Abstract
Objectives:
The coronavirus disease 2019 pandemic has caused high morbidity and mortality in older adults over the world. Because the coronavirus disease 2019 pandemic greatly affects older adults who have a preexisting health condition, they are generally susceptible to a high incidence of severe symptoms of anxiety and depression. Therefore, we aimed to assess the prevalence of anxiety and depression symptoms in older adults during the coronavirus disease 2019 pandemic.
Methods:
Community-based cross-sectional study was completed in August 2020. Standardized and pretested General Anxiety Disorder–7 and Geriatric Depression Scale were used to screen the symptoms of anxiety and depression, respectively. Data were entered into EpiData (version 4.3.2) and transferred to SPSS (version 24) for further analysis. Bivariate and multivariate logistic regression analyses were carried out to determine the significantly associated variables with a 95% confidence interval at p < 0.05.
Results:
Of the total older adults interviewed, 68.7% had developed symptoms of anxiety and 59.9% had symptoms of depression during the coronavirus disease 2019 pandemic. Female participants, having a chronic disease and poor knowledge of the coronavirus disease 2019 pandemic, were significantly associated with anxiety symptoms. Age category of 81 to 90 and above 90, lack of social support, and having a chronic disease were significantly associated with symptoms of depression.
Conclusion:
The symptoms of anxiety and depression among older adults in the North Shoa Zone during coronavirus disease 2019 were higher than before the coronavirus disease 2019 happened. The results were evidence points for developing a psychological intervention to tackle the older adults’ mental health needs in the community during and after the coronavirus disease 2019 pandemic.
Keywords: Coronavirus disease 2019, anxiety, depression, older adults, Ethiopia
Introduction
One year ago, a new disease of unknown etiology appeared in Wuhan, China, which was later rapidly identified as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2),1 causing severe respiratory illness and declared as a pandemic on 30 January 2020 by the World Health Organization (WHO). The pandemic causes high morbidity and mortality over the world, particularly the older population, and persons who have chronic diseases are generally susceptible to a high incidence of severe disease and mortality from the coronavirus disease 2019 (COVID-19).2
The COVID-19 pandemic increases day to day, affecting older adults, and leads to serious health complications. Around the world, more than 26.2 million infections with 870,700 confirmed deaths were reported by the WHO globally since 30 August 2020. In Africa, a total of 132,508 infected cases and 15,020 deaths have been reported. In Ethiopia specifically, an alarming total of 52,131 cases and 809 deaths have occurred as of 30 August 2020.3 In addition, the study conducted in Ethiopia found that older adults whose age 60 years and above have been highly affected by the COVID-19 pandemic, and 80% of admitted COVID-19 patients in the intensive care unit have died with a case fatality rate of 22.2%.4
For the most part, older adults with preexisting conditions are isolated from social support, which may increase the incidence and severity of depression and anxiety symptoms among this portion of the population.5 The WHO6 states that in many countries, older adults are facing several mental illnesses due to the high challenges of the COVID-19 pandemic. Older adults are at a higher risk of developing severe illness of COVID-19, with a fatality rate of 5.6% among 60 to 69 years and 18% above 80 years that makes them more anxious and depressed.7,8
The COVID-19 pandemic has also made a significant impact on older adults causing anxiety, adjustment disorders, depression, panic, chronic stress, and insomnia.9 In addition, it leads to social isolation, limited interaction with each other as home quarantine, and a serious public health concern due to their bio-psycho-social vulnerabilities.2
The study conducted in China found that anxiety and depression among older adults (above 60 years old) are more obvious, which was women experiencing more anxiety and depression than men.10 Also, another study done in Sweden among the older adults during the COVID-19 pandemic indicated that the majority of older adults had worried about their health condition during the COVID-19 pandemic, feeling depressed, having trouble sleeping, having difficulty concentrating, and worrying about economic downturns.11
A few studies have identified the clinical characteristic and natural course of the COVID-19 pandemic in the hospital setting in Ethiopia among older adults.12,13 However, older adults are the most vulnerable section of the population for mental problems during the COVID-19 pandemic.14 For the reason that the older adults have an underlying health condition, may have dementia or cognitive decline, may become more anxious, angry, stressed, agitated and may have withdrawn as home quarantine,6 and lack of accessible health facilities and dissatisfaction with health care services.15 Moreover, in Ethiopia, the COVID-19 infection affects all age groups, but the majority of deaths have been recorded among older adults greater than or equal to 60 years,4 which accelerate the cause of stressor for symptoms of anxiety and depression.16,17 In addition, the lockdown measures imposed during COVID-19 may have affected older adults living in the study area as they are financially incapable and supported by volunteers that might be an additional burden for mental problems.
There is a lack of detailed descriptions of the mental health problem of the COVID-19 pandemic in community-based older adults living in Sub-Saharan countries, particularly in Ethiopia. This finding was used for critical making decisions for the development of mental health intervention that capacitates older adults living in the community during and after the COVID-19 pandemic. Therefore, we aimed to assess the prevalence of depression and anxiety symptoms in older adults during the COVID-19 pandemic in Ethiopia.
Methods
Study design, area, and period
A community-based cross-sectional study was conducted in August 2020 in Debre Libanos District, North Shoa Zone of Oromia Regional State. The zone’s capital city is Fiche, located at a distance of 112 km from Addis Ababa in the north direction. North Shoa Zone has a total population of more than 1.6 million, where 820,595 are male and 818,992 are female. Eighty-eight percent (1,447,330) of the North Shoa population live in rural areas, and 12% (192,105) live in urban areas. North Shoa contained a higher number of older adults due to the presence of Debre Libanos monastery (Gedam), which consists of more than one-fourth (26.3%) of the population, aged above 60 years old. The North Shoa Zone has two general hospitals and three district hospitals, 65 health centers, and 297 health posts.
Study population
The study population was an older adult population whose age greater than or equal to 60 years and who have been living in the Debre Libanos District for more than 1 year. Those who are not eligible or critically ill and have hearing problems were excluded from the study. The definition of old age depends on various contexts of countries’ settings to determine the old age cut point. The United Nations uses 60 years to define old age and recommends the age range of 50 to 65 years to be used as a cutoff point by countries.18 In Ethiopia, the cut points of old age are started in 60 years.19
Sample size determination and sampling technique
The sample size required for this study was calculated using the formula to determine a single population proportion. Due to a lack of the previous study, we use a proportion of 50% and a 95% confidence interval (CI) with a 5% margin of error. The final sample size was 423.
A Debre Libanos District was purposely selected due to the high number of geriatrics in the district, which contains 10 rural Kebeles (the least local administration) and one town. Each list of the household folder was obtained from health extension workers in each Kebele, and then a list of the household was prepared. After that, from the list of households, 50% of the households were selected by the lottery method. Finally, every household in the selected Kebele was visited for an elderly interview.
Study variables
The outcome variables for this study were anxiety and depression. Anxiety was measured using the General Anxiety Disorder–7 (GAD-7) scale. It contains a seven-item self-reported questionnaire that is planned to screen the symptoms of anxiety. The sum score of GAD-7 is accepted with a cutoff point greater than or equal to 5.20 It was validated in Kenya with Cronbach’s alpha = 0.82 and intraclass correlation coefficient = 0.70.21 In Ethiopia, different studies used the GAD-7 tool converting into the local languages, Amharic and Afan Oromo.22–24 It was also reliable in our pretested study with Cronbach’s alpha = 0.75.
The other outcome variable was depression, which was measured with a Geriatric Depression Scale (GDS) that contains 15 items of questions. The question is self-reporting on how the person felt during the last week of his or her life, and the study participants were asked to answer them as “yes” or “no.” Each bold answer indicated depression (“yes” or “no”) counts one point and zeros the other. The sum is accepted as a total depression score with a cutoff point greater than or equal to 5. The scores to be obtained from the scale are between 0 and 15.25 Even though the GDS was not validated in Ethiopia, several studies were conducted using translated GDS into Afan Oromo and Amharic languages.26,27 The GDS was validated in other country among older adults were satisfactory with (Cronbach’s α = .80) and test–retest reliability (r = .73).28 In addition, we checked the suitability of GDS in the pretest of this study with Cronbach’s alpha = 0.84.
Independent variables
The independent variables included in this study were sociodemographic characteristics (age, gender, marital status, education, number of children, place of residence, and living status), source of income, family support, social support, chronic disease, substance use, knowledge of COVID-19, attitude toward COVID-19, preparedness, and response to COVID-19 pandemic. Social support was measured using the three-item Oslo Social Support Scale, with scores of 3 to 8 were categorized as poor social support and score above 9 was categorized as strong social support.29 In this study, it was reliable in pretested with Cronbach’s alpha = 0.68. Current substance use was defined as using at least one of the specified substances (alcohol, khat, tobacco, and coffee/caffeine) in the past 3 months.
The outcome of knowledge, attitude, preparedness, and response to the COVID-19 pandemic was measured using 12, 10, 11, and 16 questions, respectively. Taking the mean scores as a cutoff point, the outcomes were calculated after testing each outcome result’s normality distribution. The scores greater than the mean score were considered knowledgeable, positive attitude, good preparedness, and good response. Below the mean scores were considered not knowledgeable, negative attitude, poor preparedness, and poor responses to the COVID-19 pandemic.30 In this study, the questionnaires’ reliability was checked in a pretested questionnaire with Cronbach’s alpha 0.73 for knowledge, 0.85 for attitude, 0.86 for preparedness, and 0.79 for responses.
Data collection tools and procedure
The data were collected using a standardized and pretested questionnaire by face-to-face calling at each household. Ten nurses’ (BSc) data collectors and five supervisors were recruited for data collection and supervision. The questionnaire was developed from different literature that was initially written in the English language,20,25,29–33 and translated to Afan Oromo and Amharic languages and back-translated to the English language by language experts to check its consistency. The questionnaire contains different components: sociodemographic characteristics, living status, family support, social support, comorbidity and substance use, knowledge about COVID-19, attitude toward COVID-19, preparedness toward COVID-19, response to the COVID-19, depression, and anxiety (see Supplemental material).
Data collectors and supervisors were trained for 5 days on the purpose of the study, details of the questionnaire, interviewing techniques, the importance of privacy, and ensuring the respondents’ confidentiality. In addition to data collection training, the prevention technique of the COVID-19 pandemic with personal protective equipment was provided for data collectors and supervisors.
The pretest was done on 5% (21 samples) in Girar Jarso District other than the study area having the same sociodemographic characteristics of older adults. Close supervision at the end of every data collection was made; the questionnaire was reviewed and checked for completeness, accuracy, and consistency by the supervisor and principal investigator to take timely corrective measures. Accordingly, after discussion with data collectors and supervisors, modification was done before actual data collection.
Data processing and analysis
Data were coded, edited, cleaned, and entered into EpiData (version) 4.3.2 and transported to SPSS (version 24). The descriptive data analysis was done and presented in frequency, summary statistics, and table. Bivariate and multivariate logistic regression analyses were carried out, and variables with a p ⩽ 0.2 in the bivariate analysis were included in a multivariable logistic regression analysis to control the confounding effect variables.34 The model fitness was checked using the Hosmer and Lemeshow goodness-of-fit model, and the model was fitted at p = 0.795 for anxiety and p = 0.638 for depression. Finally, statistical significance was declared if p < 0.05.
Ethical consideration
The study protocol, methods, and consent form were approved by the Salale University Ethical Review Committee on 24 July 2020 Re. No. 025/2020. After thoroughly discussing the study’s ultimate purpose and method, written consent was sought from the North Shoa Zonal Health Bureau/Woreda Department. We have obtained written informed consent from participants below 90 years as they have the decisional capacity. Assent was obtained from parents/guardians for participants above 90 years old. The respondents were informed that their inclusion in the study is voluntary, and they are free to withdraw from the study if they are not willing to participate. If they do not want to answer any question, they have the right to do so. To ensure the confidentiality of respondents, their names were excluded from the questionnaire. The confidentiality of the respondents was kept.
Results
In this study, a total of 409 participants participated with response rates of 96.7% with none response rate of 3.3% that failed to respond satisfactory items response. The mean age of the study participants was 75.13 (± standard deviation (SD) = 9.38) years, with the most age category of 60 to 70 (45.0%). The majority of study participants were male (51.3%), married (37.7%), not having formal education (70.4%), living in the rural (71.9%), and living with their family (53.5%) (Table 1).
Table 1.
Sociodemographic and socioeconomic characteristics in older adults during COVID-19 at North Shoa Zone, Debre Libanos District, Oromia region, Ethiopia, 2020 (N = 409).
| Variables | n | % |
|---|---|---|
| Age | ||
| 60–70 | 184 | 45.0 |
| 71–80 | 125 | 30.6 |
| 81–90 | 71 | 17.4 |
| >90 | 29 | 7.0 |
| Sex | ||
| Male | 210 | 51.3 |
| Female | 199 | 48.7 |
| Marital status | ||
| Single | 82 | 20.0 |
| Married | 154 | 37.7 |
| Widowed | 113 | 27.6 |
| Divorced | 60 | 14.7 |
| Educational status | ||
| No formal education | 288 | 70.4 |
| Has formal education | 121 | 29.6 |
| Number of children | ||
| No children | 95 | 23.2 |
| One child | 40 | 9.8 |
| Two children | 77 | 18.8 |
| More than three children | 197 | 48.2 |
| Source of income | ||
| Retirement | 17 | 4.2 |
| Helped by family | 74 | 18.1 |
| Farmer | 122 | 29.8 |
| Merchant | 20 | 4.9 |
| Supported by NGO | 135 | 33.0 |
| No income | 41 | 10.0 |
| Place of residence | ||
| Urban | 70 | 17.1 |
| Rural | 294 | 71.9 |
| Rehabilitation center | 45 | 11.0 |
| Living status | ||
| Alone | 190 | 46.5 |
| With family | 219 | 53.5 |
COVID-19: coronavirus disease 2019; NGO: nongovernmental organization.
Table 2 documented that more than two-thirds of the older adults had no social support, and one-fourth of older participants had chronic diseases. Greater than one-third (36.9%) of older adults had gained COVID-19 information from news media (TV and radio), and 38.6% of older participants currently consumed alcohol. About 62.3% and 53.3% of the older adults had good responses and preparedness toward the COVID-19 pandemic, respectively. Conversely, 57.0% and 46.0% of the older adults had poor knowledge and a negative attitude toward the COVID-19 pandemic.
Table 2.
Variables related to older adults during COVID-19 at North Shoa Zone, Debre Libanos District, Oromia region, Ethiopia, 2020 (N = 409).
| Variables | n | % |
|---|---|---|
| Social support environment available | ||
| No | 274 | 67.0 |
| Yes | 135 | 33.0 |
| Are you currently ill? | ||
| No | 259 | 63.3 |
| Yes | 150 | 36.7 |
| Having chronic disease | ||
| No | 303 | 74.1 |
| Yes | 106 | 25.9 |
| Current substance use | ||
| Alcohol | 158 | 38.6 |
| Tobacco | 23 | 5.6 |
| Coffee/caffeine | 63 | 15.4 |
| No current substance use | 165 | 40.4 |
| Source of information about COVID-19 | ||
| News media (TV and radio) | 151 | 36.9 |
| Social media | 96 | 23.5 |
| Family or friends | 75 | 18.3 |
| Health care providers | 87 | 21.3 |
| COVID-19 response | ||
| Poor response | 154 | 37.7 |
| Good response | 255 | 62.3 |
| COVID-19 preparedness | ||
| Poor preparedness | 191 | 46.7 |
| Good preparedness | 218 | 53.3 |
| COVID-19 knowledge | ||
| Poor knowledge | 233 | 57.0 |
| Good knowledge | 176 | 43.0 |
| Attitude toward COVID-19 | ||
| Negative attitude | 188 | 46.0 |
| Positive attitude | 221 | 54.0 |
COVID-19: coronavirus disease 2019.
This study indicated that 68.7% (281) with 95% CI = (64.4–73.6) of older adults had anxiety symptoms and 31.3% (128) with 95% CI = (26.4–35.6) of the study participants had no anxiety symptoms. On the contrary, the prevalence of depressed older adults was 59.9% (245) with 95% CI = (55.5–64.2), and 40.1% (164) with 95% CI = (35.8–44.5) of older adults had no depression symptoms (Figure 1).
Figure 1.
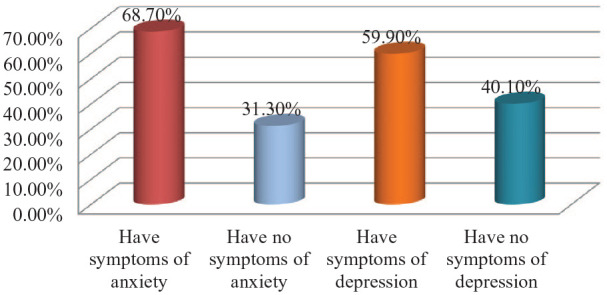
The prevalence of anxiety and depression in older adults during COVID-19 at North Shoa Zone, Debre Libanos District, Oromia region, Ethiopia, 2020 (N = 409).
Factors associated with anxiety and depression
Variables that fulfilled the criteria of p < 0.2 were included in multivariable logistic regression. Older adults who have no children, who were helped by family, who live alone, who current substance use (alcohol, tobacco, and caffeine), who have a poor response for COVID-19, and who have poor preparedness for COVID-19 were adjusted in multivariable logistic regression for symptoms of anxiety (Table 3).
Table 3.
Factors associated with symptoms of anxiety in older adults during COVID-19 at North Shoa Zone, Debre Libanos District, Oromia region, Ethiopia, 2020 (N = 409).
| Variables | Anxiety | Crude OR (95% CI) | p | Adjusted OR (95% CI) | p | |
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Sex | ||||||
| Male | 135 | 75 | 1 | 1 | ||
| Female | 146 | 53 | 1.53 (1.00–2.34) | 0.048* | 1.40 (1.06–2.94) | 0.029* |
| Marital status | ||||||
| Single | 182 | 73 | 1 | 1 | ||
| Married | 99 | 55 | 0.72 (0.47–1.11) | 0.135 | 0.55 (0.29–1.04) | 0.066 |
| Educational status | ||||||
| No formal education | 206 | 82 | 1.54 (0.98–2.41) | 0.058 | 1.16 (0.67–2.02) | 0.602 |
| Formal education | 75 | 46 | 1 | 1 | ||
| Number of children | ||||||
| No children | 44 | 51 | 0.25 (0.15–0.42) | 0.001* | 0.20 (0.15–1.49) | 0.065 |
| One child | 26 | 14 | 0.53 (0.25–1.11) | 0.093 | 0.50 (0.30–1.95) | 0.758 |
| Two children | 58 | 19 | 0.88 (0.47–1.63) | 0.679 | 0.83 (0.54–2.25) | 0.835 |
| More than three children | 153 | 44 | 1 | 1 | ||
| Source of income | ||||||
| Retirement | 11 | 6 | 1 | 1 | ||
| Helped by family | 66 | 8 | 4.50 (1.31–15.49) | 0.017* | 1.96 (0.46–8.30) | 0.347 |
| Farmer | 98 | 24 | 2.23 (0.75–6.63) | 0.150 | 1.79 (0.48–4.13) | 0.377 |
| Merchant | 14 | 6 | 1.27 (0.32–5.06) | 0.732 | 1.23 (0.25–3.79) | 0.792 |
| Supported by NGO | 66 | 69 | 0.52 (0.18–1.49) | 0.225 | 0.47 (0.20–2.50) | 0.657 |
| No income | 26 | 15 | 0.95 (0.29–3.08) | 0.926 | 0.90 (0.28–4.70) | 0.529 |
| Living status | ||||||
| Alone | 106 | 84 | 0.32 (0.20–0.49) | 0.001* | 0.29 (0.31–1.23) | 0.292 |
| With family/relatives | 175 | 44 | 1 | 1 | ||
| Social support | ||||||
| No | 181 | 93 | 0.68 (0.43–1.08) | 0.101 | 0.50 (0.28–1.64) | 0.126 |
| Yes | 100 | 35 | 1 | 1 | ||
| Chronic illness | ||||||
| No | 189 | 114 | 1 | 1 | ||
| Yes | 92 | 14 | 3.96 (2.16–7.28) | 0.001* | 2.18 (1.23–4.31) | 0.009* |
| Current substance use | ||||||
| Alcohol | 122 | 36 | 2.62 (1.62–4.25) | 0.001* | 1.48 (0.78–2.82) | 0.251 |
| Tobacco | 19 | 4 | 3.68 (1.20–11.29) | 0.023* | 1.96 (0.53–7.27) | 0.308 |
| Caffeine | 47 | 16 | 2.27 (1.19–4.34) | 0.013* | 1.86 (0.88–3.94) | 0.152 |
| No current substance use | 93 | 72 | 1 | 1 | ||
| COVID-19 response | ||||||
| Poor response | 91 | 63 | 0.49 (0.32–0.76) | 0.001* | 0.45 (0.35–1.03) | 0.065 |
| Good response | 190 | 65 | 1 | 1 | ||
| COVID-19 preparedness | ||||||
| Poor preparedness | 118 | 73 | 0.55 (0.36–0.83) | 0.005* | 0.50 (0.57–1.70) | 0.996 |
| Good preparedness | 163 | 55 | 1 | 1 | ||
| COVID-19 knowledge | ||||||
| Poor knowledge | 175 | 58 | 1.99 (1.31–3.04) | 0.001* | 1.73 (1.06–2.82) | 0.029* |
| Good knowledge | 106 | 70 | 1 | 1 | ||
COVID-19: coronavirus disease 2019; OR: odds ratio; CI: confidence interval; NGO: nongovernmental organization.
1 = reference; the Hosmer–Lemeshow test = 0.795.
p < 0.05 (in bivariate and multivariate logistic regression analyses).
In addition, study participants who have no formal education, who are married participants, who have one child, who lives alone, who have no social support, and who habituate current substance use (alcohol) were adjusted in multivariable logistic regression for symptoms of depression (Table 4).
Table 4.
Factors associated with symptoms of depression in older adults during COVID-19 at North Shoa Zone, Debre Libanos District, Oromia region, Ethiopia, 2020 (N = 409).
| Variables | Depression | Crude OR (95% CI) | p | Adjusted OR (95% CI) | p | |
|---|---|---|---|---|---|---|
| Yes | No | |||||
| Age | ||||||
| 60–70 | 88 | 96 | 1 | 1 | ||
| 71–80 | 76 | 49 | 1.69 (1.07–2.68) | 0.025* | 1.54 (0.93–2.58) | 0.097 |
| 81–90 | 58 | 13 | 4.87 (2.50–9.49) | 0.001* | 3.43 (1.65–7.13) | 0.001* |
| >90 | 23 | 6 | 4.18 (1.63–10.75) | 0.003* | 2.91 (1.03–8.24) | 0.045* |
| Marital status | ||||||
| Single | 179 | 76 | 1 | 1 | ||
| Married | 66 | 88 | 0.32 (0.21–0.48) | 0.001* | 0.63 (0.36–1.12) | 0.116 |
| Educational status | ||||||
| No formal education | 183 | 105 | 1.66 (1.08–2.55) | 0.021* | 1.27 (0.75–2.15) | 0.378 |
| Formal education | 62 | 59 | 1 | 1 | ||
| Number of children | ||||||
| No children | 62 | 33 | 1.58 (0.95–2.62) | 0.077 | 0.76 (0.35–1.65) | 0.488 |
| One child | 30 | 10 | 2.52 (1.17–5.44) | 0.018* | 1.76 (0.71–4.33) | 0.221 |
| Two children | 46 | 31 | 1.25 (0.73–2.13) | 0.417 | 1.02 (0.55–1.91) | 0.944 |
| More than three children | 107 | 90 | 1 | 1 | ||
| Source of income | ||||||
| Retirement | 10 | 7 | 1 | 1 | ||
| Helped by family | 55 | 19 | 2.03 (0.68–6.07) | 0.207 | 1.31 (0.37–4.67) | 0.678 |
| Farmer | 51 | 71 | 0.50 (0.18–1.41) | 0.191 | 0.72 (0.22–2.40) | 0.594 |
| Merchant | 7 | 13 | 0.38 (0.10–1.43) | 0.151 | 0.37 (0.09–1.66) | 0.198 |
| Supported by NGO | 93 | 42 | 1.55 (0.55–4.35) | 0.405 | 1.44 (0.46–4.58) | 0.528 |
| No income | 29 | 12 | 1.69 (0.52–5.49) | 0.381 | 1.08 (0.29–4.08) | 0.909 |
| Living status | ||||||
| Alone | 131 | 59 | 2.05 (1.36–3.07) | 0.001* | 1.53 (0.80–2.91) | 0.088 |
| With family/relatives | 114 | 105 | 1 | 1 | ||
| Social support | ||||||
| No | 145 | 129 | 0.39 (0.25–0.62) | 0.001* | 0.35 (0.36–0.97) | 0.045* |
| Yes | 100 | 35 | 1 | 1 | ||
| Chronic illness | ||||||
| No | 169 | 134 | 1 | 1 | ||
| Yes | 76 | 30 | 2.01 (1.24–3.25) | 0.004* | 1.90 (1.07–3.38) | 0.030* |
| Current substance use | ||||||
| Alcohol | 86 | 72 | 0.49 (0.31–0.78) | 0.002* | 0.88 (0.48–1.60) | 0.676 |
| Tobacco | 15 | 8 | 0.77 (0.31–1.93) | 0.577 | 0.70 (0.38–3.71) | 0.774 |
| Caffeine | 36 | 27 | 0.55 (0.30–1.00) | 0.263 | 0.43 (0.22–1.85) | 0.115 |
| No current substance use | 117 | 48 | 1 | 1 | ||
COVID-19: coronavirus disease 2019; OR: odds ratio; CI: confidence interval; NGO: nongovernmental organization.
1 = reference; the Hosmer–Lemeshow test = 0.638.
p < 0.05 (in bivariate and multivariate logistic regression analyses).
Female participants were 1.40 times more likely to have anxiety than male participants (adjusted odds ratio (AOR) = 1.40, 95% CI = (1.06–2.94)). The older adults who have the chronic disease were two times more likely to have anxiety compared to those who did not have the chronic disease (AOR = 2.18; 95% CI = (1.23–4.31)). The study participants who have poor knowledge of the COVID-19 pandemic were two times more likely to have anxiety than a good knowledge of the COVID-19 pandemic (AOR = 1.73; 95% CI = (1.06–2.82)) (Table 3).
Again, the study participants whose age category 81 to 90 were three times more likely to have depression than the age category of 60 to 70 (AOR = 343; 95% CI = (1.65–7.13)). Older adults whose age category greater than 90 years were two times more likely to develop symptoms of depression than the age category of 60 to 70 (AOR = 2.91; 95% CI = (1.03–8.24)). The older adults who have the chronic disease were two times more likely to have symptoms of depression compared to those who have no chronic diseases (AOR = 1.90; 95% CI = (1.07–3.38)), and older adults who have no social support were also associated with symptoms of depression (Table 4).
Discussion
The COVID-19 pandemic has been exposing people to anxiety and depression, especially at-risk groups like older adults. We found a higher depression and anxiety in older adults during the COVID-19 pandemic in the North Shoa Zone compared to the study done in Ethiopia before the COVID-19 pandemic.26 This finding also identified factors associated with anxiety and depression that are important for potential intervention targeted at psychological distress, anxiety, and depression for the community older adults in low-resource countries.
Of the study participants, 59.9% had depression symptoms, which was higher than studies conducted during the COVID-19 pandemic in Germany (14.3%),35 Spain (25.3%),36 China (37.1%),37 and London, the United Kingdom (12.8%)38 that older adults had symptoms of depression. On the contrary, our result is lower than the study done in Greece that 81.6% of older adults reported symptoms of depression.39 Various conditions may aggravate the symptoms of depression, including loneliness, reduced social connectivity, coexisting illness with increasing age,38 fear of high morbidity and mortality of the COVID-19 infections,40 and isolated at home and poor exposure to the health care system.41 The deference may be also due to differences in instrument and study area, and lack of adequate social support environment during COVID-19 in our findings.
The impact of the COVID-19 pandemic on older adults induced anxiety symptoms, which positively affect physical health, increase agitation, and lead to suicidal ideation and attempt.42,43 We found that 68.7% of the study participants had self-reported symptoms of anxiety. It is higher than the study conducted in Germany (44.9%),35 Spain (15.9%),36 China (37.1%),37 and London, the United Kingdom (12.3%).38 Conversely, the study in Greece found higher prevalence (84.5%) than our study findings.39 The reason for the discrepancy is explained by the difference in screening tools and study area that Europe and other developed countries are more affected by the COVID-19 pandemic.3
This study demonstrates that more than half of older adults had good COVID-19 preparedness (53.3%) and good response to COVID-19 prevention (62.3%). The current COVID-19 pandemic represents a major threat to older adults due to their coexisting health condition, having declined immunity, and high risk of infectious exposures.44 Because of this fact, the majority of older adults had better preparedness and response for the prevention of the COVID-19 pandemic. Even though the older adults responded for the prevention of COVID-19 infection according to WHO recommendation, this finding is lower than the studies conducted in the United States,45 Iran,32 and China.31 This difference may be explained that, in our study area, most of the older adults have been supported financially by different volunteers and nongovernmental organizations, which might be limited during lockdown to have enough support for COVID-19 preparedness and prevention measures.
In this study, the majority (57.0%) of older adults had poor knowledge of the COVID-19 pandemic, and having poor knowledge was significantly associated with symptoms of anxiety. This study result is higher than the study reported in China that revealed 41.8% of the study participants had below the level of cut points.33 Conversely, 54.0% of older adults had a positive attitude toward the COVID-19 pandemic, which was lower than the study reported in China (86.7%).33 This difference may be explained by the difference in the study area—instruments used and the study participants’ knowledge and perception of the COVID-19 pandemic in our study area.
We found that advanced age (age category of 81–90 and above 90) was more likely to develop symptoms of depression. It is comparable with the study conducted in the United Kingdom and Vietnam, which reported as the age of elders increases, the level of depression symptoms also increases.38,46 A study conducted in China also indicated that with increasing age, depression and anxiety also increase.47 This is because as the age increases, the risk of coping with COVID-19 decreases and makes the older adults worry more and lead to depression.
In this study, female participants were more significantly associated with symptoms of anxiety compared to male participants. A study conducted in Germany, in which female study participants reported higher mental burden,35 is comparable with other studies, in which the prevalence of anxiety is higher in women than men.37,47–51 Women are more susceptible to suffering anxiety symptoms or posttraumatic stress disorder following a stressful event.52 Study documented that lack of support, being loneliness, living alone, and alcohol consumption were contributors to differences between men and women that reported aggravation of anxiety symptoms.38
In our study, one-fourth (25.9%) of older adults have chronic diseases that were significantly associated with symptoms of anxiety and depression. It is in line with other studies in which medical history and chronic illnesses were positively associated with increased symptoms of anxiety and depression.37,53–55 This might be due to people who have chronic diseases and are also suffering from poor health may feel more vulnerable to a new disease, which confuses them and in turn causes symptoms of anxiety and depression during the COVID-19 pandemic.56
In addition, more than two-thirds of study participants had no social support. The presence of social support is very important for improving loneliness and good progress of medication adherence that can reduce symptoms of anxiety and depression.55 We found that older adults who have no social support were significantly associated with symptoms of depression. It is comparable with the study results in China that found people who had less social support were more likely to develop symptoms of depression.47 The reason behind this fact is that social isolation and loneliness were associated with worse mental health outcomes that lead to symptoms of stress, anxiety, and depression.57
Limitation of the study
This study was limited to the Debre Libanos District, which cannot be generalizable to the rest of the regions of Ethiopia, and the lack of temporality ascertainment due to its cross-sectional nature. The limited number of published articles during the COVID-19 pandemic regarding anxiety and depression among older adults in the low-resource countries had made the discussion challenging.
Conclusion
The symptoms of anxiety and depression among the older adult population during COVID-19 were high. Female participants, having a chronic disease and having poor knowledge of the COVID-19 pandemic, were significantly associated with anxiety symptoms. Age category of 81 to 90 and above 90, lack of social support, and having the chronic disease were significantly associated with symptoms of depression. The higher prevalence of anxiety and depression and associated factors in older adults were evidence points for developing a psychological intervention to tackle the older adults’ mental health needs during the COVID-19 pandemic. The Ethiopian Ministry of Health should give attention to strengthening the mental health gap through health extension workers for older adults who live in the community during and after the COVID-19 pandemic.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121211040050 for Anxiety and depression symptoms in older adults during coronavirus disease 2019 pandemic: A community-based cross-sectional study by Kemal Jemal, Tinsae Abeya Geleta, Berhanu Senbeta Deriba and Mukemil Awol in SAGE Open Medicine
Acknowledgments
The authors acknowledge the study participants for their cooperation.
Footnotes
Author contributions: K.J. conceived the study, involved in the study design and report writing, and reviewed, analyzed, and drafted the article. B.S.D., T.A.G., and M.A. contributed to data analysis and report writing, drafted the manuscript, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Salale University funds this research work. The funders had no role in study design, data collection, analysis, decision to publish, or manuscript preparation.
Availability of data and material: The datasets generated and/or analyzed during the current study are not publicly available. The sharing of data was not included in the approval from the ethics committee but is available from the corresponding author on a reasonable request.
Ethical approval and consent to participate: The study protocol, methods and consent form were approved by the Salale University Ethical Review Committee on 24 July 2020 Re. No. 025/2020. After thoroughly discussing the study’s ultimate purpose and method, written consent was sought from the North Shoa Zonal Health Bureau/Woreda Department. We have obtained written informed consent from participants below 90 years as they have the decisional capacity. Assent was obtained from parents/guardians for participants above 90 years old. The respondents were informed that their inclusion in the study is voluntary, and they are free to withdraw from the study if they are not willing to participate. If they do not want to answer any question, they have the right to do so. To ensure the confidentiality of respondents, their names were excluded from the questionnaire. The confidentiality of the respondents was kept.
ORCID iDs: Kemal Jemal  https://orcid.org/0000-0001-8922-1827
https://orcid.org/0000-0001-8922-1827
Berhanu Senbeta Deriba  https://orcid.org/0000-0002-4282-1427
https://orcid.org/0000-0002-4282-1427
Supplemental material: Supplemental material for this article is available online.
References
- 1.Du R-H, Liang L-R, Yang C-Q, et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARS-CoV-2: a prospective cohort study. Eur Respir J 2020; 55(5): 2000524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zhai P, Ding Y, Wu X, et al. The epidemiology, diagnosis and treatment of COVID-19. Int J Antimicrob Agents 2020; 55: 105955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO). Coronavirus disease (COVID-19) outbreak situation. Coronavirus disease (COVID-19) pandemic, 2020, https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed 29 March 2020).
- 4.Gebremariam BM, Shienka KL, Kebede BA, et al. Epidemiological characteristics and treatment outcomes of hospitalized patients with COVID-19 in Ethiopia. Pan Afr Med J 2020; 37(suppl. 1): 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Armitage R, Nellums LB.COVID-19 and the consequences of isolating the elderly. Lancet Public Health 2020; 5(5): e256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization (WHO). Mental health and psychosocial considerations during the COVID-19 outbreak. Geneva: WHO, 2020. [Google Scholar]
- 7.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395: 1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perez-Saez J, Lauer SA, Kaiser L, et al. Serology-informed estimates of SARS-CoV-2 infection fatality risk in Geneva, Switzerland. Lancet Infect Dis 2021; 21(4): e69–e70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Javed B, Sarwer A, Soto EB, et al. The coronavirus (COVID-19) pandemic’s impact on mental health. Int J Health Plann Manage. Epub ahead of print 22 June 2020. DOI: 10.1002/hpm.3008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID-19. The COVID-19 resource centre is hosted on Elsevier Connect, the company’s public news and information website, 2020. [Google Scholar]
- 11.Gustavsson J, Beckman L.Compliance to recommendations and mental health consequences among elderly in Sweden during the initial phase of the COVID-19 pandemic—a cross sectional online survey. Int J Environ Res Public Health 2020; 17(15): 5380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Abdela SG, Abegaz SH, Demsiss W, et al. Clinical profile and treatment of COVID-19 patients: experiences from an Ethiopian treatment center. Am J Trop Med Hyg 2020; 104: 532–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abrahim SA, Tessema M, Defar A, et al. Time to recovery and its predictors among adults hospitalized with COVID-19: a prospective cohort study in Ethiopia. PLoS One 2020; 15(12): e0244269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rowe TA, Patel M, O’Conor R, et al. COVID-19 exposures and infection control among home care agencies. Arch Gerontol Geriatr 2020; 91: 104214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deriba BS, Geleta TA, Beyane RS, et al. Patient satisfaction and associated factors during COVID-19 pandemic in North Shoa health care facilities. Patient Prefer Adherence 2020; 14: 1923–1934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.El Hayek S, Cheaito MA, Nofal M, et al. Geriatric mental health and COVID-19: an eye-opener to the situation of the Arab countries in the Middle East and North Africa Region. Am J Geriatr Psychiatry 2020; 28: 1058–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gorrochategi MP, Munitis AE, Santamaria MD, et al. Stress, anxiety, and depression in people aged over 60 in the COVID-19 outbreak in a sample collected in Northern Spain. Am J Geriatr Psychiatry 2020; 28: 993–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kowal P, Dowd JE.Definition of an older person. Proposed working definition of an older person in Africa for the MDS Project. Geneva: World Health Organization, 2001. [Google Scholar]
- 19.Gazeta FN. A proclamation to provide for the public servants’ pension. Proclamation no. 714/2011, 2011. Addis Ababa. [Google Scholar]
- 20.Spitzer RL, Kroenke K, Williams JB, et al. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 2006; 166(10): 1092–1097. [DOI] [PubMed] [Google Scholar]
- 21.Nyongesa MK, Mwangi P, Koot HM, et al. The reliability, validity and factorial structure of the Swahili version of the 7-item generalized anxiety disorder scale (GAD-7) among adults living with HIV from Kilifi, Kenya. Ann Gen Psychiatry 2020; 19: 62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dadi AF, Dachew BA, Kisi T, et al. Anxiety and associated factors among prisoners in North West of Amhara Regional State, Ethiopia. BMC Psychiatry 2016; 16(1): 83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Necho M, Birkie M, Gelaye H, et al. Depression, anxiety symptoms, Insomnia, and coping during the COVID-19 pandemic period among individuals living with disabilities in Ethiopia, 2020. PLoS One 2020; 15(12): e0244530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kassaw C, Pandey D.COVID-19 pandemic related to anxiety disorder among communities using public transport at Addis Ababa, Ethiopia, March 2020: cross-sectional study design. Hu Arenas. Epub ahead of print 4 January 2021. DOI: 10.1007/s42087-020-00166-y. [DOI] [Google Scholar]
- 25.Sheikh JI, Yesavage JA.Geriatric Depression Scale (GDS): recent evidence and development of a shorter version. Clin Gerontol 1986; 5: 165–173. [Google Scholar]
- 26.Mirkena Y, Reta MM, Haile K, et al. Prevalence of depression and associated factors among older adults at Ambo town, Oromia region, Ethiopia. BMC Psychiatry 2018; 18(1): 338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Habte E, Tekle T.Cognitive functioning among elders with symptoms of depression: the case of two selected institutionalized care centers in Addis Ababa, Ethiopia. Health Sci J 2018; 12(3): 571. [Google Scholar]
- 28.Boey KW.The use of GDS-15 among the older adults in Beijing. Clin Gerontol 2000; 21(2): 49–60. [Google Scholar]
- 29.Abiola T, Udofia O, Zakari M.Psychometric properties of the 3-item Oslo Social Support Scale among clinical students of Bayero University Kano, Nigeria. Malays J Psychiatry 2013; 22(2): 32–41. [Google Scholar]
- 30.Geleta TA, Deriba BS, Beyane RS, et al. COVID-19 pandemic preparedness and response of chronic disease patients in public health facilities. Int J Gen Med 2020; 13: 1011–1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhong B-L, Luo W, Li H-M, et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int J Biol Sci 2020; 16(10): 1745–1752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Erfani A, Shahriarirad R, Ranjbar K, et al. Knowledge, attitude and practice toward the novel coronavirus (COVID-19) outbreak: a population-based survey in Iran. Bull World Health Organ. Epub ahead of print 30 March 2020. DOI: 10.2471/BLT.20.256651. [DOI] [Google Scholar]
- 33.Lin Y, Hu Z, Alias H, et al. Knowledge, attitudes, impact, and anxiety regarding COVID-19 infection among the public in China. Front Public Health 2020; 8: 236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sperandei S.Understanding logistic regression analysis. Biochem Med 2014; 24(1): 12–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bäuerle A, Teufel M, Musche V, et al. Increased generalized anxiety, depression and distress during the COVID-19 pandemic: a cross-sectional study in Germany. J Public Health 2020; 42: 672–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.García-Fernández L, Romero-Ferreiro V, López-Roldán PD, et al. Mental health in elderly Spanish people in times of COVID-19 outbreak. Am J Geriatr Psychiatry 2020; 28(10): 1040–1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Meng H, Xu Y, Dai J, et al. Analyze the psychological impact of COVID-19 among the elderly population in China and make corresponding suggestions. Psychiatry Res 2020; 289: 112983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Robb CE, De Jager CA, Ahmadi-Abhari S, et al. Associations of social isolation with anxiety and depression during the early COVID-19 pandemic: a survey of older adults in London, UK. Front Psychiatry 2020; 11: 591120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Parlapani E, Holeva V, Nikopoulou VA, et al. Intolerance of uncertainty and loneliness in older adults during the COVID-19 pandemic. Front Psychiatry 2020; 11: 842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kang S-J, Jung SI.Age-related morbidity and mortality among patients with COVID-19. Infect Chemother 2020; 52(2): 154–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Steinman MA, Perry L, Perissinotto CM.Meeting the care needs of older adults isolated at home during the COVID-19 pandemic. JAMA Intern Med 2020; 180(6): 819–820. [DOI] [PubMed] [Google Scholar]
- 42.Bergman YS, Cohen-Fridel S, Shrira A, et al. COVID-19 health worries and anxiety symptoms among older adults: the moderating role of ageism. Int Psychogeriatr 2020; 32(11): 1371–1375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sher L.The impact of the COVID-19 pandemic on suicide rates. QJM 2020; 113(10): 707–712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Morley JE, Vellas B.COVID-19 and older adult. Berlin; Heidelberg: Springer, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Berg-Weger M, Morley JE.Loneliness and social isolation in older adults during the COVID-19 pandemic: implications for gerontological social work. Berlin; Heidelberg: Springer, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dao ATM, Nguyen VT, Nguyen HV, et al. Factors associated with depression among the elderly living in urban Vietnam. Biomed Res Int 2018; 2018: 2370284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Kong X, Zheng K, Tang M, et al. Prevalence and factors associated with depression and anxiety of hospitalized patients with COVID-19, 2020, https://www.medrxiv.org/content/10.1101/2020.03.24.20043075v2
- 48.Moghanibashi-Mansourieh A.Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J Psychiatr 2020; 51: 102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhou S-J, Zhang L-G, Wang L-L, et al. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur Child Adolesc Psychiatry 2020; 29(6): 749–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Liu D, Ren Y, Yan F, et al. Psychological impact and predisposing factors of the coronavirus disease 2019 (COVID-19) pandemic on general public in China. Epub ahead of print 7 March 2020. DOI: 10.2139/ssrn.3551415. [DOI] [Google Scholar]
- 51.Wang Y, Di Y, Ye J, et al. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med 2021; 26: 13–22. [DOI] [PubMed] [Google Scholar]
- 52.Sareen J, Erickson J, Medved MI, et al. Risk factors for post-injury mental health problems. Depress Anxiety 2013; 30(4): 321–327. [DOI] [PubMed] [Google Scholar]
- 53.Mazza C, Ricci E, Biondi S, et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res Public Health 2020; 17(9): 3165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Holmes EA, O’Connor RC, Perry VH, et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 2020; 7: 547–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health 2020; 17(5): 1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hatch R, Young D, Barber V, et al. Anxiety, depression and post traumatic stress disorder after critical illness: a UK-wide prospective cohort study. Crit Care 2018; 22(1): 310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Leigh-Hunt N, Bagguley D, Bash K, et al. An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 2017; 152: 157–171. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121211040050 for Anxiety and depression symptoms in older adults during coronavirus disease 2019 pandemic: A community-based cross-sectional study by Kemal Jemal, Tinsae Abeya Geleta, Berhanu Senbeta Deriba and Mukemil Awol in SAGE Open Medicine


