Abstract
COVID-19 is now established in Africa, and requires appropriate prioritization of resources and customized control measures. Although there have been lower than predicted number of COVID-19 cases (6,839,159 (3.4% of global cases)) and fatalities (172,413 (4.1% of cases in Africa)) compared to global estimates from other regions, as of 3rd August 2021. The World Health Organization (WHO) has warned that poor mitigation strategies could worsen the current situation in African countries. Several aspects have been attributed to the lower COVID-19 magnitude observed in Africa that include: warmer climate, a youthful population, and previous experience in managing infectious diseases. However, the level of COVID-19 risk of exposure and vulnerability to develop complications varies greatly across the continent. At present, most COVID-19 disease trajectories have been predicted using mathematical models focused solely on demographic factors. We compared the global health security and governance indices in forty-one African countries, with a population of more than 2.5 million, and matched these to the magnitude of COVID-19 burden, to establish whether there is correlation. These findings suggests that more accurate comparisons of responses to COVID-19 can only be made within clusters of African countries that share similar governance and preparedness standards. We conclude that proper implementation of the continental framework on disaster preparedness and management is required for management of the COVID-19 pandemic.
Keywords: COVID-19, Africa, Preparedness, Governance, Health indices, Dendrogram
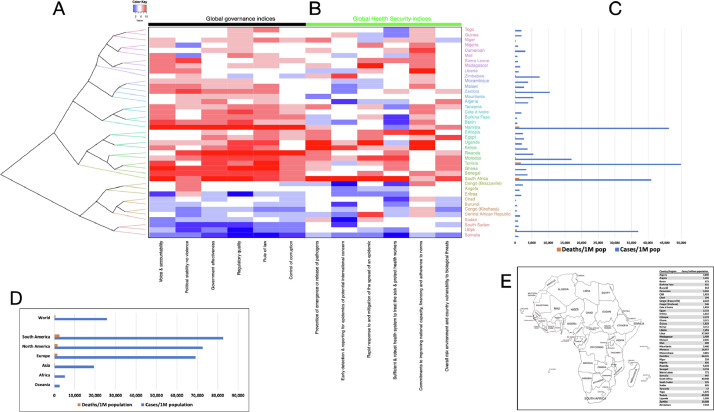
Corona virus disease 2019 (COVID-19) has been reported across all fifty-four African countries, with more than 6.8 million cases and over 172,000 deaths on the continent, as of 3rd August 2021 (Fig. 1 ) [1]. The COVID-19 pandemic coincides with other infectious disease outbreaks, for example a new Ebola outbreak in Democratic Republic of Congo [2,3]. Humanitarian emergencies causing food insecurity and threatening agriculture-based livelihoods, such as the worst locust invasion in Ethiopia and Kenya for more than 70 years; and the worst floods in East Africa in over 55 years that have affected over 1.3 million people, displacing over 450,000 are also occurring at a time [4,5].
Fig. 1.
The global health security and governance indices in forty-one African countries. (A) A dendrogram showing hierarchical relationship of global governance and health security indices in forty-one African countries. African countries that share similar governance and preparedness standards cluster together. (B) A heatmap showing the relationship of global governance and health security indices in these forty-one African countries. (C) The number of cases and fatalities per 1 million individuals in the population of each of the forty-one African countries, as at 3rd August 2021. (D) Comparison of the of cases and fatalities per 1 million individuals in between Africa and other regions. (E) the map the African continent.
Most African governments have taken commendable measures to impede widespread community transmission of COVID-19 within country borders, which include strict controls to ensure physical distancing by prohibiting large gathering in places of worship, markets, at funerals, and regulated public transport [6]. Consequently, there have been lower than predicted number of COVID-19 cases (6,839,159 (3.4% of global cases)) and fatalities (172,413 (4.1% of cases in Africa)) compared to global estimates from other regions, as of 3rd August 2021 (Fig. 1)(Supplementary Materials 1) [7]. These containment measures aim to protect all health systems that continue to provide other essential services from being overwhelmed. This has considerably averted increased rates of morbidity and mortality in African countries.
Africa has a sizeable demographic, genetic, and cultural diversity [8], and it has been challenging to understand the mosaic patterns of COVID-19 disease prevalence in different countries. A number of aspects have been attributed to the lower COVID-19 magnitude observed in Africa, some of which include warmer climate, a youthful population, and previous experience in managing infectious diseases [9,10]. Indeed there are unconfirmed arguments that Africans have heightened immune responses due to high risk of exposure to tropical infectious diseases. However, the level of COVID-19 risk of exposure and vulnerability to develop complications varies across the continent, for example the median age in Niger and Seychelles are 14.8 and 36.8 years, respectively.
The magnitude of the COVID-19 pandemic in Africa is currently small, with 3.4% and 4.1% of worldwide cases and fatalities respectively. However, the World Health Organisation (WHO) has warned that left unabated the situation could worsen, with a rise by more than 230 million cases and 150,000 deaths within a year [11]. Despite Africa's vast experience in handling epidemics of infectious diseases, the global economic impact and requirement on restricting physical interactions as a control measure for the spread of COVID-19 present new challenges to African governments. COVID-19 is already causing adverse effects, that include: widespread unemployment, the collapse of the tourism and travel industry, setbacks in commodity exports, and food insecurity due to disrupted supply chains. Since the manner of response to epidemics is intrinsic to political decisions. There is renewed emphasis on addressing preparedness gaps and strengthening culturally sensitive governance, to avoid compromising national capacity to control disease outbreaks. Well-matched mitigation strategies accounting for differences in socioeconomic, governance, demographic, and ecological factors are required to avoid a reversal of progress towards attaining Sustainable Development Goals (SDGs) [12]. A few examples of the adverse effects of COVID-19 on the SDGs progress include: pushing people further into poverty in lower- and middle-income countries, reversing SDG 1 of ending poverty of all forms everywhere; increased inequality negating progress made for SDG 5 and 10 to achieve gender equality and reduce inequality withing and among countries, respectively; and impeded progress on SDG 3, which is to ensure healthy lives and promote well-being for all at all ages [8,13,14]. Therefore, evidence-based understanding of underlying factors that could heighten COVID-19 risk is required to enable African governments guide effective long-term outbreak mitigation efforts. In addition to recognizing risks, there should be government commitment to implementing changes that address health security risks. Most COVID-19 disease trajectories have primarily been from mathematical models focused on demographic factors. In this commentary, we compared the global health security and governance indices in forty-one African countries, with a population of more than 2.5 million, and matched these to the magnitude of COVID-19 burden, to establish whether there is correlation.
Collation of these indices suggests that more accurate comparisons of responses to COVID-19 can only be made within clusters of African countries that share similar governance and preparedness standards (Fig. 1). The manner of preparedness for epidemics and good governance significantly influence the ability and speed to prevent, detect, report, and respond to infectious disease outbreaks that could overwhelm a country's health system management capacity. There is urgent need to share and apply customized practices on planning, resource allocation, and management learnt from previous outbreaks, especially within country clusters.
In conclusion, COVID-19 is now established in Africa, and an awareness of primed responses is critical to appropriately prioritise resources and customize control measures. Early identification of preparedness and management gaps will undoubtedly help to restrain global COVID-19 transmission. Proper implementation of the Global Health Security Agenda (GHSA) framework on disaster preparedness and management developed at the Africa Centers for Disease Control and Prevention (Africa CDC), by member states across the continent, is urgently required to prevent, detect and respond to public health adverse effects for successful management of the COVID-19 pandemic.
Declarations
Consent for publication
Not Applicable
Availability of data and material
All data and materials are available in the supplementary materials.
Competing interests
None declared
Authors' contributions
BWK - study design data collation and analysis, data interpretation, manuscript writing.
Funding
The author received no funding from an external source.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Editor: DR B Gyampoh
Footnotes
Editor DR B Gyampoh
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.sciaf.2021.e00948.
Appendix. Supplementary materials
Supplementary Materials
1. The data sources used for analysis.
2. An R script used to generate the heatmap.
References
- 1.CDC Africa. Coronavirus Disease 2019 (COVID-19). https://africacdcorg/covid-19 2020 (accessed 16 May 2020).
- 2.WHO. Weekly bulletin in outbreaks and other emergencies. Week 21: 18-24 May 2020. https://apps.who.int/iris/bitstream/handle/10665/332178/OEW21-1824052020.pdf 2020 (accessed 26 May 2020).
- 3.Maxmen A. World's second-deadliest Ebola outbreak ends in Democratic Republic of the Congo. Nature. 2020 doi: 10.1038/d41586-020-01950-0. https://www.nature.com/articles/d41586-020-01950-0 (accessed 1 Jul 2020) [DOI] [PubMed] [Google Scholar]
- 4.FAO. Desert Locust situation update. http://www.fao.org/ag/locusts/en/info/info/index.html (accessed 1 Jul 2020).
- 5.reliefweb. Eastern Africa Region: Floods and Locust Outbreak Snapshot (2020). https://reliefweb.int/report/ethiopia/eastern-africa-region-floods-and-locust-outbreak-snapshot-may-2020 (accessed 1 Jul 2020).
- 6.Badu K, Thorn J, Goonoo N, et al. Africa's response to the COVID-19 pandemic: a review of the nature of the virus, impacts and implications for preparedness [version 1; peer review: awaiting peer review] AAS Open Res. 2020;3 doi: 10.12688/aasopenres.13060.1. [DOI] [Google Scholar]
- 7.Worldometer. COVID-19 Coronavirus Pandemic. https://appswhoint/iris/bitstream/handle/10665/332178/OEW21-1824052020pdf 2020 (accessed 1 Jul 2020).
- 8.Kulohoma BW. Importance of human demographic history knowledge in genetic studies involving multi-ethnic cohorts. Wellcome Open Res. 2018;3:82. doi: 10.12688/wellcomeopenres.14692.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Diop BZ, Ngom M, Pougué Biyong C, et al. The relatively young and rural population may limit the spread and severity of COVID-19 in Africa: a modelling study. BMJ Glob. Health. 2020;5 doi: 10.1136/bmjgh-2020-002699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Afolabi MO, Folayan MO, Munung NS, Yakubu A, Ndow G, Jegede A, Ambe J, Kombe F. Lessons from the Ebola epidemics and their applications for COVID-19 pandemic response in sub-Saharan Africa. Dev. World Bioeth. 2021 doi: 10.1111/dewb.12275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cabore JW, Karamagi HC, Kipruto H, et al. The potential effects of widespread community transmission of SARS-CoV-2 infection in the World Health Organization African Region: a predictive model. BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2020-002647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wesonga CA, Kulohoma B. In: Africa and the Sustainable Development Goals. Ramutsindela M, Mickler D, editors. Springer International Publishing; Cham: 2020. Prioritising health systems to achieve SDGs in Africa: a review of scientific evidence; pp. 113–121. [DOI] [Google Scholar]
- 13.Laborde D, Martin W, Vos R. Impacts of COVID-19 on global poverty, food security, and diets: Insights from global model scenario analysis. Agric. Econ. 2021 doi: 10.1111/agec.12624:1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yonzan N, Lakner C, Mahler DG, Aguilar RAC, Wu H: The impact of COVID-19 on global poverty under worsening growth and inequality. https://blogsworldbankorg/opendata/impact-covid-19-global-poverty-under-worsening-growth-and-inequality 2020, (Accessed 10th May 2021).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Materials
1. The data sources used for analysis.
2. An R script used to generate the heatmap.
Data Availability Statement
All data and materials are available in the supplementary materials.