Abstract
Objective:
Research examining the prevalence and severity of eating-related psychopathology in transgender and gender nonbinary individuals is limited. This study examined how identity development and minority stress relate to the presence of disordered eating behaviors and cognitions in transgender and gender nonbinary individuals, and improvement at one-year follow-up.
Methods:
Data come from a multi-site, longitudinal study of transgender and gender nonbinary individuals (n=287) and includes assessment of transgender congruence, receipt of gender-affirming care, minority stress, and disordered eating symptoms. Hierarchical multivariable logistic regression was used to test for associations between identity development, minority stress, and eating-related psychopathology.
Results:
Eighty-three participants (28.9%) met criteria for current eating-related psychopathology. Loss of control eating was the most commonly endorsed behavior, followed by laxative, diuretic, or other medication use, and compulsive exercise. Higher transgender congruence was associated with lower odds of disordered eating symptoms (OR = 0.72, 95% CI 0.55 – 0.94), whereas increased internalized transphobia was associated with greater odds of disordered eating symptoms (OR = 1.41, 95% CI = 1.04 – 1.91). Participants with eating-related psychopathology had greater odds of having received gender-affirming psychotherapy in the year prior to assessment (OR = 2.33, 95% CI = 1.32 – 4.14).
Conclusions:
Results suggest that gender identity development and internalized transphobia are associated with eating-related psychopathology in transgender and gender nonbinary individuals. Mental health providers should consider assessing all transgender and gender nonbinary individuals for eating-related psychopathology and unique risk factors associated with disordered eating, including low transgender congruence and internalized transphobia.
Keywords: transgender, nonbinary, eating disorders, minority stress
1. Introduction
Research examining eating-related psychopathology among transgender people is limited; studies to date suggest that transgender and gender nonbinary individuals experience lower body satisfaction1–3 and higher rates of disordered eating behaviors and cognitions4–8 relative to cisgender individuals. Existing data come largely from studies focused on transgender youth2,5,6 or do not include individuals who have received gender-affirming medical interventions.3 The prevalence and severity of eating-related psychopathology in transgender and gender nonbinary adults, and across stages of gender identity development, remains poorly characterized.
There are several potentially important factors emerging from the literature on eating-related psychopathology and transgender individuals. First is whether an individual has undergone gender-affirming interventions, such as hormone therapy and/or surgery. Those who receive such interventions tend to report fewer eating disorder symptoms and less body dissatisfaction than those who have not.9,10 Second, minority stress, defined as the additional stress experienced by marginalized groups due to stigma and discrimination, is associated with increased body image concerns and disordered eating behaviors in transgender youth5 and adults,11,12 and disproportionately high rates of mental health issues overall.13–17 Together, these findings suggest that transgender congruence (i.e., congruence between gender identity and expression) and minority stress may relate to the presence and severity of eating-related psychopathology. Notably, the majority of studies examining eating-related psychopathology in the transgender population focus on binary transgender individuals (i.e., individuals who identify as women who were assigned male at birth, and vice versa). However, gender nonbinary individuals (i.e., individuals who identify as neither discretely woman or man) have been found to report higher levels of minority stress and increased psychological distress, including disordered eating, relative to binary transgender individuals.17,18
The aim of this study was to examine risk factors for eating-related psychopathology among transgender and gender nonbinary individuals. We first describe the prevalence of eating disorder-related symptoms in the sample, including how identification as transgender (i.e., transgender man or woman) or gender nonbinary impacts the presence or absence of symptoms. Building from existing research, we hypothesized that, (1) transgender congruence would be inversely related to eating-related psychopathology, (2) history of gender-affirming medical interventions would be associated with less disordered eating symptoms, and (3) minority stress would be predictive of eating-related psychopathology. Using longitudinal data, we explored how identity development and minority stress factors relate to changes in eating-related psychopathology over time.
2. Methods
2.1. Participants
This study is a secondary analysis of data from two consecutive years of Project AFFIRM, a multi-site, longitudinal cohort study of a community sample of transgender and gender nonbinary individuals ages 16 and older (R01-HD079603). Eating-related data was not collected during the first year of the parent study, thus we consider Year 2 as “baseline” and Year 3 as “one-year follow-up.” Study participants were fluent in English or Spanish and recruited in New York, San Francisco, and Atlanta using five venue categories (public spaces/commercial establishments; community events and groups; social media; transgender-specific healthcare clinics (excluding mental health clinics); and word of mouth. Enrollment was stratified by age, gender identity, and site. Exclusion criteria included cognitive impairment, inability/unwillingness to provide follow-up contact information, and plans to leave the study region within three years. Data were collected using structured interviews conducted by trained interviewers in each city. Informed consent for participation in the parent study was obtained for all participants over age 18 and informed assent was obtained for individuals under 18 years. The requirement for parental consent was waived due to potential risk related to disclosure of gender identity.
2.2. Measures
2.2.1. Demographics
Age and race/ethnicity were assessed using 2010 U.S. Census measures (2010). Sex assigned at birth was assessed by asking, “What sex were you assigned at birth (on your original birth certificate)?” Participants identified their current gender identity by selecting from one of the following options: “Woman”, “Man”, “Transgender woman/Male-to-Female (MTF)”, “Transgender man/Female-to-Male (FTM)”, “Non-binary”, “Genderqueer”, or “Another”. For multivariable analyses, gender identity was condensed into three groups: transgender woman (TGF), transgender man (TGM), and gender nonbinary. For descriptive purposes, individuals identifying as gender nonbinary were dichotomized according to sex assigned at birth: Nonbinary- Assigned Female at Birth (NB-AFAB) and Nonbinary – Assigned Male at Birth (NB-AMAB). BMI was calculated using participant self-report of current weight and height.
2.2.2. Eating-related psychopathology
To assess disordered thinking about weight and dietary restraint, participants were asked questions derived from weight concern and restraint subscales of the Eating Disorder Examination19, including “In the past year, has your weight (number on the scale) influenced how you think about (judge) yourself as a person?” and “In the past year, have you deliberately tried to limit the amount of food you eat to influence your weight or shape (whether or not you have succeeded)?” Participants were also asked, “Do you believe yourself to be fat when others say you are too thin?” This item was derived from the SCOFF20, a screening tool designed to evaluate for core features of eating disorders.20–23 Participants were asked whether they had a lifetime history of disordered eating behaviors, including loss of control (LOC) eating, self-induced vomiting, use of laxatives, diuretics or other medications to control shape or weight, or compulsive exercise. Those reporting a positive history were asked about behavior frequency during the prior 28 days.
2.2.3. Identity development
Transgender congruence was assessed using the Transgender Congruence Scale (TCS).24 This 12-item self-report measure consists of the Appearance Congruence subscale (9 items), reflecting the degree to which individuals feel their external appearance represents their gender identity, and the Gender Identity Acceptance subscale (3 items), measuring the extent to which transgender individuals have accepted the gender identity they perceive themselves to be. Internal consistency was shown to be excellent for the total TCS (Cronbach’s α = 0.92), excellent for the Appearance Congruence subscale (Cronbach’s α = 0.94), and acceptable for the Gender Identity Acceptance subscale (Cronbach’s α = 0.77) in a community sample of transgender individuals.24 Participants were also asked to indicate whether or not they had received (1) prior gender-affirming surgical interventions, or (2) gender-affirming hormones or (3) gender-affirming psychotherapy during the past year.
2.2.4. Minority stress
Enacted stigma (ES) was assessed using a 10-item version of the Everyday Discrimination Scale,25 which measures the prevalence, frequency, and perceived underlying motivation of chronic, routine, and relatively subtle experiences of discriminatory treatment in social situations. An affirmative response to an experience of discrimination for which gender identity or expression was perceived as the underlying motive was counted towards the ES score (ranging from 0–10). Internal consistency of the Everyday Discrimination Scale in the parent study was 0.81 (Cronbach’s α). Felt stigma (FS), which reflects expectations of being stereotyped or discriminated against, was measured using a 10-item adaptation of the Stigma Consciousness Questionnaire,26 which asks participants to indicate agreement with statements such as “Most non-transgender individuals have a problem viewing transgender individuals as equals” using a 7-point Likert scale. Higher scores indicate increased levels of FS. This measure demonstrated good internal consistency (Cronbach’s α = 0.77). The Transgender Identity Survey (TIS)27 is a 26-item questionnaire of internalized transphobia, defined as the degree of discomfort with one’s transgender identity as a result of internalizing society’s normative gender expectations. The TIS global score has demonstrated excellent internal consistency in transgender samples (Cronbach’s α = 0.90).27
2.2.5. Other measures
Anxiety was assessed using the Brief Symptom Inventory (BSI)-18.28 Participants indicate whether they experienced specific symptoms during the past 7 days on a 5-point Likert scale ranging from 0 – 4. Internal consistency of the anxiety subscale was 0.89 (Cronbach’s alpha) in a community sample of transgender individuals.29
2.2.6. Statistical Analysis
Means and standard deviations were calculated for demographics and baseline measures of eating-related psychopathology. Independent samples t-tests and chi-square analyses were used to test for differences between individuals with and without eating-related psychopathology, and between TGF, TGM, and gender nonbinary participants. To minimize the risk of over-pathologizing occasional aberrant eating behavior, eating-related psychopathology was defined as at least one disordered eating behavior (LOC eating, purging, laxative, diuretic or other medications to control shape or weight, or compulsive exercise) during the prior month and the endorsement of weight concern. Hierarchical multivariable logistic regression was used to test for associations between transgender congruence, receipt of gender-affirming medical and psychotherapeutic care, internalized transphobia, ES, and FS with eating-related psychopathology. The first level (Model A) of the stepwise logistic regression included age, current gender identity (TGF, TGM, gender nonbinary), and anxiety. Anxiety was included because prior research has shown that differences in eating disorder psychopathology between individuals taking and not taking gender-affirming hormones were not found when anxiety was controlled for.9 Model B added measures of identity development, including transgender congruence, lifetime history of gender-affirming surgery, and receipt of gender-affirming hormones or psychotherapy during the past year. Model C included measures of minority stress. VIF and tolerance statistics were used to test for multicollinearity. Independent samples t-tests and chi-squares were used to compare demographic and clinical characteristics of participants with and without improved eating-related psychopathology at follow-up. Data were analyzed using SPSS Version 26 (IBM Corp., 2019).
3. Results
3.1. Baseline demographics
See Table 1 for demographics and non-eating related clinical characteristics. One participant was excluded from baseline assessments due to incomplete data, resulting in a sample of 287. 40.4% (n=116) identified as TGF, 32.4% (n=93) as TGM, and 27.3% (n=78) as gender nonbinary. Among nonbinary participants, 69.2% (n=54) were NB-AFAB and 30.8% (n=24) were NB-AMAB.
Table 1.
Demographics and Clinical Characteristics (n=287)
| Mean ± SD or n (%) | Range | |
|---|---|---|
|
| ||
| Age (years) | 35.6 ± 13.3 | 17–81 |
| BMI (kg/m2) | 28.0 ± 7.1 | 15.8 – 60.35 |
| Sex assigned at birth | ||
| Female | 146 (50.9) | |
| Male | 141 (49.1) | |
| Race/ethnicity | ||
| White/non-Hispanic | 138 (48.1) | |
| Hispanic/Latino | 54 (18.8) | |
| African American | 45 (15.7) | |
| Other | 47 (16.4) | |
| Current Gender Identity | ||
| Woman | 39 (13.6) | |
| Man | 19 (6.6) | |
| Transgender woman/Male-to-female (MTF) | 77 (26.8) | |
| Transgender man/Female-to-male (FTM) | 74 (25.8) | |
| Non-binary | 41 (14.3) | |
| Genderqueer | 34 (11.8) | |
| Another | 3 (1.0) | |
| Transgender Congruence Scale (total) | 5.0 ± 1.2 | 1.58 – 7.00 |
| TCS Appearance Congruence subscale | 4.5 ± 0.87 | 1.67 – 6.67 |
| TCS Gender Identity Acceptance subscale | 4.7 ± 0.55 | 2.00 – 6.67 |
| Past year gender-affirming hormone treatment | 226 (78.7) | |
| Past year puberty blocking hormones | 11 (3.8) | |
| Lifetime gender-affirming surgery | 181 (63.1) | |
| Past year gender-affirming psychotherapy | 132 (46) | |
| Transgender Identity Survey | 3.4 ± 0.99 | 1.42 – 6.38 |
| Enacted Stigma | 2.07 ± 2.3 | 0.0 –10.0 |
| Felt Stigma | 4.9 ± 1.00 | 1.9 – 6.9 |
Note: Race/ethnicity data is missing for 3 participants. BMI data is missing for 2 participants.
Relative to TGF and TGM participants, gender nonbinary individuals reported greater anxiety (F(2,286) = 7.2, p = 0.001) and lower transgender congruence (F (2,286) = 27.0, p < 0.001), including lower scores on the TCS Appearance Congruence subscale (F(1,286) = 27.4, p < 0.001). TGF and TGM participants did not differ on these measures. Fewer gender nonbinary participants reported taking gender-affirming hormones (TGF: n=102 (87.9%); TGM: n=88 (94.6%); nonbinary: n =32 (41%); X2(2) = 69.4, p < 0.001) or receiving gender-affirming surgery (TGF: n=87 (75%); TGM: n=62 (66.7%); nonbinary: n=32 (41%); X2(2) = 23.9, p < 0.001) than either TGF or TGM, but the groups did not differ in receipt of gender-affirming psychotherapy during the prior year (X2(2) = 2.9, p=0.24) and there were no differences between TGF and TGM participants in receipt of medical interventions. Gender nonbinary individuals reported more FS (F(1,286) = 7.6, p = 0.001) but less internalized transphobia (F(2,286) = 6.9, p = 0.001) than both TGF and TGM participants. TGM participants reported significantly less ES relative to both TGF and gender nonbinary participants (TGM: Mean 1.47±2.1; TGF: Mean 2.27±2.47; gender nonbinary: Mean: 2.49±2.14; F(2,286) = 5.0, p = 0.007).
3.2. Prevalence of disordered eating behaviors and cognitions
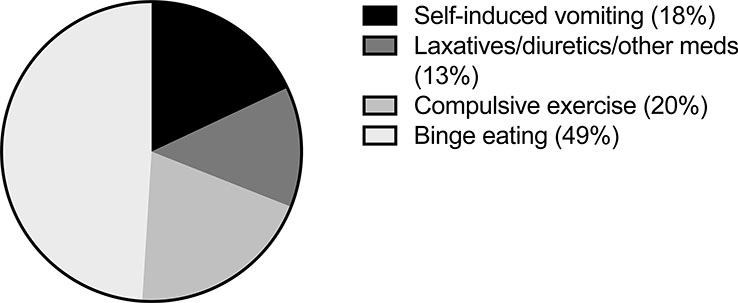
Approximately half of participants reported a lifetime history of ≥ 1 disordered eating behavior (n=153, 53.3%; See Figure 1). LOC eating was the most prevalent lifetime and current behavior reported, with 34.1% (n=98) of individuals endorsing ≥ 1 episode during the prior month and 14.9% (n=43) reporting ≥ 4 episodes. Eleven participants (3.8%) reported use of laxatives, diuretics, or other medications to control shape or weight during the prior month, and 2.8% (n=8) reported use on at ≥ 4 occasions. Ten individuals (3.5%) endorsed self-induced vomiting in the past month and 1.7% (n=5) had induced vomiting ≥ 4 times. Finally, 21 participants (7.3%) reported compulsively exercising during the prior month and 3.5% (n=10) endorsed ≥ 4 episodes. Over half of participants (56.4%, n=162) endorsed overvaluation of weight on self-concept in the past year, and 18.8% (n=54) endorsed belief that they were fat even though others said they were too thin. Shape and weight concerns were linked to eating behavior for 60.6% (n=174) of participants, who reported attempts to restrict their intake in an effort to change their shape or weight during the prior year.
Figure 1.
Lifetime history of disordered eating behaviors (% Total Sample, n=287).
More gender nonbinary participants reported a lifetime history of self-induced vomiting (X2(2) = 8.7, p = 0.013) than TGF or TGM individuals. The groups did not otherwise differ in the presence or frequency of disordered eating symptoms.
3.3. Comparison of participants with and without eating disorder-related symptoms at baseline
Eighty-three participants (28.9%) met criteria for current eating-related symptoms (see Table 2). Of this subgroup, 73.5% (n=61) were between 25 – 59 years old. Relative to participants without current symptoms, participants with eating-related psychopathology reported a higher prevalence of gender-affirming psychotherapy in the past year (X2(1) = 8.0, p = 0.005), a higher BMI (t(1,283)= −4.2, p <0.001), lower TCS appearance congruence (t(1,285) = 3.3, p = 0.001), and increased minority stress (see Table 2).
Table 2.
Bivariate comparison of baseline characteristics for transgender individuals with and without eating-related psychopathology
| No ED Symptoms (n=204) | ED Symptoms (n=83) | |||
|---|---|---|---|---|
| Mean/SD or n (%) | Mean/SD or n (%) | t(df) or X2(df) | p | |
|
| ||||
| Study Site | 1.5 (2) | 0.47 | ||
| Atlanta | 65 (31.9) | 32 (38.6) | ||
| New York | 67 (32.8) | 27 (32.5) | ||
| San Francisco | 72 (35.3) | 24 (28.9) | ||
| Age (years) | 36.0 ±13.7 | 34.8 ± 12.5 | 0.68 (285) | 0.50 |
| BMI (kg/m2) | 26.8 ± 6.6 | 30.6 ± 7.8 | −4.2 (283) | <0.001 |
| Sex assigned at birth | 1.85 (1) | 0.17 | ||
| Female | 109 (53.4) | 37 (44.6) | ||
| Male | 95 (46.6) | 46 (55.4) | ||
| Current Gender Identity | 3.1 (2) | 0.21 | ||
| Transgender woman (TGF) | 83 (40.6) | 33 (39.8) | ||
| Transgender man (TGM) | 71 (34.8) | 22 (26.5) | ||
| Gender Nonbinary | 50 (24.5) | 28 (33.7) | ||
| Race/ethnicity | 0.9 (3) | 0.82 | ||
| White/non-Hispanic | 101 (49.5) | 37 (44.6) | ||
| Hispanic/Latino | 38 (18.6) | 16 (19.3) | ||
| African American | 32 (15.7) | 13 (15.7) | ||
| Other | 31 (15.2) | 16 (19.3) | ||
| Transgender Congruence Scale (TCS) | 5.2 ± 1.2 | 4.6 ± 1.2 | 3.6 (285) | <0.001 |
| TCS Appearance Congruence subscale | 4.6 ± 0.8 | 4.2 ± 0.9 | 3.3 (285) | 0.001 |
| TCS Gender Identity Acceptance subscale | 4.7 ± 0.5 | 4.7 ± 0.6 | 0.7 (285) | 0.48 |
| Lifetime gender-affirming surgery | 128 (62.7) | 53 (63.8) | 0.03 (1) | 0.86 |
| Past year gender-affirming hormones | 164 (80.4) | 62 (74.7) | 11 (1) | 0.28 |
| Past year gender-affirming psychotherapy | 83 (40.7) | 49 (59.0) | 8.0 (1) | 0.005 |
| Transgender Identity Survey (TIS) | 3.3 ± 0.9 | 3.6 ± 1.1 | −2.5 (285) | 0.01 |
| Enacted Stigma | 1.9 ± 2.1 | 2.5 ± 2.7 | −2.0 (285) | 0.05 |
| Felt Stigma | 4.8 ±1.0 | 5.1 ± 1.0 | −2.1 (285) | 0.04 |
| BSI Anxiety | 56.2 ± 11.3 | 60.7 ± 11.2 | −2.7 (285) | 0.007 |
Note. Race/ethnicity data is missing for 2 participants in the No ED Symptoms group and 1 participant in the ED Symptoms group. BMI data is missing for 1 participant in the No-ED Symptoms category and 1 participant in the ED Symptoms category.
3.4. Predictors of eating-related psychopathology
Table 3 summarizes results of the hierarchical multivariable logistic regression examining predictors of eating-related psychopathology. In Model A, anxiety was associated with higher odds of eating-related psychopathology (OR = 1.03, 95% CI = 1.03 – 1.05). In Model B, higher transgender congruence was associated with lower odds of eating-related psychopathology (OR = 0.72, 95% CI 0.55 – 0.94), such that individuals who reported more congruence between their gender identity and external appearance were less likely to report eating-related symptoms. Neither prior gender-affirming surgery nor hormone therapy during the past year were associated with current eating-related psychopathology. However, individuals who had received gender-affirming psychotherapy during the preceding year were more likely to report eating-related symptoms (OR = 2.10, 95% CI = 1.20 – 3.68). In Model C, past-year gender-affirming psychotherapy (OR = 2.33, 95% CI = 1.32 – 4.14) and increased internalized transphobia (OR = 1.41, 95% CI = 1.04 – 1.91) were associated with greater odds of eating-related psychopathology.
Table 3.
Hierarchical multivariable logistic regression analyses among transgender individuals to identify factors associated with eating-related psychopathology (n=287).
| Model A (R2 = 0.04) | Model B (R2 = 0.12) | Model C (R2 = 0.14) | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| OR | 95%CI | OR | 95% CI | OR | 95% CI | |
| Age | 1.00 | 0.98 – 1.02 | 1.00 | 0.98 – 1.02 | 1.00 | 0.98 – 1.02 |
| Anxiety | 1.03 * | 1.03 – 1.05 * | 1.02 | 0.99 – 1.05 | 1.01 | 0.98 – 1.04 |
| Gender Identity (ref: Transgender woman) | ||||||
| Transgender man | 0.77 | 0.41 – 1.45 | 0.81 | 0.42 – 1.57 | 0.84 | 0.43 – 1.67 |
| Gender Nonbinary | 1.19 | 0.63 – 2.27 | 1.03 | 0.48 – 2.22 | 1.33 | 0.59 – 3.03 |
| Transgender Congruence Scale (total) | 0.72 * | 0.55 – 0.94 | 0.79 | 0.59 – 1.05 | ||
| Prior gender-affirming surgical intervention | 1.84 | 0.95 – 3.58 | 1.76 | 0.90 – 3.46 | ||
| Past year hormone treatment | 0.70 | 0.32 – 1.53 | 0.63 | 0.28 – 1.40 | ||
| Past year gender-affirming psychotherapy | 2.10 ** | 1.20 – 3.68 | 2.33 ** | 1.32 – 4.14 | ||
| Transgender Identity Scale (total) | 1.41 * | 1.04 – 1.91 | ||||
| Enacted Stigma | 1.03 | 0.89 – 1.18 | ||||
| Felt Stigma | 1.08 | 0.76 – 1.54 | ||||
p < 0.05
p < 0.01
3.5. Eating-related psychopathology at one-year follow-up
Twenty participants were lost to follow-up, leaving a sample of 267 participants with data at both time points. The participants lost to follow-up did not differ from those with follow-up data, with the exception of sex assigned at birth (X2(1) = 5.76, p = 0.02). Of participants with data at follow-up, 74 (27.7%) reported eating-related psychopathology at baseline and 35 individuals (47.3%) continued to report eating-related symptoms. Bivariate comparison of clinical characteristics, including age, BMI, sex assigned at birth, race/ethnicity, receipt of past-year gender-affirming medical or psychotherapeutic care, and factors related to identity development and minority stress, did not significantly differ between individuals with and without persistent symptoms at follow-up.
4. Discussion
A lifetime history of disordered eating symptoms was endorsed by over half of our sample, confirming the importance of continued study of eating-related psychopathology in this population. Consistent with our hypotheses, identity development and minority stress were associated with eating-related psychopathology. Individuals with lower transgender congruence and greater internalized transphobia were more likely to report eating disorder symptoms. We did not find an association between prior gender-affirming medical interventions and eating-related symptoms. However, receipt of gender-affirming psychotherapy was associated with the presence of current eating-related psychopathology.
4.1. Prevalence of eating disorder-related cognitions and behaviors
Consistent with prior research2,5, our sample reported increased shape and weight concerns and prevalence of disordered behaviors compared to established cisgender norms.30,31 LOC eating was the most commonly reported behavior, with approximately one third of participants reporting ≥ 1 episode during the past month, and 14.9% reporting ≥ 4 episodes. Compulsive exercise was the second most commonly endorsed behavior (with 3.5% of individuals reporting ≥ 4 episodes). This pattern is consistent with previous findings. Nagata et al.7 documented rates of objective binge episodes of 11 and 13% in transgender men and women, respectively, and found that 8% of participants endorsed compulsively exercising at least 20 days during the past month. Slight variability in prevalence of behaviors between studies may reflect differences in cohort demographics: whereas Nagata and colleagues’ cohort was predominantly white, our sample reflected greater ethnoracial diversity. Existing research highlights the presence of eating-related psychopathology across racial and/or ethnic groups.32–24 Our results provide further evidence of the need for universal screening for eating-related psychopathology.
4.2. Identity development and eating-related psychopathology
Consistent with our hypothesis, we found that less congruence between one’s external appearance and current gender identity was associated with higher odds of disordered eating symptoms. Yet, receipt of prior gender-affirming medical interventions was not associated with current eating-related psychopathology. This finding is surprising given that prior studies have found that gender-affirming medical interventions are associated with improvements in body satisfaction35–37 and eating disorder psychopathology.9,38,39 However, the majority of participants in the current study had previously received gender-affirming medical care at the time of assessment, thus potentially precluding the ability to detect a group difference.
Conversely, receipt of gender-affirming psychotherapy during the past year was associated with current eating-related psychopathology. We do not believe this finding reflects a causal relationship between psychotherapy and subsequent eating-related symptomatology, but rather suggests that these individuals may be struggling more and thus pursuing treatment. This underscores the importance of healthcare providers, and mental healthcare providers in particular, routinely assessing eating disorder-related symptoms. That nearly 75% of individuals who reported current eating-related psychopathology in the present study were between the ages of 25–59 further highlights that individuals presenting for mental healthcare should be screened for an eating disorder regardless of age. Indeed, it is possible that this finding reflects a healthcare system working well, in that individuals in need of treatment received it. However, it is unclear whether individuals’ eating disordered symptoms were addressed within the scope of the psychotherapy received.
4.3. Minority stress and eating-related psychopathology.
The positive association between minority stress and increased eating-related psychopathology is consistent with prior literature examining eating disorder-related symptoms in transgender individuals,12,17 and the broader literature examining mental health outcomes in transgender people.14–16,40,41 Our results suggest that internalized transphobia is a particular risk factor for the presence of eating disorder-related symptoms. Gender-affirming psychotherapy may help to reduce feelings of shame or alienation, which may in turn reduce disordered eating behaviors and cognitions. It may also provide a more direct pathway for screening and attending to eating disorder symptoms.
Prior research suggests that a nonbinary or genderqueer identity is associated with higher rates of minority stress and worse mental health outcomes.17,42 The results from the present study are less straightforward: while gender nonbinary participants endorsed more FS than the TGF and TGM groups, they reported lower internalized transphobia than both transgender groups, and differed from TGM but not TGF participants in the experience of ES. Further, the only eating-related difference was a higher lifetime prevalence of self-induced vomiting in the gender nonbinary group. Existing research examining the prevalence of self-reported eating disorders in gender nonconforming adults found that the odds of a prior diagnosis of anorexia nervosa or bulimia nervosa were significantly higher in gender nonbinary individuals assigned female at birth compared to transgender males, and marginally higher compared to transgender females.17 Further studies with a larger sample size are needed to clarify differences among nonbinary (assigned female versus assigned male at birth), TGM, and TGF with regard to eating disorder symptoms.
4.4. Clinical Implications
That nearly 60% of participants with eating-related psychopathology received gender-affirming psychotherapy during the prior year strongly supports the importance of universal screening for eating-related psychopathology in all transgender and gender nonbinary individuals. Knowledge of and comfort with eating disorders assessment is often limited for non-eating disorder specialists,43 but research has shown that improving eating disorders education can enhance providers’ confidence with screening and providing clinical care.44 This training may be especially useful for those already providing services to transgender and gender nonbinary individuals. Additional efforts in the dissemination of specialized eating disorders treatments for healthcare providers serving the transgender community is also warranted.
Gender-affirming psychotherapy offers an opportunity to target risk factors for eating-related psychopathology, such as internalized transphobia and low transgender congruence, by reducing feelings of shame or alienation, which may in turn reduce disordered eating behaviors and cognitions. LOC eating, the most commonly endorsed symptom in this study, is the hallmark of binge-eating disorder, which tends to respond nonspecifically and in tandem with improvement in general psychopathology, to a variety of psychotherapeutic approaches.45 It’s likely that gender-affirming psychotherapy, even if not specifically addressing disordered eating, may yield similar benefits. From a research perspective, these results highlight the need for culturally-adapted psychotherapeutic interventions which address the unique risk factors for eating-related psychopathology in trangender and gender nonbinary individuals.
4.4. Limitations
While a strength of this study is that is a large, multi-site, longitudinal project, it was not specifically designed to examine predictors of change in eating-related psychopathology. Some information was not collected at baseline and there were modifications in items assessing eating-related symptoms from one year to the next, limiting longitudinal comparisons. Given the nature of this longitudinal project, we were limited in the number of items that could be included to assess eating-related psychopathology, and our assessment of weight concern and restraint might have been improved by use of these full respective subscales of the EDE-Q. Additionally, this was not a probability sample, which could limit generalizability.
5. Conclusions
This longitudinal study of transgender and gender nonbinary adults investigated how identity development and minority stress relate to the presence of eating-related psychopathology. LOC eating was the most commonly endorsed disordered eating behavior, followed by laxative, diuretic, or other medication use, and compulsive exercise. Results indicate that transgender congruence and internalized transphobia were predictive of disordered eating symptoms. Individuals with eating-related psychopathology were more likely to have received gender-affirming psychotherapy, highlighting the importance of providers routinely evaluating eating disorder symptoms. Longitudinal research is needed to investigate how identify development and minority stress influence trajectories of illness in transgender and gender nonbinary individuals with eating disorder-related symptomatology.
Highlights:
Nearly one third of participants reported current eating-related psychopathology.
Greater congruence between current gender identity and external appearance was associated with lower odds of disordered eating behaviors and cognitions.
Increased internalized transphobia was associated with increased odds of eating-related symptoms.
Acknowledgements:
The authors would like to thank Project AFFIRM’s transgender community advisory board for their contribution to this study.
Role of Funding Sources: This work was supported by the National Institute of Health [R01-HD079603 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (Walter Bockting, PI) and T32 MH096679]. The NIH had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Conflicts of Interest: Dr. Glasofer has received honoraria from Oxford University Press. Dr. Attia serves as a Clinical Advisor to Equip Health, Inc., and receives royalties from UpToDate. Drs. Uniacke, Devlin, and Bockting report no conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bandini E, Fisher A, Castellini G, Lo Sauro C, Lelli L, Meriggiola M, Casale H, Benni L, Feruccio N, Faravelli C, Dettore D, Maggi M, Ricca V Gender Identity Disorder and Eating Disorders: Similarities and Differences in Terms of Body Uneasiness. J. Sex. Med. 10, 1012–1023 (2013). [DOI] [PubMed] [Google Scholar]
- 2.Diemer E, Grant J, Munn-Chernoff M, Patterson D, Duncan A Gender Identity, Sexual Orientation, and Eating-Related Pathology in a National Sample of College Students. J. Adolesc. Health 57, 144–9 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Witcomb G, Bouman W, Brewin N, Richards C, Fernandez-Aranda F, Arcelus J Body image dissatisfaction and eating-related psychopathology in trans individuals: A matched control study. Eur. Eat. Disord. Rev. 23, 287–293 (2015). [DOI] [PubMed] [Google Scholar]
- 4.Vocks S, Stahn C, Loenser K & Legenbauer T Eating and body image disturbances in male-to-female and female-to-male transsexuals. Arch. Sex. Behav. 38, 364–377 (2009). [DOI] [PubMed] [Google Scholar]
- 5.Watson R, Veale J, & Saewyc E Disordered eating behaviors among transgender youth: Probability profiles from risk and protective factors. Int. J. Eat. Disord. 50, 515–522 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guss C, Williams D, Reisner S, Austin S, & Katz-Wise S Disordered Weight Management Behaviors, Nonprescription Steroid Use, and Weight Perception in Transgender Youth. J. Adolesc. Heal. 60, 17–22 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nagata J, Murray S, Compte E, Pak E, Schauer R, Flentje A, Capriotti M, Lubensky M, Lunn M, Obedin-Maliver J Community norms for the Eating Disorder Examination Questionnaire (EDE-Q) among transgender men and women. Eat. Behav. 37, 101381 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Calzo J, Blashill A, Brown T, Argenal R Eating disorders and disordered weight and shape control behaviors in sexual minority populations. Curr Psychiatry Rep. 19 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jones B, Haycraft E, Bouman W, Brewin N, Claes L, Arcelus J Risk Factors for Eating Disorder Psychopathology within the Treatment Seeking Transgender Population: The Role of Cross-Sex Hormone Treatment. Eur. Eat. Disord. Rev. 26, 120–128 (2018). [DOI] [PubMed] [Google Scholar]
- 10.Jones B, Haycraft E, Murjan S & Arcelus J Body dissatisfaction and disordered eating in trans people: A systematic review of the literature. Int. Rev. Psychiatry 28, 81–94 (2016). [DOI] [PubMed] [Google Scholar]
- 11.Velez B, Breslow A, Brewster M, Cox R, Foster A Building a pantheoretical model of dehumanization with transgender men: Integrating objectification and minority stress theories. J. Couns. Psychol. 63, 497–508 (2016). [DOI] [PubMed] [Google Scholar]
- 12.Brewster M, Velez B, Breslow A, & Geiger E Unpacking body image concerns and disordered eating for transgender women: The roles of sexual objectification and minority stress. J. Couns. Psychol. 66, 131–142 (2019). [DOI] [PubMed] [Google Scholar]
- 13.Valente P, Schrimshaw E, Dolezal C, LeBlanc A, Singh A, Bockting W Stigmatization, Resilience, and Mental Health Among a Diverse Community Sample of Transgender and Gender Nonbinary Individuals in the U.S. Arch. Sex. Behav. 49, 2649–2660 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bockting W, Miner M, Swinburne Romine R, Hamilton A & Coleman E Stigma, mental health, and resilience in an online sample of the US transgender population. Am. J. Public Health 103, 943–951 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chodzen G, Hidalgo M, Chen D & Garofalo R Minority Stress Factors Associated With Depression and Anxiety Among Transgender and Gender-Nonconforming Youth. J. Adolesc. Heal. 64, 467–471 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuper L, Adams N & Mustanski B Exploring Cross-Sectional Predictors of Suicide Ideation, Attempt, and Risk in a Large Online Sample of Transgender and Gender Nonconforming Youth and Young Adults. LGBT Heal. 5, 391–400 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lefevor G, Boyd-Rogers C, Sprague B & Janis R Health disparities between genderqueer, transgender, and cisgender individuals: An extension of minority stress theory. J. Couns. Psychol. 66, 385–395 (2019). [DOI] [PubMed] [Google Scholar]
- 18.Diemer E, Hughto J, Gordon A, Guss C, Austin S, Reisner S Beyond the Binary: Differences in Eating Disorder Prevalence by Gender Identity in a Transgender Sample. Transgender Heal. 3, 17–23 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fairburn CG & Cooper Z The Eating Disorder Examination (12th edition). in Binge eating: Nature, assessment, and treatment (1993). [Google Scholar]
- 20.Morgan JF, Reid F, Lacey JH The SCOFF questionnaire. The Western Journal of Medicine. 172, 164 (2000). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Morgan JF, Reid F, Lacey JH The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ. 319, 1467–1468 (1999) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luck AJ, Morgan JF, Reid F, O’Brien A, Brunton J, Price C, Perry L, Lacey J et al. The SCOFF questionnaire and clinical interview for eating disorders in general practice: Comparative study. Br. Med. J. 325, 755–756 (2002). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Perry L, Morgan J, Reid F, Brunton J, O’Brien A, Luck A, Lacey H Screening for symptoms of eating disorders: Reliability of the SCOFF screening tool with written compared to oral delivery. Int. J. Eat. Disord. 32, 466–472 (2002). [DOI] [PubMed] [Google Scholar]
- 24.Kozee H, Tylka T & Bauerband L Measuring Transgender Individuals’ Comfort With Gender Identity and Appearance: Development and Validation of the Transgender Congruence Scale. Psychol. Women Q. 36, 179–196 (2012). [Google Scholar]
- 25.Williams D, Yan Y, Jackson J, & Anderson N Racial Differences in Physical and Mental Health: Socio-economic status, stress and discrimination. J. Health Psychol. 2, 335–351 (1997). [DOI] [PubMed] [Google Scholar]
- 26.Pinel E Stigma consciousness: The psychological legacy of social stereotypes. J. Pers. Soc. Psychol. 76, 114–128 (1999). [DOI] [PubMed] [Google Scholar]
- 27.Bockting W, Miner M, Romine R, Dolezal C, Robinson B, Rosser S, Coleman E The Transgender Identity Survey: A Measure of Internalized Transphobia. LGBT Heal. 7, 15–27 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Derogatis L The Brief Symptom Inventory: An Introductory Report. Psychol. Med. 13, 595–605 (1983). [PubMed] [Google Scholar]
- 29.Bockting W, Miner M, Swinburne R, Hamilton A, Coleman E Stigma, mental health, and resilience in an online sample of the US transgender population. AM J Public Health. 5, 943–951 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lavender J, De Young K, & Anderson D Eating Disorder Examination Questionnaire (EDE-Q): Norms for undergraduate men. Eat. Behav. 11, 119–121 (2010). [DOI] [PubMed] [Google Scholar]
- 31.Mond J, Hay P, Rodgers B & Owen C Eating Disorder Examination Questionnaire (EDE-Q): Norms for young adult women. Behav. Res. Ther. 44, 53–62 (2006). [DOI] [PubMed] [Google Scholar]
- 32.Franko D, Thompson-Brenner H, Thompson D, Boisseau C, Davis A, Forbush K, Roehrig J, Bryson S, Bulik C, Crow S, Devlin M, Gorin A, Grilo C, Kristeller J, Masheb R, Mitchell J, Peterson C, Safer D, Striegel R, Wilfley D, Wilson G Racial/ethnic differences in adults in randomized clinical trials of binge eating disorder. J. Consult. Clin. Psychol. 80, 186–195 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Marques L, Alegria M, Becker A, Chen C, Fang A, Chosak A, Diniz J Comparative prevalence, correlates of impairment, and service utilization for eating disorders across US ethnic groups: Implications for reducing ethnic disparities in health care access for eating disorders. Int. J. Eat. Disord. 44, 412–420 (2011). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Udo T & Grilo C Prevalence and Correlates of DSM-5–Defined Eating Disorders in a Nationally Representative Sample of U.S. Adults. Biol. Psychiatry 84, 345–354 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.De Vries A, McGuire J, Steensma T, Wagenaar E, Doreleijers T, Cohen-Kettenis P Young adult psychological outcome after puberty suppression and gender reassignment. Pediatrics 134, 696–704 (2014). [DOI] [PubMed] [Google Scholar]
- 36.Fisher A, Castellini G, Bandini E, Casale H, Fanni E, Benni L, Feruccio N, Meriggiola M, Manieri C, Gualerzi A, Jannini E, Oppo A, Ricca V, Maggi M, Rellini A Cross-Sex Hormonal Treatment and Body Uneasiness in Individuals with Gender Dysphoria. J. Sex. Med. 11, 709–719 (2014). [DOI] [PubMed] [Google Scholar]
- 37.van de Grift T, Elaut E, Cerwenka S, Cohen-Kettenis P, De Cuypere G, Richter-Appelt H, Kreukels B Effects of Medical Interventions on Gender Dysphoria and Body Image. Psychosom. Med. 79, 815–823 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Khoosal D, Langham C, Palmer B, Terry T & Minajagi M Features of eating disorder among maleto-female transsexuals. Sex. Relatsh. Ther. 24, 217–229(2009). [Google Scholar]
- 39.Ålgars M, Alanko K, Santtila P & Sandnabba N Disordered eating and gender identity disorder: A qualitative study. Eat. Disord. 20, 300–311 (2012). [DOI] [PubMed] [Google Scholar]
- 40.Kidd J, Levin F, Dolezal C, Hughes T, & Bockting W Understanding predictors of improvement in risky drinking in a U.S. multi-site, longitudinal cohort study of transgender individuals: Implications for culturally-tailored prevention and treatment efforts. Addict. Behav. 96, 68–75 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Connolly D & Gilchrist G Prevalence and correlates of substance use among transgender adults: A systematic review. Addictive Behaviors 111, 106544 (2020). [DOI] [PubMed] [Google Scholar]
- 42.Budge S, Rossman H & Howard K Coping and Psychological Distress Among Genderqueer Individuals: The Moderating Effect of Social Support. J. LGBT Issues Couns. 8, 95–117 (2014). [Google Scholar]
- 43.Mahr F, Farahmand P, Bixler E, Domen R, Moser E, Nadeem T, Levine R, Halmi K A national survey of eating disorder training. Int. J. Eat. Disord. 48, 443–445 (2015). [DOI] [PubMed] [Google Scholar]
- 44.Anderson K, Accurso EC, Kinasz KR & Le Grange D Residents’ and Fellows’ Knowledge and Attitudes about Eating Disorders at an Academic Medical Center. Acad. Psychiatry. 41, 381–384 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hilbert A, Petroff D, Herpertz S, Pietrowsky R, Tuschen-Caffier B, Vocks S, Schmidt R Metaanalysis on the long-term effectiveness of psychological and medical treatments for binge-eating disorder. Int J Eat Disord. 53, 1353–1376 (2020). [DOI] [PubMed] [Google Scholar]