Abstract
To quantify the extent of patient sharing and inpatient care fragmentation among patients discharged from a cohort of Chicago hospitals. Admission and discharge dates and patient ZIP codes from 5 hospitals over 2 years were matched with an encryption algorithm. Admission to more than one hospital was considered fragmented care. The association between fragmentation and socio-economic variables using ZIP-code data from the 2000 US Census was measured. Using validation from one hospital, patient matching using encrypted identifiers had a sensitivity of 99.3 % and specificity of 100 %. The cohort contained 228,151 unique patients and 334,828 admissions. Roughly 2 % of the patients received fragmented care, accounting for 5.8 % of admissions and 6.4 % of hospital days. In 3 of 5 hospitals, and overall, the length of stay of patients with fragmented care was longer than those without. Fragmentation varied by hospital and was associated with the proportion of non-Caucasian persons, the proportion of residents whose income fell in the lowest quartile, and the proportion of residents with more children being raised by mothers alone in the zip code of the patient. Patients receiving fragmented care accounted for 6.4 % of hospital days. This percentage is a low estimate for our region, since not all regional hospitals participated, but high enough to suggest value in creating Health Information Exchange. Fragmentation varied by hospital, per capita income, race and proportion of single mother homes. This secure methodology and fragmentation analysis may prove useful for future analyses.
Keywords: Health information exchange, Health information technology, Fragmentation of care
Introduction
The fragmentation of patient care and related medical information is an oft-cited area for quality improvement in healthcare [1-5]. A central aim of primary care practice is the continuity of care across providers and sites of care delivery, with studies having demonstrated improvements in preventive services in patients with regular primary care [6-9]. The concept of Continuity of Care (COC) is well established in the ambulatory care setting, but less work on both the measurement of and clinical/economic implications of continuity of inpatient care has been performed.
A hospitalist or emergency department physician treating a new patient without critical information concerning prescriptions, test, and lab results is at a disadvantage, one in which the patient may ultimately suffer [10, 11]. Information gaps between hospitals, laboratories, pharmacies, long term care facilities, payers, and physician offices create an environment where information is not readily available at the point of care. The advent and growth of e-prescribing [12] that can improve point of care access to prescription histories certainly is helping, but information needs still exist. One of the potential solutions is health information exchange [13] (HIE), which may deliver benefits for patient safety [14, 15] as well as cost reduction [16, 17].
HIE can serve an important role in public health, particularly in infection control. For example, to reduce transmission of multidrug resistant organisms such as methicillin resistant Staphylococcus aureus (MRSA) [15, 18], an HIE can help implement timely infection control precautions upon a patient’s admission to a hospital based on records of historical MRSA colonization status from other hospital admissions [15]. An HIE can also facilitate earlier recognition of epidemics, such as monitoring the number of patients in a region with influenza-like illness [19].
Two of the most commonly expressed drawbacks of HIE are the potential loss of privacy and the lack of return on investment (ROI) for the cooperating institutions [17]. In the Chicago area this concern about the ROI has impeded prior efforts [20]. While some areas like Indiana [21] have thus far demonstrated sustainability of their HIE efforts, overall only about 14 % of hospitals in the United States are connected to any type of HIE [22].
Due to prior starts and failures in Chicago and other regions, careful consideration of the value of information exchange needs to occur in order to convince stakeholders, whether private or public, that value can be produced through the development of HIE. One method to measure value is by considering the potential for improvements in the quality of, or reductions in the cost of care for, admitted patients who have information available from another institution. If there is measurable benefit per patient, this could be multiplied by the number of admitted patients that have information available from another institution in the HIE program. Likewise, value would be proportional to the number of patients shared between institutions.
The cost of the HIE is influenced by the total number of patients in a region along with the total number of institutions due to hardware, software, planning, administrative and legal costs. Thus, the ratio of value to cost will increase as the number of shared patient’s increases. In the extremes, if no patient sharing occurs, there would be no value to HIE as no exchange will occur. If all patients were seen at all institutions, there would be maximal benefits. Therefore patient overlap between institutions should be a useful surrogate for the potential value for any regional HIE project. Measurement of the degree of sharing will be an important first step in planning and determining the value of future HIE projects in the Chicago area. In addition, this data coupled to geographic information should be useful in correlating to other geographically distributed factors which may influence healthcare.
Methods
Data encryption
To encrypt patient identifiers, we used a deterministic one-way SHA-1 hash encryption system, originally developed by the National Health Service in the United Kingdom [23]. The hash routine was performed in Microsoft Excel® using a plug in [24]. A one-way hash algorithm is an internationally accepted method of data encryption and unidirectional data sharing. Any number of variables may be entered into the algorithm, which then produces a single output unique to the specific inputs, in this case patient specific information. The following four variables were used as hash keys in our project: first name, last name, date of birth (DOB) & gender. All identifiable data were encrypted prior to being merged and analyzed outside the firewall of each institution.
Validation of encryption
The SHA-1 encryption was validated at a single hospital by comparing admissions from calendar year 2007 to 2008. A definitive match was defined as the hash code and Medical Record Number (MRN) being the same. Any instances of 2 patients having the same hash code, but different MRN’s were reviewed manually as were instances where the MRN’s were the same, but the hash codes were different to determine if a match occurred. We defined sensitivity as the proportion of admissions for an identical patient for which the encryption algorithm identified the records as being from the same patient.
Mapping
Geographic shape files for all Zip Code Tabulation Areas (ZCTAs) were obtained through the US Census Bureau website [25] and imported into ESRI’s ArcMap 10 program [26]. ZCTAs are approximations of the areas covered by postal zip codes, provided by the Census Bureau because zip codes as a geographic region are defined exclusively to the Unites States Postal Service and not used by other agencies of the government. The de-identified patient data included a zip code that had been extracted from the patient record, and this zip code was used to join patient data to the appropriate ZCTA. Patients were first mapped throughout Illinois, Wisconsin, and Indiana; it was then decided to focus on Illinois since the preliminary mapping showed only relatively small amounts of patients from neighboring states.
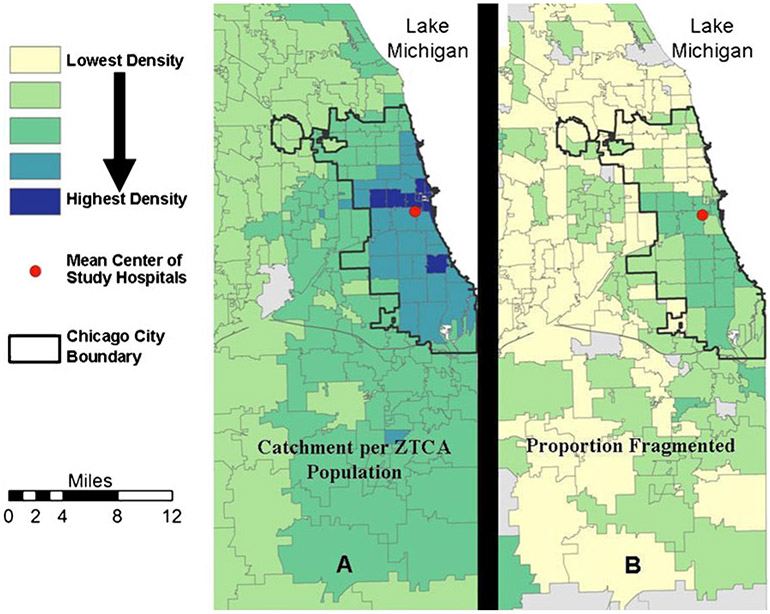
Two items were mapped in order to illustrate population distributions and look for geographic patterns. The first item mapped was the sum total of patients per ZCTA for all five hospitals (the combined hospital catchment) in our selected time frame, normalized to the total population for each ZCTA. The second item mapped was the number of patients with fragmented care per ZCTA, normalized to the total number of patients from the combined hospital catchment in each ZCTA. For both of these representations, we used the natural breaks (Jenks) method of classification [27]. To find the geographic center of the five hospitals in this study, we used the Mean Center tool from the ArcMap Spatial Statistics toolbox Measuring Geographic Distributions toolset [28].
We excluded three ZCTAs from the map of total patient population normalized to total ZCTA population due to apparent inaccuracies in the data. In all three instances, the census data indicated that there were far fewer patients residing in those ZCTAs than there were patients in the study. These ZCTA’s are in the Chicago business district and have very few residents, a total of 155 in the 2000 census. Attribution to these ZCTA’s were likely registration errors and these ZCTAs were removed completely from the analysis to prevent skewing the classification and results. Other minor errors may have occurred when matching zip codes to ZCTAs due to the age of the ZCTA data from 2000 and the fact that some zip code boundaries have changed or moved since then. However, it was necessary to use 2000 data because not all of the relevant data from the 2010 census had been released as of this analysis. In addition, the time of the study is between 2000 and 2010, making neither set of census data ideal. In the Chicago area, the main demographic trend between 2000 and 2010 was the movement of people from the edges of the city toward the center, in a generally symmetric pattern [29].
Obtaining zip code tract data
ZCTAs were only used for mapping. Zip code level social-demographic information obtained from the 2000 US Census summary file. We used that data, which is publicly available from the Census website [30], to generate aggregated ZIP code level demographic covariates for community characteristics described in further detail below.
Analysis plan
Patient admission and discharge data contained the ZIP code of the patient, but no demographic characteristics. Hence, an available alternative option to examine demographic characteristics was used that used aggregate demographic characteristics at the ZIP code level based on the ZIP code of the patient. Raw Census data at the ZIP code level was transformed for use in the subsequent multivariate logistic regression analyses. The Census tables contained population numbers overall and for several categories of race and ethnicity, including numbers of people reporting multiple races. From those data, the total population in each ZIP code that self-reported being a single race and being Caucasian, divided by the total population was calculated. Based on this calculation, ZIP codes with population more than 90 % non-Caucasian were determined.
For income, the Census directly reports per capita income. From this income, an indicator variable for those ZIP codes with per capita income in the lowest quartile of the sample (specifically, less than or equal to $13,718) was created. Also calculated was the percent of the total population in a ZIP code self-reported as having children under 18 that are being raised by single mothers, and from which we coded ZIP codes above the median on that measure.
Statistical analysis
We fit a logistic regression to examine the association between fragmentation and hospital sites, with controls for demographic characteristics at the ZIP code level. The dependent variable in the model was fragmentation coded as 1 if a patient had been admitted to more than one hospital during the observation period, or 0 otherwise. Covariates were hospital indicator, as well as controls for ZIP codes where the percent Caucasian was greater than 90 %, percent with children of single mothers above the sample median, and an indicator for per capita income being in the lowest quartile.
Results
Validation of the SHA-1 encryption
Patients from calendar year 2008 were matched to those from calendar year 2007 from a single hospital as described above. Based on analysis of the SHA-1, MRN, and chart review when the SHA-1 and MRN were discordant, the SHA-1 was found to have a sensitivity of 99.3 % and a specificity of 100 %.
Hospital and cohort characteristics
Five hospitals in the city of Chicago were selected as a convenience sample based on prior collaborations between the authors. These hospitals had no data sharing agreements at the time of the study. All admissions inclusive of January 1, 2007 and December 31, 2008 were included in the analysis. No specific information about any individual hospital is presented. The total number of beds for our 5 hospital cohort is 3191. A patient with fragmented care was defined as a patient who was admitted to more than 1 hospital during the observation period. There were a total of 334,828 admissions of 228,151 unique patients.
Characteristics of patients with fragmented care
Only 2.0 % of the unique patients had fragmented care over this 2 year period, but these patients contributed to 5.8 % of the admissions and 6.4 % of the hospital days as shown in Table 1. The lengths of stay in the hospitals were not equal as shown in Table 2. Overall, patients with fragmented care had a longer LOS, roughly 1/2 day more, than the patients with non-fragmented care, but this was only true in 3 of the 5 hospitals. Though not statistically significant, hospital 3 had a numerically shorter LOS in the patients with fragmented care.
Table 1.
Description of 5 hospital, 2 year, Cohort, 1/1/2007-12/31/2008
| ALL | Single admission | Multiple admission (Non-Fragmented) |
Fragmented | |
|---|---|---|---|---|
| # of Admissions | 334,828 | 177,775 (53.1 %) | 137,614 (41.1 %) | 19,439 (5.8 %) |
| # of Patients | 228,151 | 177,775 (77.9 %) | 45,700 (20.0 %) | 4,676 (2.0 %) |
| Avg. # of Admissions | 1.47 | 1.00 | 3.01 | 4.16 |
| Avg. LOSa (days) | 5.02 | 4.37 | 5.77 | 5.58 |
| Standard Deviation LOS | 8.16 | 7.90 | 8.42 | 8.09 |
| First Quartile LOS | 2 | 2 | 2 | 2 |
| Median LOS | 3 | 3 | 4 | 3 |
| Fourth Quartile LOS | 5 | 4 | 6 | 6 |
| Total Hospital Daysa | 1,674,213 | 774,610 (46.3 %) | 792,110 (47.3 %) | 107,493 (6.4 %) |
Some admissions with uncertain discharge dates were removed from the calculations of LOS and hospital days. These represented 0.37 % of admissions
Table 2.
Length of stay (LOS) as a function of fragmentation & hospital
| Total LOS (days) |
Non-fragmented LOS (days) |
Fragmented LOS (days) |
|
|---|---|---|---|
| Hospital 1 | 5.39 | 5.36 | 5.88b |
| Standard Deviation | 9.54 | 9.53 | 9.67 |
| First Quartile | 2 | 2 | 2 |
| Median LOS | 3 | 3 | 4 |
| Fourth Quartile | 6 | 5 | 6 |
| Hospital 2 | 5.04a | 4.99 | 5.59b |
| Standard Deviation | 9.06 | 9.03 | 9.33 |
| First Quartile | 2 | 2 | 1 |
| Median LOS | 3 | 3 | 3 |
| Fourth Quartile | 5 | 5 | 6 |
| Hospital 3 | 5.21a | 5.22 | 5.04ns |
| Standard Deviation | 8.44 | 8.50 | 7.65 |
| First Quartile | 2 | 2 | 2 |
| Median LOS | 3 | 3 | 3 |
| Fourth Quartile | 6 | 6 | 6 |
| Hospital 4 | 4.55a | 4.50 | 5.82b |
| Standard Deviation | 6.59 | 6.57 | 7.07 |
| First Quartile | 2 | 2 | 2 |
| Median LOS | 3 | 3 | 4 |
| Fourth Quartile | 4 | 4 | 7 |
| Hospital 5 | 5.35ns | 5.34 | 5.50ns |
| Standard Deviation | 8.32 | 8.42 | 6.96 |
| First Quartile | 2 | 2 | 2 |
| Median LOS | 3 | 3 | 3 |
| Fourth Quartile | 6 | 6 | 6 |
| All Hospitals | 5.02 | 4.98 | 5.58b |
| Standard Deviation | 8.16 | 8.16 | 8.09 |
| First Quartile | 2 | 2 | 2 |
| Median LOS | 3 | 3 | 3 |
| Fourth Quartile | 5 | 5 | 6 |
LOS in hospital’s 2,3,4 different than hospital 1, P<0.01
LOS in patients with fragmented care greater than in non-fragmented, P<0.01, ns = no significant difference
The catchment of the five hospital cohort had a fairly large geographic area. Figure 1a shows the distribution of patients in the Chicago metropolitan area, not shown is the extension of the catchment into the rest of Illinois and into neighboring states. The red point is the geographic center of the hospitals. It is near downtown Chicago, roughly 1.4 miles from Willis (Sears) Tower. Figure 1b displays the distributions of patients with fragmented care normalized to all patients in a ZCTA. The distribution shows an asymmetric concentration of patients with fragmented care to the south and west of the geographic center.
Fig. 1.
Geographic distribution of admissions & fragmented patients
Comparing Fig. 1a and b demonstrates that the highest rates of patients with fragmented care were not always from the ZCTAs that had the highest patient populations. This would suggest fragmentation for reasons other than proximity to the hospitals. Moving out from the city, the rates of concentration lessen. ZCTAs with high percentages of patients with fragmented care were likely the result of a small sample size within that ZCTA and should be considered atypical.
Asymmetry of patient sharing
The sharing of patients between specific hospitals was examined. Though the number of patients shared by 2 hospitals is the same, the proportion at each hospital compared to all patients is not the same due to the differences in the number of admissions at the different hospitals. These proportions varied from 0.40 % to 1.38 %, with a mean of 0.87 %.
HIE potential admission
One of the purposes of this analysis was to determine the utility of exchange of hospital data. To quantify the potential utility of HIE, the concept of a HIE Potential Admission is introduced. A HIE Potential Admission is an admission where there would have been data available from a prior admission in the cohort. In this way, care was taken not to double count the usefulness of potential HIE as an admission to hospital 1 prior to an admission to hospital 2 cannot be informed by data from the later admission. Only the later admission should be considered one in which HIE may have provided useful data.
Table 3 shows the proportion of HIE Potential Admissions as well as the proportion of hospital days. In 4 of the 5 hospitals there is a strong trend toward the LOS of potentially useful admission patients being longer, and this was clearly true when all admissions were looked at together. The percent of hospital days for HIE potential admissions is 3.8 %, with a range of 3 % to 5 %.
Table 3.
Analysis of HIE potential admissions
| Non-HIE potential admits LOS(days) |
HIE potential admits LOS(days) |
Difference between LOS |
HIE potential admits % admits |
HIE potential admits % Hosp Days |
|
|---|---|---|---|---|---|
| Hospital 1 | 5.38 | 5.74 | P=0.10 | 3.14 % | 3.34 % |
| Hospital 2 | 5.02 | 5.37 | P=0.07 | 4.50 % | 4.97 % |
| Hospital 3 | 5.21 | 5.09 | P>0.25 | 3.18 % | 3.11 % |
| Hospital 4 | 4.52 | 6.06 | P<0.001 | 2.25 % | 3.00 % |
| Hospital 5 | 5.34 | 5.60 | P=0.10 | 4.33 % | 4.53 % |
| All | 5.00 | 5.62 | P<0.001 | 3.28 % | 3.81 % |
Factors associated with fragmentation
Table 4 shows the results of logistic regression with fragmentation as the outcome variable, regressed on hospital indicators and several demographic factors at the ZIP code level. The regression results indicated significant differences between hospitals, using hospital A as a reference. In addition, ZIP codes with more than 90 % of the population self-reporting as being Caucasian were associated with lower levels of fragmentation. ZIP codes in the lowest quartile of per capita income were associated with higher odds of fragmentation. ZIP codes with relatively high (above the sample’s median) proportions of inhabitants reporting children under 18 being raised by a single mother were associated with higher odds of fragmentation.
Table 4.
Association of socioeconomic factors with fragmentation
| Factor | Relative risk of fragmentation |
[95 % Conf. Interval] |
P |
|---|---|---|---|
| Hospital Aa | 1.00a | N/A | N/A |
| Hospital B | 1.47 | 1.40–1.55 | <0.001 |
| Hospital C | 1.28 | 1.21–1.35 | <0.001 |
| Hospital D | 0.88 | 0.84–0.93 | <0.001 |
| Hospital E | 1.53 | 1.46–1.61 | <0.001 |
| Percent White>= 90 % | 0.63 | 0.59–0.66 | <0.001 |
| Per Capita Income in Lowest Quartile | 1.08 | 1.04–1.61 | <.001 |
| Above the Median in Percent with Kids being Raised by Single Moms | 1.79 | 1.72–1.85 | <.001 |
Hospital A used as reference
Discussion
This pilot study demonstrated that data on hospital admissions from multiple urban hospitals could be merged through a relatively low effort method that was acceptable to the institutional review boards (IRBs) of all the relevant hospitals. The resulting database is completely de-identified so that research and analysis of fragmentation, distributions of disease or a variety of uses can be performed without risk of loss of confidentiality.
The estimated degree of sharing of patients between hospitals is likely significantly lower than the actual degree of sharing of patients. The encryption and match process is likely less than 100 % efficient in merging unique individuals between hospitals due to its inability to account for any subtle changes in names or errors in recording the date of birth. A critical factor is that the pilot study examined 5 hospitals in a city with over 40 hospitals and 215 in the metropolitan area [31]. As a result, our overall estimate that patients with fragmented care constituted 6.4 % of hospital days on average is clearly lower than the estimate that would be obtained if one were to consider all hospitals in the city or metropolitan area and a perfect matching algorithm. In addition, our analysis did not examine the role of ambulatory offices, only hospitals.
It is interesting to note that the rate of sharing varied greatly, both geographically and by hospital. The percentage of shared patients admitted to each hospital ranged from 1.38 % to 0.40 %, a factor of just over 3. Review of the map of overall admissions (Fig. 1a), compared to that of patients with fragmented care (Fig. 1b), shows a distribution with a higher density of shared patients in the ZCTA’s immediately to the south and southwest of the geographic center, while overall patients have a generally higher density in the ZCTA’s to the northwest and north.
The causes of this variability in fragmentation rates are not known. One possibility is that hospitals may have different payer mixes that vary in the extent to which they direct care to a single hospital (e.g. managed care vs. traditional Medicare). There could also be changes in those plans over time. For instance, as managed care relationships change, a patient’s “home” hospital could change, while non-managed care patients do not have the concept of a home hospital outside of that which the patient uses in the context of their PCP or due to proximity to their home. Using the approach we have developed, it would be interesting to look at fragmentation over time and how fragmentation is affected by variations in insurance coverage in a given geographic area such as introduction and withdrawal of Medicare and Medicaid HMO’s, commercial HMO contracts with different groups and hospitals, and changes in the number and distribution of indigent patients. It is also important to note that some degree of fragmentation is likely associated with good care due to the need for referrals to locations with special capabilities or better outcomes. In these positive instances of fragmentation however, the need for HIE is just as urgent to appropriately utilize capabilities outside a patient’s usual hospital.
We chose to measure fragmentation as a simple yes/no dichotomous variable. This is clearly simplistic, but while multiple measures of continuity of care do exist for ambulatory care [32], to our knowledge, there is no absolute standard for the measurement of fragmented care among inpatient admissions. The common ambulatory measures, including the usual provider continuity index (UPC) [33], the continuity of care (COC) index [34] and the K index [35], have subtle flaws that do not make them appropriate for measuring inpatient fragmentation of care. Ideally a measurement of fragmentation would be maximal when the care is distributed among all hospitals in the cohort. In addition, an ideal index would also take into account temporal information, i.e. the order that admissions occur, and should be insensitive to the total number of admissions.
Recently, an index was used in a study of a large inpatient dataset in New York City [36]. Fragmentation was defined as “the number of distinct hospitals a patient visited in relation to the patient’s total number of hospitalizations”. Though more complex than our binary definition of fragmentation, this measure is not ideal as it would not take into account the variability in the proportion of hospitalizations across all of the hospitals, nor does it account for temporal information. More work needs to be done to develop acceptable measures of inpatient fragmentation. For our multivariate analysis, the dichotomous fragmentation variable was useful in helping to determine factors associated with fragmentation, but further, more sensitive analysis would benefit from a better measure of fragmentation.
Though we did not have any diagnostic or age/sex data to use to help control for confounders, it was not surprising to find that patients with fragmented care had an overall increased length of stay of roughly a half day. A recent study from Massachusetts also produced this finding [1]. Using ZIP codes as a method to connect to variables from the 2000 US census, we were able to determine some preliminary associations between fragmentation and some socio-economic variables. We found that non-Caucasian race was associated with fragmentation, as was also found in Massachusetts [1]. Per-capita income and single mother parenting were also associated with fragmentation. Additionally, the hospitals themselves were also associated with differing degrees of fragmentation. As this is a pilot study without sufficient data to control for likely confounders, these relationships are speculative and are meant as hypothesis generating, but suggest that this methodology could be further exploited to investigate any potential disparities based on socio-economic variables.
Limitations
The estimated fragmentation of patients care is an underestimate for two reasons: first, the cohort only represents a fraction of the hospitalizations in Chicago; second, the SHA-1 is designed to be specific, but any changes in names at the registration would reduce the sensitivity of the match. Our validation of the SHA-1 at a single institution is likely to be an overestimate of its performance across multiple institutions. Little was known about the actual patients and all correlations were made based on aggregate ZIP code information which allows for the risk of inappropriate generalization to patients living in that zip code as well as the inability to control for what are likely very important confounding differences in disease states.
Conclusions and future work
Data was aggregated from 5 hospitals with distinct information systems in a relatively inexpensive manner that protected patient’s protected health information (PHI). The data produced a lower bound on the degree of fragmentation and patient sharing which still contributed significantly to the number of patient days in our multihospital cohort.
Future work is planned using this method by including emergency department and ambulatory visits and certain diagnostic, demographic, and infectious disease data to produce more robust data sets. A fragmentation index is being developed to measure fragmentation in a more subtle, quantitative manner. These methodologies and data analysis should be very useful in examining population health in the Chicago area as well as helping to stage and plan true HIE.
Acknowledgments
This project was supported by grant number U18HS016973 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality. This project was also supported by the Chicago Health Information Technology Regional Extension Center (CHITREC).
Footnotes
Conflict of Interest The authors declare that they have no conflicts of interest.
Contributor Information
William L. Galanter, Department of Medicine, University of Illinois at Chicago (UIC), Chicago, USA
Andrew Applebaum, Department Computer Science, University of California Davis, Davis, USA.
Viveka Boddipalli, Department of Medicine, University of Wisconsin, Madison, WI, USA.
Abel Kho, Department of Medicine, Northwestern University, Chicago, USA; Chicago Health Information Technology Regional Extension Center, Chicago, USA.
Michael Lin, Department of Medicine, Rush University Medical Center, Chicago, USA.
David Meltzer, Department of Medicine, University of Chicago, Chicago, USA.
Anna Roberts, Chicago Health Information Technology Regional Extension Center, Chicago, USA.
Bill Trick, Department of Medicine, John H. Stroger Hospital of Cook County, Chicago, USA.
Surrey M. Walton, Department Pharmacy Administration (UIC), Chicago, USA
Bruce L. Lambert, Department Pharmacy Administration (UIC), Chicago, USA
References
- 1.Bourgeois FC, Olson KL, Mandl KD. Patients treated at multiple acute health care facilities: quantifying information fragmentation. Arch Intern Med 2010;170:1989–95. [DOI] [PubMed] [Google Scholar]
- 2.Elder NC, Hickner J. Missing clinical information: the system is down. JAMA 2005;293:617–9. [DOI] [PubMed] [Google Scholar]
- 3.Smith PC, Araya-Guerra R, Bublitz C, et al. Missing clinical information during primary care visits. JAMA 2005;293:565–71. [DOI] [PubMed] [Google Scholar]
- 4.Elder NC, Vonder Meulen M, Cassedy A. The identification of medical errors by family physicians during outpatient visits. Ann Fam Med 2004;2:125–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cwinn MA, Forster AJ, Cwinn AA, et al. Prevalence of information gaps for seniors transferred from nursing homes to the emergency department. CJEM 2009;11:462–71. [DOI] [PubMed] [Google Scholar]
- 6.Lambrew JM, DeFriese GH, Carey TS, et al. The effects of having a regular doctor on access in primary care. Med Care. 1996;34:138–51. [DOI] [PubMed] [Google Scholar]
- 7.Santoli JM, Rodewald LE, Maes EF, et al. Vaccines for children program, United States. Pediatrics. 1999;104:e15. [DOI] [PubMed] [Google Scholar]
- 8.Gross CP, Mead LA, Ford DE, et al. Physician, heal thyself? Regular source of care and use of preventive health services among physicians. Arch Intern Med. 2000;160:3209–14. [DOI] [PubMed] [Google Scholar]
- 9.Ettner SL. The timing of preventive services for women and children: the effect of having a usual source of care. Am J Public Health. 1996;86:1748–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim J, Chuun D, Shah A, et al. Prevalence and impact of information gaps in the emergency department. AMIA Annu Symp Proc 2008:866. [PubMed] [Google Scholar]
- 11.Stiell A, Forster AJ, Stiell IG, et al. Prevalence of information gaps in the emergency department and the effect on patient outcomes. CMAJ 2003;169:1023–8. [PMC free article] [PubMed] [Google Scholar]
- 12.http://www.surescripts.com/about-e-prescribing/progress-reports/state.aspx?state=il.Accessed 5/21/2011.
- 13.Hripcsak G, Kaushal R, Johnson KB, et al. The United Hospital Fund meeting on evaluating health information exchange. J Biomed Inform. 2007December;40(6 Suppl):S3–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kaelber DC, Bates DW. Health information exchange and patient safety J Biomed Inform. 2007December;40(6 Suppl):S40–5. [DOI] [PubMed] [Google Scholar]
- 15.Kho AN, Lemmon L, Commiskey M, et al. Use of a regional health information exchange to detect crossover of patients with MRSA between urban hospitals. J Am Med Inform Assoc 2008Mar-Apr;15(2):212–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Arrow K, Auerbach A, Bertko J, et al. Toward a 21st-Century Health Care System: Recommendations for Health Care Reform. Ann Intern Med. 2009March2. [DOI] [PubMed] [Google Scholar]
- 17.Walker J, Pan E, Johnston D, et al. The value of health care information exchange and interoperability. Health Aff (Millwood). 2005Jan-Jun; SupplWeb Exclusives:W5-10–W5-18. [DOI] [PubMed] [Google Scholar]
- 18.Tenover FC, McDonald LC . Vancomycin-resistant staphylococci and enterococci: epidemiology and control. Current Opinion in Infectious Diseases. 18(4):300–305, August 2005. [DOI] [PubMed] [Google Scholar]
- 19.Shapiro JS, Mostashari F, Hripcsak G, et al. Using health information exchange to improve public health. Am J Public Health. 2011April;101(4):616–23.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Personal experience WG.
- 21.Grannis SJ, Biondich PG, Mamlin BW, et al. How disease surveillance systems can serve as practical building blocks for a health information infrastructure: the Indiana experience. AMIA Annu Symp Proc. 2005:286–90. [PMC free article] [PubMed] [Google Scholar]
- 22.Adler-Milstein J, Bates DW, Jha AK. A survey of health information exchange organizations in the United States: implications for meaningful use. Ann Intern Med. 2011May17;154(10):666–71. [DOI] [PubMed] [Google Scholar]
- 23. http://csrc.nist.gov/publications/nistbul/b-May-2008.pdf.
- 24.United Kingdom. UK NHS. A one-way encryption function to hide person-identifiable information. 15July2002. 11 Nov 2008 <www.nibhi.org.uk>. [Google Scholar]
- 25.United States Census Bureau: Census 2000 5-Digit ZIP Code Tabulation Areas (ZCTAs) Cartographic Boundary Files. http://www.census.gov/geo/www/cob/z52000.htmlAccessed February 21, 2011. [Google Scholar]
- 26.ESRI’s ArcGIS® 10, http://www.esri.com/ [Google Scholar]
- 27.Jenks George F. 1967. “The Data Model Concept in Statistical Mapping”, International Yearbook of Cartography 7: 186–190. [Google Scholar]
- 28.http://help.arcgis.com/en/arcgisdesktop/10.0/help/index.html#//00s50000001r000000.htmAccessed May 27, 2011.
- 29.http://www.lib.uchicago.edu/e/collections/maps/chipop0010_region.htmlAccessed 1/2013.
- 30.http://factfinder.census.gov/servlet/DownloadDatasetServlet?_lang=en.Accessed 3/2011.
- 31.http://www.ihatoday.org/hospital-directory.aspx.Accessed 5/2011.
- 32.Ejlertsson G, Berg S. Continuity of care measures: An analytical and empirical comparison. Medical Care. 1984. 22(3). 231–239. [DOI] [PubMed] [Google Scholar]
- 33.Breslau N, Haug M. Service delivery structure and continuity of care: a case study of a pediatric practice in process of reorganization. J Health Soc Behav 1976;17:339. [PubMed] [Google Scholar]
- 34.Bice TE, Boxerman SB. A quantitative measure of continuity in ambulatory care. An assessment of alternative approaches. Med Care 1977;15:347. [DOI] [PubMed] [Google Scholar]
- 35.Ejlertsson G Assessment of patient/doctor continuity in primary health care. JR Coll Gen Pract 1980;7. [Google Scholar]
- 36.Schrag D, Xu F, Hanger M, et al. Fragmentation of Care for Frequently Hospitalized Urban Residents Med Care 2006;44:560–567. [DOI] [PubMed] [Google Scholar]