Abstract
COVID-19 presents in various ways, but mainly as a pulmonary disease (Marzano, 2020). Skin manifestations have been reported, including reactivation of the varicella-zoster virus (Marzano, 2020). Our case report describes two adults developing herpes zoster after vaccination with tozinameran (the Pfizer-BioNTech COVID-19 mRNA vaccine). A possible cause for this reaction is a transient lymphocytopenia that occurs after the vaccination — similar to that in COVID-19 disease (Mulligan, 2020; Wang, 2020; Qin, 2020; Brabilla, 2020; Wang, 2020; Wei, 2017). In the context of vaccinating older and/or immunocompromised adults, our observations can be the starting point for further evaluation of a possible relationship between COVID-19, COVID vaccines, and herpes zoster.
Introduction
We are in the midst of a severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2), or COVID‐19, pandemic. Although COVID-19 presents mainly as a disease affecting the pulmonary system, several skin manifestations have been reported in COVID-19 patients (Marzano, 2020). One remarkable finding is the reactivation of the varicella-zoster virus (VZV), causing herpes zoster (HZ) (Marzano, 2020; Wang, 2020; Qin, 2020; Ferreira, 2020; Tartari, 2020; Elsaie, 2020; Recalcati, 2020; Bhardwaj, 2021). In some patients, HZ was the presenting symptom of COVID-19 infection (Elsaie, 2020). Since December 2020, vaccination programs against COVID-19 have occurred throughout the world. Commonly reported adverse effects are pain at the injection site, fever, nausea, myalgia, and fatigue (http://www.adrreports.eu/ [accessed July 27, 2021]; https://wonder.cdc.gov/vaers.html [accessed July 27, 2021]). This is in concordance with the side-effects mentioned in the product information for tozinameran (the Pfizer BioNTech COVID-19 mRNA vaccine) (Comirnaty, INN-COVID-19 mRNA Vaccine (nucleoside-modified) (https://www.ema.europa.eu/en/documents/product-information/comirnaty-epar-product-information_en.pdf)s [accessed June 8, 2021] Website: Comirnaty, INN-COVID-19 mRNA Vaccine (nucleoside-modified) (europa.eu)s. Accessed June 8, 2021.). Here, we describe a rare side-effect in the form of HZ eruptions in two adults after vaccination with tozinameran.
Case presentation
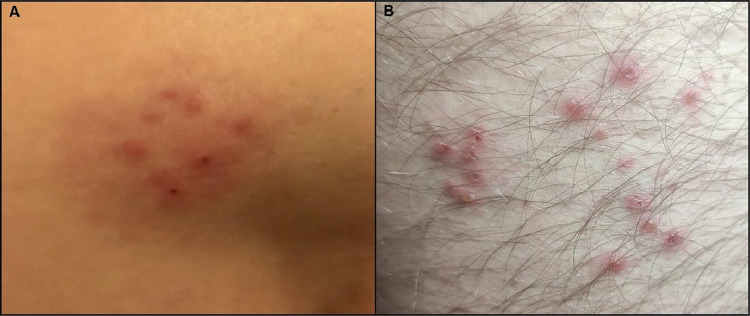
Case 1 was a 29-year-old female healthcare professional with no noteworthy medical history, except for chicken pox three times as a child, and once during adolescence. In spite of this, she never had HZ. On January 8, 2021, she received the first dose of tozinameran, with no adverse reactions until January 23, when she noticed painful grouped vesicles on the left lateral of the ox coccyges (dermatome S3), clinically diagnosed as being HZ (Figure 1 A). On January 29, she received the second dose of the vaccine. At that time, there was still some ulceration left, but there was no relapse of HZ after the second dose. After 2 weeks, the lesions had resolved without medical intervention.
Figure 1.
(A) Female patient with grouped vesicles in dermatome S3. (B) Male patient with grouped vesicles in dermatome S2.
Case 2 was a 34-year-old male healthcare professional with a medical history of ulcerative colitis, for which he had been using infliximab and, for 4 years without infectious complications. He had chicken pox as a child, but never HZ. He received his first dose of tozinameran on January 12, 2021, with no adverse reactions over the following days. On January 25, he noticed painful and swollen inguinal lymph nodes, after which he saw a rash on his right leg. He visited the ER, where a papulovesicular rash was identified in dermatome S2 (Figure 1B). Blood analysis was normal. A PCR test performed on vesical fluid was positive for VZV. He was prescribed valacyclovir, 1 gram thrice daily, for 10 days, and recovered completely. On February 2, he received the second dose of the vaccine without any complications.
Discussion
Herpes zoster is characterized by multiple, painful, and/or itching unilateral vesicles and ulcerations, typically occurring in a single dermatome (Dayan, 2017; Gershon, 2015). The average duration of the rash ranges from 7 to 10 days, and is a self-limiting condition (Van Oorschot, 2021). Although usually a limited disease, it can progress to disseminated cutaneous eruptions, encephalomyelitis, and pneumonia, especially in immunocompromised individuals (Gershon 2015).
At the time of writing, the European EudraVigilance database had reported 4103 cases of HZ after receiving tozinameran, accounting for 1.3% of total reported events following this vaccination (http://www.adrreports.eu [accessed July 27, 2021]). For mRNA-1273 (the Moderna vaccine), 590 (0.7%) cases had been reported, for CHADOX1 NCOV-19 (the Oxford-AstraZeneca vaccine) 2143 (0.6%) cases, and for AD26.COV2.S (the Janssen vaccine) 59 cases (0.3%). The United States Vaccine Adverse Event Report System (VAERS) reported 2512 HZ cases (1.3% of total reported events) after tozinameran, 1763 (0.9%) after mRNA-1273, and 302 (0.7%) after AD26.COV2.S (https://wonder.cdc.gov/vaers.html [accessed July 27, 2021]). The Dutch pharmacovigilance center Lareb reported 300 cases (0.8% of total reported events) after vaccination with tozinameran (https://coronameldingen.lareb.nl [accessed June 8, 2021]). Whether these numbers are disproportionate or not requires further analysis. However, combined with the case reports describing HZ simultaneously with COVID-19 infection, the vaccination data do suggest a possible relationship.
HZ is caused by reactivation of VZV, which tends to remain in a latent state in the dorsal root ganglia of cutaneous nerve endings following a primary episode of chicken pox (Wei, 2017; Gershon, 2015). Reactivation occurs when the immunological mechanisms that suppress VZV replication fail to contain the virus (Wei, 2017). Classic risk factors include advanced age, use of immunosuppressant medication, immunocompromising conditions (e.g. HIV, autoimmune disease), and psychological stress (Gershon, 2015; Marra, 2020). Both cases presented here had chicken pox in childhood, yet never suffered from HZ. While subject 2 had other risk factors for HZ (use of immunosuppressive agents), subject 1 did not. Both subjects received the vaccination as healthcare professionals, and were completely free of any symptoms at the time of vaccination. The occurrence of HZ after vaccination could be a simple coincidence. However, recent reports have described similar cases, mostly involving known risk factors for HZ reactivation (Bostan, 2021; Furer, 2021; Arora, 2021; Tessas, 2021; Eid, 2021).
Rodriguez et al. described five young, healthy adults without risk factors who developed HZ reactivation (Rodríguez-Jiménez et al., 2021). Furthermore, several case reports have described a link between COVID-19 and HZ reactivation in the absence of any of the classical risk factors (Marzano, 2020; Brambilla, 2020; Ferreira, 2020; Tartari, 2020; Elsaie, 2020; Márcia et al., 2020; Nofal, 2020; Wang, 2020; Pona, 2020; Saati, 2020). This led to the hypothesis that illness, with physical and psychological stress, might trigger HZ. Additionally, lymphopenia occurs in over 70% of patients with COVID-19, especially in those with a more severe clinical course (Wang, 2020; Qin, 2020). While all subsets seem to decrease, the most marked depletion and exhaustion occur in CD4+ and CD8+ lymphocytes (Wang, 2020; Qin, 2020; Marra, 2020). Since cell-mediated immunity is considered to be of great importance in protection against herpes zoster reactivation, such a functional impairment of T-lymphocytes could reactivate VZV (Brambilla, 2020; Wang, 2020; Wei 2017). Interestingly, as with COVID-19 infection, the phase-I/II trial with BNT162b1 (now called tozinameran) showed a dose-dependent decrease in lymphocytes in the first days following injection (Mulligan, 2020). With the dosage now used worldwide, which is 30 micrograms, 45.5% of the recipients had lymphocyte counts below 1 × 109, with one subject (9.1%) having grade-3 lymphopenia (0.2–0.5 × 109). These decreases were transient, with lymphocyte levels returning to normal 6–8 days after vaccination. The phase-I/II trial with ChAdOx1 nCoV-19 showed transient lymphopenia in 46% of the participants (Folegatti, 2020). It is conceivable that this short period of lymphopenia — after COVID-19 infection or vaccination — can trigger a VZV reactivation. Although a full discussion regarding the role of T-regulatory cells is beyond the scope of this report, Sahin et al. speculate that the lymphopenia might be caused by an increase in type 1 interferons (Sahin, 2020). This would cause rolling and adhesion of lymphocytes to the endothelium, and consequently fewer T-cells available to be measured in blood samples (Kamphuis, 2006). However, functionality would not be decreased, and type 1 interferons would normally inhibit varicella zoster replication (Kamphuis, 2006; Ku, 2016). It would be interesting to ascertain whether patients developing VZV after vaccination have altered interferon responses.
In conclusion, we report two cases who developed herpes zoster after vaccination with tozinameran. While frequently a harmless condition, disseminated zoster can have fatal consequences. In the context of vaccinating older and/or immunocompromised adults, our observations require further evaluation of the possible relationship between COVID-19 and herpes zoster.
Other information
None of the above-listed authors have conflicts of interest to report. There was no funding or other financial support of any organization. Written informed consent was obtained from the participants in this case report.
References
- Arora P, Sardana K, Mathachan SR, Malhotra P. Herpes zoster after inactivated COVID-19 vaccine: a cutaneous adverse effect of the vaccine. J Cosmet Dermatol. 2021;12 doi: 10.1111/jocd.14268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhardwaj A, Sapra L, Saini C, Azam Z, Mishra PK, Verma B, et al. COVID-19: immunology, immunopathogenesis and potential therapies. Int Rev Immunol. 2021;0:1–36. doi: 10.1080/08830185.2021.1883600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bostan E, Yalici-Armagan B. Herpes zoster following inactivated COVID-19 vaccine: a coexistence or coincidence? J Cosmet Dermatol. 2021;20:1566–1567. doi: 10.1111/jocd.14035. [DOI] [PubMed] [Google Scholar]
- Brambilla L, Maronese CA, Tourlaki A, Veraldi S. Herpes zoster following COVID-19: a report of three cases. European Journal of Dermatology. 2020;30:754–756. doi: 10.1684/ejd.2020.3924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dayan RR, Peleg R. Herpes zoster — typical and atypical presentations. Postgrad Med. 2017;129:567–571. doi: 10.1080/00325481.2017.1335574. [DOI] [PubMed] [Google Scholar]
- Eid E, Abdullah L, Kurban M, Abbas O. Herpes zoster emergence following mRNA COVID-19 vaccine. J Med Virol. 2021:1–2. doi: 10.1002/jmv.27036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elsaie ML, Youssef EA, Nada HA. Herpes zoster might be an indicator for latent COVID 19 infection. Dermatol Ther. 2020;33:4. doi: 10.1111/dth.13666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferreira ACA, Romão TT, Macedo YS, Pupe C, Nascimento OJM. COVID-19 and herpes zoster co-infection presenting with trigeminal neuropathy. Eur J Neurol. 2020;27:1748–1750. doi: 10.1111/ene.14361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Folegatti PM, Ewer KJ, Aley PK, Angus B, Becker S, et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet. 2020;396:467–478. doi: 10.1016/S0140-6736(20)31604-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Furer V, Zisman D, Kibari A, Rimar D, Paran Y, Elkayam O. Herpes zoster following BNT162b2 mRNA Covid-19 vaccination in patients with autoimmune inflammatory rheumatic diseases: a case series. Rheumatology. 2021 doi: 10.1093/rheumatology/keab345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gershon AA, Breuer J, Cohen JI, Cohrs RJ, Gershon MD, Gilden D, et al. Varicella zoster virus infection. Nat Rev Dis Prim. 2015;1:1–41. doi: 10.1038/nrdp.2015.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamphuis E, Junt T, Waibler Z, Forster R, Kalinke U. Type I interferons directly regulate lymphocyte recirculation and cause transient blood lymphopenia. Blood. 2006;108:3253–3261. doi: 10.1182/blood-2006-06-027599. [DOI] [PubMed] [Google Scholar]
- Ku CC, Chang YH, Chien Y, Lee TL. Type I interferon inhibits varicella-zoster virus replication by interfering with the dynamic interaction between mediator and IE62 within replication compartments. Cell Biosci. 2016;6:1–12. doi: 10.1186/s13578-016-0086-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Márcia C, Maia F, Pereira N, Hilan E, Gomes de Lucena G. Increased number of herpes zoster cases in Brazil related to the COVID-19 pandemic. International Journal of Infectious Diseases. 2020;104:732–733. doi: 10.1016/j.ijid.2021.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marra F, Parhar K, Huang B, Vadlamudi N. Risk factors for herpes zoster infection: a meta-analysis. Open Forum Infect Dis. 2020;7:1–8. doi: 10.1093/ofid/ofaa005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marzano AV, Genovese G, Fabrrocini G, Pigatto P, Monfrecola G, et al. Varicella-like exanthem as a specific COVID-19-associated skin manifestation: multicenter case series of 22 patients. J Am Acad Dermatol. 2020;83:280–285. doi: 10.1016/j.jaad.2020.04.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulligan MJ, Lyke KE, Kitchin N, Absalon J, Gurtman A, et al. Phase I/II study of COVID-19 RNA vaccine BNT162b1 in adults. Nature. 2020;586:589–593. doi: 10.1038/s41586-020-2639-4. [DOI] [PubMed] [Google Scholar]
- Nofal A, Fawzy MM, Sharaf EL Deen SM, El-Hawary EE. Herpes zoster ophthalmicus in COVID-19 patients. Int J Dermatol. 2020;59:1545–1546. doi: 10.1111/ijd.15240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Oorschot D, Vroling H, Bunge E, Diaz-Decaro J, Curran D, Yawn B. A systematic literature review of herpes zoster incidence worldwide. Hum Vaccin Immunother. 2021;17:1714–1732. doi: 10.1080/21645515.2020.1847582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pona PA, Jiwani RA, Afriyie F, Labbe J, Cook PP, Mao Y. Herpes zoster as a potential complication of coronavirus disease 2019. Dermatol Ther. 2020;33:18–19. doi: 10.1111/dth.13930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qin C, Zhou L, Hu Z, Zhang S, Yang S, et al. Dysregulation of immune response in patients with COVID-19 in Wuhan. China. SSRN Electron J. 2020 doi: 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatology Venereol. 2020;34:e212–e213. doi: 10.1111/jdv.16387. [DOI] [PubMed] [Google Scholar]
- Rodríguez-Jiménez P, Chicharro P, Cabrera LM, Seguí M, Morales-Caballero Á, Llamas-Velasco M, et al. Varicella-zoster virus reactivation after SARS-CoV-2 BNT162b2 mRNA vaccination: report of 5 cases. JAAD Case Reports. 2021;12:58–59. doi: 10.1016/j.jdcr.2021.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saati A, Al-Husayni F, Malibari AA, Bogari AA, Alharbi M. Herpes zoster co-infection in an immunocompetent patient with COVID-19. Cureus. 2020;12:4–9. doi: 10.7759/cureus.8998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahin U, Muik A, Derhovanessian E, Vogler I, Kranz LM, Vormehr M, et al. COVID-19 vaccine BNT162b1 elicits human antibody and TH1 T cell responses. Nature. 2020;586:594–599. doi: 10.1038/s41586-020-2814-7. [DOI] [PubMed] [Google Scholar]
- Tartari F, Spadotto A, Zengarini C, Zanoni R, Guglielmo A, Adorno A, et al. Herpes zoster in COVID-19-positive patients. Int J Dermatol. 2020;59:1028–1029. doi: 10.1111/ijd.15001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tessas I, Kluger N. Ipsilateral herpes zoster after the first dose of BNT162b2 mRNA COVID-19 vaccine. J Eur Acad Dermatology Venereol. 2021:0–2. doi: 10.1111/jdv.17422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B, Guo S, Yao Y, Li Y, Zhang G. Dermatologists may need to pay more attention to herpes zoster during the pandemic of COVID-19. Infect Dis. 2020;52:917–918. doi: 10.1080/23744235.2020.1797158. [DOI] [PubMed] [Google Scholar]
- Wang F, Nie J, Wang H, Zhao Q, Xiong Y, et al. Characteristics of peripheral lymphocyte subset alteration in covid-19 pneumonia. J Infect Dis. 2020;221:1762–1769. doi: 10.1093/infdis/jiaa150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei L, Zhao J, Wu W, Zhang Y, Fu X, et al. Decreased absolute numbers of CD3+ T cells and CD8+ T cells during aging in herpes zoster patients. Sci Rep. 2017;7(1):1–8. doi: 10.1038/s41598-017-15390-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Zhu G, Lai W, Zheng Y. Transmission of varicella-zoster-virus (VZV) in family: calls for attention during COVID-19 outbreak. J Cosmet Dermatol. 2020;19:3166–3167. doi: 10.1111/jocd.13808. [DOI] [PubMed] [Google Scholar]