Abstract
Background
The incidence of osteoporotic pelvic fractures in elderly patient is rising. This brings an increasing burden on health and social care systems as these injuries often lead to prolonged hospital admissions, loss of independence, morbidity and mortality. Some centres now advocate stabilisation of these injuries to reduce pain, facilitate early mobilisation, decrease hospital stay and restore independence. A systematic review of the literature was planned to establish the evidence for this intervention.
Methods
A systematic review was performed according to PRISMA guidelines. A clinical librarian performed a search of the following databases: NHS Evidence, TRIP, the Cochrane Database of Systematic Reviews, MEDLINE and EMBASE. Seventeen eligible studies were identified with 766 patients.
Results
The quality of evidence was poor with no good quality randomised trials. The majority of injuries were minimally displaced. Posterior ring injuries were most often stabilised with percutaneous screws which were sometimes augmented with void filler. A number of techniques were described for stabilisation of the anterior ring although fixation of the anterior ring was frequently not performed.
There was consistent evidence from the included studies that operative intervention significantly improved pain. Complications were minimal but there were increased failure rates when a single unaugmented sacroiliac joint screw was used. The limited availability of non-operative comparators made it difficult to draw firm conclusions about the efficacy of surgical over non-surgical management in these patients.
Conclusions
Operative management of fragility fractures of the pelvis should be considered for patients failing a brief period of non-operative management, however prospective randomised trials need to be performed to provide improved evidence for this intervention. Surgeons should consider which fixation techniques for fragility fractures of the pelvis are robust enough to allow immediate weightbearing, whilst minimising operative morbidity and post-operative complications.
PROSPERO Systematic Review ID: CRD42020171237.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12891-021-04579-w.
Keywords: Osteoporosis, Pelvic fracture, Pelvic ring, Fragility fracture of the pelvis, Percutaneous
Background
The rising incidence of osteoporosis has brought significant challenges regarding the management of associated low energy injuries. In the past, high energy pelvic fractures associated with major trauma have predominated, however the incidence of low energy fragility fractures of the pelvis (FFP) is increasing and predicted to continue rising in the future [1–3].
High energy injuries often involve both the bony pelvis and associated ligaments and soft tissues. In contrast, low energy FFP are more commonly characterised by injuries affecting only the weaker osteoporotic bone. This observation is the basis for Rommen’s classification which divides FFP into four groups of increasing instability ranging from isolated pubic rami injuries to complex bilateral displaced sacral injuries [4].
Historically the management of FFP in the elderly has involved a brief period of bed rest and analgesia followed by return to mobilisation as pain allowed [5, 6]. Despite this, significant pain caused by the injury [7, 8] often leads to prolonged immobility [9]. The consequences of this in a vulnerable population are significant. The mortality rate is similar to hip fractures, there is significant associated morbidity, prolonged inpatient stay and patients often require temporary or permanent admission to nursing homes [3, 10–15]. As with other debilitating osteoporotic fractures, this injury carries with it a significant financial burden [16] and results in a significant reduction in patient reported quality of life [17].
Some centres now advocate surgical management of these injuries to improve outcomes [18, 19]. The aim of this systematic review is to evaluate evidence for surgical management of FFP. This includes fracture patterns encountered as well as fixation methods and timing of interventions. We also aimed to identify whether these interventions improve pain and other outcomes such as mobility, length of stay, quality of life and mortality compared to conservatively managed patients.
Methods
This systematic review was registered with the International prospective register of systematic reviews (PROSPERO) Centre for Reviews and Dissemination, University of York and conducted in accordance with PRISMA guidelines [20]. A clinical librarian searched the followed databases; NHS Evidence, TRIP, the Cochrane Database of Systematic Reviews, MEDLINE and EMBASE. Bibliographic database searches were conducted using the NHS Evidence Healthcare Databases Advanced Search platform. The final search was conducted on 4th May 2020. Relevant natural language and controlled vocabulary terms were selected and combined, and final results reviewed. There were no language restrictions in the initial search, however studies not written in English were excluded.
All studies with fragility fractures of the pelvic ring including sacral insufficiency fractures were included in patients 60 years or older. Studies were excluded if they contained patients with high-energy injuries (defined as a fall greater than from standing height), or a pathological fracture from a cause other than osteoporosis. We also excluded patients managed with sacroplasty alone although included patients with augmentation of sacroiliac joint (SIJ) screws with bone cement or other void filler. Acetabular fractures and isolated iliac crest fractures were excluded as were studies with fewer than ten patients.
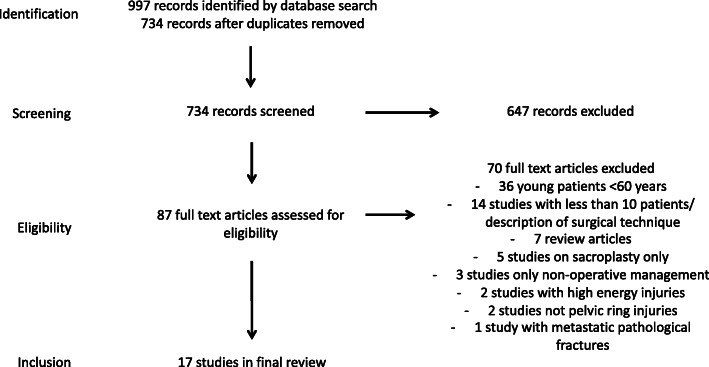
Abstracts were analysed by two authors (DW and JK). Relevant abstracts were selected for full text review and inclusion where relevant. Any disagreement on studies to include was decided by discussion and with the senior author (MR). A flowchart of the study selection can be seen in Fig. 1. Randomised and non-randomized studies were assessed for bias using The Cochrane Collaboration’s tool for assessing risk of bias [21, 22] and case series assessed by the Joanna Briggs Institute checklist for case series [23]. Studies were assessed by two authors (DW and JK) and any disagreements resolved by discussion with a third (MR). A narrative synthesis was then performed using these tools. Main outcomes were pain scores, quality of life, mobility, length of stay and mortality. Secondary outcomes were complications including re-operations, failure of fixation, neurological deficits, and infection. No meta-analysis was planned.
Fig. 1.
PRISMA flowchart of study selection
Results
Seventeen studies were identified with 766 patients, of which 463 were managed operatively. One randomised study and three studies with non-operative comparison groups were identified. The remaining studies were case series. A summary of the results is presented in Table 1.
Table 1 .
Summary of results from included studies
| Author, year and Study type | Patients | Classification and numbers | Indication for surgery | Fixation Method | Screw Augment | X-ray/CT | Post op weight bearing | Outcome measures | Results | |
|---|---|---|---|---|---|---|---|---|---|---|
| Posterior | Anterior | |||||||||
| Osterhoff et∼al. 2019 Retrospective case control [24] | 230 | “Low energy fractures of the pelvis” | Inability to mobilise 3–5 days post injury | 2 SIJ screws - Unilateral = 33 bilateral = 24 Spinopelvic = 2 plate = 2. | Plate = 8 Ramus screw = 5 Infix = 4 | – | X-ray | WBAT | 1 and 2 year mortality. Majeed score | Overall 1 year mortality 21%. 23% early operative vs 17% non-operative p = 0.29. Majeed Score 66.1 operative vs 65.7 non-op (p = 0.91) @ 61 months average f/u. LoS 12 days operative vs 8 days non-op p = < 0.001 |
| Balling et∼al. 2019 Randomised trial [25] | 52 | Rommens Type 2 = 52 | Failed conservative management for 14 days | Minimum 2 transacral screws. 26 with sacroplasty, 26 without. | none | Additional sacroplasty in 26 | CT | WBAT | VAS, ODI, Length of stay | Mean pre-op VAS SIJ 8.8 vs 9.0 SIJ + SP. Discharge VAS 3.5 and 3.6 respectively. P = < 0.05. No difference between groups. LoS 9.3 days SIJ vs 9.6 days SIJ + SP. Pre-op mean ODI SIJ 86.1 vs 86.2 SIJ + SP Decreased to 32.7 and 28.5 respectively at discharge. |
| Oikonomidis et∼al. 2019 Retrospective case series [26] | 32 | Rommens Type 1 = 1 Type 2 = 22 Type 3 = 9 | Inability to mobilise after 1 week | Single SIJ screw = 31 | Photodynamic bone stabilisation system = 32 | – | X-ray | WBAT | VAS, length of stay, mortality | 3% Mortality at 7.5 months. Mean discharge VAS 4.4, follow up VAS 3.0. Average LoS 16.5 days |
| Walker et∼al. 2018 Retrospective Cohort [27] | 41 | Young & Burgess LC1 = 26 “Sacral U” = 16 | Inability to ambulate or severe pain on ambulation | Single transacral screw = 15, Double transacral screw = 1 | none | – | X-ray | WBAT | VAS, LoS | VAS on admission operative group 7.4 improved to 3.5 on discharge, non-op 5.7 to 5.1. p = < 0.001 LoS 3.6 operative vs 4.2 non operative P = 0.51 |
| Pulley et∼al. 2018 Retrospective case series [28] | 16 | “Sacral U” = 16 | Failure of conservative management or inability to weight bear | 2 transacral screws = 13, 2 SIJ screws bilaterally = 1, 1 transacral screw + 1 SIJ screw bilaterally = 1, 1 SIJ screw bilaterally = 1 | none | – | X-ray | WBAT | VAS | Average improvement in pre to post op VAS 3.7 p = < 0.05 |
| Hoch et∼al. 2017 (1) Retrospective Case series [6] | 128 | OTA B2.1 = 115 B3.3 = 13 Operative, non-operative and failed non-operative groups | Unable to mobilise after 3 days with adequate analgesia | Single SIJ screw = 28, 2 SIJ screws = 6, Bilateral SIJ screws = 14, Triangular fixation = 2. | Plate = 3 | Additional sacroplasty in 13 | CT in 7 cases | WBAT | VAS, SF12, LoS, Mortality, EQ. 5D | 2 Year mortality 41% non-op vs 20% operative p = < 0.05. Mean LoS 18.1 operative vs 9.2 non-op P = < 0.001. Mean EQ. 5D at 2 years non-op 75.1, failed non-op 76.3, operative 74.6 - no significant difference. SF12 no difference between groups |
| Eckardt et∼al. 2017 Retrospective case series [29] | 50 | Rommens Type 2 = 15, Type 3 = 10, Type 4 = 25 | persistent mobility limiting pain | Single screw = 37, 2 screws = 11, Plate = 2. transacral screws = 23, SIJ screws = 27 | Plate = 14 (combined with single screw = 11, double screw = 1) | – | CT | WBAT | VAS, TUG, Mortality | 1 year mortality 10%. TUG test at 2 years: 0–10s 5pts (16%), 10–20s 15pts (44%), 20–30s 7pts (22%), > 30s 6pts (19%). VAS at rest 0/10 20pts (61%), VAS 1–3 7pts (21%), VAS > 3 6pts (18%). Post TUG VAS 0/10 17pts (52%), VAS 1–3 6pts (18%) VAS > 3 10pts (30%) |
| Hoch et∼al. 2017 (2) Prospective case series [14] | 34 | Rommens Type 2 = 25 Type 4 = 8 | Persistent immobilisation | Single SIJ = 25, Double SIJ = 1, Single SIJ bilaterally = 8 | Plate = 16, Ramus screw = 16 Plate and screw = 1 | All screws augmented with PMMA | X-ray | WBAT | VAS, SF12, LoS | VAS on admission 6.7 admission vs 2.7 day prior to discharge (p = < 0.001) SF12 at 1 year no difference to age matched controls. LoS 14 days |
| Sanders et∼al. 2016 Retrospective case series [30] | 11 | Bilateral sacral = 7 Jumpers variant = 1 unilateral sacral = 2, S1 stress = 1 | Failure of non-operative measures or pain limiting mobilisation | 1 transacral screw = 10, 2 transacral screws = 1 | none | – | X-ray | WBAT | VAS, ODI, LoS, Mortality | 1 year mortaility 10%. Mean VAS 9.1 pre-op vs 3.4 post-op and 2.4 final follow up P = < 0.01. Mean LoS 2.5 days, Mean ODI 71.6 pre-op to 17.6 post-op and 14.6 final follow up p = < 0.01 |
| Collinge et∼al. 2016 Retrospective case series [8] | 24 | OTA B2.2 = 15, B3.3 = 8, C3.2 = 1 | Acute fractures thought to be unstable or with marked pain limiting mobility | Single SIJ screw = 15, Single transacral screw = 9 | none | All screws augmented with CaPO4 | X-ray | WBAT | VAS | Mean VAS 7.9 pre-op vs 3.4 at discharge p = < 0.001. VAS 3.2 at 6 weeks, 2.0 at final follow up |
| Hopf et∼al. 2015 Retrospective case series [19] | 30 | Anterior and posterior = 18, Unilateral posterior = 1, Bilateral posterior = 11 | Persistent pain or unacceptable mobility reduction after 6 days conservative management | Single SIJ = 6, Double SIJ = 12, Triple SIJ = 1, Bilateral SIJ = 2, Bilateral double SIJ = 6, Bilateral triple SIJ = 1, Bilateral SIJ - 2 screws one side, 1 screw other = 2, | none | – | X-ray | WBAT | VAS | Mean VAS 6.8 on admission, 6.0 after bed rest vs 2 days post op VAS 3.6 p = < 0.001, 1.8 on discharge p = < 0.001 |
| Arduini et∼al. 2015 Retrospective case series [31] | 14 | Rommens Type 2 = 3, Type 3 = 9, Type 4 = 2 | 6 months failed conservative treatment | Single SIJ = 8, Plate and screw = 3, Spinopelvic fixation = 2 | Screw = 2, plate = 3, ‘screw or plate in Rommens Type 3’ = 9 | – | X-ray | Bed rest for 4–6 weeks | LoS | LoS 6 days post-op |
| Wahnert et∼al. 2013 Retrospective case series [32] | 12 | “insufficiency fractures” = 12 | 5–7 days conservative treatment without improvement | Single SIJ = 12 | Infix = 3 | All screws augmented with PMMA | CT | WBAT | VAS | Mean VAS 8.2 pre-op vs 2.6 post op (no statistical analysis performed) |
| Gansslen et∼al. 2013 Retrospective case series [7] | 25 | OTA B2.1 = 24, B3.3 = 1 | not described | none | Supra-acetabular external fixator = 25 | – | X-ray | Partial on side of injury | VAS, LoS | Mean VAS pre-op 7.7, Post-op VAS 2.3 (p = < 0.001), Frame removal (mean 4 weeks) VAS 0.6 p = < 0.0003. Average discharge 7 days post op |
| Mehling et∼al. 2012 Retrospective case series [18] | 11 | “insufficiency fractures” | fatigue fracture of sacrum or sacroiliac instability | Transacral bar = 11 | ORIF = 3 | – | X-ray | WBAT | German Multicentre Pelvis Study Group Score | German Multicentre Pelvis Study Group outcome score at 14 months - 7 point scale summarising radiological, clinical and social reintegration. 2 Excellent, 5 Good, 4 Fair |
| Lau et∼al. 2010 Retrospective case series [33] | 37 | Young & Burgess isolated pubic rami = 15, LC1 = 13, LC2 = 9 | not described | Plate = 7 | Screw = 1 | – | X-ray | WBAT | Mortality | 1 year mortality: 27% Rami fractures, 23% LC1, 13% LC2 (Operative intervention in 7/9 LC2 only) |
| Vanderschot et∼al. 2009 Retrospective case series [34] | 19 | Unilateral sacral = 1, Bilateral sacral = 18 | not described | Transacral bar = 19 | none | – | CT | WBAT | VAS | Mean VAS pre-op 6.8 to 2.3 at 9 months (p = < 0.001). LoS 3.6 op vs 4.2 non-op P = 0.51 |
OTA Orthopaedic Trauma Association, LC1 Lateral Compression Type 1, LC2 Lateral Compression Type 2, SIJ Sacroiliac Joint, Infix Internal fixator, PMMA Polymethylmethacrylate, CT Computed Tomography, VAS Visual anologue scale, ODI Oswestry Disability Index, TUG Timed up and go test, LoS Length of Stay, WBAT Weight bear as tolerated, SP Sacroplasty
Quality assessment
Overall the quality of evidence for surgical management of FFP was low. The only randomised trial investigated the outcomes of FFP stabilised with transacral screw fixation with and without additional sacroplasty [25]. This non-blinded study also suffered from a high risk of selection bias, therefore drawing conclusions between the two groups was difficult. Despite this, robust follow-up and comprehensive reporting gave useful information regarding the pre and post-operative outcomes of surgically managed FFP.
The three comparative studies all suffered from high levels of bias. Groups were often poorly matched, had non-standardised interventions and suffered from incomplete follow up. All studies suffered selection bias as only patients in more significant pre-operative pain were selected for operative intervention. Whilst this may reflect a common scenario facing surgeons, drawing firm conclusions between the groups was difficult.
The quality of case series was variable. A common issue with the quality was a lack of pre-operative assessment of outcomes – particularly pain scores. Only six of the 13 case series contained pre-and post-operative/discharge pain scores for comparison. Most had some assessment of mobility or independence but these were often crude and unvalidated scoring systems and assessments that lacked a pre-operative comparison. Exclusion criteria, patient demographics and comorbidities were often poorly described or absent.
Fracture patterns
A number of classification systems were used to classify injuries including the Orthopaedic Trauma Association (OTA) [35], Young and Burgess [36] and Rommen’s [4] classifications. Some studies did not utilise a recognised classification system and described fracture locations or grouped injuries as ‘sacral insufficiency’ fractures. This heterogeneity of fracture classifications made comparisons and analysis difficult between studies. Over 80% of the fractures studied consisted of minimally displaced unilateral or bilateral injuries suitable for percutaneous posterior fixation (Lateral compression type 1, Rommens Type II, OTA type B2). A minority of fractures were more displaced posterior unilateral fractures (5%), Displaced bilateral fractures (5%) and “Sacral U” type fractures (4%). This distribution is similar to those previously described [4, 37].
Fixation methods
Numerous fixation methods were described for anterior and posterior ring injuries. Most patients underwent some form of posterior fixation. Only 26 (6%) patients had anterior fixation alone.
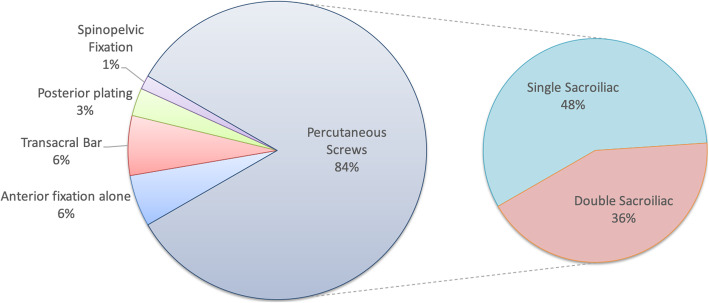
Posterior ring
The majority of studies used percutaneous screws to fix posterior ring injuries. Figure 2 summarises the main methods of posterior fixation. 48% of patients had posterior stabilisation with a single screw whereas 36% had multiple screws. Most screws were SIJ screws crossing a single sacroiliac joint, however 23% of patients had longer transacral screws, passing from one side of the pelvis through both sacroiliac joints to the contralateral ilium [8, 25, 27–30]. 16% of patients received screw augmentation with polymethymethacralate (PMMA) or other void filler [8, 14, 32].
Fig. 2.
Breakdown of posterior fixation strategies
Around 25% of patients had a single, unaugmented SIJ screw. Eckardt examined reoperation rates for different screw configurations. They found a significantly increased reoperation risk when a single SIJ screw (not transacral or augmented) was used for posterior stabilisation regardless of whether the anterior ring was stabilised or not [29].
Two papers, with a total of 30 (6%) patients, described the use of a percutaneous transacral bar [18, 34] to treat bilateral sacral fractures.
There was consistent evidence that pain scores were reduced post-operatively with any percutaneous posterior ring fixation.
Seven patients in one study had plate fixation for their iliac fractures without SIJ screws [33]. Five patients in two studies had their percutaneous screw fixation augmented with a posterior plate [29, 31] and seven patients in three studies had spinopelvic fixation [14, 24, 31]. This method of fixation was reserved for the most complex and displaced fractures, which were not suitable for other less invasive methods of fixation.
Screw augmentation
Five studies used sacroplasty or screw augmentation. Balling et al. performed a prospective randomized study comparing a minimum of two transacral screws with and without PMMA sacroplasty. There was a statistically significant reduction in post-operative VAS scores and Oswestry Disability Index (ODI) scores in both groups but there was no difference between the groups.
Four other case series described screw augmentation. One utilised the technique in some patients but didn’t comment on indications or analyse these patients separately [14]. The others all showed statistically significant improvements in post-operative pain scores. No screw loosening or failure was described in any study [6, 8, 32].
Anterior fixation
Anterior fixation of the pelvic ring was variable. 322 (70%) operatively managed patients had no anterior fixation. Seven studies did not utilise any form of anterior fixation [8, 19, 25, 27, 28, 30, 34]. Some chose to stabilise all the anterior ring injuries with either percutaneous screws or an open reduction and plate fixation [31]. Other studies performed selective fixation for more displaced injuries [6, 14]. One case series used external fixation alone for 4 weeks with significant decrease in post-operative pain [7]. Two studies used an anterior internal fixator (Infix) on seven patients of [24, 32]. Another used a photodynamic bone stabilization system to stabilise rami fractures with concurrent posterior screw fixation [26]. Overall there was no consensus regarding method or indication for anterior fixation.
Pain
Ten studies chose the Visual Analogue Scale (VAS) to quantify pain pre and post-operatively. Post-operative scores were either performed 24–48 h post-operatively or at discharge from hospital but in one case it was performed at an average of 9 months follow up [34]. All these studies in isolation showed a statistically significant improvement in average VAS scores. The average decrease in VAS amongst these studies was 4.5 which exceeds the minimally important clinical difference of 2.0 for patients with low back pain [38]. Only one study with a non-operative comparison group reported on pain pre-injury and on discharge. It showed a significant decrease in VAS from 7.4 pre-operatively to 3.5 in the operative group compared to the non-operative cohort who had an average VAS of 5.7 on admission and 5.1 on discharge. The operative patients had a significantly longer walking distance on discharge and 75% were discharged back home compared to 20% in the non-operative group [27].
Three papers reported VAS post operatively at various timepoints but with no pre-operative comparison. All of these showed low VAS scores, which were comparable to the scores of other studies [14, 26, 29].
Disability/mobility outcomes
A broad selection of disability and quality of life scoring systems were used by authors. Two studies used the Oswestry Disability Index (ODI) questionnaire pre and post-operatively. The randomised study compared transacral screws with and without sacroplasty augmentation and showed a significant average improvement from 86.2 to 30.6 between pre and post-operative assessment but with no significant difference between the two cohorts [25]. One of the better quality case series also showed a significant average improvement from 71.6 to 17.6 after management with a single transacral screw [30]. SF-12 and EQ-5D scores were reported in two studies and found no difference between uninjured comparisons at 1 year [6] or operatively and non-operatively managed patients at 2 years [14].
One retrospective case control study performed Majeed scores at an average of 61 months post operatively and found no significant difference (66.1 operative, vs 65.7 non-op p = 0.91) [24].
Mehling et al. utilised a scoring system by the German Multicentre Pelvic Registry [39] which assesses radiographic, clinical and social reintegration domains. It reported 2 excellent, 5 good and 4 fair results at an average of 14 months follow up, but with no pre-operative comparison [18].
Most studies had an assessment of mobility or degree of post-operative independence. These are summarised in Table 2. Again there was significant heterogeneity in the method and timings of assessment, which made comparisons difficult. One of the cohort studies by Walker et al. showed significantly longer walking distances with operatively managed patients who were also more likely to be discharged home (75% vs 20%) compared to non-operatively managed patients [27].
Table 2.
Mobility/Independence Outcomes
| Author/Year | Mobility/Independence | ||
|---|---|---|---|
| Osterhoff et al. 2019 [24] | 36(24%) patients returned home in operative group compared to 19(23%) in non-operative group | Sanders et al. 2016 [30] | All patients returned to pre injury level of function at an average 625 days of follow up |
| Balling et al. 2019 [25] | All patients discharged when able to mobilise upstairs | Collinge et al. 2016 [8] | Not described |
| Oikonomidis et al. 2019 [26] | Mobility at discharge: 10(31%) crutches, 21(66%) walker/rollator, 1 (3%) unable to mobilise. Follow up at 7 months: 11(34%) independent, 7(22%) crutches, 6(19%) walker, 1(3%) immobile | Hopf et al. 2015 [19] | Complete mobility regained in 73% at discharge |
| Walker et al. 2018 [27] | 75% patients discharged home in operative group compared to 20% in non-operative group (p = < 0.001). Significantly longer walking distance in operative vs non-operative at discharge (95.4 vs 35.2 ft p = < 0.01) | Arduini et al. 2015 [31] | Bed rest 4–6 weeks post op. At 6 months 11 patients (79%) had normal mobility, 1(7%) single crutch, 1 (7%) two crutches |
| Pulley et al. 2018 [28] | Average day 1 mobilisation 102 ft | Wahnert et al. 2013 [32] | All patients could be mobilised to their pre-operative levels |
| Hoch et al. 2017 (1) [6] | Not described | Gansslen et al. 2013 [7] | 24 patients full mobility pre injury and 1 patient mobile with walker. At discharge 14 (58%) regained full mobility. 7 (28%) partial weight bearing. 21 (88%) patients regained baseline mobility at frame removal (average 4 weeks) |
| Eckardt et al. 2017 [29] | 73% independent at home, 13% lost independence. 60% Performed TUG test <30s | Mehling et al. 2012 [18] | Not described |
| Hoch et al. 2017 (2) [14] | At 1 year 9(26%) patients mobile without aids, 6(18%) required 1 or 2 crutches, 12 (35%) with walker | Lau et al. 2010 [33] | At 3 months 53% baseline mobility isolated rami fractures, 62% LC1 and 56% LC2 fractures |
| Vanderschot et al. 209 [34] | 5 point ADL score used. Average 3.26 pre op improved to 1.68 at follow up (P = < 0.0001) at an average of 9 months |
LC1 Lateral Compression Type 1, LC2 Lateral compression type 2, ADL Activities of Daily Living
Length of stay
Walker et al. noted no significant difference in the length of stay between operative and non-operative groups (3.6 vs 4.2 days respectively) [27]. Hoch noted a significantly greater length of stay in operatively treated patients (18 days vs 9 days), although this did include an average of 6 days for an attempt at conservative management pre operatively [14]. Length of stay varied from an average of 2.5 to 16 days in the remaining studies reporting this outcome.
Mortality
Hoch et al. studied mortality rates at 2 years in three cohorts. They noted that 2-year mortality was significantly greater (41%) in the non-operative group compared to the operative and failed non-operative groups (18 and 21% respectively) although the operative group was noted to be younger on average [14]. Another study comparing operative and non-operative groups showed no significant difference in mortality at 1 year (23% vs 17% p = 0.29). It did however, show a survival benefit in the operative group develop after 2 years [24]. Reported 1 year mortality rates ranged from 10 to 27% in other studies.
Complications
Table 3 summarises the complications reported in the included studies. Operative complications were relatively uncommon. The main reasons for reoperation were for symptomatic screw loosening, incorrect screw placement with neurological symptoms and evacuation of post-operative haematoma. One study noted a significant rate of symptomatic screw loosening of 18% where a single percutaneous sacroiliac joint screw was used compared to two screws [29]. Two studies utilizing screw augmentation described a PMMA leak. In one paper there were 4 cases of PMMA extrusion, 2 into the spinal canal but with no symptoms [25]. Another noted asymptomatic PMMA leakage in 3(8%) of cases [6].
Table 3.
Complications and reoperations
| Reoperations (%) | Indications | Other | |
|---|---|---|---|
| Osterhoff et∼al. 2019 [24] | No reoperations reported | – | In hospital complications more common in operative group (35%) vs non-operative group (14%) p = < 0.05 |
| Balling et∼al. 2019 [25] | 1 (2%) | evacuation post op haematoma | 1 guidewire perforation into spinal canal, 4 cases cement extrusion - 2 into canal, 2 into soft tissue. All asymptomatic |
| Oikonomidis et∼al. 2019 [26] | 1 (3%) | Implant failure requiring removal | 2 pneumonia, 4 UTI |
| Walker et∼al. 2018 [27] | No reoperations reported | – | 1 GI bleed in operative group. 1 GI bleed and 2 COPD exacerbations in non-operative group. |
| Pulley et∼al. 2018 [28] | No reoperations reported | – | no complications |
| Hoch et∼al. 2017 (1) [6] | 4 (13%) | 3 screw malposition, 1 revision for infection | 2 patients (4%) required transfusion post op. Medical complications 8% non-operative group, 18% operative group |
| Eckardt et∼al. 2017 [29] | 13 (26%) | 1 screw malposition, 1 infection, 9 for symptomatic implant loosening, 2 patients revised for implant loosening required further revision for non-union | – |
| Hoch et∼al. 2017 (2) [14] | 2 (6%) | 1 screw malposition, 1 evacuation haematoma | 3 asymptomatic PMMA leaks, 1 Pulmonary embolism |
| Sanders et∼al. 2016 [30] | No reoperations reported | – | No complications |
| Collinge et∼al. 2016 [8] | No reoperations reported | – | 1 extravasation of calcium phosphate into sacroiliac joint - asymptomatic |
| Hopf et∼al. 2015 [19] | 3 (10%) | 1 screw malposition, 2 evacuation haematoma | 1 intraoperative bleed requiring 3 units blood. 2 cases HAP and 2 Cases UTI in 3 patients |
| Arduini et∼al. 2015 [31] | No reoperations reported | – | 1 intrapelvic iliac screw from spinopelvic fixation - asymptomatic and left in situ |
| Wahnert et∼al. 2013 [32] | No reoperations reported | – | No complications |
| Gansslen et∼al. 2013 [7] | No unplanned reoperations reported | All patients required planned removal of external fixator in outpatient setting | 2 pin site infections managed with antibiotics. 1 pin loosening. |
| Mehling et∼al. 2012 [18] | No reoperations reported | – | 1 temporary L5 nerve palsy |
| Lau et∼al. 2010 [33] | No reoperations reported | – | 1 fibrous non-union. 1 permanent L5 nerve palsy |
| Vanderschot et∼al. 2009 [34] | 2 (11%) | 2 evacuation post op haematoma | – |
UTI Urinary Tract Infection, GI Gastrointestinal, COPD Chronic Obstructive Pulmonary Disease, PMMA Polymethylmethacrylate, HAP Hospital Acquired Pneumonia
Discussion
Traditionally FFP have been managed non-operatively, often with a period of bed rest with analgesia and then mobilisation [5, 40]. Knowledge regarding the detrimental effect of bed rest and immobility in the elderly population has been present for decades [41]. Even short periods of immobilisation or decreased mobility lead to prolonged loss of muscle strength [42]. As a consequence there is reduced capacity to perform activities of daily living leading to loss of independence [43, 44]. Mortality from non-operatively managed pelvic fractures is also similar to matched patients treated for hip fracture [45].
Elderly patients are unable to comply with restricted weightbearing regimes [46] – any management strategy should facilitate immediate full weight bearing with sufficient control of pain. This review highlights that whilst the quality of evidence for surgical fixation of FFP is poor, there is consistent data to support the idea that the majority of fracture patterns can be stabilised through minimally invasive methods, with a consequent reduction in pain. Whether this assertion is correct or if it translates to outcomes with regards mobility, length of stay, quality of life and mortality needs further investigation.
A heterogenous selection of fracture classifications were used by the studies, which made comparisons difficult. FFP often do not fit well into the OTA, Tile or Young and Burgess classifications as elderly patients tend to have bony injuries rather than ligamentous involvement [4, 8]. Recognising this, the Rommen’s classification was developed specifically for these injuries and may be more useful in classifying these injuries in the future [47].
The decision to pursue operative intervention in most of the studies was made after failure of conservative measures rather than based on fracture morphology. Whilst some unstable fractures may mandate surgical intervention, the commonest minimally displaced posterior injuries and even some more extensive and displaced injuries may be managed successfully with conservative measures. Conservative management was normally instituted for a period of 3–7 days although it did range up to 6 months. Given that relatively short periods of immobility can lead to significant morbidity we would suggest considering intervention after 48 h of failed conservative management and ideally within 1 week to avoid complications associated with prolonged immobility.
With regard to fixation techniques, when stabilising the posterior ring, the majority of authors utilised percutaneous posterior fixation where possible. Biomechanical studies have shown that two SIJ screws, a single augmented SIJ screw and a single transacral screw offer similar levels of stability and are all superior to single SIJ screw fixation in osteoporotic models [48–52]. There is some clinical evidence identified in this review that highlights a significantly increased rate of screw loosening when one unaugmented SIJ screw was used in isolation [29]. This finding was independent of whether or not the anterior ring was stabilised. We would suggest that a single un-augmented SIJ screw may not provide sufficient stability in the osteoporotic patient to facilitate early full weightbearing and adequate pain relief. Either multiple screws, longer transacral screws, or screw augmentation should be considered. Surgeons should be mindful of the potential additional risks and benefits of each option.
Supplementary anterior fixation was sporadic if present and there was no correlation between lack of anterior fixation and overall fixation failure. Tile noted that the posterior ring contributes around 60% to pelvic stability [53] and Matta confirmed that even in unstable pelvic injuries rami fractures did not require stabilization by internal or external fixation when the posterior ring was stabilised [54]. The data presented here would support the assertion that posterior fixation in these injuries is more critical than anterior fixation. Stabilising the anterior ring contributes to overall pelvic stability and this may understandably be desirable to surgeons managing osteoporotic FFP. Percutaneous screw fixation of the ramus is an attractive option in minimally displaced fractures, however there is some biomechanical evidence in osteoporotic bone that plate fixation is superior to percutaneous retrograde screw fixation, the trade-off being that this requires an open approach [55]. External fixation is a quick and relatively easy technique but its use in the osteoporotic patient raises concerns with regard to pin-site infection, loosening and patient acceptance [4]. The Infix is a newer development and current trials are ongoing to identify whether it is a suitable method for stabilising osteoporotic type 1 lateral compression fractures [56], however its use is also not without complications [57]. A large study of the German pelvic database comparing Tile B and C type pelvic fractures with the anterior component involving the obturator foramen showed a higher rate of complications from more extensive anterior and posterior surgery compared to posterior stabilization alone with no difference in fixation failure or mortality [58]. When electing to stabilise FFP, surgeons should be mindful that supplementary anterior fixation may not be necessary with a robust posterior fixation. If electing to stabilise the anterior ring, surgeons should be mindful of potential complications associated with the chosen method. Anterior fixation alone may be appropriate depending on the strength of fixation and degree of posterior instability [7].
Observed complications from surgical interventions were low. Most studies used either computed tomography (CT) guidance or fluoroscopy to insert screws. Incorrect screw placement was noted with both techniques but was infrequent and any iatrogenic neurological deficits resolved after removal and repositioning [6, 14, 19, 29].
We noted a previous systematic review of four studies on the effectiveness of surgical fixation of osteoporotic LC1 fractures. This found insufficient evidence to support guidance on the most effective treatment for patients sustaining this injury however where reported, mobility and function did improve after surgery [59]. This systematic review is a more comprehensive overview of 17 studies encompassing all types of FFP.
This systematic review does have some weaknesses. Firstly there was a lack of good quality randomised studies on which to base conclusions and most studies suffered from significant risk of bias. There was also significant heterogeneity in fracture classification and outcome measures. This made appropriate data pooling and analysis between studies difficult. We also excluded trials with less than 10 patients and excluded papers where an English translation could not be obtained. This only resulted in the loss of a small number of cases and therefore was unlikely to change the overall impression of the review.
Conclusion
This systematic review set out to identify the evidence for surgical management of FFP. Overall the quality of evidence was low. Of the 17 studies identified only one was randomised but with high risk of bias. Three studies were identified with a non-operative comparator group but all suffered from significant bias. Despite this, consistent improvement in pain and mobility was noted with stabilisation of the pelvis, which was most often performed percutaneously to the posterior ring. Anterior fixation of the pelvic ring was often absent and variable techniques were used when present. More than one SIJ screw posteriorly, longer transacral screws or screw augmentation offer more robust fixation than single SIJ screws for stabilising the pelvis, especially in the context of osteoporosis. Surgeons should consider operative stabilisation of FFP after a brief period of conservative management to avoid morbidity associated with immobility.
Supplementary Information
Additional file 1. Example of EMBASE search strategy.
Acknowledgements
The authors would like to acknowledge Tom Roper, Clinical Librarian, Brighton and Sussex University Hospitals NHS Trust for his assistance in conducting the literature search.
Abbreviations
- FFP
Fragility fracture of the pelvis
- PROSPERO
International prospective register of systematic reviews
- PRISMA
Preferred reporting instructions for systematic review and meta-analysis
- NHS
National Health Service
- SIJ
Sacroiliac Joint
- OTA
Orthopaedic Trauma Association
- PMMA
Polymethylmethacrylate
- VAS
Visual analogue scale
- ODI
Oswestry Disability Index
- CT
Computed tomography
Authors’ contributions
DW: methodology, search, study selection and analysis, writing and editing paper, read and approved manuscript. JK: study selection and analysis, writing and editing paper, read and approved manuscript. MR: concept, methodology, editing paper, study selection, read and approved manuscript. The author(s) read and approved the final manuscript.
Funding
No funding was received by any author for preparation of this manuscript.
Availability of data and materials
The datasets analysed and/or created where not presented are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Ethical approval was not sought as this was a review of completed research studies with individual ethical approval.
Consent for publication
Not applicable.
Competing interests
The authors declare they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Boufous S, Finch C, Lord S, Close J. The increasing burden of pelvic fractures in older people, New South Wales, Australia. Injury. 2005;36(11):1323–1329. doi: 10.1016/J.INJURY.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 2.Rollmann MF, Herath SC, Kirchhoff F, Braun BJ, Holstein JH, Pohlemann T, Menger MD, Histing T. Pelvic ring fractures in the elderly now and then – a pelvic registry study. Arch Gerontol Geriatr. 2017;71:83–88. doi: 10.1016/J.ARCHGER.2017.03.007. [DOI] [PubMed] [Google Scholar]
- 3.Kannus P, Palvanen M, Niemi S, Parkkari J, Järvinen M. Epidemiology of osteoporotic pelvic fractures in elderly people in Finland: sharp increase in 1970-1997 and alarming projections for the new millennium. Osteoporos Int. 2000;11(5):443–448. doi: 10.1007/s001980070112. [DOI] [PubMed] [Google Scholar]
- 4.Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: recommendations for surgical treatment. Injury. 2013;44(12):1733–1744. doi: 10.1016/j.injury.2013.06.023. [DOI] [PubMed] [Google Scholar]
- 5.Gotis-Graham I, McGuigan L, Diamond T, Portek I, Quinn R, Sturgess A, Tulloch R. Sacral insufficiency fractures in the elderly. J Bone Joint Surg Br. 1994;76-B(6):882–886. doi: 10.1302/0301-620X.76B6.7983111. [DOI] [PubMed] [Google Scholar]
- 6.Höch A, Pieroh P, Henkelmann R, Josten C, Böhme J. In-screw polymethylmethacrylate-augmented sacroiliac screw for the treatment of fragility fractures of the pelvis: a prospective, observational study with 1-year follow-up. BMC Surg. 2017;17(1):132. doi: 10.1186/S12893-017-0330-Y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gänsslen A, Hildebrand F, Kretek C. Supraacetabular external fixation for pain control in geriatric type B pelvic injuries. Acta Chir Orthop Traumatol Cechoslov. 2013;80(2):101–105. [PubMed] [Google Scholar]
- 8.Collinge CA, Crist BD. Combined percutaneous Iliosacral screw fixation with Sacroplasty using Resorbable calcium phosphate cement for osteoporotic pelvic fractures requiring surgery. J Orthop Trauma. 2016;30(6):e217–e222. doi: 10.1097/BOT.0000000000000520. [DOI] [PubMed] [Google Scholar]
- 9.Kortebein P, Symons TB, Ferrando A, Paddon-Jones D, Ronsen O, Protas E, Conger S, Lombeida J, Wolfe R, Evans WJ. Functional impact of 10 days of bed rest in healthy older adults. J Gerontol Ser A Biol Sci Med Sci. 2008;63(10):1076–1081. doi: 10.1093/gerona/63.10.1076. [DOI] [PubMed] [Google Scholar]
- 10.Alnaib M, Waters S, Shanshal Y, Caplan N, Jones S, St Clair Gibson A, Kader D. Combined pubic rami and sacral osteoporotic fractures: a prospective study. J Orthop Traumatol. 2012;13(2):97–103. doi: 10.1007/s10195-012-0182-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.van Dijk WA, Poeze M, van Helden SH, Brink PRG, Verbruggen JPAM. Ten-year mortality among hospitalised patients with fractures of the pubic rami. Injury. 2010;41(4):411–414. doi: 10.1016/J.INJURY.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 12.Koval KJ, Aharonoff GB, Schwartz MC, Alpert S, Cohen G, McShinawy A, Zuckerman JD. Pubic rami fracture: a benign pelvic injury? J Orthop Trauma. 1997;11(1):7–9. doi: 10.1097/00005131-199701000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Breuil V, Roux CH, Testa J, Albert C, Chassang M, Brocq O, Euller-Ziegler L. Outcome of osteoporotic pelvic fractures: an underestimated severity. Survey of 60 cases. Jt Bone Spine. 2008;75(5):585–588. doi: 10.1016/J.JBSPIN.2008.01.024. [DOI] [PubMed] [Google Scholar]
- 14.Höch A, Özkurtul O, Pieroh P, Josten C, Böhme J. Outcome and 2-year survival rate in elderly patients with lateral compression fractures of the pelvis. Geriatr Orthop Surg Rehabil. 2017;8(1):3–9. doi: 10.1177/2151458516681142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fritz A, Gericke L, Höch A, Josten C, Osterhoff G. Time-to-treatment is a risk factor for the development of pressure ulcers in elderly patients with fractures of the pelvis and acetabulum. Injury. 2020;51(2):352–356. doi: 10.1016/j.injury.2019.12.007. [DOI] [PubMed] [Google Scholar]
- 16.Heinrich S, Rapp K, Rissmann U, Becker C, König H-H. Cost of falls in old age: a systematic review. Osteoporos Int. 2010;21(6):891–902. doi: 10.1007/s00198-009-1100-1. [DOI] [PubMed] [Google Scholar]
- 17.Schmitz P, Lüdeck S, Baumann F, Kretschmer R, Nerlich M, Kerschbaum M. Patient-related quality of life after pelvic ring fractures in elderly. Int Orthop. 2019;43(2):261–267. doi: 10.1007/s00264-018-4030-8. [DOI] [PubMed] [Google Scholar]
- 18.Mehling I, Hessmann MH, Rommens PM. Stabilization of fatigue fractures of the dorsal pelvis with a trans-sacral bar. Oper Tech Outcome Injury. 2012;43(4):446–451. doi: 10.1016/j.injury.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Hopf JC, Krieglstein CF, Müller LP, Koslowsky TC. Percutaneous iliosacral screw fixation after osteoporotic posterior ring fractures of the pelvis reduces pain significantly in elderly patients. Injury. 2015;46(8):1631–1636. doi: 10.1016/j.injury.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 20.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339(jul21 1):b2700. doi: 10.1136/bmj.b2700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Higgins JPT, Altman DG, Gøtzsche PC, Jüni P, Moher D, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(oct18 2):343. doi: 10.1136/BMJ.D5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sterne JA, Hernán MA, Reeves BC, Savović J, Berkman ND, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919. doi: 10.1136/bmj.i4919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, et al. Joanna Briggs institute reviewers Maunal. In: Aromatis E, Munn Z, et al., editors. Joanna Briggs institute reviewers manual. 2017. [Google Scholar]
- 24.Osterhoff G, Noser J, Held U, Werner CML, Pape H-C, Dietrich M. Early operative versus nonoperative treatment of fragility fractures of the pelvis. J Orthop Trauma. 2019;33(11):e410–e415. doi: 10.1097/BOT.0000000000001584,. [DOI] [PubMed] [Google Scholar]
- 25.Balling H. Additional Sacroplasty does not improve clinical outcome in minimally invasive navigation-assisted screw fixation procedures for nondisplaced insufficiency fractures of the sacrum. Spine (Phila Pa 1976) 2019;44(8):534–542. doi: 10.1097/BRS.0000000000002899. [DOI] [PubMed] [Google Scholar]
- 26.Oikonomidis S, Alabsi A, Ashqar G, Graf M, Sobottke R. Intramedullary stabilization of pubic ramus fractures in elderly patients with a photodynamic bone stabilization system (IlluminOss) Geriatr Orthop Surg Rehabil. 2019;10:1–8. doi: 10.1177/2151459318824904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Walker JB, Mitchell SM, Karr SD, Lowe JA, Jones CB. Percutaneous Transiliac–Transsacral screw fixation of sacral fragility fractures improves pain, ambulation, and rate of disposition to home. J Orthop Trauma. 2018;32(9):452–456. doi: 10.1097/BOT.0000000000001243. [DOI] [PubMed] [Google Scholar]
- 28.Pulley BR, Cotman SB, Fowler TT. Surgical fixation of geriatric sacral U-type insufficiency fractures. J Orthop Trauma. 2018;32(12):617–622. doi: 10.1097/BOT.0000000000001308. [DOI] [PubMed] [Google Scholar]
- 29.Eckardt H, Egger A, Hasler RM, Zech CJ, Vach W, Suhm N, Morgenstern M, Saxer F. Good functional outcome in patients suffering fragility fractures of the pelvis treated with percutaneous screw stabilisation: assessment of complications and factors influencing failure. Injury. 2017;48(12):2717–2723. doi: 10.1016/j.injury.2017.11.002. [DOI] [PubMed] [Google Scholar]
- 30.Sanders D, Fox J, Starr A, Sathy A, Chao J. Transsacral-Transiliac screw stabilization: effective for recalcitrant pain due to sacral insufficiency fracture. J Orthop Trauma. 2016;30(9):469–473. doi: 10.1097/BOT.0000000000000596. [DOI] [PubMed] [Google Scholar]
- 31.Arduini M, Saturnino L, Piperno A, Iundusi R, Tarantino U. Fragility fractures of the pelvis: treatment and preliminary results. Aging Clin Exp Res. 2015;27(S1):61–67. doi: 10.1007/s40520-015-0430-4. [DOI] [PubMed] [Google Scholar]
- 32.Wähnert D, Raschke MJ, Fuchs T. Cement augmentation of the navigated iliosacral screw in the treatment of insufficiency fractures of the sacrum. A new method using modified implants. Int Orthop. 2013;37(6):1147–1150. doi: 10.1007/s00264-013-1875-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lau T-W, Leung F. Occult posterior pelvic ring fractures in elderly patients with osteoporotic pubic rami fractures. J Orthop Surg. 2010;18(2):153–157. doi: 10.1177/230949901001800205. [DOI] [PubMed] [Google Scholar]
- 34.Vanderschot P, Kuppers M, Sermon A, Lateur L. Trans-iliac-sacral-iliac-bar procedure to treat insufficiency fractures of the sacrum. Indian J Orthop. 2009;43(3):245–252. doi: 10.4103/0019-5413.53454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Meinberg E, Agel J, Roberts C, Karam M, Kellam J. Fracture and dislocation classification compendium—2018. J Orthop Trauma. 2018;32(1):S1–S10. doi: 10.1097/BOT.0000000000001063. [DOI] [PubMed] [Google Scholar]
- 36.Manson T, O’Toole RV, Whitney A, Duggan B, Sciadini M, et al. Young-burgess classification of pelvic ring fractures: does it predict mortality, transfusion requirements, and non-orthopaedic injuries? J Orthop Trauma. 2010;24(10):603–609. doi: 10.1097/BOT.0b013e3181d3cb6b. [DOI] [PubMed] [Google Scholar]
- 37.Rommens PM, Arand C, Hopf JC, Mehling I, Dietz SO, Wagner D. Progress of instability in fragility fractures of the pelvis: an observational study. Injury. 2019;50(11):1966–1973. doi: 10.1016/j.injury.2019.08.038. [DOI] [PubMed] [Google Scholar]
- 38.Hägg O, Fritzell P, Nordwall A, Swedish Lumbar Spine Study Group The clinical importance of changes in outcome scores after treatment for chronic low back pain. Eur Spine J. 2003;12(1):12–20. doi: 10.1007/s00586-002-0464-0. [DOI] [PubMed] [Google Scholar]
- 39.Pohlemann T, Tosounidis G, Bircher M, Giannoudis P, Culemann U. The German multicentre pelvis registry: a template for an European expert network? Injury. 2007;38(4):416–423. doi: 10.1016/j.injury.2007.01.007. [DOI] [PubMed] [Google Scholar]
- 40.Babayev M, Lachmann E, Nagler W. The controversy surrounding sacral insufficiency fractures. Am J Phys Med Rehabil. 2000;79(4):404–409. doi: 10.1097/00002060-200007000-00014. [DOI] [PubMed] [Google Scholar]
- 41.Creditor MC. Hazards of hospitalization of the elderly. Ann Intern Med. 1993;118(3):219–223. doi: 10.7326/0003-4819-118-3-199302010-00011. [DOI] [PubMed] [Google Scholar]
- 42.Hvid LG, Suetta C, Nielsen JH, Jensen MM, Frandsen U, Ørtenblad N, Kjaer M, Aagaard P. Aging impairs the recovery in mechanical muscle function following 4days of disuse. Exp Gerontol. 2014;52:1–8. doi: 10.1016/j.exger.2014.01.012. [DOI] [PubMed] [Google Scholar]
- 43.Bell KE, von Allmen MT, Devries MC, Phillips SM. Muscle disuse as a pivotal problem in sarcopenia-related muscle loss and dysfunction. J frailty aging. 2016;5:33–41. doi: 10.14283/jfa.2016.78. [DOI] [PubMed] [Google Scholar]
- 44.Sonn U. Longitudinal studies of dependence in daily life activities among elderly persons. Scand J Rehabil Med Suppl. 1996;34:1–35. [PubMed] [Google Scholar]
- 45.Reito A, Kuoppala M, Pajulammi H, Hokkinen L, Kyrölä K, Paloneva J. Mortality and comorbidity after non-operatively managed, low-energy pelvic fracture in patients over age 70: a comparison with an age-matched femoral neck fracture cohort and general population. BMC Geriatr. 2019;19(1):315. doi: 10.1186/s12877-019-1320-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kammerlander C, Pfeufer D, Lisitano LA, Mehaffey S, Böcker W, Neuerburg C. Inability of older adult patients with hip fracture to maintain postoperative weight-bearing restrictions. J Bone Jt Surg. 2018;100(11):936–941. doi: 10.2106/JBJS.17.01222. [DOI] [PubMed] [Google Scholar]
- 47.Pieroh P, Höch A, Hohmann T, Gras F, Märdian S, Pflug A, Wittenberg S, Ihle C, Blankenburg N, Dallacker-Losensky K, Schröder T, Herath SC, Wagner D, Palm HG, Josten C, Stuby FM. Fragility fractures of the pelvis classification. J Bone Jt Surg. 2019;101(11):987–994. doi: 10.2106/JBJS.18.00930. [DOI] [PubMed] [Google Scholar]
- 48.Oberkircher L, Masaeli A, Bliemel C, Debus F, Ruchholtz S, Krüger A. Primary stability of three different iliosacral screw fixation techniques in osteoporotic cadaver specimens—a biomechanical investigation. Spine J. 2016;16(2):226–232. doi: 10.1016/j.spinee.2015.08.016. [DOI] [PubMed] [Google Scholar]
- 49.König A, Oberkircher L, Beeres FJP, Babst R, Ruchholtz S, Link BC. Cement augmentation of sacroiliac screws in fragility fractures of the pelvic ring—a synopsis and systematic review of the current literature. Injury. 2019;50(8):1411–1417. doi: 10.1016/j.injury.2019.06.025. [DOI] [PubMed] [Google Scholar]
- 50.van Zwienen CMA, van den Bosch EW, Snijders CJ, Kleinrensink GJ, van Vugt AB. Biomechanical comparison of sacroiliac screw techniques for unstable pelvic ring fractures. J Orthop Trauma. 2004;18(9):589–595. doi: 10.1097/00005131-200410000-00002. [DOI] [PubMed] [Google Scholar]
- 51.Suero EM, Greiner A, Becker CA, Cavalcanti Kußmaul A, Weidert S, Pfeufer D, et al. Biomechanical stability of sacroiliac screw osteosynthesis with and without cement augmentation. Injury. 2020. 10.1016/j.injury.2020.01.043. [DOI] [PubMed]
- 52.Osterhoff G, Dodd AE, Unno F, Wong A, Amiri S, Lefaivre KA, Guy P. Cement augmentation in sacroiliac screw fixation offers modest biomechanical advantages in a cadaver model. Clin Orthop Relat Res. 2016;474(11):2522–2530. doi: 10.1007/s11999-016-4934-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Vrahas M, Hern TC, Diangelo D, Kellam J, Tile M. Ligamentous contributions to pelvic stability. Orthopedics. 1995;18(3):271–274. doi: 10.3928/0147-7447-19950301-09. [DOI] [PubMed] [Google Scholar]
- 54.Matta J. Indications for anterior fixation of pelvic fractures. Clin Orthop Relat Res. 1996;329:88–96. doi: 10.1097/00003086-199608000-00011. [DOI] [PubMed] [Google Scholar]
- 55.Acklin YP, Zderic I, Buschbaum J, Varga P, Inzana JA, Grechenig S, Richards RG, Gueorguiev B, Schmitz P. Biomechanical comparison of plate and screw fixation in anterior pelvic ring fractures with low bone mineral density. Injury. 2016;47(7):1456–1460. doi: 10.1016/j.injury.2016.04.013. [DOI] [PubMed] [Google Scholar]
- 56.ISRCTN - ISRCTN16478561: Surgical vs conservative treatment of LC1 pelvic fractures in the elderly. http://www.isrctn.com/ISRCTN16478561. Accessed 28 May 2020.
- 57.Vaidya R, Woodbury D, Nasr K. Anterior subcutaneous internal pelvic fixation/INFIX. J Orthop Trauma. 2018;32(6):S24–S30. doi: 10.1097/BOT.0000000000001248. [DOI] [PubMed] [Google Scholar]
- 58.Schmal H, Froberg LS, Larsen M, Südkamp NP, Pohlemann T, et al. Evaluation of strategies for the treatment of type B and C pelvic fractures. Bone Joint J. 2018;100-B(7):973–983. doi: 10.1302/0301-620X.100B7.BJJ-2017-1377.R1. [DOI] [PubMed] [Google Scholar]
- 59.Booth A, Ingoe HMA, Northgraves M, Coleman E, Harden M, Kassam J, Kwok I, Hilton C, Bates P, McDaid C. Effectiveness of surgical fixation for lateral compression type one (LC-1) fragility fractures of the pelvis: a systematic review. BMJ Open. 2019;9(5):e024737. doi: 10.1136/bmjopen-2018-024737. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Example of EMBASE search strategy.
Data Availability Statement
The datasets analysed and/or created where not presented are available from the corresponding author on reasonable request.