Abstract
Background:
Osgood-Schlatter disease (OSD), an apophyseal injury of the tibial tuberosity, affects up to 1 in 10 adolescents. This condition has previously been assumed to be innocuous and to self-resolve with limited intervention.
Purpose:
To investigate the 24-month prognosis of OSD and examine if ultrasound (US) classification is associated with outcomes.
Study Design:
Case series; Level of evidence, 4.
Methods:
This study included a preregistered prospective cohort of 51 adolescents (aged 10-14 years) diagnosed with OSD who were evaluated for 24 months. The primary outcome at 24-month follow-up was whether participants continued to experience OSD-related knee pain. Baseline US scans were collected and characterized by OSD type (De Flaviis classification) as well as maturation of the tibial tuberosity. Secondary outcomes included sports participation, Knee injury and Osteoarthritis Outcome Score (KOOS) Sport/Recreation subscale, and health-related quality of life (European Quality of Life–5 Dimensions–Youth [EQ-5D-Y]). All participants were invited for re-examination by US at follow-up.
Results:
A total of 51 patients preregistered for the study, with 90% (n = 46) available at follow-up. Of these 46 participants, 37% (n = 17) still reported knee pain due to OSD. In this subgroup, the median duration since symptom onset was 42 months (interquartile range, 38-51 months). More than 1 in 5 participants reported stopping sport due to knee pain, and those who continued to experience knee pain reported significantly worse KOOS Sport/Recreation scores at follow-up compared with patients with no knee pain (mean 74 [95% CI, 63-84] vs 91 [95% CI, 85-97]). Participants with continued OSD-related pain also had lower health-related quality of life (mean difference in EQ-5D-Y, 0.11 [95% CI, 0.06-0.13]). Higher De Flaviis classification at baseline was significantly associated with an increased risk of knee pain at 2 years. Diagnostic US at follow-up demonstrated primarily tendon changes (thickening, positive Doppler signal), as well as an ununited ossicle in 32% of participants who underwent US scanning at follow-up.
Conclusion:
Over one-third of the study participants had knee pain at 2-year follow-up, which was associated with lower sports related function and health related quality of life. This questions the assumption that all patients with OSD experience quick recovery. Participants without any changes on imaging at baseline were less likely to report pain at follow-up.
Keywords: apophysis, growth, overuse, patellar tendon, pediatric sports medicine, imaging
Osgood-Schlatter, also known as Osgood-Schlatter “disease” (OSD), is common in adolescents and is reported to affect up to 1 in 10 of the general population.5 Osgood-Schlatter is associated with sports participation.5 It is considered an apophyseal injury of the tibial tuberosity, the site of attachment of the patellar tendon onto the tibia.1,11,15 The weak apophyseal cartilage is thought to be susceptible to injury before the apophysis is fully matured.18,31 Although the etiology is not fully understood, characteristics such as cartilage swelling and associated tendon changes (including thickening of the patellar tendon and increased Doppler activity) have been documented in patients with OSD.1,4,12,27,29
It has been reported that OSD will resolve with maturation of the tibial tuberosity with no residual symptoms in 90% of cases,2,9 although there have been no data to support this claim. On the contrary, there are documented cases of adults with residual symptoms/sequalae resulting from OSD.3,15,21,28 A retrospective study from Krause and colleagues13 in 1990 stated that at long-term follow-up (mean, 9 years), as many as 1 in 4 patients had continuing additional symptoms into adulthood. The extent of the severity and impact on sport, physical activity, and life in this group was not documented. A more recent retrospective study indicated that at median 4-years follow-up, 60% experienced frequent pain, which is associated with low health-related quality of life (HRQoL) and sports-related knee function.10 These studies are limited by their retrospective nature, and lack of imaging at follow-up. Kaya and colleagues12 documented 50% of adolescents as having continued ultrasound (US) findings consistent with OSD at 24-month follow-up. These adolescents demonstrated functional limitations in objective measures of lower limb strength, power, and endurance performance at 2-year follow-up. Such functional deficits and resulting disability may persist into adulthood. College-aged men with a history of physician-diagnosed unilateral OSD have greater disability compared with matched participants without a history of OSD.28
The aim of the current study was to prospectively determine 24-month prognosis of pain, sports participation, knee function HRQoL, and ultrasonography characteristics. A secondary aim was to investigate if baseline US pathologic findings were associated with outcome. We hypothesized that participants with continued pain at follow-up would have lower sports-related function and HRQoL than those who reported that they had recovered from OSD.
Methods
Study Design and Setting
This was a prospective cohort study conducted in 2 centers in Denmark (Copenhagen and Aalborg). The 24-month follow-up was pre-registered on clinicaltrials.gov (NCT03589001). Reporting of the study followed the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement. A total of 51 adolescents with OSD were recruited between July and November 2016, where baseline data collection was performed. Participants were offered a cinema ticket for participating. After meeting the inclusion criteria (outlined below), participants underwent a 12-week activity modification intervention (outlined in Supplemental Material). No intervention was given beyond this initial patient education and load management. The results of this intervention have already been published.25 The 24-month follow-up occurred between July and November 2018, and no incentive was provided to participate specifically in the follow-up. Parental informed consent was obtained from all participants, and participants gave assent to participate. This follow-up study was approved by a local research ethics committee.
Participants and Recruitment
The 51 participants were recruited through social media advertisements and questionnaires in local schools. All participants reporting knee pain from either of these sources were contacted. If they reported pain at the tibial tuberosity, they were offered a clinical examination by 1 of 2 physiotherapists (L.M.W. and K.K.) in order to determine eligibility. Diagnosis was made based on clinical examination, in line with previous literature.5,29
The inclusion criteria at baseline were as follows: (1) age between 10 and 14 years; (2) pain at tibial tuberosity during 2 or more of the following activities: sitting with a bent knee, squatting, running, jumping, or stair ambulation; (3) pain during palpation of tibial tuberosity; and (4) knee pain for 6 weeks or more.
Potential participants were excluded if they had any other primary knee conditions that may manifest as anterior knee pain (patellofemoral pain, iliotibial band syndrome, Sinding-Larsen-Johansson disease), previous knee surgery, pain from the hip or back that interfered with activities of daily living, habitual patellar luxations, or clinical suspicion of meniscal lesion.
Baseline Assessment
Baseline data collection was performed after inclusion. During the assessment, it was determined if participants were suffering from unilateral or bilateral OSD and which was their affected/more symptomatic knee. Participants completed a self-report questionnaire that included questions on pain intensity (worst pain in the previous week, and worst pain in the previous 24 hours), evaluated on a numeric pain rating scale in the range of 0-10, current sports participation, and sports participation before onset of knee pain. Pain duration was documented as the response to the question “For how long have you experienced your knee pain?”. Knee function was captured by the Knee injury and Osteoarthritis Outcome Score (KOOS) Sport/Recreation subscale (Sport/Rec; range, 0-100 [with 100 being best]). HRQoL was measured by the European Quality of Life–5 Dimensions–Youth (EQ-5D-Y) scale, with index scores in the range of 0 to 1 (1 being best).30 Parents were present during data collection and available to help if needed. These outcomes have previously been used in adolescents with knee pain.23,24
Assessment of Maturation
To estimate time from peak height velocity (PHV), we used the equations proposed by Moore et al17 for maturity offset that have been validated in several European cohorts.19 The equations estimate maturity offset (ie, time from PHV) using anthropometrics: −7.71 + (0.004 × [age × height]) for girls, and −7.99 + (0.004 × [age × height]) for boys.
As it has been recommended that maturity offset be assessed as a categorical rather than continuous value, participants were then classified into 3 distinct categories: (1) pre-PHV (>1 year before PHV); (2) around PHV (within 1 year from PHV); and (3) post-PHV (>1 year after PHV)
Ultrasound Assessment
After baseline data collection, participants were requested to schedule a US examination by a rheumatologist (J.L.O.) with 18 years of experience in musculoskeletal US. Ultrasonography was performed using a Hi Vision Preirus machine (Hitachi Medical Systems UK) with a 18-5 MHz linear array transducer. The US measurements were carried out with the patient in a supine position with either the knee extended when assessing the color Doppler activity or flexed 45° when measuring the thickness of the tendon and evaluating the area of the apophysis.
The color Doppler flow in the tendon and bone was estimated from a longitudinal scan and recorded from 1 to 4 according to the grading scale by Newman et al,19 with grade 1 indicating no Doppler activity. This was then dichotomized into presence or absence of Doppler signal for further descriptions. The stages of maturation of the tibial tuberosity were based on a modified version of those outlined by Nakase and colleagues18 (4 stages, with the addition of a “fully mature” category, similar to other classifications). Classifying OSD type was done using the 4-stage classification proposed by De Flaviis, which has been previously outlined (Table 1).1,4,12
TABLE 1.
OSD Classification of De Flaviis et al4
| Classification | Description |
|---|---|
| Type 1: cartilage swelling alone | Hypoechoic zone superficial to the apophysis of the anterior tibial tubercle representing pretibial cartilaginous swelling with forward displacement of the subcutaneous tissues and elevation of the patellar tendon from the tibial outline on the longitudinal view |
| Type 2: cartilage swelling and bony changes | A fragmented and hypoechoic ossification center in addition to the abovementioned findings |
| Type 3: associated tendinitis | Diffuse thickening of the insertion of the patellar tendon with or without vacuolation |
| Type 4: associated bursitis | Fluid collection in the retrotendineal soft tissue representing infrapatellar bursitis |
Follow-up
Follow-up was conducted between July and November 2018. All participants were provided a link to an online questionnaire (all data were collected and managed through the secure REDcap electronic data capture tools hosted at Aalborg University). Links were sent to parents, requesting them to help their son/daughter to complete the questionnaire. Outcomes were whether or not participants still experienced pain relating to OSD (this was clarified by the following text: “this means the same knee pain you initially had when you participated in the project about treatment of Osgood-Schlatter; Yes/No”). If participants reported “yes,” they were asked to indicate the pain frequency (rarely, monthly, weekly, almost daily), and worst pain in the previous week measured on a 10-point visual analog scale (0 represented no pain and 10 represented worst pain imaginable). Participants were also asked to report when/if their knee pain resolved (within the past week, month, 6 months, 12 months, or more than 1 year ago).
Following this, participants were asked about whether or not they changed sports interest due to knee pain (if so, how) and whether they had reduced sports participation since having knee pain. Knee function and HRQoL were assessed through the KOOS Sport/Rec26 and EQ-5D-Y.30 Participants were also asked if they sought treatment for their knee pain, or if they found it difficult to sleep on the basis of their knee pain (not at all, some nights, most nights). Finally, participants were asked if they would be willing to attend a US examination. If participants responded “yes,” a US examination was undertaken by the same experienced rheumatologist who completed the baseline assessment. This was done using the same procedure and equipment as outlined above at baseline.
Sample Size
The included sample size was one of convenience and was determined by the number of participants included in the original activity modification trial. Therefore, no formal sample size calculation was undertaken for this follow-up study.
Statistical Analysis
Descriptive statistics, including frequencies, means, and standard deviations, were used to describe the population characteristics (duration of knee pain, proportion with pain at follow-up, pain frequency, when pain stopped, US classification, etc). To evaluate the differences in the proportion of participants with pain at follow-up from each of the baseline De Flaviis classification system, the chi-square test of independence was used (with exact test to account for cells with counts <5). A between-group t test was used to determine if there was a difference in KOOS Sport/Rec or HRQoL between those still experiencing pain related to OSD at follow-up compared with those who did not.
Results
Respondents
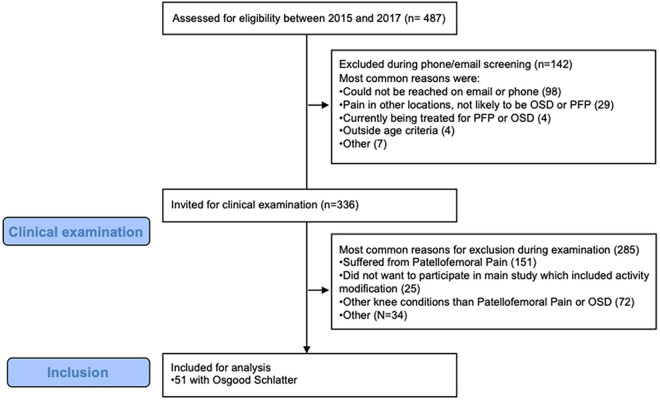
Of the original 51 adolescents included at baseline (Appendix Figure A1), 90% (n = 46) of adolescents responded to the questionnaire at follow-up. Baseline characteristics for participants are shown in Table 2. At baseline, participants reported participating for a median of 4 hours per week (interquartile range [IQR], 3-5 hours per week). Further information on baseline sports participation is shown in Table 3.
TABLE 2.
Baseline Characteristicsa
| Overall Cohort at Baseline (N = 51) | OSD-Related Pain at Follow-up (n = 17) | No OSD-Related Pain at Follow-up (n = 29) | |
|---|---|---|---|
| Female sex | 22 (48) | 9 (53) | 13 (45) |
| Age, y | 12.7 ± 1.1 | 12.7 ± 0.7 | 12.7 ± 1.3 |
| Height, cm | 165.5 ± 8.4 | 167.5 ± 7.2 | 163.7 ± 9.0 |
| Weight, kg | 56 ± 10 | 56 ± 9 | 54 ± 10 |
| Symptoms | |||
| Pain duration, mo | 21 ± 12 | 20 ± 10 | 21 ± 14 |
| Bilateral pain | 35 (66)b | 6 (38) | 8 (28) |
| Time from PHV | |||
| Pre-PHV | 8 (16) | 2 (12) | 4 (14) |
| Around-PHV | 29 (57) | 10 (59) | 17 (59) |
| Post-PHV | 14 (27) | 5 (29) | 8 (28) |
aData are presented as mean ± SD or n (%). OSD, Osgood-Schlatter disease; PHV, peak height velocity.
bMissing data from 1 participant.
TABLE 3.
Overview of Sports Participation at Baseline
| n | |
|---|---|
| Primary sport | |
| Handball | 20 |
| Ballet | 1 |
| Gymnastics/spring gymnastics | 5 |
| Tennis | 1 |
| Football | 17 |
| Swimming | 4 |
| Athletics | 2 |
| Skipping | 1 |
| Primary sport levela | |
| Competitive | 23 |
| Social | 21 |
| Elite | 0 |
| Participation in multiple sports | |
| Yes | 20 |
| No | 31 |
aMissing data from 6 participants who did not respond to this question.
Prognosis at 24-Month Follow-up
Of the respondents, 37% (n = 17) reported that they still experienced knee pain related to OSD. This gave a median pain duration of 42 months (IQR, 38-51 months) since symptom onset for this group. Median pain intensity at follow-up for those who reported pain was 3.7 (IQR, 0.3-6.4). Approximately 35% reported experiencing their pain weekly or more frequently (Table 4). Of the participants who no longer had knee pain, the majority reported that their knee pain had stopped over a year ago. Those who reported pain were of a similar age and estimated maturation status (time from PHV) at baseline with those with no knee pain at follow-up (Table 2).
TABLE 4.
Pain Frequency for Those With Knee Pain at Follow-up
| Pain Frequency | n (%) |
|---|---|
| Never | 0 (0) |
| Rarely | 7 (41.2) |
| Monthly | 4 (23.5) |
| Weekly | 3 (17.6) |
| Several times a week | 1 (5.9) |
| Nearly daily | 2 (11.8) |
Five participants reported seeking additional treatment for their knee pain: 4 with a physiotherapist, 1 with a general practitioner, 1 with an osteopath, and 1 with a body self-development system therapist (some selected >1 option).
Knee Function, HRQoL, and Sleep
Knee function evaluated by the KOOS Sport/Rec subscale increased from baseline to 24-month follow-up (mean difference [MD], 47 [95% CI, 40-55]; t(1,44) = 13.117; P < .0005). Those who continued to experience knee pain reported significantly worse scores at follow-up compared with patients without knee pain (mean, 74 [95% CI, 63-84] vs 91 [95% CI, 85-97]; t(1,43) = 3.152; P = .003) (Figure 1).
Figure 1.
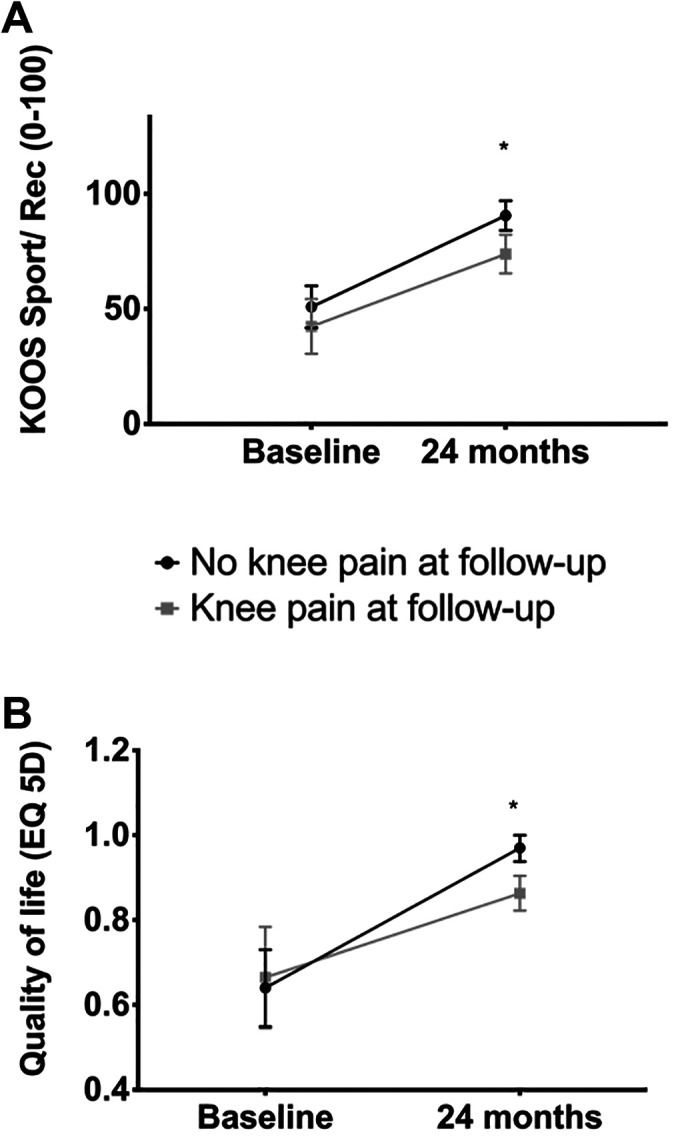
(A) KOOS Sport/Recreation (Sport/Rec) subscale and (B) EQ-5D-Y for those with and without knee pain at follow-up. *Statistically significant difference between groups (P < .05). EQ-5D-Y, European Quality of Life–5 Dimensions–Youth; KOOS, Knee injury and Osteoarthritis Outcome Score.
Similarly, the EQ-5D-Y index score significantly increased from baseline to 24-month follow-up (MD, 0.3 [95% CI, 0.2-0.4]; t(1,44) = 7.543; P < .0005). At follow-up, those with knee pain had significantly lower HRQoL (mean, 0.97 [95% CI, 0.94-1.0] vs 0.86 [95% CI, 0.81-0.91]; MD, 0.11 [95% CI, 0.06-0.13]; t(1,43) = 4.36; P < .0005) (Figure 1). Three participants (6.5%) reported knee pain interfering with their sleep “some nights.”
Sports Participation
At 24-month follow-up, more than 1 in 5 participants (22%) reported stopping their sport because of knee pain. Of those without knee pain at follow-up, 11% reported they did not play sport (currently) compared with 24% of those with knee pain at follow-up. Participants who participated in sport played 2.7 times/week (95% CI, 1.2-3.1) on average, or 2 h/week (95% CI, 1.4-2.4). Seventeen reported they had changed their sport interest since their knee pain (43% without vs 29% with knee pain). Of these, 12 reported having to stop at least 1 specific sport due to their pain (primarily handball and football). No participant reported current use of painkillers to manage their knee pain.
Baseline Ultrasound Findings
At baseline, the majority of participants had findings consistent with the De Flaviis classification (Table 5). Seven participants showed no changes, aligning with the De Flaviis classification on imaging, but all demonstrated positive Doppler activity in the tendon or at the tibial tuberosity. The Fisher exact test showed a statistically significant difference (Fisher exact = 8.9; P = .037) in the proportions of De Flaviis classification on the most symptomatic limb and having pain at follow-up (Figure 2). Those classified as “normal” according to the De Flaviis classification were less likely to report pain at follow-up (Figure 2). De Flaviis type 4 (associated bursitis) was associated with a significantly increased proportion reporting knee pain at 2 years (Figure 2). Baseline maturation of the tibial tuberosity is displayed in Table 6.
TABLE 5.
Baseline De Flaviis Categoriesa
| De Flaviis Categorization4 | Affected/More Symptomatic Limb (n = 48) | Contralateral Symptomatic Limb (bilateral pain) (n = 30) | Contralateral Asymptomatic Limb (unilateral pain) (n = 12)b |
|---|---|---|---|
| Type 1: cartilage swelling alone | 4 (7.4) | 1 (3.3) | 0 (0) |
| Type 2: cartilage swelling and bony changes | 4 (7.4) | 5 (16.7) | 0 (0) |
| Type 3: associated tendinitis | 30 (62.5) | 14 (46.7) | 4 (33) |
| Type 4: associated bursitis | 3 (6.3) | 1 (3.3) | 0 (0) |
| Not applicable (normal) | 7 (14.6) | 9 (30) | 8 (66) |
aData are reported as n (%).
bData were not recorded on the asymptomatic limb of 6 participants.
Figure 2.
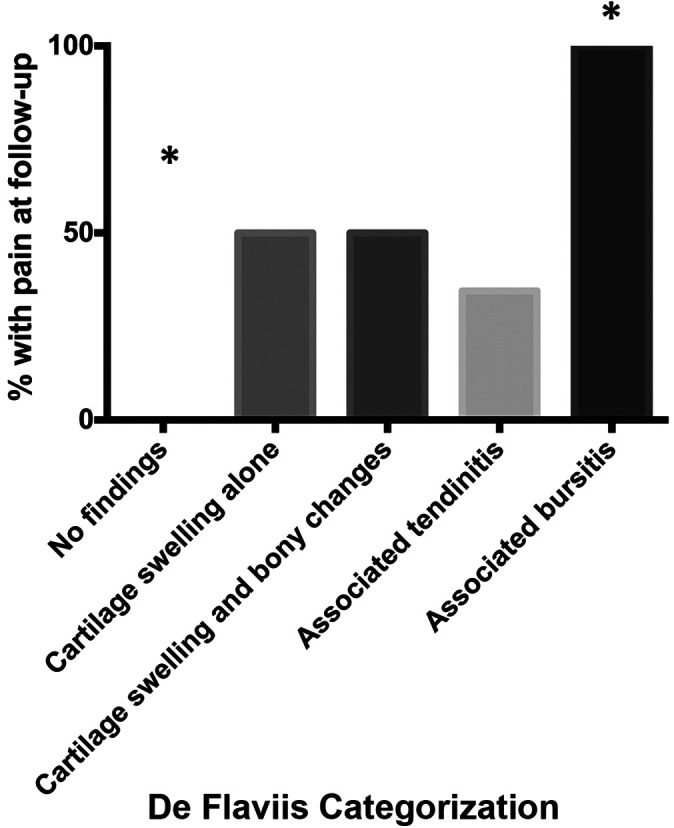
Association between baseline De Flaviis characterization and pain at follow-up.
*Significantly different observed proportion compared with expected.
TABLE 6.
Baseline Maturation of the Tibial Tuberositya
| Category | n (%) |
|---|---|
| 1 Sonolucent stage | 10 (20.8) |
| 2 Individual stage | 7 (14.6) |
| 3 Connective stage | 20 (41.7) |
| 4 Fully mature | 11 (22.9) |
aBased on the classification by Nakase et al.18
At baseline, 63% had positive Doppler signal (graded >1) at the tibial tuberosity on their most symptomatic limb (22% grade 2; 28% grade 3; 13% grade 4), while 94% had positive Doppler signal at the tendon of their affected/more symptomatic limb (7% grade 2; 24% grade 3; 63% grade 4). For those with bilateral pain, positive Doppler activity was detected at the tibial tuberosity in 67% and in the tendon in 80%, compared with 41.7% and 25%, respectively, for the unaffected limb in patients with unilateral pain.
Subgroup With Ultrasound at Follow-up
Nineteen respondents consented to and underwent a US examination at follow-up, conducted by the same experienced rheumatologist who examined them at baseline. Of these, 11 had reported pain at follow-up, with 9 presenting with bilateral pain at clinical examination. The majority (58%) were fully mature at follow-up, while the remaining were classified as Nakase grade 3 (42%). US features at follow-up were primarily related to De Flaviis type 3 associated tendinitis and thickening of the distal patellar tendon (Table 7 and Figure 3A). Additionally, 6 of the participants (32%) had a united ossicle observed in at least 1 knee at follow-up (Figure 4). Of them, 42% had positive Doppler signal in the tendon, while 16% had positive Doppler in the bone at follow-up. Findings for the contralateral limb of 5 participants (all with bilateral pain) categorized as “associated tendinitis” on their contralateral limb are displayed in Table 7.
TABLE 7.
De Flaviis Classification for Participants With Ultrasound Examination at 24-Month Follow-up (n = 19)a
| De Flaviis Categorization | Affected/More Symptomatic Limb | Contralateral limb |
|---|---|---|
| Type 1: cartilage swelling alone | — | — |
| Type 2: cartilage swelling and bony changes | 1 (5.3) | — |
| Type 3: associated tendinitis | 10 (52.6) | 5 (26.3) |
| Type 4: associated bursitis | — | — |
| Not applicable (normal) | 8 (42) | 14 (73.7) |
aData are reported as n (%). Dashes indicate no participants in this category.
Figure 3.
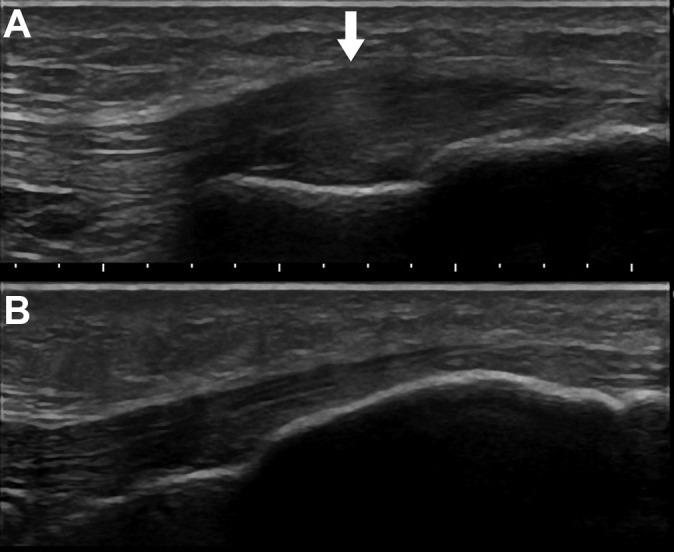
Representative images of a participant (A) with thickening of distal patellar tendon on the right knee (arrow) at follow-up and (B) contralateral asymptomatic left knee at follow-up. Participant reported continued pain (monthly) on the right knee at follow-up.
Figure 4.
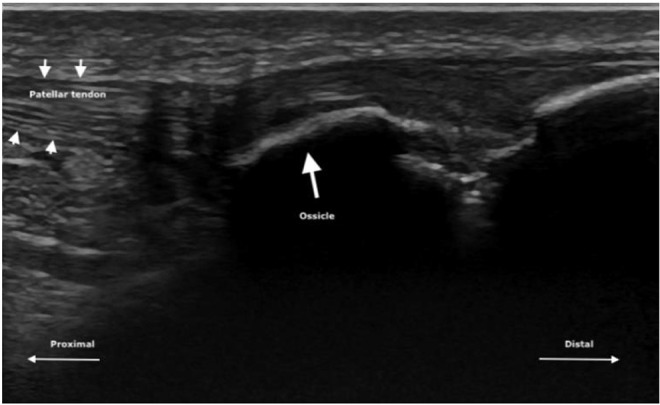
Representative image of participant presenting with ossicle on ultrasound examination at follow-up. Participant reported minimal pain on palpation at clinical examination. Small arrows demonstrate the border of the patellar tendon, while the large arrow indicates the ossicle.
Discussion
In this prospective cohort, nearly 40% of patients with OSD reported OSD-related pain at long-term follow-up. Those with pain at 24 months had a history of OSD-related pain for a median of 42 months at follow-up. This contradicts recent opinions in our survey of health care professionals, in which it was expected that the majority of patients would return to sport free of symptoms within 6 months.16 On the contrary, there may be a subgroup of patients who experience longer symptom duration and impact. Those who continued to experience OSD-related knee pain at follow-up had lower knee-related sports function and HRQoL than those who recovered from OSD during follow-up. Baseline De Flaviis categorization was associated with worse prognosis of pain, while those without identifiable changes at baseline (cartilage swelling, bony change, and/or associated tendinopathy/bursitis) demonstrated significantly better prognosis.
The participants who were “recovered” at follow-up (ie, no longer reporting pain), reported mean KOOS and EQ-5D-Y index scores lower than what has been documented for controls without knee pain.22 This indicates potential longer-term disability and functional deficits in patients with a history of OSD, corroborating previous findings.12,28 There may be a need for greater focus on rehabilitation and helping patients with OSD return to full performance after pain has subsided. This is underscored by the fact that we documented a high rate of sports dropout. Similarly, Kujala et al14 indicated that >70% of participants with OSD were restricted in their sports participation for 10 months on average and that 1 in 3 who were symptom-free for 3 months experienced a recurrence of pain. Together with the current data, this may indicate the need for ongoing management and potentially longer-term limitations than previously assumed.
OSD is considered a well-defined clinical diagnosis consisting primarily of localized pain presenting at the tibial tuberosity, with no evident history of trauma. It is commonly reported due to sports activity and is considered an “overuse injury.”5 A recent survey across health care practitioners highlighted that the majority of clinicians are confident to make the diagnosis based on clinical examination and history, without the use of imaging.16 Despite this, the pathology remains controversial, and the majority of the literature has focused on imaging to characterize the pathophysiology. Originally, OSD was described by both Osgood and Schlatter to be attributable to avulsion of the tibial tuberosity due to forceful patellar tendon contractions.20 Since these original case studies, it has been demonstrated that fragmentation may be a normal part of maturation and not necessarily indicative of pathology.7,8
The presence of soft tissue changes, such as in the patellar tendon, has been highlighted as characteristic of OSD.6,11,27,29 In our study, the majority of participants categorized as having “associated tendinitis” was a larger proportion than observed in other studies, with much variability between studies.1,4,12 This may be due to differences in raters or advances in the US equipment over time. The inter- or intrarater reliability of the De Flaviis classification has not to our knowledge been evaluated. This may be important for future research, and there may be a need to develop a new classification. Findings from Sailly et al29 highlighted positive Doppler signal, which was related to pain intensity on contraction. In the current study, >90% had positive Doppler, including participants without identifiable characteristics according to the De Flaviis categorization. This may indicate a specific phenotype or less-severe cases. It has previously been reported that in the early stages, imaging findings might be negative.11 A descriptive retrospective study by Krause and colleagues13 from 1990 described “two distinct groups” based on the extent of imaging findings (radiograph), with those who had an “abnormal tibial profile” presenting with continued pain at long-term follow-up. Despite differences in imaging modalities and characteristics documented, this may point toward different subgroups of the clinical diagnosis of OSD or that early detection of symptoms before pathological tissue changes is favorable for prognosis. Further research in this area is warranted, particularly as the relationship between tissue changes and pain is not yet fully understood.
Our sample reported pain symptoms for nearly 2 years already at baseline, and a certain proportion (23%) were fully mature at the tibial tuberosity at baseline, which may be owing to the age range (10-14 years) of our inclusion criteria. This may therefore represent a select group of the overall patients with OSD. However, the observation that some of these adolescents had pain after maturation of the tibial tuberosity is in contrast to the prevailing opinion that OSD self-resolves with ossification of the tibial tuberosity. OSD-related pain may not only be related to the tibial tuberosity, but also to soft tissues. In the present cohort study, the main US findings at follow-up were related to thickening and Doppler in the tendon, but 6 participants also had an ununited ossicle. Interestingly, in a retrospective study, Kujala et al14 also reported that participants with OSD had pain in the region of the patellar tendon at follow-up. Using magnetic resonance imaging (MRI), Hirano et al11 described a group of patients in the “terminal stage” who demonstrated a thickening of the patellar tendon at its insertion site, as well as ossicle formation in many cases. Similarly, in those defined as “healing” by Hirano et al, >50% showed thickening of the patellar tendon at its insertion onto the tuberosity. Using MRI, Demirag et al6 found a more proximal and broader patellar tendon attachment in patients with OSD. Our prospective data, together with these observations, may emphasize the potential importance of longer-term changes in patellar tendon characteristics in relation to some patients experiencing OSD. Future research should investigate the relative contribution of this to OSD; at present, it is unclear if what is considered classic OSD is actually commonly occurring with insertional patellar tendinopathy or indeed if there are differences between these conditions among youth. It may be that once the tuberosity matures, pain and tissue changes become localized to the tendon region. However, further research is needed to investigate this.
Limitations
Despite being the largest prospective study on prognosis of patients with OSD, this study was on a small sample of adolescents not recruited from the general population. Our participants were aged 10 to 14 years and reported a long duration of pain symptoms at baseline, which may indicate a severe population. These findings may not be generalizable to all adolescents with OSD, or specifically to those seeking care due to OSD. The relative proportion of patients with OSD who will experience long-standing pain cannot yet be determined. Another limitation is that only a proportion participated in US at follow-up. We did not include any measures to objectively quantify function/performance at follow-up, which is a limitation as was the use of the KOOS for quantifying a self-report function, as none have been specifically designed for this population. Furthermore, we did not include a control group and thus do not have related US findings in active adolescents without symptoms. It is possible that some participants have similar characteristics to those seen in the De Flaviis classification, but that this does not always correlate with symptoms.
Conclusion
In this prospective cohort of adolescents with OSD, over one-third experienced knee pain at 2-year follow-up, and 1 in 5 had dropped out of their sport due to knee pain. Continued pain was associated with decreased HRQoL and knee-related sports function. These findings question the short-lived self-resolving nature of OSD, with no long-term impact. The results suggest that US findings were associated with ongoing pain at 24 months, with those without any changes at baseline being less likely to report pain. Participants who were assessed by diagnostic US at follow-up primarily demonstrated patellar tendon–related changes.
Supplemental Material
Supplemental Material, sj-pdf-1-ojs-10.1177_23259671211022239 for Is the Prognosis of Osgood-Schlatter Poorer Than Anticipated? A Prospective Cohort Study With 24-Month Follow-up by Sinead Holden, Jens Lykkegaard Olesen, Lukasz M. Winiarski, Kasper Krommes, Kristian Thorborg, Per Hölmich and Michael Skovdal Rathleff in Orthopaedic Journal of Sports Medicine
Appendix
Figure A1.
Flowchart of participant inclusion. OSD, Osgood-Schlatter disease; PFP, patellofemoral pain.
Footnotes
Final revision submitted January 20, 2021; accepted February 24, 2021.
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was supported by the Danish Research Council (DFF-4004-00247B), the Independent Research Fund Denmark (IRFD: 9039-00238B), and the TRYG Foundation (grant ID: 118547). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the National Ethics Committee for Region Nordjylland (N-20140100-5).
Supplemental Material for this article is available at http://journals.sagepub.com/doi/suppl/10.1177/23259671211022239.
References
- 1.Blankstein A, Cohen I, Heim M, et al. Ultrasonography as a diagnostic modality in Osgood-Schlatter disease: a clinical study and review of the literature. Arch Orthop Trauma Surg. 2001;121:536–539. [DOI] [PubMed] [Google Scholar]
- 2.Circi E, Atalay Y, Beyzadeoglu T. Treatment of Osgood-Schlatter disease: review of the literature. Musculoskelet Surg. 2017;101:195–200. [DOI] [PubMed] [Google Scholar]
- 3.Circi E, Beyzadeoglu T. Results of arthroscopic treatment in unresolved Osgood-Schlatter disease in athletes. Int Orthop. 2017;41:351–356. [DOI] [PubMed] [Google Scholar]
- 4.De Flaviis L, Nessi R, Scaglione P, Balconi G, Albisetti W, Derchi LE. Ultrasonic diagnosis of Osgood-Schlatter and Sinding-Larsen-Johansson diseases of the knee. Skeletal Radiol. 1989;18:193–197. [DOI] [PubMed] [Google Scholar]
- 5.de Lucena GL, dos Santos Gomes C, Guerra RO. Prevalence and associated factors of Osgood-Schlatter syndrome in a population-based sample of Brazilian adolescents. Am J Sports Med. 2011;39:415–420. [DOI] [PubMed] [Google Scholar]
- 6.Demirag B, Ozturk C, Yazici Z, Sarisozen B. The pathophysiology of Osgood-Schlatter disease: a magnetic resonance investigation. J Pediatr Orthop B. 2004;13:379–382. [DOI] [PubMed] [Google Scholar]
- 7.Ducher G, Cook J, Lammers G, et al. The ultrasound appearance of the patellar tendon attachment to the tibia in young athletes is conditional on gender and pubertal stage. J Sci Med Sport. 2010;13:20–23. [DOI] [PubMed] [Google Scholar]
- 8.Ducher G, Cook J, Spurrier D, et al. Ultrasound imaging of the patellar tendon attachment to the tibia during puberty: a 12-month follow-up in tennis players. Scand J Med Sci Sports. 2010;20:e35–e40. [DOI] [PubMed] [Google Scholar]
- 9.Gholve PA, Scher DM, Khakharia S, Widmann RF, Green DW. Osgood Schlatter syndrome. Curr Opin Pediatr. 2007;19:44–50. [DOI] [PubMed] [Google Scholar]
- 10.Guldhammer C, Rathleff MS, Jensen HP, Holden S. Long-term prognosis and impact of Osgood-Schlatter disease 4 years after diagnosis: a retrospective study. Orthop J Sports Med. 2019;7:2325967119878136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hirano A, Fukubayashi T, Ishii T, Ochiai N. Magnetic resonance imaging of Osgood-Schlatter disease: the course of the disease. Skeletal Radiol. 2002;31:334–342. [DOI] [PubMed] [Google Scholar]
- 12.Kaya DO, Toprak U, Baltaci G, Yosmaoglu B, Ozer H. Long-term functional and sonographic outcomes in Osgood-Schlatter disease. Knee Surg Sports Traumatol Arthrosc. 2013;21:1131–1139. [DOI] [PubMed] [Google Scholar]
- 13.Krause BL, Williams JP, Catterall A. Natural history of Osgood-Schlatter disease. J Pediatr Orthop. 1990;10:65–68. [PubMed] [Google Scholar]
- 14.Kujala UM, Kvist M, Heinonen O. Osgood-Schlatter’s disease in adolescent athletes: retrospective study of incidence and duration. Am J Sports Med. 1985;13:236–241. [DOI] [PubMed] [Google Scholar]
- 15.Lee DW, Kim MJ, Kim WJ, Ha JK, Kim JG. Correlation between magnetic resonance imaging characteristics of the patellar tendon and clinical scores in Osgood-Schlatter disease. Knee Surg Relat Res. 2016;28:62–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lyng KD, Rathleff MS, Dean BJF, Kluzek S, Holden S. Current management strategies in Osgood Schlatter: a cross-sectional mixed-method study. Scand J Med Sci Sports. 2020;30(10):1985–1991. [DOI] [PubMed] [Google Scholar]
- 17.Moore SA, McKay HA, Macdonald H, et al. Enhancing a somatic maturity prediction model. Med Sci Sports Exerc. 2015;47:1755–1764. [DOI] [PubMed] [Google Scholar]
- 18.Nakase J, Aiba T, Goshima K, et al. Relationship between the skeletal maturation of the distal attachment of the patellar tendon and physical features in preadolescent male football players. Knee Surg Sports Traumatol Arthrosc. 2014;22:195–199. [DOI] [PubMed] [Google Scholar]
- 19.Newman JS, Laing TJ, McCarthy CJ, Adler RS. Power Doppler sonography of synovitis: assessment of therapeutic response---preliminary observations. Radiology. 1996;198:582–584. [DOI] [PubMed] [Google Scholar]
- 20.Osgood RB. Lesions of the tibial tubercle occurring during adolescence. Boston Med Surg J. 1903;148:114–117. [PubMed] [Google Scholar]
- 21.Pihlajamaki HK, Visuri TI. Long-term outcome after surgical treatment of unresolved Osgood-Schlatter disease in young men: surgical technique. J Bone Joint Surg Am. 2010;92(suppl_1):258–264. [DOI] [PubMed] [Google Scholar]
- 22.Rathleff M, Winiarski L, Krommes K, et al. Pain, sports participation, and physical function in 10-14 years olds with patellofemoral pain and Osgood Schlatter: a matched cross-sectional study of 252 adolescents. J Orthop Sports Phys Ther. 2020;50:149–157. [DOI] [PubMed] [Google Scholar]
- 23.Rathleff MS, Rathleff CR, Olesen JL, Rasmussen S, Roos EM. Is knee pain during adolescence a self-limiting condition? Prognosis of patellofemoral pain and other types of knee pain. Am J Sports Med. 2016;44:1165–1171. [DOI] [PubMed] [Google Scholar]
- 24.Rathleff MS, Roos EM, Olesen JL, Rasmussen S. High prevalence of daily and multi-site pain---a cross-sectional population-based study among 3000 Danish adolescents. BMC Pediatr. 2013;13:191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rathleff MS, Winiarski LM, Krommes K, et al. Activity modification and knee strengthening for Osgood Schlatter: a prospective cohort study. Orthop J Sports Med. 2020;8(4):2325967120911106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther. 1998;28:88–96. [DOI] [PubMed] [Google Scholar]
- 27.Rosenberg ZS, Kawelblum M, Cheung YY, Beltran J, Lehman WB, Grant AD. Osgood-Schlatter lesion: fracture or tendinitis? Scintigraphic, CT, and MR imaging features. Radiology. 1992;185:853–858. [DOI] [PubMed] [Google Scholar]
- 28.Ross MD, Villard D. Disability levels of college-aged men with a history of Osgood-Schlatter disease. J Strength Cond Res. 2003;17:659–663. [DOI] [PubMed] [Google Scholar]
- 29.Sailly M, Whiteley R, Johnson A. Doppler ultrasound and tibial tuberosity maturation status predicts pain in adolescent male athletes with Osgood-Schlatter’s disease: a case series with comparison group and clinical interpretation. Br J Sports Med. 2013;47:93–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wille N, Badia X, Bonsel G, et al. Development of the EQ-5D-Y: a child-friendly version of the EQ-5D. Qual Life Res. 2010;19:875–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yanagisawa S, Osawa T, Saito K, et al. Assessment of Osgood-Schlatter disease and the skeletal maturation of the distal attachment of the patellar tendon in preadolescent males. Orthop J Sports Med. 2014;2:2325967114542084. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material, sj-pdf-1-ojs-10.1177_23259671211022239 for Is the Prognosis of Osgood-Schlatter Poorer Than Anticipated? A Prospective Cohort Study With 24-Month Follow-up by Sinead Holden, Jens Lykkegaard Olesen, Lukasz M. Winiarski, Kasper Krommes, Kristian Thorborg, Per Hölmich and Michael Skovdal Rathleff in Orthopaedic Journal of Sports Medicine