Abstract
Backgroud
We performed a systematic review on the management of patellar fracture nonunion and report a novel suture-based non-metallic fixation technique associated with platelet-rich plasma and mesenchymal stem cell injections in the management of this injury.
Methods
A systematic search was performed up to August 2020 in PubMed and Scopus electronic databases of scholarly articles evaluating different surgical techniques used for nonunion of patellar fractures, with no restrictions on language or year of publication. Furthermore, we describe our novel non-metallic suture fixation technique and a patient in whom this technique was applied.
Results
A total of 9 articles were included in the systematic review. Tension band wiring was the most commonly used procedure (62.7%). Nonoperative procedures (8.1%) resulted in nonunion in all patients. The most common complication after open reduction and internal fixation was infection (7.8%). Our patient at the latest follow-up reported full functional recovery and full extension and flexion of the affected knee with no pain and subjectively normal strength.
Conclusions
The management of patella nonunions is still a challenge. The technique reported here can be used in patellar fracture nonunion, as well as in primary patellar fractures.
Keywords: Patella, Fracture, Non-union, Delayed union, Pseudarthrosis, Pseudoarthrosis
Patellar fractures represent 1% of all fractures.1) For the treatment of patellar fractures displaced with articular incongruity, open reduction and internal fixation (ORIF) is generally performed,2) with a high rate of success.3) Nonunion rates range between 2.7% and 12.5%.3) In these patients, different surgical options can be considered, including tension band wiring, cerclage wiring, Bunnell wiring, partial or total patellectomy, and V-Y quadricepsplasty.4,5) Tension band wiring affords the best functional outcome, while V-Y quadricepsplasty carries the worst outcomes with high complication rates and poor functional results.4,6) There is still a lack of evidence to guide surgeons in the management of nonunion of patellar fractures. We performed a systematic review of the available published peer-reviewed evidence on the management of this injury and report a novel suture-based non-metallic fixation technique associated with platelet-rich plasma (PRP)7,8) and mesenchymal stem cell (MSC) injections9) performed for the management of nonunion of a patellar fracture.
METHODS
Literature Search Strategy
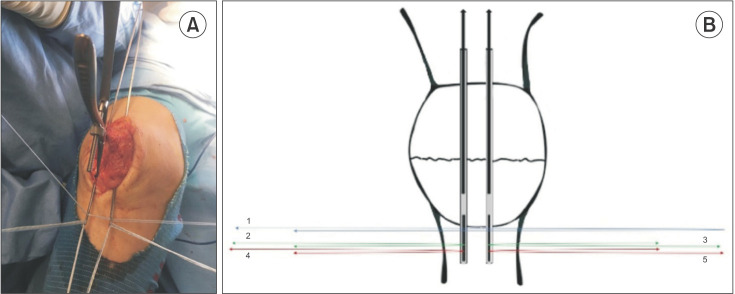
The article selection procedure was designed and carried out following the “Preferred Reporting Items for Systematic Reviews and Meta-Analyses” (PRISMA) guidelines (Fig. 1).10) A systematic search was performed up to August 2020 in PubMed and Scopus electronic databases of scholarly articles evaluating the different surgical techniques used for nonunion of patellar fractures, with no language or year of publication restrictions. Only full-text articles evaluating skeletally mature adults were considered. We used various combinations of the following key terms: patella, fracture, nonunion, delayed union, pseudarthrosis, and pseudoarthrosis. Editorials, letters to the editors and their replies, commentaries, expert opinions, narrative and systematic review articles, pediatric studies, and cadaver and animal studies were excluded, even though the reference section of review articles was scanned by hand to increase the chance to include all relevant articles. One orthopedic surgeon (EC) carried out the literature search and assessed the articles with support of an orthopedic resident (LC). A researcher (NM) with expertise in the field of systematic reviews solved cases of doubt. At the beginning of the procedure, one examiner (LC) read the titles and abstracts of all the articles according to inclusion and exclusion criteria previously determined, selected the relevant ones, and then compared the results with another examiner (NM). The same studies were read again in 4 weeks to establish the agreement of the researchers on the selection. The investigators showed no disagreement. The reviewers extracted relevant data (surname of the first author, publication year, study design, sample size, age and sex of the recruited sample, treatment procedure, main findings, and adverse events) from the full-text articles to an ad hoc Excel spreadsheet structured tables to analyze each study in a descriptive fashion. Doubts and inconsistencies were discussed until they were solved.
Fig. 1. Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
RESULTS
An initial search identified 2,387 articles with the key word “patella fracture,” 74 articles for the key word “patella nonunion," 26 articles for “patella delayed union,” and 37 articles for “patella pseudarthrosis.” The search using the other keywords did not yield any articles. With the exclusion of duplicated articles, 22 records were selected. We first excluded 8 articles after examining the titles and abstracts and then 5 articles because they did not meet the inclusion criteria. A total of 9 articles were therefore included in the present systematic review and selected for synthesis and discussion. Details concerning the number of the references and the data and methods collected from the included records are indicated in Table 1. Delayed union and nonunion were more frequent in men than women: of 86 reported patients, 60 (69.7%) were men and 26 (30.3%) were women.
Table 1. Summary of the Studies Included.
| Study | Level of evidence | Patient characteristics | Treatment | Mean follow-up | Result |
|---|---|---|---|---|---|
| Klassen and Trousdale (1997)3) | IV | Total: 20, male: 12, female: 8 | Nonoperative: 7, operative: 13 | 34 mo (range, 4–109) |
Operative: average Knee Society score of 94, function score of 93 |
| Average age: 38 yr | Nonoperative: observation, activity modification, physical therapy, local pain relief | ROM: 0°–109° | |||
| Affected side: 11 right, 9 left | Operative: tension band wiring, Bunnell wiring, cerclage wiring, screw fixation, partial patellectomy, total patellectomy | Nonoperative: average knee score of 83, function score of 75 | |||
| Fracture classification (AO): 4, 34–A1; 12, 34–C1; 4, 34–C3 | ROM: 0°–120° | ||||
| Satku and Kumar (1991)5) | IV | Total: 3, male: 1, female: 2 | Operative: 3 | 24 mo | Two patients able to fully flex (140°), 1 patient able to flex to 120°, all patients were pain-free and satisfied |
| Average age: 45 yr | Tension band wiring, cerclage wiring, | ||||
| Fracture classification (AO): 3, 34–C1 | 2 patients required bone grafting | ||||
| Uvaraj et al. (2007)11) | IV | Total: 22, male: 18, female: 4 | Operative: 22 | 5.5 yr (range, 2–9) |
ROM: 0°–110° |
| Average age: 43 yr | Tension band wiring (16), tension band wiring with cerclage wiring (3), patellectomy (3) | Bostman knee score: excellent, 5; good, 15; poor, 2 | |||
| Affected side: 11 right, 11 left | |||||
| Fracture classification (AO): 2, 34–A1; 18, 34–C1; 2, 34–C3 | |||||
| Torchia and Lewallen (1996)13) | IV | Total: 2 (male) | Operative: 2 | 9.4 yr | Both patients developed stiffness |
| Average age: 56 yr | Non-rigid internal fixation | ||||
| Affected side: 2 left | |||||
| Fracture classification (AO): 2, 34–C1 | |||||
| Al Obaedi et al. (2019)14) | IV | Total: 1 (female) | Operative: 2 stage | 1 yr | Full independent mobility and full extension of the knee |
| Age: 73 yr | First stage: tension wire transkeletal traction using a ring fixator device | ||||
| Affected side: left | Second stage: tension band wiring | ||||
| Fracture classification (AO): 34–C1 | |||||
| de Faria et al. (2019)15) | IV | Total: 1 (male) | Operative: 2 stage | 18 mo | Active and passive range of motion from 0° to a flexion of 90°, full quadriceps strength, VAS score of 1 |
| Age: 17 yr | First stage: tension wire transkeletal traction | ||||
| Affected side: left | Second stage: tension band wiring with cerclage wiring | ||||
| Fracture classification (AO): 34–C1 | |||||
| Garg et al. (2012)6) | IV | Total: 35, male: 25, female: 10 | Operative: 35 | 1 yr | Group 2 showed the better results. ROM (flexion): group 2, 130°; group 3, 110°; group 1, 80° |
| Average age: 41 yr | Group 1: tension band wiring with V-Y plasty (10); Group 2: patellar traction followed by tension band wiring (15); Group 3: patellar traction followed by partial or total patellectomy (10) | Group 1 expressed the higher rate of complications and persistent nonunion (20%). | |||
| Affected side: 15 right, 20 left | |||||
| Fracture classification (AO): 19, 34–A1; 16, 34–C1 | |||||
| Lachiewicz (2008)16) | IV | Total: 1 (female) | Operative: fixation with two cannulated, cancellous screw, cancellous allograft mixed with demineralized bone | 1 yr | ROM (flexion): 80° |
| Age: 67 yr | No pain | ||||
| Affected side: left | |||||
| Fracture classification (AO): 34–C1 | |||||
| Bhimani et al. (2018)12) | IV | Total: 1 (male) | Operative: V-Y quadricepsplasty with double tension band wiring | 3 mo | ROM: 5°–110° |
| Age: 40 yr | |||||
| Affected side: left | |||||
| Fracture classification (AO): 34–A1 |
ROM: range of motion, VAS: visual analog scale.
Nonunions and delayed unions can be treated nonoperatively or operatively. Physical therapy, pain relief, and activity modification represent the basic principles of nonoperative management. ORIF and partial or total patellectomy are listed as possible surgical options. ORIF includes several surgical procedures. Bunnel wiring, screw fixation, tension band wiring, and cerclage wiring are the common ORIF modalities. Tension band wiring was the most commonly used procedure (54 patients, 62.7%).3,5,11) In 11 patients (12.7%), a quadricepsplasty was necessary to reduce the fracture.6,12) In 3 patients, ORIF was supplemented by bone grafting.5) Nonoperative procedures (7 patients, 8.1%) resulted in nonunion in all patients.3) For outcome evaluation, the Knee Society knee and function score and the Bostman Knee score scoring system were used in 2 studies (Table 1).3,11) The other studies relied on clinical examinations and patient satisfaction. The most common complication after ORIF was infection (3 patients, 7.8%): it was related to persistent nonunion in 1 patient,3) and it led to severe stiffness in 2 patients.13)
Case Report
A 41-year-old otherwise fit and healthy female was referred to us with right knee pain and limited range of motion after a fall from stairs. Physical examination confirmed a 30° extensor lag and flexion to 85°, with marked wasting of the quadriceps. Plain radiographs revealed a right patella fracture with a 7-cm gap (Fig. 2A). After appropriate counselling, the patient opted for surgical management, and we used the modified Pyriford technique.17) With the patient in supine position and a tourniquet at the root of the thigh inflated to 250 mmHg after exsanguination, an anterior midline approach to the patella was performed. Under fluoroscopy, reduction was obtained with a reduction clamp. A peripatellar circumferential cerclage with a No. 5 FiberWire nonabsorbable suture (Arthrex Inc., Naples, FL, USA) was undertaken in a purse-string configuration as close as possible to the bone margins of the patella to allow initial fracture stabilization. To obtain an anterior tension band effect, a second No. 5 FiberWire nonabsorbable suture was then passed in a figure-of-eight configuration through the quadriceps and patellar tendons. Each of the 2 FiberWire constructs was then manually tensioned and knotted on the superior margin of the patella (Fig. 2B). The patient was immobilized with a long-hinged knee brace blocked at 0° for 3 weeks. Then, passive range of motion from 0° to 90° was started for the following 2 weeks, allowing active flexion and extension. The patient was allowed to weight bear as tolerated using crutches, progressing to complete weight bearing 1 month postoperatively. At that time, radiographs revealed a nonhealing tendency of the fracture. After 4 weeks, the radiographs revealed displacement of the fracture and an evident interfragmentary gap (Fig. 2C) probably because the patient did not follow the weightbearing restriction and the prescribed rehabilitation protocol was not correctly executed. Two days later, the patient underwent a further surgical procedure.
Fig. 2. (A) Lateral radiograph of the initial right patella fracture. (B) Immediate postoperative lateral radiograph. (C) Lateral radiograph 9 weeks after surgery.
Surgical Technique
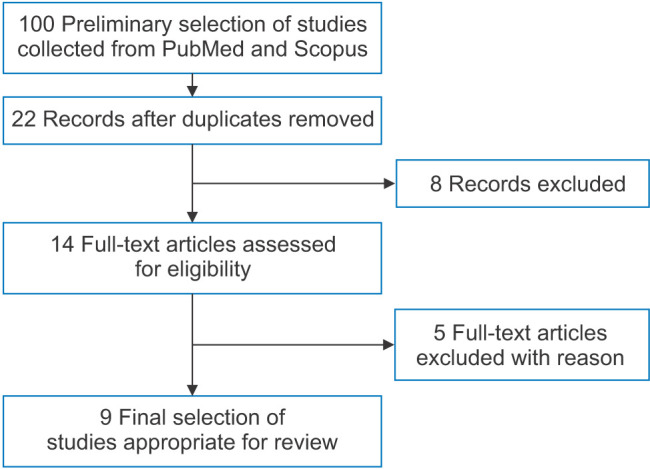
The patient was placed in supine, the ilium was penetrated 2 cm below the iliac crest with an 11-G trocar, and 60 mL of blood was withdrawn to extract MSCs. Stem cells were obtained with the Sepax Cell Processing System. The procedure produced 14 mL of autologous MSCs. The PRP was obtained with the PRP Bio Reb Kit. From 9 mL of patient's peripheral blood, 5 mL of PRP was extracted. Then, a tourniquet was placed as proximally as possible over the thigh and inflated to 250 mmHg after exsanguination. The previous scar was used to expose the whole patella and the patellar tendon. The FiberWire cerclage was found to be torn at the site of fracture. Interfragmentary fibrous tissue was then removed, and the bone surfaces were freshened. To improve bone healing, several small holes at the margin of the fracture were produced with a 1.0-mm drill. Reduction was achieved with the aid of a clamp. Two longitudinal bone tunnels were made from the inferior pole of the patella through the superior margin of the patella with two 2.4-mm slotted guide wires (Fig. 3). A No. 2 FiberWire was doubled and passed through both the slotted sections of the guide wires. Another 4 No. 2 FiberWire sutures were doubled and passed through just 1 of the slotted sections of the guide, 2 doubled wires for each guide wire (Fig. 4). The guide wires were pulled upwards with all the doubled FiberWire sutures. The resulting wire configuration is shown in Fig. 5. Before the final reduction, PRP and MSCs were applied to the fracture gap (Fig. 6). All the wires were tensioned, and reduction was obtained (Fig. 7). The 5 wires were knotted using the Nice knot suture.18) The immediate postoperative appearance is shown in Fig. 8.
Fig. 3. Slotted guide wire positioning.

Fig. 4. (A) Wire disposition before tensioning. (B) Wire disposition in the slotted guide wires.
Fig. 5. (A) Intraoperative final wire configuration. (B) Schematic representation of the wire configuration.

Fig. 6. (A) Platelet-rich plasma injection. (B) Mesenchymal stem cell injection.
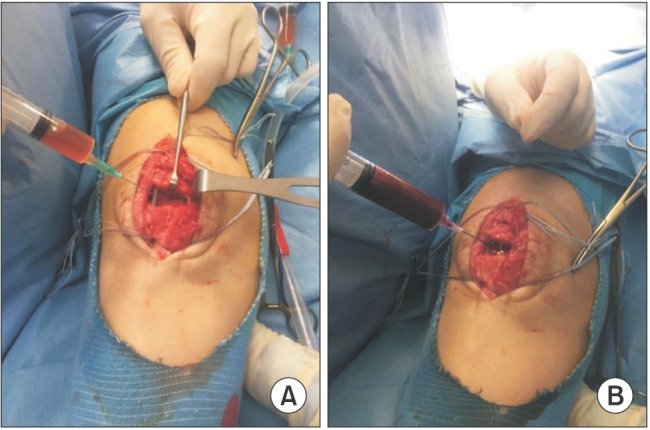
Fig. 7. (A) Wire tensioning and final reduction. (B) Further mesenchymal stem cell injection.
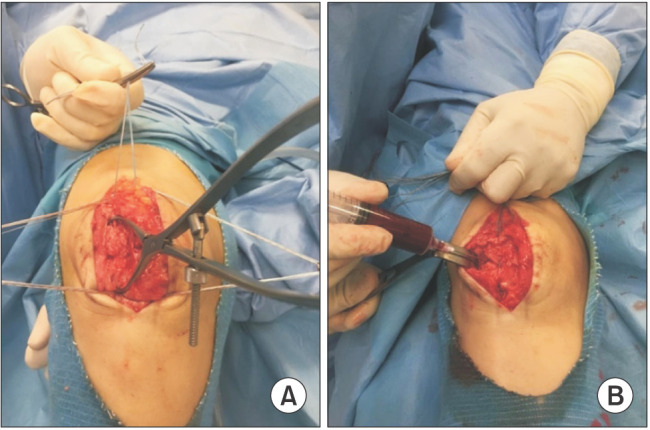
Fig. 8. Postoperative lateral radiograph.
Postoperative Care and Follow-up
The patient was kept in a hinged knee brace locked at full extension for 3 weeks. Partial weight-bearing was allowed after 2 weeks, full weight-bearing was allowed after 1 month. No knee stiffness was noticed after this period, while a moderate quadriceps weakness was detected. Active and passive knee flexion from 0° to 90° was allowed after 3 weeks. The patient was discharged 2 days after the procedure, and the first follow-up appointment was planned 2 weeks postoperatively. The patient was followed up every 4 weeks for clinical, functional, and radiographic evaluation, and at 3- to 6-month intervals thereafter. The patient was last followed up 1 year after the surgical procedure. At that time, the patient reported full functional recovery and full extension and flexion of the affected knee (Fig. 9). Knee radiographs showed complete consolidation of the fracture and restoration of the anatomic articular congruity (Fig. 10). The patient reported no pain and no subjective strength deficit.
Fig. 9. (A) Full extension of the affected knee at the final follow-up. (B) Full flexion of the affected knee at the final follow-up.
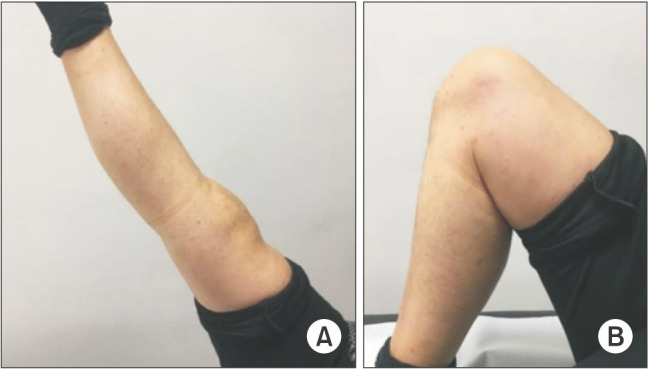
Fig. 10. Radiographic appearance at the final follow-up.
DISCUSSION
There is little published evidence to inform clinicians on the management of nonunion of patellar fractures. Thus, the decision to perform surgery to repair nonunion or excise the patella is difficult to make. For patients with low functional requirement, nonoperative management may be considered; however, ORIF is generally required for manual workers and athletes. Classically, the AO technique for fixation of patellar fractures employs Kirschner wires in combination with anterior tension wiring. As a result, patients commonly complain of soft-tissue irritation due to the presence of metallic implants subcutaneously over the anterior surface of the knee. More than one-third of patients undergo implant removal for symptomatic relief. Alternative surgical techniques have been employed, including transosseous sutures coupled with non-metallic suture-based anterior figure-of-eight cerclage. Extraosseous suture fixation with cerclage around the periphery of the whole patella combined with anterior tension banding has also been employed. Several studies have shown that non-metallic implants for patellar fracture fixation allow to achieve good clinical outcomes, reducing the rate of surgical complications and reoperation.1,4,17) There is not a clear association between risk factors and nonunion and delayed union of patellar fractures. However, open and transverse fractures and conservative management seem to be more frequently associated with nonunion and delayed union.3,13) Open fractures are the most common cause of nonunion, as the high-energy trauma often results in high-grade soft-tissue damage and disruption of the knee extensor mechanism. Torchia and Lewallen13) in a case series of 28 patients who underwent ORIF for open patellar fractures reported 2 nonunions (7%). Klassen and Trousdale3) reported nonunion in 4 of 19 patients (21%) with open patella fractures. The authors3) also reported mean scores of 72 and 78 points, respectively, in Knee Society and function scales, with an average range of knee motion of 127° in 2 patients who underwent conservative management of nonunion. Patients who underwent surgery experienced an improvement of their mean Knee Society score from 82 to 94 points, with improvement of their function score from 80 to 93 points. Furthermore, radiographic persistent nonunion was observed in all patients who were treated nonoperatively, but in only 1 of the patients who underwent ORIF. Uvaraj et al.,11) based on Bostman criteria, obtained excellent to good results in 20 of 22 patients who underwent ORIF. Poor results were observed in 2 patients who developed infection, implant failure, and loss of motion. No patients required quadricepsplasty.
Patellar fracture nonunion is still a clinical and surgical challenge.19,20,21) The currently recommended management of fracture nonunion involves surgery revising the previous operation with autologous bone grafting, considering to replace the fracture fixation according to the individual needs of each patient.22) Recently, to promote bone tissue regeneration, several approaches have been adopted, including physical means such as extracorporeal shock wave therapy, ultrasound, and pulsed electromagnetic fields, and biological modalities such as bone morphogenic proteins, MSCs, and PRP.22) Tissue engineering modalities to aid bone regeneration have included cells, at times implanted in extracellular matrix scaffolds, and biological promoters for growth, differentiation, and angiogenesis. MSCs are able to differentiate into various cells present in the musculoskeletal system, including adipocytes, osteoblasts, chondrocytes, myoblasts, and endothelial cells.23) MSCs can play a key role in the process of bone formation and fracture healing.24) The evidence in favor of the osteogenic potential of PRP has been observed in vitro and in vivo, concurrently promoting the differentiation and proliferation of MSCs.25) PRP is effective thanks to the release of the many growth and differentiation factors, including transforming growth factor-β, vascular endothelial growth factor, and platelet-derived growth factor, which are hosted within their alpha granules, playing a major role in tissue healing. PRP enhances healing of soft tissues and bone by depositing supraphysiological concentrations of autologous platelets at the site of injury. The use of autologous PRP in the management of delayed union and nonunion was explored by Bielecki et al.26) In their study, 12 patients had a delayed union and 20 had nonunion. Union was obtained in all patients with delayed union and in 13 patients with nonunion. Further investigations in basic science and clinical applications are necessary to characterize the musculoskeletal conditions, which will benefit from orthobiological modalities, the methods of their administration, and the optimal patient population.
The management of patella nonunions is still a challenge. A protocol for the treatment of patella nonunion does not exist and little scientifically valid evidence based on results of different approaches has been published. The optimal treatment concept of nonunion needs to take into account the clinical presentation and patients' features (age, comorbidities, and demand) to identify the best treatment strategy. Patients with low demands tend to modify their gait pattern and may not require surgery. Conversely, patients who perform heavy physical work or participate in sports usually require revision surgery. Many techniques have been developed, including operative and nonoperative solutions. The fixation technique reported in the present article can be used in patellar fracture nonunions and primary patellar fractures. Although over the last few years orthobiologics have been introduced to improve bone and soft-tissue healing, only few clinical studies have actually been published, and the results of both MSCs and PRP augmentation are encouraging. However, high-quality, appropriately powered, prospective, randomized studies with adequate and stringent clinically relevant end points should be planned to delineate the effectiveness of PRP and MSCs in the ailments at hand.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Heusinkveld MH, den Hamer A, Traa WA, Oomen PJ, Maffulli N. Treatment of transverse patellar fractures: a comparison between metallic and non-metallic implants. Br Med Bull. 2013;107(1):69–85. doi: 10.1093/bmb/ldt013. [DOI] [PubMed] [Google Scholar]
- 2.Yang KH, Byun YS. Separate vertical wiring for the fixation of comminuted fractures of the inferior pole of the patella. J Bone Joint Surg Br. 2003;85(8):1155–1160. doi: 10.1302/0301-620x.85b8.14080. [DOI] [PubMed] [Google Scholar]
- 3.Klassen JF, Trousdale RT. Treatment of delayed and nonunion of the patella. J Orthop Trauma. 1997;11(3):188–194. doi: 10.1097/00005131-199704000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Nathan ST, Fisher BE, Roberts CS, Giannoudis PV. The management of nonunion and delayed union of patella fractures: a systematic review of the literature. Int Orthop. 2011;35(6):791–795. doi: 10.1007/s00264-010-1105-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Satku K, Kumar VP. Surgical management of non-union of neglected fractures of the patella. Injury. 1991;22(2):108–110. doi: 10.1016/0020-1383(91)90066-n. [DOI] [PubMed] [Google Scholar]
- 6.Garg P, Sahoo S, Satyakam K, Biswas D, Garg A, Mitra S. Patellar nonunions: comparison of various surgical methods of treatment. Indian J Orthop. 2012;46(3):304–311. doi: 10.4103/0019-5413.96391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dohan Ehrenfest DM, Andia I, Zumstein MA, Zhang CQ, Pinto NR, Bielecki T. Classification of platelet concentrates (Platelet-Rich Plasma-PRP, Platelet-Rich Fibrin-PRF) for topical and infiltrative use in orthopedic and sports medicine: current consensus, clinical implications and perspectives. Muscles Ligaments Tendons J. 2014;4(1):3–9. [PMC free article] [PubMed] [Google Scholar]
- 8.Shen L, Yuan T, Chen S, Xie X, Zhang C. The temporal effect of platelet-rich plasma on pain and physical function in the treatment of knee osteoarthritis: systematic review and meta-analysis of randomized controlled trials. J Orthop Surg Res. 2017;12(1):16. doi: 10.1186/s13018-017-0521-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rubio-Azpeitia E, Andia I. Partnership between platelet-rich plasma and mesenchymal stem cells: in vitro experience. Muscles Ligaments Tendons J. 2014;4(1):52–62. [PMC free article] [PubMed] [Google Scholar]
- 10.Knobloch K, Yoon U, Vogt PM. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and publication bias. J Craniomaxillofac Surg. 2011;39(2):91–92. doi: 10.1016/j.jcms.2010.11.001. [DOI] [PubMed] [Google Scholar]
- 11.Uvaraj NR, Mayil Vahanan N, Sivaseelam A, Mohd Sameer M, Basha IM. Surgical management of neglected fractures of the patella. Injury. 2007;38(8):979–983. doi: 10.1016/j.injury.2007.02.025. [DOI] [PubMed] [Google Scholar]
- 12.Bhimani R, Singh P, Bhimani F. Double-tension wire management of nonunion patella with severe quadriceps contracture. Case Rep Orthop. 2018;2018:1364129. doi: 10.1155/2018/1364129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Torchia ME, Lewallen DG. Open fractures of the patella. J Orthop Trauma. 1996;10(6):403–409. doi: 10.1097/00005131-199608000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Al-Obaedi O, RThakrar R, Kundra R, Iqbal MJ. Gap non-union patella fractures: case report and review of the literature. J Orthop Case Rep. 2019;9(2):69–71. doi: 10.13107/jocr.2250-0685.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Faria JL, Portella DM, Titonelli VE, et al. Patellar transskeletal traction for the treatment of chronic patellar pseudoarthrosis. Case Rep Orthop. 2019;2019:5915701. doi: 10.1155/2019/5915701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lachiewicz PF. Treatment of a neglected displaced transverse patella fracture. J Knee Surg. 2008;21(1):58–61. doi: 10.1055/s-0030-1247794. [DOI] [PubMed] [Google Scholar]
- 17.Camarda L, La Gattuta A, Butera M, Siragusa F, D'Arienzo M. FiberWire tension band for patellar fractures. J Orthop Traumatol. 2016;17(1):75–80. doi: 10.1007/s10195-015-0359-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boileau P, Alami G, Rumian A, Schwartz DG, Trojani C, Seidl AJ. The doubled-suture nice knot. Orthopedics. 2017;40(2):e382–e386. doi: 10.3928/01477447-20161202-05. [DOI] [PubMed] [Google Scholar]
- 19.Cipollaro L, Ciardulli MC, Della Porta G, Peretti GM, Maffulli N. Biomechanical issues of tissue-engineered constructs for articular cartilage regeneration: in vitro and in vivo approaches. Br Med Bull. 2019;132(1):53–80. doi: 10.1093/bmb/ldz034. [DOI] [PubMed] [Google Scholar]
- 20.Atesok K, Doral MN, Bilge O, Sekiya I. Synovial stem cells in musculoskeletal regeneration. J Am Acad Orthop Surg. 2013;21:258–259. doi: 10.5435/JAAOS-21-04-258. [DOI] [PubMed] [Google Scholar]
- 21.Toosi S, Behravan N, Behravan J. Nonunion fractures, mesenchymal stem cells and bone tissue engineering. J Biomed Mater Res A. 2018;106:2552–2562. doi: 10.1002/jbm.a.36433. [DOI] [PubMed] [Google Scholar]
- 22.Longo UG, Trovato U, Loppini M, et al. Tissue engineered strategies for pseudoarthrosis. Open Orthop J. 2012;6:564–570. doi: 10.2174/1874325001206010564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gomez-Barrena E, Padilla-Eguiluz NG, Avendano-Sola C, et al. A multicentric, open-label, randomized, comparative clinical trial of two different doses of expanded hBM-MSCs plus biomaterial versus iliac crest autograft, for bone healing in nonunions after long bone fractures: study protocol. Stem Cells Int. 2018;2018:6025918. doi: 10.1155/2018/6025918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Le AD, Enweze L, DeBaun MR, Dragoo JL. Current clinical recommendations for use of platelet-rich plasma. Curr Rev Musculoskelet Med. 2018;11(4):624–634. doi: 10.1007/s12178-018-9527-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Roffi A, Di Matteo B, Krishnakumar GS, Kon E, Filardo G. Platelet-rich plasma for the treatment of bone defects: from pre-clinical rational to evidence in the clinical practice: a systematic review. Int Orthop. 2017;41(2):221–237. doi: 10.1007/s00264-016-3342-9. [DOI] [PubMed] [Google Scholar]
- 26.Bielecki T, Gazdzik TS, Szczepanski T. Benefit of percutaneous injection of autologous platelet-leukocyte-rich gel in patients with delayed union and nonunion. Eur Surg Res. 2008;40(3):289–296. doi: 10.1159/000114967. [DOI] [PubMed] [Google Scholar]