Abstract
Background
Pain is one of the most common and problematic symptoms encountered by patients with cancer. Due to the multifactorial aetiology, pain management of these patients frequently requires multidisciplinary interventions including conventional support and specialty palliative care. Acupuncture has been identified as a possible adjunctive therapy for symptom management in cancer pain, and there is currently no systematic review focused solely on the evidence of acupuncture on cancer pain in palliative care.
Objective
To critically analyse currently available publications regarding the use of acupuncture for pain management among patients with cancer in palliative care settings.
Methods
Multiple academic databases were searched from inception to 29 October 2020. Randomised controlled trials involving acupuncture in palliative care for treatment of cancer-related pain were synthesised. Data were extracted by two independent reviewers, and methodological quality of each included study was assessed using the Oxford Centre for Evidence-Based Medicine (OCEBM) 2011 Levels of Evidence.
Results
Five studies (n=189) were included in this systematic review. Results indicated a favourable effect of acupuncture on pain relief in palliative care for patients with cancer. According to OCEBM 2011 Levels of Evidence, they were level 2 in one case (20%), level 3 in two cases (40%) and level 4 in the remaining (40%). Low-level evidence adversely affects the reliability of findings.
Conclusions
Acupuncture may be an effective and safe treatment associated with pain reduction in the palliative care of patients with cancer. Further high-quality, adequately powered studies are needed in the future.
Keywords: cancer, pain, supportive care
Introduction
Cancer is the second highest cause of death globally, with rates rising rapidly due to an ageing population and widespread adoption of unhealthy lifestyles.1 2 Pain is one of the most frequent and problematic symptoms in cancer, with an incidence rate of 50.7% for all cancer stages, and 66.4% for advanced stages.3 It is also one of the most feared and burdensome issues of patients with cancer and interferes with significant aspects of their lives, including daily activity, social function, sleep quality and cognitive function.4 Pain can be caused by cancer and/or cancer-related treatments such as surgery, chemotherapy, radiation and hormone therapy.5 6 Uncontrolled pain can negatively impact the ability to complete activities of daily living, to maintain employment, to tolerate disease-directed therapy, and can impact emotional and psychological health. It is predicted that the number of cancer patients/survivors will reach over 20 million by 2026.7 Therefore, the population suffering from cancer-related pain will also increase. Barriers to optimal pain management in patients with cancer include medical providers’ lack of training or comfort with pain management, time constraints in busy oncology practices, concerns of medication side effects or addiction, reimbursement challenges and problems of accessing prescriptions. These barriers remain a major persistent public health challenge, calling for optimised treatment regimens.8
Due to the multifactorial and complex nature of cancer pain, treatment should be based on a multidisciplinary collaboration that includes opioid and non-opioid medications, surgical and minimal invasive interventions, psychotherapies, manipulative therapies and integrative medicine (formerly referred to as complementary medicine treatments).9 Opioid analgesics are the mainstay for cancer pain, yet up to two-thirds of patients with cancer report inadequate pain management and/or opioid-induced adverse events (AEs). Opioid analgesics may have unintended side effects including nausea, vomiting, constipation, sedation and cognitive impairment. Ten to twenty per cent of individuals cannot tolerate these AEs necessitating changes in approach to treatment.10 There is also an increased risk of addiction with long-term use of opioid medications, and many patients are reluctant to use these medications, in spite of their pain-relieving benefits.
Pain is the most common symptom among patients with cancer referred to palliative care.11 Safe and effective management for patients with cancer requires interdisciplinary care, including conventional support and specialty palliative care.12 Palliative care refers both to the active total care of patients with advanced, incurable disease, including preventing and relieving symptoms as well as improving the quality of life alongside curative treatment.13 The involvement of specialty palliative care services for patients with cancer can improve advanced care planning, quality of life (QOL), as well as patient and family satisfaction.14 15 There is an increasing number of symptom management techniques that are being offered to patients with cancer, with a lack of strong evidence about best modalities, including consideration for cost-effectiveness and sustainability.16
As pharmacological agents often are associated with side effects or potential concerns for drug interactions, other non-pharmacological interventions are especially important in the population with cancer. Ideally, these interventions would be effective, feasible and inexpensive. Acupuncture is one of the major modalities in integrative medicine. Having been practised for thousands of years, acupuncture is a traditional Chinese medical intervention involving the insertion of fine, metallic sterile needles into anatomical locations based on a system of meridians and channels theory.17 It has been considered an effective adjunct to conventional pharmacological treatments for many cancer-related symptoms, as well as medical conditions.18
Acupuncture has long been used for the treatment of pain, and substantial evidence supports acupuncture is effective in pain management.19–21 Although the exact analgesic mechanism is uncertain, it is speculated that the analgesic effect of acupuncture may be mediated by the release of opioid peptides and serotonin.22 In the past decade, acupuncture has been actively used for relieving cancer pain, as well as decreasing analgesic medication doses and side effects.23 24 Acupuncture offers a promising yet understudied approach to control the pain experienced by many patients with cancer.25 Acupuncture may be a safer approach to cancer-related pain, and could have synergy with conventional interventions by reducing pain, improving fatigue and improving QOL of patients receiving palliative care.26 There is additional evidence suggesting that acupuncture has a role in the supportive care of patients with cancer by relieving chemotherapy-induced or radiotherapy-induced nausea and vomiting, xerostomia and leucopenia.27 This has already been recommended in Clinical Practice Guideline through expert groups in oncology.28 29
A number of systematic reviews and meta-analyses have examined acupuncture for pain relief in patients with cancer. While previous findings have suggested that acupuncture has positive results in reducing cancer-related pain, studies inadequately addressed the issue of pain management in palliative care settings.30–35 The impact of acupuncture on cancer pain in palliative care was sparsely addressed in reviews of acupuncture on pain improvement, though reviews have included other symptoms such as fatigue, nausea, depression, chemotherapy-induced or radiotherapy-induced side effects for palliative care in patients with cancer.18 36–38
To our knowledge, this current systematic review is the first to address the use of acupuncture to treat cancer pain in palliative care. Therefore, the purpose of this review is to critically assess available publications regarding the use of acupuncture as palliative care for pain management in patients with cancer.
Methods
Inclusion and exclusion criteria
Studies were included if they met all of the following requirements: (1) participants ≥18 years old; (2) participants diagnosed with cancer; (3) received acupuncture therapy; (4) palliative care setting; (5) pain intensity assessed via validated measurement. We excluded studies that were not in English, research involving animals, cellular level or studies not relating to pain management.
Data sources and search strategies
A comprehensive electronic search of several databases was conducted from inception to 30 October 2020. The databases included Ovid MEDLINE(R) and Epub Ahead of Print, In-Process and Other Non-Indexed Citations and Daily, Ovid Embase, Ovid Cochrane Database of Systematic Reviews, Ovid Cochrane Central Register of Controlled Trials and Scopus.
The search strategy was designed and performed by an experienced librarian in Rochester Campus, Mayo Clinic with input from the investigators. Controlled vocabulary supplemented with keywords was used to search for studies describing acupuncture for palliative care in pain management of patients with cancer.
Study selection and data extraction
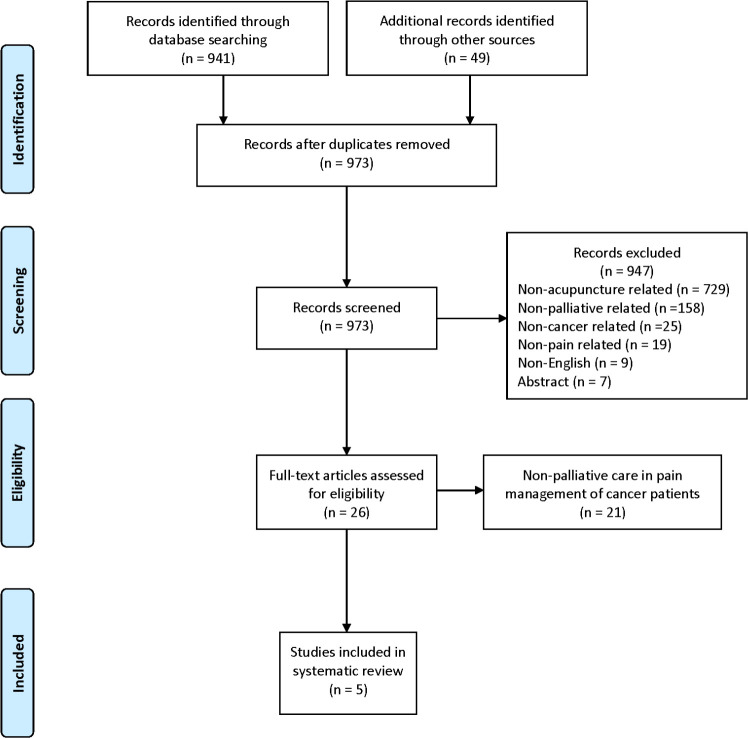
All the articles were initially selected based on their titles and abstracts. Eligibility criteria were applied to the full-text articles during the final selection. Predefined data, including the first author, publication year, country location, condition, target population, sample size, interventions, outcome, efficacy, duration, follow-up and AEs were extracted. Selection and extraction were independently completed by two investigators. Discrepancies in data selected and extracted by the investigators were resolved either through discussion with a third author or by resorting to data obtained from the original author. The whole process of study selection is summarised in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.39
Study appraisal
Quality of evidence was rated according to the Oxford Centre for Evidence-Based Medicine.40 Levels of Evidence evaluated included: level 1, randomised trials or systematic reviews of randomised trials; level 2, randomised trial or (exceptionally) observational study with dramatic effect; level 3, non-randomised controlled cohort/follow-up study; level 4, case series, case–control study or historically controlled studies; and level 5, mechanism-based reasoning. Level 1 represented the likely strongest evidence, and level 5 represented the likely weakest evidence.
Results
A total of 941 publications from the electronic databases of Ovid MEDLINE(R), Epub Ahead of Print, Embase, In-Process and Other Non-Indexed Citations and Ovid MEDLINE(R) Daily, EBM Reviews—Cochrane Database of Systematic Reviews, EBM Reviews— Cochrane Central Register of Controlled Trials using a cut-off date of 29 October 2020, and 49 from Google Scholar were reviewed in this study. Of the original 990 reviewed articles, 17 repetitious studies were excluded. Further screening excluded non-acupuncture, non-palliative, non-cancer, non-pain related, non-English and abstracted publications by examining their titles and abstracts. At the end of this screening process, 26 possible relevant studies remained. Based on selection criteria, five articles relating to the use of acupuncture for pain management in patients with cancer in palliative care settings were included in this study. Details of study selection are presented in the PRISMA flow chart (figure 1).
Figure 1.
Flowchart of the selection of clinical studies.
Five studies with 189 participants were included in this review.41–45 Reviewed articles were published between 1999 and 2019, with three studies performed in the USA,41 43 45 one in the UK44 and one in Canada.42 Two studies were retrospective chart review,41 43 and the other three were a pilot randomised controlled trial (RCT),42 a pilot prospective trial45 and a non-randomised cohort study.44 All included participants were adults. Sample sizes ranged from 20 to 68 cases. The observed interventions varied with traditional acupuncture,41 43 electroacupuncture,42 percutaneous electrical nerve stimulation (PENS), Korean hand and Japanese scalp acupuncture,41 and auricular stud.44 Stud referred to a standard ‘Seirin’ semipermanent press needle (2.9 mm×1.55 mm) inserted into the sensitive area of ears under aseptic conditions.44 The frequency and duration of the treatment session varied among the included trials. Except for the non-randomised cohort study in which medical providers were not clearly specified,44 the other acupuncture treatments of the retrospective chart review were provided by physicians certified in medical acupuncture43 or licensed acupuncturists. All the included studies focused primarily on malignant bone pain,44 cancer and cancer-related pain.
The assessment tools used to evaluate analgesic effectiveness were varied. One used subjective assessment of pain relief (ie, none, slight, moderate, good and complete) on a scale (0–4),44 and the other used the Edmonton Symptom Assessment Scale (0–10).43 All of the trials reported effective outcomes related to acupuncture therapies.
Study results showed that acupuncture provided a favourable effect on pain management for patients with cancer in palliative care. In the five studies, only one study did not mention AEs associated with acupuncture.44 Three studies reported no AEs, and one included leg stiffness and a ‘falling asleep’ sensation, which cleared without treatment after 1 hour. Therefore, in these studies, acupuncture therapy appeared to be a safe treatment for pain management. The methodological quality of the included trials was generally not strong. Based on the Oxford grading of evidence, one study was graded as level 2 (20%),42 two studies were classified as level 3 (40%)44 45 and the remaining two were level 4 (40%).41 43 Study characteristics are detailed in table 1.
Table 1.
Summary of demographic information of the included studies
| Author/year | Country | Type | Age (years) | N | Indication | Intervention | Assessment tool | Treatment sessions | Provider | Efficacy | Adverse events | Evidence level* |
| Miller et al 201943 | USA | Retrospective chart review | 31–89 | 68 | Cancer-related pain | Traditional acupuncture/Seirin filiform needles | Edmonton Symptom Assessment Scale (ESAS) | 15–40 min/ treatment, median number of treatments was 2 (range 1–13) | Palliative medicine physician certified in medical acupuncture | Acupuncture improved cancer-related pain and other symptoms | Not reported | 4 |
| Lim et al 201142 | Canada | Pilot RCT | 31–81 | 20 | Advanced cancer pain | Electroacupuncture | (ESAS) | 20 min/ treatment weekly for 4 weeks | Principal investigator, a radiation oncologist and a certified medical acupuncturist | Acupuncture had an immediate effect on all symptoms including pain and it was well tolerated | Leg stiffness; falling asleep sensation | 2 |
| Dean-Clower et al 201045 | USA | Pilot prospective trial | >21 | 32 | Advanced cancer pain | Acupuncture | Brief Pain Inventory | 12 acupuncture sessions over 8 weeks | Licensed acupuncturists | Patients’ pain severity and pain interference scores were significantly improved | None | 3 |
| Johnstone et al 200241 | USA | Retrospective chart review | 19–80 | 41 | Cancer or cancer-related pain | Traditional Chinese acupuncture, auricular acupuncture, percutaneous electrical nerve stimulation, and Korean hand and Japanese scalp acupuncture+standard allopathic care | Visual Analogue Scale | Unknown number of acupuncture sessions over 4 months | Licensed physician; acupuncturist | 55% pain patients showed at least 30% improvement, and 33% showed at least 80% improvement | None | 4 |
| Dillon and Lucas 199944 | UK | Non-randomised cohort study | 22–78 | 28 | Malignant bone pain | Auricular stud acupuncture/Seirin semipermanent press needle | Subjective assessment of pain relief (0–4 scale) | 2-week intervals for 4 weeks | – | Auricular acupuncture significantly reduced pain levels | None | 3 |
*Levels of Evidence based on the Quality Rating Scheme for Studies and Other Evidence modified from the Oxford Centre for Evidence-Based Medicine for rating of individual studies; available online at https://www.cebm.net/2016/05/ocebm-levels-of-evidence/.
RCT, randomised controlled trial.
Discussion
Our systematic review aimed to evaluate the current available evidence to determine whether acupuncture therapy is effective and safe for palliative care among patients with cancer pain. Although a considerable number of reviews concerning acupuncture for cancer pain have been published, the efficacy and safety of acupuncture for cancer pain in palliative care settings has been relatively unknown. The synthesis of the reviewed studies generated five publications including two retrospective chart reviews, one pilot RCT, a pilot prospective trial and one non-randomised cohort study. The findings from these previous studies indicated that acupuncture might be effective and safe in providing pain relief in palliative care in patients with cancer. Robust supporting evidence in the setting of palliative care is lacking, making it difficult to draw firm conclusions. More academically rigorous studies are required to examine this subject in the future.
The optimal observed interventions for studies of acupuncture are controversial. Taking into account the potential active interference of physiological or psychological effects, strict inclusion criteria were applied to reduce the heterogeneity in this review, and non-invasive acupuncture techniques in treatment groups, such as acupressure and laser acupuncture, were excluded in the screening process. Acupuncture techniques contained in this review varied, the treatment tool ranged from filiform needle, electroacupuncture, PENS, scalp acupuncture to auricular acupuncture; reported duration and frequency of sessions also varied making it difficult to define an optimal therapy session duration or frequency.
Strengths and limitations
This study is the first review acupuncture as a component of palliative care in pain management for patients with cancer. The evidence suggests that acupuncture is effective and safe in managing cancer pain in palliative settings, but the results should be interpreted cautiously due to the small number and low quality of the included studies. More high-quality studies with large sample sizes are needed in the future. However, we recognise that there are numerous hurdles to such trials, such as difficulties with recruitment, attrition, randomisation, consistency of treatment approach, duration and frequency of treatments, and conducting trials in palliative care.46 47
Beyond the research challenges, there remains a challenge from a practice perspective regarding palliative care in general. Though the WHO extended palliative care as a component of integrated treatment throughout the whole process of life-threatening illness, the clinical practice continues to face major challenges. Palliative care is very important to patients with life-threatening illnesses, but it is often misconstrued as end-of-life care, consequently resulting in referrals happening too late, and with only 10% of patients needing palliative care actually receiving it.48 Our review addresses the unmet need for acupuncture in palliative care treatment and can serve to guide further clinical studies and practice from a methodological standpoint.
Conclusions
Overall, the limited data suggest acupuncture may be safe and provide benefit in the palliative management of cancer pain. Given the methodological limitation of included trials, more high-quality clinical studies with large sample sizes are needed in the future.
Acknowledgments
The authors would like to thank the experienced librarian, Leslie C Hassett, Mayo Clinic Rochester Campus, for her significant contributions to the literature research and valuable constructive advice. We would also thank The HEAD Foundation for their support of this work.
Footnotes
Contributors: BAB and DM conceptualised the study. JY, DW and DRP designed the study. JY, XZ and MS searched, screened, extracted and analysed the data. JY and LAJ wrote the original draft. TYC, DM, BAB, AD, MS and DRP reviewed and edited the paper. All authors approved the final paper.
Funding: This study was funded by The HEAD Foundation, Singapore.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394–424. 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 2.Torre LA, Bray F, Siegel RL, et al. Global cancer statistics, 2012. CA Cancer J Clin 2015;65:87–108. 10.3322/caac.21262 [DOI] [PubMed] [Google Scholar]
- 3.van den Beuken-van Everdingen MHJ, Hochstenbach LMJ, Joosten EAJ, et al. Update on prevalence of pain in patients with cancer: systematic review and meta-analysis. J Pain Symptom Manage 2016;51:1070–90. 10.1016/j.jpainsymman.2015.12.340 [DOI] [PubMed] [Google Scholar]
- 4.Rodriguez C, Ji M, Wang H-L, et al. Cancer pain and quality of life. J Hosp Palliat Nurs 2019;21:116–23. 10.1097/NJH.0000000000000507 [DOI] [PubMed] [Google Scholar]
- 5.Fallon M, Giusti R, Aielli F, et al. Management of cancer pain in adult patients: ESMO clinical practice guidelines. Ann Oncol 2018;29:iv166–91. 10.1093/annonc/mdy152 [DOI] [PubMed] [Google Scholar]
- 6.Chiu HY, Hsieh YJ, Tsai PS. Systematic review and meta-analysis of acupuncture to reduce cancer-related pain. Eur J Cancer Care 2017;26:e12457. 10.1111/ecc.12457 [DOI] [PubMed] [Google Scholar]
- 7.Miller KD, Siegel RL, Lin CC, et al. Cancer treatment and survivorship statistics, 2016. CA Cancer J Clin 2016;66:271–89. 10.3322/caac.21349 [DOI] [PubMed] [Google Scholar]
- 8.Sanft T, Denlinger CS, Armenian S. NCCN guidelines insights: survivorship, version 2.2019: Featured updates to the NCCN guidelines. J Natl Compr Canc Netw 2019;17:784–94. 10.6004/jnccn.2019.0034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Silverman J, Gulati A, Pain C. Academic pain medicine. Springer, 2019: 177–210. [Google Scholar]
- 10.Wiffen PJ, Wee B, Derry S. Opioids for cancer pain‐an overview of Cochrane reviews. Cochrane Database Syst Rev 2017;7. 10.1002/14651858.CD012592.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Are M, McIntyre A, Reddy S. Global disparities in cancer pain management and palliative care. J Surg Oncol 2017;115:637–41. 10.1002/jso.24585 [DOI] [PubMed] [Google Scholar]
- 12.Bruera E, Paice JA. Cancer pain management: safe and effective use of opioids. Am Soc Clin Oncol Educ Book 2015;35:e593–9. 10.14694/EdBook_AM.2015.35.e593 [DOI] [PubMed] [Google Scholar]
- 13.Hartl S. Palliative care. ERS Handbook of respiratory medicine, 2019: 249. [Google Scholar]
- 14.Singer AE, Goebel JR, Kim YS, et al. Populations and interventions for palliative and end-of-life care: a systematic review. J Palliat Med 2016;19:995–1008. 10.1089/jpm.2015.0367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kavalieratos D, Corbelli J, Zhang D, et al. Association between palliative care and patient and caregiver outcomes: a systematic review and meta-analysis. JAMA 2016;316:2104–14. 10.1001/jama.2016.16840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Soares LGL. The pain Watch: it's about time to relieve cancer pain. Ann Palliat Med 2019;8:523–4. 10.21037/apm.2019.04.01 [DOI] [PubMed] [Google Scholar]
- 17.Helms JM. Acupuncture energetics: a clinical approach for physicians. Thieme, 1995. [Google Scholar]
- 18.Wu X, Chung VCH, Hui EP, et al. Effectiveness of acupuncture and related therapies for palliative care of cancer: overview of systematic reviews. Sci Rep 2015;5:16776. 10.1038/srep16776 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vickers AJ, Cronin AM, Maschino AC, et al. Acupuncture for chronic pain: individual patient data meta-analysis. Arch Intern Med 2012;172:1444–53. 10.1001/archinternmed.2012.3654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cho Y-H, Kim C-K, Heo K-H, et al. Acupuncture for acute postoperative pain after back surgery: a systematic review and meta-analysis of randomized controlled trials. Pain Pract 2015;15:279–91. 10.1111/papr.12208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murakami M, Fox L, Dijkers MP. Ear acupuncture for immediate pain Relief-A systematic review and meta-analysis of randomized controlled trials. Pain Med 2017;18:551–64. 10.1093/pm/pnw215 [DOI] [PubMed] [Google Scholar]
- 22.Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med 2002;136:374–83. 10.7326/0003-4819-136-5-200203050-00010 [DOI] [PubMed] [Google Scholar]
- 23.Lu W, Dean-Clower E, Doherty-Gilman A, et al. The value of acupuncture in cancer care. Hematol Oncol Clin North Am 2008;22:viii:631–48. 10.1016/j.hoc.2008.04.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.NIN Consensus Development Panel on Acupuncture . Acupuncture. JAMA 1998;280:1518–24. 10.1001/jama.280.17.15189809733 [DOI] [Google Scholar]
- 25.Hershman DL, Unger JM, Greenlee H, et al. Effect of acupuncture vs sham acupuncture or Waitlist control on joint pain related to aromatase inhibitors among women with early-stage breast cancer: a randomized clinical trial. JAMA 2018;320:167–76. 10.1001/jama.2018.8907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wu X, Chung VCH, Hui EP, et al. Effectiveness of acupuncture and related therapies for palliative care of cancer: overview of systematic reviews. Deutsche Zeitschrift für Akupunktur 2017;60:28–9. 10.1016/S0415-6412(17)30048-6 [DOI] [Google Scholar]
- 27.Crew KD, Capodice JL, Greenlee H, et al. Randomized, blinded, sham-controlled trial of acupuncture for the management of aromatase inhibitor-associated joint symptoms in women with early-stage breast cancer. J Clin Oncol 2010;28:1154–60. 10.1200/JCO.2009.23.4708 [DOI] [PubMed] [Google Scholar]
- 28.Birch S, Lee MS, Alraek T, et al. Evidence, safety and recommendations for when to use acupuncture for treating cancer related symptoms: a narrative review. Integr Med Res 2019;8:160–6. 10.1016/j.imr.2019.05.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Paice JA, Portenoy R, Lacchetti C, et al. Management of chronic pain in survivors of adult cancers: American Society of clinical oncology clinical practice guideline. J Clin Oncol 2016;34:3325–45. 10.1200/JCO.2016.68.5206 [DOI] [PubMed] [Google Scholar]
- 30.Chiu HY, Hsieh YJ, Tsai PS. Systematic review and meta-analysis of acupuncture to reduce cancer-related pain. Eur J Cancer Care 2017;26:e12457. 10.1111/ecc.12457 [DOI] [PubMed] [Google Scholar]
- 31.He Y, Guo X, May BH, et al. Clinical evidence for association of acupuncture and Acupressure with improved cancer pain: a systematic review and meta-analysis. JAMA Oncol 2020;6:271-278. 10.1001/jamaoncol.2019.5233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hu C, Zhang H, Wu W, et al. Acupuncture for pain management in cancer: a systematic review and meta-analysis. Evid Based Complement Alternat Med 2016;2016:1–13. 10.1155/2016/1720239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee H, Schmidt K, Ernst E. Acupuncture for the relief of cancer-related pain - a systematic review. Eur J Pain 2005;9:437–44. 10.1016/j.ejpain.2004.10.004 [DOI] [PubMed] [Google Scholar]
- 34.Paley CA, Johnson MI, Tashani OA, et al. Acupuncture for cancer pain in adults. Cochrane Database Syst Rev 2015;2015:CD007753. 10.1002/14651858.CD007753.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Paley CA, Tashani OA, Bagnall A-M, et al. A Cochrane systematic review of acupuncture for cancer pain in adults. BMJ Support Palliat Care 2011;1:51–5. 10.1136/bmjspcare-2011-000022 [DOI] [PubMed] [Google Scholar]
- 36.Lau CHY, Wu X, Chung VCH, et al. Acupuncture and related therapies for symptom management in palliative cancer care: systematic review and meta-analysis. Medicine 2016;95:e2901. 10.1097/MD.0000000000002901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lian W-L, Pan M-qi, Zhou D-han, et al. Effectiveness of acupuncture for palliative care in cancer patients: a systematic review. Chin J Integr Med 2014;20:136–47. 10.1007/s11655-013-1439-1 [DOI] [PubMed] [Google Scholar]
- 38.Towler P, Molassiotis A, Brearley SG. What is the evidence for the use of acupuncture as an intervention for symptom management in cancer supportive and palliative care: an integrative overview of reviews. Support Care Cancer 2013;21:2913–23. 10.1007/s00520-013-1882-8 [DOI] [PubMed] [Google Scholar]
- 39.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009;6:e1000100. 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Howick J, Chalmers I, Glasziou P. OCEBM Levels of Evidence Working Group ‘The Oxford 2011 Levels of Evidence’: Oxford Centre for Evidence-Based Medicine. Oxford, 2011. [Google Scholar]
- 41.Johnstone PAS, Polston GR, Niemtzow RC, et al. Integration of acupuncture into the oncology clinic. Palliat Med 2002;16:235–9. 10.1191/0269216302pm540oa [DOI] [PubMed] [Google Scholar]
- 42.Lim JTW, Wong ET, Aung SKH. Is there a role for acupuncture in the symptom management of patients receiving palliative care for cancer? A pilot study of 20 patients comparing acupuncture with nurse-led supportive care. Acupunct Med 2011;29:173–9. 10.1136/aim.2011.004044 [DOI] [PubMed] [Google Scholar]
- 43.Miller KR, Patel JN, Symanowski JT, et al. Acupuncture for cancer pain and symptom management in a palliative medicine clinic. Am J Hosp Palliat Care 2019;36:326–32. 10.1177/1049909118804464 [DOI] [PubMed] [Google Scholar]
- 44.Dillon M, Lucas C. Auricular stud acupuncture in palliative care patients. Palliat Med 1999;13:253–4. 10.1191/026921699667999073 [DOI] [PubMed] [Google Scholar]
- 45.Dean-Clower E, Doherty-Gilman AM, Keshaviah A, et al. Acupuncture as palliative therapy for physical symptoms and quality of life for advanced cancer patients. Integr Cancer Ther 2010;9:158–67. 10.1177/1534735409360666 [DOI] [PubMed] [Google Scholar]
- 46.Hudson P, Aranda S, McMurray N. Randomized controlled trials in palliative care: overcoming the obstacles. Int J Palliat Nurs 2001;7:427–34. 10.12968/ijpn.2001.7.9.9301 [DOI] [PubMed] [Google Scholar]
- 47.Holm M, Carlander I, Fürst C-J, et al. Delivering and participating in a psycho-educational intervention for family caregivers during palliative home care: a qualitative study from the perspectives of health professionals and family caregivers. BMC Palliat Care 2015;14:16. 10.1186/s12904-015-0015-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hjermstad MJ, Aass N, Aielli F, et al. Characteristics of the case mix, organisation and delivery in cancer palliative care: a challenge for good-quality research. BMJ Support Palliat Care 2018;8:456–67. 10.1136/bmjspcare-2015-000997 [DOI] [PubMed] [Google Scholar]