Abstract
Suture anchors are broadly used for attaching soft tissue (e.g., tendons, ligaments, and meniscus) to the bone and have become essential devices in sports medicine and during arthroscopic surgery. As the usage of suture anchors has increased, various material-specific advantages and challenges have been reported. As a result, suture anchors are continually changing to become safer and more efficient. In this ever-changing environment, it is clinically essential for the surgeon to understand the key characteristics of existing anchors sufficiently. This paper aims to summarize the current concepts on the characteristics of available suture anchors.
Keywords: Suture anchor, Biocompatible materials, Sports medicine, Arthroscopy, Shoulder, Knee
The use of suture anchors has revolutionized orthopedic surgery because it allows for simple and efficient fixation of soft tissue (e.g., tendons and ligaments) to the bone in both open and arthroscopic surgery around the shoulder, elbow, wrist, and lower limb joints.1,2) Shoulder surgery particularly has experienced a significant change in the type of techniques used from open repair of the rotator cuff and labrum using screws, washers, transosseous sutures, and staples to arthroscopic repair using suture anchors.
The primary function of the suture anchor is to attach tissue at the proper site and maintain its position without loosening or excessive tension until physiologic healing is accomplished. An ideal suture anchor is easy to handle, maintains enough pull-out strength, prevents suture abrasion, and is absorbable without resulting in any reactions as the material dissolves.3) Various types of anchors have been developed, and designs of anchors have evolved over the recent decade to maximize their effectiveness in creating a firm tendon-to-bone repair.2,4)
METALLIC SUTURE ANCHOR
The first suture anchor designs were nonabsorbable and metallic. A specific metal can be used combined with other metals to form an alloy or alone. The two most commonly used metal anchors are titanium and stainless steel. Titanium is widely used for orthopedic applications, and it is a strong, light material by itself, but it can also be combined with iron or aluminum (Fig. 1).5) Stainless steel is an alloy of carbon, chromium, and iron. It is more resistant to corrosion than regular steel and stronger than pure iron.5) Stainless steel anchors become encapsulated by a fibrous membrane rich in inflammatory cells, whereas titanium forms a surface layer of calcium and phosphate, which links directly to the bone without evidence of this fibrous layer and with minimal inflammatory response. An oxide layer spontaneously forms, and calcium and phosphate precipitate on this layer. Then, osteoblasts bind to the surface and actively secrete osteoid matrix.6,7)
Fig. 1. Metallic suture anchor: Super Revo FT, titanium (ConMed Linvatec, Largo, FL, USA).

Although metallic suture anchors provide rigid fixation and have been used successfully for a long time, multiple disadvantages are associated with their use, especially around the shoulder.8) The complications include migration, loosening, incarceration of the metal anchors within the joint cavity, cartilage damage, and interference with diagnostic imaging, such as computed tomography scans and magnetic resonance imaging (MRI).9,10) Furthermore, if metal anchors are located, revision surgery is more difficult because the anchors must be either avoided or removed, and they release metal ions into the surrounding tissues.5,11)
BIODEGRADABLE SUTURE ANCHOR RESULTS
Recently, biodegradable suture anchors developed to help overcome the reported complications associated with metallic anchors have been used much more widely.12) The advantages of biodegradable anchors compared with metallic anchors are as follows: (1) less complicated revision surgery, (2) better postsurgical imaging, (3) improved biocompatibility, and (4) lack of need for removal operation.
Biodegradable materials used for orthopedic applications are natural, synthetic, or biosynthetic polymers. These are designed to be biocompatible and not to elicit an immune response. Recently, more than dozens of polymers have been developed for use in surgery. These polymers are long-chain macromolecules composed of multiple covalently bonded monomers and can be composed of a single repeating monomer or combinations of more than one monomer.13,14)
Polyglycolic Acid, Poly-Lactic Acid, Poly-L-Lactic Acid
Polyglycolic acid (PGA) is one of the first degradable polymers researched in biomedical fields. Since the 1970s, surgeons used PGA as a degradable suture. While it was initially also used as a biodegradable anchor, the rapid degradation of PGA and loss of strength shortly after surgery resulted in its discontinuation.15) Degradation of PGA starts during the first week after anchor implantation; as the glycolic acid products are released, they can cause an inflammatory reaction with synovitis, bursitis, or lytic bone changes.3) Later, anchors started to be manufactured using poly-L-lactic acid (PLLA). It has been shown to dissolve very slowly and may maintain up to five years.16) Based on this attribute, poly-lactic acid (PLA), particularly its PLLA form, is not as problematic as PGA; however, very long degradation rates would not allow for complete bony replacement and may create intraosseous foreign body reactions.17,18) To regulate the degradation period of bioabsorbable anchors and reinforce their mechanical properties, copolymers such as poly (D, L-lactide) from L-lactide and D-lactide and PLLA with PGA have been developed.5)
Importantly, biodegradable suture anchors are also associated with challenges, including problems in the intraoperative or early postoperative period such as (1) implant breakage during anchor insertion, (2) initial fixation loss, (3) incomplete burial of anchors within a bone, which could damage the articular cartilage, and (4) possible anchor migration. Potential challenges occurring later relative to surgery include (1) the development of inflammatory reactions leading to osteolysis, (2) cyst formation, and (3) intra-articular granuloma formation along with swelling.19) Among these complications, cyst formation and osteolysis are crucial problems after rotator cuff repair. Clinicians expect that biodegradable anchors will be absorbable and be replaced by bone after healing of the tendon to the bone. Fluid signal around the anchor on T2-weighted MRI scan was graded as follows: grade 0, no fluid signal around anchor; grade 1, minimal fluid collection; grade 2, local collection of fluid; grade 3, fluid collection around the entire length of the anchor, with cyst diameter less than twice the anchor diameter; and grade 4, cyst diameter larger than grade.3,20)
BIOSTABLE SUTURE ANCHOR
Polyetheretherketone
Because some biodegradable anchors can be absorbed too quickly, the development of biostable anchors was pursued. Such a biostable anchor—a polyetheretherketone (PEEK) polymer—is obtained by dialkylation of bisphenol salts (Fig. 2).5,21)
Fig. 2. Biostable suture anchors. (A) ReelX STT (Stryker, San Jose, CA, USA). (B) PopLok (ConMed Linvatec, Largo, FL, USA). (C) FootPrint (Smith & Nephew, Andover, MA, USA).
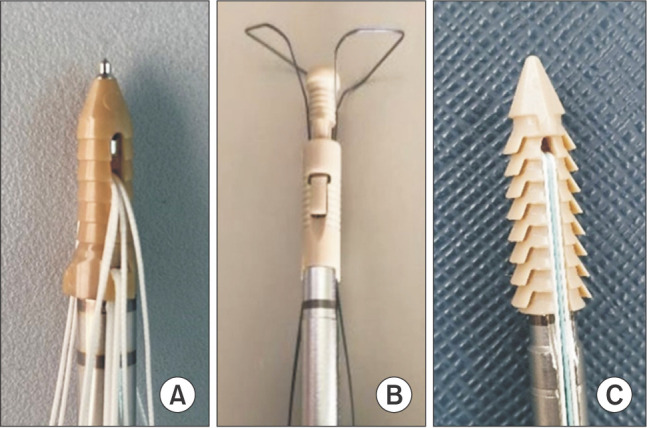
PEEK is increasingly becoming used in tribological components because of its excellent performance. PEEK materials showed high strength, strong mechanical properties, good wear- and heat-resistance, and excellent chemical and biological resistance. Therefore, it has many other applications in engineering and medicine.22) PEEK also offers advantages, such as good postoperative imaging and stable fixation, and no complications associated with polymer degradation. Importantly, the major problem with PEEK has been shown to be poor osseointegration. Overall, however, the development of PEEK anchor has led to the adoption of biocomposite materials that may support osteoconductive ingrowth.5)
BIOCOMPOSITE SUTURE ANCHOR
Biocomposite suture anchors are composed of both a biodegradable polymer material and a bone formation-promoting bioceramic material. The most commonly used bioceramic is beta-tricalcium phosphate (β-TCP); others include hydroxyapatite, calcium sulfate, and calcium carbonate.3) TCP is widely used in orthopedic surgery to fill bone defects because (1) it has a mineral content similar to that of human bone, (2) its macro-porosity and micro-porosity is osteoconductive, and (3) it has excellent biocompatibility and mechanical resistance. Unlike β-TCP, hydroxyapatite is a natural mineral substance with an affinity to bones and is highly biocompatible since it is similar to a mineral component of teeth and bones of mammals.23,24) Generally, hydroxyapatite-based bone substitute materials are considered nonabsorbable or have much lower degradation rates than β-TCP (Fig. 3).25,26)
Fig. 3. Biocomposite suture anchors. (A) BioComposite Corkscrew FT, 15% beta-tricalcium phosphate and 85% poly-L-lactic acid (Arthrex, Naples, PL, USA). (B) Genesis CrossFT, 23% beta-tricalcium phosphate and 77% poly-lactic acid (ConMed Linvatec, Largo, FL, USA).
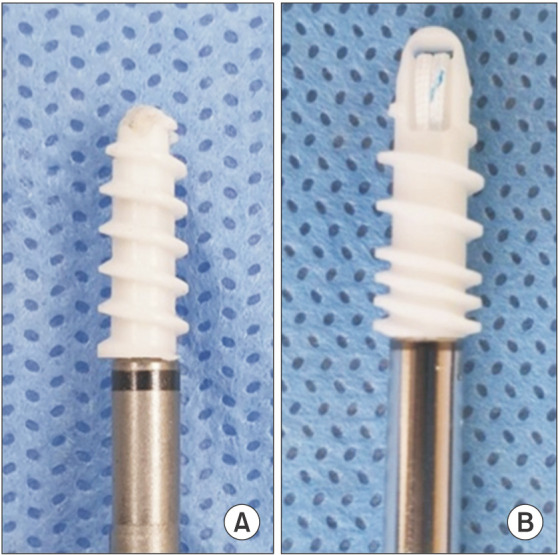
Poly-Lactic Co-Glycolide/β-TCP
Poly-lactic co-glycolide (PLGA)/β-TCP is a biocomposite material explicitly developed to promote absorption at a controlled rate.27) PLGA/β-TCP minimizes inflammatory reaction while promoting osteoconductivity at the implant site via the homogeneously disseminated β-TCP within the absorbable copolymer. This material has the highest reported osteoconductivity rate in the literature.28,29,30) A systematic review revealed that almost 90% of suture anchors composed of PLGA/β-TCP were absorbed within 3 years and promoted osteoconductivity with few reported adverse events. This particular character is highly beneficial because, if required, unexpected revision surgery is not complicated by anchor removal. Furthermore, the absorption period is slow enough to provide adequate mechanical fixation of soft tissues to the bone during the physiologic healing and to prevent inflammatory reaction and cystic formation that are common with fast-absorbing materials.31,32)
PLGA/β-TCP/Calcium Sulfate
Recent biocomposite suture anchor materials consist of 65% PLGA, 15% β-TCP, and 20% calcium sulfate (CS) (Fig. 4).33) PLGA showed a resorption time of 24 months.34) And the other two components have shorter resorption times as shown in animal models (β-TCP, 18 months and CS, 4–12 weeks).35,36) The use of this type of suture anchor is associated with: (1) strong primary stability, (2) good healing of the soft tissue, and (3) nearly complete absorption within 24 months. Furthermore, it is advantageous to prevent anchor-related cyst formation and fluid assembly by using fast-absorbing materials. Vonhoegen et al.33) analyzed 82 PLGA/β-TCP/CS anchors in 48 patients who had undergone arthroscopic rotator cuff repair. They reported that the degradation process seemed to be completed within 21 months, and there was no severe osteolysis or cyst formation observed around any of the 82 anchors. Only two retears occurred, and no anchor pull-out complications were detected.33)
Fig. 4. Biocomposite suture anchor: Healicoil Regenesorb (Smith & Nephew, Andover, MA, USA).

ALL-SOFT SUTURE ANCHOR
Solid type suture anchors (e.g., metal and polymer) have been studied extensively and found to be sufficient for maintaining physiologic loads at soft tissue to bone junctions. Usually, these solid type anchors need surgical preparation of the bony footprint site (decortication, punching, or drilling) that may cause bone loss because of the grounding piece's volume.37)
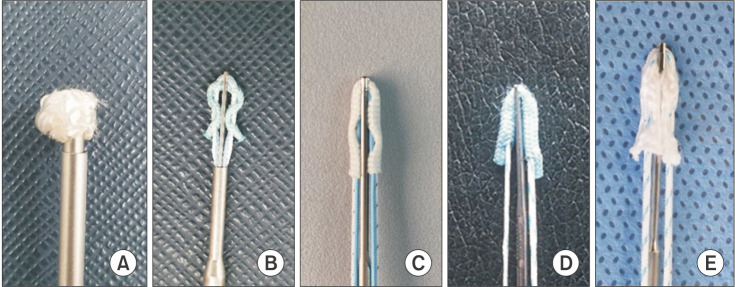
All-soft suture anchors (ASAs) were developed to minimize complications and invasiveness related to the use of solid type anchors. These ASAs consist of one or more ultra-high-molecular-weight polyethylene (UHMWPE)-containing sutures (Fig. 5).
Fig. 5. All-soft suture anchors. (A) Q-Fix (Smith & Nephew, Andover, MA, USA). (B) Suturefix (Smith & Nephew). (C) Iconix (Stryker Endoscopy, San Jose, CA, USA). (D) JuggerKnot (Biomet Sports Medicine, Warsaw, IN, USA). (E) Y-Knot (ConMed Linvatec, Largo, FL, USA).
The ASAs typically consist of a sleeve or tape made of suture material through which the UHMWPE-containing suture is woven. This fixation mechanism differs compared with screw-type suture anchors. When the ASA is inserted into the bone and the primary suture is pulled, the sleeve or tape is cinched up to compress against the overlying cortical bone creating a “ball” that works as the anchor. It allows the suture anchor to be placed in a tunnel with a smaller diameter (1–3 mm), thereby preserving bone and hypothetically allowing for more bone preservation, which may be particularly beneficial due to limited bone stock at the glenoid rim or acetabulum. Also, even if an anchor failure occurs, joint damage may be minimized because of the soft anchor body.38)
Despite these advantages of ASAs, many surgeons have been worried about weaker fixation associated with ASAs in the clinical setting. Dwyer et al.39) reported ASAs displayed more significant laxity, inferior fixation, and early displacement in the bovine bone and cadaveric bone compared to screw anchors. A biomechanical analysis by Mazzocca et al.40) compared the use of an ASA to a solid anchor, which consists of a PLLA body, in glenoid labral repair and observed no statistical difference in maximum load to failure or displacement at failure. However, the force required for 2 mm of repaired labral displacement was significantly lower with the ASA compared with the conventional anchor. With regard to rotator cuff repair, the minimum fixation load required for a rotator cuff has not been established clinically and probably can vary with the quality of bone and rotator cuff tendon. However, 250 N has been identified as the load that is needed for the rehabilitation period of rotator cuff tendon repair. According to a biomechanical study by Barber and Herbert41), all 10 different types of ASAs successfully exceeded this level.42)
CONCLUSIONS
An ideal biodegradable suture anchor would provide adequate mechanical fixation, have excellent biocompatibility, completely degrade when it is no longer needed, decrease the prevalence of peri-anchor cyst formation, and ultimately be replaced by bone. However, an ideal suitable bioresorbable suture anchor material has not yet been invented. The surgeon should consider the status of bone quality, predictable complications, material-related adverse reactions, and the need for potential future revision surgery when determining the most appropriate suture anchor. For these reasons, it is essential that surgeons understand key characteristics of a variety of currently available anchors.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Visscher LE, Jeffery C, Gilmour T, Anderson L, Couzens G. The history of suture anchors in orthopaedic surgery. Clin Biomech (Bristol, Avon) 2019;61:70–78. doi: 10.1016/j.clinbiomech.2018.11.008. [DOI] [PubMed] [Google Scholar]
- 2.Ozbaydar M, Elhassan B, Warner JJ. The use of anchors in shoulder surgery: a shift from metallic to bioabsorbable anchors. Arthroscopy. 2007;23(10):1124–1126. doi: 10.1016/j.arthro.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 3.Barber FA. Biodegradable materials: anchors and interference screws. Sports Med Arthrosc Rev. 2015;23(3):112–117. doi: 10.1097/JSA.0000000000000062. [DOI] [PubMed] [Google Scholar]
- 4.Mueller MB, Fredrich HH, Steinhauser E, Schreiber U, Arians A, Imhoff AB. Biomechanical evaluation of different suture anchors for the stabilization of anterior labrum lesions. Arthroscopy. 2005;21(5):611–619. doi: 10.1016/j.arthro.2005.01.012. [DOI] [PubMed] [Google Scholar]
- 5.Suchenski M, McCarthy MB, Chowaniec D, et al. Material properties and composition of soft-tissue fixation. Arthroscopy. 2010;26(6):821–831. doi: 10.1016/j.arthro.2009.12.026. [DOI] [PubMed] [Google Scholar]
- 6.de Medeiros WS, de Oliveira MV, Pereira LC, de Andrade MC. Bioactive porous titanium: an alternative to surgical implants. Artif Organs. 2008;32(4):277–282. doi: 10.1111/j.1525-1594.2008.00543.x. [DOI] [PubMed] [Google Scholar]
- 7.Schlegel P, Hayes JS, Frauchiger VM, et al. An in vivo evaluation of the biocompatibility of anodic plasma chemical (APC) treatment of titanium with calcium phosphate. J Biomed Mater Res B Appl Biomater. 2009;90(1):26–34. doi: 10.1002/jbm.b.31249. [DOI] [PubMed] [Google Scholar]
- 8.Kaar TK, Schenck RC, Jr, Wirth MA, Rockwood CA., Jr Complications of metallic suture anchors in shoulder surgery: a report of 8 cases. Arthroscopy. 2001;17(1):31–37. doi: 10.1053/jars.2001.18246. [DOI] [PubMed] [Google Scholar]
- 9.Marquardt B, Witt KA, Gotze C, Liem D, Steinbeck J, Potzl W. Long-term results of arthroscopic Bankart repair with a bioabsorbable tack. Am J Sports Med. 2006;34(12):1906–1910. doi: 10.1177/0363546506290404. [DOI] [PubMed] [Google Scholar]
- 10.Silver MD, Daigneault JP. Symptomatic interarticular migration of glenoid suture anchors. Arthroscopy. 2000;16(1):102–105. doi: 10.1016/s0749-8063(00)90136-1. [DOI] [PubMed] [Google Scholar]
- 11.Weiler A, Hoffmann RF, Stahelin AC, Helling HJ, Sudkamp NP. Biodegradable implants in sports medicine: the biological base. Arthroscopy. 2000;16(3):305–321. doi: 10.1016/s0749-8063(00)90055-0. [DOI] [PubMed] [Google Scholar]
- 12.Li LH, Kong YM, Kim HW, et al. Improved biological performance of Ti implants due to surface modification by micro-arc oxidation. Biomaterials. 2004;25(14):2867–2875. doi: 10.1016/j.biomaterials.2003.09.048. [DOI] [PubMed] [Google Scholar]
- 13.Nho SJ, Provencher MT, Seroyer ST, Romeo AA. Bioabsorbable anchors in glenohumeral shoulder surgery. Arthroscopy. 2009;25(7):788–793. doi: 10.1016/j.arthro.2008.08.018. [DOI] [PubMed] [Google Scholar]
- 14.Goradia VK, Mullen DJ, Boucher HR, Parks BG, O'Donnell JB. Cyclic loading of rotator cuff repairs: a comparison of bioabsorbable tacks with metal suture anchors and transosseous sutures. Arthroscopy. 2001;17(4):360–364. doi: 10.1053/jars.2001.21243. [DOI] [PubMed] [Google Scholar]
- 15.Speer KP, Warren RF, Pagnani M, Warner JJ. An arthroscopic technique for anterior stabilization of the shoulder with a bioabsorbable tack. J Bone Joint Surg Am. 1996;78(12):1801–1807. doi: 10.2106/00004623-199612000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Barber FA. Biology and clinical experience of absorbable materials in ACL fixation. Tech Orthop. 1999;14(1):34–42. [Google Scholar]
- 17.Nusselt T, Freche S, Klinger HM, Baums MH. Intraosseous foreign body granuloma in rotator cuff repair with bioabsorbable suture anchor. Arch Orthop Trauma Surg. 2010;130(8):1037–1040. doi: 10.1007/s00402-010-1125-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boden RA, Burgess E, Enion D, Srinivasan MS. Use of bioabsorbable knotless suture anchors and associated acceler ated shoulder arthropathy: report of 3 cases. Am J Sports Med. 2009;37(7):1429–1433. doi: 10.1177/0363546509332248. [DOI] [PubMed] [Google Scholar]
- 19.Barber FA. Complications of biodegradable materials: anchors and interference screws. Sports Med Arthrosc Rev. 2015;23(3):149–155. doi: 10.1097/JSA.0000000000000076. [DOI] [PubMed] [Google Scholar]
- 20.Kim SH, Oh JH, Lee OS, Lee HR, Hargens AR. Postoperative imaging of bioabsorbable anchors in rotator cuff repair. Am J Sports Med. 2014;42(3):552–557. doi: 10.1177/0363546513517538. [DOI] [PubMed] [Google Scholar]
- 21.Zhang QS, Liu S, Zhang Q, et al. Comparison of the tendon damage caused by four different anchor systems used in transtendon rotator cuff repair. Adv Orthop. 2012;2012:798521. doi: 10.1155/2012/798521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ji S, Sun C, Zhao J, Liang F. Comparison and analysis on mechanical property and machinability about polyetheretherketone and carbon-fibers reinforced polyetheretherketone. Materials (Basel) 2015;8(7):4118–4130. doi: 10.3390/ma8074118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tamai N, Myoui A, Tomita T, et al. Novel hydroxyapatite ceramics with an interconnective porous structure exhibit superior osteoconduction in vivo. J Biomed Mater Res. 2002;59(1):110–117. doi: 10.1002/jbm.1222. [DOI] [PubMed] [Google Scholar]
- 24.Lee DW, Lee JW, Kim SB, et al. Comparison of poly-L-lactic acid and poly-L-lactic acid/hydroxyapatite bioabsorbable screws for tibial fixation in ACL reconstruction: clinical and magnetic resonance imaging results. Clin Orthop Surg. 2017;9(3):270–279. doi: 10.4055/cios.2017.9.3.270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bohner M. Calcium orthophosphates in medicine: from ceramics to calcium phosphate cements. Injury. 2000;31(Suppl 4):37–47. doi: 10.1016/s0020-1383(00)80022-4. [DOI] [PubMed] [Google Scholar]
- 26.Jensen SS, Broggini N, Hjorting-Hansen E, Schenk R, Buser D. Bone healing and graft resorption of autograft, anorganic bovine bone and beta-tricalcium phosphate: a histologic and histomorphometric study in the mandibles of minipigs. Clin Oral Implants Res. 2006;17(3):237–243. doi: 10.1111/j.1600-0501.2005.01257.x. [DOI] [PubMed] [Google Scholar]
- 27.Randelli P, Compagnoni R, Aliprandi A, et al. Long-term degradation of poly-lactic co-glycolide/β-tricalcium phosphate biocomposite anchors in arthroscopic bankart repair: a prospective study. Arthroscopy. 2014;30(2):165–171. doi: 10.1016/j.arthro.2013.09.082. [DOI] [PubMed] [Google Scholar]
- 28.Ntagiopoulos PG, Demey G, Tavernier T, Dejour D. Comparison of resorption and remodeling of bioabsorbable interference screws in anterior cruciate ligament reconstruction. Int Orthop. 2015;39(4):697–706. doi: 10.1007/s00264-014-2530-8. [DOI] [PubMed] [Google Scholar]
- 29.Barber FA, Dockery WD, Cowden CH., 3rd The degradation outcome of biocomposite suture anchors made from poly L-lactide-co-glycolide and β-tricalcium phosphate. Arthroscopy. 2013;29(11):1834–1839. doi: 10.1016/j.arthro.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 30.Barber FA, Dockery WD, Hrnack SA. Long-term degradation of a poly-lactide co-glycolide/β-tricalcium phosphate biocomposite interference screw. Arthroscopy. 2011;27(5):637–643. doi: 10.1016/j.arthro.2010.11.056. [DOI] [PubMed] [Google Scholar]
- 31.Bostman O, Pihlajamaki H. Clinical biocompatibility of biodegradable orthopaedic implants for internal fixation: a review. Biomaterials. 2000;21(24):2615–2621. doi: 10.1016/s0142-9612(00)00129-0. [DOI] [PubMed] [Google Scholar]
- 32.Bostman OM, Pihlajamaki HK. Adverse tissue reactions to bioabsorbable fixation devices. Clin Orthop Relat Res. 2000;(371):216–227. [PubMed] [Google Scholar]
- 33.Vonhoegen J, John D, Hagermann C. Osteoconductive resorption characteristics of a novel biocomposite suture anchor material in rotator cuff repair. J Orthop Surg Res. 2019;14(1):12. doi: 10.1186/s13018-018-1049-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Barber FA, Dockery WD. Long-term absorption of betatricalcium phosphate poly-L-lactic acid interference screws. Arthroscopy. 2008;24(4):441–447. doi: 10.1016/j.arthro.2007.10.004. [DOI] [PubMed] [Google Scholar]
- 35.Allison DC, Lindberg AW, Samimi B, Mirzayan R, Menendez LR. A comparison of mineral bone graft substitutes for bone defects. US Oncol Hematol. 2011;7(1):38–49. [Google Scholar]
- 36.Walsh WR, Morberg P, Yu Y, et al. Response of a calcium sulfate bone graft substitute in a confined cancellous defect. Clin Orthop Relat Res. 2003;(406):228–236. doi: 10.1097/01.blo.0000030062.92399.6a. [DOI] [PubMed] [Google Scholar]
- 37.Barber FA, Herbert MA, Beavis RC, Barrera Oro F. Suture anchor materials, eyelets, and designs: update 2008. Arthroscopy. 2008;24(8):859–867. doi: 10.1016/j.arthro.2008.03.006. [DOI] [PubMed] [Google Scholar]
- 38.Lorbach O, Wilmes P, Brogard P, Seil R. Complications related to implants in arthroscopic shoulder surgery. Orthopade. 2008;37(11):1073–1079. doi: 10.1007/s00132-008-1347-9. [DOI] [PubMed] [Google Scholar]
- 39.Dwyer T, Willett TL, Dold AP, et al. Maximum load to failure and tensile displacement of an all-suture glenoid anchor compared with a screw-in glenoid anchor. Knee Surg Sports Traumatol Arthrosc. 2016;24(2):357–364. doi: 10.1007/s00167-013-2760-0. [DOI] [PubMed] [Google Scholar]
- 40.Mazzocca AD, Chowaniec D, Cote MP, et al. Biomechanical evaluation of classic solid and novel all-soft suture anchors for glenoid labral repair. Arthroscopy. 2012;28(5):642–648. doi: 10.1016/j.arthro.2011.10.024. [DOI] [PubMed] [Google Scholar]
- 41.Barber FA, Herbert MA. All-suture anchors: biomechanical analysis of pullout strength, displacement, and failure mode. Arthroscopy. 2017;33(6):1113–1121. doi: 10.1016/j.arthro.2016.09.031. [DOI] [PubMed] [Google Scholar]
- 42.Strauss E, Frank D, Kubiak E, Kummer F, Rokito A. The effect of the angle of suture anchor insertion on fixation failure at the tendon-suture interface after rotator cuff repair: deadman's angle revisited. Arthroscopy. 2009;25(6):597–602. doi: 10.1016/j.arthro.2008.12.021. [DOI] [PubMed] [Google Scholar]