Abstract
Backgroud
Slipped capital femoral epiphysis (SCFE) is a severe and catastrophic disorder that affects the hips of adolescents. Many reports about surgical procedures to treat this condition have been published, but to our knowledge, there are no published results of treatment in Latin American patients. This study describes the clinical and radiological results of the modified Dunn procedure with the surgical approach described by Ganz to treat mild to severe SCFE in a cohort of Colombian pediatric patients.
Methods
We retrospectively analyzed 21 patients (22 hips) with SCFE treated with surgical dislocation of the hip from 2005 to 2017. The same pediatric orthopedic surgeon performed all operations. Clinical outcome was assessed using the range of movement and Merle d'Aubigné score, while radiological measurements and assessment included the slip angle and Tönnis score.
Results
The average duration of follow-up was 29 months (range, 12–72 months). Of all cases, 17 presented with acute-on-chronic symptoms. Preoperatively, all 22 hips were classified as poor according to the Merle d'Aubigné score. Preoperative radiological classification showed compromise grade II or III in 20 hips. Last follow-up Merle d'Aubigné score rated 17 cases as good or excellent (p < 0.05). The postoperative radiological classification was grade I or II in all 22 cases, and the Tönnis score was stage II in 3 cases and stage III in 4 cases.
Conclusions
Our results suggest that the modified Dunn osteotomy performed through the Ganz technique could be safely and effectively used to treat patients with mild to severe SCFE.
Keywords: Slipped capital femoral epiphysis, Surgical dislocation, Femur head necrosis
Slipped capital femoral epiphysis (SCFE) is one of the most common disorders that affect the hips of adolescents. In the United States, this condition affects adolescents with an incidence of 10 per 100,000.1,2) Frequently, SCFE initially presents with pain in the hip, thigh, or knee and abnormal gait; when the pain is referred to the knee, there may be a delay in the diagnosis.1,2) Diagnosis and management should be timely since in many long-term studies, the association between SCFE deformity and the development of early osteoarthrosis of the hip has been demonstrated.3)
The goal of treatment for SCFE is to prevent the progression of the deformity through stabilization of the proximal epiphyses.4,5,6) Current advances in the surgical treatment of severe and unstable SCFE are aimed at preventing the progression or correcting the proximal deformity by protecting the blood supply of the femoral head.5) Multiple surgical techniques have been described, including in situ fixation, closed reduction with fixation, reduction by an anterior approach, and controlled open surgical dislocation of the hip, but no consensus has been reached on the selection of the treatment method; therefore, the treatment of this condition is still a challenge.4,5,7)
Controlled surgical dislocation, as first described by Ganz et al.,8) is an effective method for the correction of deformity with low avascular necrosis (AVN) rates.4,6,8,9) However, in Latin America, there is a lack of literature from studies aimed at determining the long-term radiological and functional results of this surgical technique as a treatment for SCFE. This study aimed to describe the results of controlled surgical hip dislocation and the complications that may arise with the application of this technique in a series of Colombian patients.
METHODS
Patients
A retrospective review was performed on consecutive pediatric patients who underwent surgical treatment with the technique of controlled dislocation for SCFE from 2005 to 2017 in our center. The ethics committee of our institution approved the study (IRB No. 55-2017). Details regarding demographic characteristics, operative notes, and patient follow-up data were compiled from the medical records, with the prior consent and assent of the parents and patients, respectively. Exclusion criteria for this procedure included patients with closed proximal femoral physis, a mild slip (defined as one with < 30° of lateral slip); clinical or radiological evidence of moderate or severe cartilage damage; and preexisting AVN.
Clinical examination revealed abnormal gait or inability to walk, in addition to painful mobility of the hip for acute and acute-on-chronic cases, with external rotation of the limb and limitation of flexion, internal rotation, and abduction. Slipping symptoms were categorized according to the clinical classification of O'Brien and Fahey10) into acute, chronic, or acute-on-chronic. The cases were also classified as stable or unstable based on Loder's criteria.11) Preoperative and postoperative evaluation included measurements of the range of preoperative and postoperative movement, pain, and ambulation, evaluated through the Merle d'Aubigné score. Based on the score, patients were further classified into poor (score < 13), fair (score 13 or 14), good (score 15 to 17), and excellent (score of 18).12,13)
The slipped angle was measured before and after surgery on anteroposterior hip radiographs and frog projection (Figs. 1 and 2). Radiological severity was categorized considering the angles and relative displacement of the epiphysis in the metaphysis according to Wilson's classification14) into grade I (< 25%), grade II (25%–50%), and grade III (> 50%).
Fig. 1. Acute slipped capital femoral epiphysis (SCFE). (A) A radiograph of a 13-year-old patient with acute and severe SCFE. Three-year postoperative anteroposterior (B) and frog projection (C) radiographs, showing satisfactory reduction of the femoral epiphysis with no signs of avascular necrosis.
Fig. 2. Right acute-on-chronic and left chronic slipped capital femoral epiphysis (SCFE). (A) A radiograph showing a bilateral compromise in a 16-year-old patient with severe acute-on-chronic SCFE of the right hip and mild chronic SCFE of the left hip. The patient had a preexisting condition of falciform anemia. In the right hip, the Dunn modified procedure was performed, while in situ fixation was done to the left hip. Six-year postoperative anteroposterior (B) and frog projection (C) radiographs, showing satisfactory reduction with no impingement at the right hip and mild cam of the left hip. No signs of avascular necrosis was present in any of the hips.
Surgical Procedure
The same senior pediatric orthopedic surgeon (CS) performed all operations. The modified Dunn procedure is a surgical technique for SCFE correction previously described by Ganz et al.8)
Concisely, the patient is positioned in lateral decubitus to perform surgical dislocation of the hip with an osteotomy of the greater trochanter. The incision in the skin is lateral and centered on the greater trochanter, following the axis of the femur. A slide trochanteric osteotomy is then performed. Blood supply to the femoral head is preserved through an extended retinacular soft-tissue flap. The gluteus minimus is mobilized through the gap with the pyriformis tendon to reach the capsule. Then, a capsulotomy in Z shape along the acetabular insertion is made.
After the hip has been exposed, the magnitude and direction of the slip are identified. Subsequently, a provisional in situ fixation is performed in unstable acute cases with two 1.5-mm smooth pins; thus, mobilization of the femur and dislocation of the hip can be done without risk of damaging the epiphyseal circulation. At this time, the hip is dislocated, and the pins are removed. When the SCFE is chronic, the hip is easily dislocated without the need of protecting pins.
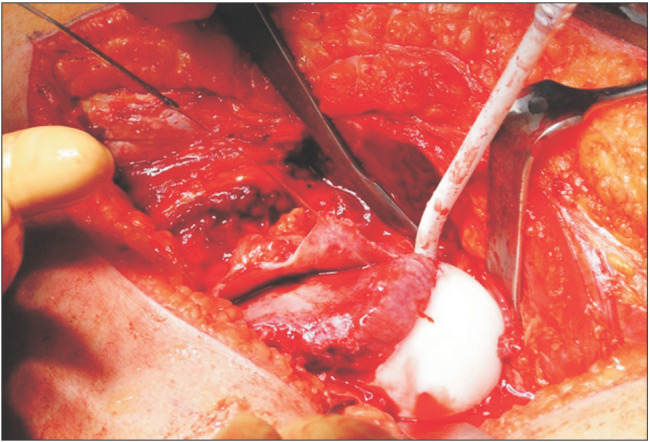
Full exposure of the femoral neck was first achieved through complete separation of the capital epiphysis from the femoral neck (Fig. 3), which allows visualization of callus formation on the posteroinferior aspect of the neck, which is then entirely removed with a curette. The remaining physis of the femoral head is excised, while manually keeping the femoral head in a stable position.
Fig. 3. Open exposure. A photograph showing the anterior capsulotomy and the longitudinally opened retinaculum that exposes the femoral head and neck.
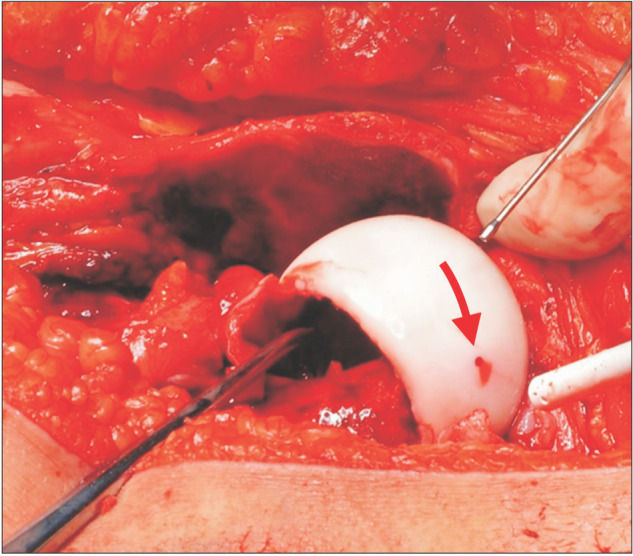
The femoral head is reduced onto the neck and then stabilized by inserting a threaded nail through the fovea capitis in an anterograde manner (Fig. 4). To further stabilize the femoral head, under fluoroscopic guidance, a second threaded nail is placed from distal to proximal in a retrograde manner towards the physis (Fig. 5). Before any manipulation, a 2-mm drill hole is made on the epiphysis to visualize bleeding that indicates the viability of the hip after reduction of the epiphysis (Fig. 6).
Fig. 4. Fixation through fovea. A photograph showing fixation of the femoral epiphysis with antegrade passage of a 3.5-mm fully threaded wire.
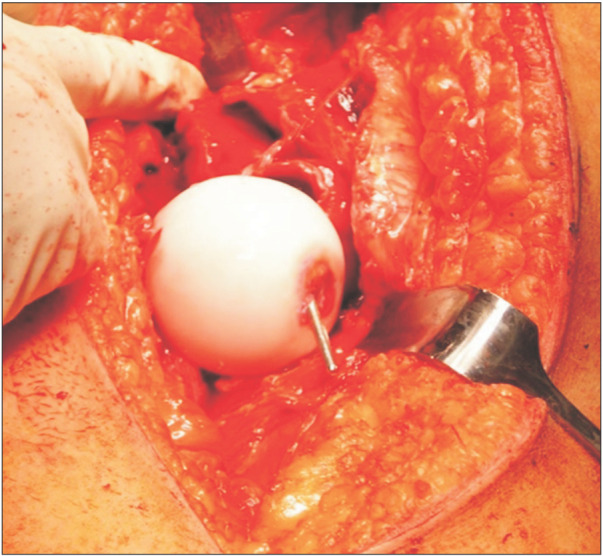
Fig. 5. Retrograde fixation. A photograph showing retrograde fixation from the lateral cortex to the subchondral femoral epiphysis with a 3.5-mm fully threaded wire.
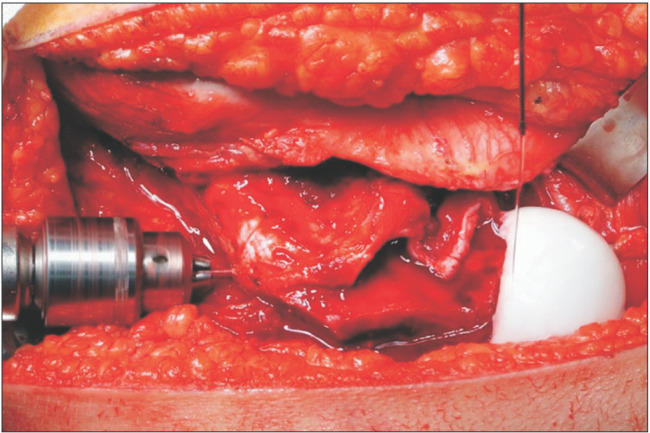
Fig. 6. Perfusion verification. A photograph showing good and permanent perfusion of the epiphysis during the whole procedure, verified through a 2-mm perforation. Arrow: point at the perforation.
The condition of the acetabular labrum and the articular cartilage is evaluated in all hips. The hip is reduced, then a capsulorrhaphy is performed, and the greater trochanter is repositioned and fixed with three 3.5-mm cortical screws.
Evaluation and Postoperative Follow-up
The patients were monitored periodically. Hip radiographs were used to measure the slip percentage and the Tönnis score.15) Measurements of the Merle d'Aubigné score were taken during follow-up. The number of patients to whom prophylactic fixation of the contralateral hip was performed was also recorded.
Statistical Analysis
The values of the radiographic measurements and the scores of the different scales were expressed as means and standard deviations. The changes between the preoperative values and those of the last follow-up were determined with the Student t-test. Values of p < 0.05 were considered significant.
RESULTS
In total, 22 hips (10 right and 12 left) were retrospectively reviewed in 21 patients (5 women and 16 men). The average follow-up was 28.9 months (range, 12–72 months). The age of the patients ranged from 10 to 18 years, with an average of 13.5 years at the time of surgery. Figs. 1 and 2 present the cases of 2 patients: 13 and 16 years of age with follow-up of 3 years and 6 years, respectively.
All patients presented with pain as an initial symptom, accompanied by abnormal gait. Concerning the presentation of symptoms, there were 2 patients with acute SCFE, 3 patients with chronic SCFE, and 17 acute-on-chronic cases. The average time during which the symptoms were present before the consultation was 5 weeks. Four patients required hospitalization for soft traction use before surgery.
The preoperative clinical classification according to the Merle d'Aubigné score was poor in all 22 hips (median, 10; range, 5–12). The preoperative radiological classification showed compromise grade II and III in 8 hips and 12 hips, respectively (Table 1). In the immediate postoperative evaluation, only 1 patient presented with a complication in the form of dehiscence of the surgical wound. No acute postoperative cases of instability were detected in the immediate radiological evaluation.
Table 1. Patients Demographics, Preoperative and Postoperative Clinical Classifications and Scores.
| Case | Sex | Age (yr) | Preoperative | Postoperative | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Fahey and O'Brien classification | Loder classifcation | Wilson's classification | Merle d'Aubigné score | Wilson's classification | Merle d'Aubigné score | Tönnis score | Complication | |||
| 1 | Male | 13 | Acute-on-chronic | Unstable | Grade III > 50% | 11 | Grade I < 25% | 10 | Stage II | Chondrolysis |
| 2 | Male | 18 | Acute-on-chronic | Unstable | Grade II 25%–50% | 9 | Grade II 25%–50% | 16 | Stage 0 | |
| 3 | Male | 14 | Acute-on-chronic | Unstable | Grade III > 50% | 11 | Grade I < 25% | 10 | Stage II | Chondrolysis/AVN |
| 4 | Male | 13 | Chronic | Stable | Grade II 25%–50% | 11 | Grade I < 25% | 17 | Stage 0 | |
| 5 | Male | 15 | Acute | Unstable | Grade II 25%–50% | 7 | Grade II 25%–50% | 15 | Stage 0 | |
| 6 | Male | 15 | Acute-on-chronic | Unstable | Grade II 25%–50% | 7 | Grade I < 25% | 18 | Stage 0 | |
| 7 | Male | 16 | Chronic | Stable | Grade III > 50% | 12 | Grade I < 25% | 16 | Stage 0 | |
| 8 | Male | 16 | Acute-on-chronic | Stable | Grade I < 25% | 10 | Grade I < 25% | 17 | Stage 0 | |
| 9 | Male | 15 | Chronic | Stable | Grade III > 50% | 10 | Grade I < 25% | 13 | Stage II | Chondrolysis |
| 10 | Male | 11 | Acute | Unstable | Grade III > 50% | 11 | Grade I < 25% | 17 | Stage 0 | |
| 11 | Female | 10 | Acute-on-chronic | Stable | Grade II 25%–50% | 11 | Grade II 25%–50% | 15 | Stage 0 | |
| 12 | Male | 17 | Acute-on-chronic | Stable | Grade III > 50% | 9 | Grade I < 25% | 18 | Stage 0 | |
| 13 | Male | 17 | Acute-on-chronic | Unstable | Grade II 25%–50% | 5 | Grade I < 25% | 10 | Stage III | AVN |
| 14 | Female | 12 | Acute-on-chronic | Stable | Grade III > 50% | 9 | Grade I < 25% | 15 | Stage 0 | |
| 15 | Female | 10 | Acute-on-chronic | Stable | Grade III > 50% | 7 | Grade I < 25% | 15 | Stage 0 | |
| 16 | Male | 15 | Acute-on-chronic | Stable | Grade III > 50% | 10 | Grade II 25%–50% | 15 | Stage I | Mild re-slipping |
| 17 | Female | 11 | Acute-on-chronic | Stable | Grade I < 25% | 10 | Grade I < 25% | 17 | Stage 0 | |
| 18 | Male | 13 | Acute-on-chronic | Stable | Grade III > 50% | 10 | Grade I < 25% | 18 | Stage 0 | |
| 19 | Male | 11 | Acute-on-chronic | Stable | Grade III > 50% | 7 | Grade I < 25% | 18 | Stage 0 | |
| 20 | Male | 12 | Acute-on-chronic | Unstable | Grade III > 50% | 10 | Grade I < 25% | 18 | Stage 0 | |
| 21 | Male | 13 | Acute-on-chronic | Stable | Grade II 25%–50% | 9 | Grade II 25%–50% | 14 | Stage 0 | Mild re-slipping |
| 22 | Female | 11 | Acute-on-chronic | Stable | Grade II 25%–50% | 10 | Grade I < 25% | 18 | Stage 0 | |
AVN: avascular necrosis.
At the last follow-up, 12 patients presented with no pain; 3 presented with mild pain with regular activity; 2 presented with mild pain with activity that improved by resting; and 4 showed limited movement due to pain. In the last evaluation, the clinical classification according to the Merle d'Aubigné score was good and excellent in 11 hips and 6 hips, respectively, with a median of 16 for total cases. The postoperative radiological classification was grade I and II in 17 cases and 5 cases, respectively (Table 1).
Postoperative Tönnis score showed stage II in 3 cases and stage III in 1 case (Table 1). As complications, 2 patients had re-slipping, 2 AVN, and 3 chondrolysis. Prophylactic fixation of the contralateral hip was performed in 5 patients.
DISCUSSION
Surgical hip dislocation (modified Dunn procedure) in pediatric patients with SCFE in this Colombian cohort showed very satisfactory results regarding functional recovery and radiological stabilization with a low rate of complications. Mid- and long-term results indicate that this surgical technique allows patients to recover the range of movement and ambulation with no or little pain. Furthermore, we showed that timely intervention with the modified Dunn procedure could lower the incidence of catastrophic complications such as AVN and chondrolysis.
To the best of our knowledge, this is the first report of a series of patients from Latin America. Our country may have similar epidemiology of SCFE compared with other countries of the region. Thus, this significant cohort is a representative sample of SCFE patients with results that may apply to the Latin American population. The results of this study contribute to the existing literature, suggesting that the modified Dunn procedure is a safe and effective procedure for the treatment of moderate and severe SCFE.
The size of our sample is comparable to other reported series such as the one from Slongo et al.6) in 2010 (n = 23), Massè et al.16) in 2012 (n = 20), Sankar et al.17) in 2013 (n = 27), Madan et al.18) in 2013 (n = 28), Ziebarth et al.19) in 2017 (n = 43), and Elmarghany et al.20) in 2017 (n = 30). SCFE treatment aims to prevent early hip osteoarthritis caused by femoroacetabular impingement with an anterior cam effect. Anatomical restoration of the femoral head and acetabulum close to normality avoids the early signs of osteoarthritis.2,3,5)
The modified Dunn procedure using Ganz et al.8) surgical hip dislocation is ideal for providing physeal stability, allowing anatomical restoration of the proximal femur, to preserve the blood supply to the epiphysis and to avoid residual deformity with minimal shortening. It also has the advantage of allowing intra-articular exploration to identify any additional chondral pathology and removing the metaphyseal callus while minimizing the risk of AVN.8,21) Even though this surgical technique is recommended for acute and acute-on-chronic SCFE, it should be used carefully in patients with chronic SCFE and only by experienced surgeons.
There is still significant controversy about the treatment of unstable or severe SCFE with the modified Dunn procedure due to the high variability in the long-term results described in several publications.5,7,22) Most of the variability has been accounted for by the experience of the different surgical teams and the severity of the condition of each of the reported series. In the current study, we presented intermediate and long-term results of the surgical hip dislocation performed by one experienced surgeon in patients with mild to severe SCFE. The surgical technique was executed following the procedure, as described by Ganz et al.8) and Slongo et al.,6) showing satisfactory functional results in challenging cases. The majority of our patients were acute and acute-on-chronic patients with radiological moderate to severe SCFE, which required anatomical reduction and stabilization and thus minimized AVN.
The incidence of AVN is considered one of the indicators of success or failure of the modified Dunn procedure with overall rates ranging from 2% to 30%.4,9,17,18,19,23,24) However, AVN incidences higher than 20% with the surgical hip dislocation are comparable to those of closed reduction and internal fixation for severe SCFE,4,9,22,23,24) while the reported incidences for mild or stable SCFE after the surgical hip dislocation range from 0% to 10%.5,7,23,24) It has been argued that the variability of the AVN rates could be due to the intervention of acute versus chronic patients.5) In our series, the 2 cases of AVN were found in patients with SCFE of acute onset.
Contralateral hip involvement in unilateral SCFE has been reported in 14%–63% of the cases.25,26,27,28) Prophylactic fixation of the unaffected hip has been shown to reduce the risk of a contralateral slip, with minimal risk of complications that include fracture, adverse reaction to osteosynthesis material, and chondrolysis among others. The contralateral hip prophylactic fixation is better suited for patients of younger age at presentation, with severe slip, obesity, or metabolic condition, and those in which long-term follow-up may be difficult.27,28) In our cohort, prophylactic fixation of the unaffected hip was performed in 5 patients indicated mainly by the severity of the slip and the sociodemographic conditions, which made almost impossible the follow-up.
This study is not without limitations, which include the retrospective design, limited information for the periodic follow-ups, shortage of preoperative clinical scores, and lack of a control group. Nevertheless, it is worthy of notice that the surgical hip dislocation can give the same favorable outcomes in Latin American patients with mild to severe SCFE as in patients from other regions and ethnicities in previously published reports.
In agreement with what has been previously demonstrated in several publications, we showed that surgical dislocation of the hip could be used successfully to treat pediatric patients with moderate to severe SCFE. The incidence of complications in our cohort was low despite the severity of the condition at the time of the intervention. To our knowledge, this is the first report of the results of the modified Dunn procedure in a Colombian and Latin American cohort, which underscores the importance and novelty of this work given the comparable sample size with that of other previous reports.
ACKNOWLEDGEMENTS
The authors wish to thank Dr. David Suarez (Clínica del Campestre) for his contribution to data acquisition.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Loder RT, Skopelja EN. The epidemiology and demographics of slipped capital femoral epiphysis. ISRN Orthop. 2011;2011:486512. doi: 10.5402/2011/486512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gholve PA, Cameron DB, Millis MB. Slipped capital femoral epiphysis update. Curr Opin Pediatr. 2009;21(1):39–45. doi: 10.1097/MOP.0b013e328320acea. [DOI] [PubMed] [Google Scholar]
- 3.Carney BT, Weinstein SL. Natural history of untreated chronic slipped capital femoral epiphysis. Clin Orthop Relat Res. 1996;(322):43–47. [PubMed] [Google Scholar]
- 4.Abu Amara S, Cunin V, Ilharreborde B French Society of Pediatric Orthopaedics (SOFOP) Severe slipped capital femoral epiphysis: a French multicenter study of 186 cases performed by the SoFOP. Orthop Traumatol Surg Res. 2015;101(6 Suppl):S275–S279. doi: 10.1016/j.otsr.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 5.Bittersohl B, Hosalkar HS, Zilkens C, Krauspe R. Current concepts in management of slipped capital femoral epiphysis. Hip Int. 2015;25(2):104–114. doi: 10.5301/hipint.5000189. [DOI] [PubMed] [Google Scholar]
- 6.Slongo T, Kakaty D, Krause F, Ziebarth K. Treatment of slipped capital femoral epiphysis with a modified Dunn procedure. J Bone Joint Surg Am. 2010;92(18):2898–2908. doi: 10.2106/JBJS.I.01385. [DOI] [PubMed] [Google Scholar]
- 7.Mahran MA, Baraka MM, Hefny HM. Slipped capital femoral epiphysis: a review of management in the hip impingement era. SICOT J. 2017;3:35. doi: 10.1051/sicotj/2017018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83(8):1119–1124. doi: 10.1302/0301-620x.83b8.11964. [DOI] [PubMed] [Google Scholar]
- 9.Sucato DJ, De La Rocha A. High-grade SCFE: the role of surgical hip dislocation and reduction. J Pediatr Orthop. 2014;34 Suppl 1:S18–S24. doi: 10.1097/BPO.0000000000000297. [DOI] [PubMed] [Google Scholar]
- 10.O'Brien ET, Fahey JJ. Remodeling of the femoral neck after in situ pinning for slipped capital femoral epiphysis. J Bone Joint Surg Am. 1977;59(1):62–68. [PubMed] [Google Scholar]
- 11.Loder RT, Richards BS, Shapiro PS, Reznick LR, Aronson DD. Acute slipped capital femoral epiphysis: the importance of physeal stability. J Bone Joint Surg Am. 1993;75(8):1134–1140. doi: 10.2106/00004623-199308000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Banaszkiewicz PA. Functional results of hip arthroplasty with acrylic prosthesis. In: Banaszkiewicz P, Kader D, editors. Classic papers in orthopaedics. London: Springer; 2014. pp. 19–22. [Google Scholar]
- 13.d'Aubigne RM, Postel M. The classic: functional results of hip arthroplasty with acrylic prosthesis: 1954. Clin Orthop Relat Res. 2009;467(1):7–27. doi: 10.1007/s11999-008-0572-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilson PD. The treatment of slipping of the upper femoral epiphysis with minimal dislacement. J Bone Jt Surg Am. 1938;20(2):379–399. [Google Scholar]
- 15.Tonnis D, Heinecke A, Nienhaus R, Thiele J. Predetermination of arthrosis, pain and limitation of movement in congenital hip dysplasia (author's transl) Z Orthop Ihre Grenzgeb. 1979;117(5):808–815. [PubMed] [Google Scholar]
- 16.Masse A, Aprato A, Grappiolo G, Turchetto L, Campacci A, Ganz R. Surgical hip dislocation for anatomic reorientation of slipped capital femoral epiphysis: preliminary results. Hip Int. 2012;22(2):137–144. doi: 10.5301/HIP.2012.9208. [DOI] [PubMed] [Google Scholar]
- 17.Sankar WN, Vanderhave KL, Matheney T, Herrera-Soto JA, Karlen JW. The modified Dunn procedure for unstable slipped capital femoral epiphysis: a multicenter perspective. J Bone Joint Surg Am. 2013;95(7):585–591. doi: 10.2106/JBJS.L.00203. [DOI] [PubMed] [Google Scholar]
- 18.Madan SS, Cooper AP, Davies AG, Fernandes JA. The treatment of severe slipped capital femoral epiphysis via the Ganz surgical dislocation and anatomical reduction: a prospective study. Bone Joint J. 2013;95(3):424–429. doi: 10.1302/0301-620X.95B3.30113. [DOI] [PubMed] [Google Scholar]
- 19.Ziebarth K, Milosevic M, Lerch TD, Steppacher SD, Slongo T, Siebenrock KA. High survivorship and little osteoarthritis at 10-year followup in SCFE patients treated with a modified dunn procedure. Clin Orthop Relat Res. 2017;475(4):1212–1228. doi: 10.1007/s11999-017-5252-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elmarghany M, Abd El-Ghaffar TM, Seddik M, et al. Surgical hip dislocation in treatment of slipped capital femoral epiphysis. SICOT J. 2017;3:10. doi: 10.1051/sicotj/2016047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leunig M, Slongo T, Ganz R. Subcapital realignment in slipped capital femoral epiphysis: surgical hip dislocation and trimming of the stable trochanter to protect the perfusion of the epiphysis. Instr Course Lect. 2008;57:499–507. [PubMed] [Google Scholar]
- 22.Zaltz I, Baca G, Clohisy JC. Unstable SCFE: review of treatment modalities and prevalence of osteonecrosis. Clin Orthop Relat Res. 2013;471(7):2192–2198. doi: 10.1007/s11999-012-2765-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sucato DJ. Approach to the hip for SCFE: the North American perspective. J Pediatr Orthop. 2018;38 Suppl 1:S5–S12. doi: 10.1097/BPO.0000000000001183. [DOI] [PubMed] [Google Scholar]
- 24.Loder RT, Dietz FR. What is the best evidence for the treatment of slipped capital femoral epiphysis? J Pediatr Orthop. 2012;32 Suppl 2:S158–S165. doi: 10.1097/BPO.0b013e318259f2d1. [DOI] [PubMed] [Google Scholar]
- 25.Bhattacharjee A, Freeman R, Roberts AP, Kiely NT. Outcome of the unaffected contralateral hip in unilateral slipped capital femoral epiphysis: a report comparing prophylactic fixation with observation. J Pediatr Orthop B. 2016;25(5):454–458. doi: 10.1097/BPB.0000000000000337. [DOI] [PubMed] [Google Scholar]
- 26.Koenig KM, Thomson JD, Anderson KL, Carney BT. Does skeletal maturity predict sequential contralateral involvement after fixation of slipped capital femoral epiphysis? J Pediatr Orthop. 2007;27:796–800. doi: 10.1097/BPO.0b013e3181558bd9. [DOI] [PubMed] [Google Scholar]
- 27.Kocher MS, Bishop JA, Hresko MT, Millis MB, Kim YJ, Kasser JR. Prophylactic pinning of the contralateral hip after unilateral slipped capital femoral epiphysis. J Bone Joint Surg Am. 2004;86(12):2658–2665. doi: 10.2106/00004623-200412000-00011. [DOI] [PubMed] [Google Scholar]
- 28.Stasikelis PJ, Sullivan CM, Phillips WA, Polard JA. Slipped capital femoral epiphysis: prediction of contralateral involvement. J Bone Joint Surg Am. 1996;78(8):1149–1155. doi: 10.2106/00004623-199608000-00004. [DOI] [PubMed] [Google Scholar]




