Abstract
Introduction
Coronavirus disease 2019 (COVID-19) has emerged as severe acute respiratory syndrome coronavirus 2 (SARS-CoV2). Recently, various complications have been reported. The aim of the current study is to report a rare case of transverse myelitis after recovering from COVID-19.
Case report
A 34-year-old lady, presented with inability to walk for one day duration due to the lower limb weakness. After two weeks from the recovery of COVID-19; she developed progressive intermittent leg pain, paresthesia and weakness on both sides. Brain and cervical MRI showed evidence of a short segment inflammatory enhancing lesion at upper cervical region (at C1 level). The patient was treated conservatively.
Discussion
Transverse myelitis has many different causes, it occurs as an autoimmune phenomenon post-infection and vaccination, or it may result from direct infection or acquired demyelinating disease like multiple sclerosis.
Conclusion
Although it is a sporadic finding, SARS-CoV-2 can cause transverse myelitis. The condition responds to medical therapy.
Keywords: SARS-CoV-2, Neurological dysfunction, Corona virus disease 2019
Highlights
-
•
Coronavirus disease 2019 has emerged as severe acute respiratory syndrome coronavirus 2.
-
•
Transverse myelitis (TM) is a very rare neurological complication of COVID-19 disease.
-
•
In this report a rare case of post-COVID19 transverse myelitis presented.
1. Introduction
Coronavirus disease 2019 (COVID-19) has emerged due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV2) [1]. Until April 23, 2021, more than 144 million cases have been reported globally including more than 3 million deaths [2]. Some neurological symptoms and complications associated with SARS-CoV-2 in mild and severe cases have been reported [3]. There are several common viral characteristics between SARS-CoV-2 and SARS-CoV. Still, it has been reported that SARS-CoV-2 has a greater affinity to angiotensin-converting enzyme 2 (ACE2) receptor presented in the human glial cells, neurons, respiratory epithelial, and vascular endothelial cells [4]. However, only a few cases of neurological complications following complete recovery from SARS-CoV-2 infection have been reported [5].
TM is characterized by focal inflammation within the spinal cord, resulting in neurological dysfunction [6]. Acute TM is an infrequent clinical condition with an annual incidence of 1–4 new cases per million people. It affects individuals at any age with bimodal peaks in the second and fourth decades of life with no gender predominance [7]. Transverse myelitis (TM) is a very sporadic neurological complication of COVID-19 disease, up to date, only ten cases of TM from acute infection of SARS-CoV-2 have been reported [8].
The current study aims to report an unusual case of TM which developed after recovery from COVID-19. The report has been arranged in line with SCARE 2020 guidelines with a brief literature review [9].
Patient's information: A 34-year-old lady presented with an inability to walk for 1-day due to lower limb weakness. The condition started gradually two weeks after recovery from COVID-19 by progressive intermittent leg pain, paresthesia and weakness on both sides of the body. In the beginning, the weakness was noted on the right side, then the left side also involved. The condition worsened on the three consecutive days. Past medical, past surgical, family and drug history was negative.
Clinical findings: She was conscious. The vital signs were within the normal range. Ophthalmological and cranial nerve examination was normal. Upper limb examination showed mild proximal weakness on both sides 4/5. Mild Paraparesis 4/5, but right side was more than the left side, especially, proximal parts. Reflexes were normal with negative Babinski bilaterally. Coordination and sensory examinations were normal including light touch and pin prick. There was a disturbance in the gait due to leg weakness.
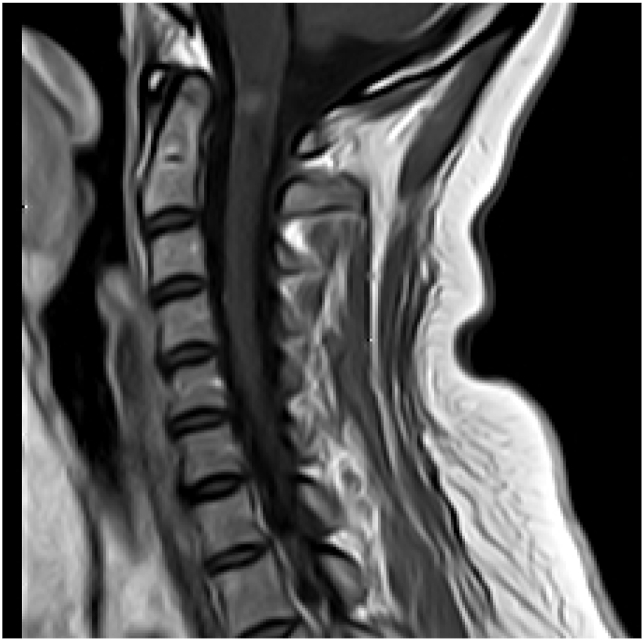
Diagnostic assessment: Hematological tests revealed high white blood cell (WBC) counts (18000), C-reactive protein (CRP): 9.4, and erythrocyte sedimentation rate (ESR): 22 Brain and cervical magnetic resonance imaging (MRI) showed evidence of short segment inflammatory enhancing lesion at upper cervical region (Fig. 1). Screening for autoimmune diseases and vasculitis was negative. Lumbar puncture showed normal cell count, protein, lactate and glucose with positive oligoclonal bands.
Fig. 1.
Pretreatment MRI showing short segment transverse myelitis.
Therapeutic intervention: Methylprednisolone 500mg i.v 1x1 for 5 days prescribed for the patient. After completing therapy her weakness improved significantly but after stopping MP she developed bilateral sever leg pain. Rheumatological consultation gave no evidence of any significant joint problems.
Follow up: After one week of follow up her pain improved substantially. Cervical MRI after ten days did not show the spinal lesion (see Fig. 2).
Fig. 2.
Post treatment MRI showing disappearance of previous inflammatory lesion at upper cervical segment.
2. Discussion
Transverse myelitis is non-compressive heterogenous myelopathy, it is acute-onset or subacute-onset spinal cord dysfunction due to inflammation [10]. TM has many different causes, most often occurs as an autoimmune phenomenon post-infection and vaccination, or may result from direct infection or acquired demyelinating disease like multiple sclerosis [11]. There are some studies that have been published recently describing the neurological manifestation of SARS-CoV-2 and its ability to invade both the central nervous system (CNS) and the peripheral nervous system (PNS). According to a comprehensive review on neurological manifestation, it was found that more than a third of hospitalized patients with COVID-19 have developed some form of neurological symptoms [6]. As reported by Srewastava et al. SARS-CoV-2 invades CNS through ACE2 receptor [4]. But there is some evidence that SARS-CoV-2 can involve CNS through blood circulation [12]. Hyper-inflammatory state characterized by hyperactivity of innate immunity with activation of inflammatory cells and overproduction of inflammatory cytokines and chemokines due to post-viral immunological reaction to COVID-19 are other mechanisms of CNS involvement [13].
Severe infection produces a greater range of neurological manifestations [14]. Some RNA and DNA viruses have been identified in acute TM, some of them infect and kill anterior horn cells of the spinal cord that results in flaccid paralysis, or others like cytomegalovirus (CMV), varicella-zoster virus (VZV), Epstein bar virus (EBV), and coxsackieviruses A and B often involve the white matter of spinal cord [15]. The present case report points towards COVID-19 as a possible cause of acute TM. As reported in the literature, coronavirus has neurotropic and neuroinvasive capability developing neuropsychiatric symptoms, seizure, encephalomyelitis, acute flaccid paralysis, Guillain-Barre syndrome, and cerebrovascular disease [16]. Up to date, only a few number of cases of spinal cord disorder related to COVID-19 have been described in the literature [6].
Paraplegia, quadriplegia, loss of deep reflexes, sensory impairment, and bladder incontinence resulting from acute partial or complete motor, sensory and autonomic spinal cord dysfunction are among the clinical manifestations of TM [17]. This case presented with pain, paresthesia, and weakness on both sides with normal reflexes, negative Babinski sign. Another symptom that differentiates this case from some other reported cases is fever, as reported previously, Post COVID-19 TM cases develop fever [17,18]. The presenting case was afebrile. Bladder and bowel dysfunction are other symptoms that develop in some cases of TM [6,10,17,19]. This case had normal sphincters.
Diagnosis of viral myelitis can be made after exclusion of all other possible diseases. Initial evaluation should focus on structural or compressive lesions of the spinal cord which should be excluded with appropriate imaging [15]. The diagnosis of TM is based on the clinical findings, the characteristic lesion on MRI, serologic, and CSF analysis (mild pleocytosis) [16].
Treatment of TM is still controversial in the literature. Corticosteroids are the first-line treatment, with plasma exchange in patients who do not respond to corticosteroids. Zachariadis et al. reported a case which first treated with IV human immunoglobulin without response while IV corticosteroid therapy for 5 days, slightly improved the condition [3]. However, Baghbanian et al. treated their case with plasmapheresis without corticosteroid [20]. This case was successfully treated with methylprednisolone for 5 days.
In conclusion, SARS-CoV-2 can cause TM. Treatment with methylprednisolone results in a rapid and significant improvement in neurological manifestations.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Ethical approval
Approval is not necessary for case report in our locality.
Sources of funding
No source to be stated.
Authors contribution
Shwan Abubakr Ahmad, Karokh H.Salih, Shaho Fatah Ahmed: Physician managing the case, follow up the patient, writing the manuscript and final approval of the manuscript.
Fahmi H.Kakamad, Abdulwahid M.Salh, Karukh K. Mohammed: literature review, writing the manuscript, final approval of the manuscript.
Shvan H. Mohammed, Rawezh Q. Salih, Dahat A Hussein: major contribution to the idea, revision and final revision of the manuscript.
Registration of research studies
According to the previous recommendation, registration is not required for case report.
Guarantor
Fahmi Hussein Kakamad is the Guarantor of submission.
Consent
Consent has been taken from the patient and the family of the patient.
Declaration of competing interest
There is no conflict to be declared.
References
- 1.Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55(3):105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization 2020. https://covid19.who.int/ Accessed on April 23.
- 3.Zachariadis A., Tulbu A., Strambo D., Dumoulin A., Di Virgilio G. Transverse myelitis related to COVID-19 infection. J. Neurol. 2020;267(12):3459–3461. doi: 10.1007/s00415-020-09997-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sriwastava S., Kataria S., Tandon M., Patel J., Patel R., Jowkar A. Guillain Barré Syndrome and its variants as a manifestation of COVID-19: a systemic review of case report and case series. J. Neurol. Sci. 2020:117263. doi: 10.1016/j.jns.2020.117263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scheidl E., Canseco D.D., Hadji‐Naumov A., Bereznai B. Guillain‐Barr é syndrome during SARS‐CoV‐2 pandemic: a case report and review of recent literature. J. Peripher. Nerv. Syst. 2020;25(2):204–207. doi: 10.1111/jns.12382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moreno-Escobar M.C., Kataria S., Khan E., Subedi R., Tandon M., Peshwe K. Acute transverse myelitis with Dysautonomia following SARS-CoV-2 infection: a case report and review of literature. J. Neuroimmunol. 2021;353:577523. doi: 10.1016/j.jneuroim.2021.577523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Krishnan C., Kaplin A.I., Deshpande D.M., Pardo C.A., Kerr D.A. Transverse myelitis: pathogenesis, diagnosis and treatment. Front. Biosci. 2004;9(1483):99. doi: 10.2741/1351. [DOI] [PubMed] [Google Scholar]
- 8.Transverse Myelitis Consortium Working Group* Proposed diagnostic criteria and nosology of acute transverse myelitis. Neurology. 2002;59(4):499–505. doi: 10.1212/wnl.59.4.499. [DOI] [PubMed] [Google Scholar]
- 9.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;84:226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 10.Chakraborty U., Chandra A., Ray A.K., Biswas P. COVID-19–associated acute transverse myelitis: a rare entity. BMJ Case Reports CP. 2020;13(8):238668. doi: 10.1136/bcr-2020-238668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Frohman E.M., Wingerchuk D.M. Transverse myelitis. N. Engl. J. Med. 2010;363(6):564–572. doi: 10.1056/NEJMcp1001112. [DOI] [PubMed] [Google Scholar]
- 12.Wu Y., Xu X., Chen Z., Duan J., Hashimoto K., Yang L. Nervous system involvement after infection with COVID-19 and other coronaviruses. Brain Behav. Immun. 2020 Jul 1;87:18–22. doi: 10.1016/j.bbi.2020.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fumery T., Baudar C., Ossemann M., London F. Longitudinally extensive transverse myelitis following acute COVID-19 infection. Multiple sclerosis and related disorders. 2021;48:102723. doi: 10.1016/j.msard.2020.102723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chowdhary A., Subedi R., Tandon M., Wen S., Patel J., Kataria S. Relevance and clinical significance of magnetic resonance imaging of neurological manifestations in COVID-19: a systematic review of case reports and case series. Brain Sci. 2020;10(12):1017. doi: 10.3390/brainsci10121017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kincaid O., Lipton H.L. Viral myelitis: an update. Curr. Neurol. Neurosci. Rep. 2006;6(6):469. doi: 10.1007/s11910-006-0048-1. [DOI] [PubMed] [Google Scholar]
- 16.Durrani M., Kucharski K., Smith Z., Fien S. Acute transverse myelitis secondary to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2): a case report. Clinical practice and cases in emergency medicine. 2020;4(3):344. doi: 10.5811/cpcem.2020.6.48462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hazrati E., Farahani R.H., Asl A.N., Shahali H. 2020. Acute Transverse Myelitis after SARS-CoV-2 Infection: a Rare Complicated Case of Rapid Onset Paraplegia in a Male Veteran. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Munz M., Wessendorf S., Koretsis G., Tewald F., Baegi R., Krämer S. Acute transverse myelitis after COVID-19 pneumonia. J. Neurol. 2020;267:2196–2197. doi: 10.1007/s00415-020-09934-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lisnic V., Nemtan V., Hacina E., Topciu G., Manole E., Thurnher M.M., von Kummer R. 2020. Acute Transverse Myelitis in a HIV-Positive Patient with COVID-19. [Google Scholar]
- 20.Baghbanian S.M., Namazi F. Post COVID-19 longitudinally extensive transverse myelitis (LETM)–a case report. Acta Neurol. Belg. 2020:1–2. doi: 10.1007/s13760-020-01497-x. [DOI] [PMC free article] [PubMed] [Google Scholar]