Abstract
Backgroud
Femoral internal rotation in total knee arthroplasty (TKA) is well known as one of the main causes of patellar maltracking. Although femoral internal rotation in TKA is considered unacceptable due to the risk of patellar maltracking, it is sometimes required for ligament balancing. We evaluated the influence of femoral internal rotation on patellar tracking in TKA performed using the gap technique.
Methods
From April 2008 to May 2018, 1,612 cases of TKA were done. Among them, 245 cases of TKA for osteoarthritis were followed up for at least 1 year and included in this study. We compared patellar tracking in two groups; group I consisted of 99 cases whose femoral rotation was less than 0° and group II consisted of 146 cases whose femoral rotation was 3°–5° external rotation. Preoperative femoral rotation was measured with the condylar twist angle (CTA) by using computed tomography. The patella was replaced in all cases. Patellar tracking was evaluated with patellar tilt angle (lateral tilt [+] and medial tilt [−]) in the merchant radiograph. Statistical analysis was done using Mann-Whitney U-test. Clinical assessment was performed using the Knee Society clinical rating system.
Results
The preoperative CTA was 5.3° ± 1.6° in group I and 5.4° ± 1.6° in group II, showing no statistically significant difference between groups (p = 0.455). Intraoperative femoral rotation was −0.5° ± 0.8° in group I and 3.9° ± 0.8° in group II when the gap technique was used (p < 0.001). The postoperative patellar tilt angle was −0.4° ± 3.6° in group I and 0.1° ± 4.1° in group II with no statistically significant difference (p = 0.251).
Conclusions
Compared with femoral external rotation, femoral internal rotation with ligament balance in TKA was not more associated with patellar maltracking. Therefore, patellar tracking might be related with ligament balance in flexion regardless of the anatomic femoral rotational alignment.
Keywords: Patellar tracking, Femoral internal rotation, Gap technique, Total knee arthroplasty
Despite the advancement in total knee arthroplasty (TKA), complications related with the patella still account for up to 10% of all postoperative complications.1) Patellar maltracking is representative and has clinical symptoms such as anterior knee pain, instability, and crepitus.2,3)
Patellar tracking after TKA is affected by not only the patient factors such as the preoperative patellar alignment and obesity, but also the surgical factors such as femoral and tibial rotational alignment and position of the components. Of these, the femoral rotational alignment is regarded as a main factor that affects postoperative patellar maltracking, which was the main cause of revision TKA in the past, and external femoral rotation is considered effective in decreasing the risk of patellar maltracking.4,5) Newbern et al.6) compared patellar tracking with the transepicondylar axis to the posterior condylar axis for femoral rotational alignment in 2,381 TKAs. They found 4.6 times increment of lateral retinacular release in the cases with the posterior condylar axis and thus recommended routine use of the transepicondylar axis for determining femoral component rotation in TKA.
However, femoral rotational alignment influences not only patellar tracking but also the ligament and gap balance in flexion, all of which should be taken into consideration in determining the femoral rotational alignment. Two main methods are used to determine femoral rotational alignment: (1) the measured resection technique based on the anatomic femoral rotational axes, transepicondylar axis, whiteside anteroposterior axis, and 3° external rotation from the posterior condylar axis and (2) the gap technique based on the ligament balancing axis.7) The most ideal form is when the same external femoral rotation can be achieved in the two methods. But, the acquisition of external femoral rotation presents some limitations. For instance, in case of ligament imbalance with a widened medial gap in flexion, external femoral rotation leads to ligament imbalance inevitably. By contrast, the gap technique, which facilitates internal femoral rotation regardless of anatomic femoral rotational axes, can correct the ligament imbalance; however, external femoral rotation is recommended over internal femoral rotation for normal patellar tracking.
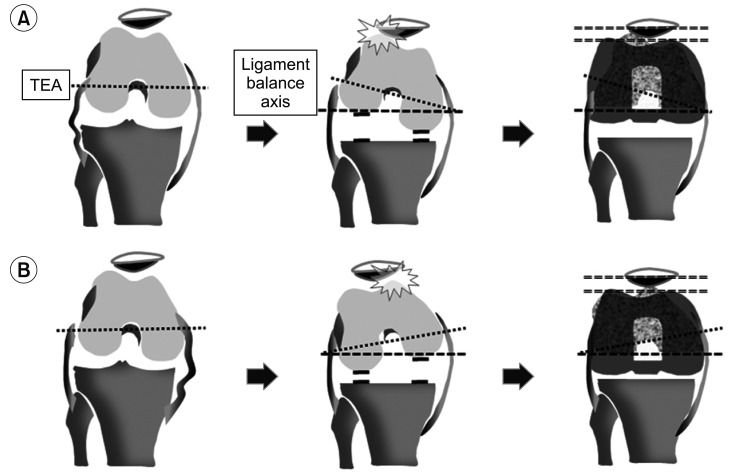
The authors assumed that if the ligament is properly balanced with the gap technique, internal femoral rotation would have no effect in patellar maltracking. We postulated that if the femoral component is positioned with ligament balance in 90° flexion regardless of the anatomic femoral axis, the trochlear groove of the femoral component would stay in the right position relative to the patella, eventually leading to an appropriate alignment of the patella (Fig. 1). We investigated the influence of femoral rotation on patella tracking by comparing internal and external femoral rotation in TKA.
Fig. 1. Relationship between femoral and patellar components in ligament balance using the gap technique. (A) In case of lateral laxity, more external femoral rotation for ligament balance with the gap technique may show appropriate patellar tracking with the femoral component. (B) In case of medial laxity, internal femoral rotation may show good ligament balance and patellar tracking. TEA: transepicondylar axis.
METHODS
Owing to the retrospective design, the requirement for informed consent was waived. This study was approved by the Institutional Review Board of Seoul Sacred Heart hospital (IRB No. P01-202009-21-008). A total of 1,612 TKAs, which were performed by a single surgeon (DOK) from April 2008 through May 2018, were retrospectively reviewed. The inclusion criteria were patients with primary osteoarthritis. Patients with rheumatoid arthritis or secondary osteoarthritis such as posttraumatic arthritis and sequelae of septic arthritis were excluded. TKAs were sorted according to the intraoperative femoral rotational alignment angle to evaluate its effect on patellar tracking. Among them, we included 1,250 TKAs whose femoral rotation was less than 0° or 3°–5° external rotation. Finally, we performed retrospective research with 245 examples: group I (n = 99) with femoral rotation less than 0° and group II (n = 146) with 3°–5° external rotation, chosen by simple random sampling among 1,141 cases. Of these, 228 were women and 17 were men with an average age of 67.3 years. The minimum follow-up period was 1 year. Preoperative range of motion was 4.3° (± 5.8°) in flexion contracture and 131.8° (± 18.4°) in further flexion. Preoperative patellar alignment was evaluated in Merchant view X-ray. Preoperative patellar tilt angle was defined as the angle subtended by the equatorial line of the patella and the line connecting anterior limits of femoral condyles, which was 9.1° (± 4.5°) in group I and 9.5° (± 5.2°) in group II. Preoperative patellar transition was measured as the distance between the line drawn parallel to tibial axis crossing the deepest part of the groove and the midline of the patella, which was 7.2 mm (± 0.7) in group I and 6.8 mm (± 1.1) in group II. The operation was conducted with the extension gap technique, using the ligament balancing axis for femoral rotational alignment. All cases were computed tomography (CT) scanned before the operation to compare the anatomical femoral rotational alignment axis to the ligament balancing axis, and we compared the effect of patellar alignment according to the intraoperative femoral rotational alignment angle.
We used Nexgen LPS-flex (154 examples; Zimmer Inc, Warsaw, IN, USA), Vanguard (53 examples; Zimmer biomet, Warsaw, IN, USA), and Attune (38 examples; DePuy Synthes, Warsaw, IN, USA) for posterior-stabilized TKA. Preoperative patient age, body mass index (BMI), range of motion, deformation of the coronal plane, and patellar alignment showed no difference between two groups (Table 1). Preoperative data were collected and regular follow-up was performed to assess clinical outcome. On the clinical assessment, knee joint pain and range of motion were all assessed and the knee score was calculated using the Knee Society clinical rating system.8)
Table 1. Demographics.
| Parameter | Group I (≤ 0° FRA) | Group II (3°–5° FRA) |
|---|---|---|
| Mean age (yr) | 66.4 ± 4.8 | 67.8 ± 5.3 |
| Male : female | 8 : 91 | 9 : 137 |
| Body mass index (kg/m2) | 25.6 ± 3.6 | 26.4 ± 4.5 |
| Range of motion (°) | 130.2 ± 0.6 | 129.7 ± 0.4 |
| Coronal axis (°) | –12.2 ± 5.7 | –11.6 ± 5.8 |
| Implant type (Nexgen : Vanguard : Attune) | 66 : 23 : 10 | 88 : 30 : 28 |
| Preoperative patellar tilt (°) | 4.1 ± 3.2 | 3.7 ± 3.1 |
| Preoperative CTA (°) | 5.3 ± 1.6 | 5.4 ± 1.6 |
Values are presented as mean±standard deviation.p > 0.05.
FRA: femoral rotation angle, CTA: condylar twist angle.
Surgical Technique
The surgery was performed using the extension gap balancing technique. After resection of the distal femur and the proximal tibia with reference to the mechanical axis, ligament balance and extension gap were achieved using spacer blocks in knee extension. To address ligament imbalance in varus knees, osteophyte removal, deep medial collateral ligament (MCL) release, posterior oblique ligament release, and reduction osteotomy were conducted in sequence as the medial soft-tissue release; for severe ligament imbalance, additional medial femoral resection or the pie-crusting technique to release the superficial MCL was conducted. In valgus knees, we preserved the medial soft tissue during bone resection. It was extended with the strained lateral soft tissue by using the pie-crusting technique, or additional resection was performed in the lateral distal femur to ensure ligament balance. With the knee in 90° flexion, the ligament balancing axis was used to determine the femoral rotational alignment, the medial and lateral joint tissues were strained using a ligament tensor.9) Next, anteroposterior resection of the femur was performed and the femoral rotational alignment angle was measured as the difference of the resected medial and lateral posterior femoral condyles.10) The patella was replaced in all cases, and lateral patellar peeling and partial facetectomy were done. No thumb test was used for the patellar tracking inspection.
Evaluation Methods
In order to assess the difference between the anatomical femoral rotational alignment axis and the ligament balance axis, preoperative femoral rotation was measured with the condylar twist angle (CTA) between the clinical transepicondylar axis and the posterior condylar axis using CT. Intraoperative femoral rotation was decided by using the ligament balance axis, and we considered the difference of 1 mm as 1° after measuring the thickness of the resected medial and lateral posterior femoral condyles. We evaluated the patellar alignment by measuring the patellar alignment angle (patellar tilt angle: lateral tilt [+] and medial tilt [−]) and patellar translation in the radiological merchant view taken 1 year after the operation. On the evaluation of the patellar alignment, a patellar alignment angle of less than ± 5° was considered as acceptable and more than ± 5° as tilt; a transposition of less than ± 5 mm was considered as acceptable and more than ± 5 mm as deviant.11)
IBM SPSS ver. 24.0 (IBM Corp., Armonk, NY, USA) was used for statistical analysis and the patellar alignment angles and transpositions were compared between the two groups using the Mann-Whitney U-test. A p-value less than 0.05 was defined as statistically significant.
RESULTS
The preoperative CTA showed no statistically significant differences between group I and group II (5.3° ± 1.6° and 5.4° ± 1.6°, respectively, p = 0.455). The femoral rotational alignment angle measured using the gap balancing technique during surgery was −0.5° ± 0.8° in group I and 3.9° ± 0.8° in group II (p < 0.001). The patellar tilt angle measured at 1 year after the operation was −0.4° ± 3.6° in group I and 0.1° ± 4.1° in group II (p = 0.251), and an angle above ± 5° was found in 5.1% in group I and in 10.3% in group II, which also showed no statistically significant difference. Patella translation also showed no statistically significant difference with 4.1 ± 2.8 mm in group I and 3.8 ± 2.8 mm in group II (p = 0.408), and translation longer than 5 mm was observed in 16.2% in group I and in 8.9% in group II. We observed no difference in American Knee Society knee score (93.1 in group I vs. 93.5 in group II, p = 0.441) and Knee Society function score (92.6 in group I vs. 92.4 in group II, p = 0.725). There was no case of lateral retinacular release.
DISCUSSION
We evaluated the effect of internal femoral rotation on patellar tracking using the gap balancing technique in TKA and confirmed that compared to external femoral rotation, internal femoral rotation would not increase the risk of patellar maltracking if the ligament was properly balanced in flexion.
Several studies have demonstrated the effect of femoral rotational alignment on patellar tracking in TKA. As internal femoral rotation may cause patellar maltracking, external femoral rotation has been recommended for normal patellar tracking. Akagi et al.11) reported that a lateral retinaculum release was conducted in 34% when the femoral rotation was parallel to the posterior condylar axis as compared to 6% when 3°–5° of external rotation alignment was applied in TKA. Terashima et al.12) reported that the alignments of the femoral component in the sagittal and coronal planes were not correlated, while patellofemoral contact pressure decreased as the external femoral rotation increased. Berger et al.13) confirmed an increase in patellar complications such as patellar maltracking and dislocation with an increase in the internal rotational alignment of the femur and tibia.
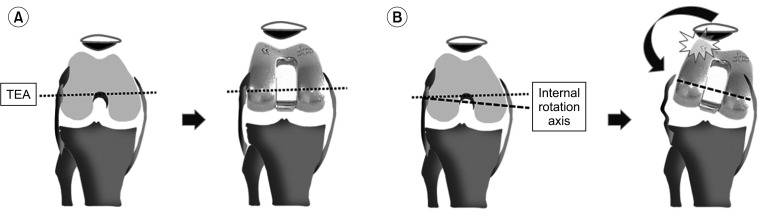
However, the theoretical mechanisms have not been clearly elucidated; the effects of femoral rotation on patellar tracking have been reported based on clinical results. We assumed a biomechanical relationship between internal femoral rotation and patellar tracking. When a femoral component is inserted with internal rotation relative to the anatomical femoral rotational axis, the femoral component becomes internally rotated, resulting in an incongruity with the patella, which is located laterally in the femoral trochlear groove, and ligament imbalance in flexion as the medial gap is tensed and the lateral gap is relaxed, which eventually lead to lateral femoral condylar lift-off and incongruity between the femoral trochlear groove and patella (Fig. 2).
Fig. 2. Postulation of biomechanical relationship between femoral rotational alignment and patellar tracking. (A) Anatomic femoral rotation shows good patellar tracking. (B) Internal femoral rotation results in lateral patellar tilt due to impingement of femoral and patellar component, and lateral femoral condylar lift-off. TEA: transepicondylar axis.
However, defining external femoral rotation as the standard axis presents some limitations. This is because femoral rotational alignment is involved not only in the patellar alignment, but also in many important procedures such as ligament and gap balancing in flexion. There are problems that may occur when the measured resection technique is based on the external femoral rotational alignment. First, in the case of medial gap laxity during flexion, the imbalance caused by the relaxation of the medial gap still remains. Thus, procedures for ligament balance are required such as suturing of medial soft tissue, release of lateral soft tissue, and use of a constrained condylar knee. Second, in the case where external femoral rotation was attempted, but internal femoral rotation relative to the anatomical femoral rotation was actually obtained due to a measurement error, both patellar tracking and ligament balance can be compromised, and measurement errors in measured resection techniques are known to be inevitable.14,15) Likewise, the external femoral rotational alignment can sometimes result in ligament imbalance. Victor16) suggested that even if increased external femoral rotation may reduce the possibility of patellar maltracking, the stability of the tibiofemoral joint should not be affected.
By contrast, gap balancing technique is based on the ligament balancing axis regardless of the anatomical femoral rotational alignment. And in the case of laxity of the medial gap, internal femoral rotation can be conducted to correct the ligament balance during flexion.17) However, the problem is that the effect of internal femoral rotation on patellar tracking has not been clearly confirmed. Therefore, we evaluated the effect on patellar tracking in TKA using the gap balancing technique, even when the femoral component was inserted relatively internal to the anatomical femoral rotation but the ligament was balanced. As a result, there was no statistically significant difference between internal femoral rotation and 3°–5° external femoral rotation in terms of the patellar tilt angle (−0.4° ± 3.6° vs. 0.1° ± 4.1°, respectively) and patellar malatracking of more than ± 5°. The results showed that patellar tracking was not affected by internal femoral rotation itself, whereas ligament balance in flexion was more influential than we had postulated.
In the present research, the cause of laxity of the medial gap in flexion might have mostly occurred after the soft-tissue release for alignment and ligament balance in the coronal plane. Therefore, in case of laxity of the medial gap in flexion, considering the ligament balance axis rather than predetermination of external femoral rotation would be beneficial not only for ligament balance but also for patellar tracking.
Heesterbeek et al.18) also reported on 49 cases of TKA using the gap balancing technique. They found that femoral rotation showed a distribution of −3° to 12°, there was no correlation between the patellar alignment and femoral rotation, and the gap technique could be used safely without the risk of patellar malalignment.
The limitation of the study is that we did not consider the influence of other factors such as preoperative deformity and various surgical techniques involving patellar alignment. In addition, internal femoral rotation is generally determined with reference to the anatomical femoral rotation axis; however, it was set to be less than 0° relative to the posterior condylar axis in the present study, considering the possibility of measurement error of the anatomical femoral rotation axis. Further, we did not conduct quantitative assessment on what extent of internal femoral rotation by the gap balancing technique can be considered acceptable compared to the anatomical femoral rotational alignment axis.
Although the role of external femoral rotation for normal patellar tracking in TKA is well known, internal femoral rotation with the gap balancing technique did not affect patellar tracking in the current study. Therefore, when determining femoral rotational alignment, ligament balance in flexion should be considered as a crucial factor for normal patellar tracking regardless of the anatomical femoral rotational axis.
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Maheshwari AV, Tsailas PG, Ranawat AS, Ranawat CS. How to address the patella in revision total knee arthroplasty. Knee. 2009;16(2):92–97. doi: 10.1016/j.knee.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 2.Putman S, Boureau F, Girard J, Migaud H, Pasquier G. Patellar complications after total knee arthroplasty. Orthop Traumatol Surg Res. 2019;105(1S):S43–S51. doi: 10.1016/j.otsr.2018.04.028. [DOI] [PubMed] [Google Scholar]
- 3.Figgie HE, 3rd, Goldberg VM, Heiple KG, Moller HS, 3rd, Gordon NH. The influence of tibial-patellofemoral location on function of the knee in patients with the posterior stabilized condylar knee prosthesis. J Bone Joint Surg Am. 1986;68(7):1035–1040. [PubMed] [Google Scholar]
- 4.Donell S. Patellar tracking in primary total knee arthroplasty. EFORT Open Rev. 2018;3(4):106–113. doi: 10.1302/2058-5241.3.170036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mochizuki RM, Schurman DJ. Patellar complications following total knee arthroplasty. J Bone Joint Surg Am. 1979;61(6A):879–883. [PubMed] [Google Scholar]
- 6.Newbern DG, Faris PM, Ritter MA, Keating EM, Meding JB, Berend ME. A clinical comparison of patellar tracking using the transepicondylar axis and the posterior condylar axis. J Arthroplasty. 2006;21(8):1141–1146. doi: 10.1016/j.arth.2006.02.171. [DOI] [PubMed] [Google Scholar]
- 7.Daines BK, Dennis DA. Gap balancing vs. measured resection technique in total knee arthroplasty. Clin Orthop Surg. 2014;6(1):1–8. doi: 10.4055/cios.2014.6.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Insall JN, Dorr LD, Scott RD, Scott WN. Rationale of the knee society clinical rating system. Clin Orthop Relat Res. 1989;(248):13–14. [PubMed] [Google Scholar]
- 9.Chang CB, Seong SC, Lee S, Lee MC. Anatomical assessment of the distal femur and tibia for optimal femoral rotational alignment in total knee arthroplasty. J Korean Knee Soc. 2010;22(1):46–55. [Google Scholar]
- 10.Bindelglass DF, Cohen JL, Dorr LD. Patellar tilt and subluxation in total knee arthroplasty: relationship to pain, fixation, and design. Clin Orthop Relat Res. 1993;(286):103–109. [PubMed] [Google Scholar]
- 11.Akagi M, Matsusue Y, Mata T, et al. Effect of rotational alignment on patellar tracking in total knee arthroplasty. Clin Orthop Relat Res. 1999;(366):155–163. doi: 10.1097/00003086-199909000-00019. [DOI] [PubMed] [Google Scholar]
- 12.Terashima T, Onodera T, Sawaguchi N, Kasahara Y, Majima T. External rotation of the femoral component decreases patellofemoral contact stress in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3266–3272. doi: 10.1007/s00167-014-3103-5. [DOI] [PubMed] [Google Scholar]
- 13.Berger RA, Crossett LS, Jacobs JJ, Rubash HE. Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res. 1998;(356):144–153. doi: 10.1097/00003086-199811000-00021. [DOI] [PubMed] [Google Scholar]
- 14.Siston RA, Patel JJ, Goodman SB, Delp SL, Giori NJ. The variability of femoral rotational alignment in total knee arthroplasty. J Bone Joint Surg Am. 2005;87(10):2276–2280. doi: 10.2106/JBJS.D.02945. [DOI] [PubMed] [Google Scholar]
- 15.Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am. 1987;69(5):745–749. [PubMed] [Google Scholar]
- 16.Victor J. Rotational alignment of the distal femur: a literature review. Orthop Traumatol Surg Res. 2009;95(5):365–372. doi: 10.1016/j.otsr.2009.04.011. [DOI] [PubMed] [Google Scholar]
- 17.Lee SY, Lim HC, Jang KM, Bae JH. What factors are associated with femoral component internal rotation in TKA using the gap balancing technique? Clin Orthop Relat Res. 2017;475(8):1999–2010. doi: 10.1007/s11999-017-5319-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Heesterbeek PJ, Keijsers NL, Wymenga AB. Femoral component rotation after balanced gap total knee replacement is not a predictor for postoperative patella position. Knee Surg Sports Traumatol Arthrosc. 2011;19(7):1131–1136. doi: 10.1007/s00167-011-1409-0. [DOI] [PubMed] [Google Scholar]