change can only be computed for linear regressions. See supplementary table 2 for additional logistic regression statistics.
*P < .05, **P < 01, ***P < .001.
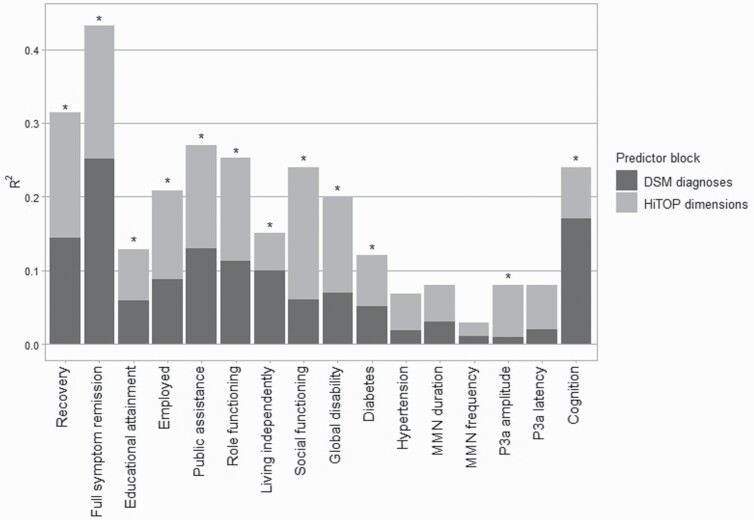
We formally tested incremental validity of the 2 systems in Step 2 of regression models (table 3). As can be seen in figure 1, HiTOP dimensions predicted all outcomes except hypertension, MMN, and P3a latency even when controlling for diagnosis. Conversely, after dimensions were controlled, diagnoses predicted psychiatric, cognitive, and some functional outcomes, but not educational attainment, employment, social functioning, physical health, or neural responses.
Fig. 1.
Total R2 for DSM diagnoses (Step 1) and HiTOP measures (Step 2) as predictors for psychiatric outcomes, physical health outcomes, neural functioning, and cognitive functioning. Asterisks denote significant ΔR2 when HiTOP dimensions were added to the models.
Discussion
The HiTOP model is hypothesized to be a more informative classification of psychotic disorders, but data on its prognostic validity is limited. We performed the first test of whether HiTOP dimensions complemented DSM diagnoses in prediction. Overall, HiTOP dimensions outperformed DSM diagnoses in predicting psychiatric and physical outcomes, community functioning, and neural functioning 20 years later, with 1.7-fold to 3.4-fold improvement in predictive power. Cognitive functioning was the sole exception, as it was predicted somewhat better by DSM diagnoses than HiTOP. This suggests specificity in the predictive advantage of HiTOP dimensions. Both systems contributed uniquely to prediction of outcomes, except educational attainment, employment, social functioning, diabetes, and neural functioning, where diagnoses did not improve prediction above dimensions. Taken together, the present results indicate that dimensional description of patients can improve prognostication when used in conjunction with DSM diagnosis. Our findings support a shift in diagnosis of psychotic disorders from exclusively categorical to one with both dimensions and categories.
The current findings are consistent with previous cross-sectional work comparing dimensions and categories in accounting for biotypes, functional impairments, and service use in psychotic disorders.5,27 The present study extends prior research to prediction and a broader range of outcomes, namely illness course, physical health, cognitive functioning, and neural functioning. This research has implications for clinical practice. Prognosis in psychotic disorders is challenging, especially with first-episode patients.58 A HiTOP-based assessment can help to forecast outcomes such as long-term recovery. This also can help to guide interventions, with more extensive services provided to patients at risk of poor outcomes. Also, given racial/ethnic and gender disparities associated with traditional diagnoses,59–61 dimensional assessments can help determine whether these disparities reflect diagnostic biases or true demographic differences in symptom prevalences. This is a promising direction for future research.
Among HiTOP dimensions, negative symptoms and functional impairments were the strongest predictors of many outcomes. This is consistent with previous literature reporting that negative symptoms have stronger relationships with functional and neurocognitive outcomes than positive symptoms.62,63 This is also consistent with findings that negative, but not positive, symptoms, track with P3a amplitude64 and with findings of more robust associations between negative (vs positive symptoms) and diabetes.65 However, positive symptoms were most informative in prediction of hypertension and MMN duration. This illustrates that although the predictive power was modest for these health and neural indicators, increased predictive specificity can be gained through empirical phenotypes such as HiTOP.
A potential concern with dimensional approaches is their feasibility in clinical research and practice. A diagnosis is a single categorical descriptor and far simpler than a profile on 5 dimensions. However, the diagnostic process can be labor-intensive. The present study required multiple interviews with the patient, an informant, and a review of medical records; psychiatrists studied the data in consensus meetings to arrive at a diagnosis. In contrast, dimensional ratings were made by a single master’s level clinician. Raters were trained and supervised by senior study staff, but in the current study, dimensional ratings were far less labor-intensive than diagnoses. It is likely that neither dimensional ratings nor diagnoses will be as predictive in applied settings as they were in our research protocol. Nevertheless, dimensional assessments done by carefully trained para-professionals or psychiatric staff (eg, psychiatric nurses and social workers) may be a feasible and informative addition to a psychiatrist’s diagnosis in applied settings. Billing is facilitated by a crosswalk that translates HiTOP dimensions into diagnostic codes (https://hitop.unt.edu/clinical-tools/billing-hitop).
Among traditional diagnoses, schizophrenia consistently predicted worse outcomes, and bipolar disorder with psychotic features predicted better outcomes. Major depressive disorder with psychotic features, substance-induced psychosis, and other psychoses also forecasted good outcomes, but these effects were weak and inconsistent. This is aligned with extensive research showing that a schizophrenia diagnosis is an indicator of poor prognosis (eg, refs.66,67) whereas bipolar disorder has the best outcomes among psychotic disorders.24 Taken together, this highlights that traditional diagnosis of psychotic disorders offers considerable prognostic validity, although much of it is concentrated in the distinction between schizophrenia and bipolar disorder. Other diagnoses may be more predictive of different outcomes not considered here (eg, liver cirrhosis).
Jointly, HiTOP dimensions and diagnoses were able to predict psychiatric outcomes (recovery and remission) and some facets of community functioning (especially role and social functioning) quite well. Recent longitudinal studies of relatively long-term outcomes (eg, 10 years68; 14 years69) have highlighted the importance of specific symptoms in individuals with psychotic disorders in predicting psychiatric and functional outcomes. The current work extends these findings by showing that HiTOP dimensions and DSM diagnoses combined have even greater predictive power for a wide variety of outcomes over a 20-year interval. Notably, although HiTOP dimensions can be measured by widely available instruments (eg, refs.13,33,70) the HiTOP consortium is developing measures to specifically assess dimensions included in the system.71 Thus, moving forward, the consideration of both HiTOP dimensions and diagnoses together will aid in long-term predictions.
Several limitations should be noted. First, analyses were limited to primary diagnosis, and comorbidities, such as substance abuse, were not considered. However, prior analyses of this sample found that adding comorbid diagnoses did not improve predictive power beyond the primary diagnoses.72 Second, only 5 HiTOP dimensions were included. To equate the number of dimensional and diagnostic predictors, we restricted analyses to components of the thought disorder spectrum, which encompasses psychotic disorders. As with any prediction, unmeasured confounders may be responsible for some of the predictive power observed in present analyses. Future research is needed to explicate other risk factors for long-term outcomes in psychotic disorders. Third, we did not include treatment among the array of outcomes primarily because it is biased by clinical state (sicker patients receiving more treatment). Lastly, this cohort is representative of first admissions with psychosis, but it is limited to one geographical region. It is important to replicate these findings in other settings.
Despite these limitations, the current study is the first to show the advantage using HiTOP dimensions in conjunction with the DSM diagnoses in predicting some long-term outcomes in psychotic disorders. Our results suggest that using both nosologies—DSM categories and HiTOP dimensions—would provide maximum information. Indeed, although the DSM emphasizes categorical classification of psychosis, a dimensional assessment has been provided in Section 3 of DSM-5,73 and HiTOP can further enhance this assessment. Taken together, the current findings support a shift away from exclusive reliance on categorical diagnoses and toward incorporating empirical symptom dimensions in research and clinical practice.
Supplementary Material
Acknowledgments
We gratefully acknowledge the support of the participants and mental health professionals of Suffolk County for their contributions to this project. We are indebted to the clinical interviewers, field coordinators, and psychiatrists who formulated the consensus diagnoses at the 6-month follow-up, including Charles Rich, Marsha Karant, Shmuel Fennig, Thomas J. Craig, Beatrice Kovasznay, and Gabrielle A. Carlson. Joseph E. Schwartz, Lina Jandorf, Alan Miller and Janet Lavelle made seminal contributions to the study’s foundations. Present findings have not been reported previously.
Funding
National Institutes of Health (MH44801 to E.J.B.; MH094398 and MH110434 to R.K.).
References
- 1.Association AP. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 2.World Health Organization. The ICD-10 Version 2016: Classification of mental and behavioural disorders: Clinical descriptions and diagnostic guidelines. Available at: https://icd.who.int/browse10/2016/en. Accessed May 8, 2020.
- 3.Mayes R, Horwitz AV. DSM-III and the revolution in the classification of mental illness. J Hist Behav Sci. 2005;41(3):249–267. [DOI] [PubMed] [Google Scholar]
- 4.Cuesta MJ, Peralta V. Integrating psychopathological dimensions in functional psychoses: a hierarchical approach. Schizophr Res. 2001;52(3):215–229. [DOI] [PubMed] [Google Scholar]
- 5.Reininghaus U, Böhnke JR, Chavez-Baldini U, et al. Transdiagnostic dimensions of psychosis in the Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP). World Psychiatry. 2019;18(1):67–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guloksuz S, van Os J. The slow death of the concept of schizophrenia and the painful birth of the psychosis spectrum. Psychol Med. 2018;48(2):229–244. [DOI] [PubMed] [Google Scholar]
- 7.Strauss GP, Cohen AS. A transdiagnostic review of negative symptom phenomenology and etiology. Schizophr Bull. 2017;43(4):712–719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Linscott RJ, van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. 2013;43(6):1133–1149. [DOI] [PubMed] [Google Scholar]
- 9.Reininghaus U, Priebe S, Bentall RP. Testing the psychopathology of psychosis: evidence for a general psychosis dimension. Schizophr Bull. 2013;39(4):884–895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Os J. “Salience syndrome” replaces “schizophrenia” in DSM-V and ICD-11: psychiatry’s evidence-based entry into the 21st century? Acta Psychiatr Scand. 2009;120:363–372. [DOI] [PubMed] [Google Scholar]
- 11.Bromet EJ, Kotov R, Fochtmann LJ, et al. Diagnostic shifts during the decade following first admission for psychosis. Am J Psychiatry. 2011;168(11):1186–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Regier DA, Narrow WE, Clarke DE, et al. DSM-5 field trials in the United States and Canada, Part II: test-retest reliability of selected categorical diagnoses. Am J Psychiatry. 2013;170(1):59–70. [DOI] [PubMed] [Google Scholar]
- 13.Kotov R, Krueger RF, Watson D, et al. The hierarchical taxonomy of psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J Abnorm Psychol. 2017;126(4):454–477. [DOI] [PubMed] [Google Scholar]
- 14.Moore TV. The empirical determination of certain syndromes underlying praecox and manic-depressive psychoses. Am J Psychiatry. 1930;86:719–738. [Google Scholar]
- 15.WITTENBORN JR. Symptom patterns in a group of mental hospital patients. J Consult Psychol. 1951;15(4):290–302. [DOI] [PubMed] [Google Scholar]
- 16.Zubin J. Classification of the behavior disorders. Annu Rev Psychol. 1967;18:373–406. [DOI] [PubMed] [Google Scholar]
- 17.Grube BS, Bilder RM, Goldman RS. Meta-analysis of symptom factors in schizophrenia. Schizophr Res. 1998;31(2-3):113–120. [DOI] [PubMed] [Google Scholar]
- 18.Kotov R, Foti D, Li K, Bromet EJ, Hajcak G, Ruggero CJ. Validating dimensions of psychosis symptomatology: neural correlates and 20-year outcomes. J Abnorm Psychol. 2016;125(8):1103–1119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Strauss GP, Gold JM. A Psychometric comparison of the clinical assessment interview for negative symptoms and the brief negative symptom scale. Schizophr Bull. 2016;42(6):1384–1394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ruggero CJ, Kotov R, Hopwood CJ, et al. Integrating the Hierarchical Taxonomy of Psychopathology (HiTOP) into clinical practice. J Consult Clin Psychol. 2019;87(12):1069–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cicero DC, Jonas KG, Li K, Perlman G, Kotov R. Common taxonomy of traits and symptoms: linking schizophrenia symptoms, schizotypy, and normal personality. Schizophr Bull. 2019;45(6):1336–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Longenecker JM, Krueger RF, Sponheim SR. Personality traits across the psychosis spectrum: a hierarchical taxonomy of psychopathology conceptualization of clinical symptomatology. Personal Ment Health. 2020;14(1):88–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clark LA, Cuthbert B, Lewis-Fernández R, Narrow WE, Reed GM. Three approaches to understanding and classifying mental disorder: ICD-11, DSM-5, and the National Institute of Mental Health’s Research Domain Criteria (RDoC). Psychol Sci Public Interest. 2017;18(2):72–145. [DOI] [PubMed] [Google Scholar]
- 24.Kotov R, Fochtmann L, Li K, et al. Declining clinical course of psychotic disorders over the two decades following first hospitalization: evidence from the Suffolk County Mental Health Project. Am J Psychiatry. 2017;174(11):1064–1074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robins E, Guze SB. Establishment of diagnostic validity in psychiatric illness: its application to schizophrenia. Am J Psychiatry. 1970;126(7):983–987. [DOI] [PubMed] [Google Scholar]
- 26.Goodwin DW, Guze SB. Preface. In: Goodwin DW, Guze SB, eds. Psychiatric Diagnosis. New York, NY: Oxford University Press; 1974:ix–xii. [Google Scholar]
- 27.Rosenman S, Korten A, Medway J, Evans M. Dimensional vs. categorical diagnosis in psychosis. Acta Psychiatr Scand. 2003;107(5):378–384. [DOI] [PubMed] [Google Scholar]
- 28.Andrews G, Goldberg DP, Krueger RF, et al. Exploring the feasibility of a meta-structure for DSM-V and ICD-11: could it improve utility and validity? Psychol Med. 2009;39(12):1993–2000. [DOI] [PubMed] [Google Scholar]
- 29.Bromet EJ, Schwartz JE, Fennig S, et al. The epidemiology of psychosis: the Suffolk County Mental Health Project. Schizophr Bull. 1992;18(2):243–255. [DOI] [PubMed] [Google Scholar]
- 30.Fett AJ, Velthorst E, Reichenberg A, et al. Long-term changes in cognitive functioning in individuals with psychotic disorders: findings from the Suffolk County Mental Health Project. JAMA Psychiatry. 2020;77(4):387–396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.First MB, Spitzer RL, Gibbon M, Williams JBM. Structured clinical interview diagnostic (SCID) for DSM-IV Axis I disorders-Clinician version (SCID-CV). 1997.
- 32.Kotov R, Leong SH, Mojtabai R, et al. Boundaries of schizoaffective disorder: revisiting Kraepelin. JAMA Psychiatry. 2013;70(12):1276–1286. [DOI] [PubMed] [Google Scholar]
- 33.Kotov R, Jonas KG, Carpenter WT, et al. ; HiTOP Utility Workgroup . Validity and utility of Hierarchical Taxonomy of Psychopathology (HiTOP): I. Psychosis superspectrum. World Psychiatry. 2020;19(2):151–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Andreasen NC.Scale for the Assessment of Positive Symptoms. Iowa City, IA: University of Iowa, College of Medicine; 1984. [Google Scholar]
- 35.Andreasen NC.Scale for the Assessment of Negative Symptoms. Iowa City, IA: University of Iowa, College of Medicine; 1983. [Google Scholar]
- 36.Heinrichs DW, Hanlon TE, Carpenter WT Jr. The Quality of Life Scale: an instrument for rating the schizophrenic deficit syndrome. Schizophr Bull. 1984;10(3):388–398. [DOI] [PubMed] [Google Scholar]
- 37.Liberman RP, Kopelowicz A, Ventura J, Gutkind D. Operational criteria and factors related to recovery from schizophrenia. Int Rev Psychiatry. 2002;14:256–272. [Google Scholar]
- 38.Overall JE, Gorham DR. The Brief Psychiatric Rating Scale (BPRS): recent developments in ascertainment and scaling. Psychopharmacol Bull. 1988;24:97–99. [PubMed] [Google Scholar]
- 39.Andreasen NC, Carpenter WT Jr, Kane JM, Lasser RA, Marder SR, Weinberger DR. Remission in schizophrenia: proposed criteria and rationale for consensus. Am J Psychiatry. 2005;162(3):441–449. [DOI] [PubMed] [Google Scholar]
- 40.Velthorst E, Fett AJ, Reichenberg A, et al. The 20-Year longitudinal trajectories of social functioning in individuals with psychotic disorders. Am J Psychiatry. 2017;174(11):1075–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Üstün TB, Kostanjsek N, Chatterji S, Rehm J.. Measuring Health and Disability: Manual for WHO Disability Assessment Schedule WHODAS 2.0. World Health Organization; 2010. Available at: https://apps.who.int/iris/handle/10665/43974. Accessed March 21, 2020. [Google Scholar]
- 42.Hennekens CH, Hennekens AR, Hollar D, Casey DE. Schizophrenia and increased risks of cardiovascular disease. Am Heart J. 2005;150(6):1115–1121. [DOI] [PubMed] [Google Scholar]
- 43.Mitchell AJ, Vancampfort D, Sweers K, van Winkel R, Yu W, De Hert M. Prevalence of metabolic syndrome and metabolic abnormalities in schizophrenia and related disorders–a systematic review and meta-analysis. Schizophr Bull. 2013;39(2):306–318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Erickson MA, Ruffle A, Gold JM. A meta-analysis of mismatch negativity in schizophrenia: from clinical risk to disease specificity and progression. Biol Psychiatry. 2016;79(12):980–987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Onitsuka T, Oribe N, Nakamura I, Kanba S. Review of neurophysiological findings in patients with schizophrenia. Psychiatry Clin Neurosci. 2013;67(7):461–470. [DOI] [PubMed] [Google Scholar]
- 46.Light GA, Swerdlow NR, Thomas ML, et al. Validation of mismatch negativity and P3a for use in multi-site studies of schizophrenia: characterization of demographic, clinical, cognitive, and functional correlates in COGS-2. Schizophr Res. 2015;163(1-3):63–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Luck SJ.An Introduction to the Event-Related Potential Technique. 2nd ed. Cambridge, MA: MIT Press; 2014. [Google Scholar]
- 48.Gratton G. Biosignal processing. In: Cacioppo JT, Tassinary LG, Bernston GG, eds. Handbook of Psychophysiology. New York, NY: Oxford University Press; 2007:834–858. [Google Scholar]
- 49.Donaldson KR, Novak KD, Foti D, et al. Associations of mismatch negativity with psychotic symptoms and functioning transdiagnostically across psychotic disorders. J Abnorm Psychol. 2020;129(6):570–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Perlman G, Foti D, Jackson F, Kotov R, Constantino E, Hajcak G. Clinical significance of auditory target P300 subcomponents in psychosis: Differential diagnosis, symptom profiles, and course. Schizophr Res. 2015;165(2-3):145–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bechtoldt HP, Benton AL, Fogel ML. An application of factor analysis in neuropsychology. Psychol Rec. 1962;12:147–156. [Google Scholar]
- 52.Wechsler D.Wechsler Memory Scale Adminstration and Scoring Manual. New York, NY: Psychological Corporation; 1987. [Google Scholar]
- 53.Wechsler D.Wechsler Adult Intelligence Scale-Revised. New York, NY: Psychological Corporation; 1981. [Google Scholar]
- 54.REITAN RM. The relation of the trail making test to organic brain damage. J Consult Psychol. 1955;19(5):393–394. [DOI] [PubMed] [Google Scholar]
- 55.Trenerry MR, Crosson B, DeBoe J, Leber W.. Stroop Neuropsychological Screening Test. Odessa, FL: Psychological Assessment Resources; 1989. [Google Scholar]
- 56.Burdick KE, Lencz T, Funke B, et al. Genetic variation in DTNBP1 influences general cognitive ability. Hum Mol Genet. 2006;15(10):1563–1568. [DOI] [PubMed] [Google Scholar]
- 57.Jonas KG, Lencz T, Li K, et al. Schizophrenia polygenic risk score and 20-year course of illness in psychotic disorders. Transl Psychiatry. 2019;9(1):300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lally J, Ajnakina O, Stubbs B, et al. Remission and recovery from first-episode psychosis in adults: systematic review and meta-analysis of long-term outcome studies. Br J Psychiatry. 2017;211(6):350–358. [DOI] [PubMed] [Google Scholar]
- 59.Chien PL, Bell CC. Racial differences in schizphrenia. Directions in Psychiatry 2008;28:297–304. [Google Scholar]
- 60.Häfner H. Gender differences in schizophrenia. Psychoneuroendocrinology. 2003;28 Suppl 2:17–54. [DOI] [PubMed] [Google Scholar]
- 61.Schwartz RC, Blankenship DM. Racial disparities in psychotic disorder diagnosis: a review of empirical literature. World J Psychiatry. 2014;4(4):133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Hanlon FM, Yeo RA, Shaff NA, et al. A symptom-based continuum of psychosis explains cognitive and real-world functional deficits better than traditional diagnoses. Schizophr Res. 2019;208:344–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Ventura J, Hellemann GS, Thames AD, Koellner V, Nuechterlein KH. Symptoms as mediators of the relationship between neurocognition and functional outcome in schizophrenia: a meta-analysis. Schizophr Res. 2009;113(2-3):189–199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ford JM. Schizophrenia: the broken P300 and beyond. Psychophysiology. 1999;36(6):667–682. [PubMed] [Google Scholar]
- 65.Perry BI, Salimkumar D, Green D, et al. Associated illness severity in schizophrenia and diabetes mellitus: a systematic review. Psychiatry Res. 2017;256:102–110. [DOI] [PubMed] [Google Scholar]
- 66.Breier A, Schreiber JL, Dyer J, Pickar D. National Institute of Mental Health longitudinal study of chronic schizophrenia. Prognosis and predictors of outcome. Arch Gen Psychiatry. 1991;48(3):239–246. [DOI] [PubMed] [Google Scholar]
- 67.Strauss JS, Carpenter WT Jr. The prognosis of schizophrenia: rationale for a multidimensional concept. Schizophr Bull. 1978;4(1):56–67. [DOI] [PubMed] [Google Scholar]
- 68.Chan SKW, Chan HYV, Pang HH, et al. Ten-year trajectory and outcomes of negative symptoms of patients with first-episode schizophrenia spectrum disorders. Schizophr Res. 2020. [DOI] [PubMed] [Google Scholar]
- 69.Sigrúnarson V, Gråwe RW, Lydersen S, Morken G. Predictors of long term use of psychiatric services of patients with recent-onset schizophrenia: 12 years follow-up. BMC Psychiatry. 2017;17(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kring AM, Gur RE, Blanchard JJ, Horan WP, Reise SP. The Clinical Assessment Interview for Negative Symptoms (CAINS): final development and validation. Am J Psychiatry. 2013;170(2):165–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Simms LJ, Wright AGC, Cicero DC, et al. Development of measures for the Hierarchical Taxonomy of Psychopathology (HiTOP): a collaborative scale development project. Assessment. In press. 2020. [DOI] [PubMed] [Google Scholar]
- 72.Kotov R, Chang SW, Fochtmann LJ, et al. Schizophrenia in the internalizing-externalizing framework: a third dimension? Schizophr Bull. 2011;37(6):1168–1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Barch DM, Bustillo J, Gaebel W, et al. Logic and justification for dimensional assessment of symptoms and related clinical phenomena in psychosis: relevance to DSM-5. Schizophr Res. 2013;150(1):15–20. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.