Abstract
This article presents a narrative review and conceptual framework for research on family involvement across the continuum of substance use disorder (SUD) services for transition-age youth (ages 15–26). Though families are powerful resources for enhancing treatment and recovery success among youth with SUDs, they are not routinely included in clinical practice. This article summarizes youth SUD prevalence and service utilization rates and presents developmental and empirical rationale for increasing family involvement in services. It then describes key research issues on family involvement across the SUD services continuum: Problem Identification, Treatment Engagement, Active Treatment, Recovery Support. Within each phase, it highlights bedrock research findings and suggests promising opportunities for advancing the scientific knowledge base on family involvement. The main goals are to endorse family-oriented practices for immediate adoption in routine care and identify areas of research innovation that could significantly enhance the quality of youth SUD services.
Keywords: family involvement, youth substance use, treatment, recovery, research
Improving the quality of treatment and recovery support services for transition-age youth (ages 15–26) with substance use disorder (SUD) remains an urgent national health priority. Both empirical and developmental research indicate that families are powerful resources for enhancing treatment and recovery success among youth with SUD. Yet, families are not routinely targeted or systematically included in common clinical practice. To address this critical shortcoming, we present a narrative review and conceptual framework for research on family involvement across the continuum of SUD services for transition-age youth. We first summarize youth SUD prevalence and service utilization rates and describe developmental and empirical rationale for increasing family involvement in services. We then discuss key research issues on family involvement within four phases of the SUD services continuum: Problem Identification, Treatment Engagement, Active Treatment, and Recovery Support. Within each phase we highlight bedrock research findings and suggest promising opportunities for advancing the scientific knowledge base on family involvement. We contend that such advances across the full continuum of services can help upgrade the quality of youth SUD care.
Substance Use Prevalence and Service Utilization among Transition-Age Youth
In recent years, transition-age youth have experienced unprecedented levels of substance-related consequences in general and opioid-related consequences in particular. According to the latest national data (Substance Abuse and Mental Health Services Administration [SAMHSA], 2020a), about 6.4 million youth under the age of 26 meet diagnostic criteria for a SUD and over 300,000 youth meet criteria specifically for an opioid use disorder. Nearly 1,800 youth initiate heroin or pain reliever misuse each day (SAMHSA, 2020a), and 8–12% of those who engage in opioid misuse develop opioid use disorder (Vowles et al., 2015). Most alarmingly, the rate of lethal overdoses attributable to opioids has increased markedly in this age cohort, from 3.4 deaths to 5.3 deaths per 100,000 between 2006 and 2015 (Ali et al., 2019).
When left untreated or ineffectively treated, risky substance use in youth often persists and contributes to an array of lifetime sequalae, including mental health disorders, sexually transmitted infections, unwanted pregnancy, accidents, and violent crime (National Center on Addiction and Substance Abuse, 2011). This developmental vulnerability highlights the critical importance of effective intervention for this age group. Unfortunately, rates of service utilization among this age group remain poor. In 2019, less than 9% of transition-age youth who met full diagnostic criteria for a SUD received any substance use treatment, and even fewer (7.2%) received treatment at a specialty SU treatment facility (SAMHSA, 2020a). Reasons reported for not receiving SU treatment despite perceived need included: not ready to stop using (39.9%), not knowing where to go for treatment (23.8%), and lacking healthcare coverage or other means to afford treatment (20.9%) (SAMHSA, 2020a). Utilization rates are even more alarming among those youth with an opioid use disorder, for whom early intervention with medication for opioid use disorder (MOUD), consisting of opioid agonist or antagonist medication (buprenorphine, naltrexone, or methadone) is the only evidence-based treatment to reduce risk of lethal overdose (Volkow et al., 2019). A retrospective cohort analysis of 9.7 million transition-age youth found that fewer than 1 in 4 insured clients with an opioid use disorder received front-line MOUD services (Hadland et al., 2017). Of even greater concern, there were marked disparities: Youth who were younger, female, Black, and/or Hispanic had lower odds of receiving MOUD. Thus, in addition to a need for evidence-based intervention services, there is vital need for effective, equitable treatment identification and engagement strategies.
Rationale for Increasing Family Involvement in Youth SUD Services
Healthy youth outcomes are grounded in supportive family relations.
Developmental science indisputably asserts that supportive family relationships are a vital predictor of healthy development for youth. Among the truisms of positive parenting is that caregivers cannot exhibit too much love or support for their adolescents, and that the royal road to psychological autonomy and well-being is caregiver involvement and responsiveness (Steinberg & Levine, 1997). A consistent and involved familial network is also a potent resource for countervailing individual-level developmental processes that predispose youth to SU and other risky behavior, including normative escalations in sensation seeking, reward sensitivity, and delay discounting, with overall difficulties in executive inhibitory control including postponement of gratification (Christakou et al., 2013; Steinberg et al., 2009). Developmental science also confirms that the maturational processes governing risky behavior—a neurodevelopmental balance between motivation/reward and cognitive control systems—continue to reconfigure and refine from early teenage years through the mid-20s (Casey et al., 2011; Steinberg, 2014). At the social level, barometers of youth independence signal a generational change in the functional period of youth reliance on families: Compared to just fifty years ago, among youth 25 years of age, twice as many are still students, half as many are married, 50% more are living with their parents, and nearly 50% total receive financial support from caregivers (Steinberg, 2014). This dynamic of extended family interdependence begets an emerging truism of contemporary parenting: Supportive family relations remain critical for healthy development throughout emerging adulthood as young adults finalize the developmental negotiation between autonomy and connectedness.
Empirical support for involving families in youth SUD treatment is extensive.
In the past decade several literature reviews and meta-analytic studies have emphasized the top-shelf effectiveness of family-based treatment for SUD across the lifespan. Family-based treatment addresses family skills (e.g., communication, coping, problem-solving), family relationships and processes, and family member relations with key extrafamilial persons and systems (Hogue et al., in press). Tanner-Smith and colleagues (2013) completed a meta-analysis that sampled 45 randomized and quasi-experimental adolescent studies reporting on 73 treatment-comparison group pairs to test the comparative effectiveness of treatment approaches; family-based models prevailed in almost every comparison, including tests against other empirically supported models. Hogue and colleagues (2018) concluded in a systematic literature review that family therapy is a well-established outpatient approach for adolescent SU that has accumulated the largest evidence base compared to all other approaches. Ariss and Fairbairn (2020) completed a meta-analysis of family-involved treatments that condensed data from 2,115 adolescents and adults across 16 independent trials. They calculated a small effect size that endured up to 12–18 months post-treatment and translated to a 5.7% reduction in SU frequency—the equivalent of approximately three fewer weeks per year of SU. They also found that family-involved treatment showed consistent impacts across client age, other characteristics, and treatment models. Moreover, both family and couple therapy produce benefits for SUD whether they are delivered as the exclusive treatment or as part of a multicomponent SUD treatment program (Hogue et al., in press).
Family involvement can be calibrated to meet the unique developmental needs of transition-age youth.
To involve families effectively in SUD services, it is essential to account for the unique developmental challenges of transition-age youth. The prevailing framework is elaborated by Arnett and colleagues, whose work synthesizes developmental science for this age group (aka emerging adults) to delineate the normative psychosocial challenges pervading their beliefs and behaviors (see Arnett, 2000; Arnett, 2015) as well as how these challenges intersect with SU and SUD service delivery (e.g., Bergman et al., 2016; Smith et al., 2014; Sussman & Arnett, 2014). This framework casts the overarching developmental theme for transition-age youth as independence seeking, a meta-label for the five psychosocial challenges: personal identity exploration, familial and societal role instability, self-focus, feeling in-between childhood and adulthood, and future possibilities (Arnett, 2000). Independence factors that impact SU risk across the youth developmental span include those associated with individual characteristics (e.g., severity and peer norms of SU habits, problem-solving and self-regulation capacity, extrinsic versus intrinsic motivation, treatment stigma) and those associated with social capital (e.g., family and social network relations, educational and work achievement, housing and financial stability, general self-sufficiency) (Bergman et al., 2016; Stone et al., 2012; Sussman & Arnett, 2014).
Youth independence factors must play a large role in efforts to design strategies for involving family members in all aspects of youth SUD care. To be sure, even within the 15–26 age range, such strategies must account for developmental variation in the interaction between youth independence and expression of SUD risk and protective factors. For example, as youth age from middle adolescence to the cusp of adulthood, autonomy in decision-making and self-definition of values increase as well; accordingly, family involvement that is viewed by youth as supportive is much more influential on youth motivation for SU treatment than involvement viewed as coercive (Goodman et al., 2011).
Articulating Family Involvement across the Youth SUD Services Continuum
Behavioral health services for youth with SUD can be conceptualized as a continuum (sometimes called a “services cascade”; see Belenko et al., 2017) consisting of the routine sequence of SUD-focused activities experienced by any given youth as they progress through the care system. For heuristic purposes we have previously described this continuum as a client flow chart anchored by four overlapping phases (Hogue et al., 2021). In the Problem Identification phase, youth are identified as having serious SU and/or SU-related problems that warrant consideration for treatment. Identification can be triggered via SUD screening by youth-involved professionals (e.g., physicians, school counselors, justice system personnel) or via voluntary referral by the client. In the Treatment Engagement phase, SUD treatment providers endeavor to contact identified clients and enroll them in services. In the Active Treatment phase, providers complete clinical needs assessments with enrolled clients and proceed as indicated with treatment planning and intervention delivery. In the Recovery Support phase, clients participate in post-treatment activities intended to support sobriety and/or SUD improvement and relapse prevention goals, strengthen personal and social supports, and enable progression toward a rewarding and civically productive lifestyle.
Figure 1 depicts an articulated version of the youth SUD services continuum. In each of the four phases, the figure differentiates activities that are primarily youth-focused from those that are family-focused; the latter, being the subject matter of current interest, are highlighted. In the remainder of this article we present bedrock empirical knowledge and promising opportunities for research on family involvement in each phase: family-focused problem identification, family engagement strategies, family assessment methods, family-based behavioral treatments and medication services, and family-focused recovery planning. Our intent is not to drill deeply into each area, which is well beyond the scope of this review. Instead, we endorse research-based family-oriented practices that can be immediately prioritized for adoption in routine care and identify areas primed for research innovation that we believe could significantly enhance the quality of youth SUD services moving forward.
Figure 1.
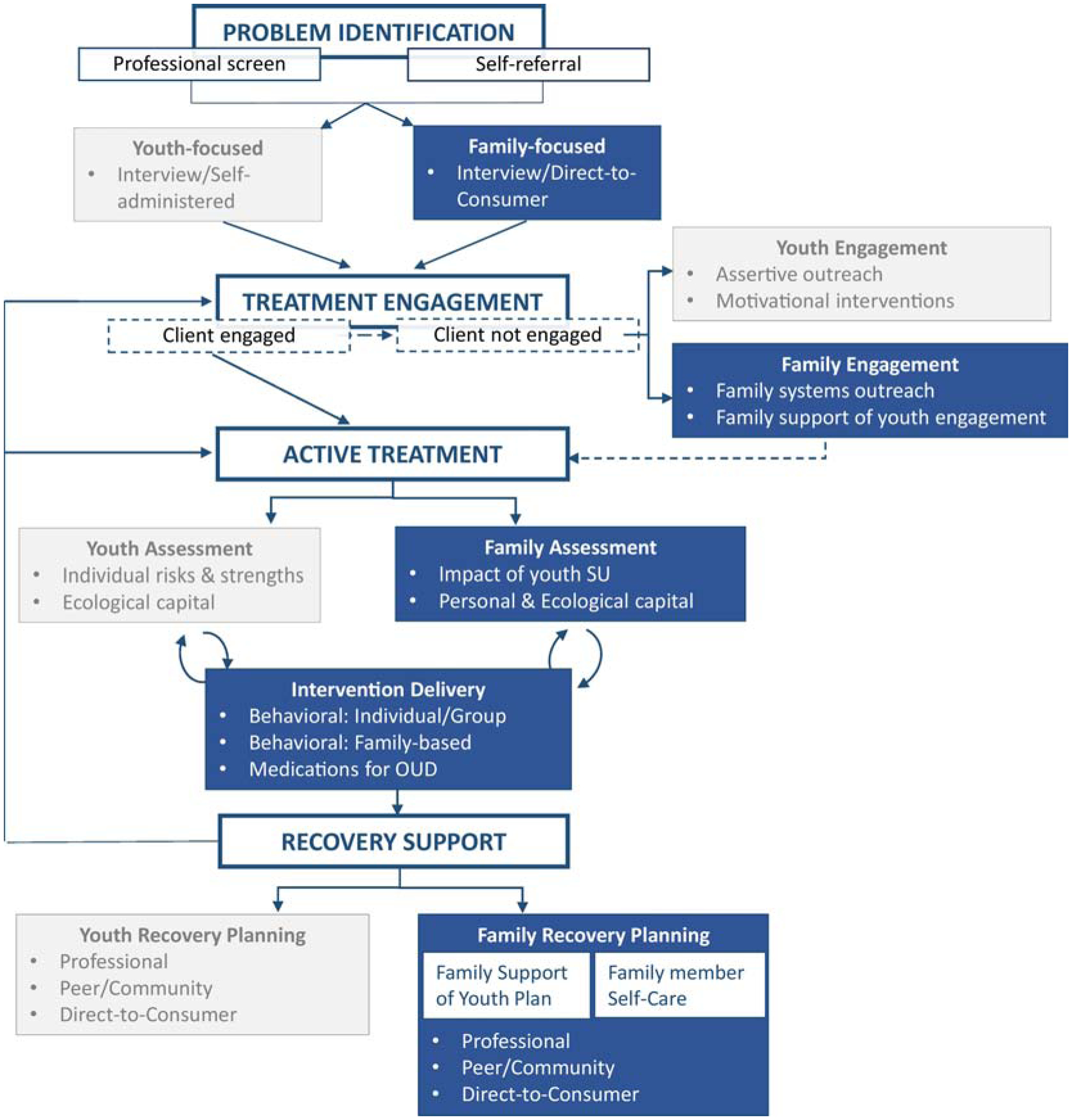
Family Involvement across Youth SUD Services Continuum: Articulated Client Flow
Two related points bear mention. First, the basic structure of the services continuum is conceptualized as similar at all levels of SUD care: outpatient, residential, inpatient. Second, as with adults, youth who enter the SUD treatment system typically experience episodic increases and decreases in use—that is, a chronic “course of disorder” marked by regular use, remission, and recurrence—over a given time span (Buckheit et al., 2018; McLellan et al., 2000). For this reason movement along the continuum is not expected to be linear, in that many youth transition both forward and backward (i.e., re-entering earlier in the continuum following a recurrence of problems) across stages.
Problem Identification
Routine SU screening is recommended as a part of routine healthcare for all youth (Levy & Williams, 2016), and evidence suggests that youth-facing healthcare providers are increasingly adopting this practice (Levy et al., 2017). However, many providers forgo validated screening tools that facilitate SUD identification and rely instead on clinical instincts, which are notably poor for detecting SU problems (Harris et al., 2012). Even when validated tools are used, rates of SU disclosure by youth in primary care remain low, in part due to ineffective implementation practices and concerns about confidentiality (Brener et al., 2003). Though self-administration of screening tools via electronic tablets has been advocated as a strategy to avert need for direct disclosure and potentially improve case finding (Levy et al., 2014), some youth choose not to disclose use even when use is suspected or has been identified by others. It is well-established that utilizing multiple sources of information to detect youth SU is more accurate than relying on any single source (Winters, 1999). Recommendations for youth screening also encourage practitioners to ask youth about family substance use, as this is a significant risk factor for youth (Winters & Kaminer, 2008).
Professional Family Screening
Bedrock.
To our knowledge there are no evidence-based screening approaches in which family members are systematically recruited to serve as sources of information on youth SU problems.
Opportunity.
Providing an opportunity for family members and other knowledgeable adults to report their observations or concerns regarding SU and related problems could enhance screening and also set the stage for a facilitated conversation that engages the family unit. Ozechowski and colleagues (2016) advocate for the no missed opportunities paradigm, in which practitioners aim to have family members complete a brief screening instrument during every youth clinical encounter. Ideally, such screening instruments are administered in parallel to youth screening tools. The goal of this conjoint approach to screening is to increase the likelihood of case detection and set the stage for family involvement in subsequent stages of the continuum. Evidence suggests that parental reports are fair-to-good proxy measures of youth substance use behavior (McGillicuddy et al., 2012), though they typically underestimate to some degree (Fisher et al., 2006). Parental report may be particularly useful when youth have minimized self-report of use or impairment. Ideally, family screening tools could help to triage youth more accurately into risk categories and increase early identification of youth who have initiated SU. Given the paucity of well-validated family screening tools, identifying and validating such measures is a priority to promote family involvement in the screening stage of the continuum.
Family Self-Referral
Bedrock.
To our knowledge there are no evidence-based strategies to guide family members toward referring their youth to SU screening and other treatment services.
Opportunity.
A potential strategy for increasing identification of youth SU problems is applying direct-to-consumer (DTC) marketing strategies to encourage families to request SU screening and associated intervention services, akin to strategies used to market psychiatric medication (Becker, 2015; Santucci et al., 2012). The most commonly reported barriers to seeking SU treatment include beliefs that treatment isn’t needed and lack of knowledge about how to access care (SAMHSA, 2020a). Marketing that directly targets families (e.g., websites, TV commercials, brochures displayed in primary care offices and schools) can increase family awareness of substance-related problems and thereby potentially increase their willingness to seek screening and intervention. In the same manner that DTC marketing for pharmaceuticals encourage people to “ask their doctor about a specific medication,” DTC marketing for SU interventions could specifically encourage families to ask their primary care doctor (or school counselor or other allied health professional) for a SU or general behavioral health screening. Recent research suggests that DTC marketing targeted towards parents is useful for promoting intentions to obtain SU treatment for their youth as long as the messaging is customized for the target population (Becker et al., 2020). National organizations such as the National Institute on Drug Abuse (https://teens.drugabuse.gov/parents) and Division of Child and Adolescent Psychology of the American Psychological Association (http://www.effectivechildtherapy.com) have employed DTC marketing to disseminate information about youth SU symptoms and treatment options to caregivers. Additional work is needed to improve the tailoring of these outreach efforts by soliciting feedback from families about their communication preferences (Becker et al., 2016).
Treatment Engagement
As seen in Figure 1, treatment engagement in youth behavioral services begins with first contact between client and provider, usually termed outreach (Becker et al., 2015). Successful outreach for youth clients requires provider commitment to promoting service accessibility and addressing potential barriers to treatment participation. Common barriers include both logistical (e.g., insufficient time, lack of resources, agency wait list) and attitudinal (e.g., perceived and actual costs versus benefits of treatment, prior unhelpful treatment experiences) obstacles experienced by both individual youth and their families (McKay & Bannon, 2004). Broadly speaking, outreach concludes when a client completes enrollment procedures and attends a first treatment session. From there, engagement interventions are used to encourage attendance and enhance readiness and motivation to participate actively (Becker et al., 2015). Research-based family engagement interventions for an array of behavioral services, derived primarily from studies on childhood populations, include emphasizing the role of family involvement in services, anticipating how family resources and dynamics could impact participation, building therapeutic alliances with multiple family members, and adroitly managing family interactions during initial clinical encounters (Becker et al., 2018; Haine-Schlagel & Walsh, 2015; Lindsey et al., 2014). These factors appear to be similar in the limited research on transition-age youth (Kim et al., 2012).
Bedrock.
In some cases, youth with SUD exhibit minimal or no readiness to enter treatment, whereas family members are motivated to assist them in doing so. A research-supported approach to boost engagement in this scenario is Community Reinforcement and Family Training (CRAFT; Smith & Meyers, 2007). A main component of CRAFT for transition-age youth is treatment entry training, which focuses on training caregivers to recognize appropriate times for them to suggest treatment, employ effective motivational strategies to endorse entry, and have treatment options available at the time a decision is made to enter (Kirby et al., 2015). CRAFT has proven superior to usual care in promoting enrollment in SUD services among both youth (Kirby et al., 2017; Waldron et al., 2007) and adults (see Archer et al., 2020), with more intensive family training producing better engagement rates (Archer et al., 2020).
In other cases, neither youth nor caregivers successfully engage with a provider during routine outreach procedures for SUD services. One evidence-based model for enhancing engagement in this scenario is Strategic Structural Systems Engagement (Szapocznik et al., 1988), which was developed on samples of high-risk youth. It teaches clinicians to recognize incompatible agendas of family members, and how this reduces the likelihood of the family attending conjointly; identify who can act as a reliable family messenger, and who has power to influence other members to attend; and provide rationale for treatment that accounts for the specific concerns of key members (Coatsworth et al., 2001; Santisteban et al., 1996).
Opportunity.
In the mental health field, family peer advocates (aka family navigators), a non-professional workforce of caregivers who connect with treatment-seeking families to provide education and help navigate enrollment barriers, have proven effective at boosting the health service literacy and self-efficacy of caregivers (see Hoagwood et al., 2018). This engagement approach has not yet been formally tested for youth with SUD (Gagne et al., 2018).
Another promising opportunity for advancing family-oriented engagement in youth SUD services is tele-intervention (Hogue et al., 2021). Given the near-ubiquity of smartphones (Smith & Page, 2015) and widespread use of the internet among youth and adults (Pew Research Center, 2020) in the US, providers can employ a comprehensive range of tele-engagement strategies. Tele-intervention’s low-cost remote delivery allows increased reach to groups with traditionally limited access to SUD services, which can reduce troubling disparities for underserved areas and populations (Gros et al., 2013). Tele-engagement also creates opportunities to counter traditional barriers to family involvement in care (see Baker-Ericzén et al., 2013) that can be protocolized and tested. For example, it offers features that protect family confidentiality, which could soften stigma-related barriers that dampen trust in providers (Livingston & Boyd, 2010). It permits family members to join “on the spot” for parts of tele-sessions, alleviating time and commuting burdens. Other engagement benefits include allowing coordinated participation of family members who live apart (Wrape & McGinn, 2019), creating direct access to home environments (Burgoyne & Cohn, 2020), and facilitating conjoint sessions with other practitioners involved in a youth’s treatment (e.g., physicians, case managers, peer counselors), which could further promote comprehensive and integrated care. As a caution, providers should take stock of functional limitations in telehealth options for those families with unreliable access to required technology platforms.
Active Treatment
Active treatment for youth SUD (see Figure 1) routinely begins with clinical assessment activities that take stock of treatment-salient youth characteristics (e.g., individual risk and strengths; ecological capital) and also family characteristics (e.g., impact of youth SUD on family members; members’ personal and ecological capital). Clinical assessment is meant to inform treatment planning and intervention delivery for each client. Intervention delivery for youth SUD typically involves individual/group behavioral services aimed at youth, family-based behavioral services, and/or OUD medication services; these types of interventions are delivered either standalone or in combination.
Clinical Family Assessment
Bedrock.
Despite longstanding evidence of the negative consequences of youth SUD on family member wellness (Schneider Institute for Health Policy, 2001), and the establishment of families as a critical resource for sustaining youth recovery (i.e., “recovery capital”; Hennessy et al., 2019), there are few validated, comprehensive tools for assessing family functioning and relations with targeted youth as a routine function of SUD treatment planning. One option is the Significant Other Survey (Benishek et al., 2012), which assesses problems experienced by family members in seven domains: emotional, relationship, family, financial, physical violence, legal, and health. More generally, several instruments are available to assess family stress and coping (e.g., Orford et al., 2005), caregiver strain and well-being (e.g., O’Malley & Qualls, 2017), and family climate (e.g., Moos & Moos, 1986), though little has been applied specifically to youth SUD treatment.
Opportunity.
As discussed above, families are lodestone sources of instrumental support and other kinds of recovery capital for transition-age youth in SUD treatment. As a starting point, clinical assessments should aim to capture the independence status (discussed above) of individual youth, focusing on factors such as education and work aspirations, financial and insurance support, family involvement and other social capital, and plans for independent living (Bergman et al., 2016; Schwartz et al., 2011; Smith et al., 2014; Stone et al., 2012; Sussman & Arnett, 2014). In addition, following Hennessy and colleagues’ (2019) model, a comprehensive measure of youth social capital would focus on four domains, each involving some aspect of family support: financial resources that enable access to recovery support and buffer youth from life stressors (e.g., stable living situation, health insurance, reliable transportation); human recovery resources used to achieve individual goals (e.g., self-efficacy and motivation, mental and physical health, religious/spiritual resources); social resources generated through an individuals’ relationship with others, especially family involvement and awareness of youths’ online connections (Anderson et al., 2018); and community resources that includes formal and informal treatment and recovery supports as well as community attitudes such as addiction-related stigma and injunctive social norms. Holistic measures would also assess how youth recovery impacts the family as a system (e.g., Edwards et al., 2018).
Another opportunity to upgrade clinical family assessment can be found in adapting existing models for assessing family involvement in child behavioral health services. A prime example is the REACH model (Becker et al., 2015; Becker et al., 2018; Lindsey et al., 2014), which provides a framework for conceptualizing and measuring use of evidence-based strategies to promote family involvement in five domains: Relationship, Expectancy, Attendance, Clarity, Homework. REACH could be leveraged to operationalize assessment of family involvement in youth SUD services, with scales and items adapted as needed for transition-age youth. Further, the model could be expanded to assess family involvement as it relates to youth recovery capital.
Intervention Delivery
Bedrock.
The extensive dossier of empirical support for involving family members in active treatment for youth SUD is summarized in the Introduction as well as in a plethora of systematic reviews and meta-analyses (e.g., Hogue et al., 2018; Hogue et al., in press; Tanner-Smith et al., 2013).
Opportunity.
SUD providers currently use various technology platforms to deliver behavioral interventions, particularly phone and video conferencing (Lin et al., 2019), and reliance on tele-intervention has skyrocketed since the outbreak of COVID-19 (US Dept Health and Human Services, 2020). Because addiction is a chronic and relapsing disorder (McLellan et al., 2000), self-management during daily routines is critical for treatment success. Yet, in conventional practice little support outside of formal treatment settings is provided to families affected by SUD, which contributes to high rates of treatment failure and relapse (Quanbeck et al., 2014). Tele-intervention’s capacity for rapid or automated response to emergent family needs via adaptive intervention software could be transformative for the field of youth SUD services, given that tele-intervention can occur when families are situated in the immediate daily environments where clients’ cravings and use most often occur (Campbell et al., 2015).
Efforts to revamp youth treatment services by increasing family involvement need to be informed by the developmental needs of transition-age youth. These include independence-related factors that are especially salient for effective SUD interventions with this age group: conceptualize SUD as a chronic medical illness with ongoing recovery, acknowledge the normalcy of autonomy-seeking and how this is a healthy developmental trope, emphasize treatment investment rather than rote compliance, support SU goals other than abstinence, address wide social network change, and employ youth-friendly communication methods (Bergman et al., 2016). The normative developmental challenge of “feeling in-between” (Arnett, 2000) corresponds to a regrettable fault line in the SUD research base, whereby transition-age youth fall between the cracks in research on family-involved treatment: They are underrepresented in samples of both family therapy studies with adolescents (Hogue et al., 2018) and couple therapy studies with adults (Hogue et al., in press). Growing a new generation of SUD treatment strategies designed to leverage the diverse family networks of transition-age youth—caregivers, extended family members, mentors, romantic partners, interdependent peers, other family-of-choice configurations—is a top clinical and research priority.
Because of the high risk of overdose among youth who misuse opioids, along with well-documented barriers to engaging youth in MOUD services (Hogue et al., 2021), it is important to develop novel strategies for involving families in MOUD. One promising family-oriented innovation is the Youth Opioid Recovery Support (YORS) intervention (Fishman et al., 2020; Wenzel & Fishman, 2020). YORS is an assertive, multi-component behavioral intervention that aims to enhance MOUD adherence and decrease opioid relapse among youth. YORS mobilizes practical parenting strategies for guiding service utilization for a young person not yet fully capable of sustaining the effort alone, while promoting youth autonomy as it strengthens with gradual maturation and healing of illness. Family involvement strategies include family member role induction, MOUD education, and collaborative treatment planning that includes stipulating contingencies and back-up plans for various course-of-treatment scenarios. When youth drop out of MOUD services, YORS increases family involvement via phone calls, text messaging, linkage to peer support, and family-focused behavioral treatment sessions to support families in leveraging their relationships and resources to bolster treatment success. In a pilot trial YORS improved treatment and relapse outcomes compared to standard treatment (Fishman et al., 2020).
Two related behavioral interventions are primed to enhance youth MOUD services are family psychoeducation and shared decision-making. Family OUD education can provide structured information about OUD symptoms, disease course, impacts on multiple domains of functioning, individual differences, and MOUD practices. Family psychoeducation has been shown to increase medication and behavioral treatment adherence and outcomes (e.g., Cummings & Fristad, 2007; Lincoln et al., 2007) and improve prosocial functioning (e.g., Ferrin et al., 2014) for clients with a variety of disorders. Family psychoeducation can be paired with family-based decision-coaching (Langer & Jensen-Doss, 2018) to enhance MOUD enrollment, retention, and adherence by helping clients prioritize their healthcare values, collaboratively process youth and family attitudes about MOUD in the context of benefit-cost decisions about MOUD services, and formulate client-centered decisions about medication use (see Davis et al., 2012; Hogue et al., 2020).
Recovery Support
Recovery support services (RSS) for SUD comprise a range of services intended to promote sustained efforts to eschew or reduce SU and improve wellness (Laudet & Humphreys, 2013; Ashford et al., 2019). Over the last decade-plus, shifts in policy and insurance practices have vastly expanded the availability, accessibility, and diversity of RSS (Laudet & Humphreys, 2013), making such services a mainstay of the treatment continuum. For heuristic purposes we organize RSS into three broad categories: (1) Professional: services offered by licensed clinicians in the context of a provider-client relationship. Professional RSS are typically adjuncts to or extensions of active treatment, in line with continuing care models, in an ongoing monitoring and maintenance phase of treatment. (2) Peer/Community: support offered by persons who have similar lived experiences in the context of a peer-to-peer relationship. These include peer recovery coaching, sober educational settings, recovery community centers, and mutual help groups, which combine peer support via shared recovery experiences during group meetings and mentoring relationships with senior peers (aka sponsors) outside meetings. (3) DTC: supports offered by social media or other information brokers that are accessed directly by affected persons. These include standardized (e.g., self-help books, website bulletins) and tailored (e.g., phone or digital helplines) educational and motivational materials. When individuals use direct-to-consumer (DTC) supports without intercession from an external agent, this is considered an “unassisted” or “natural” pathway to recovery (Kelly et al., 2017). It bears emphasizing that the RSS marketplace is dominated by services aimed at individual youth rather than families (Kelly et al., 2018).
Family Support of Youth Recovery
Bedrock.
Evidence-based models of assertive continuing care (see Godley et al., 2010, 2014) stipulate that when youth transition from acute treatment to recovery maintenance, providers make strong efforts to include family members in recovery-oriented booster sessions and clinical management procedures, either intermittently or as-needed. Beyond family participation in booster sessions, there is optimism that family involvement in youth recovery management can be facilitated by digital communication with family members and technology-based family-focused recovery supports (e.g., Dennis et al., 2014). However, currently there are no empirically supported RSS approaches or programs in which families are systematically recruited to serve as instrumental supports for ongoing youth-focused recovery activities.
Opportunity.
Professionals can avail several robust youth-focused recovery management strategies to monitor youth during aftercare, encourage linkage to peer/community RSS, and reengage them in active treatment when warranted (Fisher, 2014). The effectiveness of these youth-focused strategies could be substantially enhanced by directly involving families. In accord with a family collaboration approach (Hornberger & Smith, 2011), providers can adapt family engagement interventions (described above) with the intent of cultivating RSS management partnerships with family members. This would facilitate providers and families sharing information about promoting youth recovery, as well as providers enlisting family members to become resource advocates who actively assist youth in linking to peer/community and DTC services, thereby reducing gaps in youth aftercare (Ventura & Bagley, 2017). As needed, providers can also select evidence-based family interventions (described above) as the focal approach or a featured component of booster treatment activities scheduled during recovery periods. A similar option, but with a thin evidence base, is family recovery programs that convene groups of affected family members to explore family change and wellness processes (Buckley-Walker et al., 2017; Toumbourou & Bamberg, 2008). Another professional RSS option, with mixed evidence, is working with a caregiver to design and administer home-based contingency management plans whereby youth adhere to a consensually determined reward system for progressing toward SU reduction goals or other recovery objectives (e.g., Godley et al., 2014; Letourneau et al., 2017). And there is clearly a market for, but scant research on, DTC resources designed to improve parenting habits as a facet of SUD recovery management (see Becker et al., 2017). Recent surveys conducted in outpatient (Ryan-Pettes et al., 2019) and justice settings (Folk et al., 2020) found that most caregivers desired ongoing DTC support on parenting during aftercare.
The effectiveness of peer/community and DTC supports for youth could be bolstered if those approaches intensified their commitment to helping youth augment the strength of their familial networks. Supportive personal connections with family members are themselves a critical source of social recovery capital; moreover, positive relations with family members can open access to recovery capital of other kinds (e.g., financial, community), engendering a synergistic interaction among capital domains (Hennessy et al., 2019). This may be especially salient for young adults who are estranged from their families of origin but remain connected with other concerned adults in their family-of-choice circle. Research is needed to evaluate the potential benefits of infusing peer/community and DTC services with family-oriented programming that scaffolds youth to pursue healthy (re)connection with family and (re)investment in familial goals.
Family Member Self-Care
Bedrock.
To our knowledge there are no empirically supported RSS approaches or programs that reliably enhance self-care behaviors or well-being among family members for youth with SUD.
Opportunity.
CRAFT (discussed above; Smith & Meyers, 2007) is a provider-delivered intervention sometimes advertised as effective for improving the personal well-being of parents of youth, or spouses of adults, with SUD. However, few studies have rigorously examined CRAFT impacts on the wellness of significant others (Archer et al., 2020), and findings to date are mixed (e.g., Bischof et al., 2016; Kirby et al., 2017). The field would benefit from additional research on CRAFT and other professional approaches for addressing stress and coping mechanisms, behavioral health problems, and general wellness among family members affected by youth SUD.
Regarding peer/community RSS, there is solid evidence in the mental health field for family-to-family group psychoeducation (e.g., Dixon et al., 2011), and there is a growing workforce of credentialed family-to-family (aka family-peer) advocates, many with lived experience as SUD-affected caregivers, whose focus includes helping caregivers access self-care resources (Gagne et al., 2018). However, research on peer-based RSS for SUD is quite limited in both quantity and quality (Bassuk et al., 2016; Eddie et al., 2019), with virtually no studies testing impacts on CSO wellness specifically (but see Carpenter et al., 2020). Controlled research on family-to-family parent coaching models and mutual aid groups for youth SUD would contribute enormously to understanding whether and how such services work.
For persons with SUD, mutual help groups are the most utilized peer/community RSS in the United States (Bekkering et al., 2016; Kelly et al., 2018), and comprehensive reviews have found that group attendance has positive effects on recovery among both adults (Bassuk et al., 2016; Kelly et al., 2020) and, based on a handful of studies with limited rigor, adolescents (Bekkering et al., 2016; Hennessy & Fisher, 2015). Mutual help groups are also widely available to aid family members of persons with SUD (e.g., Al-Anon), and a few studies based on member surveys have reported gains in member self-care (e.g., Timko et al., 2016). This area of recovery practice appears poised to host rigorous studies of family member service access and outcomes among families of youth with SUD.
Arguably, DTC telehealth represents the great frontier for research on supporting family member self-care. Examples of widely available DTC tele-resources that target family members include synchronous supports (i.e., real-time communication with support persons) such as helplines, peer-to-peer coaching, networking forums, and online professional- and peer-led education and mutual aid groups; and asynchronous supports (i.e., archived or posted communication) such as automated text messaging, self-directed web-based programs, and digital web support (including social media platforms) (see Molfenter et al., 2018; Muench et al., 2020). Despite this abundance, little is known about which DTC RSS tele-resources produce measurable recovery benefits among persons with SUD (Ashford et al., 2020; Nesvåg & McKay, 2018), and still less about possible benefits to family member well-being. Whereas proliferation of such resources (e.g., drugfree.org) can be deemed a benefit in itself, their value would multiply to the degree they are proven effective.
Conclusions
Advancing research, practice, and policy agendae to increase family involvement in treatment and recovery for SUD among transition-age youth remains an arduous path. Prominent gaps and barriers to involving families in youth SUD services exist at multiple levels. Practitioners often harbor biases against families as having a role in causing or sustaining (“enabling”) SU, lack skills or motivation to pursue family involvement, believe that most or all youth with SUD need unilateral individuation from their families (Hornberger & Smith, 2011), and may rigidly apply concerns about confidentiality at the expense of consensual collaboration. Agencies frequently do not prioritize family-centered outreach or treatment planning (SAMHSA, 2020b). And families themselves experience lack of resources, low confidence, and stigma-related reticence to engage with SUD systems of care (England-Kennedy & Horton, 2011).
These and other barriers have made family involvement in SUD services the exception rather than the rule. Yet, active family involvement is developmentally crucial for effecting positive outcomes and sustaining long-term recovery among youth. If properly recruited and integrated into the SUD service continuum, families could shift the balance toward efficient problem identification and treatment engagement, help consolidate active treatment gains, and facilitate routine access to youth- and family-oriented RSS. As described above, three areas of the service continuum contain little or no evidence base on involving families in SUD care: Professional Family Screening (Problem Identification), Family Self-referral (Problem Identification), and Family Member Self-Care (Recovery Support). For these areas it is all the more important to advance promising opportunities for generating an evidence base that can subsequently function as bedrock for both researchers and practitioners.
Comprehensive roadmaps of evidence-based practice for involving families in SUD treatment and recovery exist (e.g., SAMHSA, 2020b). Discovering how to put those practices to work—achieving adoption and implementation success with counselors, provider organizations, regulatory agencies, and families—is the challenge before us. We contend that to address this challenge successfully, three foundational shifts in business-as-usual SUD services must occur. First, there needs to be dynamic reconciliation of false or misleading distinctions that pervade SUD treatment and recovery practice and research: professional versus non-professional versus DTC service options; families as impediments versus allies versus affected persons needing self-care support; and youth-versus family-focused recovery planning, to name a few. The research bedrocks and opportunities described above are offered as one means to speed this process.
Second, the national SUD treatment system needs to take sober account of the myriad mechanisms by which it may inflict negative impacts on youth and families in service contexts predicated on social control, including mandated treatment that can be overly punitive, and carceral consequences for disapproved SU behaviors (e.g., Wild, 2006). Without such accounting, initiatives to increase family involvement in those contexts are as likely to pile-up harms as to promote recovery. Congruent with system changes, individual providers can take measures to counter potentially iatrogenic treatment effects by helping youth and families recognize societal constraints on personal agency, identify strengths and resiliencies, and especially for families in oppressive contexts, acts as allies for clients aiming to resist internalized oppression and navigate systems constraints (McDowell et al., 2017). Providers should also be attuned to potential harms, but also conditional benefits, of involving family members in contexts of child abuse/neglect, family violence, and other family-related trauma.
Third, the youth SUD service system needs to become rigorously relationship-oriented. The most recent annual survey of SUD provider practices (SAMHSA, 2019) does not list any clinical or therapeutic approach that is fundamentally family-based. This omission acknowledges that although most providers purport to involve families in routine programming, evidence-based family approaches are not widely practiced. Moreover, whereas a primary goal of youth recovery support is to enhance the quality of personal and family/social life, the current landscape of behavioral services offers little in terms of a framework for what optimal family relationships can or should look like during recovery (Ashford et al., 2019). To be fair, SAMHSA’s (2020b) comprehensive roadmap makes extensive recommendations for involving families in SUD treatment. Beyond aspiration, actually transforming SUD systems of care to become relationship-oriented will require greater system-wide attunement to familial relationships and to cultural context characteristics that shape user experiences of SUD services (Kirmayer et al., 2016). It will also require a shift towards relational conceptualizations of problems and solutions, more fluid and flexible roles for youth and CSO, thicker and more complex narratives of youth and family lives, and from “alone” to “together” in SUD treatment. This shift can be greatly facilitated by training providers to recognize and address stigma and unconscious biases about youth SU, and by fostering provider comfort in speaking with families openly about SU. In doing so, providers will inevitably come to understand family involvement as routinely beneficial rather than detrimental to recovery, a premise from which more effective interventions and supports are likely to emerge (Heru, 2015).
Manuscript Highlights.
Families are key resources but not routinely included in clinical practice for youth SUD
There is strong developmental and empirical rationale to increase family involvement in services
Family involvement can be increased in each stage along the SUD treatment and recovery continuum
There are bedrock findings and promising opportunities to advance research on family involvement
Acknowledgements
Aaron Hogue and Molly Bobek, Family and Adolescent Clinical Technology & Science, Partnership to End Addiction; Sara J. Becker, Center for Alcohol and Addictions Studies, Brown University School of Public Health; Kevin Wenzel and Marc Fishman, Maryland Treatment Centers; Craig E. Henderson, Department of Psychology, Sam Houston State University; Sharon Levy, Adolescent Substance Use and Addiction Program, Boston Children’s Hospital, Harvard Medical School.
This work was supported by the NIDA-funded Family Involvement in Recovery Support and Treatment (FIRST) Research Network (R24DA051946; PI: Hogue).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of Interest: none.
Contributor Information
Aaron Hogue, Partnership to End Addiction.
Sara J. Becker, Center for Alcohol and Addictions Studies at Brown University School of Public Health
Kevin Wenzel, Maryland Treatment Centers.
Craig E. Henderson, Sam Houston State University
Molly Bobek, Partnership to End Addiction.
Sharon Levy, Boston Children’s Hospital, Harvard Medical School.
Marc Fishman, Maryland Treatment Centers.
References
- Ali B, Fisher DA, Miller TR, Lawrence BA, Spicer RS, Swedler DI, & Allison J (2019). Trends in drug poisoning deaths among adolescents and young adults in the United States, 2006–2015. Journal of Studies on Alcohol and Drugs, 80, 201–210. 10.15288/jsad.2019.80.201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson M, Jiang J, & Center PR (2018). Teens, social media, and technology. https://www.pewresearch.org/internet/2018/05/31/teens-social-media-technology-2018/
- Archer M, Harwood H, Stevelink S, Rafferty L, & Greenberg N (2020). Community reinforcement and family training and rates of treatment entry: A systematic review. Addiction, 115, 1024–1037. 10.1111/add.14901 [DOI] [PubMed] [Google Scholar]
- Ariss T, & Fairbairn CE (2020). The effect of significant other involvement in treatment for substance use disorders: A meta-analysis. Journal of Consulting and Clinical Psychology, 88, 526–540. 10.1037/ccp0000495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnett JJ (2000). Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist, 55, 469. 10.1037/0003-066X.55.5.469 [DOI] [PubMed] [Google Scholar]
- Arnett JJ (ed.) (2015). The oxford handbook of emerging adulthood. NY: Oxford. [Google Scholar]
- Ashford RD, Bergman BG, Kelly JF, & Curtis B (2020). Systematic review: Digital recovery support services used to support substance use disorder recovery. Human Behavior and Emerging Technologies, 2, 18–32. 10.1002/hbe2.148 [DOI] [Google Scholar]
- Ashford RD, Brown A, Brown T, Callis J, Cleveland HH, … & Manteuffel B (2019). Defining and operationalizing the phenomena of recovery: A working definition from the recovery science research collaborative. Addiction Research & Theory, 27, 179–188. 10.1080/16066359.2018.1515352 [DOI] [Google Scholar]
- Baker-Ericzén MJ, Jenkins MM, & Haine-Schlagel R (2013). Therapist, parent, and youth perspectives of treatment barriers to family-focused community outpatient mental health services. Journal of Child and Family Studies, 22, 854–868. 10.1007/s10826-012-9644-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassuk EL, Hanson J, Greene RN, Richard M, & Laudet A (2016). Peer-delivered recovery support services for addictions in the United States: A systematic review. Journal of Substance Abuse Treatment, 63, 1–9. 10.1016/j.jsat.2016.01.003 [DOI] [PubMed] [Google Scholar]
- Becker KD, Boustani M, Gellatly R, & Chorpita BF (2018). Forty years of engagement research in children’s mental health services: Multidimensional measurement and practice elements. Journal of Clinical Child & Adolescent Psychology, 47, 1–23. 10.1080/15374416.2017.1326121 [DOI] [PubMed] [Google Scholar]
- Becker KD, Lee BR, Daleiden EL, Lindsey M, Brandt NE, & Chorpita BF (2015). The common elements of engagement in children’s mental health services: Which elements for which outcomes? Journal of Clinical Child & Adolescent Psychology, 44, 30–43. 10.1080/15374416.2013.814543 [DOI] [PubMed] [Google Scholar]
- Becker SJ (2015). Direct- to- consumer marketing: A complementary approach to traditional dissemination and implementation efforts for mental health and substance abuse interventions. Clinical Psychology: Science and Practice, 22, 85–100. 10.1111/cpsp.12086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SJ, Helseth SA, Tavares TL, Squires DD, Clark MA, Zeithaml VA, & Spirito A (2020). User-informed marketing versus standard description to drive demand for evidence-based therapy: A randomized controlled trial. American Psychologist, 75, 1038. 10.1037/amp0000635 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SJ, Hernandez L, Spirito A, & Conrad S (2017). Technology-assisted intervention for parents of adolescents in residential substance use treatment: protocol of an open trial and pilot randomized trial. Addiction Science & Clinical Practice, 12, 1. 10.1186/s13722-016-0067-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker SJ, Spirito A, & Vanmali R (2016). Perceptions of ‘evidence-based practice’ among the consumers of adolescent substance use treatment. Health Education Journal, 75, 358–369. 10.1177/0017896915581061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bekkering GE, Mariën D, Parylo O, & Hannes K (2016). The effectiveness of self-help groups for adolescent substance misuse: A systematic review. Journal of Child & Adolescent Substance Abuse, 25, 229–244. 10.1080/1067828X.2014.981772 [DOI] [Google Scholar]
- Belenko S, Knight D, Wasserman GA, Dennis M, Wiley T, Taxman FS, Oser C, Dembo R, Robertson A, & Sales J (2017). The Juvenile Justice Behavioral Health Services Cascade: A new framework for measuring unmet substance use treatment services needs among adolescent offenders. Journal of Substance Abuse Treatment, 74, 80–91. 10.1016/j.jsat.2016.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benishek LA, Carter M, Clements NT, Allen C, Salber KE, Dugosh KL, & Kirby KC (2012). Psychometric assessment of a self-administered version of the Significant Other Survey. Psychology of Addictive Behaviors, 26, 986–993. 10.1037/a0030378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergman BG, Kelly JF, Nargiso JE, & McKowen JW (2016). “The Age of Feeling in-Between”: Addressing challenges in the treatment of emerging adults with substance use disorders. Cognitive and Behavioral Practice, 23, 270–288. 10.1016/j.cbpra.2015.09.008 [DOI] [Google Scholar]
- Bischof G, Iwen J, Freyer-Adam J, & Rumpf HJ (2016). Efficacy of the Community Reinforcement and Family Training for concerned significant others of treatment-refusing individuals with alcohol dependence: A randomized controlled trial. Drug and Alcohol Dependence, 163, 179–185. 10.1016/j.drugalcdep.2016.04.015 [DOI] [PubMed] [Google Scholar]
- Brener ND, Billy JO, & Grady WR (2003). Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: Evidence from the scientific literature. Journal of Adolescent Health, 33, 436–457. 10.1016/S1054-139X(03)00052-1 [DOI] [PubMed] [Google Scholar]
- Buckheit KA, Moskal D, Spinola S, & Maisto SA (2018). Clinical course and relapse among adolescents presenting for treatment of substance use disorders: Recent findings. Current Addiction Reports, 5, 174–191. 10.1007/s40429-018-0209-8 [DOI] [Google Scholar]
- Buckley-Walker K, Crowe TP, & Caputi P (2017). Personal and relational empowerment: a framework for family recovery. Advances in Dual Diagnosis, 10, 25–38. 10.1108/ADD-03-2016-0009 [DOI] [Google Scholar]
- Burgoyne N, & Cohn AS (2020). Lessons from the transition to relational teletherapy during COVID- 19. Family Process, epub ahead of print. 10.1111/famp.12589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell AN, Muench F, & Nunes EV (2015). Technology-based behavioral interventions for alcohol and drug use problems. In Marsch, Lord, & Dallery (Eds). Behavioral Healthcare and Technology: Using Science-based Innovations to Transform Practice (pp. 40 – 57). NY: Oxford. 10.1093/med/9780199314027.003.0004 [DOI] [Google Scholar]
- Carpenter KM, Foote J, Hedrick T, Collins K, & Clarkin S (2020). Building on shared experiences: The evaluation of a phone-based parent-to-parent support program for helping parents with their child’s substance misuse. Addictive Behaviors, 100, 106103. 10.1016/j.addbeh.2019.106103 [DOI] [PubMed] [Google Scholar]
- Casey BJ, Jones RM, & Somerville LH (2011). Braking and accelerating of the adolescent brain. Journal of Research on Adolescence, 21, 21–33. 10.1111/j.1532-7795.2010.00712.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christakou A, Gershman SJ, Niv Y, Simmons A, Brammer M, & Rubia K (2013). Neural and psychological maturation of decision-making in adolescence and young adulthood. Journal of Cognitive Neuroscience, 25, 1807–1823. 10.1162/jocn_a_00447 [DOI] [PubMed] [Google Scholar]
- Coatsworth JD, Santisteban DA, McBride CK, & Szapocznik J (2001). Brief strategic family therapy versus community control: Engagement, retention, and an exploration of the moderating role of adolescent symptom severity. Family Process, 40, 313–332. 10.1111/j.1545-5300.2001.4030100313.x [DOI] [PubMed] [Google Scholar]
- Cummings CM, & Fristad MA (2007). Medications prescribed for children with mood disorders: effects of a family-based psychoeducation program. Experimental and Clinical Psychopharmacology, 15, 555. 10.1037/1064-1297.15.6.555 [DOI] [PubMed] [Google Scholar]
- Davis CC, Claudius M, Palinkas LA, Wong JB, & Leslie LK (2012). Putting families in the center: family perspectives on decision making and ADHD and implications for ADHD care. Journal of Attention Disorders, 16, 675–684. 10.1177/1087054711413077 [DOI] [PubMed] [Google Scholar]
- Dennis ML, Scott CK, & Laudet A (2014). Beyond bricks and mortar: Recent research on substance use disorder recovery management. Current Psychiatry Reports, 16, 442. 10.1007/s11920-014-0442-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon LB, Lucksted A, Medoff DR, Burland J, Stewart B, Lehman AF, … & Murray-Swank A (2011). Outcomes of a randomized study of a peer-taught family-to-family education program for mental illness. Psychiatric Services, 62, 591–597. 10.1176/ps.62.6.pss6206_0591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eddie D, Hoffman L, Vilsaint C, Abry A, Bergman B, Hoeppner B, … & Kelly J (2019). Lived experience in new models of care for substance use disorder: A systematic review of peer recovery support services and recovery coaching. Frontiers in Psychology, 10, 1052. 10.3389/fpsyg.2019.01052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards M, Best D, Irving J, & Andersson C (2018). Life in recovery: A families’ perspective. Alcoholism Treatment Quarterly, 36, 437–458. 10.1080/07347324.2018.1488553 [DOI] [Google Scholar]
- England-Kennedy ES, & Horton S (2011). “Everything that I thought that they would be, they weren’t:” Family systems as support and impediment to recovery. Social Science & Medicine, 73, 1222–1229. https://dx.doi.org/10.1016%2Fj.socscimed.2011.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferrin M, Moreno-Granados JM, Salcedo-Marin MD, Ruiz-Veguilla M, Perez-Ayala V, & Taylor E (2014). Evaluation of a psychoeducation programme for parents of children and adolescents with ADHD: immediate and long-term effects using a blind randomized controlled trial. European Child & Adolescent Psychiatry, 23, 637–647. 10.1007/s00787-013-0494-7 [DOI] [PubMed] [Google Scholar]
- Fisher EA (2014). Recovery supports for young people: What do existing supports reveal about the recovery environment? Peabody Journal of Education, 89, 258–270. 10.1080/0161956X.2014.897104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher SL, Bucholz KK, Reich W, Fox L, Kuperman S, Kramer J, … & Bierut LJ (2006). Teenagers are right—Parents do not know much: An analysis of adolescent– parent agreement on reports of adolescent substance use, abuse, and dependence. Alcoholism: Clinical and Experimental Research, 30, 1699–1710. 10.1111/j.1530-0277.2006.00205.x [DOI] [PubMed] [Google Scholar]
- Fishman M, Wenzel K, Vo H, Wildberger J, & Burgower R (2020). A pilot randomized controlled trial of assertive treatment including family involvement and home delivery of medication for young adults with opioid use disorder. Addiction. 10.1111/add.15181 [DOI] [PubMed] [Google Scholar]
- Folk JB, Harrison A, Rodriguez C, Wallace A, & Tolou-Shams M (2020). Feasibility of social media-based recruitment and perceived acceptability of digital health interventions for caregivers of justice-involved youth: Mixed methods study. Journal of Medical Internet Research, 22, e16370. 10.2196/16370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagne CA, Finch WL, Myrick KJ, & Davis LM (2018). Peer workers in the behavioral and integrated health workforce: opportunities and future directions. American Journal of Preventive Medicine, 54, S258–S266. 10.1016/j.amepre.2018.03.010 [DOI] [PubMed] [Google Scholar]
- Godley SH, Garner BR, Passetti LL, Funk RR, Dennis ML, & Godley MD (2010). Adolescent outpatient treatment and continuing care: Main findings from a randomized clinical trial. Drug and Alcohol Dependence, 110, 44–54. 10.1016/j.drugalcdep.2010.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godley MD, Godley SH, Dennis ML, Funk RR, Passetti LL, & Petry NM (2014). A randomized trial of assertive continuing care and contingency management for adolescents with substance use disorders. Journal of Consulting and Clinical Psychology, 82, 40. 10.1037/a0035264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman I, Peterson-Badali M, & Henderson J (2011). Understanding motivation for substance use treatment: The role of social pressure during the transition to adulthood. Addictive Behaviors, 36, 660–668. 10.1016/j.addbeh.2011.01.011 [DOI] [PubMed] [Google Scholar]
- Gros DF, Morland LA, Greene CJ, Acierno R, Strachan M, Egede LE, … & Frueh BC (2013). Delivery of evidence-based psychotherapy via video telehealth. Journal of Psychopathology and Behavioral Assessment, 35, 506–521. 10.1007/s10862-013-9363-4 [DOI] [Google Scholar]
- Hadland SE, Wharam JF, Schuster MA, Zhang F, Samet JH, & Larochelle MR (2017). Trends in receipt of buprenorphine and naltrexone for opioid use disorder among adolescents and young adults, 2001–2014. JAMA Pediatrics, 171, 747–755. 10.1001/jamapediatrics.2017.0745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haine-Schlagel R, & Walsh NE (2015). A review of parent participation engagement in child and family mental health treatment. Clinical Child and Family Psychology Review, 18, 133–150. 10.1007/s10567-015-0182-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris SK, Herr-Zaya K, Weinstein Z, Whelton K, Perfas F Jr, Castro-Donlan C, … & Levy S (2012). Results of a statewide survey of adolescent substance use screening rates and practices in primary care. Substance Abuse, 33, 321–326. 10.1080/08897077.2011.645950 [DOI] [PubMed] [Google Scholar]
- Hennessy EA, Cristello JV, & Kelly JF (2019). RCAM: A proposed model of recovery capital for adolescents. Addiction Research & Theory, 27, 429–436. 10.1080/16066359.2018.1540694 [DOI] [Google Scholar]
- Hennessy EA, & Fisher BW (2015). A meta-analysis exploring the relationship between 12-step attendance and adolescent substance use relapse. Journal of Groups in Addiction & Recovery, 10, 79–96. 10.1080/1556035X.2015.999621 [DOI] [Google Scholar]
- Heru AM (2015). Family-centered care in the outpatient general psychiatry clinic. Journal of Psychiatric Practice, 21, 381–388. 10.1097/PRA.0000000000000097 [DOI] [PubMed] [Google Scholar]
- Hoagwood KE, Olin SS, Storfer-Isser A, Kuppinger A, Shorter P, Wang NM, … & Horwitz S (2018). Evaluation of a train-the-trainers model for family peer advocates in children’s mental health. Journal of Child and Family Studies, 27, 1130–1136. 10.1007/s10826-017-0961-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Becker SJ, Fishman M, Henderson CE, & Levy S (2021). Youth OUD treatment during and after COVID: Increasing family involvement across the services continuum. Journal of Substance Abuse Treatment. 10.1016/j.jsat.2020.108159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Fisher JH, Dauber S, Bobek M, Porter N, Henderson CE, & Evans SW (2020). Randomized trial of academic training and medication decision-making for adolescents with ADHD in usual care. Journal of Clinical Child and Adolescent Psychology. 10.1080/15374416.2020.1716362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Henderson CE, Becker SJ, & Knight DK (2018). Evidence base on outpatient behavioral treatments for adolescent substance use, 2014–2017: Outcomes, treatment delivery, and promising horizons. J Clinical Child and Adolescent Psychology, 47, 499–526. 10.1080/15374416.2018.1466307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hogue A, Schumm JA, MacLean A, & Bobek M (in press). Couple and family therapy for substance use disorders: Evidence base update 2010–2019. Journal of Marital and Family Therapy. [DOI] [PubMed] [Google Scholar]
- Hornberger S, & Smith SL (2011). Family involvement in adolescent substance abuse treatment and recovery: What do we know? What lies ahead? Children and Youth Services Review, 33, S70–S76. 10.1016/j.childyouth.2011.06.016 [DOI] [Google Scholar]
- Kelly JF, Abry A, Ferri M, & Humphreys K (2020). Alcoholics anonymous and 12-step facilitation treatments for alcohol use disorder: A distillation of a 2020 Cochrane review for clinicians and policy makers. Alcohol and Alcoholism, 55, 641–651. 10.1093/alcalc/agaa050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Bergman BG, & Fallah-Sohy N (2018). Mechanisms of behavior change in 12-step approaches to recovery in young adults. Current Addiction Reports, 5, 134–145. 10.1007/s40429-018-0203-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JF, Bergman B, Hoeppner BB, Vilsaint C, & White WL (2017). Prevalence and pathways of recovery from drug and alcohol problems in the United States population: Implications for practice, research, and policy. Drug and Alcohol Dependence, 181, 162–169. 10.1016/j.drugalcdep.2017.09.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim H, Munson MR, & McKay MM (2012). Engagement in mental health treatment among adolescents and young adults: A systematic review. Child and Adolescent Social Work Journal, 29, 241–266. 10.1007/s10560-012-0256-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby KC, Benishek LA, Kerwin ME, Dugosh KL, Carpenedo CM, … & Meyers RJ (2017). Analyzing components of Community Reinforcement and Family Training (CRAFT): Is treatment entry training sufficient? Psychology of Addictive Behaviors, 31, 818. 10.1037/adb0000306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby KC, Versek B, Kerwin ME, Meyers K, Benishek LA, Bresani E, … & Meyers RJ (2015). Developing Community Reinforcement and Family Training (CRAFT) for parents of treatment-resistant adolescents. J Child & Adolescent Substance Abuse, 24, 155–165. 10.1080/1067828X.2013.777379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirmayer LJ, Bennegadi R, & Kastrup MC (2016). Cultural awareness and responsiveness in person-centered psychiatry. In Person centered psychiatry (pp. 77–95). NY: Springer. 10.1007/978-3-319-39724-5_7 [DOI] [Google Scholar]
- Langer DA, & Jensen-Doss A (2018). Shared decision-making in youth mental health care: using the evidence to plan treatments collaboratively. Journal of Clinical Child & Adolescent Psychology, 47, 821–831. 10.1080/15374416.2016.1247358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laudet AB, & Humphreys K (2013). Promoting recovery in an evolving policy context: What do we know and what do we need to know about recovery support services? Journal of Substance Abuse Treatment, 45, 126–133. 10.1016/j.jsat.2013.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Letourneau EJ, McCart MR, Sheidow AJ, & Mauro PM (2017). First evaluation of a contingency management intervention addressing adolescent substance use and sexual risk behaviors: Risk reduction therapy for adolescents. Journal of Substance Abuse Treatment, 72, 56–65. 10.1016/j.jsat.2016.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy S, Weiss R, Sherritt L, Ziemnik R, Spalding A, Van Hook S, & Shrier LA (2014). An electronic screen for triaging adolescent substance use by risk levels. JAMA Pediatrics, 168, 822–828. 10.1001/jamapediatrics.2014.774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy S, & Williams JF (2016). Substance use screening, brief intervention, and referral to treatment. Pediatrics, 138. 10.1542/peds.2016-1211 [DOI] [PubMed] [Google Scholar]
- Levy S, Ziemnik RE, Harris SK, Rabinow L, Breen L, Fluet C, … & Straus JH (2017). Screening adolescents for alcohol use: tracking practice trends of Massachusetts pediatricians. Journal of Addiction Medicine, 11, 427–434. 10.1097/ADM.0000000000000340 [DOI] [PubMed] [Google Scholar]
- Lin LA, Casteel D, Shigekawa E, Weyrich MS, Roby DH, & McMenamin SB (2019). Telemedicine-delivered treatment interventions for substance use disorders: A systematic review. Journal of Substance Abuse Treatment, 101, 38–49. 10.1016/j.jsat.2019.03.007 [DOI] [PubMed] [Google Scholar]
- Lincoln TM, Wilhelm K, & Nestoriuc Y (2007). Effectiveness of psychoeducation for relapse, symptoms, knowledge, adherence and functioning in psychotic disorders: a meta-analysis. Schizophrenia Research, 96, 232–245. 10.1016/j.schres.2007.07.022 [DOI] [PubMed] [Google Scholar]
- Lindsey MA, Brandt NE, Becker KD, Lee BR, Barth RP, Daleiden EL, & Chorpita BF (2014). Identifying the common elements of treatment engagement interventions in children’s mental health services. Clinical Child and Family Psychology Review, 17, 283–298. 10.1007/s10567-013-0163-x [DOI] [PubMed] [Google Scholar]
- Livingston JD, & Boyd JE (2010). Correlates and consequences of internalized stigma for people living with mental illness: A systematic review and meta-analysis. Social Science & Medicine, 71, 2150–2161. 10.1016/j.socscimed.2010.09.030 [DOI] [PubMed] [Google Scholar]
- McDowell T, Knudson-Martin C, & Bermudez JM (2017). Socioculturally attuned family therapy: Guidelines for equitable theory and practice. Routledge. 10.4324/9781315559094 [DOI] [PubMed] [Google Scholar]
- McGillicuddy NB, Rychtarik RG, Morsheimer ET, & Bruke-Storer MR (2012). Agreement between parent and adolescent reports of adolescent substance use. Journal of Child and Adolescent Substance Abuse, 16, 59–78. 10.1300/J029v16n04_04 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay MM, & Bannon WM Jr (2004). Engaging families in child mental health services. Child and Adolescent Psychiatric Clinics, 13, 905–921. 10.1016/j.chc.2004.04.001 [DOI] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O’brien CP, & Kleber HD (2000). Drug dependence, a chronic medical illness: implications for treatment, insurance, and outcomes evaluation. JAMA, 284, 1689–1695. 10.1001/jama.284.13.1689 [DOI] [PubMed] [Google Scholar]
- Molfenter T, Brown R, O’Neill A, Kopetsky E, & Toy A (2018). Use of telemedicine in addiction treatment: Current practices and organizational implementation characteristics. International Journal of Telemedicine and Applications, 2018. 10.1155/2018/3932643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, & Moos B (1986). Family Environment Scale Manual. Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Muench F, Vitale RP, & Potenza MN (2020). 34 Digital Technologies in the Assessment and Treatment of Impulsivity and Problematic Alcohol and Drug Use. The Oxford Handbook of Digital Technologies and Mental Health, 398. 10.1093/oxfordhb/9780190218058.013.34 [DOI] [Google Scholar]
- National Center on Addiction and Substance Abuse. (2011). Adolescent substance use: America’s #1 public health problem. New York, NY: The National Center on Addiction and Substance Abuse. Retrieved from http://www.centeronaddiction.org/addiction-research/reports/adolescent-substance-use. [Google Scholar]
- Nesvåg S, & McKay JR (2018). Feasibility and effects of digital interventions to support people in recovery from substance use disorders: systematic review. Journal of Medical Internet Research, 20, e255. 10.2196/jmir.9873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Malley K & Qualls SH (2017). Preliminary evidence for the validity and reliability of the Caregiver Reaction Scale. Clinical Gerontologist, 40, 281–294. 10.1080/07317115.2016.1198858 [DOI] [PubMed] [Google Scholar]
- Orford J, Templeton L, Velleman R, & Copello A (2005). Family members of relatives with alcohol, drug and gambling problems: A set of standardized questionnaires for assessing stress, coping and strain. Addiction, 100, 1611–1624. 10.1111/j.1360-0443.2005.01178.x [DOI] [PubMed] [Google Scholar]
- Ozechowski TJ, Becker SJ, & Hogue A (2016). SBIRT-A: Adapting SBIRT to maximize developmental fit for adolescents in primary care. Journal of Substance Abuse Treatment, 62, 28–37. 10.1016/j.jsat.2015.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center (2020). Internet/Broadband fact sheet. Retrieved from: https://www.pewresearch.org/internet/fact-sheet/internet-broadband/.
- Quanbeck A, Chih MY, Isham A, Johnson R, & Gustafson D (2014). Mobile delivery of treatment for alcohol use disorders: a review of the literature. Alcohol Research: Current Reviews, 36, 111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan-Pettes SR, Lange LL, & Magnuson KI (2019). Mobile phone access and preference for technology-assisted aftercare among low-income caregivers of teens enrolled in outpatient substance use treatment: Questionnaire study. JMIR Mhealth and Uhealth, 7, e12407. 10.2196/12407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santisteban DA, Szapocznik J, Perez-Vidal A, Kurtines WM, Murray EJ, & LaPerriere A (1996). Efficacy of intervention for engaging youth and families into treatment and some variables that may contribute to differential effectiveness. Journal of Family Psychology, 10, 35. 10.1037/0893-3200.10.1.35 [DOI] [Google Scholar]
- Santucci LC, McHugh RK, & Barlow DH (2012). Direct-to-consumer marketing of evidence-based psychological interventions: Introduction. Behavior Therapy, 43, 231–235. 10.1016/j.beth.2011.07.003 [DOI] [PubMed] [Google Scholar]
- Schneider Institute for Health Policy (2001). Substance abuse: The nation’s number one health problem. Princeton, NJ: Robert Wood Johnson Foundation. [Google Scholar]
- Schwartz SJ, Beyers W, Luyckx K, Soenens B, Zamboanga BL, Forthun LF, … & Whitbourne SK (2011). Examining the light and dark sides of emerging adults’ identity: A study of identity status differences in positive and negative psychosocial functioning. Journal of Youth and Adolescence, 40, 839–859. 10.1007/s10964-010-9606-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith A, & Page D (2015). US smartphone use in 2015. Pew Research Center, 1. [Google Scholar]
- Smith DC, Bahar OS, Cleeland LR, & Davis JP (2014). Self-perceived emerging adult status and substance use. Psychology of Addictive Behaviors, 28, 935. 10.1037/a0035900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JE, & Meyers RJ (2007). Motivating substance abusers to enter treatment: Working with family members. NY: Guilford. 10.1093/alcalc/agh232 [DOI] [Google Scholar]
- Steinberg L (2014). Age of opportunity: Lessons from the new science of adolescence. NY: Houghton Mifflin Harcourt. [Google Scholar]
- Steinberg L, Graham S, O’brien L, Woolard J, Cauffman E, & Banich M (2009). Age differences in future orientation and delay discounting. Child Development, 80, 28–44. 10.1111/j.1467-8624.2008.01244.x [DOI] [PubMed] [Google Scholar]
- Steinberg L, & Levine A (1997). You and your adolescent: A parent’s guide for ages 10–20. Dunmore, PA: HarperCollins. [Google Scholar]
- Stone AL, Becker LG, Huber AM, & Catalano RF (2012). Review of risk and protective factors of substance use and problem use in emerging adulthood. Addictive Behaviors, 37, 747–775. 10.1016/j.addbeh.2012.02.014 [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2019). National Survey of Substance Abuse Treatment Services (N-SSATS): 2018. Data on Substance Abuse Treatment Facilities. Rockville, MD: SAMHSA. [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2020a). Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (HHS Publication No. PEP20–07-01-001, NSDUH Series H-55). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved: https://www.samhsa.gov/data/ [Google Scholar]
- Substance Abuse and Mental Health Services Administration (2020b). Substance Use Disorder Treatment and Family Therapy. Treatment Improvement Protocol (TIP) Series, No. 39. SAMHSA Publication No. PEP20–02-02-012. Rockville, MD: SAMHSA. [Google Scholar]
- Sussman S, & Arnett JJ (2014). Emerging adulthood: developmental period facilitative of the addictions. Evaluation & the Health Professions, 37, 147–155. 10.1177/0163278714521812 [DOI] [PubMed] [Google Scholar]
- Szapocznik J, Perez-Vidal A, Brickman AL, Foote FH, Santisteban D, Hervis O, & Kurtines WM (1988). Engaging adolescent drug abusers and their families in treatment: A strategic structural systems approach. Journal of Consulting and Clinical Psychology, 56, 552. 10.1037/0022-006X.56.4.552 [DOI] [PubMed] [Google Scholar]
- Tanner-Smith EE, Wilson SJ, & Lipsey MW (2013). The comparative effectiveness of outpatient treatment for adolescent substance abuse: A meta-analysis. Journal of Substance Abuse Treatment, 44, 145–158. 10.1016/j.jsat.2012.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Timko C, Laudet A, & Moos RH (2016). Al-Anon newcomers: Benefits of continuing attendance for six months. American J of Drug and Alcohol Abuse, 42, 441–449. 10.3109/00952990.2016.1148702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toumbourou JW, & Bamberg JH (2008). Family recovery from youth substance use related problems: A pilot study of the BEST Plus program. Substance Use & Misuse, 43, 1829. 10.1080/10826080802297385 [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services (2020). Telehealth: Delivering Care Safely During COVID-19. Website: https://www.hhs.gov/coronavirus/telehealth/index.html
- Ventura AS, & Bagley SM (2017). To improve substance use disorder prevention, treatment and recovery: engage the family. Journal of Addiction Medicine, 11, 339–341. 10.1097/ADM.0000000000000331 [DOI] [PubMed] [Google Scholar]
- Volkow ND, Jones EB, Einstein EB, & Wargo EM (2019). Prevention and treatment of opioid misuse and addiction: a review. JAMA Psychiatry, 76, 208–216. 10.1001/jamapsychiatry.2018.3126 [DOI] [PubMed] [Google Scholar]
- Vowles KE, McEntee ML, Julnes PS, Frohe T, Ney JP, & van der Goes DN (2015). Rates of opioid misuse, abuse, and addiction in chronic pain: A systematic review and data synthesis. Pain, 156, 569–576. 10.1097/01.j.pain.0000460357.01998.f1 [DOI] [PubMed] [Google Scholar]
- Waldron HB, Kern-Jones S, Turner CW, Peterson TR, & Ozechowski TJ (2007). Engaging resistant adolescents in drug abuse treatment. Journal of Substance Abuse Treatment, 32, 133–142. 10.1016/j.jsat.2006.07.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wenzel K, & Fishman M (2020). Mobile van delivery of extended-release buprenorphine and extended-release naltrexone for youth with OUD: An adaptation to the COVID-19 emergency. Journal of Substance Abuse Treatment, 108149. 10.1016/j.jsat.2020.108149 [DOI] [PubMed] [Google Scholar]
- Wild TC (2006). Social control and coercion in addiction treatment: Towards evidence- based policy and practice. Addiction, 101, 40–49. 10.1111/j.1360-0443.2005.01268.x [DOI] [PubMed] [Google Scholar]
- Winters KC (1999). Screening and assessing adolescents for substance use disorders (Treatment Improvement Protocol (TIP) Series 31. Rockville, MD: Center for Substance Abuse Treatment. [Google Scholar]
- Winters KC, & Kaminer Y (2008). Screening and assessing adolescent substance use disorders in clinical populations. Journal of the American Academy of Child and Adolescent Psychiatry, 47, 740. 10.1097/CHI.0b013e31817395cf [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wrape ER, & McGinn MM (2019). Clinical and ethical considerations for delivering couple and family therapy via telehealth. Journal of Marital and Family Therapy, 45, 296–308. 10.1111/jmft.12319 [DOI] [PubMed] [Google Scholar]


