ABSTRACT
Background
Drought has been a considerable problem for many years in northern Bangladesh. However, the health impacts of drought in this region are not well understood.
Methods
This study analyzed the impact of drought duration and severity on select causes of mortality in northern Bangladesh. Rainfall data from three meteorological stations (Rangpur, Dinajpur and Nilphamari) in northern Bangladesh were used to assess drought and non-drought periods, and the Standardized Precipitation Index was used to categorize mild, moderate, severe, and extreme drought. Mortality data from 2007 to 2017 for the three areas were collected from the Sample Vital Registration System, which is a survey of 1 million people. The generalized linear model with Poisson regression link was used to identify associations between mortality and the drought severity and 1-month preceding SPI.
Results
Only severe and extreme drought in the short-term drought periods affected mortality. Long-term drought was not associated with natural cause mortality in Rangpur and Nilphamari. In Dinajpur, mild and moderate drought was associated with circulatory- and respiratory-related mortality.
Conclusion
The impact of drought on mortality varied by region. This study improves our understanding of how droughts affect specific causes of mortality and will help policy makers to take appropriate measures against drought impacts on selected cause of mortality. Future research will be critical to reduce drought-related risks of health.
Keywords: climate change, drought, mortality, public health
Global climate change is one of the most important environmental issues facing the world today.1 In recent years, the health effects associated with climate change have been acknowledged and prioritized. There is a close relationship between the local climate and the occurrence and severity of certain diseases and other adverse health conditions.2 Humans are extremely vulnerable to the effects of climate change, particularly to the recent climate-related impacts of extreme phenomena such as heat waves, droughts, floods, hurricanes, and forest fires.3, 4 Among these, drought has a slow onset but is the most far-reaching of all natural disasters5 and has serious effects on agriculture, water resources, ecology, and society. The beginning and end of a drought are difficult to define, as is its impact. This is because drought can last for a long period of time with accumulating impacts; furthermore, many of the effects are diffuse, indirect, and cumulative.6, 7
Drought is defined as severe moisture deficit in the soil, occurs when there is insufficient precipitation.8, 9 Drought is categorized into four distinct types: meteorological (rainfall deficit), hydrological (low water levels in streams), agricultural (low soil moisture), and socioeconomic (when the water demand exceeds the supply).9 Socioeconomic choices, population growth and mobility, infrastructure, land-use changes, potential population vulnerability, and other factors affect the occurrence of drought. Poor health, poverty, and conflicts exacerbate the effects of drought. The direct and indirect consequences of drought on human well-being depend on the duration and severity of the drought, the country’s economic and social structure and the availability of resources.10
The biological mechanisms through which drought affects well-being are unclear,6, 11 but several pathways have been hypothesized. The effects of drought that have received the most attention are those related to mental health, malnutrition, and nutritional deficiencies.10, 12, 13 Other studies suggest that drought may be related to infectious diseases and respiratory diseases,14 an increased risk of mortality from diarrheal illness,15 the transmission of some mosquito-borne diseases,16 waterborne diseases such as dysentery, diarrhea, and cholera,17 and the risk of cardiovascular and upper respiratory diseases.18 There have also been studies on how drought impacts mental health and suicide in farmers.19, 20 Several studies have suggested that drought may be related to numerous other detrimental human health impacts, including hypo nutrition, various mental illnesses, and the aggravation of pre-existing chronic pathological conditions that may continue even after the end of the crisis.21, 22 Drought might impact diseases through auxiliary exposures, such as increasing the amount of airborne dust or wildfire smoke or modifying the development and dispersal of allergenic pollen and fungal spores.11 The vulnerability to drought and drought risks vary depending on the level of development and the needs of each country.23, 24 More deaths principally mediated by drought’s impact on water and food insecurity or livelihood loss25 occur in low and middle income countries (e.g., East Africa and regions in Asia), whereas in high income countries (e.g., Spain and the USA), the impact is thought to focus on economic losses or pollution exposure.26
Climate modeling shows that droughts are becoming more regular, severe, spatially broad, and of longer duration because of rapid environmental change.27 It is anticipated that global mean temperature will increase by 0.2°C per decade; however, the actual temperature rise will vary by region.28 The most recent predictions indicate that before the end of the twenty-first century, average temperatures will increase by 0.3–4.8°C.29 Bangladesh is an agricultural nation in Southeast Asia that often deals with extreme weather-related events such as flooding, tornados, severe rainstorms, coastal erosion, and drought.30 Although drought affects the economy, it has received less scientific attention than some of the other extreme weather events.31 In Bangladesh, temperatures are increasing faster than the current pace of global warming, and warming is expected to continue in the coming decades.32, 33 This continued warming will increase the demand for water and, accordingly, drought severity in the country. Drought is frequent in many places throughout Bangladesh; however, the northwest is extremely susceptible to drought owing to low levels of precipitation (1,329 mm in northwest, 4,338 mm in southwest).34
Several studies have investigated drought in Bangladesh and particularly in northern Bangladesh. These studies are related to drought risk assessment, spatiotemporal analysis, the identification of meteorological drought, the environmental impact of drought, health impacts such as cholera and dysentery, socioeconomic impacts, and agricultural impacts.30,31,32, 34,35,36,37 However, in northern Bangladesh, no studies have been conducted to ascertain the impact of drought on mortality. Therefore, we analyzed the prevalence of drought in northern Bangladesh and the association between generic drought indicators and mortality to assess the health impact of drought in this region, which is economically and geographically vulnerable. The main objective of this study was to evaluate the impact of drought, measured by the Standardized Precipitation Index (SPI) obtained for different timescales (3 and 12 months), on the daily natural cause, circulatory-related, and respiratory-related mortality from 2007 to 2017 in northern Bangladesh.
MATERIALS AND METHODS
In this study, we evaluated the short- and long-term drought characteristics in the northern region of Bangladesh using the SPI and compared them with select causes of mortality. Precipitation data from three stations in northern Bangladesh for the period of 1989–2018 were used to assess drought characteristics.
Study area
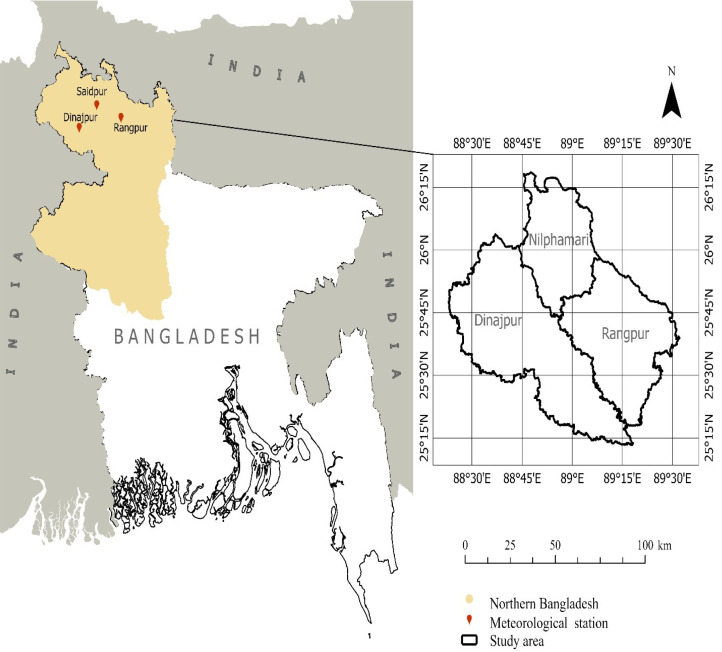
The study area covered the northernmost part of Bangladesh. Northern Bangladesh consists of two divisions, Rajshahi and Rangpur, and 16 districts. Based on the availability of weather stations (Fig. 1), we selected three districts (Rangpur, Dinajpur, and Nilphamari) in the Rangpur Division as our study area. We obtained data from the three Bangladesh Meteorological Department (BMD) weather stations located in Rangpur Division. Table 1 presents the area, population, average air temperature, and average precipitation of the regions covered by the three weather stations.
Fig. 1.
Location of study sites and meteorological stations in Bangladesh.
Table 1. Geographical characteristics of the study area38, 39.
| Study area/meteorological station |
Area covered by meteorological station (km2) |
Population of study area
(million) |
Study population selected for SVRS mortality data | Yearly average rainfall during study period (mm) | Monthly average temperature during study period (°C) | |
| Tmax | Tmin | |||||
| Rangpur/Rangpur | 2,400.56 | 2.99 | 21,375 | 1,961.58 | 29.83 | 20.56 |
| Dinajpur/Dinajpur | 3,444.30 | 2.99 | 20,250 | 1,641.16 | 30.24 | 20.33 |
| Nilphamari/Saidpur | 1,643.70 | 1.91 | 14,625 | 1,825.50 | 30.37 | 20.29 |
Tmax, maximum temperature; Tmin, minimum temperature.
Data collection
Meteorological data
The study area is situated between 25°12ʹ and 26°20ʹ latitude north and 88°20ʹ and 89°32ʹ longitude east. Monthly precipitation, temperature, and humidity data were collected from the three BMD meteorological stations located in the study area. We used precipitation data for the years 1989–2018 to generate drought indices for the years 2007–2017 (see below). Temperature and humidity were used as covariates in the analysis.
Mortality data
Mortality data are collected by SVRS and were provided by the Bangladesh Bureau of Statistics. SVRS collects vital information, such as births and deaths, on a sample population of approximately one million people. There are 1,000 primary sample units, each consisting of 250 households, with an average of 4.5 people per household.38
We analyzed the 2007–2017 daily mortality data from our study area. There were 64 individual causes of death included in the SVRS dataset, and we categorized these by area and cause. We categorized daily mortality and converted it into monthly mortality to enable comparison with the monthly drought periods. We selected three major causes of mortality in line with the ICD-10: natural cause mortality (ICD-10: A00–R99), circulatory-related mortality (ICD-10: I00–I99), and respiratory-related mortality (ICD-10: J00–J99). Other causes of death were not included in the analysis because of insufficient data.
Drought analysis
We applied the SPI to analyze drought because this index is widely used to characterize meteorological drought over a broad range of timescales.40 For short timescales, the SPI is closely related to soil moisture, while for longer timescales it is related to groundwater and reservoir storage. The SPI calculation for a location is based on the long-term precipitation record of the desired period. This long-term record is fitted to a probability/gamma distribution, which is then transformed into a normal distribution so that the mean SPI for the location and desired period is zero.41 Positive SPI values indicate greater than median precipitation, and negative values indicate less than median precipitation. Because the SPI is normalized, wetter and drier climates can be represented in the same way; thus, wet periods can also be monitored using the SPI. The gamma distribution to fit well to the climatological precipitation time series.42 The gamma distribution is defined by its frequency or probability density function:
| g(x) = 1/β Γ(a) xa−1e− x / β, for x > 0 |
in which a and β are the shape and scale parameters respectively, x is the precipitation amount and Γ (a) is the gamma function. Parameters a and β of the gamma pdf are estimated for each station and for each time scale of interest (1, 3, 6, 9, 12 months, etc.). Maximum likelihood estimations of a and β are:
and n is the number of observations.
The resulting parameters are then used to find the cumulative probability of an observed precipitation event for the given month and time scale for the location in question. Since the gamma function is undefined for x = 0 and a precipitation distribution may contain zeros, the cumulative probability becomes:
| H (x) = q + (1− q) G(x) |
in which q is the probability of zero precipitation and G(x) is the cumulative probability of the incomplete gamma function. If m is the number of zeros in a precipitation time series, then q can be estimated by m/n. The cumulative probability H(x) is then transformed to the standard normal random variable z with mean zero and variance of one,43 which is the value of the SPI.
| c0 = 2.515517, c1 = 0.802853, c2 = 0.010328 |
| d1 = 1.432788, d2 = 0.189269, d3 = 0.00130 |
Drought can be calculated on various timescales, for example, 1, 3, 6, 9, 12, 24, or 48 months. A drought event for a given timescale is defined as a period in which the SPI is continuously negative and reaches a value of –1.0 or less.44 The drought period begins when the SPI first falls below zero and ends when the SPI becomes positive after reaching a value of –1.0 or less. Though, in our study, we include (–0.85 < SPI ≤ 0) as mild drought. In case of agricultural impact, mild drought may be not included in the study for not having strong impact, but for analyzing health impact mild drought can have greater impact. In this study, a drought duration of 3 months was defined as short-term drought (3-SPI), and a drought duration of 12 months was defined as long-term drought (12-SPI). In line with previous studies, we also categorized the drought intensity based on the SPI value as follows: no drought (SPI > 0), mild drought (–0.85 < SPI ≤ 0), moderate drought (–1.27 < SPI ≤ –0.85), severe drought (–2.05 < SPI ≤ –1.28), and extreme drought (SPI ≤ –2.06).26, 45 The reason for such categorization of drought and not using direct correlation between positive and negative values of SPI is to be able to distinguish the impact for each drought severity.
Statistical analyses
We conducted an analysis to estimate the relative risks of mortality associated with exposure to drought severity. This included all-cause and cause-specific (cardiovascular, respiratory) monthly mortality and drought duration based on severity. We performed two distinct analyses: i) to define the relationship between mortality and the drought severity (based on the SPI category), and ii) to define the relationship between mortality and the 1-month preceding SPI, using a generalized linear model (GLM) based on a Poisson distribution. These analyses clarified the effects and aftereffects of drought. In the statistical analysis, the SPI value was the independent variable and mortality was the dependent variable, while temperature and humidity were covariates. A P value < 0.05 was regarded as statistically significant. The validity of each model was evaluated by goodness of fit for high and low dispersion and omnibus test. All analyses were performed using IBM SPSS Statistics 25. Drought analyses performed using R software version 3.3.6.
Ethics approval
This study did not require research ethics approval, as publicly available, anonymized aggregate data were used for all analyses.
RESULTS
Descriptive statistics of drought episodes in northern Bangladesh
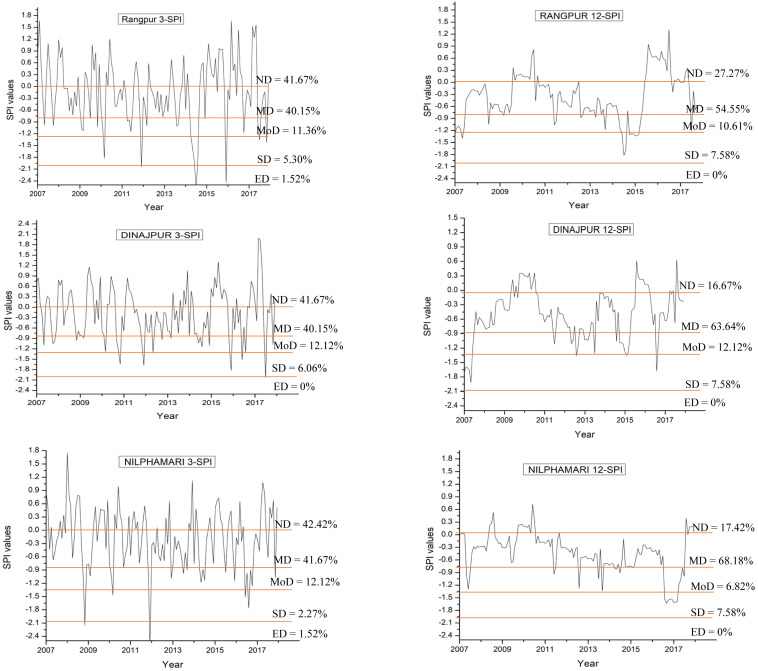
The short-term and long-term drought period from 2007-2017 along with the % of drought severity showed in Fig. 2. The percentages of drought duration during periods of short-term drought (3-SPI) for the three regions were Rangpur, 58.3%; Dinajpur, 58.3%; and Nilphamari, 57.6%. In contrast, the percentages of long-term drought (12-SPI) were in Rangpur, 72.7%; Dinajpur, 83.3%; and Nilphamari, 82.6%. These percentages were all higher than for the 3-SPI and varied by region (Fig. 2). Regarding drought severity, the duration of mild drought events during the 3-SPI was nearly the same in the three regions (Rangpur, 40.15%; Dinajpur, 40.15%; Nilphamari, 41.67%). Regarding the 12-SPI timescale, mild drought conditions occurred more often than for the 3-SPI timescale (Rangpur, 54.55%; Dinajpur, 63.64%; Nilphamari, 68.18%). Moderate drought showed the opposite trend, as these conditions were more prevalent for the 3-SPI timescale than for the 12-SPI timescale (Rangpur: 3-SPI, 11.36%; 12 SPI, 10.61%; Dinajpur: 3-SPI and 12 SPI, 12.12%; Nilphamari: 3-SPI, 12.12%, 12-SPI, 6.82%). There was a slightly higher percentage of severe drought conditions in the long-term drought period (Rangpur: 3-SPI, 5.30%, 12-SPI, 7.58%; Dinajpur: 3-SPI, 6.06%, 12-SPI, 7.58%; Nilphamari: 3-SPI, 2.27%, 12-SPI, 7.58%). During the study period, the percentage of extreme drought conditions was very low and only occurred for the 3-SPI timescale. Additionally, no extreme drought occurred in Dinajpur for any timescale. The percentage of extreme drought in both Rangpur and Nilphamari was 1.52% and occurred during short-term drought events.
Fig. 2.
Drought variability in three areas of northern Bangladesh. *ND, no drought (SPI > 0), MD, mild drought (–0.85 < SPI ≤ 0), MoD, moderate drought (–1.27 < SPI ≤ –0.85), SD, severe drought (–2.05 < SPI ≤ –1.28), and ED, extreme drought (SPI ≤ –2.06). Total drought period from 2007–2017 are given in % for individual category.
The impact of drought on daily mortality in northern Bangladesh
There were no large regional differences in number of deaths (Table 2). Tables 3–5 shows there was high variability within each area. Short-term droughts had a greater influence in each area. In Rangpur, mild drought was associated with low all-cause mortality and cardiac mortality, regardless of drought duration. However, short-term extreme drought (RR = 1.470, 95% CI 1.039 to 2.079, P = 0.029) and severe drought (RR = 1.433, 95% CI 1.169 to 1.755, P = 0.001) exacerbated natural cause mortality. For the 3-SPI 1-month preceding SPI (3-SPI lag 1), severe drought was significantly associated with natural cause mortality (RR = 1.548, 95% CI 1.262 to 1.898, P = 0.000).
Table 2. Total number of deaths for selected causes during the study period (2007–2017).
| Total number of deaths during the study period (2007–2017) | |||
| Station | Natural cause | Circulatory-related | Respiratory-related |
| Dinajpur | 856 | 204 | 184 |
| Rangpur | 1,438 | 426 | 237 |
| Nilphamari | 663 | 160 | 146 |
| Total | 2,957 | 790 | 567 |
Table 3. Coefficient value and RR for SPI Category and Selected cause mortality in Dinajpur.
| 3-SPI | 3-SPI 1 Lag | |||||||||||
| Drought Category | All cause | Cardio | Respiratory | All cause | Cardio | Respiratory | ||||||
| CV | RR | CV | RR | CV | RR | CV | RR | CV | RR | CV | RR | |
| ED | – | – | – | – | – | – | – | – | – | – | – | – |
| SD | 0.16 | 1.18 | –0.03 | 0.97 | 0.06 | 1.06 | 0.22 | 1.24 | 0.38 | 1.46 | –0.22 | 0.80 |
| MOD | 0.06 | 1.06 | 0.18 | 1.20 | 0.42** | 1.53 | –0.32* | 0.73 | –0.24 | 0.79 | –0.11 | 0.90 |
| MD | 0.05 | 1.05 | 0.38* | 1.46 | –0.27 | 0.76 | –0.10 | 0.91 | 0.13 | 1.14 | –0.27 | 0.76 |
| Temp | –0.04** | 0.96 | –0.03 | 0.97 | –0.06** | 0.94 | –0.04** | 0.96 | –0.04* | 0.96 | –0.06** | 0.95 |
| Humidity | 0.00 | 1.00 | –0.02 | 0.98 | 0.01 | 1.01 | 0.00 | 1.00 | –0.02 | 0.98 | 0.01 | 1.01 |
| 12-SPI | 12-SPI 1 Lag | |||||||||||
| ED | – | – | – | – | – | – | – | – | – | – | – | – |
| SD | –0.10 | 0.91 | –0.23 | 0.79 | –0.33 | 0.72 | 0.05 | 1.05 | –0.22 | 0.80 | –0.11 | 0.90 |
| MOD | –0.13 | 0.88 | 0.52 | 1.68 | –0.60 | 0.55 | –0.08 | 0.92 | 0.62* | 1.86 | –0.40 | 0.67 |
| MD | 0.04 | 1.04 | 0.50* | 1.65 | –0.08 | 0.93 | 0.08 | 1.08 | 0.56* | 1.76 | –0.12 | 0.89 |
| Temp | –0.04** | 0.96 | –0.04 | 0.97 | –0.06** | 0.95 | –0.04** | 0.96 | –0.04* | 0.97 | –0.05** | 0.95 |
| Humidity | 0.00 | 1.00 | –0.02 | 0.98 | 0.01 | 1.01 | 0.00 | 1.00 | –0.02 | 0.98 | 0.01 | 1.01 |
*P < 0.05, **P < 0.01, No drought used as reference. CV, coefficient value; Ed, extreme drought; MD, mild drought; MOD, moderate drought; RR, relative risk; SD, severe drought; Temp, temperature; 3-SPI, short-term drought; 3-SPI 1 Lag, 3-month preceding SPI; 12-SPI, long-term drought; 12-SPI 1 Lag, 12-month preceding SPI.
Table 5. Coefficient value and RR for SPI Category and Selected cause mortality in Nilphamari.
| 3-SPI | 3-SPI 1 Lag | |||||||||||
| Drought Category | All cause | Cardio | Respiratory | All cause | Cardio | Respiratory | ||||||
| CV | RR | CV | RR | CV | RR | CV | RR | CV | RR | CV | RR | |
| ED | 0.49* | 1.63 | 0.46 | 1.59 | 0.69 | 1.99 | 0.40 | 1.49 | –0.06 | 0.94 | 0.69 | 1.99 |
| SD | –0.60 | 0.55 | –0.02 | 0.98 | –1.11 | 0.33 | 0.03 | 1.03 | 0.28 | 1.32 | –0.97 | 0.38 |
| MOD | –0.08 | 0.93 | 0.10 | 1.11 | –0.05 | 0.96 | 0.08 | 1.08 | 0.23 | 1.25 | –0.08 | 0.92 |
| MD | –0.07 | 0.94 | 0.02 | 1.02 | 0.05 | 1.05 | 0.01 | 1.01 | –0.20 | 0.82 | 0.18 | 1.19 |
| Temp | –0.04** | 0.96 | –0.02 | 0.98 | –0.04 | 0.96 | –0.05** | 0.96 | –0.03 | 0.97 | –0.04 | 0.96 |
| Humidity | 0.01 | 1.01 | 0.02 | 1.02 | –0.02 | 0.98 | 0.01 | 1.01 | 0.02 | 1.02 | –0.01 | 0.99 |
| 12-SPI | 12-SPI 1 Lag | |||||||||||
| ED | – | – | – | – | – | – | – | – | – | – | – | – |
| SD | –0.23 | 0.79 | –0.09 | 0.91 | –0.16 | 0.85 | –0.28 | 0.75 | –0.05 | 0.95 | –0.44 | 0.64 |
| MOD | –0.30 | 0.74 | –0.35 | 0.70 | –0.91 | 0.40 | 0.18 | 1.19 | –0.20 | 0.82 | 0.51 | 1.67 |
| MD | –0.09 | 0.91 | 0.17 | 1.18 | 0.26 | 1.30 | –0.08 | 0.92 | 0.25 | 1.29 | 0.23 | 1.26 |
| Temp | –0.05** | 0.96 | –0.01 | 0.99 | –0.04 | 0.96 | –0.05** | 0.95 | –0.02 | 0.98 | –0.05** | 0.95 |
| Humidity | 0.01 | 1.01 | 0.02 | 1.02 | –0.01 | 0.99 | 0.01 | 1.01 | 0.02 | 1.03 | –0.02 | 0.98 |
*P < 0.05, **P < 0.01, No drought used as reference. CV, coefficient value; Ed, extreme drought; MD, mild drought; MOD, moderate drought; RR, relative risk; SD, severe drought; Temp, temperature; 3-SPI, short-term drought; 3-SPI 1 Lag, 3-month preceding SPI; 12-SPI, long-term drought; 12-SPI 1 Lag, 12-month preceding SPI.
Table 4. Coefficient value and RR for SPI Category and Selected cause mortality in Rangpur.
| 3-SPI | 3-SPI 1 Lag | |||||||||||
| Drought Category | All cause | Cardio | Respiratory | All cause | Cardio | Respiratory | ||||||
| CV | RR | CV | RR | CV | RR | CV | RR | CV | RR | CV | RR | |
| ED | 0.39* | 1.47 | 0.12 | 1.13 | 0.12 | 0.90 | 0.16 | 1.17 | 0.24 | 1.27 | 0.16 | 1.17 |
| SD | 0.36** | 1.43 | 0.17 | 1.18 | 0.17 | 0.84 | 0.44** | 1.55 | 0.36 | 1.44 | 0.20 | 1.23 |
| MOD | –0.29** | 0.75 | –0.52* | 0.60 | –0.52 | 1.12 | –0.07 | 0.93 | –0.24 | 0.79 | –0.30 | 0.74 |
| MD | –0.08 | 0.92 | –0.39** | 0.68 | –0.39 | 1.14 | 0.05 | 1.05 | –0.09 | 0.92 | 0.06 | 1.06 |
| Temp | –0.03** | 0.97 | –0.04* | 0.97 | –0.04 | 1.00 | –0.03** | 0.97 | –0.04** | 0.97 | 0.00 | 1.00 |
| Humidity | 0.00 | 1.00 | 0.00 | 1.00 | 0.00 | 1.00 | 0.00 | 1.00 | –0.01 | 0.99 | –0.01 | 0.99 |
| 12-SPI | 12-SPI 1 Lag | |||||||||||
| ED | – | – | – | – | – | – | – | – | – | – | – | – |
| SD | 0.12 | 1.13 | 0.18 | 1.20 | 0.23 | 1.25 | 0.04 | 1.04 | 0.17 | 1.19 | 0.30 | 1.35 |
| MOD | –0.22* | 0.81 | –0.73** | 0.48 | –0.02 | 0.98 | –0.17 | 0.84 | –0.54** | 0.58 | 0.17 | 1.18 |
| MD | –0.21** | 0.81 | –0.31** | 0.73 | 0.01 | 1.01 | –0.18** | 0.84 | –0.36** | 0.70 | –0.07 | 0.93 |
| Temp | –0.03** | 0.97 | –0.03* | 0.97 | 0.00 | 1.00 | –0.03** | 0.97 | –0.03* | 0.97 | 0.00 | 1.00 |
| Humidity | 0.00 | 1.00 | 0.00 | 1.00 | 0.00 | 1.00 | 0.00 | 1.00 | 0.00 | 1.00 | –0.01 | 0.99 |
*P < 0.05, **P < 0.01, No drought used as reference. CV, coefficient value; Ed, extreme drought; MD, mild drought; MOD, moderate drought; RR, relative risk; SD, severe drought; Temp, temperature; 3-SPI, short-term drought; 3-SPI 1 Lag, 3-month preceding SPI; 12-SPI, long-term drought; 12-SPI 1 Lag, 12-month preceding SPI.
In Dinajpur, no extreme drought occurred during the study period, and no impact from severe drought was found for any timescale. Short-term moderate drought exacerbated mortality from respiratory diseases (RR = 1.527, 95% CI 1.015 to 2.297, P = 0.042). Both short-term and long-term mild drought exacerbated circulatory-related mortality (RR = 1.455, 95% CI 1.072 to 1.976, P = 0.016 and RR = 1.647, 95% CI 1.061 to 2.558, P = 0.026, respectively). For 3-SPI 1-month preceding SPI, moderate drought was associated with low natural cause mortality (RR = 0.730, 95% CI 0.574 to 0.926, P = 0.010), while for 12-SPI 1-month preceding SPI, mild and moderate drought exacerbated circulatory-related mortality (RR = 1.856, 95% CI 1.066 to 3.232, P = 0.014 and RR = 1.756, 95% CI 1.121to 2.751, 0.029, respectively).
In Nilphamari, only extreme drought had a strong impact on all three selected causes of mortality, with a significant impact on natural cause mortality (RR = 1.632, 95% CI 1.030 to 2.585, P = 0.037).
We also found that during drought periods, the temperature was negatively associated with mortality in all regions and for all timescales, indicating that low temperatures are associated with mortality. No impact of humidity found in our study area.
DISCUSSION
In this study, a greater impact on natural cause mortality was observed in Rangpur and Nilphamari, which experienced extreme droughts during the study period. Natural cause was associated with short-term drought in Rangpur and Nilphamari and Respiratory-related mortality was associated with short-term drought in Dinajpur. In both short-term and long-term droughts, there was a significant association between drought severity and circulatory-related mortality in Dinajpur. In Rangpur, mild and moderate drought were associated with low natural cause mortality. Other studies also suggested that extreme droughts likely to cause more harm6, 7, 10, 26, 46 which explains extreme drought impact on natural cause mortality and mild and moderate drought causing low natural cause mortality.
The other main finding of this study was that no extreme droughts occurred in Dinajpur, but there was long period of mild and moderate drought was associated with increased circulatory- and respiratory-related mortality. Extreme droughts effected the natural cause mortality, but in Dinajpur no extreme drought happened during the study period, so we could not find the impact on natural cause mortality. A previous study showed that drought conditions are associated with an increased risk of morbidity and mortality.14 The indirect effects of drought events on respiratory and circulatory system health and mortality have also been described.6 Studies suggest that the impacts of drought are difficult to identify, as many of the effects are diffuse and indirect, and they can be cumulative over time.6, 7 We also investigated the lag effect of drought in Rangpur and Dinajpur. The aftereffect of short-term drought impacted the natural cause mortality in Rangpur, and the aftereffect of long-term drought impacted circulatory-related mortality in Dinajpur. No aftereffects were identified for the Nilphamari area for the investigated period.
Northern Bangladesh is vulnerable to the frequency and intensity of droughts. Owing to human activities such as barrage and dam construction, northern Bangladesh is experiencing a process of desertification. The decrease in summer water flow causes sediment to be deposited in the riverbed downstream of dams, leading to hydraulic congestion in the rainy season.47 This causes decreased river flow and insufficient water supply, leading to changes in local water quality. The climate in northern Bangladesh has experienced increased drought.48 This reduction in local precipitation has increased the region’s vulnerability to extreme drought events which can explain the regional difference in our study area. Because these factors cannot be altered, drought will intensify in the future, with exacerbated health effects.
Drought is an indirect predictor that combines and represents the impact of this climate event. Many studies have individually considered several environmental factors (e.g., heat waves, forest fires, and pollution) that have important implications for mortality, especially for vulnerable populations. High temperatures are related to more severe drought,49, 50 and both high temperatures and drought conditions are related to dry soil, deforestation, the occurrence and severity of wildfires, dust storms, and conditions that lead to reduced air quality.51 All these drought-related events lead to an increase in dust, which carries pathogens and particulate matter, and increase the release of toxic aerosols in the atmosphere, which may also have adverse health effects.4, 11 The longer dry period in Dinajpur might explain the level of respiratory-related mortality found in our study.
No significant impact of humidity was found in the study area; however, temperature did have a negative impact, suggesting that when the temperature is low, mortality is exacerbated. Relatedly, several studies in Bangladesh identified a marked increase in all-cause mortality and deaths due to cardiovascular, respiratory, and perinatal causes at low temperatures.52,53,54 Studies suggests that winter excess mortality is not a consequence of seasonal low absolute temperatures but, rather, is a consequence of a seasonal fall in average temperature.53, 55 Data on cross-country thermal-efficiency standards in housing indicated that those countries with poorest housing demonstrated the highest excess winter mortality and poorest housing was more common in countries with mildest winter climate.56
To reduce health risks, it is necessary to promote comprehensive and proactive measures based on prevention, mitigation, and adaptation to drought, because of the multiple health effects associated with drought. It is especially important to develop comprehensive plans that include measures to minimize the effects described in this study. Surveillance systems and their associated action plans should be designed in consideration of the actual conditions of an area, such as the geographic location and the local public health characteristics of a population.
Drought conditions in nearby regions can also affect a populations’ well-being. Many factors can intensify the seriousness of drought and reinforce the risks identified with its frequency, such as the vulnerability of the population, their overall health status, sex, age, and socioeconomic characteristics, and accessibility to and utilization of water.7, 46, 57 In this study, however, we were unable to control for all these variables.
The daily mortality impacts of prolonged drought might be related to mental health factors, particularly in rural populations. Although we could not measure stress levels in this study, several studies have documented an association between drought and psychological stress, psychological distress, generalized anxiety, and depression; in extreme cases, drought might be a contributing factor to suicide.6, 14, 23, 29, 52 Several studies have linked stress to deterioration of the body’s regulatory systems. In particular, stress can be an important factor in respiratory tract infections and can promote cardiac pathogenic processes, such as myocardial ischemia and the activation of inflammatory and coagulation mechanisms.58, 59 Further studies are required to better understand whether stress is a casual effector in drought. While interpreting the results of this study, the following limitations should be taken into consideration. First, this study included only three districts of northern Bangladesh, which limits the ability to generalize the conclusions over the entire population of northern Bangladesh. Second, we applied a meteorological definition of drought. The impact of other types of drought (e.g., hydrological and agricultural) should be considered in future studies. Third, the data collection was random, and the cause of death classification was rather general and did not follow the International Classification of Diseases standards. Fourth, there were few meteorological stations in our study area, and there could be some differences in drought conditions in the areas furthest away from the stations. Fifth, we were unable to examine some variables that might affect vulnerability to drought, such as individual socioeconomic status, previous health conditions, adaptive capacity of the population, mental health status, sex, and age. A Future study with a large cohort, including a specific population, age standardization, socioeconomic data may advance our understanding of the impact between drought and selected cause mortality.
In conclusion, this study identified that the highest percentage of drought period occurred in Dinajpur for both the short and long-term timescales. Short-term drought, particularly extreme drought, had the strongest impact on mortality in Rangpur and Nilphamari. Regardless of the investigated timescale, in general, the drought period and the aftereffects of drought had a significant impact on natural cause, circulatory-related, and respiratory-related mortality. The effect of drought varied by region and mainly depended on the rainfall. This indicates that localities need to consider tailored approaches to understand the true impact of drought on human health, which would help authorities implement mitigation methods more effectively. This investigation found considerable variation in the mortality and drought characteristics across the studied regions, as well as different effects of short- and long-term droughts. Our findings will aid future analyses of different drought timescales for broader regions such as South Asia.
Acknowledgments
Acknowledgments: This study was partly funded by the Research Program of the International Platform for Dryland Research and Education, Tottori University. We thank Katherine Thieltges, from Edanz (https://jp.edanz.com/ac) for editing a draft of this manuscript.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Chowdhury MHK,Debsharma SK. Climate change in Bangladesh-A statistical review. Report on IOC-UNEP workshop on impacts of sea level rise due to global warming. NOAMI. 1992;16-9. Bangladesh. [Google Scholar]
- 2.Woodward A,Hales S,Weinstein P. Climate change and human health in the Asia Pacific region: who will be most vulnerable? Clim Res. 1998;11:31-8. 10.3354/cr011031 [DOI] [Google Scholar]
- 3.IPCC. 2014. In: Field CB, Barros VR, Dokken DJ, Mach KJ, Mastrandrea MD, Bilir TE, et al. editors. Climate change 2014: impacts, adaptation, and vulnerability. Part A: global and sectoral aspects. Contribution of working group II to the fifth assessment report of the Intergovernmental Panel on Climate Change. Cambridge University Press; 2014. p. 1132.
- 4.Bell JE,Brown CL,Conlon K,Herring S,Kunkel KE,Lawrimore J,et al. Changes in extreme events and the potential impacts on human health. J Air Waste Manag Assoc. 2018;68:265-87. 10.1080/10962247.2017.1401017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.UN-Water [Internet]. Drought management [cited 2020 Dec 5]. Available from: http://www.unwater.org/activities/multi-agency-featured-projects/drought-management/en/.
- 6.Berman JD,Ebisu K,Peng RD,Dominici F,Bell ML. Drought and the risk of hospital admissions and mortality in older adults in western USA from 2000 to 2013: a retrospective study. Lancet Planet Health. 2017;1:e17-25. 10.1016/S2542-5196(17)30002-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wilhite DA. Drought as a natural hazard: concepts and definitions. In: Wilhite, D, editor. Drought: A global assessment. London: Routledge; 2000. Vol. I, chap. 1. p. 3–18.
- 8.Rafiuddin M,Dash BK,Khanam F. Diagnosis of drought in Bangladesh using standardized precipitation index. Proceedings of the International Conference on Environment Science and Engineering; 2011. Apr 1–3; Bali Island, Indonesia.
- 9.Wilhite DA,Glantz MH. Understanding the drought phenomenon: the role of definitions. Water Int. 1985;10:111-20. 10.1080/02508068508686328 [DOI] [Google Scholar]
- 10.Stanke C,Kerac M,Prudhomme C,Medlock J,Murray V. Health effects of drought: a systematic review of the evidence. PLoS Curr. 2013;5:ecurrents.dis.7a2cee9e980f91ad7697b570bcc4b004. 10.1371/currents.dis.7a2cee9e980f91ad7697b570bcc4b004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Smith LT,Aragão LEOC,Sabel CE,Nakaya T. Drought impacts on children’s respiratory health in the Brazilian Amazon. Sci Rep. 2015;4:3726. 10.1038/srep03726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alpino TA,de Sena AR,de Freitas CM. Disasters related to droughts and public health - a review of the scientific literature. Cien Saude Colet. 2016;21:809-20. 10.1590/1413-81232015213.21392015 [DOI] [PubMed] [Google Scholar]
- 13.OBrien LV,Berry HL,Coleman C,Hanigan IC. Drought as a mental health exposure. Environ Res. 2014;131:181-7. 10.1016/j.envres.2014.03.014 [DOI] [PubMed] [Google Scholar]
- 14..Menne B,Bertollini R. The health impacts of desertification and drought. Down to Earth. 2000;14:4-6.
- 15.Aziz KMA,Hoque BA,Huttly S,Minnatullah KM,Hasan Z,Patwary MK,et al. Water supply, sanitation and hygiene sanitation report series no. 1. World Bank, Washington, District of Columbia. 1990; p. 99. Climate change and health in Bangladesh. Information brief. Ministry of Environment and Forests Government of the People’s Republic of Bangladesh. [Google Scholar]
- 16.Bouma MJ,Dye C. Cycles of malaria associated with El Niño in Venezuela. JAMA. 1997;278:1772-4. 10.1001/jama.1997.03550210070041 [DOI] [PubMed] [Google Scholar]
- 17.Habiba U,Shaw R,Takeuchi Y. Socioeconomic impact of droughts in Bangladesh. In: Shaw R, Nguyen H, editors. Droughts in Asian monsoon region: volume 8. Emerald Group Publishing Limited, Bingley. p. 25-48.
- 18.Cohen S,Janicki-Deverts D,Doyle WJ,Miller GE,Frank E,Rabin BS,et al. Chronic stress, glucocorticoid receptor resistance, inflammation, and disease risk. Proc Natl Acad Sci USA. 2012;109:5995-9. 10.1073/pnas.1118355109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hanigan IC,Butler CD,Kokic PN,Hutchinson MF. Suicide and drought in New South Wales, Australia, 1970-2007. Proc Natl Acad Sci USA. 2012;109:13950-5. 10.1073/pnas.1112965109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vins H,Bell J,Saha S,Hess J. The mental health outcomes of drought: a systematic review and causal process diagram. Int J Environ Res Public Health. 2015;12:13251-75. 10.3390/ijerph121013251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Barreau T,Conway D,Haught K,Jackson R,Kreutzer R,Lockman A,et al. Physical, mental, and financial impacts from drought in two California counties, 2015. Am J Public Health. 2017;107:783-90. 10.2105/AJPH.2017.303695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Edwards B,Gray M,Hunter BH. Social and economic impacts of drought on farm families and rural communities: submission to the Productivity Commission’s Inquiry into Government Drought Support. Melbourne, Victoria: Australian Institute of Family Studies; 2008. [Google Scholar]
- 23.Sena A,Barcellos C,Freitas C,Corvalan C. Managing the health impacts of drought in Brazil. Int J Environ Res Public Health. 2014;11:10737-51. 10.3390/ijerph111010737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Salvador C,Nieto R,Linares C,Díaz J,Gimeno L. Effects of droughts on health: Diagnosis, repercussion, and adaptation in vulnerable regions under climate change. Challenges for future research. Sci Total Environ. 2020;703:134912. 10.1016/j.scitotenv.2019.134912 [DOI] [PubMed] [Google Scholar]
- 25.Miyan MA. Droughts in Asian developed countries: vulnerability and sustainability. Weather Clim Extrem. 2015;7:8-23. 10.1016/j.wace.2014.06.003 [DOI] [Google Scholar]
- 26.Salvador C,Nieto R,Linares C,Diaz J,Gimeno L. Effects on daily mortality of droughts in Galicia (NW Spain) from 1983 to 2013. Sci Total Environ. 2019;662:121-33. 10.1016/j.scitotenv.2019.01.217 [DOI] [PubMed] [Google Scholar]
- 27.Mirzabaev A,Wu J,Evans J,et al. Desertification. In: Climate Change and Land. In: P.R. Shukla, J. Skea, E. Calvo Buendia, V. Masson-Delmotte, H.-O. Pörtner, D.C. Roberts, P. Zhai, R. Slade, S. Connors, R. van Diemen, M. Ferrat, E. Haughey, S. Luz, S. Neogi, M. Pathak, J. Petzold, J. Portugal Pereira, P. Vyas, E. Huntley, K. Kissick, M. Belkacemi, J. Malley, editors. IPCC special report on climate change, desertification, land degradation, sustainable land management, food security, and greenhouse gas fluxes in terrestrial ecosystems [cited 2020 Dec 15]. Available from: https://www.ipcc.ch/site/assets/uploads/2019/11/SRCCL-Full-Report-Compiled-191128.pdf
- 28.IPCC. Technical summary of climate change 2007: the physical science basis. In: Solomon S, et al. editors. Contribution of working group I to the fourth assessment report of the intergovernmental panel on climate change. Cambridge: Cambridge University Press; 2007.
- 29.IPCC. Climate change 2014: IPCC fifth assessment synthesis report-summary for policymakers-an assessment of inter-governmental panel on climate change. Cambridge: Cambridge University Press; 2014. [Google Scholar]
- 30.Shahid S,Behrawan H. Drought risk assessment in the western part of Bangladesh, natural hazards. Journal of the International Society for the Prevention and Mitigation of Natural Hazards. 2008;46:391-413. [Google Scholar]
- 31.Brammer H. Drought in Bangladesh: lessons for planners and administrators. Disasters. 1987;11:21-9. 10.1111/j.1467-7717.1987.tb00611.x [DOI] [Google Scholar]
- 32.Rahman MR,Lateh H. Climate change in Bangladesh: a spatio-temporal analysis and simulation of recent temperature and rainfall data using GIS and time series analysis model. Theor Appl Climatol. 2017;128:27-41. 10.1007/s00704-015-1688-3 [DOI] [Google Scholar]
- 33.Shahid S. Recent trends in the climate of Bangladesh. Clim Res. 2010;42:185-93. 10.3354/cr00889 [DOI] [Google Scholar]
- 34.Shahid S,Chen X,Hazarika MK. Assessment aridity of Bangladesh using geographic information center, Dhaka, Bangladesh. 2005. [Google Scholar]
- 35.Al-Mamun A,Rahman MNF,Aziz MA,Qayum MA,Hossain MI,et al. Identification of meteorological drought prone area in Bangladesh using standardized precipitation index. J Earth Sci Clim Change. 2018;9:457. 10.4172/2157-7617.1000457 [DOI] [Google Scholar]
- 36.Dey NC,Alam MS,Sajjan AK,Bhuiyan MA,Ghose L,Ibaraki Y,et al. Assessing environmental and health impact of drought in the northwest Bangladesh. J Environ Sci Nat Resour. 2012;4:89-97. 10.3329/jesnr.v4i2.10141 [DOI] [Google Scholar]
- 37.Shahid S,Behrawan H. Drought risk assessment in the western part of Bangladesh. Nat Hazards. 2008;46:391-413. 10.1007/s11069-007-9191-5 [DOI] [Google Scholar]
- 38..BBS, Statistics and Informatics Division (SID), Ministry of Planning BBS. Report on Bangladesh sample vital statistics, (2007-2017). 2016.
- 39.Rangpurdivision.gov.bd. [Internet]. Bangladesh [cited 2020 Dec 22]. Available from: http://www.rangpurdiv.gov.bd/site/page/7be6d41d-18fd-11e7-9461-7
- 40.Patel NR,Chopra P,Dadhwal VK. Analyzing spatial patterns of meteorological drought using standardized precipitation index. Meteorol Appl. 2007;14:329-36. 10.1002/met.33 [DOI] [Google Scholar]
- 41.Edwards DC,McKee TB. Characteristics of 20th century drought in the United States at multiple time scales. Climatology Report 97-2. Fort Collins: Department of Atmospheric Science, Colorado State University; 1997.
- 42..Thom HCS. Some methods of climatological analysis. WMO Technical Note Number 81 Secretariat of the World Meteorological Organization, Geneva, Switzerland, 1966, p 53
- 43.Abramowitz M,Stegun IA. Handbook of mathematical function. New York: Dover Publications; 1965. p. 1046. [Google Scholar]
- 44.Svoboda M,Fuchs BA. World Meteorological Organization and Global Water Partnership. Handbook of drought indicators and indices. Integrated Drought Management Programme. Geneva: Integrated Drought Management Tools and Guidelines Series 2; 2016. [Google Scholar]
- 45.Agnew CT. Using the SPI to identify drought [Internet]. Drought Network News (1994–2001). 2000. Available from: http://digitalcommons.unl.edu/droughtnetnews/1.
- 46.Wilhite DA,Svoboda MD,Hayes MJ. Understanding the complex impacts of drought: A key to enhancing drought mitigation and preparedness. Water Resour Manage. 2007;21:763-74. 10.1007/s11269-006-9076-5 [DOI] [Google Scholar]
- 47.Abdullah HM. Water harvest for drought resilient agriculture: prospects and possibilities in Bangladesh [Internet]. Proceedings of the IARU Sustainability Science Congress; 2014. Oct 21–23. Denmark: University of Copenhagen. Available from: http://sustainability.ku.dk/sustainabilitylectures/previous/iarucongress2014/
- 48.Alam K. Farmers’ adaptation to water scarcity in drought-prone environments: A case study of Rajshahi District, Bangladesh. Agric Water Manage. 2015;148:196-206. 10.1016/j.agwat.2014.10.011 [DOI] [Google Scholar]
- 49.Bandyopadhyay N,Bhuiyan C,Saha AK. Heat waves, temperature extremes and their impacts on monsoon rainfall and meteorological drought in Gujarat, India. Nat Hazards. 2016;82:367-88. 10.1007/s11069-016-2205-4 [DOI] [Google Scholar]
- 50.Sapionini J,Vogt JV,Naumann G,Barbosa P,Dosio A. Will drought events become more frequent and severe in Europe? Int J Climatol. 2017;38. 10.1002/joc.5291 [DOI] [Google Scholar]
- 51.Yusa A,Berry P,J Cheng J,Ogden N,Bonsal B,Stewart R,et al. Climate change, drought, and human health in Canada. Int J Environ Res Public Health. 2015;12:8359-412. 10.3390/ijerph120708359 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hashizume M,Wagatsuma Y,Hayashi T,Saha SK,Streatfield K,Yunus M. The effect of temperature on mortality in rural Bangladesh—a population-based time-series study. Int J Epidemiol. 2009;38:1689-97. 10.1093/ije/dyn376 [DOI] [PubMed] [Google Scholar]
- 53.Burkart K,Khan MH,Krämer A,Breitner S,Schneider A,Endlicher WR. Seasonal variations of all-cause and cause-specific mortality by age, gender, and socioeconomic condition in urban and rural areas of Bangladesh. Int J Equity Health. 2011;10:32. 10.1186/1475-9276-10-32 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Alam N,Lindeboom W,Begum D,Kim Streatfield P. The association of weather and mortality in Bangladesh from 1983–2009. Glob Health Action. 2012;5: 53-60. 10.3402/gha.v5i0.19121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Burkart K,Schneider A,Breitner S,Khan MH,Krämer A,Endlicher W. The effect of atmospheric thermal conditions and urban thermal pollution on all-cause and cardiovascular mortality in Bangladesh. Environ Pollut. 2011;159:2035-43. 10.1016/j.envpol.2011.02.005 [DOI] [PubMed] [Google Scholar]
- 56.Healy JD. Excess winter mortality in Europe: a cross country analysis identifying key risk factors. J Epidemiol Community Health. 2003;57:784-9. 10.1136/jech.57.10.784 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ebi KL,Bowen K. Extreme events as sources of health vulnerability: drought as an example. Weather Clim Extrem. 2016;11:95-102. 10.1016/j.wace.2015.10.001 [DOI] [Google Scholar]
- 58.Vida C,González E,Fuente M. Increase of oxidation and inflammation in nervous and immune systems with aging and anxiety. Curr Pharm Des. 2014;20:4656-78. 10.2174/1381612820666140130201734 [DOI] [PubMed] [Google Scholar]
- 59.von Känel R,Mills PJ,Fainman C,Dimsdale JE. Effects of psychological stress and psychiatric disorders on blood coagulation and fibrinolysis: a biobehavioral pathway to coronary artery disease? Psychosom Med. 2001;63:531-44. 10.1097/00006842-200107000-00003 [DOI] [PubMed] [Google Scholar]