Abstract
Background:
Mental health symptoms, stress, and low psychosocial resources are associated with preterm delivery. It is unknown if there are groups of women who experience similar patterns of these adverse psychosocial factors during pregnancy and if the risk of preterm delivery differs among these groups.
Objective:
To identify groups of women with similar patterns of adverse psychosocial factors during pregnancy and determine if the risk of preterm delivery differs among these groups.
Methods:
Spontaneous Prematurity and Epigenetics of the Cervix (SPEC) is a prospective cohort study of pregnant women, aged 18 and older. In this analysis, we included women who enrolled after August 24, 2014 and delivered by January 20, 2019. As women could enrol more than once, our cohort included 774 women with 787 pregnancies. We conducted a latent class analysis to identify groups of women with similar patterns of adverse psychosocial factors during pregnancy based on their responses to measures assessing depression, perceived stress, anxiety (pregnancy-related and generalized), stressful life events, resilience, and social support (partner and friend/family). After identifying the latent classes, we used log-binomial regression to compare the incidence of preterm delivery among the classes.
Results:
The median age among participants was 33.2 years (interquartile range 30.3-36.3) and the majority were non-Hispanic white (56.9%). We identified three classes of adverse psychosocial factors (few, some, and many factors). In total, 63 (8.0%) pregnancies resulted in a preterm delivery. Compared to participants with few factors, the risk of preterm delivery was no different among participants with some (RR 1.23, 95% CI 0.68, 2.25) and many adverse factors (RR 1.62, 95% CI 0.73, 3.62).
Conclusions:
We identified three groups of pregnant women with similar patterns of adverse psychosocial factors. We did not observe a difference in the risk of preterm delivery among the classes.
Keywords: Psychosocial factors, premature birth, latent class analysis, pregnancy
BACKGROUND
Adverse psychosocial factors including mental health symptoms, stress, and low psychosocial resources (such as social support and resilience) have been associated with preterm delivery (<37 weeks’ gestation), both independently and when co-occurring. However, the strength of these associations varies widely .1–4 This heterogeneity may in part be due to underlying differences in the co-occurrence of many of these factors. Identifying and characterising groups of pregnant women with similar combinations of these factors could lead to a better understanding of the association between adverse psychosocial factors and preterm delivery.
Latent class analysis is an analytic technique used to identify homogenous groups (classes) of individuals. Although class membership is unknown, it can be inferred from response patterns to a set of categorical variables.5–7 It resembles cluster analysis in that the goal is to categorize individuals into groups using statistical criteria determined from fitting models with different numbers of classes to data. As with cluster analysis, the number of classes is not known a priori, but is instead determined based on model fit. Unlike cluster models, however, membership in a latent class is determined based on the posterior probability of group membership—similar to a predicted probability of the outcome estimated from a set of variables in a regression model—which is calculated for each individual from the modelled variables. This has been shown to result in less misclassification of cluster assignment than traditional cluster analysis.8
We conducted a latent class analysis to identify groups of pregnant women with similar combinations of adverse psychosocial factors as measured by widely-used psychometric instruments. In addition, we investigated how gestational age at delivery and preterm delivery differed among the latent classes.
METHODS
Cohort selection
Spontaneous Prematurity and Epigenetics of the Cervix (SPEC) is a prospective cohort study of pregnant women. Patients who were at least 18 years old and were seeking prenatal care at Beth Israel Deaconess Medical Center (BIDMC)) were eligible to participate. Participants could enrol in SPEC at any point during pregnancy (median gestational age at enrolment: 18.0 weeks; range 5.0-34.0 weeks), and those who conceived more than once could reenroll. Participants enrolled during prenatal appointments. They completed demographic and psychosocial questionnaires in-person at enrolment, though those who did not have time to do so completed them in-person at a later appointment or online. This study was approved by the institutional review board at BIDMC.
Participants with singleton gestations, who enrolled in the study after August 24, 2014 (when the resilience instrument was added), and who delivered by January 20, 2019 were eligible for inclusion in this analysis (n=1,011). We excluded participants who reported a pregnancy loss prior to 20 weeks’ gestation (n=141). We also excluded women who completed their psychometric questionnaires after delivery (n=83). Thirteen (1.7%) participants contributed more than one pregnancy to the analysis. Our final analytic cohort included 774 women with 787 pregnancies (Figure 1).
Figure 1:
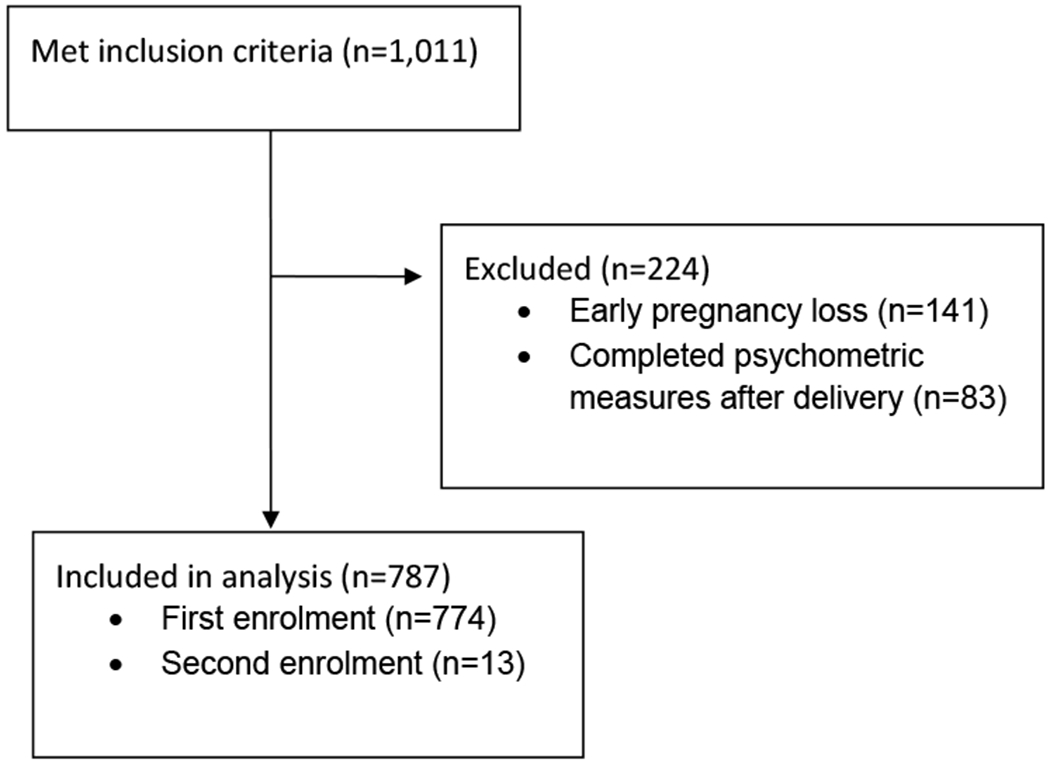
Flow diagram of participant exclusion
Demographic information
Demographic data were primarily self-reported by participants on the demographic questionnaire. Specifically, we collected data on race/ethnicity (as a proxy for racism), education, household income, partnership, employment, smoking, history of preterm delivery, and history of depression or anxiety (experience of symptoms, clinical diagnosis, and pharmacological treatment). Additionally, we abstracted age, gravidity, and parity from medical records. We used data on self-reported race/ethnicity from medical records to fill in missing data if participants did not report it.
Exposures
Depression
Antenatal depressive symptoms were measured using the 10-item Edinburgh Postnatal Depression Scale (EPDS), which has been validated for use among pregnant women.9,10 Participants reported the frequency with which they experienced depressive symptoms within the previous seven days on a scale from zero (“not at all”) to three (“all of the time”). Scores range from 0-30, with higher scores indicating more depressive symptoms.
General anxiety
General anxiety was measured using the 10-item version of the Trait Anxiety Scale, which is part of the State-Trait Anxiety Inventory.11 Participants rated how often they experienced symptoms of anxiety on a scale from one (“almost never”) to four (“almost always”). Scores range from 10-40, with higher scores indicating more anxiety symptoms. Although the 10-item version has not been validated for use among pregnant women, the 20-item version has.12
Pregnancy-related anxiety
Participants completed the 7-item Pregnancy-Related Anxiety Scale 13 Participants were asked to rate their level of concern from one (“not at all”) to four (“very much”). Scores range from 4-28, with higher scores indicating higher anxiety. This instrument has not been validated, but has been used in similar populations of pregnant women.13,14
Perceived stress
Perceived stress was ascertained using Cohen’s 4-item Perceived Stress Scale, which has been used in other studies of pregnant women.12,15–17 Participants reported the frequency of stressful experiences within the past month on a scale from zero (“never”) through five (“very often”). Overall scores range from 0-20, with higher scores indicating greater perceived stress.
Stressful events
Participants completed the Crisis in Family Systems-Revised based on their experience within the last six months.18 This scale asks about stressful events within 11-domains, including: financial, relationship, safety at home, and medical issues.18 If a participant stated that she experienced at least one of the events within a given domain and that it had a negative impact on her, she received one point towards her total score. Scores range from 0-11, with 11 indicating that a participant has experienced many stressful events within the past six months. This scale has not been validated among pregnant women, but has been used in other studies of pregnant women.19,20
Social support
Participants completed two sets of five Likert-scale questions regarding their social support. The first set was specific to support from their partner, and are a subset of the eight questions developed by Turner et al. to evaluate partner support among pregnant teenagers.21 The second set are a subset of the Provisions of Social Relation Scale and were used to capture support from family and friends.21 Participants were asked to rate how strongly they agreed to a number of statements about the support they received from one (“strongly agree”) to four (“strongly disagree”). Although these questions are not specific to pregnancy, both scales were developed and validated for use among pregnant women.21 Scores range from 0-15 for each scale, with higher scores indicating higher support. Consistent with prior research, we classified women who reported not having a partner as having low partner support.22
Resilience
Resilience was measured using the 25-item Connor-Davidson Resilience Scale.23 Although this scale has not been validated for use among pregnant women, it has been used in other studies of pregnancy.24,25 Participants were asked to respond to each item based on their experience within the past month on a scale from zero (“not true at all”) to four (“true nearly all of the time”). Scores range from 0-100, with higher scores indicating higher resilience.
Outcomes
We abstracted gestational age at delivery as determined by best obstetric estimate from the medical records of participants who delivered at BIDMC (92.3%). We telephoned participants who delivered elsewhere to obtain delivery information, including gestational age. We attempted to contact participants three times. After the third attempt we considered unreachable participants as lost to follow-up. We considered deliveries after 20 weeks’ and before 37 weeks’ gestation as preterm. No pregnancies among participants included in the analytic cohort resulted in stillbirths.
Statistical analysis
Missing data
We used multiple imputation to impute missing demographic and psychometric data, as well as gestational age at delivery for participants lost to follow-up.26 We generated fifty imputation datasets using a Markov chain Monte Carlo method (Appendix 1).27 We imputed missing responses to individual questions and then scored each psychometric measure, rather than imputing the overall score. The proportion of missingness for questions on the psychometric measures ranged from 13.9% to 19.2%. Gestational age at delivery was missing for 1.1% of participants. All reported frequencies and descriptive statistics are from the first imputed dataset.
Latent class analysis
We conducted a latent class analysis to identify combinations of mental health symptoms (depression, general anxiety, and pregnancy-related anxiety), stress (perceived and experience of stressful events within the past six months), and low psychosocial resources (social support and resilience) experienced by participants. In order to model adverse levels of each factor, we created dichotomous variables for each psychometric measure. We used the established cut-point of 13 on the EPDS to classify participants as having probable depression (vs. non-probable depression).28,29 To our knowledge there are no validated cut-points for the other psychometric measures, so we created cut-points based on the distribution of scores in the cohort. We considered participants with scores ≥ the 90th percentile on the general anxiety (23 points), pregnancy-related anxiety (21 points), perceived stress (10 points), and experience of stressful life events (4 events) measures as having high anxiety or stress (vs. moderate/low). We classified participants with scores ≤ 10th percentile on the resilience (58 points) and both social support scales (9 points for friend/family and 10 points for partner) as having low psychosocial resources (vs. moderate/high). We chose these cut-points because we felt that scores ≥ 90th and ≤ 10th percentiles were most indicative of adverse symptomology, which was overall fairly low in the cohort (eTable 1).
Because we had no a prior hypothesis regarding the number of latent classes likely to exist within our cohort, we fit models with two through five classes. We fit these models in each imputed dataset and then averaged the model fit statistics and conditional probabilities across the datasets. We assessed model fit using the log-likelihood, the Akaike information criterion (AIC), the Bayesian information criterion (BIC), the sample-size adjusted BIC, and entropy values. For the AIC, BIC, and sample-size adjusted BIC, lower values indicate better fit, while for the log-likelihood higher values indicate better fit. Entropy values range from zero to one, with values closer to one indicating better separation between the classes.5 Although we prioritized these model fit statistics, we also considered the differences in the conditional probabilities of class membership when selecting our final model. After identifying the model that fit our data best, we used the conditional probabilities of class membership to characterise the classes. Finally, we used participants’ posterior probability of class membership to assign them to their most likely class (eTable 2).
We qualitatively compared participants’ demographics among the classes. We used linear regression to compare mean gestational age at delivery and log-binomial regression to compare the cumulative incidence of preterm delivery among the classes. We used generalized estimating equations to account for correlations among participants with multiple pregnancies. We estimated the models in each imputed dataset and then averaged the point and variance estimates across the datasets.30 Given the predictive nature of these analyses, we did not adjust for any covariates.31 We conducted all analyses in SAS 9.4 (SAS Institute Inc., Cary, NC).
Sensitivity analyses
Since we used percentiles to create binary variables for all of the psychometric measures except the EPDS, we repeated the latent class analysis using lower thresholds for adverse levels of anxiety, stress, and low psychosocial resources to evaluate the effect of our chosen cut-points. We considered scores ≥ the 75th percentile on the anxiety and stress measures as having high anxiety or stress. We classified participants with scores ≤ the 25th percentile on the resilience and social support scales as having low psychosocial resources. We used the same validated cut-point for the EPDS.
Although severity of adverse psychosocial factors may vary throughout pregnancy, we measured these factors at one time point only. The majority (72.1%) of the 650 participants with complete psychometric data completed the measures during their second trimester; thus, we were unable to conduct a latent class analysis stratifying by trimester as too few participants completed the psychometric measures during the first and third trimester (n=85 and n=95, respectively) to allow for meaningful estimation of a latent model. Thus, to evaluate whether the combinations of adverse psychosocial factors differed depending on when in pregnancy participants completed the psychometric measures, we repeated the latent class analysis among the 650 (82.3%) participants with complete psychometric data including a grouping variable for pregnancy half. Among participants who completed the measures, 378 (58.2%) did so during the first half of pregnancy (<20 weeks’ gestation) and 272 (41.9%) completed them during the second half of pregnancy (≥20 weeks’ gestation).
RESULTS
Sample Description
The median age at enrolment among participants was 33.2 years (IQR 30.3-36.3). A majority of participants were non-Hispanic white (56.9%), married or living with their partner (88.8%), and had completed a bachelor’s degree or higher (73.1%). Prior to their current pregnancy, 247 (31.4%) participants reported having experienced symptoms of depression or anxiety and 219 (17.8%) reported having received a clinical diagnosis of depression or anxiety (Table 1).
Table 1:
Baseline characteristics of 787 participants in the SPEC study
| Overall n=787 |
|
|---|---|
| Age at enrolment (years) | 33.2 (30.3, 36.3) |
| Gravidity | 2.0 (1.0, 3.0) |
| Parity | 1.0 (0.0, 1.0) |
| Race/ethnicity | |
| Non-Hispanic white | 448 (56.9) |
| Non-Hispanic black | 110 (14.0) |
| Asian | 80 (10.2) |
| Hispanic | 69 (8.8) |
| Other | 80 (10.2) |
| Partnership status | |
| Married or living with partner | 699 (88.8) |
| Never married | 63 (8.0) |
| Divorced/separated | 25 (3.2) |
| Current smoker | 24 (3.1) |
| History of preterm birtha | 86 (21.8) |
| Education | |
| High school diploma or less | 90 (11.4) |
| Some college or associate’s degree | 122 (15.5) |
| Bachelor’s degree or higher | 575 (73.1) |
| Employment status | |
| Employed full-time | 519 (66.0) |
| Employed part-time | 109 (13.9) |
| Not employed | 159 (20.2) |
| Annual household income | |
| <$25,000 | 130 (16.5) |
| $25,000-$49,999 | 72 (9.2) |
| $50,000-$74,999 | 79 (10.0) |
| $75,000-$99,999 | 94 (11.9) |
| ≥$100,000 | 412 (52.4) |
| Experienced symptoms of depression or anxiety prior to current pregnancy | 247 (31.4) |
| Clinical diagnosis of depression or anxiety prior to current pregnancy | 219 (27.8) |
| Took medications for depression or anxiety prior to current pregnancy | 222 (28.2) |
Data presented as median (interquartile range) or n (%)
Restricted to 430 women who reported a prior delivery
Characterisation of latent classes
Results from the latent class analysis indicated that a two- or three-class model fit the data best. The three-class model had lower AIC and sample-size adjusted BIC values, as well as a higher log-likelihood than the two-class model, although the two-class model had higher entropy (eTable 3). However, we observed clearer separation of the conditional probabilities among the classes for the three-class model. Based on the conditional probabilities and the model fit statistics, we determined that the three-class model fit our data best. The conditional probabilities for the two-class model are presented in eTable 4.
The majority (74.7%) of participants were assigned to class 1, while 163 (20.7%) were assigned to class 2, and 36 (4.6%) were assigned to class 3. Participants in class 1 had a low conditional probability of having mental health symptoms, stress, or low psychosocial resources (Table 2). Participants in class 2 had a higher probability of having mental health symptoms (0.04 -0.11). and low psychosocial resources (0.13 – 0.24). Participants in class 3 had a high probability of depressive symptoms (0.82), high general anxiety (0.84), and low support from friends and family (0.66). Additionally, the conditional probabilities for high pregnancy-related anxiety (0.42), low resilience (0.39), and high perceived stress (0.44) were much higher in this class than the other classes (Table 2). We labelled the latent classes as few (class 1), some (class 2), and many (class 3) adverse psychosocial factors.
Table 2:
Conditional probabilities of latent class membership
| Class 1 | Class 2 | Class 3 | |
|---|---|---|---|
|
| |||
| Few adverse psychosocial factors n=588 |
Some adverse psychosocial factors n=163 |
Many adverse psychosocial factors n=36 |
|
| Depressive symptoms | |||
| No probable depression (<13) | 0.99 | 0.96 | 0.18 |
| Probable depression (≥13) | 0.01 | 0.04 | 0.82 |
| General anxiety | |||
| Moderate/low symptomology (<90th percentile) | 0.92 | 0.89 | 0.16 |
| High symptomology (≥90th percentile) | 0.08 | 0.11 | 0.84 |
| Pregnancy-related anxiety | |||
| Moderate/low symptomology (<90th percentile) | 0.93 | 0.90 | 0.58 |
| High symptomology (≥90th percentile) | 0.07 | 0.10 | 0.42 |
| Perceived stress | |||
| Moderate/low symptomology (<90th percentile) | 0.81 | 0.79 | 0.56 |
| High symptomology (≥90th percentile) | 0.19 | 0.21 | 0.44 |
| Stressful life events | |||
| 0-3 events (<90th percentile) | 0.88 | 0.84 | 0.44 |
| 4 or more events (≥90th percentile) | 0.12 | 0.16 | 0.56 |
| Resilience | |||
| Moderate/high (>10th percentile) | 0.87 | 0.87 | 0.61 |
| Low (≤10th percentile) | 0.13 | 0.13 | 0.39 |
| Partner support | |||
| Moderate/high (>10th percentile) | 0.89 | 0.83 | 0.60 |
| Low (≤10th percentile) | 0.11 | 0.17 | 0.40 |
| Friend and family support | |||
| Moderate/high (>10th percentile) | 0.79 | 0.76 | 0.34 |
| Low (≤10th percentile) | 0.21 | 0.24 | 0.66 |
The median age among participants with few adverse factors was 33.5 years (IQR 30.8-36.6), which was slightly higher than the median age among participants with some (31.8 years, IQR 28.2-35.5) and few (30.4 year, IQR 25.0-35.9) factors (Table 3). Participants with some (80.4%) and few (92.5%) adverse factors were more likely to report being married or living with their partner than participants with many factors (66.7%). The reported experience of depression and anxiety symptoms prior to the current pregnancy differed among the classes, as the majority (80.6%) of participants with many adverse factors reported experiencing symptoms prior to their current pregnancy, while the same was true for 49.7% of participants with some adverse factors and 23.3% of women with few factors. Participants with many factors were more likely to be black or Hispanic and have annual household incomes <$25,000 than participants with some or few factors. Among the three classes there was no difference with respect to history of preterm delivery.
Table 3:
Baseline characteristics of SPEC participants by latent class
| Class 1: Few adverse psychosocial factors n=588 |
Class 2: Some adverse psychosocial factors n=163 |
Class 3: Many adverse psychosocial factors n=36 |
|
|---|---|---|---|
| Age at enrolment (years) | 33.5 (30.8, 36.6) | 31.8 (28.2, 35.5) | 30.4 (25.0, 35.9) |
| Gravidity | 2.0 (1.0, 3.0) | 2.0 (1.0, 3.0) | 3.0 (1.5, 4.0) |
| Parity | 1.0 (0.0, 1.0) | 1.0 (0.0, 1.0) | 1.0 (0.0, 1.0) |
| Race/ethnicity | |||
| Non-Hispanic white | 350 (59.5) | 83 (50.9) | 15 (41.7) |
| Non-Hispanic black | 70 (11.9) | 31 (19.0) | 9 (25.0) |
| Asian | 64 (10.9) | 14 (8.6) | 2 (5.6) |
| Hispanic | 47 (8.0) | 15 (9.2) | 7 (19.4) |
| Other | 57 (9.7) | 20 (12.3) | 3 (8.3) |
| Partnership status | |||
| Married or living with partner | 544 (92.5) | 131 (80.4) | 24 (66.7) |
| Never married | 32 (5.4) | 25 (15.3) | 6 16.7) |
| Divorced/separated | 12 (2.0) | 7 (4.3) | 6 16.7) |
| Current smoker | 12 (2.0) | 9 (5.5) | 3 (8.3) |
| History of preterm birtha | 64 (17.8) | 19 (19.2) | 3 (14.3) |
| Education | |||
| High school diploma or less | 48 (8.2) | 33 (20.3) | 9 (25.0) |
| Some college or associate’s degree | 81 (13.8) | 32 (19.6) | 9 (20.0) |
| Bachelor’s degree or higher | 459 (78.1) | 98 (60.1) | 18 (50.0) |
| Employment status | |||
| Employed full-time | 408 (69.4) | 93 (57.1) | 18 (50.0) |
| Employed part-time | 79 (13.4) | 26 (16.0) | 4 (11.1) |
| Not employed | 101 (17.2) | 44 (27.0) | 14 (38.9) |
| Annual household income | |||
| <$25,000 | 67 (11.4) | 48 (29.5) | 15 (41.7) |
| $25,000-$49,999 | 49 (8.3) | 17 10.4) | 6 (16.7) |
| $50,000-$74,999 | 53 (9.0) | 20 (12.3) | 6 (16.7) |
| $75,000-$99,999 | 78 (13.3) | 14 (8.6) | 2 (5.6) |
| ≥$100,000 | 341 (58.0) | 64 (39.3) | 7 (19.4) |
| Experienced symptoms of depression or anxiety prior to current pregnancy | 137 (23.3) | 81 (49.7) | 29 (80.6) |
| Clinical diagnosis of depression or anxiety prior to current pregnancy | 127 (21.6) | 69 (42.3) | 23 (63.9) |
| Took medications for depression or anxiety prior to current pregnancy | 135 (23.0) | 68 (41.7) | 19 (52.8) |
Data presented as median (interquartile range) or n (%)
Restricted to 430 women who reported a prior delivery
Gestational age at delivery and preterm delivery
The mean gestational age of delivery in the cohort was 39.0 weeks (SD: 2.0). The average gestational age at delivery did not differ between participants with some adverse psychosocial factors (mean difference −0.17 weeks, 95% CI −0.53, 0.20) and many adverse factors (mean difference −0.38, 95% CI −0.95, 0.19), compared to those with few factors.
Overall, 63 of 787 (8.0%) pregnancies resulted in a preterm delivery; the incidence was 7.1% (n=42) among participants with few factors, 9.8% (n=16) among those with some factors, and 13.9% (n=5) among those with many factors. Participants with some (RR 1.23, 95% CI 0.68, 2.25) and many adverse psychosocial factors (RR 1.62, 95% CI 0.73, 3.62) were as likely to deliver preterm as participants with few factors.
Sensitivity analyses
When we used lower thresholds for adverse levels of anxiety, stress, and low psychosocial resources, we found that a four-class model fit the data best (eTables 5 and 6), indicating that our results were sensitive to our chosen cut-points.
When we accounted for when in pregnancy participants completed the psychometric measures, we identified similar latent classes between participants who completed the measures in the first half of pregnancy and those who completed them in the second half of pregnancy. While the model fit statistics indicated that the two-class models fit the data somewhat better than the three-class models (eTable 7), we again observed clearer separation between the conditional probabilities in the three-class models (Table 4). The three classes we identified in both groups were similar to those identified among the full cohort.
Table 4:
Conditional probabilities of latent class membership among women in the first and second halves of pregnancy
| First half n=378 |
Second half n=272 |
|||||
|---|---|---|---|---|---|---|
|
| ||||||
| Class 1 | Class 2 | Class 3 | Class 1 | Class 2 | Class 3 | |
|
| ||||||
| Few adverse psychosocial factors n=280 |
Some adverse psychosocial factors n=75 |
Many adverse psychosocial factors n=23 |
Few adverse psychosocial factors n=198 |
Some adverse psychosocial factors n=58 |
Many adverse psychosocial factors n=16 |
|
| Depressive symptoms | ||||||
| No probable depression (<13) | 0.99 | 0.92 | 0.13 | 1.00 | 0.92 | 0.20 |
| Probable depression (≥13) | 0.01 | 0.08 | 0.87 | 0.00 | 0.08 | 0.80 |
| General anxiety | ||||||
| Moderate/low symptomology (<90th percentile) | 0.97 | 0.73 | 0.23 | 0.99 | 0.81 | 0.05 |
| High symptomology (≥90th percentile) | 0.03 | 0.27 | 0.77 | 0.01 | 0.19 | 0.95 |
| Pregnancy-related anxiety | ||||||
| Moderate/low symptomology (<90th percentile) | 0.89 | 1.00 | 0.34 | 0.99 | 0.74 | 0.72 |
| High symptomology (≥90th percentile) | 0.11 | 0.00 | 0.66 | 0.01 | 0.26 | 0.28 |
| Perceived stress | ||||||
| Moderate/low symptomology (<90th percentile) | 0.79 | 0.85 | 0.49 | 0.81 | 0.77 | 0.55 |
| High symptomology (≥90th percentile) | 0.21 | 0.15 | 0.51 | 0.19 | 0.23 | 0.45 |
| Stressful life events | ||||||
| 0-3 events (<90th percentile) | 0.96 | 0.83 | 0.43 | 1.00 | 0.88 | 0.45 |
| 4 or more events (≥90th percentile) | 0.04 | 0.17 | 0.57 | 0.00 | 0.12 | 0.55 |
| Resilience | ||||||
| Moderate/high (>10th percentile) | 1.00 | 0.71 | 0.59 | 0.99 | 0.81 | 0.75 |
| Low (≤10th percentile) | 0.00 | 0.29 | 0.41 | 0.01 | 0.19 | 0.25 |
| Partner support | ||||||
| Moderate/high (>10th percentile) | 0.98 | 0.87 | 0.47 | 0.97 | 0.87 | 0.78 |
| Low (≤10th percentile) | 0.02 | 0.13 | 0.53 | 0.03 | 0.13 | 0.22 |
| Friend and family support | ||||||
| Moderate/high (>10th percentile) | 0.91 | 0.58 | 0.34 | 0.91 | 0.68 | 0.36 |
| Low (≤10th percentile) | 0.09 | 0.42 | 0.66 | 0.09 | 0.32 | 0.63 |
COMMENT
Principal findings
We identified three clusters of adverse psychosocial factors among women in pregnancy. Participants with few psychosocial factors were unlikely to have depressive symptoms, high anxiety, and low psychosocial resources, though 20% reported high perceived stress. Participants with some psychosocial factors were more likely to have mental health symptoms, stress, and low resources, with low support from friends and family being the most prevalent factor. Participants who experienced many adverse factors were most likely to have depressive symptoms and high anxiety. We did not observe a difference in gestational age at delivery or the incidence of preterm delivery among the classes.
Strengths of the study
Our use of multiple imputation reduced the likelihood of selection bias occurring as participants with missing data were not excluded. We also reduced the likelihood of outcome misclassification by abstracting gestational age at delivery from participants’ medical records whenever possible. Finally, we used validated or widely used psychometric measures to measure each adverse factor among participants.
Limitations of the data
A notable limitation of this study was the homogeneity of our sample, as our cohort was comprised predominantly of white, college-educated women, with annual household income of $75,000 or higher. This homogeneity may limit the generalizability of our findings. Additionally, our ability to estimate the correct number of classes may have been limited by our sample size. Our sample size and the low incidence of preterm delivery in our cohort also precluded precise estimation of the association between the latent classes and preterm delivery. We also did not collect data on active treatment for mental health symptoms or stress, or any additional support services.
By dichotomizing each psychometric measure, we may have lost meaningful information about the spectrum of symptom severity experienced by participants. This may be especially true for the psychometric measures that do not have validated cut-points. While our approach to categorizing the psychosocial measures is consistent with other studies that utilized the same resilience, general anxiety, perceived stress, and partner support measures, results from our sensitivity analysis using different cut-points indicate that our findings are sensitive to our chosen cut-points.22,32–35
Interpretation
The latent classes we identified are consistent with those from other studies of psychosocial factors among pregnant women. Loomans et al. identified five classes of pregnant women based on their depressive symptoms, anxiety, and stress. Similar to our study, they identified two classes with low probabilities of these factors, one with slightly higher probabilities, and two with high probabilities of several factors, particularly depression and general anxiety. They also did not observe significant differences in delivery timing among the classes.36 However, they did not include psychosocial resources in their latent class analysis. In contrast, Grobman et al. included resilience and social support in their latent class analysis; however, they did not assess the relationship between the estimated classes and delivery outcomes. They identified four classes of women with similar patterns of adverse psychosocial factors to those we identified, including a group with high levels of depression, anxiety, and stress, and low levels of resilience.25 Findings from our study provide additional evidence about the prevalence of adverse psychosocial factors among groups of pregnant women, and suggest that delivery timing may not differ among these groups.
Although we did not observe a difference in delivery timing among the classes, pregnancy represents a unique opportunity to identify and address adverse psychosocial factors among women given their increased exposure to health and social services. The American College of Obstetricians and Gynecologists recommends that women be screened once during pregnancy for depression and anxiety.37 Screening for multiple adverse factors, however, may provide valuable information to help providers tailor treatment. For example, women with many adverse factors may need more involved treatments and social support services to treat their mental health symptoms. As women with many adverse factors are more likely to be low-income and racial/ethnic minorities, clinicians may be able to best serve these women by recommending community- or home-based interventions. These interventions are likely to be more comfortable and convenient for women, which may overcome some of the challenges that prevent women from minority racial/ethnic groups or with low income from receiving adequate treatment for mental health symptoms in pregnancy, including stigma, lack of money, and childcare.38
Conclusions
Among pregnant women there are groups who experience similar combinations of adverse psychosocial factors. However, our results indicate that delivery timing does not differ among these groups.
Supplementary Material
SOCIAL MEDIA QUOTE.
Using latent class analysis, we identified three groups of women with similar combinations of adverse psychosocial factors: few, some, and many factors. The incidence of preterm delivery did not differ among these groups.
SYNOPSIS.
Study questions:
Are there groups of pregnant women with similar combinations of adverse psychical factors and does the risk of preterm delivery differ among these groups?
What is already known:
Adverse psychosocial factors including mental health symptoms, stress, and low psychosocial resources are associated with increased risk of preterm delivery. Many of these factors are co-occurring, and women who experience more than one factor during pregnancy are more likely to deliver preterm. It is not well understood what combinations of adverse psychosocial factors women commonly experience during pregnancy.
What this study adds:
Using latent class analysis, we identified three groups of women with similar combinations of adverse psychosocial factors: few, some, and many factors. The incidence of preterm delivery did not differ among these groups.
ACKNOWLEDGEMENTS
We are grateful to Melissa Ada, Allison O’Neill, Emily Nuss, Erin Kennedy, Dayna Neo and Allyson Redhunt who all served as research assistants for the SPEC study. We acknowledge the clinical staff that made this study possible at the Center for Maternal-Fetal Medicine and outpatient prenatal clinics at Beth Israel Deaconess Medical Center, as well as the Bowdoin Street Health Center. We also are grateful to the SPEC study participants.
FUNDING
Funding for this work came from the Charles H. Hood Foundation. This work was also conducted with support from Harvard Catalyst- The Harvard Clinical and Translational Science Center (National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health Award UL1 TR001102), NIH/NIEHS K23ES022242, and NIHCD T32 HD052458. Additional support came from the Chrissy and Jesse Brown Family.
Appendix 1: Multiple imputation model
PROC MI Specifications
Number of imputations: 50
Coverage: 0.01
Max iteration: 600
MCMC imputation: Full
Prior: Jeffrey’s (non-informative)
Log transformation of all continuous variables
Categorial variables
All categorical variables were dummy coded prior to inclusion in the multiple imputation model
Following imputation, a random number generator (ranuni) was used to round binary variables
Variables included
| Variable | Percentage missing |
|---|---|
| Age at enrolment | 0.0 |
| Gravidity | 0.3 |
| Parity | 0.1 |
| Gestational age at delivery | 1.1 |
| Race/ethnicity | 0.8 |
| Education | 11.2 |
| Current student status | 11.9 |
| History of preterm birth | 9.8 |
| Current smoker | 11.6 |
| Current exposure to household smoke | 11.7 |
| Household income | 15.0 |
| Employment status | 12.3 |
| Marital status | 13.5 |
| Zip code of residence | 10.5 |
| Average family income in zip code of residence | 26.4 |
| Proportion of households that own homes in zip code of residence | 26.4 |
| Proportion of households that rent homes in zip code of residence | 26.4 |
| Experience of recent bacterial vaginosis infection | 13.6 |
| Experience of recent yeast infection | 13.6 |
| Experience of symptoms of depression or anxiety prior to current pregnancy | 16.5 |
| Clinical diagnosis of depression or anxiety prior to current pregnancy | 16.6 |
| Medication used to treat depression or anxiety prior to current pregnancy | 16.5 |
| 10 items of Edinburgh Postnatal Depression Scale | 16.1-16.9 |
| 10 items of the Trait Anxiety Scale | 15.9-16.8 |
| 7 items of Pregnancy-Related Anxiety Scale | 15.1-16.3 |
| 4 items of Cohen’s Perceived Stress Scale | 15.1-15.4 |
| 70 items of Crisis in Family Systems-Revised scale | 16.8-19.2 |
| 25 items of Connor-Davidson Resilience Scale | 17.4-18.0 |
| 5 items of partner support scale | 16.4-17.0 |
| 5 items of friend and family support scale | 13.9-14.4 |
REFERENCES
- 1.Jarde A, Morais M, Kingston D, Giallo R, MacQueen GM, Giglia L, et al. Neonatal Outcomes in Women With Untreated Antenatal Depression Compared With Women Without Depression. JAMA Psychiatry 2016;73:826–837. [DOI] [PubMed] [Google Scholar]
- 2.Hetherington E, Doktorchik C, Premji SS, McDonald SW, Tough SC, Sauve RS. Preterm Birth and Social Support during Pregnancy: A Systematic Review and Meta-Analysis. Paediatric and Perinatal Epidemiology 2015;29:523–535. [DOI] [PubMed] [Google Scholar]
- 3.Coughlin C, Blackwell K, Bartley C, Hay M, Yonkers K, Blouch M. Obstetric and Neonatal Outcomes After Antipsychotic Medication Exposure During Pregnancy. Obstetrics & Gynecology 2015;125:1224–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Liou S-R, Wang P, Cheng C-Y. Effects of prenatal maternal mental distress on birth outcomes. Women and Birth 2016;29:376–380. [DOI] [PubMed] [Google Scholar]
- 5.Collins LM, Lanza ST. Latent class and latent transition analysis: with applications in the social, behavioral, and health sciences. New York: Wiley; 2010. [Google Scholar]
- 6.Oberski D. Mixture models: Latent profile and latent class analysis. Modern Statistical Methods for HCI 2016:275–287. [Google Scholar]
- 7.Lanza ST, Rhoades BL. Latent Class Analysis: An Alternative Perspective on Subgroup Analysis in Prevention and Treatment. Prevention Science 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Magidson J, Vermunt JK. Latent class models for clustering: A comparison with K-means.; 2002. [Google Scholar]
- 9.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. The British Journal of Psychiatrysychiatry 1987;150:782–786. [DOI] [PubMed] [Google Scholar]
- 10.Kozinszky Z, Dudas RB. Validation studies of the Edinburgh Postnatal Depression Scale for the antenatal period. Journal of Affective Disorders 2015;176:95–105. [DOI] [PubMed] [Google Scholar]
- 11.Julian LJ. Measures of Anxiety: State-Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), and Hospital Anxiety and Depression Scale-Anxiety (HADS-A). Arthritis Care and Research 2011;63:S467–S472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bann CM, Parker CB, Grobman WA, Willinger M, Simhan HN, Wing DA, et al. Psychometric properties of stress and anxiety measures among nulliparous women. Journal of Psychosomatic Obstetrics and Gynecology 2017;38:53–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rini CK, Dunkel-Schetter C, Wadhwa PD, Sandman CA. Psychological adaptation and birth outcomes: the role of personal resources, stress, and sociocultural context in pregnancy. Health Psychology 1999;18:333–45. [DOI] [PubMed] [Google Scholar]
- 14.Fairlie TG, Gillman MW, Rich-Edwards J. High pregnancy-related anxiety and prenatal depressive symptoms as predictors of intention to breastfeed and breastfeeding initiation. Journal of Women’s Health 2009;18:945–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior 1983;24:385–96. [PubMed] [Google Scholar]
- 16.Silveira ML, Pekow PS, Dole N, Markenson G, Chasan-Taber L. Correlates of high perceived stress among pregnant hispanic women in western massachusetts. Maternal and Child Health Journal 2013;17:1138–1150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rieger KL, Heaman MI. Factors Associated With High Levels of Perceived Prenatal Stress Among Inner-City Women. Journal of Obstetric, Gynecologic & Neonatal Nursing 2016;45:180–195. [DOI] [PubMed] [Google Scholar]
- 18.Berry C, Shalowitz M, Quinn K, Wolf R. Validation of the Crisis in Family Systems-Revised, a contemporary measure of life stressors. Psychological reports 2001;88:713–24. [DOI] [PubMed] [Google Scholar]
- 19.Suglia SF, Staudenmayer J, Cohen S, Enlow MB, Rich-Edwards JW, Wright RJ. Cumulative Stress and Cortisol Disruption among Black and Hispanic Pregnant Women in an Urban Cohort. Psychological Trauma 2010;2:326–334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu S, Gennings C, Wright RJ, Wilson A, Burris HH, Just AC, et al. Prenatal stress, methylation in inflammation-related genes, and adiposity measures in early childhood. Psychosomatic Medicine 2018;80:34–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Turner RJ, Grindstaff CF, Phillips N. Social support and outcome in teenage pregnancy. Journal of Health and Social Behavior 1990;31:43–57. [PubMed] [Google Scholar]
- 22.Cheng ER, Rifas-Shiman SL, Perkins ME, Rich-Edwards JW, Gillman MW, Wright R, et al. The Influence of Antenatal Partner Support on Pregnancy Outcomes. Journal of Women’s Health 2016;25:672–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Connor KM, Davidson JRT. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC). Depression and Anxiety 2003;18:76–82. [DOI] [PubMed] [Google Scholar]
- 24.Johnson K, Paley F, Modest A, Hacker M, Shaughnessy S, Ricciotti H, et al. An assessment of depression, psychosocial factors, and resilience among women seeking prenatal care at an urban community health center. Obstetrics & Gynecology 2018;140:153–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grobman WA, Parker CB, Willinger M, Wing DA, Silver RM, Wapner RJ, et al. Racial Disparities in Adverse Pregnancy Outcomes and Psychosocial Stress. Obstetrics & Gynecology 2018;131:328–335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Donders ART, van der Heijden GJMGMG, Stijnen T, Moons KGMM. Review: A gentle introduction to imputation of missing values. Journal of Clinical Epidemiology 2006;59:1087–1091. [DOI] [PubMed] [Google Scholar]
- 27.Schafer JL. Analysis of Incomplete Multivariate Data. CRC Press; 1997. [Google Scholar]
- 28.Matthey S, Henshaw C, Elliott S, Barnett B. Original contribution Variability in use of cut-off scores and formats on the Edinburgh Postnatal Depression Scale-implications for clinical and research practice. Archives of Women’s Mental Health 2006;9:309–315. [DOI] [PubMed] [Google Scholar]
- 29.Tse AC, Rich-Edwards JW, Rifas-Shiman SL, Gillman MW, Oken E. Association of maternal prenatal depressive symptoms with child cognition at age 3 years. Paediatric and Perinatal Epidemiology 2010;24:232–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rubin D. Multiple imputation for nonresponse in surveys. Wiley; 2004. [Google Scholar]
- 31.Shmueli G. To explain or to predict? Statistical Science 2010;25:289–310. [Google Scholar]
- 32.Kolte AM, Olsen LR, Mikkelsen EM, Christiansen OB, Nielsen HS. Depression and emotional stress is highly prevalent among women with recurrent pregnancy loss. Human Reproduction 2015;30:777–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chinchilla-Ochoa D, Barriguete Chávez-Peón P, Farfán-Labonne BE, Garza-Morales S, Leff-Gelman P, Flores-Ramos M. Depressive symptoms in pregnant women with high trait and state anxiety during pregnancy and postpartum. International Journal of Women’s Health 2019;11:257–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nie C, Dai Q, Zhao R, Dong Y, Chen Y, Ren H. The impact of resilience on psychological outcomes in women with threatened premature labor and spouses: a cross-sectional study in Southwest China. Health and Quality of Life Outcomes 2017;15:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Scali J, Gandubert C, Ritchie K, Soulier M, Ancelin M-L, Chaudieu I. Measuring resilience in adult women using the 10-items Connor-Davidson Resilience Scale (CD-RISC). Role of trauma exposure and anxiety disorders. PloS one 2012;7:e39879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Loomans EM, Van Dijk AE, Vrijkotte TGM, Van Eijsden M, Stronks K, Gemke RJBJ, et al. Psychosocial stress during pregnancy is related to adverse birth outcomes: Results from a large multi-ethnic community-based birth cohort. European Journal of Public Health 2013;23:485–491. [DOI] [PubMed] [Google Scholar]
- 37.The American College of Obstetricians and Gynecologists. Screening for Perinatal Depression. 2018.
- 38.Nillni YI, Mehralizade A, Mayer L, Milanovic S. Treatment of depression , anxiety , and trauma-related disorders during the perinatal period : A systematic review. Clinical Psychology Review 2018;66:136–148. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


