Abstract
Purpose
Weight bias internalization, or the process of applying negative weight-related attitudes and beliefs to oneself, is an important construct in regard to patients pursuing bariatric surgery. Weight bias internalization (or internalized weight bias) has been previously associated with depressive symptoms and binge eating among pre-surgical bariatric patients. However, a gap in the literature exists pertaining to how certain eating behaviors may mediate the relationship between weight bias internalization and binge eating. The present study assessed the role of eating behaviors (i.e., cognitive restraint, disinhibition, and hunger) as mediators between weight bias internalization and binge eating symptoms when controlling for depression.
Materials and Methods
A total of 708 adults (Mage = 42.91; White = 95.3%; women =79.4%) seeking bariatric surgery at a tertiary academic medical center in the Appalachia region of the USA were included in this retrospective study. Patients completed validated measures of weight bias internalization, eating behaviors, and depression as part of a routine, psychological evaluation in order to determine surgical clearance.
Results
Disinhibition and hunger were significant mediators in the relationship between weight bias internalization and binge eating beyond the role of depressive symptoms alone.
Conclusion
Disinhibited eating, or the tendency to experience a loss of control and eating in response to negative emotions, as well as subjective feelings of hunger are important dimensions of eating, particularly as related to weight bias internalization and binge eating. Weight bias internalization is an important factor to consider among pre-surgical bariatric patients and warrants additional treatment considerations.
Keywords: Weight bias internalization, Bingeeating, Disinhibited eating, Three-FactorEatingQuestionnaire, Bariatric surgery, Preoperative care
Introduction
Weight bias is defined as negative attitudes, beliefs, and discriminatory behaviors based on an individual’s weight [1, 2] that disproportionately affects individuals with obesity [3]. In the USA, perceived weight discrimination increased in the past decade (i.e., 1995 to 2005) by 66% [4]. In an effort to mitigate the negative impact of weight bias, the American Society for Metabolic and Bariatric Surgery (ASMBS) released a position statement emphasizing the importance of recognizing weight bias among individuals pursuing bariatric surgery [5].
Further, it has also been recognized that individuals not only endure overt acts of weight bias but also apply these negative attitudes and beliefs to themselves. The term weight bias internalization (or internalized weight bias) captures this negative self-evaluative process [6]. A systematic review found that weight bias internalization has been associated with depression, anxiety, and disordered eating among persons with excess weight and obesity [7, 8]. For bariatric surgery patients specifically, weight bias internalization has been associated with symptoms of depression [8-10] and disordered eating [11]. Thus, it is unsurprising that more research on weight bias internalization among bariatric patients is needed [5, 12]. To date, it has been documented that individuals with excess weight or obesity with high levels of internalized weight bias endorse more binge eating episodes per week [13]. For bariatric surgery patients, this is of notable concern given some research that has found that the presence of binge eating is associated with suboptimal weight loss following surgery [14].
However, it is not expected that every patient who experiences weight bias internalization engages in binge eating behaviors. Therefore, it is imperative for research to further explore what other variables may place bariatric surgery candidates who experience weight bias internalization at risk for binge eating. A previous study conducted among pre-surgical bariatric patients found that emotion dysregulation may mediate the relationship between weight bias internalization and disordered eating [15]. Cox and Brode [16] found that among pre-surgical bariatric patients, disinhibited eating (i.e., inclination toward an overconsumption of food, difficulty restraining eating impulses, and loss of control eating) explained the relationship between depressive symptoms and binge eating. However, it is unclear to what extent weight bias internalization influences binge eating by way of disordered eating above and beyond the role of depression.
The main aim of the present study was to determine if particular behavioral and cognitive aspects of eating behaviors explain the relationship between high levels of weight bias internalization and binge eating symptoms. The present study explored three dimensions of eating behaviors, measured by the Three-Factor Eating Questionnaire (TFEQ; [17]). The three dimensions of eating behaviors and cognitions included (1) cognitive restraint (the tendency to consciously restrict one’s food intake in an effort to control weight), (2) disinhibition (the tendency to overeat and/or experience a loss of control while eating related to negative emotions), and (3) hunger (the level of susceptibility to bodily signs and symptoms, as well as subjective feelings that signal one’s drive for food).
Based on previous research that has found a significant association between binge eating and disinhibition [16, 18], as well as a significant relationship between depression and binge eating [16, 19], it was hypothesized that disinhibition would mediate the relationship between weight bias internalization and binge eating when controlling for the impact of depressive symptoms (Model 1; Hypothesis 1). Given more limited theoretical justification and research to date, it was hypothesized that the eating dimensions of cognitive restraint (Model 2) and hunger (Model 3) would not mediate the relationship between weight bias internalization and binge eating when controlling for depression (Hypothesis 2).
Methods
Participants
A total of 708 adult patients presenting for bariatric surgery at an MBSAQIP-accredited tertiary academic medical center located in the Appalachia region of the USA were evaluated between June 1st, 2018 and March 31st, 2020. Patients ranged in age from 19 to 70 years old (M= 42.91; SD = 11.00) and consisted of predominantly White (95.3%), heterosexual (93.1%), cisgender (i.e., individuals whose gender identity corresponds to their sex assigned at birth) women (79.4%). Body mass index (BMI; M = 48.92; SD = 7.81) was calculated as kg/m2 and ranged from 34.70 to 85.04 kg/m2. The majority of patients reported interest in pursuing sleeve gastrectomy (71.8%), followed by Roux-en-Y gastric bypass (26.3%), and a small number reported uncertainty of what type of bariatric surgery would be pursued (1.8%). Additional characteristics of the full sample are presented in Table 1.
Table 1.
Demographic characteristics of the full sample (n = 708)
| Characteristic | Frequency (n) | Percent (%) | |
|---|---|---|---|
| Gender identity | Cisgender man | 146 | 20.6 |
| Cisgender woman | 562 | 79.4 | |
| Race/ethnicity | Asian/Pacific Islander | 1 | 0.1 |
| Black/African American | 17 | 2.4 | |
| Hispanic or Latin/o/a/x | 8 | 1.1 | |
| Native American or American Indian | 1 | 0.1 | |
| White | 675 | 95.3 | |
| Other (e.g., multi-racial) | 6 | 0.8 | |
| Sexual orientation | Bisexual | 14 | 2.0 |
| Heterosexual/straight | 659 | 93.1 | |
| Gay | 6 | 0.8 | |
| Lesbian | 11 | 1.6 | |
| Questioning | 5 | 0.7 | |
| Other (e.g., pansexual) | 4 | 0.6 | |
| Prefer not to disclose | 9 | 1.3 | |
| Highest level of education | High school not completed | 32 | 4.5 |
| High school graduate/GED | 192 | 27.1 | |
| Some college | 194 | 27.4 | |
| Associates degree | 127 | 17.9 | |
| Bachelor’s degree | 116 | 16.4 | |
| Master’s degree or higher | 47 | 6.6 | |
| Employment status | None/unemployed | 63 | 8.9 |
| Part-time (< 20 h/week) | 41 | 5.8 | |
| Full-time (> 20 h/week) | 415 | 58.6 | |
| Disabled | 92 | 13.0 | |
| Retired | 29 | 4.1 | |
| Student | 16 | 2.3 | |
| Homemaker | 52 | 7.3 | |
| Body mass index (BMI) | 35.0–39.9 kg/m2 | 61 | 8.6 |
| 40.0–49.9 kg/m2 | 443 | 62.6 | |
| 50.0–59.9 kg/m2 | 139 | 19.6 | |
| 60.0–69.9 kg/m2 | 52 | 7.3 | |
| > 70.0 kg/m2 | 13 | 1.8 |
Measures
Demographics
Patients were asked to provide demographic information consisting of age, gender identity, race/ethnicity, sexual orientation, education level, employment status, and height and weight in order to calculate BMI.
Weight Bias Internalization Scale
The Weight Bias Internalization Scale (WBIS) [6] is an 11-item measure of internalized weight stigma and one of the most commonly used measures to assess the construct. Respondents answer each item based on a 7-point scale (1 = strongly disagree, 7 = strongly agree). Scores range from 11 to 77, with higher scores indicative of greater weight bias internalization. The WBIS has demonstrated high internal consistency in its development [6] and has recently been used among samples of bariatric surgery patients [11, 15].
Binge Eating Scale
The Binge Eating Scale (BES) [20] is a 16-item measure of binge eating symptomatology. Respondents are presented with different response options ranging in severity for each item characteristic. A total score is calculated with scores ranging from 0 to 46, with higher scores indicating more binge eating symptoms. Scores are further categorized into three groups: absent/minimal binge eating (≤ 17), mild to moderate binge eating (18 to 26), and severe binge eating (≥27). The BES has been previously used among pre-surgical bariatric samples [16] and has demonstrated high internal consistency and strong factorial validity [21].
Three-Factor Eating Questionnaire
The Three-Factor Eating Questionnaire (TFEQ) [17] consists of items measuring cognitive and behavioral aspects of eating. The measure is comprised of 51 total items: 36 items prompt participants to respond to yes/no questions, 14 items are based on a 1-to-4 response scale, and one item is based on a 1-to-6 response scale from no restraint in eating to total restraint. The TFEQ assesses three dimensions of eating behavior: cognitive restraint, disinhibition, and hunger. Scores from the three subscales range from 0 to 21 (cognitive restraint; TFEQ-CR), 0–16 (disinhibition; TFEQ-D), and 0–14 (hunger; TFEQ-H). The TFEQ has demonstrated adequate internal consistency for each of the three subscales among a sample of participants with obesity [22] and pre-surgical bariatric patients [16].
Beck Depression Inventory-II
The Beck Depression Inventory-II (BDI-II) [23] consists of 21 items assessing symptoms of depression in the past 2 weeks. All items are summed in order to yield a total score and are further categorized based on level of severity: minimal (0–13), mild (14–19), moderate (20–28), and severe (29–63). The BDI-II has been administered among samples of bariatric samples and has yielded strong psychometric properties [16, 24, 25].
Procedure
The Institutional Review Board at West Virginia University approved all study procedures. Patients completed several self-report questionnaires on an electronic tablet as part of a standard, routine psychological evaluation for surgical clearance prior to bariatric surgery. The prospectively collected data were retrospectively reviewed. All data were collected and managed in a HIPAA-compliant, REDCap (Research Electronic Data Capture, Vanderbilt University, Tennessee) database. Data were subsequently downloaded from REDCap to SPSS (IBM, New York) version 25.0 for all statistical analyses.
Statistical Analysis
Descriptive statistics and correlations were calculated for all study variables (n = 708). The effect of demographic variables, such as age, BMI, and gender, was assessed on all study variables via Pearson correlations or t-tests. For the present study, the sample size was considered to be sufficient to achieve 0.80 power to detect a medium effect size from mediation analyses [26], Based on a bootstrapping approach of n = 5000, Hayes’ [27] PROCESS command was used for the three mediation analyses. Significant mediation was determined based on whether zero was contained within the lower and upper confidence interval (CI) limits for the indirect effect. For each model, WBIS and BES were the predictor and outcome variables, respectively. The three subscales of the TFEQ were entered separately into each model in order to assess whether TFEQ-CR, TFEQ-D, and TFEQ-H mediated the relationship between WBIS and BES.
Results
Descriptive statistics, including means and standard deviations, and Pearson correlations for all study variables, including age and BMI, are presented in Table 2. Age was significantly correlated with each study variable (ps < 0.05) except for the WBIS and BDI-II. BMI was only significantly correlated with the TFEQ-CR and BDI-II (ps < 0.05). Significant correlations with age were between a small-to-moderate strength, whereas significant correlations with BMI were small [28]. The WBIS was significantly correlated with the BES and all subscales of the TFEQ, with the strengths of the correlations ranging from small to large. The only difference in gender was found for the TFEQ-CR, t(706) = 12.30, p < 0.001, with women (M = 13.75, SD = 3.84) endorsing higher levels of restraint compared to men (M = 11.60, SD = 4.62). No statistically significant differences in gender were found (ps > 0.05) for the WBIS (women: M = 42.90, SD = 12.35; men: M = 41.13, SD = 13.54), TFEQ-D, (women: M = 5.93, SD = 3.11; men: M = 6.24, SD = 3.38), TFEQ-H (women: M = 3.76, SD = 3.03; men: M = 4.23, SD = 3.25), BES (women: M= 12.34, SD = 6.94; men: M = 12.63, SD = 7.68), or BDI-II (women: M = 8.36, SD = 8.13; men: M = 8.98, SD = 9.62). As expected, the BDI-II was significantly correlated with all study variables (ps < 0.01). Thus, the BDI-II and age were included as covariates in all study analyses.
Table 2.
Descriptive statistics, reliability, and correlations for age, BMI, and study variables (n = 708)
| Variables | M (SD) | α | Pearson correlation coefficients | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | |||
| 1. Age | 42.91 (11.00) | -- | |||||||
| 2. BMI | 48.92 (7.81) | -- | − 0.19*** | ||||||
| 3. BDI-II | 8.48 (8.46) | 0.92 | − 0.02 | 0.08* | |||||
| 4. WBIS | 42.54 (12.62) | 0.87 | < 0.01 | 0.05 | 0.64*** | ||||
| 5. BES | 12.40 (7.09) | 0.87 | 0.10** | − 0.01 | 0.44*** | 0.53*** | |||
| 6. TFEQ-D | 5.99(3.17) | 0.76 | 0.13** | – 0.02 | 0.37*** | 0.42*** | 0.74*** | ||
| 7. TFEQ-CR | 13.31 (4.11) | 0.80 | − 0.13** | 0.08* | − 0.11** | − 0.08* | − 0.34*** | − 0.36*** | |
| 8. TFEQ-H | 3.86 (3.08) | 0.80 | 0.08* | − 0.04 | 0.29*** | 0.35*** | 0.66*** | 0.63*** | − 0.32*** |
Note. M mean, SD standard deviation, μ Cronbach’s alpha, BMI body mass index, BDI-II Beck Depression Inventory-II, WBIS Weight Bias Internalization Scale, BES Binge Eating Scale, TFEQ Three-Factor Eating Questionnaire, D disinhibition subscale, CR cognitive restraint subscale, H hunger subscale
p < 0.05
p < 0.01
p < 0.001
Model 1: Disinhibition as a Mediator Between Weight Bias Internalization and Binge Eating
Results of the indirect effect of WBIS on BES through TFEQ-D revealed that zero was not contained within the CIs (b = 0.11, CI [0.08, 0.14]). Therefore, results indicate that TFEQ-D significantly mediated the relationship between WBIS and BES (see Fig. 1 for the unstandardized coefficients, standard errors (SEs), and p values of the mediation model).
Fig. 1.
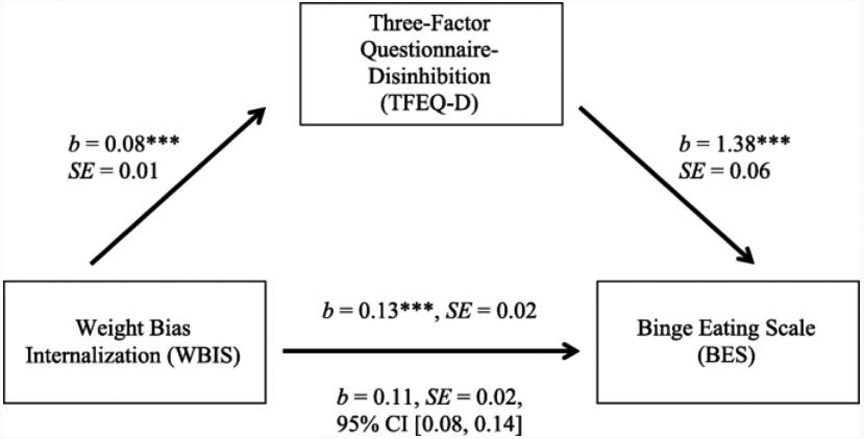
Significant indirect effect of WBIS on BES as mediated by TFEQ-D, controlling for age and BDI-II. For the lower path, values above the arrow refer to unmediated pathway (direct effect), and values below the arrow refer to the mediated pathway (indirect effect). Asterisks indicate significant unstandardized coefficients (n = 708; ***p < 0.001)
Model 2: Cognitive Restraint as a Mediator Between Weight Bias Internalization and Binge Eating
Results of the indirect effect of WBIS on BES through TFEQ-CR revealed that zero was contained within the CIs (b = 0.004, CI [− 0.01, 0.02]), thus indicating that TFEQ-CR did not significantly mediate the relationship between WBIS and BES (see Fig. 2 for the unstandardized coefficients, standard errors (SEs), and p values of the mediation model).
Fig. 2.
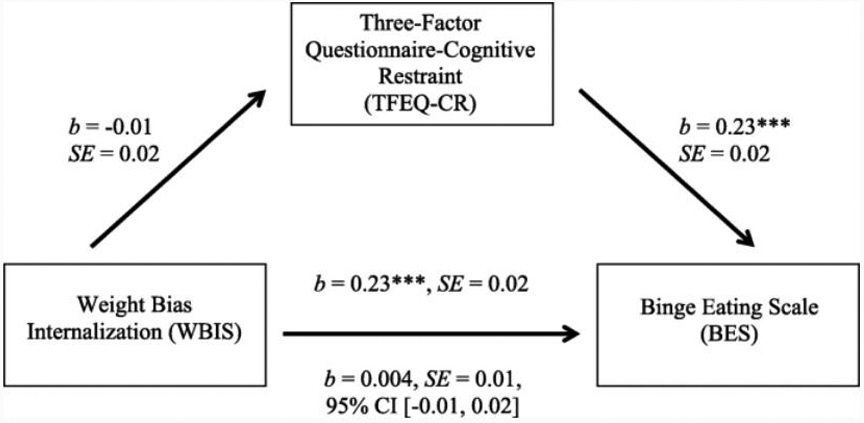
Non-significant indirect effect of WBIS on BES as mediated by TFEQ-CR, controlling for age and BDI-II. For the lower path, values above the arrow refer to unmediated pathway (direct effect), and values below the arrow refer to the mediated pathway (indirect effect). Asterisks indicate significant unstandardized coefficients (n = 708;***p < 0.001)
Model 3: Hunger as a Mediator Between Weight Bias Internalization and Binge Eating
Results of the indirect effect of WBIS on BES through TFEQ-H revealed that zero was not contained within the CIs (b = 0.08, CI [0.05, 0.11]). Therefore, results indicate that TFEQ-H significantly mediated the relationship between WBIS and BES (see Fig. 3 for the unstandardized coefficients, standard errors (SEs), and p values of the mediation model).
Fig. 3.
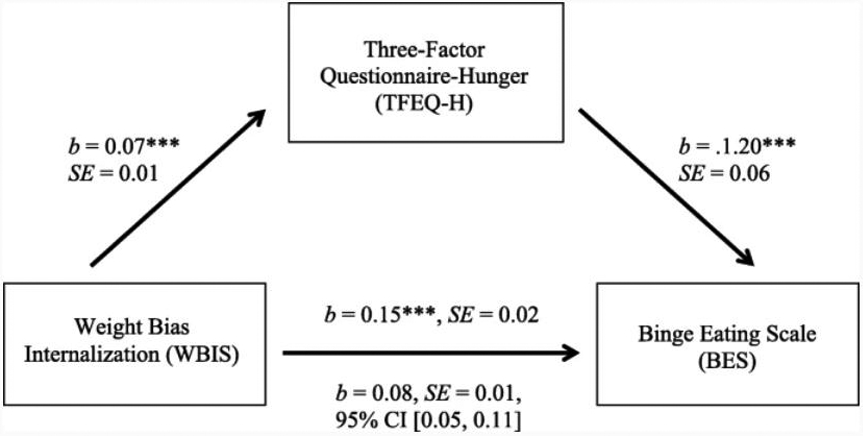
Significant indirect effect of WBIS on BES as mediated by TFEQ-H, controlling for age and BDI-II. For the lower path, values above the arrow refer to unmediated pathway (direct effect), and values below the arrow refer to the mediated pathway (indirect effect). Asterisks indicate significant unstandardized coefficients (n = 708; ***p < 0.001)
Discussion
The purpose of the present study was to assess the relationship between weight bias internalization and binge eating as influenced by different dimensions of eating behaviors. Results support the hypothesis that disinhibition mediates the relationship between weight bias internalization and binge eating among pre-surgical bariatric patients. It is notable that even when controlling for depression, higher levels of weight bias internalization predicted greater binge eating symptoms as influenced by greater levels of disinhibition. In other words, the act of shaming oneself based on weight may influence one’s difficulty in regulating impulses to eat and/or use food as a method of coping. Furthermore, such disinhibited eating may give way for patients to eat an uncomfortably large amount of food that is indicative of a binge episode. Future research may consider exploring more complex associations between disinhibited eating, binge eating, and other variables not examined in the present study, such as exposure to adverse life events or emotion dysregulation which could serve as factors that further explain disordered eating among pre-surgical bariatric patients.
Results from the present study supported the hypothesis that cognitive restraint would not mediate the relationship between weight bias internalization and binge eating. Hunger, however, was found to be a significant mediator, even when controlling for depression. One explanation for this finding could be that pre-surgical bariatric patients with high levels of internalized weight bias may be more susceptible to misattributing hunger cues and differentiating between their bodily cues of hunger versus emotionally driven feelings for hunger. Alternatively, patients with strong, negative attitudes toward themselves because of their weight may place excessive focus on these internalized attitudes, thus making it challenging to recognize genuine bodily cues that signal hunger. This relationship between internalized weight bias and subjective feelings of hunger may present as problematic eating behaviors, such as grazing/picking and nibbling, mindless eating, and emotional eating which are commonly found among bariatric patients [29].
Thus, the current study has important clinical implications. Findings highlight the importance of assessing the extent to which patients apply societally-driven and stigmatizing attitudes and beliefs about their weight to themselves (i.e., patients’ level of internalized weight bias). These results emphasize the importance of assessing for internalized weight bias among pre-surgical bariatric patients—regardless of whether symptoms of depression are present or not—given its influence on binge eating in the presence of high levels of disinhibition. By including aspects of internalized weight bias in a patient’s case conceptualization, providers may gain further insight into how these internalized, weight-related attitudes may be associated with one’s eating behaviors. Increased vigilance in diagnosing internalized weight bias may yield greater opportunities for pre-surgical therapeutic intervention and concerted post-surgical surveillance of behaviors known to lessen health improvement after bariatric surgery.
Findings from this study also support the need for future clinical research focused on creating or adapting interventions to address internalized weight bias, as well as disinhibited eating and subjective feelings of hunger among patients pursuing bariatric surgery. Cognitive-behavioral interventions in previous studies focused on internalized weight bias and disinhibited eating have shown to reduce symptoms of disordered eating among adults pursuing bariatric surgery [30]. Such interventions could not only reduce the frequency of binge eating symptoms but also increase the chances of greater weight loss outcomes [31, 32] yielding greater improvement in health. With further understanding of weight bias internalization, better therapeutic interventions may be developed, which may alter preoperative and postoperative patient care. Prior research has shown that multidisciplinary care with preoperative preparation and close continued follow-up postoperative care improves effectiveness of bariatric surgery [33]. Gaining a greater understanding of weight bias internalization could further help to mitigate the adverse effects on surgical outcomes.
Limitations of the present study should be noted. First, the study sample consisted of mostly White, heterosexual women. Therefore, the results cannot be generalized to people of color or sexual minority patients pursuing bariatric surgery. Second, the cross-sectional design of the study led to the utilization of atemporal mediation analyses, thus limiting the implications that can be made due to the analyses not providing evidence for causality [34]. Future research should utilize methodology that enables temporal design-based mediation, such as assessing the same patients pre- and post-surgery. Relatedly, the present study utilized self-report questionnaires that ultimately only measured current as opposed to lifetime eating pathology. Based on previous research, future studies may benefit from considering the use of semi-structured interviews when specifically assessing binge eating behaviors [35]. The current study’s sample only consisted of pre-surgical bariatric patients; therefore, it is unclear if similar findings apply to patients in postoperative phases of care. Similarly, the present study did not utilize a control group. Future research should assess whether the present study’s findings are found among people with obesity who are not pursuing bariatric surgery. Such research could determine to what extent results in the present study are unique to patients pursuing bariatric surgery. Lastly, a purpose of the routine evaluation was to determine psychological clearance; therefore, it is possible that demand characteristics (e.g., presenting in an overly favorable way) may have impacted the patients’ responses [36].
In summary, the current study recognizes the importance of assessing weight bias internalization among pre-surgical bariatric patients given its relationships to eating behaviors, including binge eating. Furthermore, the present study highlights the influence of disinhibition and subjective feelings of hunger on the relationship between weight bias internalization and binge eating. Findings suggest clinical implications in both the assessment of pre-surgical bariatric patients, as well potential interventions to address internalized weight bias, disinhibition, and subjective hunger in hopes of reducing symptoms of binge eating and increasing providers’ sensitivity to patients’ needs. Future research based on longitudinal designs and with control groups should be conducted to clarify the directional relationship among these variables, such as between pre- and post-surgery bariatric patients.
Footnotes
Conflict of Interest Dr. Cassie Brode was supported by the National Institute of General Medical Sciences, 5U54GM104942-03. Dr. Nova Szoka reports serving as a consultant for Johnson & Johnson and CMR Surgical. No other disclosures among the authors exist.
Ethical Statement All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent Statement Informed consent does not apply.
Disclaimer The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
References
- 1.Puhl RM, Brownell KD. Bias, discrimination, and obesity. Obes Res. 2001;9:788–805. 10.1038/oby.2001.108. [DOI] [PubMed] [Google Scholar]
- 2.Puhl RM, Brownell KD. Psychosocial origins of obesity stigma: toward changing a powerful and pervasive bias. Obes Rev. 2003;4:213–27. 10.1046/j.1467-789X.2003.00122.x. [DOI] [PubMed] [Google Scholar]
- 3.Lee M, Ata RN, Brannick MT. Malleability of weight-biased attitudes and beliefs: a meta-analysis of weight bias reduction interventions. Body Image. 2014;11:251–9. 10.1016/j.bodyim.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Andreyeva T, Puhl RM, Brownell KD. Changes in perceived weight discrimination among Americans, 1995-1996 through 2004-2006. Obesity. 2008;16:1129–34. 10.1038/oby.2008.35. [DOI] [PubMed] [Google Scholar]
- 5.Eisenberg D, Noria S, Grover B, et al. American Society for Metabolic and Bariatric Surgery Clinical Issues Committee. ASMBS position statement on weight bias and stigma. Surg Obes Relat Dis. 2019;15:814–21. 10.1016/j.soard.2019.04.031. [DOI] [PubMed] [Google Scholar]
- 6.Durso LE, Latner JD. Understanding self-directed stigma: development of the weight bias internalization scale. Obesity. 2008;16:S80–6. 10.1038/oby.2008.448. [DOI] [PubMed] [Google Scholar]
- 7.Papadopoulos S, Brennan L. Correlates of weight stigma in adults with overweight and obesity: a systematic literature review. Obesity. 2015;23:1743–60. 10.1002/oby.21187. [DOI] [PubMed] [Google Scholar]
- 8.Puhl RM, Himmelstein MS, Pearl RL. Weight stigma as a psychosocial contributor to obesity. Am Psychol. 2020;75:274–89. 10.1037/amp0000538. [DOI] [PubMed] [Google Scholar]
- 9.Lent MR, Napolitano MA, Wood GC, et al. Internalized weight bias in weight-loss surgery patients: psychosocial correlates and weight loss outcomes. Obes Surg. 2014;24:2195–9. 10.1007/s11695-014-1455-z. [DOI] [PubMed] [Google Scholar]
- 10.Roberto CA, Sysko R, Bush J, et al. Clinical correlates of the weight bias internalization scale in a sample of obese adolescents seeking bariatric surgery. Obesity. 2012;20:533–9. 10.1038/oby.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lawson JL, LeCates A, Ivezaj V, et al. Internalized weight bias and loss-of-control eating following bariatric surgery. Eat Disord J Treat Prev. 2020:1–14. 10.1080/10640266.2020.1731920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kahan S, Puhl RM. The damaging effects of weight bias internalization. Obesity. 2017;25:280–1. 10.1002/oby.21772. [DOI] [PubMed] [Google Scholar]
- 13.Puhl RM, Moss-Racusin CA, Schwartz MB. Internalization of weight bias: implications for binge eating and emotional well-being. Obesity. 2007;15:19–23. 10.1038/oby.2007.521 [DOI] [PubMed] [Google Scholar]
- 14.Meany G, Conceição E, Mitchell JE. Binge eating, binge eating disorder and loss of control eating: effects on weight outcomes after bariatric surgery. Eur Eat Disord Rev. 2014;22:87–91. 10.1002/erv.2273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baldofski S, Rudolph A, Tigges W, et al. Weight bias internalization, emotion dysregulation, and non-normative eating behaviors in prebariatric patients. Int J Eat Disord. 2016;49:180–5. 10.1002/eat.22484. [DOI] [PubMed] [Google Scholar]
- 16.Cox S, Brode C. Predictors of binge eating among bariatric surgery candidates: disinhibition as a mediator of the relationship between depressive symptoms and binge eating. Obes Surg. 2018;28:1990–6. 10.1007/s11695-018-3129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stunkard AJ, Messick S. The three-factor eating questionnaire to measure dietary restraint, disinhibition and hunger. J Psychosom Res 1985;29:71–83. 10.1016/0022-3999(85)90010– 8. [DOI] [PubMed] [Google Scholar]
- 18.Kalarchian MA, Marcus MD, Wilson GT, et al. Binge eating among gastric bypass patients at long-term follow-up. Obes Surg. 2002;12:270–5. 10.1381/096089202762552494. [DOI] [PubMed] [Google Scholar]
- 19.Linde JA, Jeffery RW, Levy RL, et al. Binge eating disorder, weight control self-efficacy, and depression in overweight men and women. Int J Obes. 2004;28:418–25. 10.1038/sj.ijo.0802570. [DOI] [PubMed] [Google Scholar]
- 20.Gormally J, Black S, Daston S, et al. The assessment of binge eating severity among obese persons. Addict Behav. 1982;7:47–55. 10.1016/0306-4603(82)90024-7. [DOI] [PubMed] [Google Scholar]
- 21.Grupski AE, Hood MM, Hall BJ, et al. Examining the binge eating scale in screening for binge eating disorder in bariatric surgery candidates. Obes Surg. 2013;23:1–6. 10.1007/s11695-011-0537-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Allison DB, Kalinsky LB, Gorman BS. A comparison of the psychometric properties of three measures of dietary restraint. Psychol Assess. 1992;4:391–8. 10.1037/1040-3590.4.3.391. [DOI] [Google Scholar]
- 23.Beck AT, Steer RA, Brown GK. Beck Depression Inventory-II 1996. 10.1037/t00742-000. [DOI] [Google Scholar]
- 24.Hood MM, Grupski AE, Hall BJ, et al. Factor structure and predictive utility of the binge eating scale in bariatric surgery candidates. Surg Obes Relat Dis. 2013;9:942–8. 10.1016/j.soard.2012.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Marek RJ, Heinberg LJ, Lavery M, et al. A review of psychological assessment instruments for use in bariatric surgery evaluations. Psychol Assess. 2016;28:1142–57. 10.1037/pas0000286. [DOI] [PubMed] [Google Scholar]
- 26.Pan H, Liu S, Miao D, et al. Sample size determination for mediation analysis of longitudinal data. BMC Med Res Methodol. 2018;18(1):32. 10.1186/s12874-018-0473-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. 2nd ed New York: The Guilford Press; 2018. [Google Scholar]
- 28.Cohen J. A power primer. Psychol Bull. 1992;112:155–9. 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 29.Adler S, Fowler N, Robinson AH, et al. Correlates of dietary adherence and maladaptive eating patterns following roux-en-y bariatric surgery. Obes Surg. 2018;28:1130–5. 10.1007/s11695-017-2987-9. [DOI] [PubMed] [Google Scholar]
- 30.Mensinger JL, Calogero RM, Tylka TL. Internalized weight stigma moderates eating behavior outcomes in women with high BMI participating in a healthy living program. Appetite. 2016;102:32–43. 10.1016/j.appet.2016.01.033. [DOI] [PubMed] [Google Scholar]
- 31.Sienko RM, Saules KK, Carr MM. Internalized weight bias mediates the relationship between depressive symptoms and disordered eating behavior among women who think they are overweight. Eat Behav. 2016;22:141–4. 10.1016/j.eatbeh.2016.06.002. [DOI] [PubMed] [Google Scholar]
- 32.Matthew B, Flesher M, Sampath S, et al. The effect of intensive preconditioning and close follow-up on bariatric surgery outcomes: does multidisciplinary care contribute to positive results whether a gastric bypass or sleeve gastrectomy is performed? B C Med J. 2015;57(6):238–43. [Google Scholar]
- 33.McVay MA, Friedman KE. The benefits of cognitive behavioral groups for bariatric surgery patients. Bariatr Times. 2012;9:22–8. [Google Scholar]
- 34.Winer ES, Cervone D, Bryant J, et al. Distinguishing mediational models and analyses in clinical psychology: atemporal associations do not imply causation. J Clin Psychol. 2016;72:947–55. 10.1002/jclp.22298. [DOI] [PubMed] [Google Scholar]
- 35.Quilliot D, Brunaud L, Mathieu J, et al. Links between traumatic experiences in childhood or early adulthood and lifetime binge eating disorder. Psychiatry Res. 2019;276:134–41. 10.1016/j.psychres.2019.05.008. [DOI] [PubMed] [Google Scholar]
- 36.Ambwani S, Boeka AG, Brown JD, et al. Socially desirable responding by bariatric surgery candidates during psychological assessment. Surg Obes Relat Dis. 2013;9:300–5. 10.1016/j.soard.2011.06.019. [DOI] [PubMed] [Google Scholar]


