Abstract
Subtalar instability remains a topic of debate, and its precise cause is still unknown. The mechanism of injury and clinical symptoms of ankle and subtalar instabilities largely overlap, resulting in many cases of isolated or combined subtalar instability that are often misdiagnosed. Neglecting the subtalar instability may lead to failure of conservative or surgical treatment and result in chronic ankle instability. Understanding the accurate anatomy and biomechanics of the subtalar joint, their interplay, and the contributions of the different subtalar soft tissue structures is fundamental to correctly diagnose and manage subtalar instability. An accurate diagnosis is crucial to correctly identify those patients with instability who may require conservative or surgical treatment. Many different nonsurgical and surgical approaches have been proposed to manage combined or isolated subtalar instability, and the clinician should be aware of available treatment options to make an informed decision. In this current concepts narrative review, we provide a comprehensive overview of the current knowledge on the anatomy, biomechanics, clinical and imaging diagnosis, nonsurgical and surgical treatment options, and outcomes after subtalar instability treatment.
Keywords: subtalar, instability, current concepts
Subtalar instability was first described by Rubin150 in 1962, but it still remains a controversial topic. Although subtalar injuries are commonly associated with acute lateral ankle injuries,97,108,156,173 subtalar instability is still an uncertain clinical entity, and its involvement in lateral ankle instability is still unknown. Clinical symptoms of subtalar instability largely overlap with those of lateral ankle instability, making subtalar instability a diagnostic challenge.8,84,86 The precise cause of subtalar instability remains a topic of debate, and only in recent years has subtalar instability been viewed as a distinct clinical entity. Proposed theories include the chronic tear of the calcaneofibular ligament (CFL), the cervical ligament (CL), or the interosseous talocalcaneal ligament (ITCL).5 Isolated injuries of the CFL, the CL, and the ITCL are very uncommon, suggesting a concomitant involvement of other ankle and subtalar ligament injuries. As lateral ankle instability presents a similar mechanism of injury and symptoms, the subtalar instability is often misdiagnosed. Neglecting subtalar instability may lead to failure of surgical treatment of patients presenting with mechanical ankle instability (MAI)5,8 or persistent functional ankle instability (FAI).63,84 It is thus crucial to correctly identify subtalar instability and decide on the best treatment approach. Herein, we provide an overview of the current knowledge on the anatomy, biomechanics, clinical and imaging diagnosis, nonsurgical and surgical treatment options, and outcomes after subtalar instability treatment.
Anatomy of the Subtalar Joint
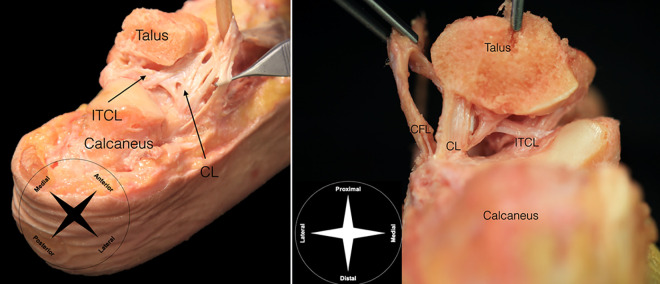
The subtalar joint is composed of the anterior, middle, and posterior articulating facets between the inferior talus and the dorsal aspect of the calcaneus (Figure 1).132 The posterior facet of the talus forms a saddle-shaped joint with the calcaneus covering the largest area of the articular surface of the subtalar joint complex.22 The tarsal canal and the tarsal sinus separate the posterior facet from the anterior and middle facets.23 The posterior facet articulation is set at an oblique axis offset 45° from the longitudinal axis of the foot.60 In some individuals, the middle surface is supported by the sustentaculum tali, and the anterior surface is supported by the anterior process of the calcaneus, creating a new articular surface. The talar head, the calcaneus, and the navicular bony surfaces articulate anteriorly to form the talocalcaneonavicular joint, also known as the acetabulum pedis.22
Figure 1.
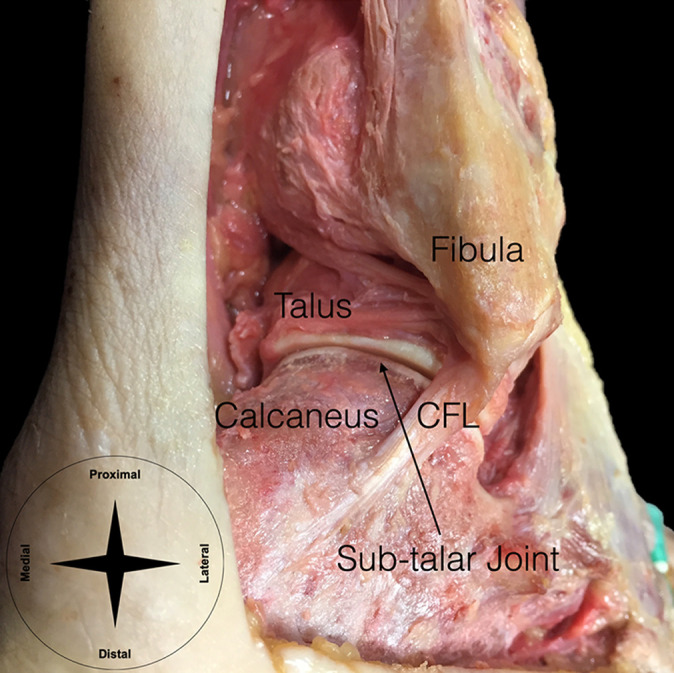
Bony anatomy of the subtalar joint. CFL, calcaneofibular ligament.
The anterolateral ligament complex provides most of the protection against excessive inversion while the central pivot of the subtalar joint occurs at the ITCL,141 which is positioned at the intersection of the long axis of the leg and the axis of Hencke. The lateral subtalar ligament complex is divided into intrinsic and extrinsic ligaments (Figure 2). Intrinsic ligaments include the ITCL and the CL—also called anterolateral talocalcaneal and oblique talocalcaneal ligament—which provide anterior and medial support to the subtalar joint. There are variations in orientation of the CL and the ITCL, which should be considered during surgical interventions. The CL is composed of 2 or more bands and usually runs obliquely at a 45° angle through the tarsal sinus, with insertions at the superolateral surface of the calcaneus and the talar neck107,110; however, occasionally, it is seen to course in a vertical manner, suggestive of a stress adaptation.144 The ITCL is usually shaped as a band-type ligament (92.5%) but can also appear as a fan-type (5%) or a multiple-type (2.5%) ligament.76 It is usually described as running obliquely superomedial to inferomedial, although in some specimens fibers that lie in a superolateral to inferomedial direction have been found.87
Figure 2.
Ligamentous anatomy of the subtalar joint. CFL, calcaneofibular ligament; CL, cervical ligament; ITCL, interosseous talocalcaneal ligament.
The anterolateral extrinsic ligament complex consists mostly of the CFL. The CFL is the only ligament at the lateral ankle that crosses both the ankle and the subtalar joint. A few anatomic variants have been described in the literature, including fibers that diverge anteriorly and insert at the lateral talus forming a Y-shaped and a V-shaped CFL139 and that are also possibly related to the lateral talocalcaneal ligament (LTCL). The CFL acts to restrain the anterolateral ankle laxity and is assisted by the LTCL. The talocalcaneal ligament complex is formed by 2 compartments: (1) the superficial lateral compartment, comprising the CL and the sinus tarsi ligaments, along with the inferior extensor retinaculum (IER) and (2) the deep central compartment, including canalis tarsi ligaments, with the ITCL and the deep band of the IER.114
The IER is continuous with the lower leg lateral fascia and is subdivided into 3 layers: (1) the superficial layer inserts into the lateral border of the anterosuperior tubercle of the calcaneus and extends laterally to reinforce the sheath of the peroneal tendons; (2) the intermediate layer forms the pulley for reflection of the extensor digitorum longus and peroneus tertius tendons and inserts into the lateral aspect of the anterior process of the calcaneus; and (3) the deep layer is a part of the central compartment and forms a sling at the neck of the talus, penetrating the canalis tarsi and blending with the ITCL.9 The IER contributes to the stabilization of the central and lateral compartments; the superficial and intermediate layers of the IER, together with the CL, form the most superficial part of the anterolateral ligamentous support, while the deep layer of the IER connects the structures of the lateral and central compartments.114 The CL serves as the strongest connection between the talus and calcaneus and inserts in the dorsal surface of the anterior calcaneal tubercle, where it blends with the fibers of the intermediate layer of the IER. The long axis of the CL fibers is oriented at 45° to 50° to the calcaneus in the sagittal plane.114
The medial ligament complex is composed of the anterior tibiosubtalar section of the deltoid ligament and, in combination with the superomedial aspect of the spring ligament, contributes to keep the subtalar joint stable during sliding, rolling, and torsion.9 The spring ligament complex (also known as the plantar calcaneonavicular ligament) is a group of ligaments that originate on the anterior calcaneus below and between the anterior and medial facets.7 The spring ligament plays a key role in supporting and stabilizing the talar head along with the articulating surfaces of the calcaneus and the navicular and assists in stabilizing the anterior subtalar joint.34,171 The superficial layer of the medial deltoid ligament attaches to the spring ligament via its tibionavicular and anterior tibiotalar portions that together provide anteromedial stabilization to the peritalar joint, known as the “coxa pedis.”142
Biomechanics of the Subtalar Joint
Biomechanics
The position of maximal ankle stability, that is, the close-packed position of the subtalar joint, occurs in the squatting position, which places the talocrural joint in maximum dorsiflexion and the subtalar joint in eversion with calcaneal valgus.154 During dorsiflexion-plantarflexion and inversion-eversion movements, the subtalar joint acts as a uniaxial joint in which the calcaneus rotates under the talus from dorsolateral to medioplantar. In the calcaneal rotation axis, which runs obliquely from anterodorsomedial to posteroplantolateral and penetrates the talar neck, the rotation angle tends to be higher in inversion-eversion (20° ± 2°) than in dorsiflexion-plantarflexion (16° ± 3°). The calcaneal motion occurs predominantly around maximum dorsiflexion and plantarflexion during dorsiflexion-plantarflexion, but it displays an uninterrupted motion during inversion-eversion movements.54 The subtalar joint inclines 42° ± 9° in the sagittal plane and deviates 23° ± 11° medially in the horizontal plane relative to the axis of the foot, allowing for accommodation to uneven surfaces.36 The subtalar joint range of motion (ROM) can vary according to the measurement technique11 and should be carefully interpreted when measured clinically.8
The articular surfaces are not the main source of limitation of talar tilt.25 Primary stabilization of the subtalar joint is variably attributed to the ITCL, the CFL, and the CL.16,30,138,148,175,190 The anterior talofibular ligament (ATFL) and the CFL act synergistically to prevent talar tilt within the ankle mortise.25 The ATFL elongates more during plantarflexion and supination, whereas the CFL increases in length with dorsiflexion and pronation.35 During supination, the CL provides initial stabilization, but when supination is followed by plantarflexion to produce inversion, the ATFL acts to provide secondary stabilization.16 The ATFL primarily restricts internal rotation of the talus in the mortise and adduction in plantarflexion.129 Forced inversion with the ankle in dorsiflexion or neutral sagittal position can lead to damage to the CFL, the CL, and the ITCL, resulting in subtalar joint injury.138
The Role of the CFL and ITCL in Subtalar Instability
The CFL provides exclusive stabilization of the subtalar joint when the ankle is in neutral dorsiflexion-plantarflexion and almost exclusively restricts adduction when the ankle is in neutral position and in dorsiflexion159; during plantarflexion, it is assisted by the ATFL.129 The CFL tightens in supination-dorsiflexion and becomes lax in plantarflexion-eversion.60 It is the second weakest ligament of the ankle, with a load to failure 2 to 3.5 times higher than that of the ATFL.4 After the ATFL, the CFL is the most frequently injured ligament of the lateral ankle complex.37,46,67 Disruption of the CFL leads to a significantly increased laxity in all 3 planes of motion, resulting in mechanical laxity of the joint.105,118,190 Cadaveric studies have shown that ankle sprains that include CFL injury result in decreased rotation stiffness and peak torque, alteration of contact mechanics, increased inversion of the talus and calcaneus, and increased medial translation coupled with anterior or posterior displacement of the calcaneus.6,73,146,200 Repairing both the ATFL and the CFL simultaneously is the cornerstone of hindfoot and midfoot kinematics after combined injury.15 When repairing the CFL and the ATFL simultaneously in a cadaveric model and applying an inversion torque from 0° to 20° of inversion, D’Hooghe et al41 reported that the CFL failed first (before the ATFL) and at significantly lower torque (the ATFL failed at 40% more torque) and lower rotation angle (the ATFL failed at more 62% rotation), which indicated vulnerability of the repaired CFL. These findings suggest that we should allow sufficient time for ligament healing before loading the ankle in the rehabilitation course. Combined injuries of the CFL, the ITCL, and the CL potentially cause chronic subtalar instability. Interestingly, Kamada et al80 reported a case of clinically diagnosed chronic subtalar instability that revealed during arthroscopy an elongated and fibrotic CFL at its calcaneal insertion while the ATFL, the ITCL, and the CL appeared normal. In a cadaveric model, Pellegrini et al138 noted that significant increases in subtalar motion occurred after transection of only the CFL, resulting in increased inversion and external rotation, particularly with dorsiflexion.
Failure of the ITCL can cause subtalar instability because of an unconstrained subtalar axis.16,30,148,174 The combined failure of the ITCL and the ATFL can cause abnormal anterolateral rotatory laxity of the ankle-subtalar joint complex while weightbearing, especially during walking and running.175 Several biomechanical and cadaveric studies16,30,92,148,174,175 have investigated the ITCL role in the ankle-subtalar complex; however, its role remains controversial. Associated injury to the LTCL and/or the IER adds rotational inversion-eversion instability.190 While several authors have considered the CFL as the main restrictor for subtalar instability,138,190 other authors have placed equal or greater importance on the ITCL and CL intrinsic ligaments.8,16,30,148,175
The Role of the Spring Ligament in Subtalar Instability
Deltoid and spring ligament insufficiency are classified according to their location using the Hintermann classification: type 1 is a proximal tear or avulsion of the deltoid ligament, type 2 is an intermediate tear of the deltoid ligament, and type 3 is a distal tear/avulsion of the deltoid and spring ligaments.66 Injuries of the spring ligament are mainly determined by the mechanism and intensity of injury and have a significant clinical relevance, as they cause complex ankle laxity. In peritalar subluxation—characterized by hindfoot valgus, midfoot abduction, and forefoot supination—the spring ligament and other medial soft tissues are weakened, resulting in loss of the medial longitudinal arch. Peritalar subluxation results in an anatomic deformity, placing the forefoot in supination and the midfoot in abduction, with plantarflexion of the talus within the mortise and posterolateral subluxation of the subtalar joint. Rupture or attrition of the spring ligament is now recognized as a contributing factor to hindfoot valgus deformity.133 Fusion of the anterior and middle calcaneal articular facets occurs in 67% of patients, and this pattern can cause laxity of the spring ligament via increased mobility and uneven weight distribution of the talar head.1
How Does Chronic Functional Lateral Ankle Instability Differ From Subtalar Instability?
Whereas MAI is determined purely via physical examination and stress radiography, a diagnosis of FAI involves subjective symptoms and clinical signs. FAI develops from postural deficiency,21,62,120 proprioceptive impairment,20,49,157 neuromuscular control deficits,38,136,191 and muscle weakness,42,81,194 as opposed to MAI that originates from ligamentous laxity.63,70,71 Patients with chronic ankle instability (CAI) may display mechanical laxity, functional instability, or recurrent sprains, which can occur independently or in combination.65
Patients with CAI may express signs of apprehension and avoidance of weightbearing, describe a history of recurrent ankle sprains, and often require the use of braces and other precautions.65,186 On physical examination, subtalar instability can display similar presentation to CAI.2 Intricate anatomy and biomechanics of the ankle joint complex make it difficult to diagnose the subtalar component of CAI, as ankle function cannot be dissociated from the subtalar function. Patients with CAI show reduced supination joint position sense, highlighting the importance of considering the anatomic subtalar joint axis when assessing pronation and supination proprioception.59 Hindfoot varus, plantarflexed first ray, or a cavus foot type are common findings in patients with both CAI and subtalar joint instability,17,103,155 but patients with isolated subtalar instability present an increased foot inward rotation as compared with patients with CAI.2 A report of gait analysis has indicated that patients with CAI show more tibiotalar and subtalar kinematic variation during balanced heel testing, as compared with healthy controls.149
Identifying MAI in functionally unstable ankles is important to understand the origin of instability. Instrumented arthrometer-based assessment has shown that functionally unstable ankles display greater anteroposterior displacement after loading compared with uninjured ankles.72 Still, functionally unstable ankles without MAI can also show abnormal arthrokinematics compared with the contralateral healthy ankle.94 More specifically, ankles with FAI show significantly greater subtalar internal rotation during ankle dorsiflexion as well as during dorsiflexion concurrently with ankle internal rotation.
Diagnosis of Subtalar Instability
Currently, there is no consensus regarding which is the best method for evaluating subtalar instability or laxity.128 It is difficult to correctly establish the diagnosis, and it is often overlooked in traditional lateral ankle instability.5 However, clinical examination is the most common method used, and stress radiographs and magnetic resonance imaging (MRI) can also play an important role.128 There are several available diagnostic procedures that should be combined to assess subtalar instability (Table 1).
TABLE 1.
Available Diagnostic Methods for Subtalar Instabilitya
| Diagnostic Method | Purpose |
|---|---|
| Clinical history | Mechanism of injury, symptoms |
| Physical examination | Signs of ligament injury, lower leg alignment, manual stress testing |
| Imaging | |
| Stress radiography | Objective assessment of subtalar laxity |
| Using MRI | Assess structural integrity of subtalar ligaments and peripheral structures |
| Subtalar arthrography | Assess structural integrity of subtalar ligaments and peripheral structures |
| CT | Hindfoot alignment and damage of peripheral bony structures; useful if combined with stress measurements |
| Using US | Assess structural integrity of subtalar ligaments with dynamic testing |
| Diagnostic arthroscopy | In cases that show equivocal findings; helpful to visualize ligaments that are difficult to assess in MRI/US (eg, ITCL) |
aCT, computed tomography; ITCL, interosseous talocalcaneal ligament; MRI, magnetic resonance imaging; US, ultrasound.
There are a few researchers who have suggested a set of 5 clinical criteria to diagnose subtalar instability.78,91,199 Patients with subtalar instability present at least 4 of the 5 following criteria: (1) recurrent ankle sprain, (2) sinus tarsi pain and tenderness, (3) hindfoot looseness or giving way, (4) hindfoot instability on physical examination, and (5) radiographic subtalar instability on ankle and Broden varus stress views (ipsilateral subtalar tilt >10° or contralateral subtalar tilt difference >5°). These diagnostic guidelines can help clinicians when establishing the diagnosis in patients in whom subtalar instability is suspected, but they still require further research to validate their accuracy in identifying patients with isolated and combined subtalar instability and laxity.
Clinical Evaluation
A thorough clinical history is the cornerstone of correct diagnosis. On initial evaluation of an acute injury, the clinical information in terms of the injury mechanism can help the clinician to understand how the injury occurred and which structures may be injured. Symptoms of ankle and subtalar instability are similar, and distinguishing between these pathological entities is challenging.8,84,86 Most patients give a history of an acute inversion injury and may describe hearing a “pop” upon injury.84 Patients with chronic injuries may describe other symptoms, such as a feeling of “giving way,” recurrent swelling, subtalar joint stiffness, and diffuse pain in the hindfoot, with significant aggravation during sports activities or walking on uneven ground. Questioning when and how the instability symptoms initiated can help to differentiate clinical instability from patient apprehension.
Initial physical examination should include assessment of the lower leg alignment in all planes. The foot should be assessed for cavus or planus deformities and, when present, whether they are flexible or fixed. Examination should also include the Silfverskiöld test to rule out gastrocnemius tightness.180 A positive Molloy impingement test is indicative of posttraumatic synovial impingement.131 Maximal tenderness is usually elicited over the ATFL. Pain inhibition in the acute stage can produce false-negative results, making initial clinical evaluation challenging. Repeating the examination several days later can help to clarify the initial findings and distinguish between minor and more severe injuries involving ligamentous damage. Tenderness is not effective for diagnosing ligamentous injury, although in combination with ecchymosis or hematoma it reaches 90% sensitivity.26
Manual stress testing is an essential component of the clinical evaluation, but it is inherently difficult to quantify and is limited to the practitioner’s sensibility and experience.50 Pain may preclude the ability to perform provocative tests in patients with acute symptoms or lead to false-negative results.129,180 Delayed physical diagnostic examination (4 to 5 days postinjury) provides higher diagnostic accuracy, with high sensitivity and specificity (96% and 84%, respectively).182 When the level of pain allows, the clinician should stress the hindfoot and will usually find an increased amount of inversion.86 With delayed assessment, the ecchymosis or the hematoma disappears, but the lateral sinus tarsi tenderness remains.8
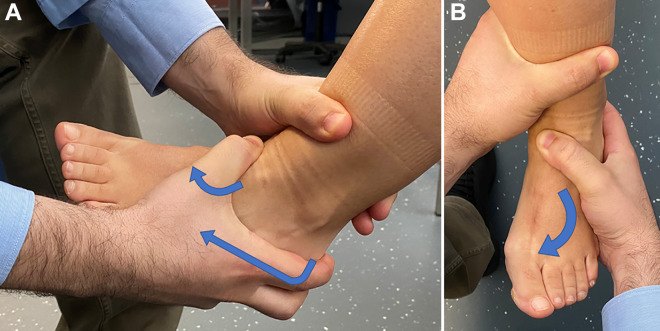
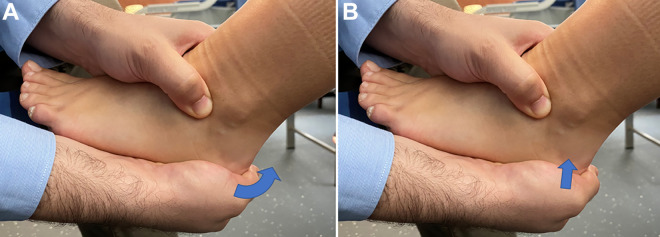
There are a few manual tests for assessing the subtalar joint, but none can be used to reliably diagnose subtalar instability or truly differentiate between subtalar and lateral ankle instability.125 In 1997, Thermann et al173 introduced the rotation stress test assisted by radiography, where the clinician applied inversion and internal rotation stress, followed by an adduction stress to the forefoot, while holding the heel and the forefoot rigid, with the foot in 10° of dorsiflexion. They noticed that in cases of subtalar instability, there was an increased medial shift of the calcaneus (>5 mm) or a larger opening of the subtalar angle (>5°). The anterolateral drawer test is used to assess subtalar joint laxity (Figure 3). In case of subtalar laxity, the test stress will cause increased anteromedial shift and varus tilt of the hindfoot.130 In a cadaveric study with selective ligament sectioning, this test showed high sensitivity (100%) and reasonable specificity (67%).184 The talar tilt stress test (Figure 4A) will usually be positive in the presence of complete disruption of the CFL; however, a negative result does not rule out instability.180 The medial subtalar glide test (Figure 4B) can also identify a subgroup of patients who display subtalar instability in addition to CAI.63
Figure 3.
The anterolateral drawer test to assess subtalar joint laxity. The tibia is stabilized and the hindfoot is held with maximum ankle dorsiflexion to lock the joint in the ankle mortise and avoid tibiotalar movement. Then, (A) anterior stress is applied at the posterior calcaneus, (B) combined with inversion, internal rotation, and adduction of the forefoot, as shown by arrows.
Figure 4.
The talar tilt test to assess subtalar joint laxity. The tibia and fibula are stabilized proximally and (A) a varus stress (arrow) is applied while holding the calcaneus for the talar tilt stress test or (B) it is applied a medially directed stress (arrow) while holding the calcaneus for the medial subtalar glide test.
Imaging Evaluation
Several imaging options are available to diagnose subtalar instability, including stress radiography, MRI, computed tomography (CT), arthrography, and ultrasound (US) imaging. However, none of these imaging modalities can reliably distinguish between lateral ankle instability and subtalar instability.96
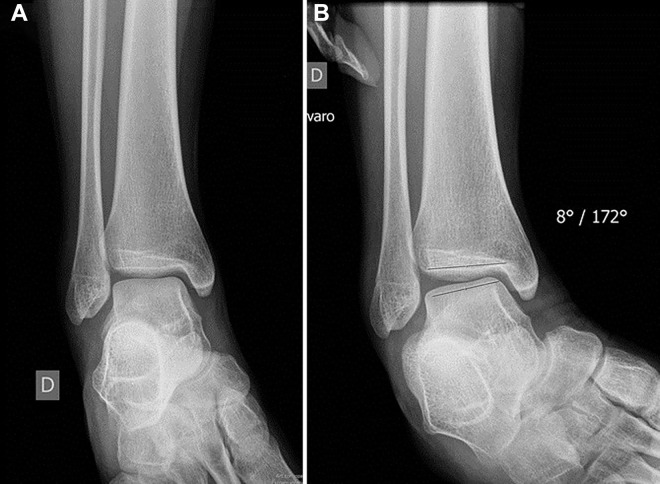
Stress radiography has been used for decades to assess ankle laxity. Stress radiography can be performed using manual stress (Figure 5) or arthrometers, which can show an increased anterior calcaneus translation and higher subtalar talar tilt.85,198,202 However, the subtalar tilt varies substantially among patients with CAI, and the same subtalar tilt seen on stress radiographies does not always reproduce into the same results when using helical CT, which puts into question the reliability and validity of stress radiographs to accurately measure subtalar tilt.183 Combining CT with the Broden view at 45° allows visualization of the posterior subtalar facets and provides better discernment between talocalcaneal and talotibial instability.84 A separation of the posterior facet of the calcaneus and talus >7 mm is indicative of subtalar instability.60 Some caution is advised because the Broden view may give a false impression of tilt, as only the posterior aspect of the subtalar joint is visualized, implying that only the “subluxated” part of the joint is being considered.162 Measuring the medial calcaneal displacement and subtalar tilt after varus stress can detect ITCL injury (100% detection rate).202 Kato85 reported that ≥4 mm of anterior talocalcaneal displacement was indicative of subtalar instability when applying anterior stress during lateral and anteroposterior radiography of the hindfoot. Nonetheless, the correlation with pathological subtalar instability is still uncertain.125 Lee et al98 reported the results of a manual stress radiographic assessment of the anterior-supination drawer test—a variation of the anterolateral manual test (with high intra- and intertester reliability)—and showed an increased talar rotation when there was a combined ATFL and CFL injury and even higher talar rotation if an additional CL injury was also associated. The test showed a fair predictive value for an ATFL and CFL combined injury (area under the curve, 0.78). Still, it must be acknowledged that this test is limited to the experience and sensibility of the examiner. Rather than using 45° Broden stress radiographs, clinicians may consider the measurement of talar rotation using the anterior-supination drawer test and radiography.98,125
Figure 5.
Manual stress radiography under varus stress to assess talar tilt: (A) no stress and (B) with varus stress.
In the setting of a patient with subtalar instability, MRI can be used to assess the ligamentous structural integrity and identify any associated injury that may be associated with subtalar instability.125 MRI offers a precise visualization of the primary subtalar ligaments.109 The ATFL was visualized in all patients; the CFL in the coronal plane, in 80% of patients; the CL, in 88%; and the talocalcaneal ligament in the sagittal plane, in 56% of the patients. The ITCL (Figure 6A) and the extensor retinaculum are visible on coronal oblique views. The CL is well visualized in all planes, with the coronal plane being the best plane to assess the ligamentous integrity. The anterior capsular ligament is a thickening of the anterior capsule of the posterior subtalar joint and is situated lateral and posterior to the ITCL.109 Patients with subtalar instability display thinner and a narrower anterior capsular ligament compared with those with lateral ankle instability199 and healthy controls.91 A thickness of ≤2.1 mm has a 66.7% sensitivity and specificity for subtalar instability, and a width of ≤7.9 mm has a sensitivity of 80% and a specificity of 76.2%.91
Figure 6.
(A) T1-weighted MRI scan with a coronal view showing rupture of interosseous talocalcaneal ligament (arrow). (B) T2-weighted fat-suppressed MRI scan with a sagittal view showing absence of the anterior capsular ligament (arrow). MRI, magnetic resonance imaging.
Absence or complete tear of the anterior capsular ligament (Figure 6B) occurs in up to 60% of patients with subtalar instability, as opposed to 13% of those with lateral ankle instability.199 The anterior capsular ligament appears to be associated with subtalar laxity,91,199 and its role in subtalar laxity requires further research. The ATFL thickness and complete ATFL tear are significantly more expressed in patients with lateral ankle instability, but Yoon et al199 noted no significant differences for complete CFL tear, ITCL thickness and width, or CFL thickness. Properties of the ITCL, the CL, or the IER are similar between patients with subtalar instability and lateral ankle instability and healthy controls.91,199 MRI seems to better detect CL (73% sensibility and 89% specificity) versus ITCL tears (44% sensibility and 60% specificity).99 Isolated CL or combined CL and ITCL are found in 7% and 26% of patients with subtalar instability, respectively.104 Research on ankle and subtalar ligament tears and structural consistency has shown heterogeneous results; no single ligament has been identified as the only cause of subtalar instability, but rather a combined involvement of these ligaments appears to be leading to subtalar instability.125
Using MRI to find CL and ITCL injuries is useful because CL and ITCL tears are associated with worst clinical outcomes (giving way and residual pain) at follow-up.176 To better assess the structural abnormalities and functional competence of ligaments on MRI scans, forced inversion should be applied to increase the sensitivity and accuracy. Seebauer et al161 used stress MRI to measure bony displacement and found increased subtalar tilt and anterior and medial talocalcaneal displacement in patients with subjective instability.
Subtalar arthrography has been used to evaluate the damage of the peripheral structures and can evidence disruption of ankle and subtalar capsule ligamentous structures.124 Subtalar arthrography is also useful in assessing patients with CLF insufficiency. It provides variable sensitivity and specificity values in identifying CLF rupture.167,168 The most commonly reported findings associated with CLF injury include leakage to the ankle, peroneal tendon sheaths, and the subcutaneous tissue; absence of the microrecess; and presence of the lateral recess.167
CT may be useful for assessing the hindfoot alignment or joint laxity during stress testing. However, the value of CT imaging is limited, as it does not allow direct visualization of the capsular ligamentous structures. Coronal tomosynthesis stress imaging provides clearer visualization of the subtalar joint compared with other cross-sectional imaging, such as CT or MRI, with lower dose of exposure to radiation and shorter examination time than those of CT.172 Quantitative dynamic CT provides a detailed analysis of subtalar motion and can assist in the evaluation of subtalar instability.53
Subtalar joint instability may also be assessed using US imaging with high correlation to the Zwipp stress radiography method.188 A fibulotrochlear angle ratio >1.6 between neutral and inversion stress on US is indicative of subtalar laxity.188 The use of US is, however, limited to the clinician’s experience and sensibility. US is probably underutilized as a diagnostic tool because of the required expertise.129
Diagnostic Arthroscopy
Ankle and hindfoot arthroscopy can have a role in the diagnosis of subtalar instability in patients in whom clinical history, physical examination, and imaging procedures are equivocal.48,195 It allows visualization of ligaments that are difficult to assess during the physical examination and imaging procedures (eg, the ITCL) and evaluates functional competence while applying stress under direct visualization.195
Subtalar Instability and Sinus Tarsi Syndrome
The underlying cause and definition of sinus tarsi syndrome is still under debate. Many patients with chronic subtalar instability may also present with sinus tarsi syndrome61,143 that can be caused by scarring of the ITCL.48 Some studies have reported an association between sinus tarsi syndrome and CL and ITCL injuries.48,99,104 Sammarco154 found that 10 in 14 patients with sinus tarsi syndrome had tears of the ITCL. Although only 1 patient demonstrated instability on preoperative stress radiographs, 7 patients evidenced subtalar instability during intraoperative measures (medial glide of the calcaneus out from under the talus). Lee et al100 found 33% partial tears of the CL and 88% partial tears of ITCL in patients with sinus tarsi syndrome. In patients presenting with chronic subtalar instability and sinus tarsi syndrome, an anesthetic injection into the sinus tarsi can alleviate symptoms and allow better identification of the location of pain.143 Subtalar arthroscopy can be used to assess subtalar joint instability, especially in patients in whom the diagnosis of a sinus tarsi syndrome is inconclusive.48,100
Treatment
The choice between nonsurgical and surgical treatment is still controversial because of the limited literature, heterogeneity in terms of the combination of ligamentous injuries, and the lack of studies focusing on the nonsurgical treatment of subtalar instability. A systematic review comparing functional treatment, plaster cast immobilization, and surgical treatment of acute ankle sprains showed that while the surgical treatment was associated with higher complication rates, longer time away from work, higher costs, and no significant clinical outcome advantages over the nonsurgical management, it resulted in improved laxity restoration, fewer recurrences, and less residual pain.89
Nonsurgical Treatment
Nonsurgical treatment of subtalar instability is similar to that of ankle instability and should be tailored to the patient’s individual deficits. The algorithm for nonsurgical treatment is based on the assessment of 4 potential deficits (ROM, strength, balance, and functional activities).45 Nonsurgical management is mostly based on the early functional rehabilitation focusing on controlling clinical symptoms and restoration of the neuromuscular deficits (eg, ankle inversion-eversion weakness, proprioceptive deficits, and peroneal muscle latency).68,194 Patients presenting with MAI are less likely to benefit from nonsurgical approaches than are those with FAI. The nonsurgical treatment of subtalar instability is similar to that of injuries of the lateral ankle ligaments, and it is based on bracing to limit supination, foot insoles, and a tailored exercise program focusing on proprioceptive training and strengthening of all ankle/hindfoot muscles, especially of the peroneal muscles, for 6 weeks in acute cases and 12 to 16 weeks in chronic cases.130
Ankle bracing has been shown to be helpful in the treatment of ankle instability and reduction of the odds for recurrent episodes,43,88 but we advise some caution when recommending bracing alone, as it can lead to decreased normalized electromyographic muscle activity (ie, motor recruitment).47 Lace-up ankle orthosis has shown better results than have semirigid ankle support, elastic bandage, and tape.88 When administered together with functional rehabilitation, taping and bracing provide mechanical support for ligament injury31 while improving proprioceptive feedback to the joint75 and, most importantly, help prevent recurrent sprains.43 Although ankle taping or bracing appears to not improve joint position sense and sense of movement in functionally unstable ankles,147 the positive outcomes on improving ankle stability should encourage its use. Athletes with FAI have shown decreased radiographic talar tilt after ankle bracing.181 The use of semirigid bracing is known to have a stabilizing effect of foot inversion in the subtalar joint.29,95 A semirigid ankle brace has been shown to limit subtalar inversion by 5° after sectioning of the CFL in a cadaveric simulated subtalar joint instability model.29 Bracing has also been shown to limit subtalar rotation by 30% in an intact ankle; by 36% when the CFL was cut; and by 34% when the CFL, the CL, and the ITCL were cut.29 A similar reduction in subtalar inversion has also been observed with bracing in subtalar unstable ankles (CFL, CL, and ITCL).82 A 1-week immobilization followed by a functional brace has shown excellent results; after 5-year follow-up, 88% of the patients with isolated ATFL injury were symptom-free, but only 30% of patients with combined ATFL and CFL injuries were asymptomatic.156
Combining a lateral subtalar sling with traditional ankle taping helps to resist subtalar inversion and supination after 2 to 3 hours of physical activity192 as well as the postexercise posteroanterior translation and inversion-eversion tilt.193 However, the semirigid brace or taping has limited effects in ankles with CAI during weightbearing ankle and subtalar internal rotation in plantarflexion.95 Moreover, although bracing is able to limit inversion of the subtalar joint, it did not restrict motion after application of internal or external rotational torques in a cadaveric model.82 This means that in more severe ankle sprains involving the CFL, the CL, and the ITCL injuries, the application of an ankle brace might be less effective in limiting internal-external rotational instability than in cases of inversion instability of the subtalar joint.82
Insoles supporting the mediolongitudinal and transverse arches reduced abnormal maximum ankle internal rotation from 3.3° to 2.3° in cadaveric simulation with ATFL and ITCL sectioning.174 This effect is likely because of improved arch configuration stability.174 When instability symptoms during walking or running do not decrease using ankle bracing, medial longitudinal arch support strategies may be considered.
A functional tailored rehabilitation program should aim to improve muscle strength and coordination and address the potential proprioceptive deficits, regardless of the use of ankle taping or bracing. Exercise therapy has been shown to improve self-reported function and prevent recurrent episodes. Functional rehabilitation strategies seem to be more effective than is immobilization in managing ankle injuries.12,90 Strategies that increase the ankle ROM, flexibility, and strength of the peripheral musculature are also effective.14,90 Improving the muscle strength and coordination of peroneal muscles provides protection against ankle inversion.3 Ankle mobilization techniques should be used to improve dorsiflexion and joint function.33,39,187 Neuromuscular and balance training helps reeducate the nerve network or improve proprioception, and it is effective in improving ankle function and reducing recurrence episodes.40,121,185
Surgical Treatment
There is considerable controversy about the optimal surgical management of subtalar laxity. Surgery should only be considered after failure of nonsurgical treatment properly administered for at least 3 to 6 months.128
Many techniques have been described for subtalar instability, including anatomic repair and reconstruction techniques, which may be augmented using tenodesis procedures. However, none of these techniques appear to restore the native contact mechanics of the ankle joint or motion patterns of the hindfoot.146 Choosing the most suitable treatment can be influenced by many factors, and making an informed decision is challenging because there are only a few high-quality controlled trials. Treatment may vary depending on the treatment of isolated subtalar laxity or when it is combined with CAI. In cases of combined instability, the reconstruction of the CFL is crucial to restore subtalar laxity.128,177 Anatomic reconstruction techniques; ligament repair using augmentation for reinforcement, either autologous (distal extensor retinaculum) or synthetic (suture tape or internal brace); or the older nonanatomic reconstruction techniques have all been well described.¶¶ The anatomic reconstruction or repair aims to restore the ankle anatomy of main subtalar stabilizers (ITCL, CFL, and CL) and recover normal arthrokinematics, and it is usually considered superior to nonanatomic reconstructions.8,130,177 In cases of isolated subtalar laxity, anatomic reconstruction techniques are recommended.
Nonanatomic Reconstruction. Nonanatomic reconstruction techniques use various configurations of grafts using the peripheral tendon to provide stability when it is not possible to repair the ligament remnants. Early reports of nonanatomic reconstruction include mostly tenodesis techniques, such as the Elmslie, Watson-Jones, Evans tenodesis, Chrisman-Snook, and Larsen techniques.86 Smith et al163 later described a modification of the Chrisman-Snook technique with a more anatomic reconstruction of the CFL. Several grafts choices and lengths can be used, and there are many pearls and pitfalls of which the surgeons must be aware during the tunnel placement to avoid injury.122
Thermann et al173 suggested the Evans tenodesis (Figure 7A) or the Chrisman-Snook (Figure 7B) procedure for isolated or combined subtalar laxity. For a single ligamentous lesion with adequate ligamentous tissue available, they recommended direct reconstruction of the ligament or, if no tissue is available, a periosteal flap repair to replace the ATFL or the CFL. For a double ligament lesion, they recommended a combination of direct and indirect reconstruction techniques or, in the absence of the ATFL and the CFL, a modified Evans tenodesis. For isolated subtalar instability, they recommended that the Chrisman-Snook procedure should be preferred. The Larsen procedure can be improved by using anchors, which make it technically easier to secure the end of the tendon to the calcaneal bone tunnel.
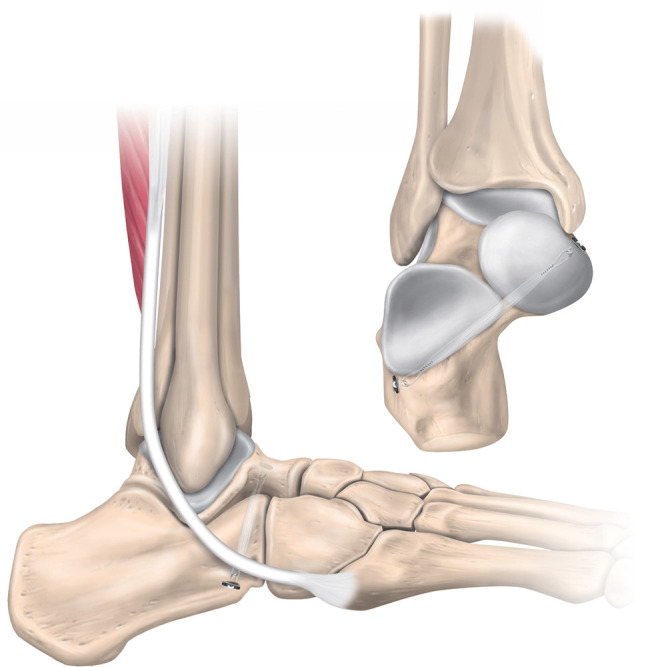
Figure 7.
(A) The nonanatomic Evans tenodesis procedure. The peroneus brevis muscle is separated, and its proximal end is sutured to the peroneus longus muscle. The peroneus brevis tendon is detached at the musculotendinous junction, but its distal insertion is preserved. A tunnel is created connecting the posterosuperior side of the fibula to the lateral malleolar tip, and the peroneus brevis tendon is routed through the tunnels from anterior to posterior and sutured on itself at the muscle belly. (B) The nonanatomic Chrisman-Snook procedure. Half of the peroneus brevis tendon is harvested proximally, but its distal attachment is preserved. A diagonal tunnel is made at the lateral malleolus, and another is made on the calcaneofibular ligament insertion at the calcaneus. The peroneus brevis graft is passed anteroposteriorly through the lateral malleolar tunnel, routed below the peroneal tendons, and then passed posteroanteriorly through the calcaneal tunnel. The graft is tensioned with the ankle in neutral flexion and rotation and sutured on itself. (C) The nonanatomic modified Elmslie procedure. Half of the peroneus brevis tendon is harvested proximally, but its distal attachment is preserved. A horizontal tunnel is made at the lateral malleolus, and another is made on the calcaneofibular ligament insertion at the calcaneus. The peroneus brevis graft is passed anteroposteriorly through the lateral malleolar tunnel, routed below the peroneal tendons, passed posteroanteriorly through the calcaneal tunnel, and then sutured on itself.
The modified Elmslie procedure (Figure 7C) preserves half of the peroneus brevis tendon and provides adequate graft for reconstruction while preserving muscle function. The peroneus longus is superficial to the peroneus brevis, is easier to dissect, and is also longer and thicker. Using a split peroneus longus tendon to reconstruct the ATFL and the CFL allows the foot to be in neutral in the sagittal plane, avoiding loss of inversion and inversion strength that is common with other techniques.166 Alternatively, by using the plantaris tendon instead of the peroneus brevis tendon, the procedure preserves proprioceptive stability function of the peroneus brevis muscle.160 Although nonanatomic reconstruction techniques reduce subtalar motion, they do not restore proper ankle biomechanics and are associated with higher risk of subtalar stiffness and secondary osteoarthritis.86
Anatomic Reconstruction. Anatomic reconstruction procedures use tendon grafts and replicate the ATFL and CFL anatomic positions, aiming to recreate normal ankle biomechanics. Techniques diverge related to graft positioning, number and angle of tunnels in the fibula, and the fixation techniques.18,32,77,113,137,189 Multiple auto- and allografts have been suggested, including semitendinosus,77,78 gracilis,18,32,64,170 Achilles,85 and plantaris tendon.113,134,135 The use of most of these grafts is appealing because the graft is easily harvested with no or low donor-site morbidity and does not compromise peroneal function.
Schon et al160 described the isolated reconstruction of the CL early in 1991 using one-half of the peroneus brevis graft through tunnels in the calcaneus and the talar neck, which is indicated for patients with mild isolated subtalar instability (Figure 8A). Schon et al160 also described the triligamentous reconstruction using a plantaris tendon (Figure 8B) or using half or the entire peroneus brevis tendon (Figure 8C), which consists of the anatomic reconstruction of the CFL, the ATFL, and the CL. The graft is weaved through tunnels at the calcaneus, the fibula, the talar neck, and floor of the tarsal canal. Variations of this technique have been suggested using different grafts, including one-half of the peroneus brevis152 and medial one-third of the Achilles tendon.165 Kato,85 Pisani,141 and Pisani et al143 described anatomic reconstruction of the ITCL using a strip of the Achilles tendon (Figure 8D) or the peroneus brevis tendon (Figure 8E).
Figure 8.
(A) Anatomic isolated reconstruction of the CL described by Schon et al.160 Half of the peroneus brevis tendon is harvested proximally, but its distal attachment is preserved. The graft is routed through the calcaneus vertical tunnel and passed through the talar neck tunnel, and then it is brought back and sutured on itself. (B) Triligamentous reconstruction using a plantaris tendon graft described by Schon et al. The graft is routed through a calcaneus (exiting at the posterior calcaneal tuberosity) and fibular tunnels, recreating the CFL and the ATFL, respectively. Then, it is passed through a tunnel at the talar neck (exiting at the floor of talar canal) and to a tunnel at the anterior and lateral calcaneus, replicating the CL. The graft is brought back by the same tunnels and secured to itself. (C) Triligamentous reconstruction, described by Schon et al, using half or the entire peroneus brevis tendon when the plantaris tendon is not available. The peroneus brevis tendon is harvested, but its distal insertion is preserved. The graft is routed through a tunnel at the anterior and lateral calcaneus (exiting at the floor of the talar canal) and then to a tunnel at the talar neck, replicating the CL. The graft is passed posteroinferiorly through a fibular tunnel, routed beneath the peroneal longus tendon then through a calcaneal tunnel (at the posterior calcaneal tuberosity), and attached to itself and the surrounding soft tissue. (D) ITCL anatomic reconstruction using a strip of the Achilles tendon described by Kato.85 The graft is passed though oblique tunnels at the calcaneus and the talar neck. The graft ends are fixed using staples. (E) ITCL anatomic reconstruction using half of the peroneus brevis tendon described by Pisani141 and Pisani et al.143 Half of the peroneus brevis is passed through the calcaneus and talar neck tunnels and then brought back through another calcaneal tunnel. The 2 tunnels aim to replicate the double-stranded ITCL. The graft end is looped and sutured on itself. ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; CL, cervical ligament; ITCL, interosseous talocalcaneal ligament.
More recent variations of ATFL and CFL reconstruction are performed arthroscopically for easily identifying the correct insertion points and for better graft positioning using suture anchors, staples, or endobuttons for graft fixation.130 Correctly identifying bony landmarks of the ATFL and the CFL is important during minimally invasive reconstruction procedures.119 As there is no difference in identifying the CFL insertion at the calcaneus between the percutaneous and the arthroscopic techniques, both techniques are suitable as reconstruction procedures.106 So et al164 proposed a standardized method for tunnel placement to reconstruct the ITCL via a suture-button fixation device (Figure 9) using a fluoroscopically guided percutaneous technique. Excessive initial graft tension of the CFL should be avoided, as it can overconstrain the graft and lead to abnormal subtalar kinematics.151
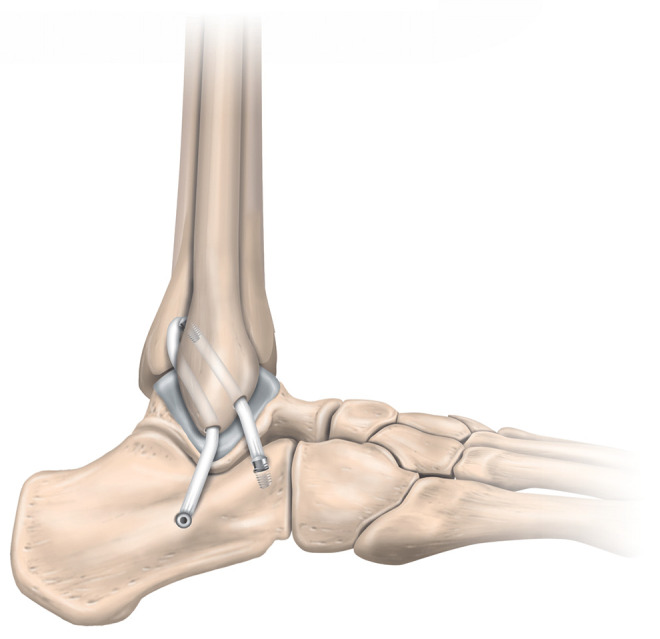
Figure 9.
Interosseous talocalcaneal ligament reconstruction using a suture-button fixation device. The tunnel placement can be safely achieved using a fluoroscopically guided percutaneous technique described by So et al.164 The graft is then fixed using a suture-button fixation device.
Several approaches have been suggested to perform anatomic reconstruction, with more recent techniques being performed arthroscopically or via the assistance of endoscopy. Lui113 described an anatomic arthroscopy-assisted reconstruction using a free plantaris tendon autograft to reconstruct the CFL as an extra-articular structure and the ATFL as a capsular structure. Coughlin et al32 reconstructed the ATFL and the CFL using a free gracilis tendon transfer combined with a direct repair of the ATFL with minimal exposure, while Michels et al126,127 described an endoscopic technique to reconstruct both the ATFL and the CFL. Wang and Xu189 recommended a minimally invasive reconstruction of the ATFL and the CFL using a semitendinosus tendon autograft, and Takao et al169 described a minimally invasive all–inside out ATFL and CFL reconstruction technique using an anatomic Y-shaped graft. These techniques can be performed arthroscopically with or without remnant preservation,44,56 with similar stiffness and load to ultimate failure.44 The arthroscopic procedure may be combined with lateral ankle endoscopy to provide a better view of the internal anatomy of the ankle.57,58 Surgeons may opt to use a percutaneous technique to identify the lateral malleolus as the cutaneous reference for the calcaneal tunnel placement of the CFL reconstruction, as it seems more reliable than does the pure arthroscopic technique. Caution is advised, as the sural nerve is at risk of injury during the procedure.112
However, the described ATFL and CFL anatomic reconstructive techniques neglect important subtalar ligaments, such as the ITCL, the CL, and the LTCL. Jung et al78 suggested a reconstruction of the anterior and posterior subtalar ligaments using a free semitendinosus allograft by which the anterior limb assumed the function of the ITCL and the CL and the posterior limb anatomically reconstructed the CFL (Figure 10). Higashiyama et al64 suggested an arthroscopic reconstruction of the ATFL, the LTCL, and the CFL using a triangle-shaped tendon graft from the gracilis tendon. This is a good salvage technique when there is an LTCL dissection during arthroscopic reconstruction of the ATFL and the CFL.
Figure 10.
Anatomic reconstruction of subtalar ligaments using a semitendinosus allograft described by Jung et al.78 The allograft is passed through 2 fibular tunnels: one from the fibular distal tip to the posterior fibula (origin of the CFL) to the midfibular axis and another from above the origin of the ATFL, obliquely directed (45°) to the midfibular axis (1 cm proximal to the previous tunnel). The graft is then fixed using a 2-cm whip stitch at the posterior calcaneus and an interference screw at the anterior calcaneus. This technique aims to replicate the anterior and posterior subtalar ligaments in which the anterior limb assumes the function of the ITCL and the CL and the posterior limb anatomically reconstructs the CFL. ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; CL, cervical ligament; ITCL, interosseous talocalcaneal ligament.
Anatomic Repair
Anatomic repair techniques aim to restore the native anatomy and normal joint mechanics via in situ repair of the injured ligaments, which includes repair by either shortening and fixing them to the bone surfaces or augmenting them using local structures.24
The primary Broström-Gould procedure is the most widely used anatomic repair technique for ankle and subtalar joint instability. Broström and Sundelin19 originally described a direct anatomic repair of the ATFL and the CFL without the use of a peroneal tendon transfer. Later, Gould et al55 modified this procedure, adding a portion of the IER connected to the fibula to augment the superficial and deep lateral ligaments. The Broström-Gould procedure (Figure 11) was designed to limit inversion in the ankle and subtalar joints in combined instability.
Figure 11.
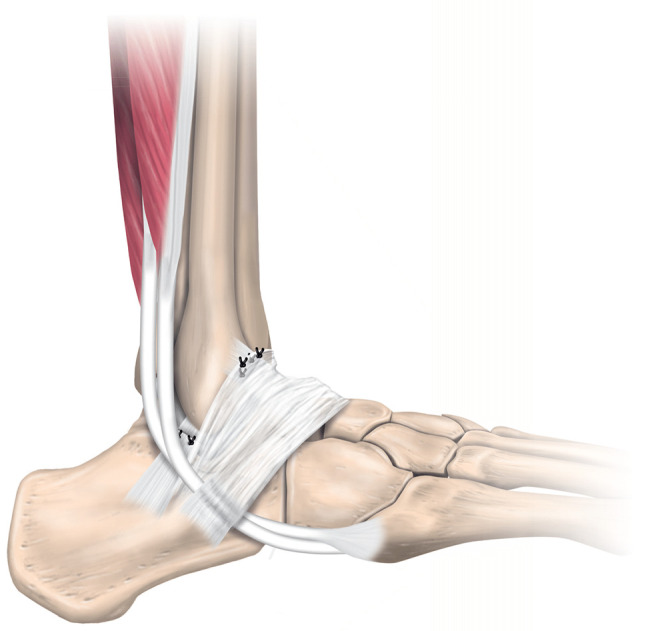
Anatomic repair using the Broström-Gould procedure. The calcaneofibular ligament and the anterior talofibular ligament rupture ends are directly repaired and reinforced using the extensor retinaculum.
The Broström procedure can be augmented using the IER,74,130,178 a peroneal split,140 or a suture tape.27,179,197 If there is poor consistency of the CFL remnants, a doubled and distally pedicled periosteal flap130 or the distal extensor retinaculum55 can be performed to augment the CFL reconstruction. By augmenting the repair using the IER, the extensor flap works as an actual neoligament, providing reinforcement, collagen input, and peripheral stabilization at the calcaneal insertion, thus reinforcing the CFL.178 The modified Broström-Gould procedure can reinforce the CL using a rectangular flap of the superior section of the IER.158 The modified Broström-Gould procedure with a semisingle ATFL reconstruction using an IER advancement provides similar stability to the reconstruction of the ATFL and the CFL.101 Some studies, nonetheless, have shown that there is no biomechanical advantage in augmenting the Broström-Gould procedure.10,74 The Broström-Gould procedure augmented using an autogenous split (one-third to one-half) of the peroneus longus free tendon graft is relatively simple and offers improved laxity restoration, preservation of the peroneus brevis tendon, preservation of a portion of the peroneus longus tendon, near anatomic reconstruction, and an aesthetic result.140 Performing the Broström repair in an open or arthroscopic fashion does not affect load to failure or stiffness,52 and thus both approaches may be used. A modified Broström-Gould technique using an allograft tenodesis decreases subtalar inversion and internal rotation, but it is unable to improve subtalar instability during neutral inversion.28 There are reports of good outcomes of ATFL isolated repair after combined ATFL and CFL injury93,101,102; however, in cases of subtalar instability, repair of both ligaments (if feasible) using an augmentation strategy (IER or synthetic) is recommended.
Outcomes
Most studies related to the surgical outcomes of subtalar instability are case series with a small number of participants, limiting the recommendations on the best treatment approach. Table 2 displays the outcomes of available studies in the past 26 years (with N ≥ 10) on the surgical treatment of subtalar instability that have at least 12 months of follow-up.
TABLE 2.
Surgical Outcomes of Stabilization Techniques for Subtalar Instability for Studies With 10 or More Patients and a Minimum 12-Month Follow-upa
| Outcomes | |||||
|---|---|---|---|---|---|
| Study (Year) | No. of Ankles | Stabilization Technique | Follow-up, mo, Mean (range) | Pain and Functional Scores | Instability and Other Outcomes |
| Smith et al163 (1995) | 18 | Modified Chrisman-Snook procedure using a more anatomic reconstruction of the CFL | 37 (24-68) | None | Talar tilt reduced from 13.7° to 2.3° |
| Kato85 (1995) | 20 | ITCL reconstruction using partial Achilles tendon graft (n = 14) or triligamentous reconstruction (n = 6) | 54 (36-84) | None | Anterior talus displacement decreased from 4.9 to 2.3 mm (ITCL reconstruction) and from 4.8 to 3.8 mm (triligamentous reconstruction) |
| Liu and Jacobson111 (1995) | 39 | Lateral shift of the entire lateral capsule-ligament complex and proximal advancement of the LTCL and IER | 55 (24-84) | 26 excellent, 8 good, 3 fair, and 2 poor results 92% were satisfied |
34 (9 of 11 college-level and 25 of 28 recreational athletes) returned to preinjury level of sports |
| Thermann et al173 (1997) | 34 | Chrisman-Snook tenodesis for isolated (n = 16) or combined subtalar instability (n = 18) | 60 | 13 excellent, 18 good, and 3 satisfactory results | Medial displacement of the calcaneus improved from 9 mm (6-14 mm) to 2 mm (0-5 mm); the talocalcaneal tilt, from 11° (6°-16°) to 3° (0°-5°) |
| Karlsson et al83 (1998) | 22 | Anatomic reconstruction in which the CL, the CFL, and the LTCL were imbricated and reinforced using the lateral root of the IER | 36 (24-60) | 15 with good to excellent results (Karlsson-Peterson instability score) | Decrease of talar tilt from 7° (4°-11°) to 4° (0°-6°) and
talocalcaneal displacement from 3 mm (2-5 mm) to 1 mm (0-3
mm) Complications: lateral branch of the superficial peroneal nerve (14%) |
| Coughlin et al32 (2004) | 29 (5 cases with subtalar instability) | Anatomic reconstruction of ATFL and CFL using free gracilis graft | 23 (12-52) | Patient satisfaction: 86% excellent and 14%
good AOFAS score improved from 57 to 98, the VAS pain improved from 7.2 to 0.6, and the postoperative Karlsson score was 95.3 6 patients reported mild pain at final follow-up |
Return to daily activities at 12 wk (5-24 wk) and to sports
at 6.5 mo (3-12 mo) 25% had residual laxity Talar tilt decreased from 13° to 3°; talar anterior translation, from 10 to 5 mm 21% reported mild swelling after exercise; 24%, morning stiffness after exercise 4 patients reported 5 recurrent injuries (3 mild sprains between 6 and 12 mo and 2 after return to sports) |
| Mabit et al; SOFCOT115 (2010) | 310 (28% had subtalar involvement) | Direct capsular ligamentous reattachment Augmented repair (periosteum, IER, and peroneus tertius) Nonanatomic reconstruction using part of the peroneus brevis (hemi-Castaing) Nonanatomic reconstruction using the whole peroneus brevis (Castaing) |
156 (60-360) | The Karlsson score with 87% good and very good
results Stability and pain subscores were satisfactory Karlsson scores were poorer using Castaing peroneus brevis plasty (compared with direct capsular ligamentous reattachment) because of the pain and residual instability |
Complications: neurologic lesions (9%), infection (5%),
hematoma (3%), reflex sympathetic dystrophy (3%), and DVT
(1%) Osteoarthritis (grades 2 and 3) was present in 3% of patients, and 92% were satisfied |
| Jung et al78 (2015) | 20 | Anatomic reconstruction of the ATFL and the CFL using semitendinosus allograft with biotenodesis screws | 15 (all >12) | The VAS pain score improved from 6 to 2; the AOFAS hindfoot
score, from 66 to 90; and the Karlsson-Peterson instability
score, from 57 to 91 100% were satisfied |
Patients resumed work in 2.6 ± 1.1 mo The subtalar tilt angle decreased from 11.5° ± 2.7° to 3° |
aAOFAS, American Orthopaedic Foot & Ankle Society; ATFL, anterior talofibular ligament; CFL, calcaneofibular ligament; CL, cervical ligament; DVT, deep venous thrombosis; IER, inferior extensor retinaculum; ITCL, interosseous talocalcaneal ligament; LTCL, lateral talocalcaneal ligament; SOFCOT, Societe Francaise d’Orthopedie-Traumatologie; VAS, visual analog scale.
Subtalar Dislocations
Subtalar dislocation (Figure 12) is rare, but it is the most serious condition leading to subtalar laxity and functional instability. Medial dislocation is the most common (80%-85% of the cases)69 and involves rupture of all the lateral subtalar ligaments (CFL, ITCL, and CL) because of an inversion force. The foot is in plantarflexion and inversion, which are combined with external rotation of the talus. The CL tears first, the ITCL tears second (from anterior to posterior), and thereafter the anterior and posterior talocalcaneal joints dislocate.117
Figure 12.
(A) The lateral view and (B) the anteroposterior view radiographs of a patient with subtalar dislocation.
Management starts with an immediate closed reduction. This should be performed as soon as possible to prevent further damage to the skin and neurovascular structures.13,51 Open reduction is performed by flexing the knee to relax the gastrocnemius muscle, with constant countertraction maneuvers to accentuate the deformity. Thereafter, longitudinal traction and force is applied in the opposite direction of the dislocation to reverse the deformity.69,153 When the closed reduction fails, open reduction is indicated as soon as possible,5 but it should be taken into account that an open reduction results in poorer clinical outcomes.196 Management after reduction consists of immobilization and full weightbearing in a walker boot or a walking cast for 4 to 6 weeks.5 However, some surgeons suggest avoiding weightbearing during immobilization.79,123 After immobilization, the patients should start physiotherapy treatment to improve strength, ROM, and proprioception.5
Chronic subtalar instability may occur after the subtalar dislocation in up to 55% of the patients.201 The risk of developing functional instability is associated with younger age and shorter time of immobilization, and thus immobilization should be maintained for at least 6 weeks in young and active patients.145 Progression to posttraumatic subtalar arthritis is common in these patients, and isolated subtalar arthrodesis can achieve good results as long as the anatomy and alignment were well maintained.116
Authors’ Preferred Diagnosis and Treatment Procedures
In our clinical practice, we establish the diagnosis of subtalar instability via clinical history; physical examination; and when required, imaging procedures. After suspicion of subtalar ligament injury (clinical history, signs, and symptoms), we proceed with manual testing of joint laxity (anterolateral drawer and talar tilt tests). If symptoms (pain and subjective instability) are combined with pathological laxity, we refer the patient for an imaging assessment. We use manual stress radiography to objectively measure the talar tilt, and we use MRI to assess the structural integrity of the subtalar ligaments. In patients with equivocal findings and persistent pain and instability symptoms, we occasionally perform a diagnostic arthroscopy to directly visualize the subtalar ligaments and search for other potential causes of symptoms.
We perform surgery as the first-line treatment in patients presenting with catching and/or locking of the joint with a bony fragment or extensive articular cartilage damage. For all other patients with subtalar instability, we manage them using 6 months of nonoperative treatment protocol aiming to restore ROM, neuromuscular deficits (strength, muscle activation, flexibility, and balance/proprioception), and functional/sports ability. In patients participating regularly in sports, we augment the rehabilitation strategy using short-term ankle bracing (either taping or lace-up brace). If we find foot posture deficits, we refer the patient to a podiatrist for foot insoles. When symptoms and/or functional deficits do not resolve after the 6-month nonoperative strategy, we opt for surgical treatment. We prefer the anatomic augmented repair using a synthetic ligament or a gracilis tendon autograft. In patients with subtalar dislocation, we perform an immediate closed reduction (or open if closed reduction fails), which is followed by 4 to 6 weeks of immobilization and full weightbearing in a walker boot. After the immobilization period, the patient follows the traditional rehabilitation protocol as described for subtalar instability.
Conclusion
The precise cause of functional subtalar instability remains a topic of debate, but the recognition of subtalar instability or laxity as a distinct clinical entity in recent years reflects an improved understanding of the ankle joint complex in both healthy and injured states. Identifying those patients with CAI who also display subtalar instability is the cornerstone for treatment choice. Clinical symptoms largely overlap with those of lateral ankle instability, making diagnosing subtalar instability or laxity a challenge. Some manual tests (eg, the anterolateral drawer test) have been proposed to identify subtalar instability with higher sensitivity. MRI is a useful tool to identify injury of the subtalar ligaments. Surgeons should look for spring ligament injury, as it can contribute to rotatory laxity. Stress MRI can have an important role in correlating the capsuloligamentous structural integrity with the functional competence of the subtalar ligaments.
Nonsurgical approaches are always the first line of treatment. If these fail for 6 months, surgical treatment should be considered, including reconstructive and repair procedures. Surgical treatment choice can be guided based on whether there is isolated or combined instability or laxity. The CFL and the ITCL have a clear role in subtalar stability, and these should be adressed in treatment protocols. Making an informed decision is still challenging because most studies are case series and there are only a few high-quality controlled trials. Future research should focus on finer diagnostic tools to better identify the cause of subtalar instability or laxity and to differentiate subtalar from combined ankle instability and laxity. High-quality and adequately powered randomized clinical trials are warranted to investigate the superiority of anatomic reconstruction or repair techniques.
Acknowledgment
The authors thank Pontus Andersson for his exceptional work in producing the illustrations.
Footnotes
Final revision submitted January 8, 2021; accepted February 23, 2021.
The authors declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1.Agarwal S, Garg S, Vasudeva N. Subtalar joint instability and calcaneal spurs associated with the configuration of the articular facets of adult human calcaneum in Indian population. J Clin Diagn Res. 2016;10(9):AC05–AC09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al-Mohrej OA, Al-Kenani NS. Chronic ankle instability: current perspectives. Avicenna J Med. 2016;6(4):103–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ashton-Miller JA, Ottaviani RA, Hutchinson C, Wojtys EM. What best protects the inverted weight-bearing ankle against further inversion? Evertor muscle strength compares favorably with shoe height, athletic tape, and 3 orthoses. Am J Sports Med. 1996;24(6):800–809. [DOI] [PubMed] [Google Scholar]
- 4.Attarian DE, McCrackin HJ, DeVito DP, McElhaney JH, Garrett WE, Jr. Biomechanical characteristics of human ankle ligaments. Foot Ankle. 1985;6(2):54–58. [DOI] [PubMed] [Google Scholar]
- 5.Aynardi M, Pedowitz DI, Raikin SM. Subtalar instability. Foot Ankle Clin. 2015;20(2):243–252. [DOI] [PubMed] [Google Scholar]
- 6.Bahr R, Pena F, Shine J, Lew WD, Tyrdal S, Engebretsen L. Biomechanics of ankle ligament reconstruction: an in vitro comparison of the Broström repair, Watson-Jones reconstruction, and a new anatomic reconstruction technique. Am J Sports Med. 1997;25(4):424–432. [DOI] [PubMed] [Google Scholar]
- 7.Barbaix E, Van Roy P, Clarys JP. Variations of anatomical elements contributing to subtalar joint stability: intrinsic risk factors for posttraumatic lateral instability of the ankle? Ergonomics. 2000;43(10):1718–1725. [DOI] [PubMed] [Google Scholar]
- 8.Barg A, Tochigi Y, Amendola A, Phisitkul P, Hintermann B, Saltzman CL. Subtalar instability: diagnosis and treatment. Foot Ankle Int. 2012;33(2):151–160. [DOI] [PubMed] [Google Scholar]
- 9.Bartoníček J, Rammelt S, Naňka O. Anatomy of the subtalar joint. Foot Ankle Clin. 2018;23(3):315–340. [DOI] [PubMed] [Google Scholar]
- 10.Behrens SB, Drakos M, Lee BJ, et al. Biomechanical analysis of Broström versus Broström-Gould lateral ankle instability repairs. Foot Ankle Int. 2013;34(4):587–592. [DOI] [PubMed] [Google Scholar]
- 11.Beimers L, Tuijthof GJ, Blankevoort L, Jonges R, Maas M, van Dijk CN. In vivo range of motion of the subtalar joint using computed tomography. J Biomech. 2008;41(7):1390–1397. [DOI] [PubMed] [Google Scholar]
- 12.Beynnon BD, Renstrom PA, Haugh L, Uh BS, Barker H. A prospective, randomized clinical investigation of the treatment of first-time ankle sprains. Am J Sports Med. 2006;34(9):1401–1412. [DOI] [PubMed] [Google Scholar]
- 13.Bibbo C, Anderson RB, Davis WH. Injury characteristics and the clinical outcome of subtalar dislocations: a clinical and radiographic analysis of 25 cases. Foot Ankle Int. 2003;24(2):158–163. [DOI] [PubMed] [Google Scholar]
- 14.Bleakley CM, O’Connor SR, Tully MA, et al. Effect of accelerated rehabilitation on function after ankle sprain: randomised controlled trial. BMJ. 2010;340:C1964. [DOI] [PubMed] [Google Scholar]
- 15.Boey H, Verfaillie S, Natsakis T, Vander Sloten J, Jonkers I. Augmented ligament reconstruction partially restores hindfoot and midfoot kinematics after lateral ligament ruptures. Am J Sports Med. 2019;47(8):1921–1930. [DOI] [PubMed] [Google Scholar]
- 16.Bonnel F, Toullec E, Mabit C, Tourne Y. Chronic ankle instability: biomechanics and pathomechanics of ligaments injury and associated lesions. Orthop Traumatol Surg Res. 2010;96(4):424–432. [DOI] [PubMed] [Google Scholar]
- 17.Bosien WR, Staples OS, Russell SW. Residual disability following acute ankle sprains. J Bone Joint Surg Am. 1955;37-A(6):1237–1243. [PubMed] [Google Scholar]
- 18.Boyer DS, Younger AS. Anatomic reconstruction of the lateral ligament complex of the ankle using a gracilis autograft. Foot Ankle Clin. 2006;11(3):585–595. [DOI] [PubMed] [Google Scholar]
- 19.Broström L, Sundelin P. Sprained ankles, IV: histologic changes in recent and “chronic” ligament ruptures. Acta Chir Scand. 1966;132(3):248–253. [PubMed] [Google Scholar]
- 20.Brown C, Ross S, Mynark R, Guskiewicz K. Assessing functional ankle instability with joint position sense, time to stabilization, and electromyography. J Sport Rehabil. 2004;13(2):122–134. [Google Scholar]
- 21.Brown CN, Bowser B, Orellana A. Dynamic postural stability in females with chronic ankle instability. Med Sci Sports Exerc. 2010;42(12):2258–2263. [DOI] [PubMed] [Google Scholar]
- 22.Budny A. Subtalar joint instability: current clinical concepts. Clin Podiatr Med Surg. 2004;21(3):449–460, viii. [DOI] [PubMed] [Google Scholar]
- 23.Cahill DR. The anatomy and function of the contents of the human tarsal sinus and canal. Anat Rec (Hoboken). 1965;153(1):1–17. [DOI] [PubMed] [Google Scholar]
- 24.Cao Y, Hong Y, Xu Y, Zhu Y, Xu X. Surgical management of chronic lateral ankle instability: a meta-analysis. J Orthop Surg Res. 2018;13(1):159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cass JR, Settles H. Ankle instability: in vitro kinematics in response to axial load. Foot Ankle Int. 1994;15(3):134–140. [DOI] [PubMed] [Google Scholar]
- 26.van Dijk CN. Diagnosis of ankle sprain: history and physical examination. In: Chan KM, Karlsson J, eds. International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine—International Federation of Sports Medicine (ISAKOS–FIMS). World Consensus Conference on Ankle Instability; 2005. [Google Scholar]
- 27.Cho BK, Park JK, Choi SM, SooHoo NF. A randomized comparison between lateral ligaments augmentation using suture-tape and modified Broström repair in young female patients with chronic ankle instability. Foot Ankle Surg. 2019;25(2):137–142. [DOI] [PubMed] [Google Scholar]
- 28.Choisne J, Hoch MC, Alexander I, Ringleb SI. Effect of direct ligament repair and tenodesis reconstruction on simulated subtalar joint instability. Foot Ankle Int. 2017;38(3):324–330. [DOI] [PubMed] [Google Scholar]
- 29.Choisne J, Hoch MC, Bawab S, Alexander I, Ringleb SI. The effects of a semi-rigid ankle brace on a simulated isolated subtalar joint instability. J Orthop Res. 2013;31(12):1869–1875. [DOI] [PubMed] [Google Scholar]
- 30.Choisne J, Ringleb SI, Samaan MA, Bawab SY, Naik D, Anderson CD. Influence of kinematic analysis methods on detecting ankle and subtalar joint instability. J Biomech. 2012;45(1):46–52. [DOI] [PubMed] [Google Scholar]
- 31.Cordova ML, Ingersoll CD, Palmieri RM. Efficacy of prophylactic ankle support: an experimental perspective. J Athl Train. 2002;37(4):446–457. [PMC free article] [PubMed] [Google Scholar]
- 32.Coughlin MJ, Schenck RC, Jr, Grebing BR, Treme G. Comprehensive reconstruction of the lateral ankle for chronic instability using a free gracilis graft. Foot Ankle Int. 2004;25(4):231–241. [DOI] [PubMed] [Google Scholar]
- 33.Cruz-Diaz D, Lomas Vega R, Osuna-Perez MC, Hita-Contreras F, Martinez-Amat A. Effects of joint mobilization on chronic ankle instability: a randomized controlled trial. Disabil Rehabil. 2015;37(7):601–610. [DOI] [PubMed] [Google Scholar]
- 34.Davis WH, Sobel M, DiCarlo EF, et al. Gross, histological, and microvascular anatomy and biomechanical testing of the spring ligament complex. Foot Ankle Int. 1996;17(2):95–102. [DOI] [PubMed] [Google Scholar]
- 35.de Asla RJ, Kozanek M, Wan L, Rubash HE, Li G. Function of anterior talofibular and calcaneofibular ligaments during in vivo motion of the ankle joint complex. J Orthop Surg Res. 2009;4:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.de Asla RJ, Wan L, Rubash HE, Li G. Six DOF in vivo kinematics of the ankle joint complex: application of a combined dual-orthogonal fluoroscopic and magnetic resonance imaging technique. J Orthop Res. 2006;24(5):1019–1027. [DOI] [PubMed] [Google Scholar]
- 37.Debieux P, Wajnsztejn A, Mansur NSB. Epidemiology of injuries due to ankle sprain diagnosed in an orthopedic emergency room. Einstein (Sao Paulo). 2020;18: eAO4739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Delahunt E, Monaghan K, Caulfield B. Ankle function during hopping in subjects with functional instability of the ankle joint. Scand J Med Sci Sports. 2007;17(6):641–648. [DOI] [PubMed] [Google Scholar]
- 39.Denegar CR, Hertel J, Fonseca J. The effect of lateral ankle sprain on dorsiflexion range of motion, posterior talar glide, and joint laxity. J Orthop Sports Phys Ther. 2002;32(4):166–173. [DOI] [PubMed] [Google Scholar]
- 40.de Vries JS, Krips R, Sierevelt IN, Blankevoort L, Van Dijk C. Interventions for treating chronic ankle instability. Cochrane Database Syst Rev. 2011;10(8):CD004124. [DOI] [PubMed] [Google Scholar]
- 41.D’Hooghe P, Pereira H, Kelley J, et al. The CFL fails before the ATFL immediately after combined ligament repair in a biomechanical cadaveric model. Knee Surg Sports Traumatol Arthrosc. 2020;28(1):253–261. [DOI] [PubMed] [Google Scholar]
- 42.Docherty CL, Moore JH, Arnold BL. Effects of strength training on strength development and joint position sense in functionally unstable ankles. J Athl Train. 1998;33(4):310–314. [PMC free article] [PubMed] [Google Scholar]
- 43.Doherty C, Bleakley C, Delahunt E, Holden S. Treatment and prevention of acute and recurrent ankle sprain: an overview of systematic reviews with meta-analysis. Br J Sports Med. 2017;51(2):113–125. [DOI] [PubMed] [Google Scholar]
- 44.Dong P, Gu S, Jiang Y, et al. All arthroscopic remnant-preserving reconstruction of the lateral ligaments of the ankle: a biomechanical study and clinical application. Biochem Biophys Res Commun. 2018;505(4):985–990. [DOI] [PubMed] [Google Scholar]
- 45.Donovan L, Hertel J. A new paradigm for rehabilitation of patients with chronic ankle instability. Phys Sportsmed. 2012;40(4):41–51. [DOI] [PubMed] [Google Scholar]
- 46.Fallat L, Grimm DJ, Saracco JA. Sprained ankle syndrome: prevalence and analysis of 639 acute injuries. J Foot Ankle Surg. 1998;37(4):280–285. [DOI] [PubMed] [Google Scholar]
- 47.Feger MA, Donovan L, Hart JM, Hertel J. Effect of ankle braces on lower extremity muscle activation during functional exercises in participants with chronic ankle instability. Int J Sports Phys Ther. 2014;9(4):476–487. [PMC free article] [PubMed] [Google Scholar]
- 48.Frey C, Feder KS, DiGiovanni C. Arthroscopic evaluation of the subtalar joint: does sinus tarsi syndrome exist? Foot Ankle Int. 1999;20(3):185–191. [DOI] [PubMed] [Google Scholar]
- 49.Fu AS, Hui-Chan CW. Ankle joint proprioception and postural control in basketball players with bilateral ankle sprains. Am J Sports Med. 2005;33(8):1174–1182. [DOI] [PubMed] [Google Scholar]
- 50.Fujii T, Luo ZP, Kitaoka HB, An KN. The manual stress test may not be sufficient to differentiate ankle ligament injuries. Clin Biomech (Bristol, Avon). 2000;15(8):619–623. [DOI] [PubMed] [Google Scholar]
- 51.Garofalo R, Moretti B, Ortolano V, et al. Peritalar dislocations: a retrospective study of 18 cases. J Foot Ankle Surg. 2004;43(3):166–172. [DOI] [PubMed] [Google Scholar]
- 52.Giza E, Shin EC, Wong SE, et al. Arthroscopic suture anchor repair of the lateral ligament ankle complex: a cadaveric study. Am J Sports Med. 2013;41(11):2567–2572. [DOI] [PubMed] [Google Scholar]
- 53.Gondim Teixeira PA, Formery AS, Jacquot A, et al. Quantitative analysis of subtalar joint motion with 4D CT: proof of concept with cadaveric and healthy subject evaluation. AJR Am J Roentgenol. 2017;208(1):150–158. [DOI] [PubMed] [Google Scholar]
- 54.Goto A, Moritomo H, Itohara T, Watanabe T, Sugamoto K. Three-dimensional in vivo kinematics of the subtalar joint during dorsi-plantarflexion and inversion-eversion. Foot Ankle Int. 2009;30(5):432–438. [DOI] [PubMed] [Google Scholar]
- 55.Gould N, Seligson D, Gassman J. Early and late repair of lateral ligament of the ankle. Foot Ankle. 1980;1(2):84–89. [DOI] [PubMed] [Google Scholar]
- 56.Gui J, Jiang Y, Li Y, et al. All arthroscopic remnant-preserving technique to reconstruct the lateral ankle ligament complex. Arthrosc Tech. 2017;6(3):e549–e557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Guillo S, Archbold P, Perera A, Bauer T, Sonnery-Cottet B. Arthroscopic anatomic reconstruction of the lateral ligaments of the ankle with gracilis autograft. Arthrosc Tech. 2014;3(5):e593–e598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Guillo S, Cordier G, Sonnery-Cottet B, Bauer T. Anatomical reconstruction of the anterior talofibular and calcaneofibular ligaments with an all-arthroscopic surgical technique. Orthop Traumatol Surg Res. 2014;100(8)(suppl):S413–S417. [DOI] [PubMed] [Google Scholar]
- 59.Hagen M, Lemke M, Lahner M. Deficits in subtalar pronation and supination proprioception in subjects with chronic ankle instability. Hum Mov Sci. 2018;57:324–331. [DOI] [PubMed] [Google Scholar]
- 60.Heilman AE, Braly WG, Bishop JO, Noble PC, Tullos HS. An anatomic study of subtalar instability. Foot Ankle. 1990;10(4):224–228. [DOI] [PubMed] [Google Scholar]
- 61.Helgeson K. Examination and intervention for sinus tarsi syndrome. N Am J Sports Phys Ther. 2009;4(1):29–37. [PMC free article] [PubMed] [Google Scholar]
- 62.Hertel J, Braham RA, Hale SA, Olmsted-Kramer LC. Simplifying the star excursion balance test: analyses of subjects with and without chronic ankle instability. J Orthop Sports Phys Ther. 2006;36(3):131–137. [DOI] [PubMed] [Google Scholar]
- 63.Hertel J, Denegar CR, Monroe MM, Stokes WL. Talocrural and subtalar joint instability after lateral ankle sprain. Med Sci Sports Exerc. 1999;31(11):1501–1508. [DOI] [PubMed] [Google Scholar]
- 64.Higashiyama R, Sekiguchi H, Takata K, Endo T, Takaso M. Arthroscopic reconstruction of the anterior talofibular ligament, lateral talocalcaneal ligament, and calcaneofibular ligament using a triangle-shaped tendon graft (ALC-triangle). Arthrosc Tech. 2020;9(2):e217–e223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hiller CE, Kilbreath SL, Refshauge KM. Chronic ankle instability: evolution of the model. J Athl Train. 2011;46(2):133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Hintermann B. Medial ankle instability. Foot Ankle Clin. 2003;8(4):723–738. [DOI] [PubMed] [Google Scholar]
- 67.Holmer P, Sondergaard L, Konradsen L, Nielsen PT, Jorgensen LN. Epidemiology of sprains in the lateral ankle and foot. Foot Ankle Int. 1994;15(2):72–74. [DOI] [PubMed] [Google Scholar]
- 68.Hopkins JT, Brown TN, Christensen L, Palmieri-Smith RM. Deficits in peroneal latency and electromechanical delay in patients with functional ankle instability. J Orthop Res. 2009;27(12):1541–1546. [DOI] [PubMed] [Google Scholar]
- 69.Horning J, DiPreta J. Subtalar dislocation. Orthopedics. 2009;32(12):904. [DOI] [PubMed] [Google Scholar]
- 70.Hubbard TJ, Cordova M. Mechanical instability after an acute lateral ankle sprain. Arch Phys Med Rehabil. 2009;90(7):1142–1146. [DOI] [PubMed] [Google Scholar]
- 71.Hubbard TJ, Hertel J. Mechanical contributions to chronic lateral ankle instability. Sports Med. 2006;36(3):263–277. [DOI] [PubMed] [Google Scholar]
- 72.Hubbard TJ, Kaminski TW, Vander Griend RA, Kovaleski JE. Quantitative assessment of mechanical laxity in the functionally unstable ankle. Med Sci Sports Exerc. 2004;36(5):760–766. [DOI] [PubMed] [Google Scholar]
- 73.Hunt KJ, Pereira H, Kelley J, et al. The role of calcaneofibular ligament injury in ankle instability: implications for surgical management. Am J Sports Med. 2019;47(2):431–437. [DOI] [PubMed] [Google Scholar]
- 74.Jeong BO, Kim MS, Song WJ, SooHoo NF. Feasibility and outcome of inferior extensor retinaculum reinforcement in modified Broström procedures. Foot Ankle Int. 2014;35(11):1137–1142. [DOI] [PubMed] [Google Scholar]
- 75.Jerosch J, Hoffstetter I, Bork H, Bischof M. The influence of orthoses on the proprioception of the ankle joint. Knee Surg Sports Traumatol Arthrosc. 1995;3(1):39–46. [DOI] [PubMed] [Google Scholar]
- 76.Jotoku T, Kinoshita M, Okuda R, Abe M. Anatomy of ligamentous structures in the tarsal sinus and canal. Foot Ankle Int. 2006;27(7):533–538. [DOI] [PubMed] [Google Scholar]
- 77.Jung HG, Kim TH. Subtalar instability reconstruction with an allograft: technical note. Foot Ankle Int. 2012;33(8):682–685. [DOI] [PubMed] [Google Scholar]
- 78.Jung H-G, Park J-T, Shin M-H, Lee S-H, Eom J-S, Lee D-O. Outcome of subtalar instability reconstruction using the semitendinosus allograft tendon and biotenodesis screws. Knee Surg Sports Traumatol Arthrosc. 2015;23(8):2376–2383. [DOI] [PubMed] [Google Scholar]
- 79.Jungbluth P, Wild M, Hakimi M, et al. Isolated subtalar dislocation. J Bone Joint Surg Am. 2010;92(4):890–894. [DOI] [PubMed] [Google Scholar]
- 80.Kamada K, Watanabe S, Yamamoto H. Chronic subtalar instability due to insufficiency of the calcaneofibular ligament: a case report. Foot Ankle Int. 2002;23(12):1135–1137. [DOI] [PubMed] [Google Scholar]
- 81.Kaminski TW, Buckley BD, Powers ME, Hubbard TJ, Ortiz C. Effect of strength and proprioception training on eversion to inversion strength ratios in subjects with unilateral functional ankle instability. Br J Sports Med. 2003;37(5):410–415 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Kamiya T, Kura H, Suzuki D, Uchiyama E, Fujimiya M, Yamashita T. Mechanical stability of the subtalar joint after lateral ligament sectioning and ankle brace application: a biomechanical experimental study. Am J Sports Med. 2009;37(12):2451–2458. [DOI] [PubMed] [Google Scholar]
- 83.Karlsson J, Eriksson BI, Renström P. Subtalar instability of the foot: a review and results after surgical treatment. Scand J Med Sci Sports. 1998;8(4):191–197. [DOI] [PubMed] [Google Scholar]
- 84.Karlsson J, Eriksson BI, Renström PA. Subtalar ankle instability: a review. Sports Med. 1997;24(5):337–346. [DOI] [PubMed] [Google Scholar]
- 85.Kato T. The diagnosis and treatment of instability of the subtalar joint. J Bone Joint Surg Br. 1995;77(3):400–406. [PubMed] [Google Scholar]
- 86.Keefe DT, Haddad SL. Subtalar instability: etiology, diagnosis, and management. Foot Ankle Clin. 2002;7(3):577–609. [DOI] [PubMed] [Google Scholar]
- 87.Kelikian AS, Sarrafian SK. Sarrafian’s Anatomy of the Foot and Ankle: Descriptive, Topographic, Functional. Lippincott Williams & Wilkins; 2011. [Google Scholar]
- 88.Kerkhoffs G, Struijs P, Marti R, Assendelft W, Blankevoort L, van Dijk C. Different functional treatment strategies for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 2002;3:CD002938. [DOI] [PubMed] [Google Scholar]
- 89.Kerkhoffs GM, Handoll HH, de Bie R, Rowe BH, Struijs PA. Surgical versus conservative treatment for acute injuries of the lateral ligament complex of the ankle in adults. Cochrane Database Syst Rev. 2007;18(2):CD000380. [DOI] [PubMed] [Google Scholar]
- 90.Kerkhoffs GM, Rowe BH, Assendelft WJ, Kelly KD, Struijs PA, Van Dijk C. Immobilisation and functional treatment for acute lateral ankle ligament injuries in adults. Cochrane Database Syst Rev. 2002;3:CD003762. [DOI] [PubMed] [Google Scholar]
- 91.Kim TH, Moon SG, Jung HG, Kim NR. Subtalar instability: imaging features of subtalar ligaments on 3D isotropic ankle MRI. BMC Musculoskelet Disord. 2017;18(1):475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Knudson GA, Kitaoka HB, Lu CL, Luo ZP, An KN. Subtalar joint stability: talocalcaneal interosseous ligament function studied in cadaver specimens. Acta Orthop Scand. 1997;68(5):442–446. [DOI] [PubMed] [Google Scholar]
- 93.Ko KR, Lee WY, Lee H, Park HS, Sung KS. Repair of only anterior talofibular ligament resulted in similar outcomes to those of repair of both anterior talofibular and calcaneofibular ligaments. Knee Surg Sports Traumatol Arthrosc. 2020;28(1):155–162. [DOI] [PubMed] [Google Scholar]
- 94.Kobayashi T, No Y, Yoneta K, Sadakiyo M, Gamada K. In vivo kinematics of the talocrural and subtalar joints with functional ankle instability during weight-bearing ankle internal rotation: a pilot study. Foot Ankle Spec. 2013;6(3):178–184. [DOI] [PubMed] [Google Scholar]
- 95.Kobayashi T, Saka M, Suzuki E, et al. The effects of a semi-rigid brace or taping on talocrural and subtalar kinematics in chronic ankle instability. Foot Ankle Spec. 2014;7(6):471–477. [DOI] [PubMed] [Google Scholar]
- 96.Krahenbuhl N, Weinberg MW, Davidson NP, et al. Currently used imaging options cannot accurately predict subtalar joint instability. Knee Surg Sports Traumatol Arthrosc. 2019;27(9):2818–2830. [DOI] [PubMed] [Google Scholar]
- 97.Larsen E. Tendon transfer for lateral ankle and subtalar joint instability. Acta Orthop Scand. 1988;59(2):168–172. [PubMed] [Google Scholar]
- 98.Lee BH, Choi KH, Seo DY, Choi SM, Kim GL. Diagnostic validity of alternative manual stress radiographic technique detecting subtalar instability with concomitant ankle instability. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1029–1039. [DOI] [PubMed] [Google Scholar]
- 99.Lee KB, Bai LB, Park JG, Song EK, Lee JJ. Efficacy of MRI versus arthroscopy for evaluation of sinus tarsi syndrome. Foot Ankle Int. 2008;29(11):1111–1116. [DOI] [PubMed] [Google Scholar]
- 100.Lee KB, Bai LB, Song EK, Jung ST, Kong IK. Subtalar arthroscopy for sinus tarsi syndrome: arthroscopic findings and clinical outcomes of 33 consecutive cases. Arthroscopy. 2008;24(10):1130–1134. [DOI] [PubMed] [Google Scholar]
- 101.Lee KT, Lee JI, Sung KS, et al. Biomechanical evaluation against calcaneofibular ligament repair in the Broström procedure: a cadaveric study. Knee Surg Sports Traumatol Arthrosc. 2008;16(8):781–786. [DOI] [PubMed] [Google Scholar]
- 102.Lee KT, Park YU, Kim JS, Kim JB, Kim KC, Kang SK. Long-term results after modified Broström procedure without calcaneofibular ligament reconstruction. Foot Ankle Int. 2011;32(2):153–157. [DOI] [PubMed] [Google Scholar]
- 103.Lee MS, Hofbauer MH. Evaluation and management of lateral ankle injuries. Clin Podiatr Med Surg. 1999;16(4):659–678. [PubMed] [Google Scholar]
- 104.Lektrakul N, Chung CB, Lai Y, et al. Tarsal sinus: arthrographic, MR imaging, MR arthrographic, and pathologic findings in cadavers and retrospective study data in patients with sinus tarsi syndrome. Radiology. 2001;219(3):802–810. [DOI] [PubMed] [Google Scholar]
- 105.Leonard MH. Injuries of the lateral ligaments of the ankle: a clinical and experimental study. J Bone Joint Surg Am. 1949;31A(2):373–377. [PubMed] [Google Scholar]
- 106.Li HY, Li SK, Zhou R, Chen SY, Hua YH. No difference between percutaneous and arthroscopic techniques in identifying the calcaneal insertion during ankle lateral ligament reconstruction: a cadaveric study. Biomed Res Int. 2019;2019:2128960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Li SY, Hou ZD, Zhang P, Li HL, Ding ZH, Liu YJ. Ligament structures in the tarsal sinus and canal. Foot Ankle Int. 2013;34(12):1729–1736. [DOI] [PubMed] [Google Scholar]
- 108.Li X, Killie H, Guerrero P, Busconi BD. Anatomical reconstruction for chronic lateral ankle instability in the high-demand athlete: functional outcomes after the modified Broström repair using suture anchors. Am J Sports Med. 2009;37(3):488–494. [DOI] [PubMed] [Google Scholar]
- 109.Linklater J, Hayter CL, Vu D, Tse K. Anatomy of the subtalar joint and imaging of talocalcaneal coalition. Skeletal Radiol. 2009;38(5):437–449. [DOI] [PubMed] [Google Scholar]
- 110.Liu C, Jiao C, Hu Y, Guo QW, Wand C, Ao Y. Interosseous talocalcaneal ligament reconstruction with hamstring autograft under subtalar arthroscopy: case report. Foot Ankle Int. 2011;32(11):1089–1094. [DOI] [PubMed] [Google Scholar]
- 111.Liu SH, Jacobson KE. A new operation for chronic lateral ankle instability. J Bone Joint Surg Br. 1995;77(1):55–59. [PubMed] [Google Scholar]
- 112.Lopes R, Noailles T, Brulefert K, Geffroy L, Decante C. Anatomic validation of the lateral malleolus as a cutaneous marker for the distal insertion of the calcaneofibular ligament. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):869–874. [DOI] [PubMed] [Google Scholar]
- 113.Lui TH. Arthroscopic-assisted lateral ligamentous reconstruction in combined ankle and subtalar instability. Arthroscopy. 2007;23(5):554.e551-555. [DOI] [PubMed] [Google Scholar]
- 114.Mabit C, Boncoeur-Martel MP, Chaudruc JM, Valleix D, Descottes B, Caix M. Anatomic and MRI study of the subtalar ligamentous support. Surg Radiol Anat. 1997;19(2):111–117. [DOI] [PubMed] [Google Scholar]
- 115.Mabit C, Tourne Y, Besse JL, et al. ; Sofcot. Chronic lateral ankle instability surgical repairs: the long-term prospective. Orthop Traumatol Surg Res. 2010;96(4):417–423. [DOI] [PubMed] [Google Scholar]
- 116.Mann RA, Beaman DN, Horton GA. Isolated subtalar arthrodesis. Foot Ankle Int. 1998;19(8):511–519. [DOI] [PubMed] [Google Scholar]
- 117.Marotte JH, Samuel P, Moati JC, Lord G, Bombart M. [Subtalar dislocations with medial or lateral displacement (author’s transl)]. Article in French. Rev Chir Orthop Reparatrice Appar Mot. 1979;65(7):377–385. [PubMed] [Google Scholar]
- 118.Martin LP, Wayne JS, Owen JR, Smith RT, Martin SN, Adelaar RS. Elongation behavior of calcaneofibular and cervical ligaments in a closed kinetic chain: pathomechanics of lateral hindfoot instability. Foot Ankle Int. 2002;23(6):515–520. [DOI] [PubMed] [Google Scholar]
- 119.Matsui K, Oliva XM, Takao M, et al. Bony landmarks available for minimally invasive lateral ankle stabilization surgery: a cadaveric anatomical study. Knee Surg Sports Traumatol Arthrosc. 2017;25(6):1916–1924. [DOI] [PubMed] [Google Scholar]
- 120.McKeon PO, Hertel J. Spatiotemporal postural control deficits are present in those with chronic ankle instability. BMC Musculoskelet Disord. 2008;9:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.McKeon PO, Hertel J. Systematic review of postural control and lateral ankle instability, part II: is balance training clinically effective? J Athl Train. 2008;43(3):305–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Meacham BP, Granata JD, Berlet GC. Tenodesis reconstruction for chronic ankle instability: graft considerations and structures at risk with tunnel placement. Foot Ankle Spec. 2012;5(6):378–381. [DOI] [PubMed] [Google Scholar]
- 123.Merchan EC. Subtalar dislocations: long-term follow-up of 39 cases. Injury. 1992;23(2):97–100. [DOI] [PubMed] [Google Scholar]
- 124.Meyer JM, Garcia J, Hoffmeyer P, Fritschy D. The subtalar sprain: a roentgenographic study. Clin Orthop Relat Res. 1988;226:169–173. [PubMed] [Google Scholar]
- 125.Michels F, Clockaerts S, Van Der Bauwhede J, Stockmans F, Matricali G. Does subtalar instability really exist? A systematic review. Foot Ankle Surg. 2020;26(2):119–127. [DOI] [PubMed] [Google Scholar]
- 126.Michels F, Cordier G, Burssens A, Vereecke E, Guillo S. Endoscopic reconstruction of CFL and the ATFL with a gracilis graft: a cadaveric study. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1007–1014. [DOI] [PubMed] [Google Scholar]
- 127.Michels F, Cordier G, Guillo S, Stockmans F. Endoscopic ankle lateral ligament graft anatomic reconstruction. Foot Ankle Clin. 2016;21(3):665–680. [DOI] [PubMed] [Google Scholar]
- 128.Michels F, Pereira H, Calder J, et al. Searching for consensus in the approach to patients with chronic lateral ankle instability: ask the expert. Knee Surg Sports Traumatol Arthrosc. 2018;26(7):2095–2102. [DOI] [PubMed] [Google Scholar]
- 129.Miller CA, Bosco JA, III. Lateral ankle and subtalar instability. Bull Hosp Jt Dis. 2001;60(3-4):143–149. [PubMed] [Google Scholar]
- 130.Mittlmeier T, Rammelt S. Update on subtalar joint instability. Foot Ankle Clin. 2018;23(3):397–413. [DOI] [PubMed] [Google Scholar]
- 131.Molloy S, Solan MC, Bendall SP. Synovial impingement in the ankle: a new physical sign. J Bone Joint Surg Br. 2003;85(3):330–333. [DOI] [PubMed] [Google Scholar]
- 132.Mullen JE, O’Malley MJ. Sprains: residual instability of subtalar, Lisfranc joints, and turf toe. Clin Sports Med. 2004;23(1):97–121. [DOI] [PubMed] [Google Scholar]
- 133.Orr JD, Nunley JA. Isolated spring ligament failure as a cause of adult-acquired flatfoot deformity. Foot Ankle Int. 2013;34(6):818–823. [DOI] [PubMed] [Google Scholar]
- 134.Pagenstert GI, Hintermann B, Knupp M. Operative management of chronic ankle instability: plantaris graft. Foot Ankle Clin. 2006;11(3):567–583. [DOI] [PubMed] [Google Scholar]
- 135.Pagenstert GI, Valderrabano V, Hintermann B. Lateral ankle ligament reconstruction with free plantaris tendon graft. Tech Foot Ankle Surg. 2005;4(2):104–112. [Google Scholar]
- 136.Palmieri-Smith RM, Hopkins JT, Brown TN. Peroneal activation deficits in persons with functional ankle instability. Am J Sports Med. 2009;37(5):982–988. [DOI] [PubMed] [Google Scholar]
- 137.Paterson R, Cohen B, Taylor D, Bourne A, Black J. Reconstruction of the lateral ligaments of the ankle using semi-tendinosis graft. Foot Ankle Int. 2000;21(5):413–419. [DOI] [PubMed] [Google Scholar]
- 138.Pellegrini MJ, Glisson RR, Wurm M, et al. Systematic quantification of stabilizing effects of subtalar joint soft-tissue constraints in a novel cadaveric model. J Bone Joint Surg Am. 2016;98(10):842–848. [DOI] [PubMed] [Google Scholar]
- 139.Pereira BS, van Dijk CN, Andrade R, Casaroli-Marano RP, Espregueira-Mendes J, Oliva XM. The calcaneofibular ligament has distinct anatomic morphological variants: an anatomical cadaveric study. Knee Surg Sports Traumatol Arthrosc. 2020;28(1):40–47. [DOI] [PubMed] [Google Scholar]
- 140.Peterson KS, Catanzariti AR, Mendicino MR, Mendicino RW. Surgical approach for combined ankle and subtalar joint chronic mechanical instability. J Foot Ankle Surg. 2013;52(4):537–542. [DOI] [PubMed] [Google Scholar]
- 141.Pisani G. Chronic laxity of the subtalar joint. Orthopedics. 1996;19(5):431–437. [DOI] [PubMed] [Google Scholar]
- 142.Pisani G. The coxa pedis. Foot Ankle Surg. 1994;1(2-3):67–74. [DOI] [PubMed] [Google Scholar]
- 143.Pisani G, Pisani PC, Parino E. Sinus tarsi syndrome and subtalar joint instability. Clin Podiatr Med Surg. 2005;22(1):63–77, vii. [DOI] [PubMed] [Google Scholar]
- 144.Poonja AJ, Hirano M, Khakimov D, et al. Anatomical study of the cervical and interosseous talocalcaneal ligaments of the foot with surgical relevance. Cureus. 2017;9(6):e1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Prada-Canizares A, Aunon-Martin I, Vila YRJ, Pretell-Mazzini J. Subtalar dislocation: management and prognosis for an uncommon orthopaedic condition. Int Orthop. 2016;40(5):999–1007. [DOI] [PubMed] [Google Scholar]
- 146.Prisk VR, Imhauser CW, O’Loughlin PF, Kennedy JG. Lateral ligament repair and reconstruction restore neither contact mechanics of the ankle joint nor motion patterns of the hindfoot. J Bone Joint Surg Am. 2010;92(14):2375–2386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Raymond J, Nicholson LL, Hiller CE, Refshauge KM. The effect of ankle taping or bracing on proprioception in functional ankle instability: a systematic review and meta-analysis. J Sci Med Sport. 2012;15(5):386–392. [DOI] [PubMed] [Google Scholar]
- 148.Ringleb SI, Dhakal A, Anderson CD, Bawab S, Paranjape R. Effects of lateral ligament sectioning on the stability of the ankle and subtalar joint. J Orthop Res. 2011;29(10):1459–1464. [DOI] [PubMed] [Google Scholar]
- 149.Roach KE, Foreman KB, Barg A, Saltzman CL, Anderson AE. Application of high-speed dual fluoroscopy to study in vivo tibiotalar and subtalar kinematics in patients with chronic ankle instability and asymptomatic control subjects during dynamic activities. Foot Ankle Int. 2017;38(11):1236–1248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Rubin G. The subtalar joint and the symptom of turning over on the ankle. Am J Orthop. 1962;4:16–19. [Google Scholar]
- 151.Sakakibara Y, Teramoto A, Takagi T, et al. Effect of initial graft tension during calcaneofibular ligament reconstruction on ankle kinematics and laxity. Am J Sports Med. 2018;46(12):2935–2941. [DOI] [PubMed] [Google Scholar]
- 152.Saltzman C, Anderson RB. Athletic injuries to the soft tissues of the foot and ankle. In: Coughlin M, ed. Surgery of the Foot and Ankle. 7th ed. Mosby; 1999:1153–1165. [Google Scholar]
- 153.Saltzman C, Marsh JL. Hindfoot dislocations: when are they not benign? J Am Acad Orthop Surg. 1997;5(4):192–198. [DOI] [PubMed] [Google Scholar]
- 154.Sammarco G. Biomechanics of the ankle: a kinematic study. Orthop Clin North Am. 1973;4:75–96. [PubMed] [Google Scholar]
- 155.Sammarco VJ. Complications of lateral ankle ligament reconstruction. Clin Orthop Relat Res. 2001;391:123–132. [DOI] [PubMed] [Google Scholar]
- 156.Samoto N, Sugimoto K, Takaoka T, Fujita T, Kitada C, Takakura Y. Comparative results of conservative treatments for isolated anterior talofibular ligament injury and injury to both the ATFL and calcaneofibular ligament of the ankle as assessed by subtalar arthrography. J Orthop Sci. 2007;12(1):49–54. [DOI] [PubMed] [Google Scholar]
- 157.Santos MJ, Liu W. Possible factors related to functional ankle instability. J Orthop Sports Phys Ther. 2008;38(3):150–157. [DOI] [PubMed] [Google Scholar]
- 158.Saragaglia D, Fontanel F, Montbarbon E, Tourne Y, Picard F, Charbel A. Reconstruction of the lateral ankle ligaments using an inferior extensor retinaculum flap. Foot Ankle Int. 1997;18(11):723–728. [DOI] [PubMed] [Google Scholar]
- 159.Sarrafian SK. Anatomy of the Foot and Ankle: Descriptive, Topographic, Functional. Lippincott Williams & Wilkins; 1993. [Google Scholar]
- 160.Schon LC, Clanton TO, Baxter DE. Reconstruction for subtalar instability: a review. Foot Ankle. 1991;11(5):319–325. [DOI] [PubMed] [Google Scholar]
- 161.Seebauer CJ, Bail HJ, Rump JC, Hamm B, Walter T, Teichgraber UK. Ankle laxity: stress investigation under MRI control. AJR Am J Roentgenol. 2013;201(3):496–504. [DOI] [PubMed] [Google Scholar]
- 162.Sijbrandij ES, van Gils AP, van Hellemondt FJ, Louwerens JW, de Lange EE. Assessing the subtalar joint: the Brodén view revisited. Foot Ankle Int. 2001;22(4):329–334. [DOI] [PubMed] [Google Scholar]
- 163.Smith PA, Miller SJ, Berni AJ. A modified Chrisman-Snook procedure for reconstruction of the lateral ligaments of the ankle: review of 18 cases. Foot Ankle Int. 1995;16(5):259–266. [DOI] [PubMed] [Google Scholar]
- 164.So E, Weber J, Berlet G, Bull P. Surgical treatment of subtalar joint instability: safety and accuracy of a new technique in a cadaver model. J Foot Ankle Surg. 2020;59(1):38–43. [DOI] [PubMed] [Google Scholar]
- 165.Solheim LF, Denstad TF, Roaas A. Chronic lateral instability of the ankle: a method of reconstruction using the Achilles tendon. Acta Orthop Scand. 1980;51(1):193–196. [DOI] [PubMed] [Google Scholar]
- 166.Srinivasan VB, Downes EM. Split peroneus longus tenodesis for chronic lateral ligamentous instability of ankle. Injury. 1996;27(7):467–469. [DOI] [PubMed] [Google Scholar]
- 167.Sugimoto K, Samoto N, Takaoka T, Takakura Y, Tamai S. Subtalar arthrography in acute injuries of the calcaneofibular ligament. J Bone Joint Surg Br. 1998;80(5):785–790. [DOI] [PubMed] [Google Scholar]
- 168.Sugimoto K, Takakura Y, Samoto N, Nakayama S, Tanaka Y. Subtalar arthrography in recurrent instability of the ankle. Clin Orthop Relat Res. 2002;394:169–176. [DOI] [PubMed] [Google Scholar]
- 169.Takao M, Glazebrook M, Stone J, Guillo S. Ankle arthroscopic reconstruction of lateral ligaments (ankle anti-ROLL). Arthrosc Tech. 2015;4(5):e595–e600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Takao M, Oae K, Uchio Y, Ochi M, Yamamoto H. Anatomical reconstruction of the lateral ligaments of the ankle with a gracilis autograft: a new technique using an interference fit anchoring system. Am J Sports Med. 2005;33(6):814–823. [DOI] [PubMed] [Google Scholar]
- 171.Taniguchi A, Tanaka Y, Takakura Y, Kadono K, Maeda M, Yamamoto H. Anatomy of the spring ligament. J Bone Joint Surg Am. 2003;85(11):2174–2178. [DOI] [PubMed] [Google Scholar]
- 172.Teramoto A, Watanabe K, Takashima H, Yamashita T. Subtalar joint stress imaging with tomosynthesis. Foot Ankle Spec. 2014;7(3):182–184. [DOI] [PubMed] [Google Scholar]
- 173.Thermann H, Zwipp H, Tscherne H. Treatment algorithm of chronic ankle and subtalar instability. Foot Ankle Int. 1997;18(3):163–169. [DOI] [PubMed] [Google Scholar]
- 174.Tochigi Y. Effect of arch supports on ankle-subtalar complex instability: a biomechanical experimental study. Foot Ankle Int. 2003;24(8):634–639. [DOI] [PubMed] [Google Scholar]
- 175.Tochigi Y, Amendola A, Rudert MJ, et al. The role of the interosseous talocalcaneal ligament in subtalar joint stability. Foot Ankle Int. 2004;25(8):588–596. [DOI] [PubMed] [Google Scholar]
- 176.Tochigi Y, Yoshinaga K, Wada Y, Moriya H. Acute inversion injury of the ankle: magnetic resonance imaging and clinical outcomes. Foot Ankle Int. 1998;19(11):730–734. [DOI] [PubMed] [Google Scholar]
- 177.Tourne Y, Mabit C. Lateral ligament reconstruction procedures for the ankle. Orthop Traumatol Surg Res. 2017;103(1)(suppl):S171–S181. [DOI] [PubMed] [Google Scholar]
- 178.Tourne Y, Peruzzi M. Lateral collateral ligament repair: anatomical ligament reinsertion with augmentation using inferior extensor retinaculum flaps. Oper Orthop Traumatol. 2019;31(3):169–179. [DOI] [PubMed] [Google Scholar]
- 179.Ulku TK, Kocaoglu B, Tok O, Irgit K, Nalbantoglu U. Arthroscopic suture-tape internal bracing is safe as arthroscopic modified Broström repair in the treatment of chronic ankle instability. Knee Surg Sports Traumatol Arthrosc. 2020;28(1):227–232. [DOI] [PubMed] [Google Scholar]
- 180.Usuelli FG, Mason L, Grassi M, Maccario C, Ballal M, Molloy A. Lateral ankle and hindfoot instability: a new clinical based classification. Foot Ankle Surg. 2014;20(4):231–236. [DOI] [PubMed] [Google Scholar]
- 181.Vaes P, Duquet W, Handelberg F, Casteleyn PP, Van Tiggelen R, Opdecam P. Objective roentgenologic measurements of the influence of ankle braces on pathologic joint mobility: a comparison of 9 braces. Acta Orthop Belg. 1998;64(2):201–209. [PubMed] [Google Scholar]
- 182.van Dijk CN, Lim LS, Bossuyt PM, Marti RK. Physical examination is sufficient for the diagnosis of sprained ankles. J Bone Joint Surg Br. 1996;78(6):958–962. [DOI] [PubMed] [Google Scholar]
- 183.van Hellemondt FJ, Louwerens JW, Sijbrandij ES, van Gils AP. Stress radiography and stress examination of the talocrural and subtalar joint on helical computed tomography. Foot Ankle Int. 1997;18(8):482–488. [DOI] [PubMed] [Google Scholar]
- 184.Vaseenon T, Gao Y, Phisitkul P. Comparison of 2 manual tests for ankle laxity due to rupture of the lateral ankle ligaments. Iowa Orthop J. 2012;32:9–16. [PMC free article] [PubMed] [Google Scholar]
- 185.Verhagen E, van der Beek A, Twisk J, Bouter L, Bahr R, van Mechelen W. The effect of a proprioceptive balance board training program for the prevention of ankle sprains: a prospective controlled trial. Am J Sports Med. 2004;32(6):1385–1393. [DOI] [PubMed] [Google Scholar]
- 186.Verhagen RA, de Keizer G, van Dijk CN. Long-term follow-up of inversion trauma of the ankle. Arch Orthop Trauma Surg. 1995;114(2):92–96. [DOI] [PubMed] [Google Scholar]
- 187.Vicenzino B, Branjerdporn M, Teys P, Jordan K. Initial changes in posterior talar glide and dorsiflexion of the ankle after mobilization with movement in individuals with recurrent ankle sprain. J Orthop Sports Phys Ther. 2006;36(7):464–471. [DOI] [PubMed] [Google Scholar]
- 188.Waldecker U, Blatter G. Sonographic measurement of instability of the subtalar joint. Foot Ankle Int. 2001;22(1):42–46. [DOI] [PubMed] [Google Scholar]
- 189.Wang B, Xu XY. Minimally invasive reconstruction of lateral ligaments of the ankle using semitendinosus autograft. Foot Ankle Int. 2013;34(5):711–715. [DOI] [PubMed] [Google Scholar]
- 190.Weindel S, Schmidt R, Rammelt S, Claes L, Campe Av, Rein S. Subtalar instability: a biomechanical cadaver study. Arch Orthop Trauma Surg. 2010;130(3):313–319. [DOI] [PubMed] [Google Scholar]
- 191.Wikstrom EA, Bishop MD, Inamdar AD, Hass CJ. Gait termination control strategies are altered in chronic ankle instability subjects. Med Sci Sports Exerc. 2010;42(1):197–205. [DOI] [PubMed] [Google Scholar]
- 192.Wilkerson GB. Comparative biomechanical effects of the standard method of ankle taping and a taping method designed to enhance subtalar stability. Am J Sports Med. 1991;19(6):588–595. [DOI] [PubMed] [Google Scholar]
- 193.Wilkerson GB, Kovaleski JE, Meyer M, Stawiz C. Effects of the subtalar sling ankle taping technique on combined talocrural-subtalar joint motions. Foot Ankle Int. 2005;26(3):239–246. [DOI] [PubMed] [Google Scholar]
- 194.Willems T, Witvrouw E, Verstuyft J, Vaes P, De Clercq D. Proprioception and muscle strength in subjects with a history of ankle sprains and chronic instability. J Athl Train. 2002;37(4):487–493. [PMC free article] [PubMed] [Google Scholar]
- 195.Williams MM, Ferkel RD. Subtalar arthroscopy: indications, technique, and results. Arthroscopy. 1998;14(4):373–381. [DOI] [PubMed] [Google Scholar]
- 196.Woodruff MJ, Brown JN, Mountney J. A mechanism for entrapment of the tibialis posterior tendon in lateral subtalar dislocation. Injury. 1996;27(3):193–194. [DOI] [PubMed] [Google Scholar]
- 197.Xu DL, Gan KF, Li HJ, et al. Modified Broström repair with and without augmentation using suture tape for chronic lateral ankle instability. Orthop Surg. 2019;11(4):671–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Yamamoto H, Yagishita K, Ogiuchi T, Sakai H, Shinomiya K, Muneta T. Subtalar instability following lateral ligament injuries of the ankle. Injury. 1998;29(4):265–268. [DOI] [PubMed] [Google Scholar]
- 199.Yoon DY, Moon SG, Jung HG, Kim NR. Differences between subtalar instability and lateral ankle instability focusing on subtalar ligaments based on three-dimensional isotropic magnetic resonance imaging. J Comput Assist Tomogr. 2018;42(4):566–573. [DOI] [PubMed] [Google Scholar]
- 200.Ziai P, Benca E, Skrbensky GV, et al. The role of the medial ligaments in lateral stabilization of the ankle joint: an in vitro study. Knee Surg Sports Traumatol Arthrosc. 2015;23(7):1900–1906. [DOI] [PubMed] [Google Scholar]
- 201.Zimmer TJ, Johnson KA. Subtalar dislocations. Clin Orthop Relat Res. 1989;238:190–194. [PubMed] [Google Scholar]
- 202.Zwipp H, Tscherne H. Radiological diagnosis of instability of the subtalar joint. Unfallheilkunde-Traumatology. 1982;85(12):494–498. [PubMed] [Google Scholar]