Abstract
Backgroud
It has been widely reported that vitamin D (vit D) affects preoperative, postoperative, and long-term outcomes after total knee arthroplasty (TKA). Our aim was to study vit D trajectory after TKA and compare effects of oral versus intramuscular (IM) supplementation in insufficient patients and assess its effects on immediate functional recovery in the first 2 weeks after TKA.
Methods
Vit D levels < 30 ng/mL are considered insufficient. We prospectively enrolled 60 patients (20 per group): group I, vit D sufficient patients; group II, vit D insufficient patients given IM supplementation (cholecalciferol 6,00,000 IU); and group III, vit D insufficient patients given oral supplementation (cholecalciferol 600,000 IU). Vit D levels, knee flexion, Timed Up and Go (TUG) test results, and visual analog scale (VAS) score were recorded preoperatively and postoperatively on day 3 and 14.
Results
In group I, mean preoperative vit D significantly dropped at postoperative day (POD) 3 and POD 14 (p = 0.001). In group II, mean preoperative vit D rose at POD 3 and rose significantly at POD 14 (p = 0.001). In group III, mean preoperative vit D increased significantly at both POD 3 and POD 14 (p < 0.001). Also, in group III, the rise in vit D was significantly higher than that in group II both at POD 3 and POD 14 (p < 0.05). In group III, 19 of 20 insufficient patients became sufficient on POD 3 and all 20 by POD 14. In group II, even by POD 14, only 11 of 20 insufficient patients became sufficient. Functional parameters (flexion, change in flexion, TUG test results, and VAS score) were comparable (p > 0.05) in all groups. Changes in TUG test showed a significant increase in group II (48.5 seconds) when compared to group I (35.5 seconds) at POD 3 (p < 0.05), suggesting a slower recovery. It remained comparable (p > 0.05) between group III and group I.
Conclusions
We found that vit D insufficient patients can be rapidly supplemented on the morning of surgery with a large dose of oral cholecalciferol 600,000 IU, and the effect was consistent over 2 weeks after surgery. Orally supplemented vit D insufficient patients also showed functional recovery comparable to vit D sufficient patients. IM supplementation increased vit D levels only at 2 weeks and the rise was significantly lower than oral supplementation. Interestingly, approximately 25% of vit D sufficient patients who were not supplemented after TKA became insufficient in the first 2 weeks postoperatively.
Keywords: Vitamin D supplementation, Oral administration, Intramuscular injection, Total knee arthroplasty, Results
Vitamin D (Vit D) has an important role in bone mineralization and remodeling, muscle function, and physical health.1) Most experts define vit D deficiency as a 25-hydroxy vit D level of less than 20 ng/mL (< 50 nmol/L).2,3,4) A level of 21–29 ng/mL (52.5–72.5 nmol/L) can be considered to indicate relative insufficiency, a level of 30 ng/mL or greater (> 72.5 nmol/L) sufficiency, and > 150 ng/mL (> 375 nmol/L) hypervitaminosis.5,6,7,8)
Vit D levels are found to be low in as many as 40%–82% of patients undergoing arthroplasty.9,10,11,12) A great interest has been generated in vit D in recent years because of the growing evidence of its association with poorer preoperative functional activity13,14,15) and adverse effects on the postoperative function.16,17) Besides, vit D deficiency has been specifically linked to periprosthetic joint infections18,19,20,21) and to a higher rate of several other postoperative complications.22,23) The length of hospital stay was also reported to be significantly longer for patients with low vit D levels.10,16) At the same time, studies report fewer complications following arthroplasty in patients with normal vit D levels.24)
Several studies point to vit D as a modifiable risk factor and suggest optimizing preoperative vit D levels in patients considering arthroplasty. Alamanda and Springer21) have prepared a systematic review of 12 modifiable risk factors for periprosthetic joint infection and have recommended guidelines for correction of vit D. Also, studies have shown that there is a drop in vit D levels after surgery.9,25) Our earlier study14) found that vit D deficient patients who were supplemented after surgery achieved functional results comparable to vit D sufficient patients by 3 months. Thus, it is well established in the literature that vit D has significant effects on longer-term functional outcome after total knee arthroplasty (TKA). In the last decade, TKA management has aimed to improve immediate function to help patients recover faster. There are currently no reports showing if vit D levels have an effect on immediate recovery after TKA.
We hypothesized that vit D levels could be rapidly corrected by high-dose oral and intramuscular (IM) supplementation on the day of surgery. We undertook our study with two aims: (1) to examine the trajectory of vit D levels in our series of vit D sufficient and insufficient TKA patients over the first 2 weeks after surgery and compare the effect of the mode of supplementation (oral vs IM) on the vit D trajectory in insufficient patients and (2) to assess and compare the immediate functional recovery after TKA in the first 2 weeks in vit D sufficient and insufficient patients.
METHODS
After obtaining Institutional Review Board and Ethics Committee approval (Registration No. ECR/606/Inst/MH/2014), we prospectively enrolled all patients undergoing primary TKA between May 2018 and June 2019 performed by a single surgeon (RNM) for this study and all patients gave an informed consent. Based on their preoperative vit D levels and the means of supplementation, we divided them into three groups. Group I was the vit D sufficient8) control group (25 hydroxy vit D level > 30 ng/mL) and no preoperative supplementation; group II was the vit D insufficient group (25 hydroxy vit D level < 30 ng/mL) with IM supplementation; and group III was the vit D insufficient group (25 hydroxy vit D level < 30 ng/mL) with oral supplementation.
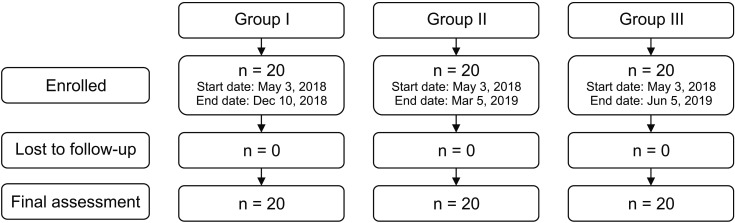
Recruitment for each group stopped when we had 20 patients in each group (Fig. 1). Insufficient patients were randomized to be in group II or III using computer-generated randomization sequence on computer software (https://www.randomizer.org/). Injection of Arachitol, Cholecalciferol IP 600,000 IU (Abbott India Ltd., Bhiwandi, India) was used for both IM and oral supplementation on the morning of surgery.
Fig. 1. Flowchart of study.
Sixty patients were enrolled, 20 patients in each group. All patients underwent TKA by the same surgeon (RNM) with uniform intraoperative and postoperative protocols. Vit D levels were assessed preoperatively (6–8 pm 1 day preoperatively) and on postoperative day (POD) 3 and 14 (7–10 am). For assessing the functional outcome, parameters including flexion, Timed Up and Go (TUG) test, and visual analog scale score (VAS score) for pain were recorded by unblinded observers (DJ, NB). Flexion was measured in degrees using a standard handheld goniometer by the same resident doctor (DJ) in all cases at 8 PM (± 1 hour) on POD 3 and 8 AM (± 1 hour) on POD 14. Its center of rotation was placed in line with the center of the knee, the fixed arm was aligned with the greater trochanter, and the mobile arm was aligned with the lateral malleolus. Range of motion was measured at the edge of bed with the patient sitting with his thighs parallel and horizontal to the floor. Two trials were performed for both measurements. If the difference was less than 5°, then an average of the two readings was taken. If the difference was more than 5°, then a third measurement was taken and the average of the closest two measurements was taken. TUG test records the time in seconds required to get up from a chair with armrests, walk 3 m, turn around, walk back to the chair, and sit down.26,27) Our chair seat was 46 cm in height, and the 3-m walkway was delimited by permanent painted lines on the floor. The standardized procedure included a demonstration for the subject and a trial round preoperatively. Test timing was recorded on a smartphone stopwatch. TUG tests were conducted at 8 PM (± 1 hour) on POD 3 and at 8 AM (± 1 hour) on POD 14. The test was performed using a walker by all patients on POD 3 and POD 14. VAS score is a subjective score of pain and was measured on a scale of 0 (no pain) to 10 (very severe pain) at 8 PM (± 1 hour) preoperatively and 8 AM (± 1 hour) on POD 3 and POD 14.
Sample size of the study was determined using SAS 9.2 package (SAS Institute Inc., Cary, NC, USA). To calculate the sample size for assessing oral supplementation, we followed the study by Cipriani et al.28) and arrived at a sample size of 6 patients per group (power = 90%, α = 0.05). We found no reference study to calculate the sample size for IM supplementation and functional recovery evaluation in the first 2 weeks after surgery, so we decided to increase the sample size to 20 patients in each group (60 patients in all) and perform a power analysis post hoc for immediate functional recovery results.
Data were analyzed using SPSS ver. 15.0 (SPSS Inc., Chicago, IL, USA). Data were checked for normality by Shapiro Wilk statistical test. Shapiro-Wilk test confirmed normality of all variables. Data were given as mean and standard deviation for quantitative variables and number (percentage, %) for qualitative variables. Student paired t-test was applied to compare mean values at two different timepoints. One-way analysis of variance (F test) was applied to compare mean values of three groups. Only after getting significant difference by F test, Scheffe post-hoc test was applied to compare the pair of means. Chi-square tests were applied to compare percentages of three groups. All tests were two-tailed. Level of Significance was taken as p ≤ 0.05. Using SAS 9.2 package (SAS Institute, Cary, NC, USA) and considering the increase in TUG time from preoperative to POD 3 as an efficacy variable, the power was calculated to be 81.4 at an alpha error of 0.05.
RESULTS
Demographics of all three groups were comparable (Table 1).
Table 1. General Demographics.
| Variable | Group I (n = 20) | Group II (n = 20) | Group III (n = 20) | p-value | |
|---|---|---|---|---|---|
| Age (yr) | 66.0 ± 5.2 | 64.0 ± 8.3 | 65.1 ± 7.9 | 0.7 | |
| Height (cm) | 154.9 ± 6.4 | 159.4 ± 10.9 | 156.9 ± 9.8 | 0.3 | |
| Weight (kg) | 74.8 ± 10.0 | 80.1 ± 15.8 | 78.7 ± 15.8 | 0.5 | |
| Body mass index (kg/m2) | 31.2 ± 3.7 | 31.6 ± 4.1 | 31.8 ± 3.8 | 0.9 | |
| Sex | 0.2 | ||||
| Male | 3 (15) | 5 (25) | 8 (40) | ||
| Female | 17 (85) | 15 (75) | 12 (60) | ||
Values are presented as mean ± standard deviation or number (%).
Vit D Trajectory
In group I, there was a significant fall in the preoperative mean vit D at POD 3 (p = 0.001) and at POD 14 (p = 0.001) (Table 2). Of the 20 patients in group I, 6 patients became insufficient by POD 3 and 4 remained insufficient at POD 14. Thus, 30% of the vit D sufficient patients had become vit D insufficient by POD 3 (Table 3). In group II, there was a rise in the preoperative mean vit D at POD 3 (p = 0.06) and POD 14 (p = 0.001) (Table 2). Of the 20 patients in group II, 7 patients became sufficient by POD 3 and 11 patients (55%) became sufficient by POD 14 (Table 3). In group III, the preoperative mean vit D rose significantly at POD 3 (p < 0.001) and at POD 14 (p < 0.001) (Table 2). Of the 20 patients, 19 patients became sufficient by POD 3 and all 20 (100%) became sufficient at POD 14 (Table 3).
Table 2. Comparison of Vitamin D Level between Two Points for Each Group.
| Variable | Group I | Group II | Group III | |
|---|---|---|---|---|
| Preop | 48.3 ± 11.6 (31.2–70) | 21.5 ± 7.7 (8.1–30) | 20.2 ± 6.6 (5.2–8.2) | |
| POD 3 | 40.4 ± 10.7 (24.6–56.7) | 31.2 ± 24.9 (3–107.7) | 69.9 ± 16.4 (29.6–99) | |
| POD 14 | 38.9 ± 8.9 (27.4–57.7) | 38.9 ± 21.5 (6–97.3) | 68.5 ± 17.9 (42.5–106) | |
| p-value | ||||
| Preop to POD 3 | 0.001 | 0.06 | < 0.001 | |
| Preop to POD 14 | 0.001 | 0.001 | < 0.001 | |
Values are presented as mean ± standard deviation (range).
Preop: preoperative, POD: postoperative day.
Table 3. Vitamin D Based on Sufficient and Insufficient Levels at Three Timepoints.
| Group | Preop | POD 3 | POD 14 | p-value | |
|---|---|---|---|---|---|
| Group I | 0.018 | ||||
| Sufficient | 20 (100) | 14 (70) | 16 (80) | ||
| Insufficient | 0 | 6 (30) | 4 (20) | ||
| Group II | < 0.001 | ||||
| Sufficient | 0 | 7 (35) | 11 (55) | ||
| Insufficient | 20 (100) | 13 (65) | 9 (45) | ||
| Group III | < 0.001 | ||||
| Sufficient | 0 | 19 (95) | 20 (100) | ||
| Insufficient | 20 (100) | 1 (5) | 0 | ||
Values are presented as number (%).
Preop: preoperative, POD: postoperative day.
On preoperative comparison, group II and group III had significantly (p < 0.05) lower vit D levels as compared to group I. There was no statistical difference between group II and group III preoperatively. Group III had significantly (p < 0.05) higher vit D levels than group II and group I at POD 3 and POD 14. There was no statistical difference between group I and group II at POD 3 and POD 14 (Table 4). A maximum vit D level of 107 ng/mL was observed. There were no complications due to vit D supplementation.
Table 4. Comparison of Vitamin D Levels between Groups.
| Variable | Vitamin D (ng/mL) | p-value | ||
|---|---|---|---|---|
| Group I | Group II | Group III | ||
| Preop | 48.3 ± 11.6 | 21.5 ± 7.7 | 20.2 ± 6.6 | < 0.001 |
| POD 3 | 40.4 ± 10.7 | 31.2 ± 24.9 | 69.9 ± 16.4 | < 0.001 |
| POD 14 | 38.9 ± 8.9 | 38.9 ± 21.5 | 68.5 ± 17.9 | < 0.001 |
Values are presented as mean ± standard deviation.
Preop: preoperative, POD: postoperative day.
If p-value is significant, post-hoc Scheffe test will be applied. Significant difference: group I vs. II (p < 0.05) and group I vs. III (p < 0.05) at preop; group I vs. III (p < 0.05) and group II vs. III (p < 0.05) at POD 3; and group I vs. III (p < 0.05) and group II vs. III (p < 0.05) at POD 14.
Functional Recovery
Flexion
In groups I, II, III, the preoperative flexion and flexion achieved at POD 3 and POD 14 were comparable (p > 0.05) (Table 5). The change in flexion was also comparable between the groups (Table 5). This indicates that the range of flexion achieved was comparable in all three groups at all times.
Table 5. Outcome Parameters.
| Variable | Day | Group I | Group II | Group III | p-value |
|---|---|---|---|---|---|
| Flexion (°) | Preop | 133 ± 9.6 | 128.5 ± 16.1 | 125 ± 14 | 0.5 |
| POD 3 | 88 ± 5 | 84 ± 11.7 | 83 ± 7.5 | 0.2 | |
| POD 14 | 99 ± 9.2 | 90 ± 7.8 | 94.5 ± 10 | 0.013 | |
| Change in flexion from preop (°) | POD 3 | 45 ± 9.6 | 44.2 ± 15.8 | 41.8 ± 16.2 | 0.75 |
| POD 14 | 34.3 ± 12.9 | 38.5 ± 19 | 30.5 ± 14.1 | 0.28 | |
| TUG test (sec) | Preop | 17.1 ± 5.9 | 14.1 ± 3 | 14.7 ± 3.7 | 0.5 |
| POD 3 | 52.5 ± 12.2 | 62.6 ± 14.4 | 58.2 ± 13.9 | 0.07 | |
| POD 14 | 33 ± 7.2 | 38.8 ± 13.9 | 37.8 ± 10.7 | 0.2 | |
| Change in TUG test from preop (sec) | POD 3 | 35.5 ± 10.2 | 48.5 ± 15.1 | 43.4 ± 12.9 | 0.009* |
| POD 14 | 15.9 ± 9.8 | 24.8 ± 14.3 | 23 ± 9 | 0.038 | |
| VAS | Preop | 6 ± 1 | 6.2 ± 0.9 | 6 ±1 | 0.7 |
| POD 3 | 5.2 ± 1.1 | 5.7 ± 1.4 | 5.6 ± 1.1 | 0.07 | |
| POD 14 | 3.8 ± 0.8 | 4 ± 1 | 4.1 ± 1.1 | 0.7 | |
| Change in VAS from preop | POD 3 | 0.8 ± 1.5 | 0.5 ± 1.6 | 0.4 ± 0.9 | 0.71 |
| POD 14 | 2.2 ± 1 | 2.2 ± 1.2 | 1.9 ± 0.9 | 0.70 |
Values are presented as mean ± standard deviation.
Preop: preoperative, POD: postoperative day, TUG: Timed Up and Go, VAS: visual analog scale.
*Post-hoc test shows significant difference for change in TUG at POD 3 between group I and group II (p = 0.009).
TUG test
In groups I, II, III, the preoperative TUG time and TUG time at POD 3 and at POD 14 were comparable with no statistical difference (p > 0.05) (Table 5). However, the change in TUG time from preoperative to POD 3 value and to POD 14 value in group II was higher compared to group I with a statistical significance (p = 0.009 for POD 3, p = 0.038 for POD 14). The post-hoc test showed significance only for the POD 3 value. The change in TUG time for group III was comparable to group I at all times with no statistical difference (p > 0.05) (Table 5). This indicates that IM supplemented patients had significantly slower functional recovery at POD 3 compared to vit D sufficient patients while orally supplemented patients had comparable recovery as vit D sufficient patients at all times.
VAS score
VAS scores in all groups at all times and their change in values from preoperative levels to POD 3 and POD 14 showed no significant difference amongst the groups (p > 0.05) at all times (Table 5).
DISCUSSION
Our hypothesis was proved correct. Both supplementation methods raised the postoperative TKA vit D levels; however, oral supplementation was not only quicker but also effective in bringing 95% and 100% of the patients into sufficient range by POD 3 and POD 14, respectively. We also found that vit D levels after TKA dropped in sufficient patients and approximately 25% of the patients reached insufficient levels.
On the trajectory of vit D levels in our three study groups, we noted that more than a quarter (30%) of our vit D sufficient patients became insufficient by POD 3. Kelly et al.9) have reported that there was a significant fall in vit D as early as 2 days after the surgery. Blomberg Jensen et al.25) have reported that generation of vit D was impaired in women after elective knee replacement, resulting in low circulating levels of activated vit D. We therefore think that even vit D sufficient patients should be supplemented to maintain their levels. However, whether a large single dose used in our study was appropriate for this group or not needs to be studied first to avert hypervitaminosis.
On the trajectory of vit D levels in our deficient groups, we found that with IM supplementation, a slower rise in vit D levels was obtained as compared to the same, large dose oral administration. Only 55% of patients with IM administration became sufficient by POD 14, whereas 95% of patients with oral administration were sufficient by POD 3 and 100% by POD 14. At POD 3 and POD 14, there was a statistical difference in vit D levels between those supplemented by oral and IM administration. A large, single-dose, oral administration achieved a rapid rise, the levels achieved were significantly higher, and all (i.e., 100%) of our patients achieved sufficiency.
Kearns et al.29) have also reported a consistent rise in serum vit D levels with a large, single-dose oral vit D supplementation in their review of 30 different studies. It is noteworthy that the highest value attained in the present study by an individual subject was 107 ng/mL, which is well below the widely accepted toxic blood levels of 150 ng/mL. Heaney et al.30) demonstrated that vit D administration induces a biphasic response, with a rapid increase of serum 25(OH)D at low serum vit D3 concentrations and a slower response at higher levels. Hence, we can hypothesize that the huge increase of 25(OH)D levels after supplementation could probably be due to the low basal vit D3 concentration. Cipriani et al.28) reported similar results as our study with the same large oral dose as us and attributed it to rapid absorption and conversion of the oral load of cholecalciferol to the 25-hydroxy metabolite. On the other hand, with a single IM dose of 600,000 IU of cholecalciferol, Diamond et al reported that in subjects with vit D deficiency, 25(OH)D levels were enhanced above the threshold of sufficiency only at 4 months.31) Nugent et al.32) have reported that 11% of patients remained insufficient at 3 months after IM administration of 300,000 IU of vit D3. Ours is the only paper that has studied high-dose oral vit D supplementation in relation to TKA.
On assessment of functional recovery, we detected noteworthy findings in the TUG test. TUG test is an objective measure of function, balance, and walking ability for people with knee osteoarthritis.26,27) This test is specifically designed to evaluate function immediately after surgery when all patient-reported outcome measures and scores are not possible to administer. Though there was no significant difference in the TUG test values between all groups at all times, the change in TUG time from preoperative to POD 3 (i.e., increase in time taken to do the same activity) in the IM supplemented group was significantly longer than the vit D sufficient group. On the other hand, in the vit D insufficient group, which was orally supplemented, range of flexion was achieved, and TUG time along with the change in flexion and TUG time from preoperative to POD 3 and 14 values were all comparable with the vit D sufficient group with no statistical difference. This is an important finding as this would imply that patients with low vit D can undergo total knee replacement with the vit D levels being easily corrected by oral supplementation on the day of surgery with no compromise to their immediate postoperative functional recovery. We have no data on the functional outcome in vit D insufficient patients because we chose to supplement them all. Shin et al.17) have reported that in vit D deficiency, the Knee Society Score and Alternate Step test were adversely affected at 3 months after arthroplasty while the sit-to-stand test and TUG time, despite recording more time, did not show statistical difference. Jansen et al.16) have reported that vit D insufficient patients had a significantly worse functional outcome even at a long-term follow-up of 8 years.
Our study was limited for a duration of 2 weeks after TKA and we have compared the effect of a single oral versus IM supplementation. We remain unaware of the long-term effect of our protocols on vit D levels. Secondly, although our study was amply powered for our primary aim of detecting effects of vit D supplementation on its trajectory, the sample size may be small for functional evaluation. Considering this, we did a post-hoc analysis and found that the power of this study was more than 80% when considering only the change in TUG test as the parameter. For the other functional parameters, a larger sample size may be necessary. We believe our study results can serve to arrive at appropriate sample size for these future investigations. Lastly, since we had to choose to supplement all vit D insufficient patients, we have no data on the functional outcome in vit D insufficiency status.
We found that vit D insufficient patients can be rapidly supplemented on the morning of surgery with a large dose of oral cholecalciferol 600,000 IU, and the effect was consistent over 2 weeks after surgery. Orally supplemented vit D insufficient patients also showed functional recovery comparable to vit D sufficient patients. IM supplementation increased vit D levels only at 2 weeks and the rise was significantly lower than oral supplementation. IM supplemented patients also showed slower immediate functional activity recovery at POD 3 in the form of the change in TUG time, which was significantly longer than that in vit D sufficient patients. Interestingly, approximately 25% of vit D sufficient patients who were not supplemented after TKA became insufficient in the first 2 weeks postoperatively.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Wintermeyer E, Ihle C, Ehnert S, et al. Crucial role of vitamin D in the musculoskeletal system. Nutrients. 2016;8(6):319. doi: 10.3390/nu8060319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bischoff-Ferrari HA, Giovannucci E, Willett WC, Dietrich T, Dawson-Hughes B. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr. 2006;84(1):18–28. doi: 10.1093/ajcn/84.1.18. [DOI] [PubMed] [Google Scholar]
- 3.Malabanan A, Veronikis IE, Holick MF. Redefining vitamin D insufficiency. Lancet. 1998;351(9105):805–806. doi: 10.1016/s0140-6736(05)78933-9. [DOI] [PubMed] [Google Scholar]
- 4.Thomas MK, Lloyd-Jones DM, Thadhani RI, et al. Hypovitaminosis D in medical inpatients. N Engl J Med. 1998;338(12):777–783. doi: 10.1056/NEJM199803193381201. [DOI] [PubMed] [Google Scholar]
- 5.Heaney RP, Dowell MS, Hale CA, Bendich A. Calcium absorption varies within the reference range for serum 25-hydroxyvitamin D. J Am Coll Nutr. 2003;22(2):142–146. doi: 10.1080/07315724.2003.10719287. [DOI] [PubMed] [Google Scholar]
- 6.Dawson-Hughes B, Heaney RP, Holick MF, Lips P, Meunier PJ, Vieth R. Estimates of optimal vitamin D status. Osteoporos Int. 2005;16(7):713–716. doi: 10.1007/s00198-005-1867-7. [DOI] [PubMed] [Google Scholar]
- 7.Vogiatzi MG, Jacobson-Dickman E, DeBoer MD Drugs, and Therapeutics Committee of The Pediatric Endocrine Society. Vitamin D supplementation and risk of toxicity in pediatrics: a review of current literature. J Clin Endocrinol Metab. 2014;99(4):1132–1141. doi: 10.1210/jc.2013-3655. [DOI] [PubMed] [Google Scholar]
- 8.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 9.Kelly MA, Campbell J, Sheahan J, Murphy P. Vitamin D insufficiency in patients undergoing total knee arthroplasty in Ireland. Ir Med J. 2017;110(10):649. [PubMed] [Google Scholar]
- 10.Maier GS, Maus U, Lazovic D, Horas K, Roth KE, Kurth AA. Is there an association between low serum 25-OH-D levels and the length of hospital stay in orthopaedic patients after arthroplasty? J Orthop Traumatol. 2016;17(4):297–302. doi: 10.1007/s10195-016-0414-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Goula T, Kouskoukis A, Drosos G, et al. Vitamin D status in patients with knee or hip osteoarthritis in a Mediterranean country. J Orthop Traumatol. 2015;16(1):35–39. doi: 10.1007/s10195-014-0322-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Piuzzi NS, George J, Khlopas A, et al. High prevalence and seasonal variation of hypovitaminosis D in patients scheduled for lower extremity total joint arthroplasty. Ann Transl Med. 2018;6(16):321. doi: 10.21037/atm.2018.08.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jacob EA, Blum L, Bedair HS, Freiberg AA, Quraishi SA. The association of vitamin D status and pre-operative physical activity in patients with hip or knee osteoarthritis. J Restor Med. 2015;4(1):3–10. doi: 10.14200/jrm.2015.4.0101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maniar RN, Patil AM, Maniar AR, Gangaraju B, Singh J. Effect of preoperative vitamin D levels on functional performance after total knee arthroplasty. Clin Orthop Surg. 2016;8(2):153–156. doi: 10.4055/cios.2016.8.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jansen JA, Haddad FS. High prevalence of vitamin D deficiency in elderly patients with advanced osteoarthritis scheduled for total knee replacement associated with poorer preoperative functional state. Ann R Coll Surg Engl. 2013;95(8):569–572. doi: 10.1308/003588413X13781990150374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jansen J, Tahmassebi J, Haddad FS. Vitamin D deficiency is associated with longer hospital stay and lower functional outcome after total knee arthroplasty. Acta Orthop Belg. 2017;83(4):664–670. [PubMed] [Google Scholar]
- 17.Shin KY, Park KK, Moon SH, Yang IH, Choi HJ, Lee WS. Vitamin D deficiency adversely affects early post-operative functional outcomes after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2017;25(11):3424–3430. doi: 10.1007/s00167-016-4209-8. [DOI] [PubMed] [Google Scholar]
- 18.Zajonz D, Prager F, Edel M, et al. The significance of the vitamin D metabolism in the development of periprosthetic infections after THA and TKA: a prospective matched-pair analysis of 240 patients. Clin Interv Aging. 2018;13:1429–1435. doi: 10.2147/CIA.S171307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maier GS, Horas K, Seeger JB, Roth KE, Kurth AA, Maus U. Is there an association between periprosthetic joint infection and low vitamin D levels? Int Orthop. 2014;38(7):1499–1504. doi: 10.1007/s00264-014-2338-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hegde V, Dworsky EM, Stavrakis AI, et al. Single-dose, preoperative vitamin-D supplementation decreases infection in a mouse model of periprosthetic joint infection. J Bone Joint Surg Am. 2017;99(20):1737–1744. doi: 10.2106/JBJS.16.01598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Alamanda VK, Springer BD. Perioperative and modifiable Risk Factors for Periprosthetic Joint Infections (PJI) and Recommended Guidelines. Curr Rev Musculoskelet Med. 2018;11(3):325–331. doi: 10.1007/s12178-018-9494-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hegde V, Arshi A, Wang C, et al. Preoperative vitamin D deficiency is associated with higher postoperative complication rates in total knee arthroplasty. Orthopedics. 2018;41(4):e489–e495. doi: 10.3928/01477447-20180424-04. [DOI] [PubMed] [Google Scholar]
- 23.Schwartz FH, Lange J. Factors that affect outcome following total joint arthroplasty: a review of the recent literature. Curr Rev Musculoskelet Med. 2017;10(3):346–355. doi: 10.1007/s12178-017-9421-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Traven SA, Chiaramonti AM, Barfield WR, et al. Fewer complications following revision hip and knee arthroplasty in patients with normal vitamin D levels. J Arthroplasty. 2017;32(9S):193–196. doi: 10.1016/j.arth.2017.02.038. [DOI] [PubMed] [Google Scholar]
- 25.Blomberg Jensen M, Husted H, Bjerrum PJ, Juul A, Kehlet H. Compromised activation of vitamin D after elective surgery: a prospective pilot study. JBMR Plus. 2018;2(5):281–288. doi: 10.1002/jbm4.10053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mathias S, Nayak US, Isaacs B. Balance in elderly patients: the “get-up and go” test. Arch Phys Med Rehabil. 1986;67(6):387–389. [PubMed] [Google Scholar]
- 27.Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–148. doi: 10.1111/j.1532-5415.1991.tb01616.x. [DOI] [PubMed] [Google Scholar]
- 28.Cipriani C, Romagnoli E, Scillitani A, et al. Effect of a single oral dose of 600,000 IU of cholecalciferol on serum calciotropic hormones in young subjects with vitamin D deficiency: a prospective intervention study. J Clin Endocrinol Metab. 2010;95(10):4771–4777. doi: 10.1210/jc.2010-0502. [DOI] [PubMed] [Google Scholar]
- 29.Kearns MD, Alvarez JA, Tangpricha V. Large, single-dose, oral vitamin D supplementation in adult populations: a systematic review. Endocr Pract. 2014;20(4):341–351. doi: 10.4158/EP13265.RA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Heaney RP, Armas LA, Shary JR, Bell NH, Binkley N, Hollis BW. 25-Hydroxylation of vitamin D3: relation to circulating vitamin D3 under various input conditions. Am J Clin Nutr. 2008;87(6):1738–1742. doi: 10.1093/ajcn/87.6.1738. [DOI] [PubMed] [Google Scholar]
- 31.Diamond TH, Ho KW, Rohl PG, Meerkin M. Annual intramuscular injection of a megadose of cholecalciferol for treatment of vitamin D deficiency: efficacy and safety data. Med J Aust. 2005;183(1):10–12. doi: 10.5694/j.1326-5377.2005.tb06879.x. [DOI] [PubMed] [Google Scholar]
- 32.Nugent C, Roche K, Wilson S, et al. The effect of intramuscular vitamin D (cholecalciferol) on serum 25OH vitamin D levels in older female acute hospital admissions. Ir J Med Sci. 2010;179(1):57–61. doi: 10.1007/s11845-009-0410-9. [DOI] [PubMed] [Google Scholar]