Abstract
Social anxiety is common in psychosis and associated with impaired functioning, poorer quality of life, and higher symptom severity. This study systematically reviewed factors maintaining social anxiety in people with attenuated, transient, or persistent psychotic experiences. Other correlates of social anxiety were also examined. MEDLINE, Embase, CENTRAL, and PsycINFO were searched for relevant literature up to October 19, 2020. Forty-eight articles were eligible for narrative synthesis: 38 cross-sectional studies, 8 prospective studies, 1 uncontrolled trial, and 1 qualitative study. From 12060 participants, the majority was general population (n = 8771), followed by psychosis samples (n = 2532) and those at high risk of psychosis (n = 757). The methodological quality and risk of bias were assessed using the Mixed Methods Appraisal Tool. Ninety percent of studies were rated as high to very-high quality. Poorer quality studies typically failed to adequately control for confounds and provided insufficient information on the measurement validity and reliability. Prominent psychological factors maintaining social anxiety included self-perceptions of stigma and shame. Common correlates of social anxiety included poorer functioning and lower quality of life. In conclusion, stigma and shame could be targeted as a causal mechanism in future interventional studies. The integration of findings from this review lead us to propose a new theoretical model to guide future intervention research.
Keywords: shame, social anxiety, social stigma, models (theoretical), psychotic disorders, quality of life
Introduction
Social anxiety disorder (SAD) is a common mental health problem for people at risk of psychosis (prevalence 6.1%–42.3%)1–3 or with an established psychotic disorder (pooled prevalence 16%–26%).4 SAD is characterized by exaggerated fears of evaluation by others, leading to distress and/or avoidance of social interactions.5 It is a disabling disorder and a preceding cause of anxiety, affective, and substance dependence/abuse disorders.6 Many people with schizophrenia report having problems with social relationships and activities.7 With comorbid SAD, people with schizophrenia report significantly lower functioning, lower self-esteem, higher symptom severity,8 poorer quality-of-life (QoL),9 higher depression,4 and higher rates of suicide attempts.10 Despite SAD being a significant problem for people with psychosis,4,11 there has been little treatment-relevant research.12
Cognitive behavioral therapy (CBT) is a recommended psychological intervention for people with schizophrenia,13,14 effectively reducing psychotic symptoms in people with psychosis or those at risk of psychosis.15–21 In addition to the evidence that CBT is the treatment of choice for a single diagnosis of SAD,22,23 the mechanisms of therapeutic change are increasingly well understood. In particular, the use of experiential exercises to help people with SAD learn the adverse effects of self-focused attention and safety-seeking behaviors are core components of recommended treatments.24 However, clinical guidelines are silent on treatment choice when SAD is a comorbid condition,12 and it remains to be ascertained how CBT for SAD in people with psychosis may reduce social anxiety.12,25,26 Hence, further examination of the therapeutic mechanisms underpinning CBT for SAD in psychosis require further investigation.12
To understand mechanisms underpinning SAD and psychosis, we adhered to 3 principles recommended in the interventionist-causal model approach27 to identify candidate causal factors. These are: (1) a focus on a single factor that is measurable; (2) the putative causal process is amenable to change by the causal factor; and (3) the causal factor is integrated with a theoretical understanding to guide therapy. We set out to determine, integrate, and critically analyze the evidence for psychological factors in the maintenance of social anxiety in people with psychosis. Additionally, we explored other correlates of social anxiety.
Methods
Protocol and Registration
The present systematic review was reported according to the Preferred Reporting Items of Systematic Reviews and Meta-analyzes (PRISMA).28 The protocol was registered on PROSPERO and can be accessed at www.crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42018117616.
Search Strategy and Information Sources
Four databases were searched on October 19, 2020: Cochrane Central Register of Controlled Trials (1996 to October 2020); Embase (1947 to October 2020); Ovid MEDLINE(R) (1946 to October 2020); and PsycINFO (1806 to October 2020).
Search terms used for population were ((psychosis) or (psychotic) or (schizophreni*) or (schizoaffective) or (delusion*) or (paranoi*) or (clinical high risk*) or (ultra high risk*) or (attenuated) or (at risk mental state*) or (recent onset) or (first episode psycho*) or (early psycho*)) and outcomes were ((social anxi*) or (social phob*)). Limits were applied for English language and human. Electronic search strategies for Embase and MEDLINE are shown in supplementary table 1. A manual search was completed for identified articles from the electronic search, and their reference lists, those articles meeting criteria for inclusion were subjected to forward and backward citation to identify further eligible papers. The journal Schizophrenia Bulletin was hand-searched. Authors were contacted when published studies had insufficient data or where there was a need for more data to clarify results. We also asked active researchers for unpublished or recently submitted studies. Ten percent of study selection, data extraction and quality assessment were independently performed by 2 researchers with excellent agreement, the rest was performed by one researcher (supplementary table 2). Due to difference in study designs, we used the Mixed Methods Appraisal Tool (MMAT)–version 201829 for critical appraisal. MMAT is widely used for evaluation of study strengths and weaknesses.30
Eligibility Criteria
We examined studies involving people diagnosed with psychosis, those experiencing attenuated and milder forms of psychotic experiences (eg, schizotypy), since psychotic experiences are seen in the general population,31,32 and distributed along a continuum.31,33
Inclusion Criteria.
(1) study samples included people diagnosed with schizophrenia and psychosis spectrum disorders or people deemed to be at high risk of developing psychosis and psychotic experiences; (2) analog studies measuring psychotic-like experiences such as paranoia; and (3) measurement of any psychological factors linked to social anxiety and psychotic experiences.
Exclusion Criteria.
(1) literature reviews, single-case series, or case reports; (2) studies of mixed diagnostic samples that do not present data in sub-groups or only provide pooled or aggregated data.
Data Synthesis
We planned a narrative synthesis due to the anticipated high heterogeneity of populations, measurements, and outcomes. Psychological “maintenance factors” that lead to the persistence of social anxiety in psychotic experiences such as stigma, low self-esteem, and metacognition were considered. We also explored factors associated with social anxiety and referred to these as “correlated factors.”
Results
Identification of the Studies
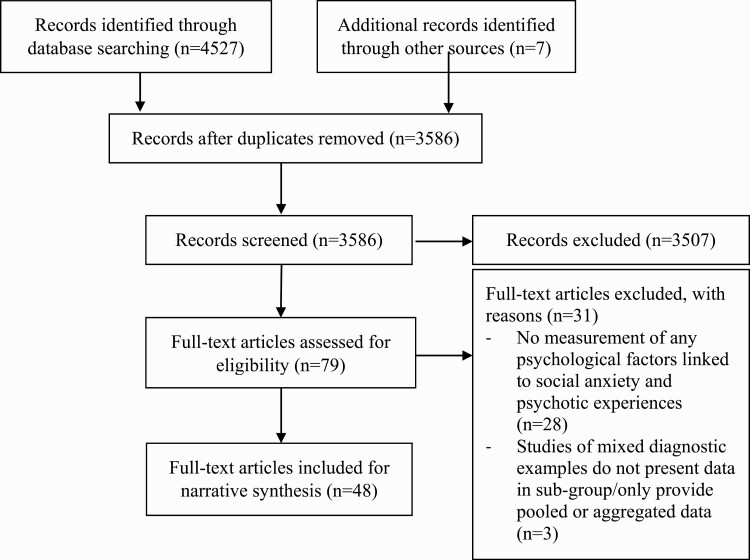
Four thousand five hundred twenty-seven records were identified through database searching and 7 records from additional sources. After duplicates were removed, 3586 records were screened, resulting in 79 full-texts to be assessed against eligibility criteria. Excluded papers with reasons are presented in supplementary table 3. A total of 48 papers were included for narrative synthesis (figure 1).
Fig. 1.
Study selection process.
Study and Participant Characteristics
Included studies were cross-sectional (n = 38), prospective (n = 8), uncontrolled trial (n = 1) and qualitative (n = 1), published between 1992 and 2020, and originated from North America (n = 15), United Kingdom (n = 10), Asia (n = 10), Europe (n = 9), Australia (n = 3) and Africa (n = 1). The total number of participants across 48 studies was 12060, of which the majority were from the general population (n = 8771); followed by people with established psychosis (n = 2532) and high psychosis risk samples (n = 757), other participant details see supplementary table 4.
Assessment of Social Anxiety or Social Phobia and Psychosis
Table 1 shows the measures used to assess the level of social anxiety/social phobia and psychosis, including their brief details and evidence of psychometric properties. The Liebowitz Social Anxiety Scale,34 the Social Interaction Anxiety Scale, and the Social Phobia Scale35 were most frequently used for social anxiety or social phobia assessment. The Positive and Negative Syndrome Scale,36 the Scale for the Assessment of Positive Symptoms37 and the Scale for the Assessment of Negative Symptoms38 were most commonly used to index psychosis.
Table 1.
Measurements Used to Assess Level of Social Anxiety or Social Phobia and Psychosis
| Measurements Used for Social Anxiety or Social Phobia | Frequency of Use | Measures | Items | Evidence of Reliability/Validity |
|---|---|---|---|---|
| Liebowitz Social Anxiety Scale (LSAS), LSAS self- rating (LSAS-SR) | 18 | Fear and avoidance of social situations and used mostly in the social anxiety research34 and in schizophrenia10 | 24 | Good reliability and validity in social anxiety,110,111 and good reliability in schizophrenia.10 |
| Social Interaction Anxiety Scale (SIAS) | 14 | Anxiety in interpersonal encounters, used alongside with SPS and mostly in the social anxiety research35 | 20 | Good reliability and validity,35 good discriminant validity with SPS and SPAI.112 |
| Social Phobia Scale (SPS) | 6 | Performance anxiety in situations where the individual fears being observed and scrutinized by others, used alongside with SIAS and mostly in the social phobia research35 | 20 | Good reliability and validity,35 good discriminant validity with SIAS and SPAI112 |
| Fear of Negative Evaluation (FNE) | 3 | Anxiety about being negatively evaluated by others and mostly in the social phobia research113 | 12 | Good reliability and validity113 |
| State trait anxiety inventory (STAI) | 3 | Various experiences of anxiety including social anxiety. Trait anxiety refers to persistent anxiety, while State anxiety reflects momentary anxiety114 | 40 | Good reliability115 and validity116 |
| Multidimensional Anxiety Questionnaire (MAQ) | 3 | Various experiences of anxiety including social anxiety, assessing worries about social embarrassment and social avoidance,117 used in schizophrenia118 | 40 | Good reliability and validity in people with mental illness, 117 and good validity in schizophrenia.118 |
| Brief Social Phobia Scale (BSPS) | 1 | Fear, avoidance and physiological symptoms associated with common social situations119 | 11 | Acceptable reliability and validity119 |
| Social Avoidance and Distress Scale (SADS) | 1 | Fear, discomfort, subjective distress and the avoidance of social situations and used mostly in social anxiety113 | 28 | Good reliability and validity113 |
| Social Phobia and Anxiety Inventory (SPAI) | 1 | Somatic, cognitive, and behavioral aspects of social phobia across a wide range of social situations and settings120 | 45 | Good reliability and validity,120,121 good discriminant validity with SIAS and SPS112 |
| Interaction Anxiousness Scale (IAS) | 1 | Subjective experience of anxiety associate with social interactions122 | 15 | Good reliability and validity122 |
| Unsicherheits-Fragebogen (U-scale)a | 1 | Experiences of social anxiety123 | 65 | The scale was proved to be valid and transferable across samples124 |
| Simulated social interaction test (SSIT) | 1 | Social skills responded to 8 social interactions (eg, disapproval/ criticism, social visibility/assertiveness)125 | 8 | Good reliability and validity in schizophrenia126 |
| Measurements Used for Characterizing Psychosis | Frequency of Use | Measures | Items | Evidence of Reliability/Validity |
| Positive and Negative Syndrome Scale (PANSS) | 28 | Psychopathology (positive, negative and emotional discomfort) in schizophrenia36 | 30 | Good to excellent reliability127 |
| Scale for the Assessment of Positive Symptoms (SAPS) | 5 | Positive symptoms of schizophrenia, used alongside with SANS37 | 34 | Good validity and reliability37 |
| Scale for the Assessment of Negative Symptoms (SANS) | 5 | Negative symptoms of schizophrenia, used alongside with SAPS38 | 25 | Good validity and reliability128 |
| Brief Psychiatric Rating Scale (BPRS) | 3 | Psychopathology during the week prior to the assessment129 | 18 | Good validity and reliability130 |
| Clinical Global Impression (CGI) | 2 | All symptomatology together (psychotic symptoms, anxiety, and depressive) in one number (CGI-severity subscale)131 | 1 | Strong validity and good reliability, but lack of correlation coefficient with depression132 |
| Green Paranoid Thoughts Scale–Persecutory Paranoia Subscale (GPTS) | 1 | Two specific subtypes of paranoia: social reference paranoia and persecutory paranoia133 | 16 | Good validity and reliability133 |
| Details of Threat questionnaire (DoT) | 1 | Nature of the perceived threat arising from persecutory delusions: the power of persecutor, the strength of delusional conviction, the perceived impact or awfulness of threat and perceived controllability of the threat134 | 4 | NA |
| Community Assessment of Psychic Experiences (CAPE) | 1 | Lifetime prevalence of positive, negative and depressive symptoms on scales regarding frequency and distress in general population135 | 42 | May overestimate the prevalence of positive symptoms, psychiatrists required to validate patient’s self-report136 |
| Paranoid checklist | 1 | A multidimensional representation of paranoid ideation rating on frequency, conviction and distress associated with paranoia32 | 18 | Good validity and excellent reliability32 |
| Inventory of hostility and suspiciousness | 1 | Paranoia and related concepts: Interpersonal Suspiciousness/ Hostility, Negative Mood/Withdrawal, Anger/Impulsiveness, Mistrust/Wariness and Perceived Hardship/Resentment137 | 47 | Satisfactory validity and reliability137 |
Note: aUnsicherheits-Fragebogen scale assessing for social anxiety.
Quality Assessment
Using MMAT, methodological quality of included studies ranged from 2** to 5***** quality criteria met, of which 43 studies (89.6%) were met at least 4**** quality criteria (tables 2 and 3). The most frequent limitations were the absence of expected confounding or appropriate methods to control for confounders10,11,25,39–45 and failure to use measures with established validity and reliability.39,40,44,46–52 Other reasons for lower quality were the high risk of non-response bias,53–55 insufficient representativeness of the study population53,56,57 and incomplete outcome data,40,46 which decreased the generalizability of the results (supplementary table 5).
Table 2.
Studies Addressing Psychological Maintenance Factors of Social Anxiety in Psychotic Experiences Contexts
| Citation | Design | Sample Characteristic (N) | Measurements 1. Diagnostic Criteria 2. Symptom Scales |
Maintenance Factors | Findings | Quality Criteria Meta | |
|---|---|---|---|---|---|---|---|
| Psychosis | Social anxiety | ||||||
| Michail et al25 | Cross-sectional | Total 135 FEP (60) FEP+SAD (20) SAD (31) NC (24) | 1. ICD-10 2. PANSS | 1. ICD-10 2. SIAS, SPS |
Stigma - PBIQ Shame - OAS Social rank - SCS |
FEP+SAD reported higher levels of PBIQ: entrapment, loss of social goals, poorer illness control and lower perceived social status (F1,79 = 14.5, F1,79 = 12 and F1,79 = 13.1 and F1,79 = 12 respectively) than FEP. Plus, FEP+SAD reported higher level of OAS (F1,135 = 123.1) and lower level of SCS (F1,135 = 49.6) than SAD. All ps < 0.01. | 4**** |
| Gumley et al58 | Cross-sectional | Total 38 SZ (19) SZ+SAD (19) | 1. DSM-IV 2. PANSS | 1. DSM-IV |
Stigma - PBIQ Self-esteem - RSES |
SZ+SAD reported higher levels of PBIQ: self vs illness (F1,36 = 5.0, P < .05); entrapment (F1,36 = 12.7, P < .01); and shame (F1,36 = 10.6, P < .01)) and lower level of RSES (F1,36 = 10.2, P < .01) than SZ. | 5***** |
| Birchwood et al59 | Cross-sectional | Total 79 SZ (56) SZ+SAD (23) | 1. ICD-10 2. PANSS, IS | 2. SIAS, FNE |
Stigma - PBIQ Social rank - SCS Shame - OAS |
SZ+SAD reported less controllable of being psychosis and more entrapping (multivariate F = 15.6, P < .001), and more SCS (F = 27.4, P < .001) compared to SZ. Regarding regression analysis, the PBIQ shame (OR = 1.4, P = .038), PBIQ group fit (OR = 1.3, P = .018) and OAS (OR = 1.1, P = .039) were associated with the presence of SAD, after controlling depression. | 5***** |
| Lysaker et al60 | Prospective | SZ (78) | 1. DSM-IV 2. PANSS | 2. MAQ social anxiety |
Stigma - ISMIS |
Regarding stepwise regression, baseline ISMIS discrimination experience and PANSS negative symptoms significantly predicted MAQ social anxiety at 5 months, after controlling social anxiety at baseline (R2 = 0.45, P < .001). | 5***** |
| Pyle et al61 | Prospective | CAARMS (288) | 1. CAARMS 2. GPTS-PP | 2. SIAS |
Stigma - PBEQ |
Based on hierarchical regression, SIAS at baseline predicted SIAS at 6 months (B = 0.218, partial r = .205, t = 2.347, P = <.05). Plus, internalized stigma: negative appraisal and social acceptance experiences, did not predict SIAS at follow-up. | 5***** |
| Vrbova et al62 | Cross-sectional | Total 61 SZ (42) SZ+SAD (19) | 1. ICD-10 2. PANSS, CGI | 2. LSAS |
Stigma - ISMIS |
SZ+SAD reported higher level of ISMIS (t = 4.251, P < .0001). | 5***** |
| Sutliff et al75 | Cross-sectional | Total 42 SZ (24) SZ+SAD (18) | 1. DSM-IV 2. PANSS | 2. LSAS |
Social rank - SCS |
SZ+SAD reported lower level of SCS than SZ (t = 2.90, P = .006). | 5***** |
| Aherne et al63 | Cross-sectional | FEP (45) | 1. ICD-10 2. Paranoid checklist | 2. SIAS, SPS |
Shame - TADS - CES - IES-R - ISS - OAS |
Regression model showed TADS, CES, IES-R, ISS and OAS were associated with SPS (R2 = 0.299, F1,37 = 6.587, P < .000) and SIAS (R2 = 0.242, F1,37 = 7.134, P < .000). TADS, CES, IES-R, ISS and OAS was associated with paranoia (R2 = 0.092, F4,37 = 3.007, P = .032). | 5***** |
| Romm et al70 | Cross-sectional | FEP (144) | 1. DSM-IV 2. PANSS | 2. LSAS-SR |
Self-esteem - RSES |
Regarding regression analysis, RSES and PANSS suspiciousness were associated with LSAS-SR (B = -0.04, P = .000 and B = 0.07, P = .047, adjusted R2 = 0.46). | 5***** |
| Romm et al71 | Cross-sectional | Total 144 FEP (30) FEP+NonGSAD (46) FEP+GSAD (68) |
1. DSM-IV 2. PANSS, IS | 2. LSAS-SR |
Self-esteem - RSES |
FEP+GSAD reported lower level of RSES than FEP+NonGSAD and FEP alone (F40.39, P < .001). | 5***** |
| Lysaker et al72 | Prospective | SZ (39) | 2. PANSS | 2. LSAS |
Self-esteem - MSEI |
Regarding regression analysis, baseline MSEI predicted LSAS at 6 months (R2 = 0.06, P < .05), after controlling for baseline LSAS (F2,36 = 17.93, P < .001). | 5***** |
| Lecomte et al73 | Cross-sectional | Total 47 SZ (25) SZ+SAD (22) | 1. DSM-IV-TR | 2. BSPS, SIAS |
Self-esteem - SERS-SF ToM - FEIT - FEDT - METT - Emotional recognition (a real- life situation) |
SZ+SAD reported lower level of SERS-SF compared to SZ (P < .01). There were no significant differences between SZ and SZ+SAD for any of the total scores for emotional recognition. | 5***** |
| Katherine et al43 | Cross-sectional | Total 48 SZ (13) SAD (13) Panic (10) NC (12) | 1. DSM-IV-TR 2. PS | 1. DSM-IV-TR 2. SIAS |
Negative self- referent appraisals - SCQ - SAQ-R - EBS |
There were no significant differences of automatic thought (SCQ), underlying assumptions (SAQ-R) and schema (EBS) between people with SZ (with persecutory delusions) and social phobia. | 4**** |
| Voges et al76 | Cross-sectional | SZ (60) | 1. DSM-IV 2. PANSS | 1. DSM-IV 2. SPAI |
Negative self- referent appraisals - SISST |
Patients reported SISST negative self- statement subscale positively correlated with lower level of SPAI (r = .74, P < .004). | 5***** |
| Wong77 | Cross-sectional | SZ (137) | 1. DSM-IV 2. SAPS, SANS | 1. LSAS-SR |
Negative self- referent appraisals - SUMD - IRIS - SPQ - SAPS |
After removing all non-significant paths in the hypothetical model, the final model suggested only 2 direct paths to social anxiety: ideas of reference (standardized path coefficient β = 0.26, P = .002) and negative symptoms (β = 0.29, P < .001) | 5***** |
| Stopa et al78 | Cross-sectional (Qualitative study) | Total 18 SZ (9) Social phobia (9) | 1. DSM-IV-TR | 1. DSM-IV-TR | Negative self- referent appraisals (interview) | Three common themes of interpersonal threat experiences were found in both groups: participants’ experience of threat, reactions while under threat, and subsequent reflections on threat situations, as well as the superordinate theme of narrative coherence. Key differences emerged between the groups in their perceptual experiences, ability to stand back from the threat following the event, and narrative coherence. | 5***** |
| Piccirillo et al53 | Cross-sectional | General population (179) | 2. GPTS | 2. SIAS |
Post-event processing - PEP questionnaire |
Higher SIAS and higher GPTS persecutory paranoia subscale (GPTS-PP) were significantly associated with higher levels of PEP at post-social exclusion intervention (SIAS: B = 0.36, P < .001 and GPTS-PP: B = 0.16, P < .05) and 1 week later (SIAS: B = 0.09, P < .05 and GPTS-PP: B = 0.09, P < .05). | 3*** |
| Achim et al82 | Cross-sectional | Total 140 SZ (29) SZ+SAD (26) NC (84) | 1. DSM-IV 2. PANSS | 2. LSAS |
Mentalization - BICS |
Across all SZ patients or when assessed separately for the SZ− or the SZ+ groups, there were no significant correlations between level of LSAS and BICS. All ps > 0.26. | 5***** |
| Lysaker et al79 | Cross-sectional | Total 88 (all SZ) Paranoia+/ Poorest ToM (14) Paranoia-/Low- middle ToM (29) Paranoia+/High- middle ToM (23) Paranoia-/Highest ToM (22) | 1. DSM-IV 2. PANSS | 2. LSAS |
Theory of Mind - ToM test batteryb |
Paranoia+/high-middleToM group reported higher levels of LSAS than other groups: paranoia+/poorestToM; paranoia-/ highestToM and paranoia-/low-middleToM (LSAS avoidance: F = 5.03, P < .01; and LSAS fear: F = 3.31, P < .05), where paranoia+ refers to significantly higher paranoia than paranoia-. | 5***** |
| Pepper et al80 | Cross-sectional | Total 199 ASD (53) EP (51) SAD (64) NC (31) | 1. DSM-IV | 1. ADIS-IV/V |
Theory of Mind - FPRT - FBPST - FEEST - EQ - RMET - Movie Stills task (with and without face condition) |
SAD reported higher score of RMET (P < .01) and Movie Still with (P < .001) and without face (P < .01) than EP. There were no significant differences of ToM (FPRT, FBPST, FEEST and EQ) between SAD and EP. | 5***** |
| Lysaker et al81 | Cross-sectional | Total 98 (All SZ) Low mastery (33) Intermediate- mastery (52) High mastery (13) | 1. DSM-IV | 2. MAQ social anxiety |
Metacognitive mastery - MAS |
Intermediate-mastery group reported more MAQ social anxiety (F = 3.48, P < .05). | 5***** |
| Achim et al46 | Cross-sectional | Total 82 SZ (29) SZ+SAD (12) NC (41) | 2. PANSS | 1. DSM-IV 2. LSAS |
Reasoning bias - brief-IPSAQ |
SZ+SAD reported significantly lower level of brief-IPSAQ externalizing bias subscale than controls. There were no significant differences of brief-IPSAQ personalizing bias subscale amongst the 3 groups (F2,79 = 0.39, P = .68). | 4**** |
| Rus-Calafell et al55 | Non- randomized controlled trials | SZ (12) Intervention: avatars for social skills enhancement | 1. DSM-IV-TR 2. PANSS | 2. SADS, AI, SSIT | Social avoidance - SADS | When compared between pre- and post-treatment, and post-treatment and follow-up, patient reported significantly improvement of levels of social anxiety: SSIT anxiety subscale (F2,22 = 39.76, P < .05, Cohen’s d = 0.48); and SADS avoidance (F2,22 = 14.80, P < .05, Cohen’s d = 0.58). | 4**** |
| Gajwani et al85 | Cross-sectional | UHR (51) | 2. SIPS | 2. SIAS, SPS |
Attachment - RAAS |
RAAS was associated SIAS and SPS (β = 0.47, P < .001, R2 = 0.22 and 0.39, P < .01, R2 = 0.15). A significant relationship between SIAS and RAAS was mediated by BDI (F 2,49 = 14.66, P < .001, R2 = 0.38). | 5***** |
| Michail et al86 | Cross-sectional | Total 135 FEP (60) FEP+SAD (20) SAD (31) NC (24) | 1. ICD-10 2. PANSS | 1. ICD-10 2. SIAS, SPS |
Attachment - RAAS |
FEP+SAD and SAD reported higher level of insecure adult attachment than FEP and NC (x21 = 38.5, P < .01). | 5***** |
| Russo et al45 | Cross-sectional | Total 120 UHR (60) NC (60) | 1. CAARMS | 2. SSI social anxiety subscale |
Attachment - PAM anxiety and avoidance subscale |
Amongst UHR, there were no significant correlations between SSI social anxiety and insecure anxiety (r = .36, P = .07), and SSI social anxiety and avoidant attachment (r = .28, P = .14). | 3*** |
| Achim et al87 | Cross-sectional | Total 62 FEP (31) NC (31) | 1. DSM-IV 2. PANSS | 2. LSAS |
Empathy - IRI |
Amongst FEP, there was significant correlations between LSAS and IRI perspective taking subscale (r = −.51, P = .004). | 5***** |
| Armando et al88 | Cross-sectional | Total 169 PLEs+SAD (32) SAD (96) Control Group (41) | 1. CAPE | 1. DSM-IV |
Intolerance of uncertainty - IUS |
PLEs+SAD reported higher levels of IUS and BDI-II, BAI and CAPE negative than those SAD alone (P < .0001). | 5***** |
Note: ADIS, Anxiety Disorders Interview Schedule for DSM-IV or V; AI, Assertion Inventory; ASD, Autism Spectrum Disorder; BAI, Beck Anxiety Inventory; BDI, Beck Depression Inventory; BDI-II, BDI 2nd edition; BFNE, Brief Fear of Negative Evaluation scale; BICS, Batterie Intégrée de Cognition Sociale; CAARMS, Comprehensive Assessment of At Risk Mental State; CAPE, Community Assessment of Psychic Experiences; CES, Centrality of events Scale; CGI, Clinical Global Impression; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders 4th edition; DSM-IV-TR, DSM-IV Total Revision; EBS, Evaluative Beliefs Scale; EP, Early Psychosis; EQ, Empathy Quotient of Cambridge Behaviour Scale; ES, Effect Size; FBPST, False Belief Picture Sequencing Task; FEDT, Facial Emotion Discrimination Test; FEEST, Facial Expressions of Emotions: Stimuli and Tests; FEIT, Facial Emotion Identification Test; FEP, First Episode Psychosis; FNE, Fear of Negative Evaluation scale; FPRT, Faux Pas Recognition Task; GPTS, Green Paranoid Thoughts Scale; GSAD, Generalized SAD; IAS, Interaction Anxiousness Scale; ICD-10, International Classification of Diseases 10th edition; IES-R, Impact of Event scale-Revised; IHS, Inventory of Hostility and Suspiciousness; IPSAQ, Internal Personal and Situational Attributions Questionnaire; IRI, Interpersonal Reactivity Index; IRIS, Ideas and Delusions of Reference Interview Scale; IS, Insight Scale; ISMIS, Internalised Stigma of Mental Illness Scale; ISS, Internalised Shame Scale; IUS, Intolerance of Uncertainty Scale; LSAS, Liebowitz Social Anxiety Scale; LSAS-SR, LSAS Self Rating version; MAQ, Multidimensional Anxiety Questionnaire; MAS, Metacognition Assessment Scale; METT, Ekman’s Micro-Expression Training Tool; MSEI, Multidimensional Self-Esteem Inventory; NC, Normal Control; OAS, Other as Shame Scale; PAM, Psychosis Attachment Measure; PANSS, Positive and Negative Syndrome Scale; PBEQ, Personal Beliefs about Experiences Questionnaire; PBIQ, Personal Beliefs about Illness Questionnaire; PEP, Post-Event Processing; PLE, Psychotic-Like Experiences; PS, Paranoia Scale; RAAS, Revised Adult Attachment Scale; RMET, Reading the Mind in the Eyes; RSES, Rosenberg Self-Esteem Scale; SAD, Social Anxiety Disorder; SADS, Social Avoidance and Distress Scale; SANS, Scale for the Assessment of Negative Symptoms; SAPS, Scale for the Assessment of Positive Symptoms; SAQ-R, Social Attitudes Questionnaire Revised; SCQ, Social Cognitions Questionnaire; SCS, Social Comparison Scale; SERS-SF, Self-Esteem Rating Scale-Short Form; SIAS, Social Interaction Anxiety Scale; SIPS, Structured Interview for Prodromal Syndromes; SISST, Social Interaction Self-Statement Test; SPAI, Social Phobia and Anxiety Inventory; SPS, Social Phobia Scale; SPQ, Schizotypal Personality Questionnaire; SSI, Schizotypal Symptoms Inventory Brief Version; SSIT, Simulated Social Interaction Test; SUMD, Scale to Assess Unawareness of Mental Disorder; SZ, SchiZophrenia spectrum disorder; TADS, Trauma And Distress Scale; ToM, Theory of Mind; UHR, Ultra High Risk; VR-CBT, Virtual-Reality-based Cognitive Behavioural Therapy
aScoring as number of quality criteria met; for example, 4**** means 4 criteria (of totally 5) of a study design were met.
bToM test battery includes the Hinting Test, the Bell-Lysaker Emotional Recognition Task, the eyes test, and the Picture arrangement subtest of Wechsler Adult Intelligence Scale III.
Table 3.
Studies Addressing Correlated Factors of Social Anxiety in Psychotic Experiences Contexts
| Citation | Design | Sample Characteristic (N) | Measurements 1. Diagnostic Criteria 2. Symptom Scales |
Correlated Factors | Findings | Quality Criteria Meta | |
|---|---|---|---|---|---|---|---|
| Psychosis | Social Anxiety | ||||||
| Nemoto et al52 | Prospective | SZ (118) | 1. DSM-IV 2. PANSS, CGI-severity scale | 2. LSAS |
Quality of life - WHO-QOL26 Functioning - GAF - SFS Well-being - SWNS |
Regarding a stepwise regression adjusted with demographic data, change in LSAS was significantly associated with change of the outcome models in predicting WHO- QOL26 (β = -0.01, P = .005, adjusted R2 = 0.167), SFS (β = -0.33, P < .001, adjusted R2 = 0.212) and SWNS (β = -0.25, P < .001, adjusted R2 = 0.234). | 4**** |
| Kumazaki et al47 | Prospective | Total 36 SZ+Worsenedb LSAS (12) SZ+Stable LSAS (24) |
1. ICD-10 2. PANSS | 2. LSAS |
Quality of life - WHO-QOL26 Functioning - GAF - SFS |
WHO-QOL26 significantly predicted level of LSAS at follow-up (adjusted 0.85, P < .05, respectively) after controlling baseline of LSAS. PANSS, SFS and GAF were not significantly associated with development of social anxiety. | 4**** |
| Vrbova et al62 | Cross-sectional | Total 61 SZ (42) SZ+SAD (19) |
1. ICD-10 2. PANSS, CGI | 2. LSAS |
Quality of life - Q-LES-Q Personality factors - TCI-R Hopelessness - ADHS |
SZ+SAD reported lower level of Q-LES-Q (t = 4.863, P < .0001) and ADHS (t = 2.710, P < .01) than SZ. SZ+SAD revealed higher level of TCI-R harm avoidance and lower self-directed subscales (t = 4.203, P < .0001 and t = 4.447, P < .0001) than SZ. | 5***** |
| Kwong et al92 | Cross-sectional | SZ (159) | 1. DSM-IV 2. PANSS | 2. LSAS |
Quality of life - SF-36 MCS and PCS subscales |
Total score of LSAS significantly correlated with SF-36 MCS (r/tc = −0.484, P < .001) and PCS (r/t = −0.302, P < .001). | 5***** |
| Lowengrub et al48 | Cross-sectional | Total 50 SZ (31) SZ+SAD (19) |
1. ICD-10 2. PANSS, CGI |
2. LSAS |
Quality of life - SQLS |
Total score of LSAS significantly correlated with SQLS (r = −.47, P < .01). | 4**** |
| Huppert et al49 | Cross-sectional | SZ (32) | 2. PANSS, SAPS, SANS, IHS | 1. DSM-IV, ADIS 2. SIAS, SPS |
Quality of life - QOLI |
Levels of QOLI significantly correlated with level of SPS (r = −.48, P < .01), SIAS (r = −.48, P < .01) and ADIS social phobia (r = −.42, P < .05). | 4**** |
| Blanchard et al41 | Prospective | Total 52 SZ (37) NC (15) |
1. DSM- III-R 2. BPRS | 2. BFNE, IAS |
Well-being - WB Social anhedonia - SAS |
Amongst SZ, level of SAS positively correlated with level of IAS and BFNE (r = .64 and .48), while WB negatively correlated with level of IAS and BFNE (r = −.52 and −.48), all Ps < .005. | 4**** |
| Bipeta et al50 | Cross-sectional | Total 64 SZ (47) SZ+SAD (17) | 1. ICD-10 2. PANSS | 2. SIAS |
Well-being - WHO-5 Functioning - GAF |
SZ+SAD reported lower level of WHO-5 (t = 2.66, P = .01) and GAF (t = 2.1437, P = .036) than SZ. | 4**** |
| Romm et al71 | Cross-sectional | Total 144 FEP (30) FEP+NonGSAD (46) FEP+GSAD (68) |
1. DSM-IV 2. PANSS, IS | 2. LSAS-SR |
Quality of life - QOLI Functioning - GAF - Premorbid adjustment scale |
FEP+GSAD reported lower level of premorbid social functioning, academic functioning, GAF and QOLI (F = 7.62 and 15.13, 12.51 and 10.91, all ps < 0.001) than FEP and FEP+NonGSAD. | 5***** |
| El-Masry et al44 | Cross-sectional | Total 107 SZ (67) SZ+SAD (19) SAD (21) |
1. DSM-IV 2. SAPS, SANS | 2. LSAS |
Quality of life - SF-36 |
SZ+SAD reported lower levels of SF-36 subscales: general health, vitality, social function, role-emotional and mental health than SZ, all ps < 0.05. | 3*** |
| Chudleigh et al42 | Cross-sectional | Total 60 FEP (20) At risk of psychosis (20) NC (20) |
1. CAARMS 2. BPRS | 2. BSPS |
Functioning - SFS - WHODAS |
Amongst FEP, level of SFS: performance and competence of independence subscales correlated with BSPS (r = −.52 and r = −.58), plus level of WHODAS: self-care and getting along with people subscales correlated with level of BSPS (r = .71 and r = .53). All all Ps < .01. | 4**** |
| Voges et al76 | Cross-sectional | SZ (60) | 1. DSM-IV 2. PANSS | 1. DSM-IV 2. SPAI |
Functioning - SFS |
SPAI significantly correlated with SFS (r = −.32, P < .001). | 5***** |
| Pallanti et al10 | Cross-sectional | Total 107 SZ (51) SZ+SAD (29) SAD (27) |
1. DSM-IV 2. SAPS, SANS | 1. DSM-IV 2. LSAS |
Quality of life - SF-36 Functioning - SAS* Suicidality - Suicide behavior (by interview) and the number of lifetime suicide |
SZ+SAD reported lower level of SAS* (F4.85, P < .04), higher number of suicide attempts (F5.19, P < .03) and lethality of suicide attempts (F34.14, P < .001) than SZ. SZ+SAD reported lower level of SF-36: general health, vitality, social functioning, role-emotional and mental health subscales (F1,78 = 8.71, 4.79, 25.41, 9.94 and 8.96; P < .01, P < .05, P < .001, P < .01 and P < .01, respectively) than SZ. | 4**** |
| Aikawa et al90 | Cross-sectional | Total 207 SZ (177) SZ+SAD (30) | 1. DSM-IV 2. PANSS | 1. MINI 2. LSAS |
Functioning - SFS |
Lower level of SFS, female, younger age of onset and longer untreated duration were associated with LSAS (β = -0.42, P < .001, adjusted R2 = 0.255). | 5***** |
| Lecomte et al73 | Cross-sectional | Total 47 SZ (25) SZ+SAD (22) | 1. DSM- IV-TR | 2. BSPS, SIAS |
Functioning - SFS |
SIAS was associated with SFS engaging in conversations subscales (β = -0.61, P < .001, adjusted R2 = 0.35). | 5***** |
| Cacciotti-Saija et al51 | Cross-sectional | SZ (51) | 1. DSM- IV-TR 2. SAPS, SANS |
2. SIAS | Functioning - SFS | SIAS (β = -0.56, P < .001) and SANS (-0.37, P < .01) were associated with SFS (adjusted R2 = 0.66). | 4**** |
| Khaliln et al54 | Cross-sectional | SZ (53) | 1. ICD-9 | 2. U-Scale | Family factors - EMBU - AfS | Level of social anxiety (U-scale) positively correlated with a paternal rejection (P < .005), but not correlated with mother. Those with SZ who scored their key relatives as more critical and hostile attributed to themselves (Afs) reported higher scores on social anxiety dimensions: fear of failure and criticism (P < .01), social contact anxiety (P < .001), inability to refuse (P < .001) and decency (P < .01). | 4**** |
| Michail et al86 | Cross-sectional | Total 135 FEP (60) FEP+SAD (20) SAD (31) NC (24) |
1. ICD-10 2. PANSS | 1. ICD-10 2. SIAS, SPS | Family factors - MOPS Traumatic experiences - CTQ | FEP+SAD and SAD reported higher level of traumatic experiences (CTQ: emotional abuse (F1,97 = 4.8, P < .05) and sexual abuse (F1,97 = 3.7, P < .05)) and dysfunctional parental behaviors (MOPS: paternal indifference (F1,97 = 5.6, P < .05) and paternal abuse (F1,97 = 6.1, P < .05)) than FEP and NC. | 5***** |
| Schutters et al56 | Prospective | General population (2548) | 1. DIA-X⁄M- CIDI | 1. DSM-IV | Personality factors - RSRI - TPQ | Regarding multinomial logistic regression analysis, people having comorbid paranoid with social phobia associated with RSRI behavioral inhibition and TPQ harm/avoidance (Relative Risk = 26.22 and 1.12, all ps < 0.001), when compared to those without a history of social phobia or paranoid symptoms. | 4**** |
| Park et al40 | Cross-sectional | Total 54 SZ (27) NC (27) | 1. DSM- IV-TR 2. PANSS, SAS** |
2. STAI trait anxiety | Anomalous experiences - SAS | SZ reported higher level of STAI than NC in happy condition (t = -5.00, df = 42.7, P < .01). Amongst SZ, STAI correlated with SAS** in happy (r = .56, P < .01) and angry conditions (r = .54, P < .01), and with SAS in happy condition (r = .38, P < .05). | 2** |
| Jang et al39 | Cross-sectional | Total 30 SZ (15) NC (15) |
2. PANSS | 2. STAI state anxiety | Anomalous experiences | Virtual avatar could evoke level of STAI, showing positive correlation between the STAI and PANSS negative subscales: blunted affect (evoked by happy avatar: r = .549, P = .034; and neutral avatar: r = .536, P = .039); and passive/apathetic social withdrawal (happy avatar: r = .536, P = .039; and neutral avatar: r = .658, P = .008). | 3*** |
| Lysaker et al95 | Cross-sectional | Total 71 (All SZ) WCST impaired+no delusions (39) WCST impaired+delusions (11) WCST not impaired+no delusions (15) WCST not impaired+delusions (6) | 1. DSM- III-R 2. PANSS | 2. LSAS, STAI |
Executive functionings - WCST |
Patients having impaired cognitive flexibility with significant delusion group reported higher level of LSAS (F = 4.12, P < .05) than all other groups. Subgroup analysis showed this group reporting higher on LSAS particularly fear subscale (Fisher LSD P < .05). | 5***** |
| Rietdijk et al57 | Prospective | General population (7076) | 1. DSM- III-R 2. CIDI Psychosis section | 2. CIDI Social anxiety section | Subclinical paranoia - CIDI Psychosis section | Of 489 subjects who did have lifetime subclinical paranoid symptoms but no lifetime social phobia at baseline, 23 subjects (4.7%) developed social phobia (OR = 4.07; 95% CI = 2.50–6.63; P < .001). The OR remained significant after controlling for neuroticism (OR = 2.62; 95% CI = 1.57–4.36; P < .001). | 4**** |
| Michail et al11 | Cross-sectional | Total 111 FEP (60) FEP+SAD (20) SAD (31) |
1. ICD-10 2. PANSS, DoT | 1. ICD-10 2. SIAS, SPS, BFNE | Persecutory threat - DoT | FEP+SAD (n = 9/20 (45%)) had higher number of express persecutory threat (DoT) than FEP alone (n = 7/60 (11.6%)), x21 = 10.4, P < .01. | 4**** |
| Lysaker et al94 | Cross-sectional | SZ (143) | 1. DSM-IV 2. PANSS | 2. MAQ social anxiety |
Hopelessness - BHS |
MAQ social anxiety significantly correlated with BHS hope (r = −.44, P < .001). | 5***** |
Note: ADHS, Adult Dispositional Hope Scale; ADIS, Anxiety Disorders Interview Schedule for DSM-IV; AfS, Angehbrigen-Fragebogen fur Schizophrene patienten (assessing for patient’s attitude towards him); BHS, Beck Hopelessness Scale; BFNE, Brief Fear of Negative Evaluation scale; BPRS, Brief Psychiatric Rating Scale; BSPS, Brief Social Phobia Scale; CAARMS, Comprehensive Assessment of At Risk Mental State; CGI, Clinical Global Impression; CIDI, Composite International Diagnostic Interview; CTQ, Childhood Trauma Questionnaire; DIA-X/M-CIDI, Munich-CIDI (a modified CIDI version 1.2); DoT, Details of Threat questionnaire; DSM-III-R, Diagnostic and Statistical Manual of Mental Disorders 3rd edition Revision; DSM-IV, DSM 4th edition; DSM-IV-TR, DSM-IV Total Revision; EMBU, Egna Minnen av Barndoms Uppfostran (assessing for memories of parental behavior); FEP, First Episode Psychosis; GAF, Global Assessment of Functioning scale; GSAD, Generalized SAD; IAS, Interaction Anxiousness Scale; ICD-9, International Classification of Diseases 9th edition; ICD-10, ICD 10th edition; LSAS, Liebowitz Social Anxiety Scale; LSAS-SR, LSAS Self-Rating version; MAQ, Multidimensional Anxiety Questionnaire; MINI, Mini International Neuropsychiatric Interview; MOPS, Measure Of Parental Style; NC, Normal Control; PANSS, Positive and Negative Syndrome Scale; Q-LES-Q, Quality of Life Enjoyment and Satisfaction Questionnaire; QoL, Quality of Life; QOLI, Lehman Quality Of Life Interview; RSRI, Retrospective Self-Report of Inhibition; SAD, Social Anxiety Disorder; SANS, Scale for the Assessment of Negative Symptoms; SAPS, Scale for the Assessment of Positive Symptoms; SAS, Social Anhedonia Scale; SAS*, Social Adjustment Scale score; SAS**, Schizotypal Ambivalence Scale; SF-36, 36-tem Short Form health survey (Mental and Physical Component Summary (MCS and PCS)); SFS, Social Functioning Scale; SIAS, Social Interaction Anxiety Scale; SPAI, Social Phobia and Anxiety Inventory; SPS, Social Phobia Scale; SQLS, Schizophrenia Quality of Life Scale; STAI, State Trait Anxiety Inventory; SWNS, Subjective Well-being under Neuroleptic drug treatment Short form; SZ, SchiZophrenia spectrum disorder; TCI-R, Temperament and Character Inventory-Revised; TPQ, Tridimensional Personality Questionnaire; U-Scale, Unsicherheits-Fragebogen scale (assessing for social anxiety); WB, Well-Being scale; WCST, Wisconsin Card Sorting Test; WHO-5, World Health Organisation-5 Well-Being Index; WHODAS, WHO Disability Assessment Scale II; WHO-QOL26, WHO-Quality of Life 26
a coring as number of quality criteria met; for example, 4**** means 4 criteria (of totally 5) of a study design were met.
bworsened means an LSAS total score a ≥30% increase from baseline.
cr/t means Pearson’s product-mean correlation analyzes and independent t-tests were performed to examine the relationships of SF-36 scores with continuous and categorical variables.
Psychological Factors Maintaining Social Anxiety in the Context of Psychotic Experiences
Psychological factors maintaining social anxiety in people with psychotic experiences contexts were extracted and described (table 2). We divided these factors into 4 main categories: Cognitive, Metacognitive, Behavioral, and Other (supplementary table 6). Generally, the studies related to metacognitive factors revealed inconsistent patterns with social anxiety outcomes, while other factors appeared more consistent.
Cognitive Factors.
The most frequently reported factors were cognitive variables, with the most common being stigma and shame, followed by self-esteem, social rank, and negative self-referent appraisals.
Stigma and Shame
Seven studies focused on stigma and shame.25,58–63 The presence of SAD was significantly associated with higher stigma and external shame amongst patients with First Episode Psychosis (FEP),25,59 and schizophrenia spectrum disorders (SZ).58,62 Amongst FEP, stigma (OR = 1.3, P = .018) and external shame (OR = 1.1, P = .039) were associated with social anxiety after controlling for depression.59 Severity of social anxiety in FEP was significantly associated with childhood trauma; shame memories; traumatic impact from memories; and internal and external shame,63 using the Trauma and Distress Scale; 64 Centrality of Event Scale; 65 Impact of Event Scale-Revised; 66 Internal Shame Scale; 67 and Other as Shamer Scale,68 respectively. A 5-month follow-up study of SZ found that SAD at follow-up was predicted by the Discriminative Experiences of Stigma Scale69 at baseline and negative symptoms (total R2 = 0.46 and 0.42, P < .001).60 Amongst those at risk of psychosis internalized stigma did not predict social anxiety at 6-month follow-up once baseline social anxiety was controlled for.61
Self-esteem
Five studies investigated low self-esteem in people with SAD and paranoia.58,70–73 SZ with SAD was associated with poorer self-esteem than those without SAD.58,73 Amongst FEP with generalized SAD, self-esteem was lower compared to FEP with non-generalized SAD and FEP without SAD.71 Generalized SAD is characterized by a more pervasive fear of most social situations, whereas non-generalized SAD is restricted to more specific situations (eg, a fear of public speaking but no experience of anxiety in casual social gatherings), according to DSM-IV.74 Amongst FEP, SAD was associated with low self-esteem (β = −0.04, P < .001, adjusted R2 = 0.46).70 A prospective study of SZ, SAD at 6-month follow-up was predicted (P < .001) by the level of self-esteem (R2 = 0.06, P < .05) after controlling SAD at baseline.72
Social rank
Three studies investigated how people compare themselves to others focusing on appraisals of social rank.25,59,75 FEP plus SAD25,59 and SZ plus SAD75 reported seeing themselves as having lower social rank compared to people with psychosis alone. Furthermore, FEP plus SAD reported lower social rank than those with only SAD.25
Negative Self-Referent Appraisals
Negative self-referent appraisals were investigated in 4 studies43,76,77 including one qualitative study.78 SZ who had higher social anxiety rated themselves more negatively (r = .74, P < .001), while those with lower social anxiety rated themselves more positively (r = −.37, P < .004).76 SZ (persecutory delusions) and social phobia showed no significant differences in automatic thoughts, underlying assumptions and core beliefs.43 In people with early operationalized psychosis, ideas of reference was found directly related to social anxiety (standardized path coefficient β = 0.26, P = .002), using path analysis.77
A qualitative approach was used to examine interpersonal threat experiences in people with SZ (persecutory delusions) and SAD, between the 2 groups there were 3 major processes including “experience of threat,” “reactions” while under threat, and subsequent “reflections” on threat situations. There were differences found only in the SZ group, which were poor metacognitive awareness in perceptual experiences, inability to stand back from the threat following the event and lack of narrative coherence.78
Metacognitive Factors.
Six studies examined metacognitive factors in social anxiety amongst patients with psychosis. Metacognitive factors included Theory of Mind (ToM); 73,79,80 metacognitive mastery; 81 mentalization; 82 or reasoning biases.46
Starting with ToM findings, compared to FEP, people with SAD alone had higher scores for emotional recognition tasks.80 In another study comparing those with FEP and SAD, there were no significant differences in emotional recognition.80 Comparing SZ and SZ plus SAD there were no differences in emotional recognition.73 In SZ, the level of ToM and paranoia were combined for cluster analysis. Those with SZ in the high-middleToM/paranoia+ group (where paranoia+ refers to significantly higher paranoia than paranoia-) reported greater social anxiety level than other groups (poorestToM/paranoia+; highestToM/paranoia- and low-middleToM/paranoia-).79
With regards to metacognitive mastery,83 (the ability to utilize knowledge of mental states to intentionally manage conflicts and subjective distress), SZ with intermediate levels of mastery reported higher social anxiety than those with low and high mastery group (P < .05).81 When assessed separately for the SZ with or without SAD groups, there were no significant correlations between mentalization and social anxiety.82
Lastly, reasoning biases, including personalizing and externalizing biases were measured amongst 3 groups: SZ, SZ with SAD and normal control. Compared across 3 groups, there were no significant differences levels of personalizing bias. SZ with SAD reported a significantly lower level of externalizing bias than control.46
Behavioral Factors.
Social avoidance has been examined in a single-arm trial using Virtual Reality to deliver a treatment to enhance social skills in SZ. This found improved social anxiety (effect size = 0.48, P < .05) and reduced social avoidance (effect size = 0.58, P < .05) at post-treatment and follow-up, respectively.55
One study investigated post-event processing (PEP)53–a ruminative process occurring after a distressing social event and attempts to reduce the likelihood of negative social consequences.84 In other words, PEP is a covert behavior that functions as a safety behavior preventing disconfirmation of negative social anxiety beliefs. This study included undergraduate students in the game to assess the perception of exclusion, and 2 confederates as additional participants to act and lead participants believing that they were excluded.53 The game was preset so that in the first 5 passes the participant received the ball twice, then the 2 confederates chose to toss the ball to each other for the duration of the game–the participant was socially excluded. PEP, SIAS and GPTS-PP were measured at pre- and post-social exclusion intervention, and 24-hour and 1-week followed-up. It was found that higher levels of social anxiety and paranoia predicted the higher PEP after the intervention (SIAS: B = 0.36, P < .001 and GPTS-PP: B = 0.16, P < .05) and 1-week later (SIAS: B = 0.09, P < .05 and GPTS-PP: B = 0.09, P < .05).
Other Maintenance Factors.
Other factors maintaining social anxiety in psychosis were examined, including attachment,45,85,86 empathy87 and intolerance of uncertainty.88
Three studies examined self-reported attachment. FEP plus SAD or SAD alone reported better adult attachment than those with FEP and normal controls.86 Amongst ultra-high risk (UHR) participants, an insecure adult attachment was associated with social anxiety using SIAS (β = 0.47, P < .001, R2 = 0.22) and SPS (β = 0.39, P < .01, R2 = 0.15) and the relationship between adult attachment and SIAS was mediated by depression.85 However, amongst people with UHR, there were no significant correlations between social anxiety and insecure anxious attachment, or avoidant attachment.45
Empathy was reported using the Interpersonal Reactivity Index,89 consisting of cognitive (perspective taking and fantasy scales) and affective components (empathic concern and personal distress scales). Amongst FEP, the lower perspective-taking of empathy scale was associated with higher social anxiety (r = −.51, P = .004). Other empathy scales were not associated with social anxiety.87
People with Psychotic-Like Experiences (PLE) with SAD reported higher Intolerance of Uncertainty (IU) than those with SAD alone and healthy controls (P < .001).88
Correlates of Social Anxiety
Correlates were categorized into 7 groups: functioning, QoL, well-being, family factors, personality factors, anomalous experiences and others (subclinical paranoia, persecutory threat, traumatic experiences, suicidality and hopelessness, social anhedonia and executive functioning; see table 3). Evidence related to correlates of social anxiety generally showed consistent findings, associations with functioning and QoL/well-being were commonly investigated compared to others.
Functioning.
Ten studies reported on SAD and functioning across psychosis groups.10,42,47,50–52,71,73,76,90 FEP plus generalized SAD reported a lower level of premorbid social functioning and daily functioning compared to FEP plus non-generalized SAD or FEP alone.71 In SZ, those with SAD returned lower functioning scores than SZ alone.10,50 The lower level of Social Functioning Scale (SFS)91 was related to the greater social anxiety amongst FEP,42 and SZ.76 Furthermore, in SZ the lower SFS was associated with the higher social anxiety in a cross-sectional study (β = -0.42, P < .001, adjusted R2 = 0.255)90 and a longitudinal study (β = -0.33, P < .001, adjusted R2 = 0.212).52 Lower social anxiety was associated with the higher SFS (β = -0.56, P < .001, adjusted R2 = 0.66)51 and SFS Engaging in conversations subscale (β = -0.61, P < .001, adjusted R2 = 0.35).73 A prospective study of SZ reported that higher level of SFS was not associated with worsening social anxiety at 5-year follow-up, the development of worsened of social anxiety defined by an LSAS score ≥30% from the baseline value.47
Quality of Life and Well-Being.
Nine studies examined QoL related to SAD with psychosis.10,44,47–49,52,62,71,92 In FEP, those with generalized SAD reported lower QoL than FEP with nongeneralized SAD or FEP alone.71 Amongst SZ, those with SAD significantly reported lower QoL than those with SZ alone.10,44,62 Additionally, a higher severity of social anxiety was associated with a lower level of QoL.48,49,92 In prospective studies of SZ, higher social anxiety was associated with lower QoL (β = -0.01, P = .005, adjusted R2 = 0.167),52 and lower QoL predicted increased social anxiety at 5-year follow-up (adjusted OR 0.85, P < .05) after adjusting the baseline social anxiety.47
When QOL is conceptualized as the broader notion of well-being, those with SZ and SAD had significantly lower well-being compared to those without SAD.50 Also, amongst SZ higher SAD was associated with lower well-being,41 and the higher social anxiety was prospectively associated with the lower patients’ well-being (β = -0.25, P < .001, adjusted R2 = 0.234).52
Family Factors.
A study of FEP found that parental rearing style reported by those with SAD (FEP plus SAD or SAD alone) revealed higher dysfunctional paternal indifference (F1,97 = 5.6, P < .05) and abuse (F1,97 = 6.1, P < .05) than those without SAD (FEP alone and normal control).86 Furthermore, higher social anxiety in SZ was significantly associated with the higher paternal rejection, but not maternal rejection. Those with SZ who scored their key relatives (eg, spouse, father or mother) as more critical and hostile towards themselves reported higher scores on social anxiety.54
Temperament and Personality Factors.
In an analogue study, general population were interviewed using Munich-Composite International Diagnostic Interview (M-CIDI)93 to define any/subclinical/clinical paranoid or phobia symptoms. They were then observed prospectively including completed temperamental and personality measurements. Lifetime comorbid condition (paranoia and social phobia symptoms) was associated with behavioral inhibition temperament (Relative Risk = 26.22, P < .001) and harm avoidance personality (Relative Risk = 1.12, P < .001) compared to individuals without a history of social phobia or paranoid symptoms.56 In SZ, those with SAD had higher harm avoidance and lowered self-directed personality than those without SAD (t = 4.203, P < .0001 and t = 4.447, P < .0001).62
Anomalous Experiences.
Two virtual reality studies examined perceptual disturbances in SZ.39,40 The first study provided avatars with happy and neutral face conditions to evoke patients’ social anxiety. Amongst SZ higher social anxiety was correlated with higher PANSS negative subscales: blunted affect and passive/apathetic social withdrawal, when evoked by happy (r = .55, P = .034 and r = .54, P = .039) or neutral faces (r = .54, P = .039 and r = .66, P = .008), respectively.39 Another avatar study in SZ reported higher social anxiety in the happy condition, compared to normal controls (t = −5.00, P < .01). In SZ group, the higher social anxiety was related to the higher schizotypal ambivalence (r = .56, P < .01) and social anhedonia scores (r = .38, P < .05) when evoked by happy conditions, and related to the higher schizotypal ambivalence scores (r = .54, P < .01) when evoked by angry conditions.40
Other Factors.
In a general population prospective study, subclinical paranoid symptoms were a predictor of the development of social phobia, controlling for neuroticism (OR = 2.62; 95%CI = 1.57–4.36; P < .001).57Amongst FEP, those with SAD expressed more persecutory threat than those with FEP alone.11 Considering reported traumatic experiences, people with SAD (FEP plus SAD or SAD alone) reported higher emotional abuse (F1,97 = 4.8, P < .05) and sexual abuse (F1,97 = 3.7, P < .05) than those without SAD (FEP alone and normal controls).86
Regarding suicidality and hopelessness, those with SZ and SAD reported a higher number of suicide attempts (F5.19, P < .03) and lethality of suicide attempts (F34.14, P < .001) compared to SZ alone.10 SZ with SAD reported lower hope than those without SAD (t = 2.710, P < .01),62 and the lower hope was associated with higher social anxiety (r = −.44, P < .001).94Social anhedonia was investigated in SZ, where greater social anhedonia correlated with higher social anxiety.41
SZ were investigated for executive functioning, delusion severity and social anxiety. SZ who had impaired cognitive flexibility plus a significant delusion (PANSS Delusions Score≥5) reported higher social anxiety (LSAS: F = 4.12, P < .05) than other groups (impaired cognitive flexibility plus no delusion, not impaired plus no delusion, not impaired plus delusion).95
Discussion
This review sought to identify, describe, and critically analyze candidate factors that maintain social anxiety in people experiencing psychosis. We synthesized the data using interventionist-casual model criteria that stipulate the candidate factors should be: (1) measurable; (2) amenable to change in a putative casual process; and (3) theoretically relevant. We also justified the factors and developed an integrated-theoretical model for improvement of targeted treatment of SAD with psychosis.
Psychological Maintenance Factors
We identified a number of factors from the eligible studies included in the current review. We clustered the findings according to Cognitive, Metacognitive and Behavioral factors. Amongst people with psychosis or schizophrenia who had an additional diagnosis of SAD, there were higher levels of perceived stigma and shame, lower levels of self-esteem and social rank and more negative self-appraisals. These findings were derived from high quality studies.
Although there were identified metacognitive factors including ToM, metacognitive mastery, mentalization and reasoning biases, not all relationships between social anxiety and metacognition were linear. This is perhaps because those people with a lower level of metacognition might not be aware of a socially feared event, while those with higher level might have a better adaptation to deal with problems with social anxiety, resulting in reduced severity, when compared to those with a moderate level.79,81 It was evidenced that metacognitive beliefs were found to empirically contribute to social anxiety,96 and metacognitive processes of people with psychosis can be changed in an experimental study.97 Though there is promising evidence, findings on metacognitive factors were mixed and synthesis of these findings is made difficult by different approaches to the definition and measurement of metacognition.
We found limited evidence that behavioral factors have been systematically investigated. This is a neglected area of research and our findings show promise in delineating the role of social avoidance and other defensive behaviors (ie, PEP) in the maintenance of social anxiety. Because safety behaviors, such as social avoidance play a role in maintaining social anxiety,84 then intervention on these factors should reduce social anxiety experiences in psychotic contexts.
Importantly, although largely findings were drawn from cross-sectional studies, we found consistent evidence for the potential role of cognitive factors, which the candidate factors can be the stigma and shame. Because they fit with the substantial characteristics of potential mechanism in the interventionist-causal approach,27 which the stigma and shame were measurable67,68,98 and can be developed in the theoretical understanding to guide therapy.59 Furthermore, these factors are likely to be amenable to change with psychological interventions targeting these factors as a causal mechanism. Therefore, cognitive factors such as appraisals of stigma and shame may be amenable for the development of interventionist-causal approaches to SAD in psychosis.
Correlates of Social Anxiety in Psychosis
Social anxiety was frequently associated with 2 correlates including poorer functioning and lower QoL, followed by lower well-being, family factors and personality factors, anomalous experiences, and other correlates presented in the result section. From our review, lower functioning was consistently associated with higher social anxiety amongst people with psychosis. The poor functioning also influences the defeatist performance belief (DPB),99 which is overgeneralized negative thoughts about one’s ability to successfully perform tasks. This DPB is important because it can lead to preventing the initiation of goal-directed behaviors and engagement in social interactions.99 We also commonly found that higher social anxiety was related to poorer QoL and well-being. It is evident that lower QoL and lower well-being was associated with higher symptoms of psychosis.100,101 Notably we found consistent evidence that social anxiety was correlated with poorer functioning and QoL. It is important that functioning and QoL should be included as outcomes in future intervention studies targeting SAD in psychosis.52,102
Integration of Theoretical Model and its Implication
Based on our findings we propose a theoretical integration as shown in figure 2, based on previous work on social anxiety; 84,103 paranoia; 32 and stigma.59
Fig. 2.
The cognition model processing of social anxiety to severe threat. Note: the gradient shading box shows the intensity continuum of social anxiety to paranoia; the darker color the more paranoia, as followed: Perceived self as ridiculed/embarrassment (eg, I look awkward/sick); Ideas of reference (eg, people talking about me); Mild threat and harm from others (eg, people trying to cause minor distress, such as irritation); Moderate threat and harm (eg, people deliberately trying to approach me, such as being hostile towards me); and Severe threat and harm (eg, people trying to cause significant physical psychological or social harm).
Three major processes of the model were constructed. We will use stigma and shame to explain the model. With the proximal social assumptions, individuals with bio-psycho-social vulnerabilities are, firstly, aware that other people are critical when encountering feared social situation. Due to negative processing the self as a social object, individuals may feel different, vulnerable or stigmatized, the internalized negative self-representation is formed.
Secondly, activation of the internalized self-representations, are then subject to metacognitive processing. The individual with internal stigma- and shame-based representations may perceive their self as ridiculed (eg, I look awkward), or at risk of social harm from others (eg, others are threatening). One can perceive threat at different level consistent with the hierarchy model (see the shading box in figure 2).32 Then, their perceived assumptions will be assessed relating to: social attitudes, called other-to-self focus (eg, neighbors disgust people like me); and self-image, called self-to-self focus (eg, I am indeed despicable).
Lastly, negative appraisals about stigma and shame result in defensive behaviors (eg, avoiding eye contact), and cognitive (eg, hypervigilance due to anticipating other attitudes) and physical symptoms (eg, sweating, tremor) of anxiety. These symptoms interact in vicious circles via PEP. These defensive behaviors also maintain and prevent disconfirmation of the negative belief of social anxiety in psychosis. Negative consequences may appear as poorer daily functioning, QoL, well-being, and increased hopelessness and suicidality. Additionally, although negative affect can be a negative consequence, nonetheless, it was not included in the model, because negative affect also increases accessibility of negative appraisals and feelings of stigma/shame that, in turn, increases social anxiety.
Our model aims to help people suffering from social anxiety in the context of psychosis. Although the psychological factors related to experiencing discrimination (stigma/shame) are not unique to SAD in psychosis, these factors are very relevant in SAD in psychosis compared to the established cognitive model of social anxiety.84 Due to our findings being drawn mostly from cross-sectional studies with limited evidence of experimental and manipulationist tests, additional studies will be needed to develop better effective treatment of SAD in psychosis. Stigma and shame should be tested in interventionist-causal manipulation designs, using social anxiety as the dependent variable and stigma/shame as the mediator variables.
Strengths and Limitations
This review has a number of strengths. The factors that maintain significant social anxiety problems in psychosis and other relevant correlates were thoroughly examined. We used rigorous methods (eg, independent study selection), took a broad and inclusive approach, and assessed the quality of the literature. But there are also limitations to be considered. We did not include non-English-language studies and unpublished gray literature which may have resulted in publication bias and exclusion of some relevant evidence. However, we believe this limitation is minimal as we utilized a comprehensive literature searching and covered studies from diverse geographical regions (Africa, Asia-Pacific, North America, and Europe). Secondly, the quality assessment, indicates that many studies did not address confounding factors and may not have proven the validity/reliability of study measures. This could lead to erroneous conclusions104 and minimize trustworthiness105 of a study. Majority of studies, nonetheless, were met at least 4**** (of 5*****) quality criteria. We observed a gender disparity across studies with men over-represented in the psychosis samples. In contrast, the general population and high-risk samples showed comparable proportions of male and female participants. Lastly, the heterogeneity of data prevented us from applying meta-analysis.
Directions for Future Research
Most studies were cross-sectional and conducted with Westernized English-speaking populations. Cross-cultural studies are required to improve understanding of the role that culture plays in the experience of stigma and the expression of psychopathology.106 It is already known that the content of persecutory delusion is likely to depend on culturally prevalent threats or beliefs about malevolent influence107,108 and so it is relevant to examine whether these effects extend to social anxiety related beliefs and appraisals. The development of experimental designs using interventionist-causal methods with targeted factor and focus whether modifying safety behaviors associated with reducing social anxiety in psychosis should be tested. Moreover, due to lack of evidence on other psychotic experiences, given the potential impact of psychotic experiences; for example, voices in social interactions,109 this also seems to be an important topic for exploration.
Conclusion
Our analysis of the literature suggest that stigma and shame are key candidate psychological mechanisms with a strong role in maintaining social anxiety in the context of psychosis. Given the generally strong methodological quality of the included studies we can be reasonably confident that these cognitive factors warrant further investigation. For example, further studies using psychometrically robust methods and applying mediation analyses will help disentangle the different factors involved the spectrum of problems from social anxiety to paranoia. Both stigma and shame meet the criteria for being treated as relevant factors in an interventionist-causal model that we offer. This clinical model could be used as a basis for treatment development. Given that social anxiety was reliably associated with poorer functioning and QoL there is an important clinical need to improve targeted treatments for these problems.
Supplementary Material
Supplementary material is available at Schizophrenia Bulletin online.
References 138 to 167 are cited in supplementary table 3.
Acknowledgments
The authors thank our reviewer team for collaboration in various parts of this project. The authors have declared that there are no conflicts of interest in relation to the subject of this study.
Funding
This study was conducted primarily by W.A. as part of a PhD program supervised by H.M. and A.G., under funding from Faculty of Medicine, Prince of Songkla University, Thailand.
References
- 1.Rietdijk J, Ising HK, Dragt S, et al. . Depression and social anxiety in help-seeking patients with an ultra-high risk for developing psychosis. Psychiatry Res. 2013;209(3):309–313. [DOI] [PubMed] [Google Scholar]
- 2.Lim J, Rekhi G, Rapisarda A, et al. . Impact of psychiatric comorbidity in individuals at ultra high risk of psychosis - findings from the Longitudinal Youth at Risk Study (LYRIKS). Schizophr Res. 2015;164(1-3):8–14. [DOI] [PubMed] [Google Scholar]
- 3.Hui C, Morcillo C, Russo DA, et al. . Psychiatric morbidity, functioning and quality of life in young people at clinical high risk for psychosis. Schizophr Res. 2013;148(1-3):175–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McEnery C, Lim MH, Tremain H, Knowles A, Alvarez-Jimenez M. Prevalence rate of social anxiety disorder in individuals with a psychotic disorder: a systematic review and meta-analysis. Schizophr Res. 2019;208:25–33. [DOI] [PubMed] [Google Scholar]
- 5.Heimberg RG, Hofmann SG, Liebowitz MR, et al. . Social anxiety disorder in DSM-5. Depress Anxiety. 2014;31(6):472–479. [DOI] [PubMed] [Google Scholar]
- 6.Wittchen HU, Fehm L. Epidemiology, patterns of comorbidity, and associated disabilities of social phobia. Psychiatr Clin North Am. 2001;24(4):617–641. [DOI] [PubMed] [Google Scholar]
- 7.Agid O, McDonald K, Siu C, et al. . Happiness in first-episode schizophrenia. Schizophr Res. 2012;141(1):98–103. [DOI] [PubMed] [Google Scholar]
- 8.Karatzias T, Gumley A, Power K, O’Grady M. Illness appraisals and self-esteem as correlates of anxiety and affective comorbid disorders in schizophrenia. Compr Psychiatry. 2007;48(4):371–375. [DOI] [PubMed] [Google Scholar]
- 9.Vrbova K, Prasko J, Ociskova M, et al. . Quality of life, self-stigma, and hope in schizophrenia spectrum disorders: a cross-sectional study. Neuropsychiatr Dis Treat. 2017;13:567–576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pallanti S, Quercioli L, Hollander E. Social anxiety in outpatients with schizophrenia: a relevant cause of disability. Am J Psychiatry. 2004;161(1):53–58. [DOI] [PubMed] [Google Scholar]
- 11.Michail M, Birchwood M. Social anxiety disorder in first-episode psychosis: incidence, phenomenology and relationship with paranoia. Br J Psychiatry. 2009;195(3):234–241. [DOI] [PubMed] [Google Scholar]
- 12.Michail M, Birchwood M, Tait L. Systematic review of cognitive-behavioural therapy for social anxiety disorder in psychosis. Brain Sci. 2017;7(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kuipers E, Garety P, Fowler D, et al. . London-East Anglia randomised controlled trial of cognitive-behavioural therapy for psychosis. I: effects of the treatment phase. Br J Psychiatry. 1997;171:319–327. [DOI] [PubMed] [Google Scholar]
- 14.National Collaborating Centre for Mental Health. Psychological therapy and psychosocial interventions. In: The NICE Guideline on Treatment and Management Updated Edition 2014. Psychosis and Schizophrenia in Adults: Treatment and Management. London, UK: National Institute for Health and Care Excellence; 2014:208–300. [Google Scholar]
- 15.Sensky T, Turkington D, Kingdon D, et al. . A randomized controlled trial of cognitive-behavioral therapy for persistent symptoms in schizophrenia resistant to medication. Arch Gen Psychiatry. 2000;57(2):165–172. [DOI] [PubMed] [Google Scholar]
- 16.Lewis S, Tarrier N, Haddock G, et al. . Randomised controlled trial of cognitive-behavioural therapy in early schizophrenia: acute-phase outcomes. Br J Psychiatry Suppl. 2002;43:s91–s97. [DOI] [PubMed] [Google Scholar]
- 17.Bechdolf A, Knost B, Kuntermann C, et al. . A randomized comparison of group cognitive-behavioural therapy and group psychoeducation in patients with schizophrenia. Acta Psychiatr Scand. 2004;110(1):21–28. [DOI] [PubMed] [Google Scholar]
- 18.Garety PA, Fowler DG, Freeman D, Bebbington P, Dunn G, Kuipers E. Cognitive–behavioural therapy and family intervention for relapse prevention and symptom reduction in psychosis: randomised controlled trial. Br J Psychiatry. 2008;192(6):412–423. [DOI] [PubMed] [Google Scholar]
- 19.Klingberg S, Wölwer W, Engel C, et al. . Negative symptoms of schizophrenia as primary target of cognitive behavioral therapy: results of the randomized clinical TONES study. Schizophr Bull. 2011;37 Suppl 2:S98–110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stafford MR, Jackson H, Mayo-Wilson E, Morrison AP, Kendall T. Early interventions to prevent psychosis: systematic review and meta-analysis. BMJ. 2013;346:f185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bird V, Premkumar P, Kendall T, Whittington C, Mitchell J, Kuipers E. Early intervention services, cognitive-behavioural therapy and family intervention in early psychosis: systematic review. Br J Psychiatry. 2010;197(5):350–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mayo-Wilson E, Dias S, Mavranezouli I, et al. . Psychological and pharmacological interventions for social anxiety disorder in adults: a systematic review and network meta-analysis. Lancet Psychiatry. 2014;1(5):368–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Acarturk C, Cuijpers P, van Straten A, de Graaf R. Psychological treatment of social anxiety disorder: a meta-analysis. Psychol Med. 2009;39(2):241–254. [DOI] [PubMed] [Google Scholar]
- 24.National Collaborating Centre for Mental Health (UK). Social Anxiety Disorder: Recognition, Assessment and Treatment. Leicester (UK): British Psychological Society. Available at: https://www.ncbi.nlm.nih.gov/books/NBK327654/. [PubMed] [Google Scholar]
- 25.Michail M, Birchwood M. Social anxiety disorder and shame cognitions in psychosis. Psychol Med. 2013;43(1):133–142. [DOI] [PubMed] [Google Scholar]
- 26.Wykes T, Steel C, Everitt B, Tarrier N. Cognitive behavior therapy for schizophrenia: effect sizes, clinical models, and methodological rigor. Schizophr Bull. 2008;34(3):523–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kendler KS, Campbell J. Interventionist causal models in psychiatry: repositioning the mind-body problem. Psychol Med. 2009;39(6):881–887. [DOI] [PubMed] [Google Scholar]
- 28.Beller EM, Glasziou PP, Altman DG, et al. ; PRISMA for Abstracts Group . PRISMA for Abstracts: reporting systematic reviews in journal and conference abstracts. PLoS Med. 2013;10(4):e1001419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hong QN, Pluye P, Fàbregues S, et al. . Mixed Methods Appraisal Tool (MMAT), version 2018. Canadian Intellectual Property Office: Industry Canada; 2018. [Google Scholar]
- 30.Hong QN, Gonzalez-Reyes A, Pluye P. Improving the usefulness of a tool for appraising the quality of qualitative, quantitative and mixed methods studies, the Mixed Methods Appraisal Tool (MMAT). J Eval Clin Pract. 2018;24(3):459–467. [DOI] [PubMed] [Google Scholar]
- 31.van Os J, Reininghaus U. Psychosis as a transdiagnostic and extended phenotype in the general population. World Psychiatry. 2016;15(2):118–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Freeman D, Garety PA, Bebbington PE, et al. . Psychological investigation of the structure of paranoia in a non-clinical population. Br J Psychiatry. 2005;186:427–435. [DOI] [PubMed] [Google Scholar]
- 33.Unterrassner L, Wyss TA, Wotruba D, Haker H, Rössler W. The intricate relationship between psychotic-like experiences and associated subclinical symptoms in healthy individuals. Front Psychol. 2017;8:1537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Liebowitz MR. Social phobia. Mod Probl Pharmacopsychiatry. 1987;22:141–173. [DOI] [PubMed] [Google Scholar]
- 35.Mattick RP, Clarke JC. Development and validation of measures of social phobia scrutiny fear and social interaction anxiety. Behav Res Ther. 1998;36(4):455–470. [DOI] [PubMed] [Google Scholar]
- 36.Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. [DOI] [PubMed] [Google Scholar]
- 37.Andreasen N.Scale for the Assessment of Positive Symptoms (SAPS). Iowa City: University of Iowa; 1984. [Google Scholar]
- 38.Andreasen N.Scale for the Assessment of Negative Symptoms (SANS). Iowa City: University of Iowa; 1983. [Google Scholar]
- 39.Jang HJ, Ku J, Park SH, et al. . Investigation of social anxiety of patients with schizophrenia using virtual avatar. Annu Rev CyberTherapy Telemed. 2005;3:129–134. [Google Scholar]
- 40.Park IH, Kim JJ, Ku J, et al. . Characteristics of social anxiety from virtual interpersonal interactions in patients with schizophrenia. Psychiatry. 2009;72(1):79–93. [DOI] [PubMed] [Google Scholar]
- 41.Blanchard JJ, Mueser KT, Bellack AS. Anhedonia, positive and negative affect, and social functioning in schizophrenia. Schizophr Bull. 1998;24(3):413–424. [DOI] [PubMed] [Google Scholar]
- 42.Chudleigh C, Naismith SL, Blaszczynski A, Hermens DF, Hodge MA, Hickie IB. How does social functioning in the early stages of psychosis relate to depression and social anxiety? Early Interv Psychiatry. 2011;5(3):224–232. [DOI] [PubMed] [Google Scholar]
- 43.Newman Taylor K, Stopa L. The fear of others: a pilot study of social anxiety processes in paranoia. Behav Cogn Psychother. 2013;41(1):66–88. [DOI] [PubMed] [Google Scholar]
- 44.El Masry N, Abdel Fattah N, Fouad A. Comorbidity of Social Phobia in a Sample of Out-patients with Schizophrenia. Curr Psychiatry [Egypt]. 2009;16(4):397–402. [Google Scholar]
- 45.Russo DA, Stochl J, Hodgekins J, et al. . Attachment styles and clinical correlates in people at ultra high risk for psychosis. Br J Psychol. 2018;109(1):45–62. [DOI] [PubMed] [Google Scholar]
- 46.Achim AM, Sutliff S, Samson C, Montreuil TC, Lecomte T. Attribution bias and social anxiety in schizophrenia. Schizophr Res Cogn. 2016;4:1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kumazaki H, Kobayashi H, Niimura H, et al. . Lower subjective quality of life and the development of social anxiety symptoms after the discharge of elderly patients with remitted schizophrenia: a 5-year longitudinal study. Compr Psychiatry. 2012;53(7):946–951. [DOI] [PubMed] [Google Scholar]
- 48.Lowengrub KM, Stryjer R, Birger M, Iancu I. Social anxiety disorder comorbid with Schizophrenia: The importance of screening for this under recognized and under treated condition. Isr J Psychiatry Relat Sci. 2015;52(1): 40–45. [PubMed] [Google Scholar]
- 49.Huppert JD, Smith TE. Anxiety and schizophrenia: the interaction of subtypes of anxiety and psychotic symptoms. CNS Spectr. 2005;10(9):721–731. [DOI] [PubMed] [Google Scholar]
- 50.Rajshekhar B, Srinivasa YSRR, Ram L, Majeed KA. Social anxiety disorder co-morbid with schizophrenia: a cross-sectional study from India. Int J Med Res Rev. 2016;4(11):1953–1957. [Google Scholar]
- 51.Cacciotti-Saija C, Langdon R, Ward PB, Hickie IB, Guastella AJ. Clinical symptoms predict concurrent social and global functioning in an early psychosis sample. Early Interv Psychiatry. 2018;12(2):177–184. [DOI] [PubMed] [Google Scholar]
- 52.Nemoto T, Uchino T, Aikawa S, et al. . Impact of changes in social anxiety on social functioning and quality of life in outpatients with schizophrenia: A naturalistic longitudinal study. J Psychiatr Res. 2020;131:15–21. [DOI] [PubMed] [Google Scholar]
- 53.Piccirillo ML, Heimberg RG. Dealing with rejection: post-event processing in social anxiety and paranoia. J Exp Psychopathol. 2016;7(4):549–563. [Google Scholar]
- 54.Khalil N, Stark FM. Do perceived parental rearing patterns influence social behaviour dimensions and disease severity in schizophrenia? Acta Psychiatr Scand. 1992;86(2):146–152. [DOI] [PubMed] [Google Scholar]
- 55.Rus-Calafell M, Gutiérrez-Maldonado J, Ribas-Sabaté J. A virtual reality-integrated program for improving social skills in patients with schizophrenia: a pilot study. J Behav Ther Exp Psychiatry. 2014;45(1):81–89. [DOI] [PubMed] [Google Scholar]
- 56.Schutters SI, Dominguez MD, Knappe S, et al. . The association between social phobia, social anxiety cognitions and paranoid symptoms. Acta Psychiatr Scand. 2012;125(3):213–227. [DOI] [PubMed] [Google Scholar]
- 57.Rietdijk J, van Os J, de Graaf R, Delespaul P, van der Gaag M. Are social phobia and paranoia related, and which comes first? Psychosis. 2009;1(1):29–38. [Google Scholar]
- 58.Gumley A, O’grady M, Power K, Schwannauer M. Negative beliefs about self and illness: a comparison of individuals with psychosis with or without comorbid social anxiety disorder. Aust N Z J Psychiatry. 2004;38(11-12):960–964. [DOI] [PubMed] [Google Scholar]
- 59.Birchwood M, Trower P, Brunet K, Gilbert P, Iqbal Z, Jackson C. Social anxiety and the shame of psychosis: a study in first episode psychosis. Behav Res Ther. 2007;45(5):1025–1037. [DOI] [PubMed] [Google Scholar]
- 60.Lysaker PH, Yanos PT, Outcalt J, Roe D. Association of stigma, self-esteem, and symptoms with concurrent and prospective assessment of social anxiety in schizophrenia. Clin Schizophr Relat Psychoses. 2010;4(1):41–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pyle M, Stewart SL, French P, et al. . Internalized stigma, emotional dysfunction and unusual experiences in young people at risk of psychosis. Early Interv Psychiatry. 2015;9(2):133–140. [DOI] [PubMed] [Google Scholar]
- 62.Vrbova K, Prasko J, Ociskova M, Holubova M. Comorbidity of schizophrenia and social phobia - impact on quality of life, hope, and personality traits: a cross sectional study. Neuropsychiatr Dis Treat. 2017;13:2073–2083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Aherne K.The role of childhood trauma and shame in social anxiety and paranoia within an early intervention in psychosis population [Clin.Psy.D. thesis.]. UK: Clinical Psychology, University of Birmingham; 2014. [Google Scholar]
- 64.Patterson P, Skeate A, Schultze-Lutter F, et al. . The Trauma and Distress Scale. Birmingham, UK: University of Birmingham; 2002. [Google Scholar]
- 65.Berntsen D, Rubin DC. The centrality of event scale: a measure of integrating a trauma into one’s identity and its relation to post-traumatic stress disorder symptoms. Behav Res Ther. 2006;44(2):219–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wilson JP, Keane TM.. Assessing Psychological Trauma and PTSD: A Handbook for Practitioners. New York: Guilford; 1997. [Google Scholar]
- 67.Cook DR.The Internalised Shame Scale: Professional Manual. Menomonie, WI: Channel Press; 1994. [Google Scholar]
- 68.Goss K, Gilbert P, Allan S. An exploration of shame measures: I: the other as shamer scale. Pers Individ Dif. 1994;17:713–717. [Google Scholar]
- 69.Ritsher JB, Otilingam PG, Grajales M. Internalized stigma of mental illness: psychometric properties of a new measure. Psychiatry Res. 2003;121(1):31–49. [DOI] [PubMed] [Google Scholar]
- 70.Romm KL, Rossberg JI, Berg AO, Hansen CF, Andreassen OA, Melle I. Assessment of social anxiety in first episode psychosis using the Liebowitz Social Anxiety scale as a self-report measure. Eur Psychiatry. 2011;26(2):115–121. [DOI] [PubMed] [Google Scholar]
- 71.Romm KL, Melle I, Thoresen C, Andreassen OA, Rossberg JI. Severe social anxiety in early psychosis is associated with poor premorbid functioning, depression, and reduced quality of life. Compr Psychiatry. 2012;53(5):434–440. [DOI] [PubMed] [Google Scholar]
- 72.Lysaker PH, Ringer JM, Davis LW. Associations of social anxiety and self-esteem across six months for persons living with schizophrenia spectrum disorders. Psychiatr Rehabil J. 2008;32(2):132–134. [DOI] [PubMed] [Google Scholar]
- 73.Lecomte T, Théroux L, Paquin K, Potvin S, Achim A. Can Social Anxiety impact facial emotion recognition in Schizophrenia? J Nerv Ment Dis. 2019;207(3):140–144. [DOI] [PubMed] [Google Scholar]
- 74.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders DSM IV. 4th ed.Washington, DC: American Psychiatric Association; 1994. [Google Scholar]
- 75.Sutliff S, Roy MA, Achim AM. Social anxiety disorder in recent onset schizophrenia spectrum disorders: The relation with symptomatology, anxiety, and social rank. Psychiatry Res. 2015;227(1):39–45. [DOI] [PubMed] [Google Scholar]
- 76.Voges M, Addington J. The association between social anxiety and social functioning in first episode psychosis. Schizophr Res. 2005;76(2-3):287–292. [DOI] [PubMed] [Google Scholar]
- 77.Wong GH. Social anxiety within a network of mild delusional ideations, negative symptoms and insight in outpatients with early psychosis: A psychopathological path analysis. Anxiety Stress Coping. 2020;33(3):342–354. [DOI] [PubMed] [Google Scholar]
- 78.Stopa L, Denton R, Wingfield M, Taylor KN. The fear of others: a qualitative analysis of interpersonal threat in social phobia and paranoia. Behav Cogn Psychother. 2013;41(2):188–209. [DOI] [PubMed] [Google Scholar]
- 79.Lysaker PH, Salvatore G, Grant ML, et al. . Deficits in theory of mind and social anxiety as independent paths to paranoid features in schizophrenia. Schizophr Res. 2010;124(1-3):81–85. [DOI] [PubMed] [Google Scholar]
- 80.Pepper KL, Demetriou EA, Park SH, et al. . Autism, early psychosis, and social anxiety disorder: understanding the role of social cognition and its relationship to disability in young adults with disorders characterized by social impairments. Transl Psychiatry. 2018;8(1):233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Lysaker PH, Erickson M, Ringer J, et al. . Metacognition in schizophrenia: the relationship of mastery to coping, insight, self-esteem, social anxiety, and various facets of neurocognition. Br J Clin Psychol. 2011;50(4):412–424. [DOI] [PubMed] [Google Scholar]
- 82.Achim AM, Ouellet R, Lavoie MA, Vallières C, Jackson PL, Roy MA. Impact of social anxiety on social cognition and functioning in patients with recent-onset schizophrenia spectrum disorders. Schizophr Res. 2013;145(1-3):75–81. [DOI] [PubMed] [Google Scholar]
- 83.Semerari A, Carcione A, Dimaggio G, et al. . How to evaluate metacognitive function in psychotherapy? The metacognition assessment scale its applications. Clin Psychol Psychother. 2003;10:238–261. [Google Scholar]
- 84.Clark DM, Wells A.. A Cognitive Model of Social Phobia. New York: Guilford Press; 1995. [Google Scholar]
- 85.Gajwani R, Patterson P, Birchwood M. Attachment: developmental pathways to affective dysregulation in young people at ultra-high risk of developing psychosis. Br J Clin Psychol. 2013;52(4):424–437. [DOI] [PubMed] [Google Scholar]
- 86.Michail M, Birchwood M. Social anxiety in first-episode psychosis: the role of childhood trauma and adult attachment. J Affect Disord. 2014;163:102–109. [DOI] [PubMed] [Google Scholar]
- 87.Achim AM, Ouellet R, Roy MA, Jackson PL. Assessment of empathy in first-episode psychosis and meta-analytic comparison with previous studies in schizophrenia. Psychiatry Res. 2011;190(1):3–8. [DOI] [PubMed] [Google Scholar]
- 88.Armando M, Lin A, Girardi P, et al. . Prevalence of psychotic-like experiences in young adults with social anxiety disorder and correlation with affective dysregulation. J Nerv Ment Dis. 2013;201(12):1053–1059. [DOI] [PubMed] [Google Scholar]
- 89.Davis M. A multidimensional approach to individual differences in empathy. JSAS Catalog of Selected Documents in Psychology. 1980;10:85. [Google Scholar]
- 90.Aikawa S, Kobayashi H, Nemoto T, et al. . Social anxiety and risk factors in patients with schizophrenia: Relationship with duration of untreated psychosis. Psychiatry Res. 2018;263:94–100. [DOI] [PubMed] [Google Scholar]
- 91.Birchwood M, Smith J, Cochrane R, Wetton S, Copestake S. The social functioning scale. The development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. Br J Psychiatry. 1990;157:853–859. [DOI] [PubMed] [Google Scholar]
- 92.Kwong VW, Chang WC, Chan GH, et al. . Clinical and treatment-related determinants of subjective quality of life in patients with first-episode psychosis. Psychiatry Res. 2017;249:39–45. [DOI] [PubMed] [Google Scholar]
- 93.Lachner G, Wittchen HU, Perkonigg A, et al. . Structure, content and reliability of the Munich-Composite International Diagnostic Interview (M-CIDI) substance use sections. Eur Addict Res. 1998;4(1-2):28–41. [DOI] [PubMed] [Google Scholar]
- 94.Lysaker PH, Salyers MP, Tsai J, Spurrier LY, Davis LW. Clinical and psychological correlates of two domains of hopelessness in schizophrenia. J Rehabil Res Dev. 2008;45(6):911–919. [DOI] [PubMed] [Google Scholar]
- 95.Lysaker PH, Hammersley J. Association of delusions and lack of cognitive flexibility with social anxiety in schizophrenia spectrum disorders. Schizophr Res. 2006;86(1-3):147–153. [DOI] [PubMed] [Google Scholar]
- 96.Gkika S, Wittkowski A, Wells A. Social cognition and metacognition in social anxiety: a systematic review. Clin Psychol Psychother. 2018;25(1):10–30. [DOI] [PubMed] [Google Scholar]
- 97.Garety PA, Freeman D. The past and future of delusions research: from the inexplicable to the treatable. Br J Psychiatry. 2013;203(5):327–333. [DOI] [PubMed] [Google Scholar]
- 98.Wei Y, McGrath P, Hayden J, Kutcher S. The quality of mental health literacy measurement tools evaluating the stigma of mental illness: a systematic review. Epidemiol Psychiatr Sci. 2018;27(5):433–462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Campellone TR, Sanchez AH, Kring AM. Defeatist performance beliefs, negative symptoms, and functional outcome in Schizophrenia: a meta-analytic review. Schizophr Bull. 2016;42(6):1343–1352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Aunjitsakul W, Teetharatkul T, Vitayanont A, Liabsuetrakul T. Correlations between self-reported and psychiatrist assessments of well-being among patients with schizophrenia. Gen Hosp Psychiatry. 2019;56:52–53. [DOI] [PubMed] [Google Scholar]
- 101.Chino B, Nemoto T, Fujii C, Mizuno M. Subjective assessments of the quality of life, well-being and self-efficacy in patients with schizophrenia. Psychiatry Clin Neurosci. 2009;63(4):521–528. [DOI] [PubMed] [Google Scholar]
- 102.Aunjitsakul W, Pitanupong J. Schizophrenias’ quality of life and emotional intelligence in Songklanagarind Hospital. Songkla Med J. 2018;36(1):61–71. [Google Scholar]
- 103.The British Psychological Society. Good practice guidelines on the use of psychological formulation. Leicester: The British Psychological Society; 2011. [Google Scholar]
- 104.Skelly AC, Dettori JR, Brodt ED. Assessing bias: the importance of considering confounding. Evid Based Spine Care J. 2012;3(1):9–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hong QN, Pluye P, Fàbregues S, et al. . Improving the content validity of the mixed methods appraisal tool: a modified e-Delphi study. J Clin Epidemiol. 2019;111:49–59.e1. [DOI] [PubMed] [Google Scholar]
- 106.Tseng W. Culture and psychopathology. In Handbook of Cultural Psychiatry. San Diego, CA: Academic Press; 2001:175–433. [Google Scholar]
- 107.Suhail K. Phenomenology of delusions in Pakistani patients: effect of gender and social class. Psychopathology. 2003;36(4):195–199. [DOI] [PubMed] [Google Scholar]
- 108.Skodlar B, Dernovsek MZ, Kocmur M. Psychopathology of schizophrenia in Ljubljana (Slovenia) from 1881 to 2000: changes in the content of delusions in schizophrenia patients related to various sociopolitical, technical and scientific changes. Int J Soc Psychiatry. 2008;54(2):101–111. [DOI] [PubMed] [Google Scholar]
- 109.Freeman D. Suspicious minds: the psychology of persecutory delusions. Clin Psychol Rev. 2007;27(4):425–457. [DOI] [PubMed] [Google Scholar]
- 110.Fresco DM, Coles ME, Heimberg RG, et al. . The Liebowitz social anxiety scale: a comparison of the psychometric properties of self-report and clinician-administered formats. Psychol Med. 2001;31(6):1025–1035. [DOI] [PubMed] [Google Scholar]
- 111.Hambrick JP, Turk CL, Heimberg RG, Schneier FR, Liebowitz MR. Psychometric properties of disability measures among patients with social anxiety disorder. J Anxiety Disord. 2004;18(6):825–839. [DOI] [PubMed] [Google Scholar]
- 112.Peters L. Discriminant validity of the Social Phobia and Anxiety Inventory (SPAI), the Social Phobia Scale (SPS) and the Social Interaction Anxiety Scale (SIAS). Behav Res Ther. 2000;38(9):943–950. [DOI] [PubMed] [Google Scholar]
- 113.Watson D, Friend R. Measurement of social-evaluative anxiety. J Consult Clin Psychol. 1969;33(4):448–457. [DOI] [PubMed] [Google Scholar]
- 114.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA.. Manual for the State-Trait Anxiety Inventory. CA: Consulting Psychologists Press; 1983. [Google Scholar]
- 115.Barnes LLB, Harp D, Jung WS. Reliability generalization of scores on the Spielberger State-Trait Anxiety Inventory. Educ Psychol Meas. 2002;62(4):603–618. [Google Scholar]
- 116.Kabacoff RI, Segal DL, Hersen M, Van Hasselt VB. Psychometric properties and diagnostic utility of the Beck Anxiety Inventory and the State-Trait Anxiety Inventory with older adult psychiatric outpatients. J Anxiety Disord. 1997;11(1):33–47. [DOI] [PubMed] [Google Scholar]
- 117.Reynolds W.Multidimensional Anxiety Questionnaire. Lutz (FL): Psychological Assessment Resources Incorporation; 1999. [Google Scholar]
- 118.Lysaker PH, Salyers MP. Anxiety symptoms in schizophrenia spectrum disorders: associations with social function, positive and negative symptoms, hope and trauma history. Acta Psychiatr Scand. 2007;116(4):290–298. [DOI] [PubMed] [Google Scholar]
- 119.Davidson JR, Potts NL, Richichi EA, et al. . The brief social Phobia scale. J Clin Psychiatry. 1991;52 Suppl:48–51. [DOI] [PubMed] [Google Scholar]
- 120.Turner SM, Beidel DC, Dancu CV, Stanley MA. An empirically derived inventory to measure social fears and anxiety: the social Phobia and anxiety inventory. J Consult Clin Psychol. 1989;1(1):35–40. [Google Scholar]
- 121.Bunnell BE, Joseph DL, Beidel DC. Measurement invariance of the Social Phobia and Anxiety Inventory. J Anxiety Disord. 2013;27(1):84–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Leary MR. Social anxiousness: the construct and its measurement. J Pers Assess. 1983;47(1):66–75. [DOI] [PubMed] [Google Scholar]
- 123.Ullrich R, Muynck RU.. Der Unsicherheits-Fragebogen. Testmanual U. Anleitung Fur Den Therapeuten. Vol 1979. 2nd ed. Munchen: Pfeiffer; 1977. [Google Scholar]
- 124.Revenstor FKW, Ullrich R, Ullrich DE, Muynck R.. Faktorenstrukturvergleiche Des U-Fragebogens Fur Sechs Stichproben. Munchen: Pfeiffer; 1977. [Google Scholar]
- 125.Curran JP.A Procedure for the Assessment of Social Skills: The Simulated Social Interactions Test. New York: Guilford Press; 1982. [Google Scholar]
- 126.Tsang H, Pearson V. Reliability and validity of a simple measure for assessing the social skills of people with schizophrenia necessary for seeking and securing a job. Can J Occup Ther. 2000;67(4):250–259. [DOI] [PubMed] [Google Scholar]
- 127.Bell MD, Lysaker PH, Beam-Goulet JL, Milstein RM, Lindenmayer JP. Five-component model of schizophrenia: assessing the factorial invariance of the positive and negative syndrome scale. Psychiatry Res. 1994;52(3):295–303. [DOI] [PubMed] [Google Scholar]
- 128.Andreasen NC. The scale for the Assessment of Negative Symptoms (SANS): conceptual and theoretical foundations. Br J Psychiatry. 1989;155(S7):49–52. [PubMed] [Google Scholar]
- 129.Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10(3):799–812. [Google Scholar]
- 130.Andersen J, Larsen JK, Schultz V, et al. . The brief psychiatric rating scale. Dimension of schizophrenia–reliability and construct validity. Psychopathology. 1989;22(2-3):168–176. [DOI] [PubMed] [Google Scholar]
- 131.Guy W.ECDEU Assessment Manual for Psychopharmacology. Rockville, MD: U.S DHEW; 1976. [Google Scholar]
- 132.Haro JM, Kamath SA, Ochoa S, et al. . The Clinical Global Impression-Schizophrenia scale: a simple instrument to measure the diversity of symptoms present in schizophrenia. Acta Psychiatr Scand Suppl. 2003(416):16–23. [DOI] [PubMed] [Google Scholar]
- 133.Green CE, Freeman D, Kuipers E, et al. . Measuring ideas of persecution and social reference: the Green et al. Paranoid Thought Scales (GPTS). Psychol Med. 2008;38(1):101–111. [DOI] [PubMed] [Google Scholar]
- 134.Freeman D, Garety PA, Kuipers E. Persecutory delusions: developing the understanding of belief maintenance and emotional distress. Psychol Med. 2001;31(7):1293–1306. [DOI] [PubMed] [Google Scholar]
- 135.Stefanis NC, Hanssen M, Smirnis NK, et al. . Evidence that three dimensions of psychosis have a distribution in the general population. Psychol Med. 2002;32(2):347–358. [DOI] [PubMed] [Google Scholar]
- 136.Hanssen MS, Bijl RV, Vollebergh W, van Os J. Self-reported psychotic experiences in the general population: a valid screening tool for DSM-III-R psychotic disorders? Acta Psychiatr Scand. 2003;107(5):369–377. [DOI] [PubMed] [Google Scholar]
- 137.Rawlings D, Freeman JL. A questionnaire for the measurement of paranoia/suspiciousness. Br J Clin Psychol. 1996;35(3):451–461. [DOI] [PubMed] [Google Scholar]
- 138.Argyle N. Panic attacks in chronic schizophrenia. Br J Psychiatry. 1990;157:430–433. [DOI] [PubMed] [Google Scholar]
- 139.Badcock JC, Dragović M, Garrett C, Jablensky A. Action (verb) fluency in schizophrenia: getting a grip on odd speech. Schizophr Res. 2011;126(1-3):138–143. [DOI] [PubMed] [Google Scholar]
- 140.de la Asuncion J, Docx L, Sabbe B, Morrens M, de Bruijn ER. Converging evidence of social avoidant behavior in schizophrenia from two approach-avoidance tasks. J Psychiatr Res. 2015;69:135–141. [DOI] [PubMed] [Google Scholar]
- 141.Hayes RL, Halford WK. Time use of unemployed and employed single male schizophrenia subjects. Schizophr Bull. 1996;22(4):659–669. [DOI] [PubMed] [Google Scholar]
- 142.Lopes BC. Differences between victims of bullying and nonvictims on levels of paranoid ideation and persecutory symptoms, the presence of aggressive traits, the display of social anxiety and the recall of childhood abuse experiences in a Portuguese mixed clinical sample. Clin Psychol Psychother. 2013;20(3):254–266. [DOI] [PubMed] [Google Scholar]
- 143.Park IJ, Chung Jung D, Suk-Hyun Hwang S, et al. . Longitudinal relationship between Personal and Social Performance (PSP) and anxiety symptoms in schizophrenia. J Affect Disord. 2016;190:12–18. [DOI] [PubMed] [Google Scholar]
- 144.Martin JA, Penn DL. Social cognition and subclinical paranoid ideation. Br J Clin Psychol. 2001;40(3):261–265. [DOI] [PubMed] [Google Scholar]
- 145.Freeman D, Gittins M, Pugh K, Antley A, Slater M, Dunn G. What makes one person paranoid and another person anxious? The differential prediction of social anxiety and persecutory ideation in an experimental situation. Psychol Med. 2008;38(8):1121–1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Tone EB, Goulding SM, Compton MT. Associations among perceptual anomalies, social anxiety, and paranoia in a college student sample. Psychiatry Res. 2011;188(2):258–263. [DOI] [PubMed] [Google Scholar]
- 147.Cooper S, Klugman J, Heimberg RG, Anglin DM, Ellman LM. Attenuated positive psychotic symptoms and social anxiety: along a psychotic continuum or different constructs? Psychiatry Res. 2016;235:139–147. [DOI] [PubMed] [Google Scholar]
- 148.Prochwicz K, Kłosowska J, Karpowska M. Threatening events theme of cognitive biases mediates the relationship between fear of social situations and delusion-like experiences among healthy adults. Psychiatry Res. 2017;256:482–489. [DOI] [PubMed] [Google Scholar]
- 149.Matos M, Pinto-Gouveia J, Gilbert P. The effect of shame and shame memories on paranoid ideation and social anxiety. Clin Psychol Psychother. 2013;20(4):334–349. [DOI] [PubMed] [Google Scholar]
- 150.Sun X, So SH, Chiu CD, Chan RC, Leung PW. Paranoia and anxiety: a cluster analysis in a non-clinical sample and the relationship with worry processes. Schizophr Res. 2018;197:144–149. [DOI] [PubMed] [Google Scholar]
- 151.Gilbert P, Boxall M, Cheung M, Irons C. The relation of paranoid ideation and social anxiety in a mixed clinical population. Clin Psychol Psychother. 2005;12(2):124–133. [Google Scholar]
- 152.Morrison AP, Shryane N, Fowler D, et al. . Negative cognition, affect, metacognition and dimensions of paranoia in people at ultra-high risk of psychosis: a multi-level modelling analysis. Psychol Med. 2015;45(12):2675–2684. [DOI] [PubMed] [Google Scholar]
- 153.Taylor HE, Stewart SL, Dunn G, et al. . Psychopathology and affect dysregulation across the continuum of psychosis: a multiple comparison group study. Early Interv Psychiatry. 2014;8(3):221–228. [DOI] [PubMed] [Google Scholar]
- 154.Mueller SA.Paranoid ideation and social anxiety in undergraduates and clinical populations [Thesis]. Michigan: Psychology, University of Michigan; 2016. [Google Scholar]
- 155.Ghada E, Maha EG. Social anxiety in schizophrenia: a clinical quantitative and qualitative analysis. Middle East Curr Psychiatry. 2011;18(1):37–44. [Google Scholar]
- 156.Penn DL, Hope DA, Spaulding W, Kucera J. Social anxiety in schizophrenia. Schizophr Res. 1994;11(3):277–284. [DOI] [PubMed] [Google Scholar]
- 157.Mazeh D, Bodner E, Weizman R, et al. . Co-morbid social phobia in schizophrenia. Int J Soc Psychiatry. 2009;55(3):198–202. [DOI] [PubMed] [Google Scholar]
- 158.Gorun A, Cieslak K, Harkavy-Friedman J, et al. . Frequent comorbidity and predictors of social anxiety in persons with schizophrenia: a retrospective cohort study. Prim Care Companion J Clin Psychiatry. 2015;17(5):289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 159.Pisano S, Catone G, Pascotto A, et al. . Paranoid thoughts in adolescents with social anxiety disorder. Child Psychiatry Hum Dev. 2016;47(5):792–798. [DOI] [PubMed] [Google Scholar]
- 160.Lee TY, Chang SC, Chu H, et al. . The effects of assertiveness training in patients with schizophrenia: a randomized, single-blind, controlled study. J Adv Nurs. 2013;69(11):2549–2559. [DOI] [PubMed] [Google Scholar]
- 161.Halperin S, Nathan P, Drummond P, Castle D. A cognitive-behavioural, group-based intervention for social anxiety in schizophrenia. Aust N Z J Psychiatry. 2000;34(5):809–813. [DOI] [PubMed] [Google Scholar]
- 162.Kingsep P, Nathan P, Castle D. Cognitive behavioural group treatment for social anxiety in schizophrenia. Schizophr Res. 2003;63(1-2):121–129. [DOI] [PubMed] [Google Scholar]
- 163.Pot-Kolder RMCA, Geraets CNW, Veling W, et al. . Virtual-reality-based cognitive behavioural therapy versus waiting list control for paranoid ideation and social avoidance in patients with psychotic disorders: a single-blind randomised controlled trial. Lancet Psychiatry. 2018;5(3):217–226. [DOI] [PubMed] [Google Scholar]
- 164.Zaffar W, Arshad T. The relationship between social comparison and submissive behaviors in people with social anxiety: Paranoid social cognition as the mediator. Psych J. 2020;9(5):716–725. [DOI] [PubMed] [Google Scholar]
- 165.Bosanac P, Mancuso SG, Castle DJ. Anxiety symptoms in psychotic disorders: results from the Second Australian National Mental Health Survey. Clin Schizophr Relat Psychoses. 2016;10(2):93–100. [DOI] [PubMed] [Google Scholar]
- 166.Ciapparelli A, Paggini R, Marazziti D, et al. . Comorbidity with axis I anxiety disorders in remitted psychotic patients 1 year after hospitalization. CNS Spectr. 2007;12(12):913–919. [DOI] [PubMed] [Google Scholar]
- 167.Rüsch N, Corrigan PW, Powell K, et al. . A stress-coping model of mental illness stigma: II. Emotional stress responses, coping behavior and outcome. Schizophr Res. 2009;110(1-3):65–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.