Abstract
Objective:
Ethiopia is planning to vaccinate 20% of its population against the coronavirus disease 2019 pandemic by the end of 2021—however, there is no single piece of evidence regarding pregnant women’s intention to be vaccinated against coronavirus disease 2019; hence, the objective of this study was to investigate predicting factors of intention to be vaccinated against coronavirus disease 2019 among pregnant women in Bench-Sheko Zone, southwest Ethiopia.
Methods:
Facility-based cross-sectional study was undertaken from 1 February to 1 March 2021 in southwest Ethiopia. The study was carried out among pregnant women who came for antenatal care service in the selected public health facilities. Interviewer-administered structured tool was used to collect the data. Data were entered into EpiData (version 3.1) and then analyzed using SPSS (version 20).
Results:
The study revealed that only 31.3% (95% confidence interval: 26.7–35.2) of the participants had an intention to be vaccinated against coronavirus disease 2019 when the vaccine will be made available in Ethiopia. Participants’ intention to be vaccinated against coronavirus disease 2019 was significantly associated with attaining secondary school and above (adjusted odds ratio = 4.24, 95% confidence interval: 2.23–9.32), residing in urban areas (adjusted odds ratio = 2.57, 95% confidence interval: 1.22–5.40), being compliant with coronavirus disease 2019 guidelines (adjusted odds ratio = 5.86, 95% confidence interval: 3.40–10.09), and having good perception toward coronavirus disease 2019 vaccine (adjusted odds ratio = 3.04, 95% confidence interval: 1.64–5.62).
Conclusion:
Above all, in this study, pregnant women’s intention to vaccinate against coronavirus disease 2019 was very low when compared with previous studies. Hence, before commencing the coronavirus disease 2019 vaccination program in Ethiopia, it is essential to launch a widespread public health education campaign that could improve people’s perception of the vaccine. Besides, the upcoming public health intervention programs better put special emphasis on community members with lower educational attainment backgrounds and rural residents.
Keywords: Intention to vaccinate, vaccine acceptance, coronavirus disease 2019, vaccine, Ethiopia
Introduction
The coronavirus disease 2019 (COVID-19) is spread rapidly and reached about 221 countries in the world.1,2 Globally, 123,942,893 people were infected by the virus, and 2,729,111 were died as of 22 March 2021.3 In Ethiopia, the first COVID-19 case was reported by the Ministry of Health on 20 March 2020. In 2020, Ethiopia was affected by the devastating effects of the COVID-19 pandemic, with 187,365 cases and 2659 deaths as of 22 March 2021, and the overtiredness of health care systems, as well as its adverse socioeconomic and psychological impacts.4,5
Preventive actions such as tiring a facial mask, removing crowded areas, reducing direct contact, and keeping a safe distance demonstrated to be effective in limiting the spread of the disease.6 However, they do not serve as a sustainable remedy of the COVID-19 pandemic, and the development and applying an active vaccine will be indispensable for monitoring the COVID-19 pandemic.7 Worldwide, more than 35 biotech and pharmaceutical businesses were competing to find a safe COVID-19 vaccine; to date, three vaccines were approved worldwide: AstraZeneca, Pfizer-Biotech, and Moderna.8
Governments must be prepared to safeguard large-scale, unbiased access and supply of a COVID-19. This will necessitate adequate health system ability, as well as strategies to develop confidence in and acceptance of the vaccine and those who deliver it.9 In Ethiopia, the government has planned a vaccination program to reach herd immunity against the disease for those people who are more vulnerable to the pandemic than the general population. However, the program is not implemented yet due to the low accessibility of the vaccine. Surprisingly, the vaccination program’s attainment will fully depend on the public attitude toward the vaccine.10
Vaccine acceptance is reported as one of the major challenges to global health by World Health Organization (WHO). Mass vaccination has been highly successful in inducing herd immunity for many diseases, protecting those that are unable to build up immunity, such as people with immune deficiencies or whose immune systems are being suppressed for medical reasons.7 Vaccine acceptance affects not only the individual who refuses to take the vaccine but the whole communities. There are some beliefs and barriers concerning vaccination among the entire population. Vaccine coverage and its acceptance differ regarding behavior of the people, socioeconomic factors, and many more.11
In addition, some key factors such as the severity of the disease, former vaccination history, lack of trust in health care facilities, way of administration of vaccine, income and academic status of the individuals, recommendations from physician, and cost of vaccine also determine the acceptance of vaccines.9,12,13
Even though the overall chance of severe illness is low, expectant women are at higher risk for severe illness from COVID-19 when compared to nonpregnant women. Moreover, pregnant women who are infected by COVID-19 might be at a greater risk of adverse pregnancy outcomes such as low birth weight and preterm birth compared with pregnant women free of COVID-19.14 Investigating factors that hinder pregnant women’s intention to vaccinate against COVID-19 is another important battle against the pandemic. As per the reviewed literature, there are few studies conducted regarding pregnant women’s hesitancy toward COVID-19 vaccination.10,13,14 However, there is no single piece of evidence about determinants of COVID-19 vaccine uptake intention among pregnant women in Africa. Hence, the objective of this study was to investigate predicting factors of intention to be vaccinated against COVID-19 among pregnant women in Bench-Sheko Zone, southwest Ethiopia.
Methods
Study area and design
A facility-based cross-sectional study was conducted in Bench-Sheko Zone, southwest Ethiopia, from 1 February to 1 March 2021. The zone is found 561 km from Addis Ababa, which is the capital city of Ethiopia. The population of the zone is expected to be 829,493; of them, 418,213 are females. Bench-Sheko zone has a city administration (Mizan-Teferi), six woredas (districts), and 246 kebeles (smallest administrative units) (229 rural and 17 urban). Regarding facilities available in the zone, there are 26 health centers, 182 health posts, and 1 hospital.15
Source and study population
All pregnant women attending ANC (antenatal care) service found in Bench-Sheko zone were the source population, and systematically selected pregnant women utilizing ANC service from 1 February to 1 March 2021 were the study population.
Sample size and sampling technique
When calculating the sample size, the proportion of pregnant women who would have the intention to vaccinate against COVID-19 was assumed to be 50%, as there is no study conducted in a similar setting in Ethiopia. Based on the above assumption, the actual sample size for this study was calculated by employing single population proportion formula with a marginal error of 5% and 95% CL. Finally, 10% nonresponse rate was considered, and the sample size became 423.
During study participant selection, first, a list of all public health facilities in Bench-Sheko zone providing antenatal and delivery care service was obtained from zonal health office; then six health centers were included by employing a simple random sampling technique and one hospital, Mizan-Tepi University Teaching Hospital, was also selected as it is the only teaching hospital with the larger catchment area. Depending on the average number of ANC followers in the most recent quarterly report of each public health institutions, the calculated sample size was proportionally allocated to each of the selected public health institution. Finally, the study participants were recruited by employing a systematic random sampling technique.
Data collection tool and procedure
Interviewer-administered structured tool was used to collect the data. The tool was adopted from similar studies16–18 done outside of Ethiopia; however, few modifications were made to contextual it into the local situation. The tool has six sections: the first section was about sociodemographic characteristics of the study participants, the second section was about clinical and reproductive characteristics of the participants, the third one was about participants’ knowledge of the COVID-19 vaccine, the fourth one was about participants’ perception toward COVID-19 vaccine, the fifth one was about participants’ compliance with COVID-19 guidelines, and the last section inquires women’s intention to vaccinate against COVID-19. Ten data collectors (BSc in nursing) and three supervisors (MPH degree holders) who had experience in survey data collection techniques were hired to handle the data collection process. Before actual data collection began, 3 days of training on the purpose of the study and the overall data collection procedure were provided for the data collectors and supervisors as well. During data collection, the data were checked for completeness and consistency of information (the questionnaire is provided as Supplemental Material).
Measures
Knowledge of the COVID-19 vaccine was measured by five items, and it was analyzed as a binary variable. Participants who had correctly answered three and more questions were designated as having “Good knowledge,” otherwise “Poor knowledge.” The items were as follows: “have you heard vaccine for COVID-19?” “The vaccine doesn’t interfere with the pregnancy,” “the vaccine can decrease the risk of COVID-19 transmission,” “the vaccine can severely affect my health condition,” and “the vaccine can cure already affected people.”
Perception toward COVID-19 vaccine was measured by four items, and the responses were rated on a 6-point scale from 1 = “strongly agree” to 6 = “strongly disagree.” The items were as follows: “I have a mistrust of vaccine benefits,” “I worry about unforeseen future effects,” “I have a concern that it may cause infertility,” and “I prefer natural immunity.”16 It was dichotomized into “Negative perception” and “Positive perception” based on the threshold which was calculated using the demarcation threshold formula: {(Total highest score – Total lowest score)/2} + Total lowest score.17 The Cronbach’s alpha of perception items was 0.87.
The response to the question on compliance with government COVID-19 guidelines was on a scale from 1 = “none at all” to 7 = “very much so.” This was analyzed as a binary variable reflecting higher (6–7) and lower (1–5) compliance.18
Intention to vaccinate against COVID-19 when available was measured based on one item (“How likely do you think you are to get a COVID-19 vaccine when one is available?”). Response options ranged from 1 = “very unlikely” to 6 = “very likely.” It was dichotomized into “Intended to vaccinate” (if greater than or equal to mean score) and “Unwilling to vaccinate” (if less than mean score).18
Inclusion and exclusion criteria
Pregnant women within the age group >18 and residing for more than 6 months in the area were included in this study, whereas pregnant women who were unable to respond due to illness or other physical impairment were excluded from the study.
Data processing and analysis
The collected data were checked for completeness, edited, cleaned, coded, and entered into EpiData (version 3.1). The analysis was carried out by using SPSS (version 20). Descriptive statistics, proportions, frequencies, and mean were calculated, and the finding of the analysis was presented in text, tables, and graphs. Binary logistic regression was carried out to identify the association of different explanatory variables with the dependent variable (likelihood of having the intention to vaccinate against COVID-19). Independent variables with a p value of <0.25 on the binary logistic regression analysis were taken as a candidate for the final multivariate logistic regression analysis. Finally, multivariate logistic regression analysis was fitted to identify factors having statistically significant associations with pregnant women’s intention to vaccinate against COVID-19.
Data quality assurance
The questionnaire that was prepared in English was translated into Amharic, and then back translated into English to ensure its consistency. A pretest was conducted on 5% of the actual sample size in Debrework Health Center that was not included in the study. Three days of training on the purpose of the study and data collection procedure were given for both data collectors and supervisors. Supervision was made on daily basis and checking on 10% of the collected data. Finally, error reports were checked after entry to EpiData using each case code.
Ethical consideration
Ethical clearance was obtained from College of Medicine and Health Science, Mizan-Tepi University. In addition, a letter of permission was granted from the zonal health office administration. Upon clarifying the aim of the study, written consent was secured from each of the study participants. Anonymity and confidentiality of the data were kept throughout the study by having only the essential information without using the name of the study participants.
Results
Sociodemographic characteristics
A total of 412 pregnant women attending ANC were included in the survey with a 97.4% response rate. The mean (standard deviation (SD)) age of the participants was 30.6 ± 5.9; 262 (61.2%) and 161 (39.1%) of the participants were rural residents and protestants in religion, respectively. One-third (130; 31.6%) of the participants were housewives, and above half (225; 54.6%) of the participants had >2500 Ethiopian Birr income (Table 1).
Table 1.
Sociodemographic characteristics of women attending ANC in Bench-Sheko public health facilities, southwest Ethiopia, 2021 (N = 412).
| Variables | Category | n (%) |
|---|---|---|
| Age | 18–24 | 55 (13.3) |
| 25–34 | 276 (76.0) | |
| ⩾35 | 81 (19.7) | |
| Residence | Urban | 252 (61.2) |
| Rural | 160 (38.8) | |
| Religion | Protestant | 161 (39.1) |
| Orthodox | 134 (32.5) | |
| Muslim | 117 (28.4) | |
| Ethnicity | Bench | 155 (37.6) |
| Amhara | 85 (20.6) | |
| Kaffa | 78 (18.9) | |
| Oromo | 52 (12.6) | |
| Others | 42 (10.2) | |
| Marital status | Single | 113 (27.4) |
| Married | 255 (61.9) | |
| Widowed | 22 (5.3) | |
| Divorced | 22 (5.3) | |
| Education level | Uneducated | 88 (21.4) |
| Primary | 165 (40.0) | |
| Secondary and above | 159 (38.6) | |
| Occupation | Unemployed | 65 (15.8) |
| Housewife | 130 (31.6) | |
| Merchant | 88 (21.4) | |
| Government employee | 63 (15.3) | |
| Private business | 66 (16.0) | |
| Average monthly income | ⩽2500 ETB | 187 (45.4) |
| ⩾2500 ETB | 225 (54.6) |
ANC: antenatal care; ETB: Ethiopian Birr.
Reproductive and clinical characteristics
Nearly half (198; 48.1%) of the women were in 12- to 24-week gestational age, and only 65 (15.8%) were diagnosed for COVID-19. Regarding pregnant women’s compliance with COVID-19 guidelines, about one-third (118; 28.6%) of the participants had made compliance with COVID-19 guidelines. Majority (301; 73.1%) believe that pregnancy is risk for COVID-19 (Table 2).
Table 2.
Reproductive and COVID-19-related clinical characteristics of women attending ANC in Bench-Sheko public health facilities, southwest Ethiopia, 2021 (N = 412).
| Variables | Category | Frequency (n) | % |
|---|---|---|---|
| Gestational age | ⩽12 weeks | 88 | 21.4 |
| 12–24 weeks | 198 | 48.1 | |
| ⩾24 weeks | 126 | 30.6 | |
| Chronic disease | Yes | 52 | 12.6 |
| No | 360 | 87.4 | |
| Children | Yes | 163 | 39.6 |
| No | 249 | 60.4 | |
| Compliance with COVID-19 guidelines | Yes | 118 | 28.6 |
| No | 294 | 71.4 | |
| Risk for COVID-19 | Yes | 301 | 73.1 |
| No | 111 | 26.9 | |
| Diagnosed for COVID-19 | Yes | 65 | 15.8 |
| No | 347 | 84.2 | |
| Care for COVID-19 patient | Yes | 113 | 27.4 |
| No | 299 | 72.6 |
COVID-19: coronavirus disease 2019; ANC: antenatal care.
Knowledge of COVID-19 vaccine
This study assessed the knowledge status of the women about the COVID-19 vaccine. The majority (361; 87.6%) of the participants heard about the COVID-19 vaccine. More than half (224; 54.4%) of the participants mentioned that the vaccine does not interfere with pregnancy, 180 (43.7%) claimed that the vaccine can decrease the risk of COVID-19 transmission, and 131 (31.8%) reported that the vaccine could severely affect their health condition. Overall, 140 (34%) of the participants had good knowledge about the COVID-19 vaccine. (Table 3).
Table 3.
Assessments of knowledge about COVID-19 vaccine among women attending ANC at public health facilities of Bench-Sheko zone, southwest Ethiopia, 2021 (N = 412).
| Variables | Category | Frequency (n) | % |
|---|---|---|---|
| Have you heard about COVID-19 vaccine? | Yes | 361 | 87.6 |
| No | 22 | 5.3 | |
| I don’t know | 29 | 7.0 | |
| The vaccine does not interfere with pregnancy | Yes | 224 | 54.4 |
| No | 105 | 25.5 | |
| I don’t know | 83 | 20.1 | |
| The vaccine can decrease the risk of COVID-19 transmission | Yes | 180 | 43.7 |
| No | 145 | 35.2 | |
| I don’t know | 87 | 21.1 | |
| The vaccine can severely affect my health condition | Yes | 160 | 39.8 |
| No | 164 | 39.4 | |
| I don’t know | 88 | 21.4 | |
| The vaccine can cure already infected people | Yes | 131 | 31.8 |
| No | 161 | 39.1 | |
| I don’t know | 120 | 29.1 |
COVID-19: coronavirus disease 2019; ANC: antenatal care.
Perception toward COVID-19 vaccine
Regarding pregnant women’s perception toward COVID-19 vaccine, about half (211; 51.2%) of the participants prefer for natural immunity rather than COVID-19 vaccine, and more than half (229; 55.6%) of the participants had a mistrust of vaccine benefit. Overall, 217 (52.6%) of the participants had a positive perception to the COVID-19 vaccine (Figure 1).
Figure 1.
Women’s perception toward COVID-19 vaccines among pregnant women attending ANC in public health facilities of Bench-Sheko zone, southwest Ethiopia, 2021 (N = 412).
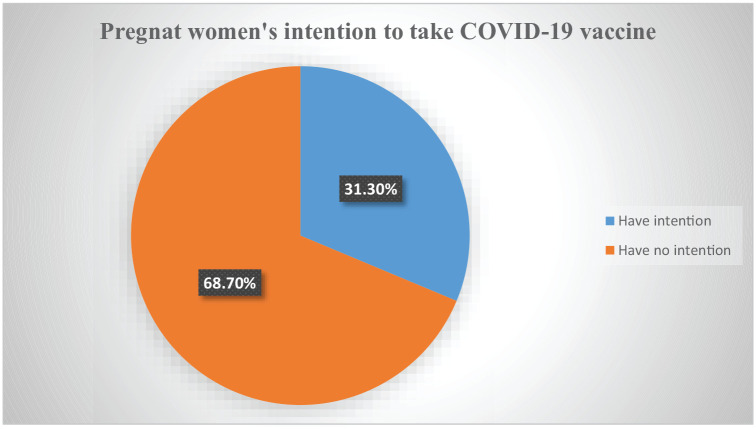
Intention to take COVID-19 vaccine
Pregnant women were asked how likely they think they are to get a COVID-19 vaccine when one is available. Their response was dichotomized as mentioned in the “Methods” section, and only 31.3% (95% confidence interval (CI): 26.7–35.2) of the participants had an intention to take the COVID-19 vaccine when available (Figure 2).
Figure 2.
Intention to take vaccine among women attending ANC in public hospitals of Bench-Sheko zone, southwest Ethiopia, 2021 (N = 412).
Predictors of intention to take COVID-19 vaccine
From the total seven candidate variables entered into multivariable analysis, four variables—namely, residence, education level, compliance to COVID-19 guidelines, and perception toward COVID-19 vaccine—were found to be independently associated with intention to take the COVID-19 vaccine among women attending ANC.
The odds of intention to take COVID-19 vaccine were nearly 2.6 times (adjusted odds ratio (AOR): 2.57, 95% CI: 1.22–5.40) higher among women who live in urban residences. Women with secondary and higher education were four times (AOR: 4.24, 95% CI: 2.23–9.32) more likely intended to take the COVID-19 vaccine than women with no formal education. Compared with those women who had not made compliance with the COVID-19 guidelines, women who had made compliance with the COVID-19 guidelines were nearly six times (AOR: 5.86, 95% CI: 3.40–10.09) more likely to have an intention for COVID-19 vaccination. Moreover, women who had good knowledge were three times (AOR: 3.04, 95% CI: 1.64–5.62) more likely to have an intention for COVID-19 vaccination than those who had poor knowledge (Table 4).
Table 4.
Predictors of women’s intention to take COVID-19 vaccine among women attending ANC at public health facilities of Bench-Sheko zone, southwest, Ethiopia, 2021 (N = 412).
| Variables | Category | Intention to vaccinate | COR (95% CI) | AOR (95% CI) | p value | |
|---|---|---|---|---|---|---|
| Yes, n (%) | No, n (%) | |||||
| Age | 18–24 | 10 (7.8) | 45 (15.9) | 1 | 1 | |
| 25–34 | 93 (72.1) | 183 (64.7) | 2.28 (1.10–4.74) | 2.44 (0.96–6.15) | 0.06 | |
| ⩾35 | 26 (20.2) | 55 (19.4) | 2.13 (0.93–4.87) | 1.75 (0.61–5.00) | 0.298 | |
| Residence | Urban | 112 (86.8) | 140 (49.5) | 6.73 (3.84–11.79) | 2.57 (1.22–5.40) | 0.013* |
| Rural | 17 (13.2) | 143 (50.5) | 1 | 1 | ||
| Educational status | No formal education | 16 (12.4) | 72 (25.4) | 1 | 1 | |
| Primary education | 23 (17.5) | 142 (50.2) | 0.73 (0.36–1.46) | 0.4 (0.67–1.34) | 0.067 | |
| Secondary and above | 90 (69.8) | 69 (24.4) | 5.87 (3.14–10.97) | 4.24 (2.23–9.32) | 0.001* | |
| Compliance with COVID-19 guidelines | Yes | 70 (54.3) | 48 (17.0) | 5.81 (3.65–9.23) | 5.86 (3.40–10.09) | 0.001* |
| No | 594 (5.7) | 235 (83.0) | 1 | 1 | ||
| Risk for COVID-19 | Yes | 107 (82.9) | 194 (68.6) | 2.23 (1.23–3.76) | 1.74 (0.86–3,52) | 0.122 |
| No | 22 (13.1) | 89 (31.4) | 1 | 1 | ||
| Perception toward COVID-19 vaccine | Negative | 31 (24.0) | 164 (58.0) | 1 | 1 | |
| Positive | 98 (76.0) | 119 (42.0) | 4.35 (2.73–6.95) | 3.04 (1.64–5.62) | 0.001* | |
| Knowledge on COVID-19 vaccine | Poor | 97 (75.2) | 175 (61.8) | 1 | 1 | |
| Good | 32 (24.8) | 108 (38.2) | 1.87 (1.17–2.98) | 1.68 (0.88–3.21) | 0.115 | |
COVID-19: coronavirus disease 2019; ANC: antenatal care; COR: crude odds ratio; CI: confidence interval; AOR: adjusted odds ratio; 1: reference category.
p < 0.005.
Discussion
Vaccines have been a successful indicator of disease prevention program for decades.19 Nevertheless, vaccine uncertainty and mistrust are major concerns globally, prompting the WHO to state this hesitation among the top 10 public health threats in 2019.20 Vaccines from several companies have recently been approved; however, their distribution is still limited.21 Ethiopia also planned to vaccinate 20% of her population,22 thus identifying pregnant women’s intention to be vaccinated, and factors hampering vaccination could help the Federal Ministry of Health (FMoH) and other relevant entities tackle the factors in advance and improve COVID-19 vaccine acceptability.
In this study, only 31.3% (95% CI: 26.7–35.2) of the participants had an intention to be vaccinated against COVID-19 when the vaccine will be made available. This finding is more or less comparable with the studies conducted in the Middle East (36.8%), Jordan (28.4%), and Turkey (37%).23–25 However, the finding is much lower when compared with previous studies conducted in different countries.1,26–29 The discrepancy in the above finding might be attributable to the study setting difference where our study employed face-to-face interviews, whereas the other studies were web-based surveys. Besides, since our study participants were pregnant women, more negative responses could occur as pregnant women might have apprehension of vaccine effect on pregnancy.
The current study demonstrated that pregnant women with a higher educational status were more likely to have an intention to be vaccinated against COVID-19; this was corroborated by previous studies, mentioning high hesitancy toward COVID-19 vaccine among less educated people.1 This might be due to the fact that more educated people have better access to vaccine information and are also able to comprehend information regarding COVID-19 vaccine benefits and safety; on the contrary, it is more likely that less educated people would be prone to vaccine misinformation.
According to this study, pregnant women residing in urban areas were more likely to have an intention to be vaccinated against COVID-19, which is quite consistent with previous studies.30,31 A higher vaccine acceptance among urban residents could be explained as people living in urban areas have improved health coverage and have more exposure to different media than people living in rural areas. Furthermore, when compared with the urban community, a rural community might oppose vaccination due to certain cultural values and religious standpoints denouncing vaccination.32
A significant proportion of the pregnant women in this study had poor compliance with government COVID-19 guidelines; however, it is essential to note that those pregnant women who had good compliance with the government COVID-19 guidelines were more likely to have the intention to vaccinate against COVID-19. In line with the current study, high vaccine hesitancy and unwillingness to COVID-19 vaccine were noted among people who demonstrated poor compliance with COVID-19 guidelines such as social distancing, use of facemask, and frequent hand washing.18 Evidence suggests that people who trust government’s message are more likely to adhere with disease preventive behavioral guidelines. Thus, it is indispensable for the government to build trust with the public and explicitly communicate vaccine efficacy, side effect, and safety via mainstream media and some other means.
The other most important predictor of vaccine intention among pregnant women was their perception of the COVID-19 vaccine. Pregnant women who had a good perception of the COVID-19 vaccine were more likely to vaccinate against COVID-19. Other studies also affirmed this claim revealing the fact that the widespread mistrust and negative vaccine perception are adversely impacting vaccine uptake among the general population group in the United Kingdom.18 Tackling of the COVID-19 misconceptions is very crucial to improve vaccine uptake and ultimately attain herd immunity.
Limitations of the study
The finding of this study should be seen in light of the following limitations: due to time and resource constraints, we were unable to consider a larger sample size that would further improve the representativeness of the data.
Conclusion
In conclusion, intention to vaccinate against COVID-19 among pregnant women in Bench-Sheko zone was very low when compared with previous studies, and pregnant women’s intention to vaccinate against COVID-19 was significantly associated with attaining secondary education and above, residing in urban areas, being compliant with government COVID-19 guidelines, and having good perception toward COVID-19 vaccine. Hence, before commencing the COVID-19 vaccination program in Ethiopia, it is essential for the Ethiopian FMoH and other relevant entities to launch a widespread public health education campaign that could improve people’s perception of the vaccine by tackling the existing misinformation and mistrust regarding the vaccine. Besides, the upcoming public health intervention programs better put special emphasis on community members with lower educational attainment backgrounds and rural residents. Finally, we call upon future qualitative research to further explore people’s perceptions and mistrust surrounding the vaccine.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121211038454 for Predictors of pregnant women’s intention to vaccinate against coronavirus disease 2019: A facility-based cross-sectional study in southwest Ethiopia by Shewangizaw Hailemariam, Besufekad Mekonnen, Nigusie Shifera, Biruk Endalkachew, Molla Asnake, Ashenafi Assefa and Qaro Qanche in SAGE Open Medicine
Acknowledgments
The authors would like to thank Mizan-Tepi University for technical support and ethical approval, study participants, and data collectors.
Footnotes
Author contributions: S.H., B.M., N.S., B.E., A.A., and Q.Q. wrote the protocol and participated in data collection. S.H., B.M., and N.S. analyzed the data and wrote the manuscript. S.H., M.A., Q.Q., B.M., and B.E. performed manuscript edition. All authors read and approved the final manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Data availability: The dataset collected and analyzed for the current study is available from the corresponding author and can be obtained upon reasonable request.
Ethical approval: Ethical approval for this study was obtained from College of Health Science, Mizan-Tepi University, Ref HSE/004112/2013.
Informed consent: Written informed consent was obtained from all participants (including who could not read and write).
ORCID iDs: Shewangizaw Hailemariam  https://orcid.org/0000-0001-8733-8474
https://orcid.org/0000-0001-8733-8474
Molla Asnake  https://orcid.org/0000-0001-6665-7900
https://orcid.org/0000-0001-6665-7900
Supplemental material: Supplemental material for this article is available online.
References
- 1.Malik AA, McFadden SM, Elharake J, et al. Determinants of COVID-19 vaccine acceptance in the US. EClinicalMedicine 2020; 26: 100495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mekonnen B, Hailemariam S, Ejigu A, et al. Preparedness and readiness against COVID-19 pandemic in prison institutions and detention centers in southwest Ethiopia. Int J Gen Med 2021; 14: 337–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Worldometer. Countries where COVID-19 has spread, https://www.worldometers.info/coronavirus/countries-where-coronavirus-has-spread/ (accessed 20 March 2021).
- 4.Hailemariam S, Agegnehu W, Derese M.Exploring COVID-19 related factors influencing antenatal care services uptake: a qualitative study among women in a rural community in southwest Ethiopia. J Prim Care Commun Health 2021; 12: 1996892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mekonnen B, Solomon N, Wondimu W.Healthcare waste status and handling practices during COVID-19 pandemic in Tepi General Hospital, Ethiopia. J Environ Public Health 2021; 2021: 6614565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sallam M, Dababseh D, Eid H, et al. High rates of COVID-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines 2021; 9(1): 42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mohamud AI, Mohamed SA, Abdullahi K.Assessments of a COVID-19 vaccine acceptance rate in population of Benadir region, Somalia. J Dent Med Sci 2021; 20(1): 1–4. [Google Scholar]
- 8.CDC. Building confidence in COVID-19 vaccines, https://www.cdc.gov/vaccines/covid-19/vaccinate-with-confidence.html (accessed 20 March 2021).
- 9.Lazarus JV, Ratzan SC, Palayew A, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med 2021; 27: 225–228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Skjefte M, Ngirbabul M, Akeju O, et al. COVID-19 vaccine acceptance among pregnant women and mothers of young children: results of a survey in 16 countries. Eur J Epidemiol 2021; 36: 197–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Enitan SS, Oyekale AO, Akele RY, et al. Assessment of knowledge, perception and readiness of Nigerians to participate in the COVID-19 vaccine trial. Int J Vaccines Immun 2020; 4: 1–13. [Google Scholar]
- 12.Kreps S, Prasad S, Brownstein JS, et al. Factors associated with US adults’ likelihood of accepting COVID-19 vaccination. JAMA Netw 2020; 3(10): e2025594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hrynick T, Ripoll S, Schmidt-Sane M.Rapid review: vaccine hesitancy and building confidence in COVID-19 vaccination, https://www.socialscienceinaction.org/resources/rapid-review-vaccine-hesitancy-and-building-confidence-in-covid-19-vaccination/ (accessed 20 March 2021).
- 14.Mortazavi F, Mehrabadi M, KiaeeTabar R.Pregnant women’s well-being and worry during the COVID-19 pandemic: a cross-sectional study. BMC Pregnancy Childbirth 2021; 21: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bench Maji Zone. Wacha-Maji road upgrading project, https://www.afdb.org/fileadmin/uploads/afdb/Documents/Project-and-Operations/Ethiopia_-_Wacha-Maji_Road_Upgrading_Project_-_Appraisal_Report.pdf (accessed 20 March 2021).
- 16.Martin LR, Petrie KJ.Understanding the dimensions of anti-vaccination attitudes: the vaccination attitudes examination (VAX) scale. Ann Behav Med 2017; 51(5): 652–660. [DOI] [PubMed] [Google Scholar]
- 17.Parker B.Unhappy consciousness: recognition and reification in Victorian fiction, https://academiccommons.columbia.edu/doi/10.7916/D8SQ8ZX4 (accessed 20 March 2021).
- 18.Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: implications for public health communications. Lancet Reg Health Eur 2021; 1: 100012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vaccines and immunization, https://www.who.int/health-topics/vaccines-and-immunization?gclid=Cj0KCQjw2or8BRCNARIsAC_ppyZIpSAUsqJtN6zatE-G_pjHFu7IaD7d4WvtsYoA1bV_Xh1ntb6hRxUaAnv2EALw_wcB#tab=tab_1 (accessed 1 January 2021).
- 20.Geoghegan S, O’Callaghan KP, Offit PA.Vaccine safety: myths and misinformation. Front Microbiol 2020; 11: 372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.UCHealth. COVID-19 vaccine: vaccine safety, distribution & FAQs, https://www.uchealth.org/services/infectious-diseases/coronavirus-covid-19/covid-19-vaccine/ (accessed 1 January 2021).
- 22.Ethiopia plans to vaccinate 20% population in 202, https://www.aa.com.tr/en/africa/ethiopia-plans-to-vaccinate-20-population-in-2021/2133346 (accessed 6 February 2021).
- 23.Al-Qerem WA, Jarab AS.COVID-19 vaccination acceptance and its associated factors among a middle eastern population. Front Public Health 2021; 9: 632914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sallam M.COVID-19 vaccine hesitancy worldwide: a systematic review of vaccine acceptance rates. BMJ. Epub ahead of print 4 January 2021. DOI: 10.1101/2020.12.28.20248950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mohan S, Reagu S, Lindow S, et al. COVID-19 vaccine hesitancy in perinatal women: a cross sectional survey. J Perinat Med 2021; 49: 678–685. [DOI] [PubMed] [Google Scholar]
- 26.Mappa I, Luviso M, Distefano FA, et al. Women perception of SARS-CoV-2 vaccination during pregnancy and subsequent maternal anxiety: a prospective observational study. J Matern Fetal Neonatal Med. Epub ahead of print 11 April 2021. DOI: 10.1080/14767058.2021.1910672. [DOI] [PubMed] [Google Scholar]
- 27.Carbone L, Mappa I, Sirico A, et al. Pregnant women’s perspectives on severe acute respiratory syndrome coronavirus 2 vaccine. Am J Obstet Gynecol MFM 2021; 3(4): 100352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ceulemans M, Foulon V, Panchaud A, et al. Vaccine willingness and impact of the COVID-19 pandemic on women’s perinatal experiences and practices-a multinational, cross-sectional study covering the first wave of the pandemic. Int J Environ Res Public Health 2021; 18(7): 3367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sutton D, D’Alton M, Zhang Y, et al. COVID-19 vaccine acceptance among pregnant, breastfeeding, and nonpregnant reproductive-aged women. Am J Obstet Gynecol MFM 2021; 3: 100403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Goncu Ayhan S, Oluklu D, Atalay A, et al. COVID-19 vaccine acceptance in pregnant women. Int J Gynaecol Obstet 2021; 154: 291–296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.U.S. Pharmacist. Overcoming COVID-19 vaccine hesitancy, https://www.uspharmacist.com/article/overcoming-covid19-vaccine-hesitancy (accessed 6 February 2021).
- 32.Assfaw YT.Determinants of antenatal care, institutional delivery and skilled birth attendant utilization in Samre Saharti district, Tigray, Ethiopia. Umeå: Umeå University, 2010. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121211038454 for Predictors of pregnant women’s intention to vaccinate against coronavirus disease 2019: A facility-based cross-sectional study in southwest Ethiopia by Shewangizaw Hailemariam, Besufekad Mekonnen, Nigusie Shifera, Biruk Endalkachew, Molla Asnake, Ashenafi Assefa and Qaro Qanche in SAGE Open Medicine