Abstract
Data from a survey of 1478 travelers and multistep group structural equation model analysis revealed that the Health Belief Model constructs of cues to action (trust in third-party information sources), perceived severity of and susceptibility to COVID-19, and beliefs about the protection benefits of a COVID-19 vaccine, subsequently elicited willingness to vaccinate and beliefs that others should vaccinate prior to travel and enhanced support for pre-travel vaccination mandates. Also, significant differences in the perceived protection benefits of the vaccine and willingness to vaccinate were found across groups of travelers who travel more or less frequently and those with and without a prior positive test for COVID-19. The study provides a theoretically informed understanding of the dynamics that may enable the success of important health-related travel policy in the wake of COVID-19 and future pandemics and identifies the communication mechanisms that must be leveraged by governments and travel authorities in enforcing policy.
Keywords: COVID-19, Willingness to vaccinate, COVID-19 vaccination, Health Belief Model, Regulation
1. Introduction
The rapid spread of COVID-19 and the drastic decrease in global travel has been accompanied by an increase in research on the tourism industry's resilience and economic recovery. While researchers have examined a variety of topics pertaining to travel and COVID-19 (Luo & Lam, 2020), beliefs about contracting COVID-19 and spreading it to others and travel intentions in the ongoing pandemic have emerged as more immediate areas of interest (Adongo et al., 2021). More specifically, it is undeniable that vaccination is intended to help reduce the spread of COVID-19 (Wong, Alias, Wong, Lee, & AbuBakar, 2020) and, in doing so, facilitate leisure travel. By the end of 2020, many institutions, including governments, medical and pharmaceutical companies, and private organizations rushed to develop a vaccine for COVID-19, with some products in nascent stages of distribution. Given the rapid progress on vaccine administration for COVID-19, immediate investigation on uptake is merited to forecast adoption by the public (Böhm et al., 2019; Betsch, 2019 Dodd et al., 2020; Neumann-Böhme et al., 2020; Wong et al., 2020). Moreover, as COVID-19 vaccinations become widespread, international authorities may require travelers to vaccinate before they can apply for visas to travel abroad. For example, Qantas was among the first airlines to announce the prospect of a “vaccination passport” (Bloomberg, 2020), with digital technologies rapidly implemented. Such initiatives are critical to the recovery of global business and leisure travel and the resumption of global economic activity to pre-pandemic levels.
In a travel context, some research has been undertaken to understand travelers’ willingness to vaccinate(Adongo et al., 2021; Baeyens, 2010; Goldman et al., 2020; Kreps et al., 2020; Smith, Khairullah, Song, Chen, & Torresi, 2004; Schunk, Wachinger, & Nothdurft, 2001; Seale, Kaur, Mahimbo, MacIntyre, Zwar, Smith, Worth, & Heywood, 2016; Toovey, Jamieson, & Holloway, 2004). However, the present situation with the COVID-19 pandemic is significantly more serious, and the successful resumption of global travel relies heavily on society having achieved some level of herd immunity Centers for Disease Control and Prevention (2021), 2021, U.S. Travel Association, 2021; Spinks, 2020). If the availability of COVID-19 vaccination represents a game changer to stimulate increased travel (Read, 2020; Wilson & Chen, 2020) then the beliefs of individuals surround the need for the vaccine, particularly as a requirement for travel, are important to understand. This is particularly relevant in the context of governments and businesses, and more airlines (Pitrelli, 2021), mulling vaccination mandates for travel. As indicated by Hall, Scott, and Gössling (2020):
We are likely [to] see a scenario in which medical certificates (for either being clear of, or having had the disease), clearances and vaccination, when eventually available for COVID-19, may come to be required for entry and for tourist visas being granted, in a similar fashion to what is already commonplace for some destinations or for the short-term movement of natural persons for employment or study purposes (p. 588).
Research that leverages health behavior theory to support or reject the underlying basis for such policy is lacking in the tourism literature more generally and in the specific case of COVID-19 (French, 2020). In light of this gap, the present study develops a Health Belief Model (HBM) to provide a better understanding of an emerging phenomenon of vaccination intention and support for requirements to vaccinate in the travel industry. While developed in the context of COVID-19 and travel for the purpose of leisure or vacation, the present study's framework can be applied to future research that comprehensively examines the dynamics of diverse travel-related intentions and beliefs about vaccination in the midst of pandemics. From a practitioner standpoint, the present study offers current intervention strategies surrounding the critical implementation of pre-travel vaccination mandates by national and international governments, transportation authorities, and tourism industries, to reduce spread of COVID-19.
2. Literature review
2.1. COVID-19 and the travel industry
Tourism is among the world's largest industries, having grown to $8.8 trillion in 2018, with a 3.5% increase in 2019, and it was predicted to grow on average 3–5% each year through 2023 (World Travel & Tourism Council [WTTC], 2020). Particularly, travel from the United States increased steadily over the last decade, with a notable rise in the past two years due mostly to the strong dollar, reaching 97 million outbound trips in 2019 (World Bank, 2020). However, in December 2019, COVID-19—severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)—advanced to a global pandemic within a month (Lu, Stratton, & Tang, 2020) and brought domestic and international travel to an abrupt halt. In fact, analysts predeicted U.S. outbound travel to have plummeted by approximately 80% near the end of 2020 (Deloitte, 2020). In addition to outbound travel, inbound travel into the United States, accounting for 79 million inbound trips in 2019, decreased overall by approximately 40% (Deloitte, 2020).
Several countries have implemented measures against international visitor arrivals from countries with high infection incidences (e.g., United States, Spain, Iran, China, Italy). Namely, outbound travelers from the United States, a significant economic source ($139 billion), have been unwelcome in many nations abroad. Moreover, recent news highlights that domestic and international travel authorities will require proof of vaccination and registry prior to travel in the future (Press Associated, 2020). For example, Australia has been among the first countries to portend requiring evidence of a COVID-19 vaccination prior to issuing visas for entry to the country. Relatedly, Qantas airlines announced their advocacy of proof of vaccination for Australian inbound travelers and suggested a “vaccination passport” for international travelers (Ryan and Patel, 2020). In the United States, two river cruise companies announced a COVID-19 vaccination mandate for guests and crew for all sailing beginning July 2021 (Burke, 2021).
From a public health perspective, vaccination is considered to be the most effective approach to combat the spread of infectious diseases (Kennedy, LaVail, Nowak, Basket, & Landry, 2011). In the past, outbreaks of contagious diseases such as cholera, Ebola virus, SARS, influenza A (H1N1), and avian influenza (H5N1) were best controlled by vaccination (Myers & Goodwin, 2012; Palache, 2011; Scherr, Jensen, & Christy, 2016). Vaccines are also the most efficient means of controlling ongoing infectious diseases spread through travel, including malaria, diphtheria, hepatitis A and B, and tuberculosis (Toovey et al., 2016) and often recommended to visitors of countries where the diseases are still prevalent (Seale et al., 2016). Similarly, it is undeniable that a vaccination would help manage the spread of COVID-19 (Neumann-Böhme et al., 2020; Wong et al., 2020), and, in doing so, facilitate travel. However, uptake has been contentious (Palamenghi et al., 2020) moreover, antivaccine movements are common and characterized as a ‘public health crisis’ by Schunk et al. (2001). Extant literature highlights many adults electing not to vaccinate both themselves and their children against a variety of infectious diseases, citing ignorance of the risks about related diseases, relevant facts, financial expenses, unfounded fears of side effects, and doubt of 100% effectiveness, as the factors influencing their decisions not to vaccinate (Baeyens, 2010; Goldman et al., 2020; Hoeffe, 2020). Such anti-vaccine sentiment has also been prevelant in the United States in response to the COVID-19 pandemic (Chabria, 2020; Wu, 2020).
In light of the questions surrounding vaccination uptake and its implications for the resumption of travel activity amidst ongoing COVID-19 infections, the Health Belief Model (HBM) can be employed to determine vaccination intention in the current context. Previously, Wong et al. (2020) assessed the predictors of intention to receive a COVID-19 vaccine using the HBM framework and found that key constructs of the model—high-perceived benefits, lower perceived barriers, and higher perceived susceptibility—were significantly related to intentions to vaccinate . Based on this research, there is a strong case for suggesting that HBM could also be used to explain travelers’ vaccination intentions in addition to support for vaccination requirements for travelers, as national and international vaccination mandates are likely to become commonplace in an effort to safely resume domestic and global travel activity (Hall et al., 2020). Thus, the present study leverages HBM to provide a better understanding of the dynamics of vaccination intention as a determinant of successful travel health policy.
2.2. The Health Belief Model
The Health Belief Model (HBM) is a framework that “has been one of the most widely used conceptual frameworks in health behavior research, both to explain change and maintenance of health-related behaviors and as a guiding framework for interventions” (Champion & Skinner, 2008, p. 45). The HBM comprises the following key constructs: perceived susceptibility, perceived severity, perceived benefits, perceived barriers, self-efficacy to engage in a behavior, and cues to action (Champion & Skinner, 2008, p. 45). According to Rosenstock (1974b), HBM was developed to explain preventive health behavior and originated from the research of Hochbaum in 1952, which explored hidden factors that influence chest X-ray decisions in order to detect tuberculosis (Tarkang & Zotor, 2015). At the time, there was a widespread failure among the population to participate in preventive actions such as screening tests for early detection (Rosenstock, 1974a). HBM has since expanded and evolved (Carpenter, 2010; Champion & Skinner, 2008, pp. 45–65; Erkin and Özsoy, 2012; Gillam, 1991; Harrison et al., 1989; Jones et al., 2014; Manika and Golden, 2011) and has been used in preventative vaccination research (Coe, Gatewood, & Moczygemba, 2012; Marlow, Waller, Evans, & Wardle, 2009) and to explain behavior amidst COVID-19 (Carico et al., 2020; Mukhtar, 2020).
Applied to explain vaccination intention, HBM has been specified in research on a plethora of diseases, both noninfectious or infectious, such as dengue fever, human papillomavirus, seasonal influenza, and influenza A (Lennon, 2005; Marlow et al., 2009; Nexøe, Kragstrup, & Søgaard, 1999; Najimi & Golshiri, 2013; Manika & Golden, 2011; Scherr et al., 2016; Cummings, Jette, Brock, & Haefner, 1979; Setbon & Raude, 2010; Zijtregtop et al., 2009; Coe et al., 2012). For the novel (2009) H1N1 influenza vaccine, Coe et al. (2012) found that most participants in their study recognized the risk of the novel H1N1 virus and indicated their intention to receive the vaccine. Further, their study showed that perceived clinical barriers, history of receiving the previous year's seasonal influenza vaccine, and physicians' recommendations were significant predictors of intention to receive a vaccination. Similarly, Nexøe et al. (1999) found that perceived barriers, perceived benefits, and perceived severity of illness are significant predictors of intentions to vaccinate for influenza. Thus, the key constructs offered by the HBM provide a relevant basis for understanding vaccination intentions in a travel context.
2.3. Perceived susceptibility and perceived severity
Perceived susceptibility refers to an individual's beliefs about their vulnerability to infection (Champion & Skinner, 2008, pp. 45–65; Janz & Becker, 1984; Klohn & Rogers, 1991; Mermelstein & Riesenberg, 1992; D’Souza, Zyngier, Robinson, Shlotterlein & Sullivan-Mort, 2011), while perceived severity refers to one's beliefs about the degree of seriousness of the disease and potential health effects from contracting an infection (Rahmati-Najarkolaei, Tavafian, Fesharaki, & Jafari, 2015). The importance of perceived susceptibility and severity lies within the association of threat to one's health and its utility in motivating a positive health behavior, which was substantiated by Janz and Becker (1984), Klohn & Rogers (1991), Mermelstein and Riesenberg (1992), and D’Souza et al. (2011). As such, both perceived susceptibility and perceived severity have been found to be strongly related to the intention to receive a vaccine (Najimi & Golshiri, 2013). ). Relatedly, Manika & Golden (2011) identified that perceived threat strongly influences disease prevention behaviors. Also, Setbon and Raude (2010) cited that the degree of risk perceived influences actual vaccination behavior. However, despite these studies the use of perceived severity and susceptibility in explaining vaccination behavior is relatively scant (e.g., Manika & Golden, 2012; Scherr et al., 2016; Weldon et al., 2012). Moreover, little data exist on whether concepts of health, illness severity, susceptibility, benefits, and vaccine intentions are meaningful to a traveler who would be at risk for contracting an illness and spreading it to others while traveling. Furthermore, missing from the travel health behavioral theory literature is the consideration of whether or how to consider specific contexts such as travel and vaccination amid pandemics (Golets et al., 2020). In the current context of COVID-19 risk, there is a good case for suggesting that susceptibility to the infection and severity of symptoms would be significant predictors of vaccination intention and beliefs about the protection benefits associated with the impending vaccination, which constitutes the basis of willingness to vaccinate and belief that others should vaccinate prior to travel. Thus the following hypotheses are put forth:
H1
Perceived susceptibility to COVID-19 influences the perceived protection benefits of a COVID-19 vaccine for travel.
H2
Perceived severity of COVID-19 influences the perceived protection benefits of a COVID-19 vaccine for travel.
2.4. Protection benefits of the vaccine for travel
Past research has highlighted the role of protection from fear or threat in activating a person's subsequent behavior (Horng et al., 2014; Milne, Sheeran, & Orbell, 2000; Rogers, 1975; Suess, Woosnam, & Erul, 2020). Protection was initially conceptualized to explain behavior in a health-related attitude model by Rogers (1975). Wheldon, Daley, Buhi, Nyitray, and Giuliano (2011) who studied young gay and bisexual men and the HPV vaccine and found that perceived physical prophylaxis and psychological benefits of protection from cancer are strongly associated with the intention to take a vaccine. Gerend and Shepherd (2012) found a similar positive relationship between perceived protection benefits offered by the HPV vaccine and young adult women's intentions to take the vaccine. In this regard, the benefits of protection from a perceived threat may influence a person's receptiveness toward vaccine uptake, a relationship that has been found to hold in other vaccination contexts as well, such as parental acceptance of childhood vaccination coverage (Barnack et al., 2010; Smith et al., 2011). In their study of at-risk individuals resistant to the influenza vaccination, Cheney and John (2013) found that the perceived benefits of the vaccine, particularly the reduced threat to significant others, can be a pivotal determinant of these individuals' willingness to get vaccinated.
In a COVID-19 context, Wong et al. (2020) assessed the predictors of intention to receive the COVID-19 vaccine using the Health Belief Model framework (HBM) and found that in addition to perceived severity of and susceptibility to COVID-19, high perceived benefits of a vaccination are significantly related to intentions to vaccinate. Reiter, Pennell, and Katz (2020) found similar results, in that the constructs of perceived severity of and susceptibility to COVID-19 and the perceived benefits of vaccination were significant predictors of willingness to vaccinate. Moreover, they also found that individuals who were willing to get a COVID-19 vaccine were more likely to indicate recent or upcoming travel outside of the United States as a determinant of their willingness to vaccinate. While this provides preliminary evidence of travelers' willingness to comply with vaccination mandates for travel, an understanding of how individual health beliefs translate into support for vaccination in a travel context would allow administrators to design effective policy and communication pegs that bridge two of the three elements required for a successful return to safe travel—travelers’ personal risk stratification, as reflected in their health beliefs, and government regulations outside of the traveler's control (Wilson & Chen, 2020).
Thus, in light of this initial evidence, in the context of the present study, protection benefits—conceptualized as the individual's beliefs about the protection from COVID-19 a vaccination would offer both themselves and others in a travel situation—are considered a pivotal intermediary mechanism in the dynamics of individuals' decision-making toward COVID-19 vaccination for travel. Applied in an HBM framework, perceived protection benefits from a COVID-19 vaccine, as influenced by perceived severity of and susceptibility to COVID-19 illness, is hypothesized to influence individuals' willingness to vaccinate before traveling, beliefs others should vaccinate before traveling, and subsequent support for mandated vaccination requirements prior to travel. Accordingly, it is hypothesized
H3
Perceived protection benefits of vaccine influences willingness to vaccinate for COVID-19 prior to any travel
H4
Perceived protection benefits of vaccine influences the belief that others should vaccinate for COVID-19 prior to any travel
H5
Willingness to vaccinate for COVID-19 influences support for COVID-19 vaccination requirement prior to travel
H6
Belief that others should vaccinate for COVID-19 influences support for COVID-19 vaccination requirement prior to travel
2.5. Antecedents to perceived severity and perceived susceptibility: trust in third-party information
In the context of COVID-19, people must assess the associated risks of contracting the virus, its spread, and severity based on their level of knowledge, which is influenced by medical and science practitioners, exposure to media, and information provided by governments or other authorities. Particularly, prior knowledge about the risks of a specific disease was a significant factor in increasing vaccinations received among nurses in a study by Shahrabani, Benzion, and Din (2009). Payakachat, Hadden, and Ragland (2016) also investigated pregnant women and found that the provision of a Vaccine Information Statement (VIS) influences their Tdap vaccine intention. Gargano et al. (2013) discovered the strong influence of physician recommendation on parental immunization and on adolescents' attitudes and intentions to vaccinate. Coe et al. (2012) found that most participants in their study recognized the risk of the novel H1N1 virus, and physicians’ recommendations were significant predictors of intention to take a vaccine.
Information conveyed by physicians, government officials, the media, and other authorities has the propensity to influence how people perceive risk of illness and react to vaccinations (Baumgaertner et al., 2018). In the context of HBM, information from third parties serves as the “cues to action” that provide an awareness of disease threat—the perceived severity of and perceived susceptibility to a disease—that may prompt health-related behavior, including the decision to vaccinate (Adams, Hall, & Fulghum, 2014; Sarwar, Panatik, & Jameel, 2020). The government has conveyed information related to the risks of COVID-19, the severity of the disease, and forthcoming vaccination, with travel restrictions, commercial closures, curfews and other social and economic measures. Broadly, the scientific community has portrayed municipalities' inability to manage COVID-19 effectively and has strengthened the illness-phobic sentiment among the public, suggesting that the government continue to take strict regulatory actions in the interest of public safety, which has enhanced perceptions of risks of spreading the virus, support for regulation, closures of commercial industries, and isolation of vulnerable populations. The media has translated scientific rhetoric and government deliberation to generalized information, in addition to highlighting COVID-19 severity, broadcasting most extreme cases. The coverage in the media about COVID-19, overflowing hospitals, and high mortality rates has played a key role in influencing the public's ability to subjectively judge susceptibility to and severity of COVID-19. In addition, leading experts have cautioned for vigilance against the “rumors, misinformation, and conspiracy theories” perpetuated by anti-vaccination advocates, who use specific media channels to perpetuate their rhetoric, which has an impact on individuals' beliefs pertaining to the COVID-19 vaccine and their willingness to be vaccinated (IHME, 2020).
In sum, government, media, and the scientific community, both individually and collectively, shape the extent to which COVID-19 illness risks are perceived by the public, as evidenced in recent studies (Jose et al., 2021, pp. P41–P46; Tadesse, Alemu, Amogne, Endazenaw, & Mamo, 2020). Moreover, in light of evidence suggesting a progressive decline in trust in government and media sources pertaining to COVID-19 information (Ali et al., 2020; Edelman Trust Barometer, 2020), and even scientific institutions including the Centers for Disease Control and Prevention (CDC) (Wen, 2020), identifying how these various sources of information impact beliefs about the pandemic is critical to developing preemptive COVID-19 vaccination uptake promotion strategies and effective policies to contain the pandemic, either through voluntary or enforced mechanisms such as mandated vaccination for travel (French, Deshpande, Evans, & Obregon, 2020; Schmelz, 2021).
As such, it is hypothesized:
H7
Trust in the information about COVID-19 risk provided by the government influences perceived susceptibility to COVID-19
H8
Trust in the information about COVID-19 risk provided by the government influences the perceived severity of COVID-19
H9
Trust in the information about COVID-19 risk provided by scientists influences perceived susceptibility to COVID-19
H10
Trust in the information about COVID-19 risk provided by scientists influences the perceived severity of COVID-19
H11
Trust in the information about COVID-19 risk provided by the media influences perceived susceptibility to COVID-19
H12
Trust in the information about COVID-19 risk provided by the media influences the perceived severity of COVID-19
2.6. Moderating effect of travel frequency
A recognition of situational variables can substantially enhance the ability to explain and understand travel intentions (Walls, Okumus, Raymond et al., 2011; Mody, Suess, & Dogru, 2019; Suess, Kang, Dogru & Mody, 2020). In the context of HBM, Adams et al. (2014) indicated that modifying variables used in the model assist in explanations regarding an individual's choice of action; in the present case, the willingness to receive a COVID-19 vaccine and to support mandated vaccination for travel. Particularly, frequent leisure travel invokes demands and motivations unique to an individual and shapes subsequent travel patterns (Lehto et al., 2004); the psychological mechanisms through which past behavior helps predict future behavior are well-established in the travel literature (Ouellette & Wood, 1998; Sonmez and Graefe, 1998). Moreover, evidence suggests that individuals with a higher frequency of travel are more likely to demonstrate travel health-seeking behavior prior to travel, including seeking vaccinations (Lee & Smith, 2006). For example, Pedersini, Marano, De Moerlooze, Chen, and Vietri (2016) found that frequent European travelers had significantly higher vaccination rates for Hepatitis A and Hepatitis B than occasional traveler and nontravelers. In the context of the present study, we hypothesize that the effect of the frequency of prior travel may influence willingness to vaccinate. Knowledge about the role of frequency of travel as a situational factor would be instrumental for government and tourism organizations targeting vaccination uptake for critical market segments. Thus, it is hypothesized that:
H13
The model relationships will significantly differ for those with higher levels of previous leisure/vacation travel
2.7. Moderating effect of prior infection with COVID-19
Past studies have investigated a variety of individual-level factors associated with intentions to vaccinate for diseases, including pregnancy, adolescence, working in the health care industry, and classification in higher-risk demographic groups that could potentially moderate the relationships outlined in an HBM model (Adams et al., 2014; Gargano et al., 2013; Krawczyk et al., 2012; Mehta, Sharma, & Lee, 2014; Payakachat et al., 2016; Shahrabani et al., 2009; Wheldon et al., 2011; Zijtregtop et al., 2009). Of these individual factors, the impact of personal experience with infection represents an important determinant of vaccination coverage for COVID-19, particularly as stimulated by the need to travel. Wells and Bauch (2012) found that longer term memory associated with past infections contributed to increased vaccine coverage for seasonal influenza. Similarly, Mortensen (2010) found that personal experiences with HPV-related diseases was a significant driver for acceptance of HPV vaccination among young women in Denmark. In the context of the present pandemic of COVID-19, Reiter et al. (2020) found that U.S. adults with a personal history of COVID-19 infection were more willing to get a COVID-19 vaccine. Following this research, the present study proposes that differences in beliefs about susceptibility to and severity of COVID-19, the perceived benefits of a COVID-19 vaccine, and intentions to vaccinate as a requirement for travel may exist among groups: those who have tested positive for COVID-19 and those who have not. The following is hypothesized:
H14
The model relationships will significantly differ among groups of travelers who have tested positive for COVID-19
3. Methodology
3.1. Data collection
The sample for the study was acquired through a panel from Qualtrics. Respondents included in Qualtrics database (over 30 million members) were self-selected to be part of the present study, with an incidence rate of 19 %. To minimize self-selection bias, Qualtrics sends a survey link to its panel members so that respondents participate in the survey without knowing the nature of the survey beforehand, effectively facilitating a more random sampling procedure. Furthermore, Qualtrics engineers survey questions to enable better targeting and randomly assigns respondents to a survey that they will likely qualify for based on their responses. This helps further minimize self-selection bias and ensure that non-response is more of a random event versus a systematic event, compared to other sampling platforms (Suess & Mody, 2017). A total of 1478 useable responses from individuals in the United States were collected. Data collection was completed over a six-day period at the end of November 2020 prior to the public availability of vaccines, and respondents were stratified by age, gender, and region within the United States across forty-five states. The sample included respondents who indicated they had traveled at least one time for the purpose of leisure or vacation (including both internationally and nationally) between March 1, 2019, and November 15, 2020. This timeframe captured travel in the twelve months prior to the onset of the COVID-19 pandemic as well as during the pandemic. Consistent with the principles of effective survey design (Kasunic, 2005), questions measuring respondents' attitudes towards more general ideas (i.e., constructs of attitudes toward vaccine) were asked before the questions pertaining to travel requirements (i.e., requirement of a vaccine prior to travel) and advocacy for vaccine mandates prior to travel to avoid the latter from narrowing the scope of respondents’ thinking toward the more general constructs.
3.2. Survey design
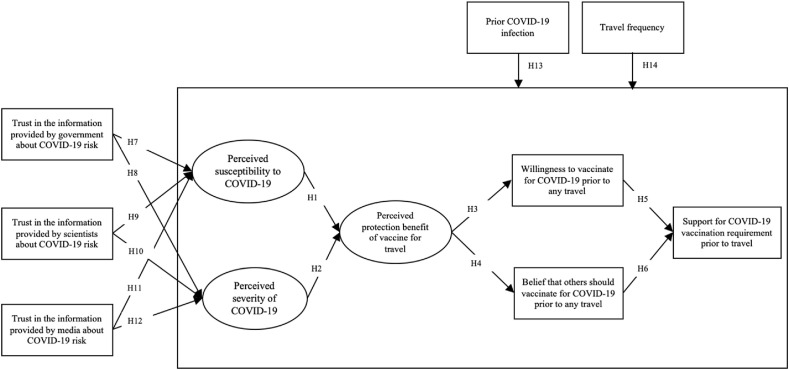
All constructs included in the model (Fig. 1 ) were comprised of indicators measured as questions in a survey. Indicators were measured by 5-point Likert scales developed from the existing Health Belief Model literature for the present study's COVID-19 context based on expert triangulation across tourism, psychology, and public health disciplines. The three antecedent constructs' indicators for trust in the information provided by the government, media, and scientists about the risks of COVID-19 were adapted from Mody, Woosnam, Suess, and Dogru (2020) trust in political-decision making (adapted from Boley et al. (2014)). The potential for protection benefits scale is similar, in principle, to the personal (vaccine) benefits scale from Wong et al. (2020); two items were adapted, and two items developed based on face-validity to capture perceived protection benefits from a COVID-19 vaccination related to travel. Six items measuring perceived susceptibility and perceived severity were adapted to the context of travel and COVID-19 from the Arthritis Health Belief Scale (Barr, 1991) and the AIDS Health Belief Scale (Zagumny & Brady, 1998). A single item measuring willingness to get the COVID-19 vaccine was adapted from Dodd, Cvejic, Bonner, Pickles, and McCaffery (2020). In addition, a question related to whether or not others should get a COVID-19 vaccination prior to any travel was asked. The single-item variable was adapted from a study by Mody et al. (2020) related to support for regulation of peer-to-peer accommodations based on face-validity.
Fig. 1.
Proposed model and hypotheses.
3.3. Data analysis
Using the statistical software STATA 15.1, descriptive statistics and distributions were analyzed for the study's overall sample. Next, a CFA was conducted to validate the constructs specified in the HBM framework. This was followed by structural equation modeling (SEM) to test hypotheses in the proposed model (Fig. 1). Multiple group SEM was then conducted and subsequently compared using the goodness of fit indices, path significance, and effect size testing. In the final stage of analysis, the authors used pairwise parameter comparisons to determine whether any of the structural parameters were significantly different between the models tested in the SEM stage. Multiple measures suggested by Hair et al. (2010) were used to assess the fit between both the measurement and structural components of the models and the data, comparative fit index (CFI), Tucker Lewis index (TLI), root mean square error of approximation (RMSEA), and standardized root means square residual (SRMR).
4. Results
Table 1 indicates that about a third of the respondents were younger than 35 (35.9 %) and classified as Millennials (between 18 and 35 years of age). Also, respondents were highly educated; over 60 % of the group had a college or graduate degree. Almost half of the respondents were married with children (45.3 %). Approximately 56.0 % of the sample indicated that they had taken a vacation more than once during the time period March 1, 2019, and November 15, 2020. In sum, the sample of travelers were slightly younger, better educated, and more likely to be married with children. In addition to demographics.
Table 1.
Respondent profile.
|
Demographic Category |
Sample Size (n = 1478) |
% |
|---|---|---|
| Age | ||
| 18-25 | 299 | 20.2 % |
| 26-34 | 224 | 15.16 % |
| 35-44 | 460 | 31.12 % |
| 45-54 | 140 | 9.47 % |
| 55-64 | 140 | 9.47 % |
| 65-74 | 259 | 17.52 % |
| Older than 74 | 39 | 2.64 % |
| Gender | ||
| Male | 759 | 51.84 % |
| Female | 705 | 48.16 % |
| Income | ||
| Less than $15,000 | 135 | 9.16 % |
| $15,000 - less than $30,000 | 196 | 13.31 % |
| $30,000 - less than $45,000 | 180 | 12.22 % |
| $45,000 - less than $60,000 | 155 | 10.52 % |
| $60,000 - less than $75,000 | 140 | 9.50 % |
| $75,000 - less than $90,000 | 139 | 9.44 % |
| $90,000 - less than $105,000 | 92 | 6.25 % |
| $105,000 - less than $120,000 | 84 | 5.70 % |
| $120,000 - less than $135,000 | 46 | 3.12 % |
| $135,000 - less than $150,000 | 102 | 6.92 % |
| More than $150,000 | 204 | 13.85 % |
| Education | ||
| Grade school | 14 | 0.95 % |
| High school | 240 | 16.29 % |
| Some college | 294 | 19.96 % |
| College | 456 | 30.96 % |
| Graduate school | 469 | 31.84 % |
| Hispanic | ||
| Yes | 304 | 20.64 % |
| No | 1169 | 79.36 % |
| Ethnicity | ||
| White/Caucasian | 1070 | 72.64 % |
| Black/African American | 243 | 16.50 % |
| Asian | 97 | 6.59 % |
| Native Hawaiian | 18 | 1.22 % |
| American Indian/Alaskan | 23 | 1.56 % |
| Other | 74 | 5.02 % |
| Household | ||
| Single, never married | 384 | 26.07 % |
| Married without child | 179 | 12.15 % |
| Married with children | 667 | 45.28 % |
| Divorced | 84 | 5.70 % |
| Separated | 25 | 1.70 % |
| Widowed | 26 | 1.77 % |
| Living w/partner | 108 | 7.33 % |
| Travel Frequency- Domestic (Leisure/Vacation) | ||
| One time | 521 | 35.25 % |
| 2–3 times | 588 | 39.78 % |
| 4–6 times | 236 | 15.97 % |
| More than six times | 133 | 9.00 % |
| Travel Frequency- International (Leisure/Vacation) | ||
| One time | 384 | 25.98 % |
| 2–3 times | 357 | 24.15 % |
| 4–6 times | 142 | 9.61 % |
| More than six times | 81 | 5.48 % |
Table 2 includes the critical situational factor of a prior positive test for COVID-19.
Table 2.
Health situational factor.
| Tested Positive for COVID-19 | ||
|---|---|---|
| Yes | 216 | 14.6 % |
| No | 1164 | 78.8 % |
| Not Sure | 98 | 6.6 % |
Table 3 presents the summary statistics, including all items used to measure the model's various constructs for both groups. Cronbach's α ranged from 0.70 to 0.89, at or above the recommended 0.70 level according to Anderson and Gerbing (1988) and an indication of sufficient internal consistency. Since the measures were adapted from validated measures in the literature (see sources in Table 3), a confirmatory factor analysis was conducted without an exploratory phase.
Table 3.
Summary of statistics and literature sources.
| Constructs and Measurement Items | Mean | SD | Cronbach's α |
Adapted from |
|---|---|---|---|---|
| Trust in governmenta | ||||
| I trust the information from the government about the risks of COVID-19 since the start of the pandemic | 3.31 | 1.33 | – | Mody et al. (2020) |
| Trust in sciencea | ||||
| I trust the information from the scientists about the risks of COVID-19 since the start of the pandemic | 3.76 | 1.17 | – | Mody et al. (2020) |
| Trust in mediaa | ||||
| I trust the information from the media about the risks of COVID-19 since the start of the pandemic | 3.24 | 1.34 | – | Mody et al. (2020) |
| Perceived susceptibility to COVID-19a | .79 | (Zagumny & Brady, 1998; Barr, 1991) | ||
| I worry a lot about getting COVID-19 from travel | 3.65 | 1.31 | ||
| The chances that I will get COVID-19 if I travel are great | 3.46 | 1.26 | ||
| My physical health makes it more likely that I will contract COVID-19 if I travel | 3.19 | 1.40 | ||
| Perceived severity of COVID-19a | .70 | (Zagumny & Brady, 1998; Barr, 1991) | ||
| If I were to contract COVID-19, my symptoms would be severe | 3.31 | 1.75 | ||
| It worries me to think about the effect of COVID-19 on my health | 3.78 | 1.61 | ||
| COVID-19 is deadly | 3.96 | 1.64 | ||
| Perceived protection benefit of vaccine for travela | .86 | Wong et al. (2020) | ||
| A COVID-19 vaccine would help protect me when I travel | 3.64 | 1.27 | ||
| A COVID-19 vaccination will help stop the spread of the virus through travel | 3.82 | 1.23 | ||
| It is my responsibility to protect others from getting COVID-19 if I travel | 3.92 | 1.20 | ||
| It is everyone's responsibility to protect others from COVID-19 when they travel | 4.07 | 1.15 | ||
| Willingness to vaccinate for COVID-19 prior to travelb | .91 | Dodd et al. (2020) | ||
| If a vaccination for COVID-19 becomes available, how willing would you be to receive it in order to travel within the U.S.? | 3.55 | 1.33 | ||
| If a vaccination for COVID-19 becomes available, how willing would you be to receive it in order to travel internationally? | 3.52 | 1.39 | ||
| The belief that others should vaccinate for COVID-19 prior to travela | ||||
| I feel everyone should receive a vaccination for COVID-19 prior to travel | 3.41 | 1.35 | ||
| Support for COVID-19 vaccination requirement prior to travela | Mody et al. (2019) | |||
| I would support restrictions on travel for people without a COVID-19 vaccine | 3.71 | 1.49 |
Measured using a 5-point Likert scale (1 = Strongly disagree to 5 = Strongly agree).
Measured using a 5-point Likert Scale (1 = Not at all willing 5 = Very willing).
4.1. CFA results
As the first step in the CFA, common method bias was tested using a latent variable approach outlined in Podsakoff, Mackenzie, Lee, and Podsakoff (2003). A common factor was added to a second CFA with all of the measures as indicators. Next, standardized regression weights for all loadings across the two models were compared. Significant differences were not found that would suggest the presence of common method bias.
The sample indicated that the CFA model fit the data (CFI = 0.926, TLI = 0.900, SRMR = 0.048, RMSEA = 0.097). Although the χ2 was significant, this tends to be the case with large sample sizes and complex models and the RSMEA and TLI are both largely based on the χ2/df square ratio, and thus determined to be sufficient indications of model fit (Keith, 2020). Items loading onto constructs were significant (p < .001) standardized factor loadings ranging from 0.617 to 0.927, indicating convergent validity. The AVE was higher than 0.50 for all but one construct (0.488) demonstrating partial support for convergent validity (Hair, 2010; Nunnally & Bernstein, 1994). The square roots of the AVE for all constructs were greater than inter-construct correlations, demonstrating discriminant validity (Table 4 ).
Table 4.
Comparison of square root of AVE and inter-construct correlations—.
| Perceived Susceptibility to COVID-19 | Perceived Severity of COVID-19 | Perceived protection benefits of vaccine prior to travel | Willingness to vaccinate for COVID-19 prior to any travel | |
|---|---|---|---|---|
| Perceived Susceptibility to COVID-19 | .699 | |||
| Perceived Severity of COVID-19 | .684 | .754 | ||
| Perceived protection benefits of vaccine prior to travel | .579 | .570 | .781 | |
| Willingness to vaccinate for COVID-19 prior to any travel | .440 | .481 | .523 | .876 |
Note: Square root of AVE is on the diagonal (in bold). Inter-construct correlations are on the off-diagonal.
The data was found to be multivariate non-normal. Mardia's normalized estimate of multivariate skewness was found to be 21.82 and kurtosis was found to be 422.23 indicating significant (p < .001) positive skewness and significant (p < .001) kurtosis. A further examination of the univariate skewness indices for all variables specified in the model indicated that the data were moderately non-normal. Although maximum likelihood estimation technique is fairly robust, a Satorra-Bentler procedure with maximum likelihood estimation was used to the address moderate non-normality (Burke, 2016).
4.2. SEM results (Fig. 1)
The structural model indicated an acceptable fit to the data despite the significant χ2 result (p < .001): CFI = 0.911; TLI = 0.900; SRMR = 0.061; RMSEA = 0.094. Satorra–Bentler scaled chi-squared test was used for the SEM because it is robust to nonnormality (Byrne, 2016). Table 5 presents the parameter estimates for the hypothesized model. Overall, the results indicate that the constructs derived from the Health Belief Model framework have significant direct impacts on intentions and beliefs about vaccinating prior to travel and support for requiring a vaccination prior to travel, as hypothesized. These results collectively emphasize the importance of the protection benefit of the vaccine in effecting a willingness to vaccinate and a belief that others should vaccinate prior to travel, in addition, to support for vaccine mandates prior to travel. Furthermore, the model indicates that travelers have a greater sense of trust in the information provided by scientists about COVID-19 risk, related to their self-assessment of susceptibility to COVID-19 and the perceived severity of the virus.
Table 5.
Main model (Fig. 1): SEM results.
| Structural Path | Unstandardized estimates | Critical Ratio | p-value |
|---|---|---|---|
| Perceived susceptibility to COVID-19 → Perceived protection benefit of vaccine for travel (H1) | .402 | 14.82 | *** |
| Perceived severity of COVID-19 → Perceived protection benefit of vaccine for travel (H2) | .788 | 12.91 | *** |
| Perceived protection benefits of the vaccine for travel → Willingness to vaccinate for COVID-19 prior to any travel (H3) | .906 | 24.70 | *** |
| Perceived protection benefits of the vaccine for travel → Belief that others should vaccinate for COVID-19 prior to any travel (H4) | 1.11 | 42.14 | *** |
| Willingness to vaccinate for COVID-19 prior to any travel → Support for COVID-19 vaccination requirement prior to travel (H5) | .252 | 6.17 | *** |
| The belief that others should vaccinate for COVID-19 prior to any travel → Support for COVID-19 vaccination requirement prior to travel (H6) | .464 | 12.70 | *** |
| Trust in the information provided by the government about COVID-19 risk → Perceived susceptibility to COVID-19 (H7) | .040 | 2.44 | ** |
| Trust in the information provided by the government about COVID-19 risk → Perceived severity of COVID-19 (H8) | .088 | 9.20 | *** |
| Trust in the information provided by scientists about COVID-19 risk → Perceived susceptibility to COVID-19 (H9) | .254 | 12.04 | *** |
| Trust in the information provided by scientists about COVID-19 risk→ Perceived severity of COVID-19 (H10) | .064 | 2.41 | ** |
| Trust in the information provided by media about COVID-19 risk → Perceived susceptibility to COVID-19 (H11) | .244 | 9.20 | *** |
| Trust in the information provided by media about COVID-19 risk → Perceived severity (H12) |
.292 | 9.76 | *** |
*** indicates significance at p < .001; * indicates significance at p < .05. The amount of variance explained (squared multiple correlations) in the final dependent construct—support for COVID-19 vaccination requirement prior to travel — was determined using Cohen's f2, a measure of effect size. The overall model was (R2 = 0.684).
4.3. Moderation testing: model (Fig. 1)
The effects of two situational moderators in the formation of beliefs about the vaccine and intentions were tested: one moderator of prior leisure travel frequency and one moderator indicating prior infection with COVID-19. A two-step analysis was employed: an initial test for measurement invariance, followed by confirmatory factor analysis (CFA). The results of the CFA indicated acceptable fit of the measurement model to the data: CFI = 0.923; TLI = 0.912; RMSEA = 0.091; SRMR = 0.070 and established configural invariance. There were no substantial differences among fit indices (ΔCFI = 0.007, ΔTLI = 0, ΔRMSEA = 0, and ΔSRMR = 0.009) between the configural and metric-invariant models, establishing metric invariance and allowing for the next stage of a multiple group modeling to test differences among structural coefficients. Satorra–Bentler scaled chi-squared test was used to estimate the multiple group SEM because it is robust to nonnormality (Byrne, 2016). Group level goodness of fit statistics indicated the coefficient of determination ranged from .957 to .982 and RMSEA ranged from 0.096 to 0.109, respectively. While there were mostly similarities among groups (results are presented in Table 6 ) and model relationships were significant (p < .001), thus confirming H1 - H6 for the groups of more and less frequent leisure travelers and those with and without prior positive COVID-19 tests. Pairwise comparisons of parameters indicated a few significantly different relationships among variables. Specifically, the estimates associated with willingness to vaccinate and support for vaccine requirements prior to travel were significantly higher for the more frequent leisure travelers than for the less frequent travelers, partially supporting H13 (difference in parameter estimates = 0.191).
Table 6.
Moderation testing.
| Structural Path | Group 1a estimate | Group 2 estimate | t |
|---|---|---|---|
| Travelers: Less frequent (n = 466) vs. More frequent (n = 872) | |||
| Perceived susceptibility to COVID-19 → Perceived protection benefit of vaccine for travel (H1) | .395*** | .450*** | 1.10 |
| Perceived severity of COVID-19 → Perceived protection benefit of vaccine for travel (H2) | .735** | .679** | .475 |
| Perceived protection benefit of vaccine for travel → Willingness to vaccinate for COVID-19 prior to any travel (H3) | .903*** | .898*** | .054 |
| Perceived protection benefit of vaccine for travel → Belief that others should vaccinate for COVID-19 prior to any travel (H4) | 1.13*** | 1.10*** | .034 |
| Willingness to vaccinate for COVID-19 prior to any travel → Support for COVID-19 vaccination requirement prior to travel (H5) | .189** | .335*** | 2.50* |
| Belief that others should vaccinate for COVID-19 prior to any travel → Support for COVID-19 vaccination requirement prior to travel (H6) | .393*** | .453*** | .050 |
| Press COVID-19 infection: Have tested positive (n = 216) vs. Have not tested positive (n = 1164) | |||
| Perceived susceptibility to COVID-19 → Perceived protection benefit of vaccine for travel (H1) | .632*** | .410*** | 4.09*** |
| Perceived severity of COVID-19 → Perceived protection benefit of vaccine for travel (H2) | .536 | .698*** | 1.99* |
| Perceived protection benefit of vaccine for travel → Willingness to vaccinate for COVID-19 prior to any travel (H3) | .841*** | .913*** | .767 |
| Perceived protection benefit of vaccine for travel → Belief that others should vaccinate for COVID-19 prior to any travel (H4) | 1.20*** | 1.10*** | .854 |
| Willingness to vaccinate for COVID-19 prior to any travel → Support for COVID-19 vaccination requirement prior to travel (H5) | .431** | .235*** | 1.52 |
| The belief that others should vaccinate for COVID-19 prior to any travel → Support for COVID-19 vaccination requirement prior to travel (H6) | .355*** | .475*** | 1.34 |
***significant at p < .001; **significant at p < .01; *significant at p < .05.
Group 1 refers to the first group presented in the table for each moderating variable (less frequent travelers and have tested positive for COVID-19).
In addition, the relationship between the perceived susceptibility to COVID-19 and protection benefit of a vaccine for travel was significantly higher for those who had a prior positive test for COVID-19 (difference in parameter estimates = 0.22), but significantly lower for the influence of perceived severity of COVID-19 on the perceived protection benefit of a vaccine for travel (difference in parameter estimates = 0.162); results that partially upheld H14. In sum, the results demonstrate the significant potential of leisure travel frequency on a stronger willingness to vaccinate prior to travel. Furthermore, the perceived protection benefit of the COVID-19 vaccine for travel is enhanced by perceived severity of COVID-19 among travelers who have not had a prior positive test and by perceived susceptibility among those who have tested positive for COVID-19. The results of the moderation testing support the need to investigate how willingness to vaccinate is formed on the foundation of specific travel policies. The results of the multiple group model and comparisons are presented in Table 6.
Equation level testing was conducted to determine the models’ explanatory power. The amount of variance explained (squared multiple correlations) by support for COVID-19 vaccination requirement prior to travel, as predicted by the constructs included in the Health Belief Model ranged from 0.41 to 0.70 as indicated in Table 7 .
Table 7.
Equation level statistics.
| Travel frequency |
Prior COVID-19 infection |
|||||||
|---|---|---|---|---|---|---|---|---|
| Less frequent |
More frequent |
Have tested positive |
Have not tested positive |
|||||
| Variance predicted | R2 | Variance predicted | R2 | Variance predicted | R2 | Variance predicted | R2 | |
| Perceived protection benefits of vaccine prior to travel | .355 | .413 | .416 | .466 | .561 | .842 | .375 | .400 |
| Willingness to vaccinate for COVID-19 prior to any travel | .690 | .533 | .712 | .640 | .470 | .582 | .765 | .596 |
| Belief others should vaccinate for COVID-19 prior to any travel | 1.11 | .720 | 1.08 | .725 | .968 | .677 | 1.12 | .743 |
| Support for COVID-19 vaccination requirement prior to travel |
.413 |
.254 |
.698 |
.432 |
.536 |
.354 |
.619 |
.372 |
| Overall R2 | .961 | .957 | .982 | .958 | ||||
The difference (0.18) in the R2 for more frequent travelers compared to the group of less frequent travelers indicated that frequency of leisure travel adds explanatory power to the dependent variable of general support for vaccination requirements prior to any travel. In addition, not having a prior infection of COVID-19 added some explanatory power to the support for vaccination requirements prior to any travel variable when the models were compared across the groups.
5. Discussion
5.1. Practical implications
The COVID-19 pandemic “once again illuminates the pivotal role that travelers play in emerging infectious diseases and their spread” (Wilson & Chen, 2020, p. 4). There is an urgent need to determine effective ways to stop the spread of COVID-19 and facilitate future travel. The case for suggesting that factors influencing vaccination intention are twofold: 1) a strong belief in the protection benefits of the vaccine, and 2) a higher level of perceived susceptibility to COVID-19, with an anticipation of more severe symptoms. Regarding travel, the results of our study provide convincing evidence that willingness to vaccinate and beliefs that others should vaccinate predict support for federal and international authorities imposing vaccination mandates, both domestic and international alike. Implementation of such requirements will be a key factor in the global endeavor by authorities to ensure vaccine coverage, with travel administrators at the forefront of vaccine campaigns. A similar study of 28 countries found that 78 % of adults supported vaccine passports for international travel (Ipsos, 2021). Tourism industry businesses should become strong advocates for travel vaccination programs for their potential consumers. As highlighted in current media discourse, major airlines (e.g., Qantas and American Airlines) leading by example can impact overall results. Further, it is reasonable to hypothesize that given the risk of infection due to the asymptomatic transmission of COVID-19, governments and travel authorities around the globe, and even locals in destinations, will be more antagonistic towards visitors in their communities and demonstrate support for strict regulations and requirements for proof of vaccination prior to issuing visas or allowing entry to travelers. Information about willingness to vaccinate should inform such policy development and shape regulation logistics. Lack of requirements for vaccines may change global travel to focus more on rural areas or virtual attractions (Itani & Hollebeek, 2021; Zhu & Deng, 2020).
The support for mandate must begin with the population's willingness to be vaccinated in order to travel and enforcing vaccine requirements requires strategies at the governmental level. Governments should work together to implement regulations, such as “vaccine passports,” registration through embassies and consulates, vaccination records in national and international travel databases, vaccination kiosks at airports, and upon arrival. The benefits of travel industry restrictions are wide-ranging and include increased immunity to COVID-19 and controlling of spread to vulnerable populations. Focusing the communication of marketing messages on perceived benefits includes elaboration and discussion of resumption of travel and prevention of spreading COVID-19 to others and a sense of social responsibility toward the protection of others. Given that people in the United States are still largely reluctant to plan future trips due to concern of exposure to other people (Read, 2021), for travel to become part of the solution to overcome lingering anti-vaccine sentiment and facilitate improved vaccination coverage, understanding population support for travel vaccination mandates that alleviate such concerns is critical. The results of the present study suggest that such vaccination mandates may prove to be an effective mechanism in the policy toolkit to tackle the spread of COVID-19 (French, 2020; Schmelz, 2020). While governments may be responsible for developing such policy, communication about policy may be better facilitated by the media and scientific community, given that higher levels of trust in these institutions provide higher awareness of disease threat, which subsequently triggers the mechanisms that lead to higher willingness to vaccinate oneself and also support for vaccination mandates for travel. In the United States, the Biden administration's renewed emphasis on science-based approaches to fighting COVID-19 are only likely to enhance trust in scientific institutions that are key to garnering public support for vaccination mandates for travel and in other policy contexts (Keith, 2021). However, CDC guidance issued May 13, 2021 removed the recommendation for wearing masks and social distancing for people who were fully vaccinated but specifically exempted travel from this recommendation (CDC, 2021).
5.2. Theoretical implications
The present study is the first in the hospitality and tourism literature to apply the Health Belief Model. While the literature on travel medicine has extensively examined factors affecting pre-travel health-seeking behavior (Kain et al., 2019), the scale of the COVID-19 pandemic and its impact on global travel necessitates an understanding of the extent to which policy measures such as travel vaccination mandates can be effective in enabling the resumption of domestic and international travel. Our model provides a theoretically informed understanding of the dynamics that may enable the success of important health-related travel policy, and it can be applied to examine future health-impacted travel behavior. Moreover, using the constructs and tenets of HBM allows us to examine the underlying psychosocial triggers that governments and travel authorities can subsequently leverage to potentially enhance support for travel vaccination mandates. The validity and theoretical salience of the model are indicated by Wilson and Chen (2020), who identify that restarting travel safely involves “some elements under personal control and those that the individual cannot control” (p. 4). The use of HBM to examine support for travel vaccination mandates bridges these two elements, thus providing a timely theoretical contribution to the domain of hospitality and tourism policy. Previous research in the hospitality and tourism literature on the impact of pandemics has largely focused on issues of travel intentions (Lee et al., 2012; Sánchez-Cañizares et al., 2020) and travel avoidance (Cahyanto, Wiblishauser, Pennington-Gray, & Schroeder, 2016); however, our study is the first to identify the role that travel policy can play as part of a broader multipronged solution to controlling a pandemic, which is particularly important given the role of travel in enabling its spread in the first place.
5.3. Future research
Our study opens up several avenues for future research on COVID-19 policy in hospitality and tourism. Evidence about social responsibility and consideration for the well-being of others through the COVID-19 vaccine is essential to evaluate the feasibility of the implementation of vaccination programs and to provide insights into the potential increase in the number of travelers in travel demand forecasts (Melendez, 2020); vaccination-related behavioral intentions will be useful in estimating traveler numbers and economic recovery. Moreover, in the context of those precluded from travel due to an unwillingness to vaccinate, research should include barriers to vaccination (Paul et al., 2020) as part of the HBM framework, in determining the efficacy of travel vaccination mandates. In this regard, Adondo et al.’. s (2021) recently developed measure of travel vaccination concerns would be a particularly relevant addition to the HBM framework. Future research should also link personality and situational predictors of travel, such as risk-taking, COVID-induced travel anxiety (Luo & Lam, 2020), motivation to protect others, political orientation (Reiter et al., 2020), and demographic factors (e.g., family composition) to travel-related vaccination behavior. Studying particularly vulnerable groups such as senior tourists and previously vaccine-marginalized groups such as Black travelers (Okorodudu & Okorodudu, 2021), and specific travel contexts such as cruise tourism (Spurrell, 2020), can offer deeper insights into health-related travel policy that enables global travel recovery in this and future pandemics. Finally, while travelers represent an important stakeholder group informing health policy, local destination resident sentiment toward and support for vaccination mandates for travelers should provide important consideration for health-related travel policy formulation (Girma, 2021).
5.4. Limitations
The constructs included in the present study's HBM framework (Fig. 1) were developed for the generic U.S. population, and its concepts of susceptibility, severity, and benefits around vaccination are meaningful in the context of travel and vaccination-related intentions within the specific timeframe of the COVID-19 pandemic. The model, therefore, may be limited in its generalizability to other pandemics or infectious disease crises. In this vein, as COVID-19 has progressed and more is known about the virus and the vulnerabilities of the population infected, the perceived susceptibility and severity of COVID-19 has changed. In addition, exposure to information put forth by the government, scientific community, and media, over time, would alter the general public's perceptions dynamically. Thus, changes in intervention strategies would need to be consistent with the stages of COVID-19 and account for the fact that beliefs about the risks of COVID-19, the risks and or benefits of a vaccine, attitudes about travel, and associated restrictions would not be static and would instead evolve over different stages of the pandemic. Particularly, a stronger willingness to vaccinate may be associated with the length of time of a pandemic and the longevity of travel restrictions. Individuals deprived of travel and anxious to take a vacation may be more motivated to vaccinate. Conversely, as pandemics become long-lived, the concept of herd-immunity may be associated with less willingness to vaccinate among many individuals. While the model (Fig. 1) captures perceptions related to the time frame of the initial release of the COVID-19 vaccine available for public adoption, a study after the vaccination is available and demonstrating efficacy may drive proclivity to vaccinate—subsequently changing the promotion tactics among a variety of stakeholders, including the local health care industry and governments. A longitudinal study would capture the modulations of beliefs about vaccination, intentions to vaccinate, and support for a proof of vaccine requirement prior to travel as subsequent versions of the vaccine are released and vaccination becomes more widespread among the population. Finally, while understanding intentions to vaccinate and support for travel vaccination mandates is important, longitudinal examination can also capture actual vaccination uptake among respondents, thus providing a stronger basis for causal inference, including examining the effects of interventions that stimulate pro-health behaviors in a travel and hospitality context.
Author statement
Dr. Courtney Suess and Dr. Jay Maddock developed the theoretical framework and designed the study and its methodology, and implemented the empirical analysis. Dr. Courtney Suess wrote the manuscript with support from Dr. Makarakand Mody and Seunghoon Lee. Dr. Tarik Dogru discussed and contributed to the theoretical framework, empirical strategy, results, and commented on the manuscript.
Declaration of competing interest
None.
Acknowledgements
Thank you to Texas A & M University's Presidential Excellence Fund (T3) for providing funding for this study and Dr. Mary Steinhardt at University of Texas at Austin for reviewing the manuscript.
Biographies

Dr. Courtney Suess, Ph.D., is an Assistant Professor in the department of Recreation, Parks and Tourism Sciences and a Fellow in the School of Architecture at Texas A & M University. She holds a Bachelor's degree from the School of the Art Institute of Chicago, and a Master's degree and Doctor of Philosophy from the University of Nevada, Las Vegas, in Hospitality Administration. She is completing a second Master's degree, studying Architecture at the University of Texas at Austin. Her research focuses on the planning and development of tourism, hospitality facilities design, and environmental psychology.

Dr. Jay Maddock is co-director of the Center for Health and Wellness a joint initiative of Texas A&M University, Houston Methodist Research Institute and Texan by Nature. He also serves as Interim Director of the Institute for Advancing Health through Agriculture and as Professor in the Department of Environmental and Occupational Health at Texas A&M. He previously served as Chair of the Hawaii Board of Health and Dean of the Texas A&M School of Public Health. His research has been featured in several national and international media outlets including The Today Show, the BBC, Le Monde, Eating Well, Prevention and Good Housekeeping and he has authored over 130 scientific articles and has served as principal investigator on over $18 million in extramural funding.

Dr. Tarik Dogru is an assistant professor of hospitality management in the Dedman School of Hospitality at Florida State University. He earned a bachelor's and master's degree in business administration from Zonguldak Karaelmas University and earned a doctorate degree in hospitality management from University of South Carolina. Prior to joining Florida State University, Dr. Dogru worked at Boston University as an assistant professor for two years. His research interests include sharing economy, corporate finance, franchising, hotel investments, tourism economics, climate change, and blockchain technology.

Dr. Makarand Mody, an Assistant Professor of Hospitality Marketing at Boston University's School of Hospitality Administration, graduated with his Ph.D. from Purdue University. He received his M.Sc in Human Resource Management for Tourism and Hospitality from the University of Strathclyde, and a Higher Diploma in Hospitality Management from IMI University Centre, Switzerland. Dr. Mody has worked in the hotel and airlines industries in the areas of learning and development and quality control. His research focuses on issues pertaining to the supply and demand of responsible tourism, the sharing economy, and the modeling of consumer behavioral pathways.

Seunghoon Lee is a completing a Ph.D. in in the department of Recreation, Park and Tourism Sciences at Texas A & M University. He holds a master's degree in Urban Geography from Seoul National University. Research interests are heritage tourism, sustainable tourism, tourism marketing, ethical tourism marketing, community development, and justice. Prior to graduate studies, he worked at the Korean local government research institute for promoting and planning tourism.
References
- Adams A., Hall M., Fulghum J. Utilizing the Health Belief Model to assess vaccine acceptance of patients on hemodialysis. Nephrology Nursing Journal. 2014;41(4) [PubMed] [Google Scholar]
- Adongo C.A., Amenumey E.K., Kumi-Kyereme A., Dubé E. Beyond fragmentary: A proposed measure for travel vaccination concerns. Tourism Management. 2021;83:104180. doi: 10.1016/j.tourman.2020.104180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ali S.H., Foreman J., Tozan Y., Capasso A., Jones A.M., DiClemente R.J. Trends and predictors of COVID-19 information sources and their relationship with knowledge and beliefs related to the pandemic: Nationwide cross-sectional study. JMIR public health and surveillance. 2020;6(4):e21071. doi: 10.2196/21071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Press A. International travelers may soon be required to get COVID-19 vaccination before flying. USA Today. 2020 https://www.usatoday.com/story/travel/airline-news/2020/11/23/vaccination-passport-qantas-looking-new-requirement-travelers/6402846002/ November 24. [Google Scholar]
- Baeyens J.P. Ensuring the willingness to vaccinate and be vaccinated. Expert Review of Vaccines. 2010;9(sup3):11–14. doi: 10.1586/erv.10.28. [DOI] [PubMed] [Google Scholar]
- Böhm R., Meier N.W., Groß M., Korn L., Betsch C. The willingness to vaccinate increases when vaccination protects others who have low responsibility for not being vaccinated. Journal of Behavioral Medicine. 2019;42(3):381–391. doi: 10.1007/s10865-018-9985-9. [DOI] [PubMed] [Google Scholar]
- Baumgaertner B., Carlisle J.E., Justwan F. The influence of political ideology and trust on willingness to vaccinate. PloS One. 2018;13(1) doi: 10.1371/journal.pone.0191728. e0191728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnack J.L., Reddy D.M., Swain C. Predictors of parents' willingness to vaccinate for human papillomavirus and physicians' intentions to recommend the vaccine. Women's Health Issues. 2010;20(1):28–34. doi: 10.1016/j.whi.2009.08.007. [DOI] [PubMed] [Google Scholar]
- Burke M. Two U.S. cruise lines announce covid vaccination mandate for guests, crew. NBC News. 2021. https://www.nbcnews.com/news/us-news/two-u-s-cruise-lines-announce-covid-vaccination-mandate-guests-n1256937 February 6.
- Carico R.R., Sheppard J., Thomas C.B. Community pharmacists and communication in the time of COVID-19: Applying the Health Belief Model. Research in Social and Administrative Pharmacy. 2020 doi: 10.1016/j.sapharm.2020.03.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter C.J. A meta-analysis of the effectiveness of Health Belief Model variables in predicting behavior. Health Communication. 2010;25(8):661–669. doi: 10.1080/10410236.2010.521906. [DOI] [PubMed] [Google Scholar]
- Cahyanto I., Wiblishauser M., Pennington-Gray L., Schroeder A. The dynamics of travel avoidance: The case of Ebola in the US. Tourism Management Perspectives. 2016;20:195–203. doi: 10.1016/j.tmp.2016.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2021) 2021. Interim public health recommendations for fully vaccinated people.https://www.cdc.gov/coronavirus/2019-ncov/vaccines/fully-vaccinated-guidance.html on May 18. [Google Scholar]
- Chabria A. Anti-vaccine and alt-right groups team up to stoke fears of COVID-19 vaccine. 2020. Retrieved from https://www.latimes.com/california/story/2020-12-18/anti-vaxxers-team-up-alt-right-against-covid-19-vaccine.
- Champion V.L., Skinner C.S. In: Health behavior and health education: Theory, research, and practice. Glanz K., Rimer B., Viswanath K., editors. Jossey-Bass; 2008. The Health Belief Model. 4th ed. [Google Scholar]
- Cheney M.K., John R. Underutilization of influenza vaccine: A test of the Health Belief Model. Sage Open. 2013;3(2) 2158244013484732. [Google Scholar]
- Coe A.B., Gatewood S.B., Moczygemba L.R. The use of the Health Belief Model to assess predictors of intent to receive the novel (2009) H1N1 influenza vaccine. Innovations in Pharmacy. 2012;3(2):1–11. doi: 10.24926/iip.v3i2.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings K.M., Jette A.M., Brock B.M., Haefner D.P. Psychosocial determinants of immunization behavior in a swine influenza campaign. Medical Care. 1979:639–649. doi: 10.1097/00005650-197906000-00008. [DOI] [PubMed] [Google Scholar]
- Dodd R.H., Cvejic E., Bonner C., Pickles K., McCaffery K.J. Willingness to vaccinate against COVID-19 in Australia. The lancet. Infectious Diseases. 2020 doi: 10.1016/S1473-3099(20)30559-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- D'Souza C., Zyngier S., Robinson P., Schlotterlein M., Sullivan-Mort G. Health belief model: Evaluating marketing promotion in a public vaccination program. J. Nonprofit & Public Sect. Mark. 2011;23(2):134–157. [Google Scholar]
- Erkin Ö., Özsoy S. Validity and reliability of health belief model applied to influenza. Academic Research International. 2012;2(3):31. [Google Scholar]
- French J., Deshpande S., Evans W., Obregon R. Key guidelines in developing a pre- emptive COVID-19 vaccination uptake promotion strategy. International Journal of Environmental Research and Public Health. 2020;17(16):5893. doi: 10.3390/ijerph17165893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gargano L.M., Herbert N.L., Painter2 J.E., Sales J.M., Morfaw3 C., Rask2 K., Hughes J.M. Impact of a physician recommendation and parental immunization attitudes on receipt or intention to receive adolescent vaccines. Human Vaccines & Immunotherapeutics. 2013;9(12):2627–2633. doi: 10.4161/hv.25823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerend M.A., Shepherd J.E. Predicting human papillomavirus vaccine uptake in young adult women: Comparing the health belief model and theory of planned behavior. Annals of Behavioral Medicine. 2012;44(2):171–180. doi: 10.1007/s12160-012-9366-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillam S. Understanding the uptake of cervical cancer screening: The contribution of the health belief model. British Journal of General Practice. 1991;41:510–551. [PMC free article] [PubMed] [Google Scholar]
- Golets A., Farias J., Pilati R., Costa H. COVID-19 pandemic and tourism: The impact of health risk perception and intolerance of uncertainty on travel intentions. Preprints. 2020:2020100432. doi: 10.1007/s12144-021-02282-6. (doi: 10.20944/preprints202010.0432.v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldman R.D., Yan T.D., Seiler M., Cotanda C.P., Brown J.C., Klein E.J., Griffiths M.A. Caregiver willingness to vaccinate their children against COVID-19: Cross sectional survey. Vaccine. 2020;38(48):7668–7673. doi: 10.1016/j.vaccine.2020.09.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall C.M., Scott D., Gössling S. Pandemics, transformations and tourism: Be careful what you wish for (commentary) Tourism Geographies. 2020;22(3):577–598. doi: 10.1080/14616688.2020.1759131. [DOI] [Google Scholar]
- Harrison J.A., Mullen P.D., Green L.W. 1989. A meta-analysis of studies of the health belief model (Master's thesis, University of Texas Health Science Center at Houston, School of Public Health) [Google Scholar]
- Hoeffe J. Willingness to vaccinate children against influenza after the Coronavirus disease 2019 pandemic. The Journal of Pediatrics. 2020 doi: 10.1016/j.jpeds.2020.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horng J.S., Hu M.L.M., Teng C.C.C., Lin L. Energy saving and carbon reduction behaviors in tourism–a perception study of Asian visitors from a protection motivation theory perspective. Asia Pacific Journal of Tourism Research. 2014;19(6):721–735. [Google Scholar]
- Itani O.S., Hollebeek L.D. Light at the end of the tunnel: Visitors' virtual reality (versus in-person) attraction site tour-related behavioral intentions during and post-COVID-19. Tourism Management. 2021;84:104290. doi: 10.1016/j.tourman.2021.104290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ipsos . 2021. Global public backs COVID-19 vaccine passports for international travel.https://www.ipsos.com/en/global-public-backs-covid-19-vaccine-passports-international-travel on May 17, 2021. [Google Scholar]
- Janz N.K., Becker M.H. The health belief model: A decade later. Health Education Quarterly. 1984;11(1):1–47. doi: 10.1177/109019818401100101. [DOI] [PubMed] [Google Scholar]
- Jones C.J., Smith H., Llewellyn C. Evaluating the effectiveness of health belief model interventions in improving adherence: a systematic review. Health Psychology Review. 2014;8(3):253–269. doi: 10.1080/17437199.2013.802623. [DOI] [PubMed] [Google Scholar]
- Jose R., Narendran M., Bindu A., Beevi N., Manju L., Benny P.V. Public perception and preparedness for the pandemic COVID 19: A Health Belief Model approach. Clinical Epidemiology and Global Health. 2021;9:P41–P46. doi: 10.1016/j.cegh.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kain D., Findlater A., Lightfoot D., Maxim T., Kraemer M.U., Brady O.J., Bogoch I.I. Factors affecting pre-travel health seeking behaviour and adherence to pre-travel health advice: a systematic review. Journal of Travel Medicine. 2019;26(6) doi: 10.1093/jtm/taz059. [DOI] [PubMed] [Google Scholar]
- Keith T. Will Biden's Science-Based COVID-19 Approach Be Enough To Regain Public Trust? 2020. Retrieved from https://www.npr.org/2021/01/27/961278989/will-bidens-science-based-covid-19-approach-be-enough-to-regain-public-trust.
- Krawczyk A., Lau E., Perez S., Delisle V., Amsel R., Rosberger Z. How to inform: comparing written and video education interventions to increase human papillomavirus knowledge and vaccination intentions in young adults. Journal of American College Health. 2012;60(4):316–322. doi: 10.1080/07448481.2011.615355. [DOI] [PubMed] [Google Scholar]
- Kreps S., Prasad S., Brownstein J.S., Hswen Y., Garibaldi B.T., Zhang B., et al. Factors Associated With US Adults' Likelihood of Accepting COVID-19 Vaccination. JAMA network open. 2020;3(10) doi: 10.1001/jamanetworkopen.2020.25594. e2025594–e2025594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klohn L.S., Rogers R.W. Dimensions of the severity of a health threat: The persuasive effects of visibility, time of onset, and rate of onset on young women's intentions to prevent osteoporosis. Health Psychol. 1991;10(5):323. doi: 10.1037//0278-6133.10.5.323. [DOI] [PubMed] [Google Scholar]
- Lu H., Stratton C.W., Tang Y.-W. Outbreak of pneumonia of unknown etiology in Wuhan China: the mystery and the miracle. Journal of Medical Virology. 2020;92(4):401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luo J.M., Lam C.F. Travel Anxiety, Risk Attitude and Travel Intentions towards “Travel Bubble” Destinations in Hong Kong: Effect of the Fear of COVID-19. International Journal of Environmental Research and Public Health. 2020;17(21):7859. doi: 10.3390/ijerph17217859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manika D., Golden L.L. Self-efficacy, threat, knowledge and information receptivity: Exploring pandemic prevention behaviors to enhance societal welfare. Academy of Health Care Management Journal. 2011;7(1):31. [Google Scholar]
- Marlow L.A., Waller J., Evans R.E., Wardle J. Predictors of interest in HPV vaccination: A study of British adolescents. Vaccine. 2009;27(18):2483–2488. doi: 10.1016/j.vaccine.2009.02.057. [DOI] [PubMed] [Google Scholar]
- Mermelstein R.J., Riesenberg L.A. Changing knowledge and attitudes about skin cancer risk factors in adolescents. Health Psychol. 1991;11(6):371. doi: 10.1037//0278-6133.11.6.371. [DOI] [PubMed] [Google Scholar]
- Mehta P., Sharma M., Lee R.C. Designing and evaluating a health belief model-based intervention to increase intent of HPV vaccination among college males. The International Quarterly of Community Health Education. 2014;34(1):101–117. doi: 10.2190/IQ.34.1.h. [DOI] [PubMed] [Google Scholar]
- Milne S., Sheeran P., Orbell S. Prediction and intervention in health-related behavior: A meta-analytic review of protection motivation theory. Journal of Applied Social Psychology. 2000;30(1):106–143. [Google Scholar]
- Mody M., Woosnam K.M., Suess C., Dogru T. Hapless victims or empowered citizens? Understanding residents' attitudes towards Airbnb using Weber's Theory of Rationality and Foucauldian concepts. Journal of Sustainable Tourism. 2020:1–23. [Google Scholar]
- Mody M., Suess C., Dogru T. Not in my backyard? Is the anti-Airbnb discourse truly warranted? Annals of Tourism Research. 2019;74(C):198–203. [Google Scholar]
- Mortensen G.L. Drivers and barriers to acceptance of human-papillomavirus vaccination among young women: a qualitative and quantitative study. BMC Public Health. 2010;10(1):1–14. doi: 10.1186/1471-2458-10-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mukhtar S. 2020. Mental health and emotional impact of COVID-19: applying health belief model for medical staff to general public of Pakistan. Brain, Behavior, and Immunity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers L.B., Goodwin R. Using a theoretical framework to determine adults' intention to vaccinate against pandemic swine flu in priority groups in the U.K. Public Health. 2012;126:S53–S56. doi: 10.1016/j.puhe.2012.05.024. [DOI] [PubMed] [Google Scholar]
- Najimi A., Golshiri P. 2013. Knowledge, beliefs and preventive behaviors regarding Influenza A in students: a test of the health belief model. Journal of education and health promotion, 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neumann-Böhme S., Varghese N.E., Sabat I., Barros P.P., Brouwer W., van Exel J., Stargardt T. 2020. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nexøe J., Kragstrup J., Søgaard J. Decision on influenza vaccination among the elderly: a questionnaire study based on the Health Belief Model and the Multidimensional Locus of Control Theory. Scandinavian Journal of Primary Health Care. 1999;17(2):105–110. doi: 10.1080/028134399750002737. [DOI] [PubMed] [Google Scholar]
- Palamenghi L., Barello S., Boccia S., Graffigna G. Mistrust in biomedical research and vaccine hesitancy: the forefront challenge in the battle against COVID-19 in Italy. European Journal of Epidemiology. 2020;35(8):785–788. doi: 10.1007/s10654-020-00675-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palache A. Seasonal influenza vaccine provision in 157 countries (2004–2009) and the potential influence of national public health policies. Vaccine. 2011;29(51):9459–9466. doi: 10.1016/j.vaccine.2011.10.030. [DOI] [PubMed] [Google Scholar]
- Payakachat N., Hadden K.B., Ragland D. Promoting Tdap immunization in pregnancy: Associations between maternal perceptions and vaccination rates. Vaccine. 2016;34(1):179–186. doi: 10.1016/j.vaccine.2015.09.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersini R., Marano C., De Moerlooze L., Chen L., Vietri J. HAV & HBV vaccination among travellers participating in the National Health and Wellness Survey in five European countries. Travel Medicine and Infectious Disease. 2016;14(3):221–232. doi: 10.1016/j.tmaid.2016.03.008. [DOI] [PubMed] [Google Scholar]
- Pitrelli M.B. No vaccine, no service: How vaccinations may affect travel plans in the future. CNBC. 2021. https://www.cnbc.com/2021/01/14/will-vaccines-be-required-to-fly-or-travel-its-likely-say-experts.html January 14.
- Rahmati-Najarkolaei F., Tavafian S.S., Fesharaki M.G., Jafari M.R. Factors predicting nutrition and physical activity behaviors due to cardiovascular disease in Tehran university students: application of health belief model. Iran Red Crescent Med J. 2015. 2015;17(3):e18879. doi: 10.5812/ircmj.18879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Read J. What vaccines mean for the return of travel. 2020. https://www.nationalgeographic.com/travel/article/what-will-covid-19-vaccines-mean-for-travel-coronavirus Retrieved from.
- Reiter P.L., Pennell M.L., Katz M.L. Acceptability of a COVID-19 vaccine among adults in the United States: How many people would get vaccinated? Vaccine. 2020;38(42):6500–6507. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers R.W. A protection motivation theory of fear appeals and attitude change1. Journal of Psychology. 1975;91(1):93–114. doi: 10.1080/00223980.1975.9915803. [DOI] [PubMed] [Google Scholar]
- Rosenstock I.M. Historical origins of the health belief model. Health Education Monographs. 1974;2(4):328–335. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- Rosenstock I.M. The health belief model and preventive health behavior. Health Education Monographs. 1974;2(4):354–386. doi: 10.1177/109019817800600406. [DOI] [PubMed] [Google Scholar]
- Ryan C., Patel T. Covid Passports Seen as Key to Resuming International Travel. Bloomberg. 2020 https://www.bloomberg.com/news/articles/2020-11-23/airline-lobby-is-building-a-covid-travel-pass-to-spur-flights November 24. [Google Scholar]
- Sánchez-Cañizares S.M., Cabeza-Ramírez L.J., Muñoz-Fernández G., Fuentes-García F.J. Impact of the perceived risk from Covid-19 on intention to travel. Current Issues in Tourism. 2020:1–15. [Google Scholar]
- Sarwar F., Panatik S.A., Jameel H.T. Understanding Public’s Adoption of Preventive Behavior during COVID-19 pandemic using Health Belief Model: Role of Appraisals and. Psychological Capital Advance Preprint. 2020 doi: 10.31124/advance.12661178.v1. [DOI] [Google Scholar]
- Scherr C.L., Jensen J.D., Christy K. Dispositional pandemic worry and the health belief model: promoting vaccination during pandemic events. J. Public Health. 2016;39(4):e242–e250. doi: 10.1093/pubmed/fdw101. [DOI] [PubMed] [Google Scholar]
- Schmelz K. 2021. Enforcement may crowd out voluntary support for COVID-19 policies, especially where trust in government is weak and in a liberal society. Proceedings of the National Academy of Sciences, 118(1) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schunk M., Wachinger W., Nothdurft H.D. Vaccination status and prophylactic measures of travelers from Germany to subtropical and tropical areas: results of an airport survey. Journal of Travel Medicine. 2001;8(5):260. doi: 10.2310/7060.2001.24031. [DOI] [PubMed] [Google Scholar]
- Setbon M., Raude J. Factors in vaccination intention against the pandemic influenza A/H1N1. The European Journal of Public Health. 2010;20(5):490–494. doi: 10.1093/eurpub/ckq054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shahrabani S., Benzion U., Din G.Y. Factors affecting nurses' decision to get the flu vaccine. The European Journal of Health Economics. 2009;10(2):227–231. doi: 10.1007/s10198-008-0124-3. [DOI] [PubMed] [Google Scholar]
- Sonmez S.F., Graefe A.R. Determining future travel behavior from past travel experience and perceptions of risk and safety. Journal of Travel Research. 1998;37(2):171–177. [Google Scholar]
- Smith P.J., Humiston S.G., Marcuse E.K., Zhao Z., Dorell C.G., Howes C., et al. Parental delay or refusal of vaccine doses, childhood vaccination coverage at 24 months of age, and the Health Belief Model. Public Health Reports. 2011;126(2_suppl):135–146. doi: 10.1177/00333549111260S215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spinks R. Will American Outbound Travel Ever be the Same? 2020. https://skift.com/2020/06/16/will-american-outbound-travel-ever-be-the-same/ October 3). Retrieved from.
- Suess C., Woosnam K.M., Erul E. Stranger-danger? Understanding the moderating effects of children in the household on non-hosting residents' emotional solidarity with Airbnb visitors, feeling safe, and support for Airbnb. Tourism Management. 2020;77:103952. [Google Scholar]
- Suess C., Kang S., Dogru T., Mody M. Understanding the influence of “feeling at home” on healthcare travelers’ well-being: a comparison of Airbnb and hotel homescapes. J. Trav. Tourism Market. 2020;37(4):479–494. [Google Scholar]
- Suess C., Mody M. Hospitality healthscapes: A conjoint analysis approach to understanding patient responses to hotel-like hospital rooms. International Journal of Hospitality Management. 2017;61:59–72. [Google Scholar]
- Tadesse T., Alemu T., Amogne G., Endazenaw G., Mamo E. Predictors of Coronavirus Disease 2019 (COVID-19) Prevention Practices Using Health Belief Model Among Employees in Addis Ababa, Ethiopia, 2020. Infection and Drug Resistance. 2020;13:3751. doi: 10.2147/IDR.S275933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tarkang E.E., Zotor F.B. Application of the health belief model (HBM) in HIV prevention: A literature review. Central African Journal of Public Health. 2015;1(1):1–8. [Google Scholar]
- The World Travel & Tourism Council (WTTC) represents the Travel & Tourism sector globally. 2020. https://wttc.org/ October 3). Retrieved from.
- U.S. Travel Association: Industry Guidance for Promoting the Health and Safety of All Travelers. (2020, October 7). Retrieved from https://www.ustravel.org/toolkit/industry-guidance-promoting-health-and-safety-all-travelers.
- Wheldon C.W., Daley E.M., Buhi E.R., Nyitray A.G., Giuliano A.R. Health beliefs and attitudes associated with HPV vaccine intention among young gay and bisexual men in the southeastern United States. Vaccine. 2011;29(45):8060–8065. doi: 10.1016/j.vaccine.2011.08.045. [DOI] [PubMed] [Google Scholar]
- Wells C.R., Bauch C.T. The impact of personal experiences with infection and vaccination on behaviour–incidence dynamics of seasonal influenza. Epidemics. 2012;4(3):139–151. doi: 10.1016/j.epidem.2012.06.002. [DOI] [PubMed] [Google Scholar]
- Weldon W.C., Zarnitsyn V.G., Esser E.S., Taherbhai M.T., Koutsonanos D.G., Vassilieva E.V., Compans R.W. Effect of adjuvants on responses to skin immunization by microneedles coated with influenza subunit vaccine. PLoS One. 2012;7(7):e41501. doi: 10.1371/journal.pone.0041501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen L. Opinion: The U.S. is facing a crisis of confidence in our government scientists. 2020. Retrieved from https://www.washingtonpost.com/opinions/2020/09/02/us-is-facing-crisis-confidence-our-government-scientists/
- Wilson M.E., Chen L.H. Re-starting travel in the era of COVID-19: preparing anew. Journal of travel medicine. 2020;27(5) doi: 10.1093/jtm/taaa108. taaa108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong L.P., Alias H., Wong P.-F., Lee H.Y., AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Human Vaccines & Immunotherapeutics. 2020;16(9):2204–2214. doi: 10.1080/21645515.2020.1790279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank Database International Tourism, number of Arrivals. 2020. October 7). Retrieved from https://data.worldbank.org/indicator/ST.INT.ARVL.
- Wu J. 2020. COVID-19 Experts.http://www.healthdata.org/news-release/covid-19-experts-americans-must-be-vigilant-against-anti-vax-rumors-%E2%80%98fractured-media Americans Must be Vigilant Against Anti-Vax Rumors in ‘Fractured Media Universe’ Retrieved from. [Google Scholar]
- Zhu H., Deng F. How to influence rural tourism intention by risk knowledge during COVID-19 Containment in China: mediating role of risk perception and attitude. International Journal of Environmental Research and Public Health. 2020;17(10):3514. doi: 10.3390/ijerph17103514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zijtregtop E.A.M., Wilschut J., Koelma N., Van Delden J.J.M., Stolk R.P., Van Steenbergen J., Hak E. Which factors are important in adults' uptake of a (pre) pandemic influenza vaccine? Vaccine. 2009;28(1):207–227. doi: 10.1016/j.vaccine.2009.09.099. [DOI] [PubMed] [Google Scholar]