Abstract
The emerging field of outbreak analytics calls attention to the need for data from multiple sources to inform evidence-based decision making in managing infectious diseases outbreaks. To date, these approaches have not systematically integrated evidence from social and behavioural sciences. During the 2018–2020 Ebola outbreak in Eastern Democratic Republic of the Congo, an innovative solution to systematic and timely generation of integrated and actionable social science evidence emerged in the form of the Cellulle d’Analyse en Sciences Sociales (Social Sciences Analytics Cell) (CASS), a social science analytical cell. CASS worked closely with data scientists and epidemiologists operating under the Epidemiological Cell to produce integrated outbreak analytics (IOA), where quantitative epidemiological analyses were complemented by behavioural field studies and social science analyses to help better explain and understand drivers and barriers to outbreak dynamics. The primary activity of the CASS was to conduct operational social science analyses that were useful to decision makers. This included ensuring that research questions were relevant, driven by epidemiological data from the field, that research could be conducted rapidly (ie, often within days), that findings were regularly and systematically presented to partners and that recommendations were co-developed with response actors. The implementation of the recommendations based on CASS analytics was also monitored over time, to measure their impact on response operations. This practice paper presents the CASS logic model, developed through a field-based externally led consultation, and documents key factors contributing to the usefulness and adaption of CASS and IOA to guide replication for future outbreaks.
Keywords: epidemiology, health services research, public health, viral haemorrhagic fevers, other study design
Summary box.
During the 2018–2020 Ebola outbreak in Eastern Democratic Republic of the Congo, an innovative solution to systematic and timely generation of integrated and actionable social science evidence emerged in the form of the Cellulle d’Analyse en Sciences Sociales (CASS).
The CASS worked closely with data scientists and epidemiologists operating under the Epidemiological Cell to produce integrated outbreak analytics (IOA).
IOA is a transdisciplinary approach where quantitative epidemiological analyses, health services and systems data, behavioural field studies, social science analyses, contextual data (eg, socioeconomic, population data) and operational programmes data are analysed holistically to help better explain and understand drivers and barriers to outbreak dynamics.
The CASS conducted rapid, operational social science analyses to complement epidemiological, health services and programmes data which were analysed in an integrated manner and were systematically presented and used to inform response activities and strategies.
The implementation of the recommendations based on CASS analytics was monitored over time, to measure the use of evidence and its impact on response operations.
Introduction
The 2018–2020 Ebola outbreak in Eastern Democratic Republic of the Congo (DRC) was the second largest in recorded history.1 By the time the outbreak was declared over on 25 June 2020, there had been 3481 confirmed cases, including 2299 fatalities, in an area affected by a protracted crisis due to long standing political tensions and conflicts, and widespread historic mistrust in government and public authority.2 The DRC is a country at high risk of epidemics; at the time of the 10th Ebola outbreak, the Eastern region experienced concurrent epidemics of polio, cholera, measles and plague.3 4 Coordinating an Ebola response in this challenging context required decision makers to have situational awareness of multiple aspects of a dynamic and fast-paced public health crisis from which to make timely strategic and operational decisions.5 6
The emerging field of outbreak analytics calls attention to the need for data from multiple sources to inform evidence-informed decision making in managing infectious diseases outbreaks.7 8 To date, these approaches have not systematically integrated evidence from social and behavioural sciences as a core part of integrated outbreak analytics (IOA).9 During the 2018–2020 Ebola outbreak, an innovative solution to systematic and timely generation of integrated and actionable social science evidence emerged in the form of the Cellulle d’Analyse en Sciences Sociales (CASS), a social science analytics cell. CASS was embedded within the national response structure and worked closely with data scientists and epidemiologists operating under the Epidemiological Cell to produce IOA, where quantitative epidemiological analyses were complemented by behavioural field studies and social science analyses to help better explain and understand drivers and barriers to outbreak dynamics. CASS delivered 58 integrated studies, which led to 112 evidence-informed recommendations co-developed with response pillars to improve and adapt response interventions and strategies.
This paper details the operational processes of the CASS based on an extensive review of CASS documents and tools, strategies and reports and a 2-week externally led consultation (NG University of Oxford), funded by the Wellcome Trust and UK Foreign, Commonwealth and Development Office. This consultation included interviews with 79 stakeholders from different levels of the Ebola outbreak response in the DRC to understand their views on key characteristics of the CASS model, usefulness and challenges as well as aspects that could be improved and what would be needed to replicate the model for future outbreaks. The outcome of this consultation led to refinements in how CASS achieved its outcomes and impact, and informed subsequent CASS support in the DRC to COVID-19, cholera, the 11th and 12th Ebola outbreaks as well as to the Ebola outbreak in Guinea (April 2021).10–12
The origins of CASS
The CASS developed organically and in response to needs expressed by response actors to better understand the determinants of epidemiological trends, transmission dynamics and differences across affected communities, from a holistic epidemiological, social and behavioural perspective. The studies which led to a more formal set up of CASS started in October 2018, with a UNICEF-deployed social epidemiologist (SEC). In October 2018, SEC conducted a qualitative study to better understand the situation for pregnant and lactating women who were not eligible for the vaccine and not reported by vaccination or surveillance teams. This first study directly supported response pillars including psychosocial, surveillance, vaccination and epidemiological teams to better integrate those non-eligible for the vaccine. In November 2018, Medair, an Ebola healthcare provider, requested support to better understand reasons for non-reporting or referral of suspected Ebola cases in one of their supported healthcare facilities.13 This request led to the first CASS partnership study, a qualitative study with healthcare workers and community members to better understand barriers to healthcare access. SEC led this study and provided training for Medair staff to lead future groups. In January 2019, partnerships continued to expand and included working with the Infection Prevention and Control-Water Sanitation Hygiene (IPC-WASH) pillar and WHO IPC teams to conduct studies to better understand perceptions and use of healthcare facilities and IPC measures and again, this reinforced a multiactor approach to the collection and use of data. The CASS was able to rapidly provide evidence and understanding that was relevant and adapted, responding to critical questions. The inclusion of a broad range of response actors, including government and non-government organisations within the CASS studies, reinforced relationships with the end line data users, contributing to CASS credibility and trust.
Operationalisation of the CASS during the Ebola outbreak
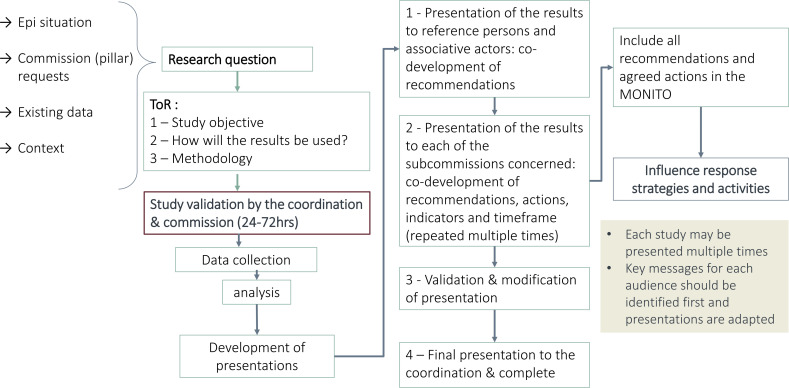
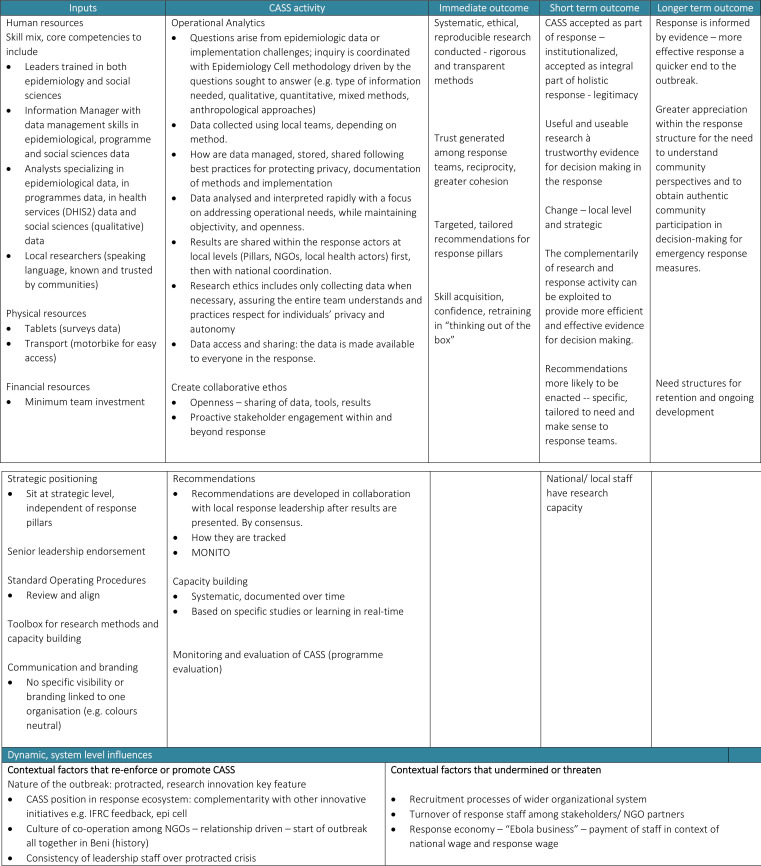
CASS was set up as an operational analytics service embedded within the national Ebola response structure. Figure 1 presents a programme logic model that sets out core activities of the service, together with their short-term, medium-term and long-term outcomes. Programme inputs were also defined to guide planning for future replication of this initiative.
Figure 1.
Flow of Cellulle d’Analyse en Sciences Sociales analytics process.
Inputs
Key human and financial resource inputs
A retrospective review of the CASS allowed for identifying the resources necessary to replicate the experience in future outbreaks and public health crises. This included detailing the human resources (multidisciplinary skillset, mix of national and international staff, levels of seniority, job descriptions, etc), physical resources (office space, research resources, etc), financial resources (budget estimates per study, budget estimates for staff posts and by location, etc), standard operating procedures, communications (advocacy documents, branding, etc) and tools for delivering analytics and building capacity of the CASS teams.
Key strategic inputs
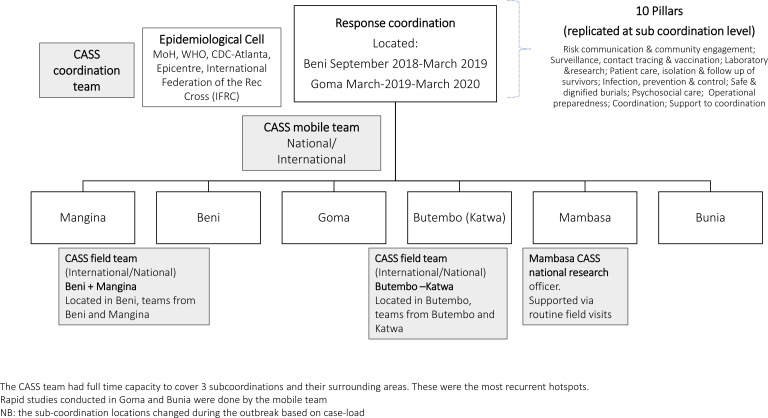
Key features related to the success of the CASS were identified. These included (1) the importance of senior leadership endorsement of the approach, (2) the practical translation and use of evidence in coordination meetings, (3) the strategic positioning of the unit, alongside the Epidemiological Cell and under the coordination and (4) physical presence at both field and response coordination level of the response, to ensure the operational relevance of key questions addressed by the CASS and that both epidemiological and sociobehavioural approaches to those could be addressed in concert. The CASS team maintained a full-time presence at (local) subcoordination-level meetings. This built trust and familiarity with the CASS and reinforced the interest of multiple stakeholders in the response to request and use CASS evidence. Subcoordination, locally based CASS teams routinely presented localised data and evidence, facilitating the co-development of recommendations and uptake of evidence-based decision-making. The strategic positioning of the CASS both at subcoordination and coordination level helped engage with local response actors and decision makers, and ensured that the evidence could be presented to multiple audiences and response pillars (figure 2).
Figure 2.
Structure and placement of Cellulle d’Analyse en Sciences Sociales (CASS) teams across the coordination and subcoordination structure of the Ebola response.13 The CASS team had full time capacity to cover three subcoordinations and their surrounding areas. These were the most recurrent hostpots. Rapid studies conducted in Goma and Bunia were done by the mobile team. Note: the subcoordination locations changed during the outbreak based on case-load. MoH, Ministry of Health.
Activities
Conducting operational social science research
The primary activity of the CASS was to conduct operational social science analyses to orient decision-making (see table 1 for examples of CASS studies). CASS research questions were prioritised in collaboration with partners and Ministry of Health (MoH) local-level and national-level leadership as a response to critical unknowns or as a complement to epidemiological analyses. Analyses from the CASS provided critical evidence on factors influencing outbreak dynamics and intervention uptake by location, specific groups and over time. CASS studies were rapidly conducted, taking 3–15 days from idea development to study outputs depending on the question and methodology applied (see figure 1 for the CASS process).
Table 1.
Additional examples of changes and impact of the use of CASS studies during the 2018–2020 Eastern Democratic Republic of the Congo Ebola outbreak
| Study | Rationale for study, key partners, study aim and methods | Results/Recommendations | Change and impact on outbreak intervention | |
| 1 | Perceptions of risk among pregnant and breastfeeding women (October 2018)18 |
Rationale: routinely collected surveillance data on uptake of the novel Ebola vaccine did not include information on pregnant or breastfeeding women as they were not considered eligible for vaccination at that time Key partner: MoH, UNICEF, surveillance pillar, psychosocial pillar Study aim: to understand views of pregnant and breastfeeding women who had been identified as contacts (self-reported) and their partners in relation to accessing the novel Ebola vaccine Methods: rapid qualitative study |
|
|
| 2 | Perceptions of infection prevention control (IPC) and healthcare services measures (January 2019)19 |
Rationale: low uptake of recommended IPC decontamination practices among local communities Key partner: MoH, IPC pillar, WHO Study aim: to understand local community views on IPC decontamination practices in order to inform community engagement and improve practice Methods: qualitative interviews and focus group discussions |
Community members saw the value and benefit of decontamination practices. Reluctance to engage with decontamination practices was linked to the fact that decontamination for Ebola was being undertaken by unknown external teams in a context of significant mistrust. For other infectious disease scenarios requiring decontamination, local community members were used to this being conducted at the level of the health facilities by local healthcare workers. |
|
| 3 | Understanding delays in treatment- seeking (July 2019)20 |
Rationale: epidemiological data highlighted continued long delays in treatment- seeking (5–12 days), increasing the risk of mortality of those affected by Ebola Key partner: MoH, Epidemiology Cell, CDC-Atlanta Study aim: to explain the potential causes in delays related to treatment-seeking among those with symptoms of Ebola Methods: meta- analysis of existing qualitative and quantitative data form CASS studies |
Barriers to treatment-seeking were largely due to misunderstanding of Ebola symptoms (posters and images focused on severe rather than more common symptoms) as well as fear that Ebola Treatment Centres would result in death. |
|
| 4 | Understanding nosocomial transmission 21 |
Rationale: epidemiological analysis indicated that, when a nosocomial transmission occurred, there was a greater likelihood of further spread Key partner: IPC-WASH pillar Study aim: to explain potential reasons and factors related to nosocomial infection Methods: integrated analysis including a meta-synthesis of healthcare worker surveys, household surveys and qualitative studies on healthcare-seeking behaviour integrated with epidemiological analysis of transmission chains, DHIS2 data and programmes data from IPC teams |
|
|
| 5 | Factors of risk for children under 5 years of age (multiple studies Octobers 2018, December 2019, March 2020)22 |
Rationale: children under 5 years of age continued to represent 14% of caseloads throughout the outbreak; however, limited understanding of the factors contributing to a greater exposure and infection than anticipated. Key partner: Epidemiology Cell Study aim: understand the factors (situation, behaviours, services use) recurrent among children under 5 years of age and drivers influencing risk and transmission among small children Methods: integrated analysis using illness narratives and verbal autopsies, DHIS2 analysis (interrupted time series), transmission chain analysis, programmes data (IPC data), household and healthcare worker surveys, epidemiological analysis, no delays in treatment-seeking, symptoms and health outcomes for children under 5 years of age |
|
|
This list is not exhaustive. A complete list of CASS studies conducted during the outbreak can be found online.23
CASS, Cellulle d’Analyse en Sciences Sociales; CDC, Centers for Disease Control and Prevention; DHIS2, The District Health Information Software (https://dhis2.org/); IPC-WASH, Infection Prevention and Control-Water Sanitation Hygiene; MoH, Ministry of Health.
Each CASS study had terms of reference (ToR) endorsed by the response leadership. As a result, MoH and response partners had some ownership of the process and in turn, could influence the uptake of recommendations based on evidence. When a study theme was identified, the CASS team would develop the ToR and rapid tools within 24–48 hours and ensure relevant approvals with local and national leadership. ToRs were rapidly approved because the analyses were requested and required to guide response interventions, and due to the close working relationships, which were established over time between the full-time field-based CASS teams, the MoH and response actors. On average, data collection was conducted over 2–6 days. Local research teams collected data in local languages. Pairs of local researchers (one asking and discussing, the second taking notes and supporting to probe on questions) collected qualitative data. Participants provided informed consent verbally, however these were not audio recorded as, in agreement with local research teams, this was often perceived as intrusive, especially in a context where distrust of the Ebola response was high. Quantitative studies required, on average, 5–7 days for data collection.
In-country CASS teams, with periodic support from the US Centers for Disease Control and Prevention (CDC-Atlanta) social and behavioural sciences teams, conducted analyses over the course of 5–10 days, using Atlas-ti (qualitative data) and Epi Info or SPSS (quantitative data). CASS team leads analysed qualitative studies at field locations and validated by local researchers validated these analyses prior to these being presented to partners. Data analysis to presentation took between 48 hours and 7 days, depending on the study and data collected.
Team structure, coordination and capacity building
The CASS team consisted of local, national and international members. Local and national staff were key to the CASS’s ability to rapidly conduct studies. These researchers were familiar with local culture, community and language and were able to rapidly build trust and respectfully gain access to households as well as to healthcare facilities and staff. The CASS local research teams were operational across the four main subcoordination areas at all time. The consistency and presence of local, permanent CASS teams at each subcoordination meant that relationships were built with the subcoordination MoH leadership as well as pillars and implementing partners. The CASS field teams actively participated in daily response meetings and presented findings on a weekly basis adapted for different audiences. A key CASS priority was to reinforce the operational research capacity of the Congolese teams. Weekly trainings of the local research teams were organised to improve their analytical skills (including qualitative and quantitative research methodology), as well as their ability to communicate results and to build relationships with stakeholders and reinforce the use of data. At the end of the outbreak, the local research teams were supported to build a small network among themselves for future, localised and evidence-based programmes and response.
Ensuring a collaborative ethos and facilitating platform
A key success of the CASS was the collaborative ethos and open sharing of all tools, studies and results. This way of working provided a shared space to link research leadership, implementing partners and donors. Although hosted, supported and championed by UNICEF, the CASS was promoted as a service for all response partners in its organisation and ownership of results.14 The CASS also sought humanitarian and government partners to contribute to its activities via data sharing or human resources, for example, via sharing healthcare facility data from partners such as Medair, data collection support from IRC and deployment of surge capacity from CDC-Atlanta and MSF-Epicentre. Hence, the CASS provided a platform to bring various actors together in order to support transdisciplinary analytics and led to the unique opportunity to bridge the gap between the worlds of field research and humanitarian practice. CASS presentations also ensured that response actors remained up-to-date with understanding of the outbreak dynamics and changes to response interventions and strategies based on evidence, creating a space for exchange and collaboration. The CASS ethos was perceived to encourage an open discourse on challenges and successes which helped to identify gaps (in analytics and interventions) and ensured evidence-based decision making for the outbreak responders (see table 1).14 The CASS used the space to obtain feedback and adapted its analyses to meet partner requests.
Knowledge mobilisation
CASS routinely presented evidence on a weekly basis at coordination and subcoordination levels. Formats of the presentation included slide deck and short briefs narrative which presented adapted and easy to understand evidence summaries for the specific audience with links to the full studies. The in-country participants in presentations and recipients of briefs included civil society organisations, local MoH, national and international non-government organisations (NGOs), strategic government leadership and donors. The presentations targeted different audiences through adapted presentations and ensured that the evidence collected was being used to inform ongoing and planned interventions. The inclusion of national-level and local-level response actors and communities was regarded as very positive to ensure co-ownership and to improve support of the interventions to contain the outbreak. Examples of local-level inclusion included1 the presentation of results directly to the local-level health leadership who participated in healthcare worker studies2; presenting to local NGOs made up of community members who could contribute to the co-development of recommendations3; returning to specific women’s associations to share and present on how evidence was being used (based on their study contributions) and4 via local researchers who, from the communities, would share back results among youth and other associations.
Co-development and monitoring recommendations
Each CASS study aimed to provide evidence that could lead to concrete, operational action for strengthening the Ebola response. Subcoordination pillars or implementing partners (local actors representing community members) co-developed recommendations after each presentation of the results. The results presented by the CASS, when appropriate, included specific community-based recommendations that had been collected. See table 1 for examples of how evidence from CASS analytics impacted the outbreak response. To ensure that the evidence was being used, between June and August 2019, the CASS and the MoH, organised a series of workshops with pillars and response actors to identify preferences for the development and monitoring of evidence-based recommendations. Following this process, the CASS developed a tool (MONITO), available online, to track and follow implementation of the co-developed recommendations. Recommendations and actions were tracked by study, by location and by pillar or actor.15 CASS local research teams in each subcoordination were responsible for following up recommendations and collecting documentation to demonstrate its application. CASS presented regular updates on progress against recommendations based on the MONITO. The bilateral exchanges and discussions with pillars supported implementation of the co-developed recommendations. MONITO highlights the use of CASS analyses to inform response interventions and the impact of using integrated social sciences evidence in outbreak response. Over the 23 months of the outbreak, the CASS was able to track 112 recommendations that were adopted and followed up using the MONITO. At the end of the outbreak, 86% of recommendations had been completely (63%) or partially (23%) implemented.
Short-term, medium-term and long-term outcomes of CASS activities
The overarching long-term goal of the CASS was to contribute to a swift end to the Ebola outbreak by integrating epidemiological analyses with evidence on social and behavioural perspectives and drivers to better understand outbreak dynamics and inform response strategies and activities. Several short-term and medium-term outcomes identified as part of the consultations are presented in the programme logic model (see figure 3). Key immediate outcomes of CASS activities include the rapid production of systematic, operational, ethical and trustworthy evidence based on the needs of the response and targeted, tailored action-oriented recommendations to inform response activities. The collaborative ethos of CASS operations was key to build trust among partners and achieve its success. In this way, the CASS became institutionalised as part of the response and gained legitimacy. This legitimacy enabled the CASS to influence change at local and strategic levels. Recommendations were more likely to be seen as credible and relevant and to be acted on. CASS recognition within UNICEF, WHO and the MoH, and participation in the strategy planning, was perceived as critical for its credibility. The participatory partnership with the MoH and the Epidemiological Cell led also to an exchange of expertise and improved the quality of epidemiological and social sciences data collection tools and of the analyses conducted. An intermediate outcome of the establishment of the CASS is it seeks to better understand broader health dynamics influencing the Ebola outbreak and community health outcomes resulting from the outbreak. The CASS also created space for the integration and use of DHIS2 data on health services use and health outcome reports from healthcare facilities across the country on a monthly basis. This integration addresses the critical need to understand preoutbreak healthcare-seeking behaviours and health outcomes which take concurrently within an outbreak. For example, understanding the relationships between the free-healthcare policy applied during the Eastern DRC Ebola outbreak, increased healthcare services use and increased risks for nosocomial infection. The CASS and Epidemiological Cell facilitated systematic integrated outbreak analytics (IOA), which aims to understand and describe epidemiological findings through the social, environmental behavioural drivers and barriers that influence outbreak dynamics and the impacts of outbreaks on communities. During the stakeholder and modelling process, this approach was recognised as creating a richer understanding of the outbreak’s dynamics and making both epidemiological and social sciences evidence more useful.
Figure 3.
Cellulle d’Analyse en Sciences Sociales (CASS) logic model.
Where is CASS now?
Since the end of the North Kivu outbreak, the CASS has been active in four events: three in the DRC (Ebola in Equateur province, cholera and COVID-19) and one in Guinea (Ebola). These experiences demonstrate the transferability of the model and its potential for expansion to respond to different disease scenarios. CASS’s response to the Equateur Ebola outbreak (2020) was a natural extension of the support provided in the Eastern region. For this event, IOA as an approach to evidence generation was successful, with 86 new recommendations produced of which 58% in November 2020 had been fully or partially applied). In the DRC, COVID-19 presented a new scenario for CASS response. CASS worked to bring in additional data sources to extend the integration of different perspectives, combining social, behavioural and health services analyses with epidemiological trends, markets and context analyses (political events and conflict).16 A key focus of CASS research has been on providing evidence of the negative impacts of COVID-19 Public Health and Social Measures on communities, notably focusing on the socioeconomic and sexual and reproductive health, nutrition and safety and security on women and girls, and aiming to influence and change response strategies.17 The adaptation has, however, presented its own challenges, in part, due to the scale of the needs (eg, the impact of the increase of the exchange has had on communities which cannot be addressed at the local level), the dispersion of the disease and the prioritisation of limited funds for the biomedical response excluding the assessment of socioeconomic impacts of COVID-19 on populations. The DRC CASS continues to have the support of the MoH and has hosted workshops supported by the MoH COVID-19 leadership to bring together different actors to understand the impacts of COVID-19 and identify opportunities to mitigate them. CASS teams have continued to provide routine support via presentations and coaching on the use of key study results, lessons learnt and supported strategies to replicate similar approaches both at a global and regional level. In the DRC, the CASS has started setting up IOA for cholera outbreak response in the East.
The 2021 Guinea Ebola outbreak provided opportunity for the CASS model to be replicated in an integrated way from the outset. An IOA cell was set up, supported by the same partners and experts with the DRC experience. Based on the success of the DRC model, the cell structure (ToR) was rapidly approved and integrated into the MoH coordination and response within weeks of the outbreak, and integrated analyses to support the response were presented from immediately thereafter. The MoH and the Agence Nationale de Sécurité sanitaire in Guinea led and WHO, UNICEF, CDC, IFRC and MSF-Epicentre, including specific deployments supported via DRC CASS leadership, staffed the cell. With support of Global Outbreak Alert and Response Network and other partnerships, mechanisms are being identified to replicate similar structures for future outbreaks.
Conclusions
In this paper, we describe the CASS as a successfully applied good practice service for integrated, operational analytics in outbreak response. A wide range of stakeholders consulted in the development of this work recognised CASS practices and technical guidance as innovative and successful in changing the way analytics are conducted and used in outbreaks.
The CASS model evolved organically in response to a critical gap in understanding of outbreak dynamics in an integrated way as well as to a need to bring outbreak response actors together for improved use of evidence in decision-making. Its success requires availability or capacity to collect data from different sources, buy-in from leadership, response teams working towards a common goal and a collaborative ethos of partners interested in an evidence-based approach to outbreak response. Uptake and effective use of evidence to inform response actions remains a challenge. The documentation of all tools, training materials as well as question banks, lessons learnt and hands on available support from CASS teams has been made available to actors working in outbreak response. In this way, others can access the CASS model and ways of working and adapt it for different contexts and outbreak scenarios, to generate and use integrated outbreak analytics for more effective response to public health emergencies.
Footnotes
Handling editor: Seye Abimbola
Twitter: @simone_tweets, @SophieMeakin, @AnokoJulienne
Collaborators: Pia Huq; Isabel Scott Moncrieff; Francklin Soung Iballa Brice; Sonya Sagan; Emilie Buttarelli; Philomene Mwanza Palaku; Jessica Petz.
Contributors: SEC set up and managed the CASS and developed and drafted the manuscript and logic model. SA-M oversaw the coordination and integration of the CASS and the Epidemiological Cell to inform response interventions and reviewed and contributed to manuscript. JPZ, CNC and CU worked as part of the UNICEF response leadership to support the CASS. They further reviewed and contributed to the manuscript revision. EVK, OlPdW, SM, PL and TJ all contributed to the in-country application of integration of CASS and Epidemiological Cell. They contributed to the manuscript review and revision. MM and DBN supervised and supported the integrated CASS and Epidemiological cells, both reviewed and revised manuscript. M-AD provided remote support to the Epidemiological Cell throughout the outbreak and contributed to manuscript review. GE-R supported remote data analysis for the CASS during the DRC Ebola outbreak and contributed to manuscript review and revision. ME contributed to the drafting of the manuscript. JNA collaborated with the CASS during the Ebola response and contributed to manuscript review. NG identified the funding for the consultation process and work described in the paper and led the consultation process to model and replicate the CASS in future outbreaks. She developed the logic model, contributed to draft and all revisions of the manuscript.
Funding: This study was funded by Wellcome Trust (BZR02530) and Foreign, Commonwealth and Development Office (BZR02530).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Rohan H, McKay G. The Ebola outbreak in the Democratic Republic of the Congo: why there is no 'silver bullet'. Nat Immunol 2020;21:591–4. 10.1038/s41590-020-0675-8 [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization . Ebola outbreak 2018-2020- North Kivu/Ituri, DRC. Available: https://www.who.int/emergencies/situations/Ebola-2019-drc- [Accessed 20 Jun 2021].
- 3.Nachega JB, Mbala-Kingebeni P, Otshudiema J, et al. The colliding epidemics of COVID-19, Ebola, and measles in the Democratic Republic of the Congo. Lancet Glob Health 2020;8:e991–2. 10.1016/S2214-109X(20)30281-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Roberts L. Polio outbreaks in the DRC threaten eradication effort. Science 2018;361:10–11. 10.1126/science.361.6397.10 [DOI] [PubMed] [Google Scholar]
- 5.Social science in humanitarian action. key considerations: the context of North Kivu Province, DRC, Aug 2018:1–8. Available: https://opendocs.ids.ac.uk/opendocs/bitstream/handle/20.500.12413/13995/SSHAP_North_Kivu_context.pdf?sequence=1&isAllowed=y
- 6.Sweet R, Bedford J, Gercama I. Politics, factions and violence: listening to local voices on Ebola, 2019. Local media update #3 (Feb-Apr 2019). Available: https://opendocs.ids.ac.uk/opendocs/bitstream/handle/20.500.12413/14497/SSHAP_Local_and_social_media_brief_3_February_April_2019.pdf%0Ahttps://www.cabdirect.org/cabdirect/abstract/20193525334
- 7.Polonsky JA, Baidjoe A, Kamvar ZN, et al. Outbreak analytics: a developing data science for Informing the response to emerging pathogens. Philos Trans R Soc Lond B Biol Sci 2019;374:374:20180276. 10.1098/rstb.2018.0276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cori A, Donnelly CA, Dorigatti I, et al. Key data for outbreak evaluation: building on the Ebola experience. Philos Trans R Soc Lond B Biol Sci 2017;372:372:20160371. 10.1098/rstb.2016.0371 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bardosh KL, de Vries DH, Abramowitz S. Integrating the social sciences in epidemic preparedness and response: a strategic framework to strengthen capacities and improve global health security. Global Health 2020;16:1–18. 10.1186/s12992-020-00652-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Social Sciences Analytics Cell (CASS) . Social science support for COVID-19: briefings from the Cellule d’Analyse en Sciences Sociales, 2020. Social science in humanitarian action platform. Available: https://www.socialscienceinaction.org/blogs-and-news/social-science-support-covid-19-briefings-cellule-danalyse-en-sciences-sociales/ [Accessed 18 Jun 2021].
- 11.Social Sciences Analytics Cell (CASS) . Tor integrated analytics cell – Google drive, 2020. Available: https://drive.google.com/drive/folders/1Rapw2LqVIwClB_XfgUWvPbwmo_JSLnnl [Accessed 18 Jun 2021].
- 12.World Health Organization . Ebola virus disease outbreak, guinea: Multi-country strategic readiness and response plan, 2021. Available: https://www.who.int/publications/m/item/ebola-guinea-multi-country-strategic-readiness-and-response-plan [Accessed 18 Jun 2021].
- 13.Ministry of Health (DRC) . Strategic response plan for the Ebola virus disease outbreak in the provinces of North Kivu and Ituri, Democratic Republic of Congo, 2019
- 14.Dewulf A, Ciza AM, Irenge L. Collective approaches to risk communication and community engagement in the Ebola response in North Kivu, Democratic Republic of Congo, 2020
- 15.Social Sciences Analytics Cell (CASS) . Documentations sur les recommendations, 2020
- 16.Carter SE, Gobat N, Pfaffmann Zambruni J, et al. What questions we should be asking about COVID-19 in humanitarian settings: perspectives from the social sciences analysis cell in the Democratic Republic of the Congo. BMJ Glob Health 2020;5:e003607. 10.1136/bmjgh-2020-003607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Social Sciences Analytics Cell (CASS) . The impacts of the COVID-19 outbreak response on women and girls in the Democratic Republic of the Congo, 2020
- 18.Social Sciences Analytics Cell (CASS) . Perceptions des risques des femmes (enceintes & allaitantes) et enfants – Google Drive, 2018. Available: https://drive.google.com/drive/folders/1UN854nB40x7uRPYQQX0gr3PxzFRzIYSp [Accessed cited 2021 Jun 20].
- 19.Social Sciences Analytics Cell (CASS) . Perceptions et comportements Du personnel de santé- Google drive, 2019. Available: https://drive.google.com/drive/folders/1bxV9PUV15qSeLFl8WCciy8LRPaJACJfG [Accessed 20 Jun 2021].
- 20.Social Sciences Analytics Cell (CASS) . Perceptions et utilisation des services de santé en fonction de l’évolution de l’épidémie et des interventions de la riposte, 2019. Available: https://drive.google.com/drive/folders/1xTvyE-VFFuiv4hXjrnKAgdA25j8tP1sU [Accessed 20 Jun 2021].
- 21.Social Sciences Analytics Cell (CASS) . Présentations EOC – Google drive, 2020. Available: https://drive.google.com/drive/folders/1hfmrFe5KgVeqloEsT2QQ-RKOLf_COtgn [Accessed 21 Jun 2021].
- 22.Social Sciences Analytics Cell (CASS) . Perception des risques d’infection de la MVE chez les enfants – Google Drive, 2020. Available: https://drive.google.com/drive/folders/1Il5e5unktQsU-Z-QTpZ4R7g-hA6Tcdw_ [Accessed 20 Jun 2021].
- 23.Social Sciences Analytics Cell (CASS) . Eastern DRC EBOLA studies- full list and access to ressources 2018-20.xlsx - Google Drive, 2020. Available: https://drive.google.com/file/d/1C4zDhNHlD-lgfdA5meomxWeKmdJtIKGw/view [Accessed 21 Jun 2021].
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available in a public, open access repository.