Abstract
Objectives:
To evaluate whether a fall prevention intervention reduces fall risk in older adults who have previously fallen.
Design:
Randomized controlled pilot trial.
Setting:
Participants’ homes.
Intervention:
LIVE-LiFE, adapted from Lifestyle-Intervention Functional Exercise (LiFE) integrates strength and balance training into daily habits in eight visits over 12 weeks. The adaptations to LiFE were to also provide (a) US$500 in home safety changes, (b) vision contrast screening and referral, and (c) medication recommendations. Control condition consisted of fall prevention materials and individualized fall risk summary.
Measurement:
Timed Up and Go (TUG) and Tandem stand. Falls efficacy, feasibility, and acceptability of the intervention.
Results:
Sample (N = 37) was 65% female, 65% White, and average 77 years. Compared with the control group, each outcome improved in the intervention. The LIVE-LiFE intervention had a large effect (1.1) for tandem stand, moderate (0.5) in falls efficacy, and small (0.1) in the TUG.
Conclusion:
Simultaneously addressing preventable fall risk factors is feasible.
Keywords: accidental falls, lifestyle-integrated exercise, community-dwelling, home hazards, medication review
Introduction
Falls are the leading cause of fatal and nonfatal injuries among individuals aged 65 years and older (Centers for Disease Control and Prevention [CDC], National Center for Injury Prevention and Control, 2019; Sterling et al., 2001). Falls sequelae include hip fractures, loss of independence, and fall-related mortality which has increased 30% from 2007 to 2016 for older adults, even controlling for population aging (Burns & Kakara, 2018). Besides the cost of human suffering, medical expenses for falls total more than US$50 billion per year (Florence et al., 2018).
The multifactorial causes for falls are well known. Less understood is how to meaningfully intervene. Exercise, such as strength and balance training, is effective in preventing falls but only 20% of individuals with fall risks participate in exercise fall prevention programs (Casteel et al., 2018; Christmas & Andersen, 2000) and, for those who do participate, adherence levels vary (Malik et al., 2020; Nyman & Victor, 2012). This low participation suggests the importance of seeking new ways to engage older adults in fall prevention exercise such as integrating fall prevention movements into incidental exercise (Weber et al., 2018). Recent knowledge from neuroscience and behavioral science tells us that changing habits require multiple daily cues building from intrinsic motivation (Clemson & Munro, 2017; Smith & Graybiel, 2016). The Lifestyle-Intervention Functional Exercise (LiFE) intervention is a novel evidence-based fall prevention approach which does exactly that. An occupational therapist (OT) assesses a person’s daily routines to design strength and balance exercises that are then integrated into daily activities, such as bending from the knees while unloading the dishwasher or standing in tandem (on one heel to the next toe) while brushing teeth (Clemson et al., 2014). Tested in a randomized control trial in Australia, the LiFE intervention decreased the number of falls in a sample of older adults who had previously fallen compared with a structured exercise program (Clemson et al., 2012). This intervention has not been tested in the U.S. context nor expanded to address other fall risk factors.
Beyond decreased strength and balance which exercise addresses, falls can be caused by other risks such as home hazards (e.g., uneven flooring or lack of banisters), polypharmacy (especially when drugs cause dizziness or sedation), and decreased ability to see contrast (such as between stairs and rug). Therefore, when we adapted LiFE to the U.S. context, we also added: (a) home modifications to remove hazards and to allow safe and confident performance of daily tasks, (b) identification of medications that put participants at increased fall risk and working with prescribers to change treatment, and (c) vision contrast screening and referral (Florence et al., 2018; Guirguis-Blake et al., 2018; Stevens & Burns, 2015). To our knowledge, there is no intervention that addresses these multiple fall risks, is tailored to the individual, and addresses adherence challenges.
The purpose of this single-blind, two-group pilot trial was to test feasibility and acceptability and obtain initial effect sizes of the intervention’s effect on objective measures of balance and strength and subjective perceptions of falls efficacy.
Method
The process for deriving adaptations for the LiFE program and the resultant Live-LiFE protocol is detailed elsewhere (Granbom et al., 2019). Figure 1 outlines the design and timeline of the pilot trial.
Figure 1.
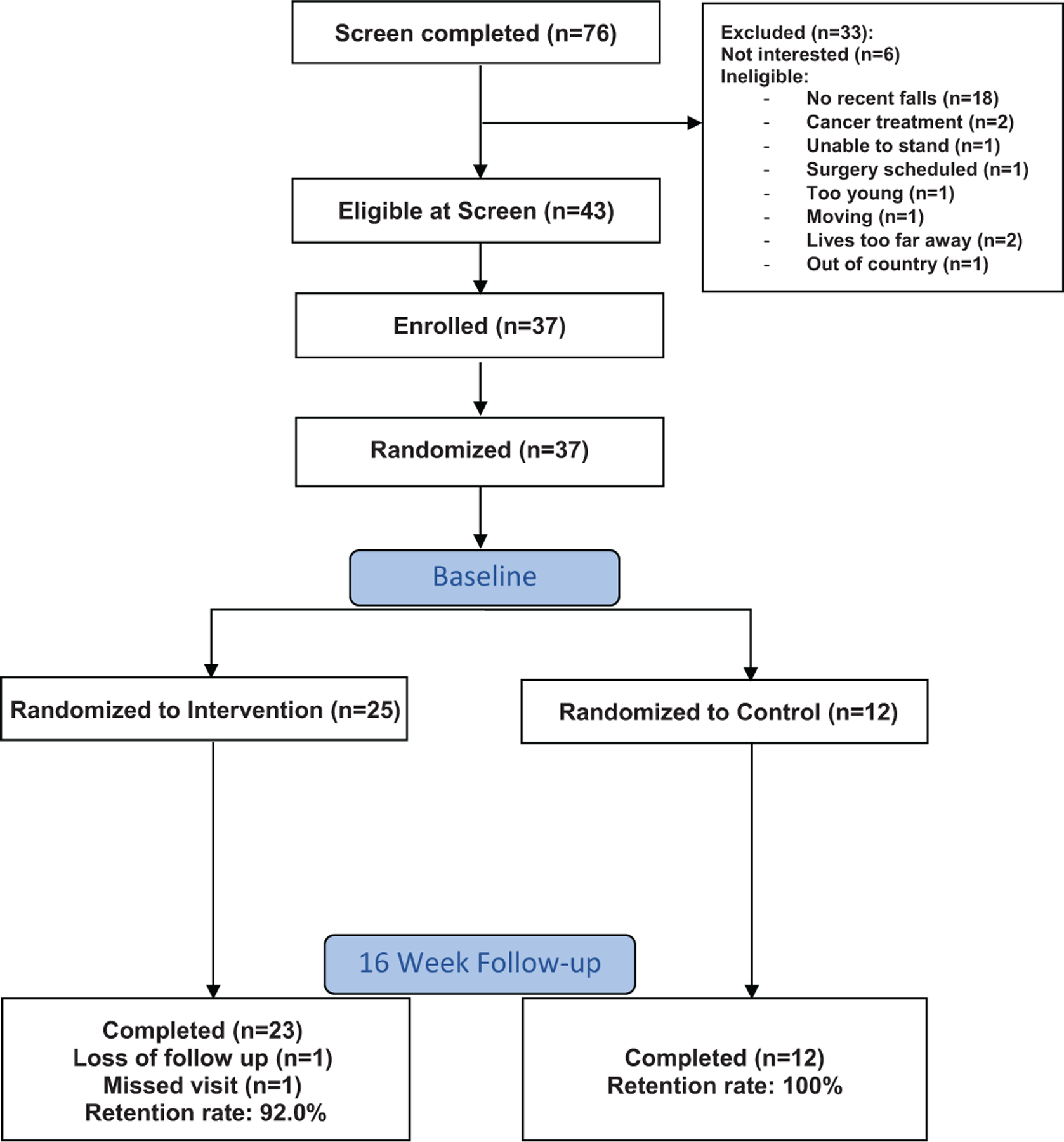
LIVE-LiFE consort diagram.
Recruitment and Randomization
The sample was recruited from multiple sources including flyers in senior housing and studies for which participants had been ineligible or participated in the control group. After receiving letters inviting participation, interested older adults were screened by telephone for fall history, age and then were further screened at an in-person visit for cognitive function and ability to stand. Eligible participants were community-dwelling people aged 70 or older who reported two or more falls or one injurious fall in the past 12 months. Exclusion criteria included moderate to severe cognitive problems based on the Short Portable Mental Status Questionnaire (Pfeiffer, 1975), no conversational English, inability to stand, resident in a nursing home or assisted living facility, hospitalized more than 3 times in the last year, or having a terminal diagnosis (<1 year expected survival or getting active cancer treatment). Trained evaluators assessed recruited persons who provided informed consent at baseline; participants were then randomized to treatment or control. Evaluators masked to study assignment reassessed all participants at 16 weeks (Figure 1).
Randomization was computer generated with a block size of six. Upon enrollment, the study coordinator was provided intervention or control assignment from a non-study staff member who retained the computer-generated assignment scheme. We used a 2:1 allocation ratio for intervention and control which allowed us to better observe variability in intervention implementation for planning future research, while still providing similar power for preliminary between-group comparisons.
The LIVE-LiFE intervention.
The intervention consists of four components and was delivered by an OT, with referral to a pharmacist and vision specialist as needed. The first component was the LiFE intervention which involves learning and then integrating eight static and dynamic balance and six strength (hip, knee, and ankle) exercises into daily activities. The OT and participant collaborated to determine how best to integrate these exercises into their daily routines based on their own goals and schedules of activities. For example, participants learned to practice balance exercises while they were in a checkout line at a store, reduce their base of support to a tandem stand when folding laundry at home, squat every time they closed a drawer, or stand on toes to reach a mug in a cupboard (see quotations in Table 3). These exercises were tailored to the capacity of the person and upgraded slowly over time. The goal was to have daily activities trigger the use of exercises while carrying out the activities to build habits that in turn could maximize adherence.
Table 3.
Sample Enactment Responses From Intervention Participants of Each Component.
| Domain | |
|---|---|
| Exercising in daily activities | “I was waiting in line to get my medicine and all the sudden I realized I was standing in a tandem stand. I was shocked. I didn’t even know I was doing it.” Woman, 81 years old |
| Effect of exercises | “I turned around and caught my foot in the rug. I started going down and I thought this was going to be bad, but I caught myself. I thought, these exercises must be working. Before this program, I would not have caught myself.” Woman, 74 years old |
| Vision screening | “I took the vision letter to my provider and he says I am developing cataracts. He says to check back in a year because eventually I will need surgery. If there is a measure to improve my vision, I will.” Man, 80 years old |
| Home safety additions | “I almost fell in the shower and I don’t normally fall there. I was able to grab onto the grab bars to stop me.” Woman, 76 years old, who got grab bars installed in shower |
OTs are licensed to modify activity based on physical function and in fall prevention. They specialize in graded activity analysis to find the right challenge for participants. The intervention was delivered by an OT who had been trained in all components and conceptual underpinnings. The LiFE program is personally tailored to participants’ baseline activity levels. Activities are introduced in incremental steps with consideration for ability and opportunity to embed in daily routines. We expected the intervention to be safe because the original LiFE trial of 317 people older than 70 with a recent fall had only one adverse event and it was not study related. In this pilot study, there were no adverse events.
LIVE-LiFE also includes an overall motivational goal identified by the older adult that links the exercise to a personal goal they wanted to achieve. These goals, for example, to be able to go out more easily or reach for kitchen items without falling, were written on a whiteboard located on their refrigerator or other location that was visually accessible. Participants used the same whiteboard to keep track of exercises performed.
Occupational therapy home visits took place in eight 1-hr visits over 12 weeks: approximately once per week in Weeks 1 to 6 and in Week 8 and a booster visit at Week 12. The visits included checking in about the progress of what the participant chose to integrate into their habits and adjusting difficulty or brainstorming other activities to use if necessary. The 12-week booster visit is intended to boost the motivation of the participant and to modify the exercises by upgrading or making more challenging or other modification if appropriate and desired by the participant. Participants self-monitored their exercises using the goal whiteboard.
The second intervention component was modifying home safety hazards (Szanton et al., 2019). The OT assessed the home for fall risk using the Home Safety Self-Assessment Tool (HSSAT). The OT then worked with the participant to identify fall hazards and problem-solve environmental and behavioral solutions. Together, they prioritized home repairs and adaptations and agreed on which safety modifications were implemented by a licensed handyperson. Up to US$500 for parts and labor combined was provided as part of the study and with no cost to the participant.
The third intervention component was medication review. A list of all prescribed and over-the-counter medications obtained by the baseline data interviewer through a brown bag review was sent to a collaborating pharmacist for those in the intervention group. The pharmacist evaluated medications and medication combinations which place participants at heightened risk of falls (Fick et al., 2019). For any medications or medication combinations that increased the participant’s fall risk, the pharmacist provided a written assessment of the participant’s medication regimen for the participant to give to his or her primary care provider. The assessment also included recommendations for medication regimen changes that would decrease the risk of falls. The OT followed up with each participant to encourage that the list be shared with his or her primary care provider.
The fourth intervention component was a vision contrast screening using the Mars Letter Contrast Sensitivity Test (Dougherty et al., 2005) which can be performed anywhere with adequate light. Intervention participants who scored in the risky category of the Mars were provided a letter at the first visit to give to their primary care provider or optician and then asked about follow-up at the third visit.
Control condition.
After randomization, the control group received a letter with their scores on the fall risk assessment to bring to their primary care providers. They also received a CDC pamphlet about fall prevention which included steps to take to reduce their fall risk (CDC, 2005, 2019).
Measures
Data collectors masked to treatment assignment obtained assessments at baseline (T0) and after pilot trial completion at approximately 16 weeks (T1).
Primary outcomes.
The objective Timed Up and Go (TUG) was gathered in continuous seconds by measuring the time taken for a participant to rise from a chair, walk 3 m, turn, return to the chair, and sit down with their cane or other assistive device if needed. The TUG is a predictor of falls in those with lower functioning such as the participants in our sample (Schoene et al., 2013).
Tandem stand is the time a participant can stand with one foot directly in front of the other, touching heel to toe. If an older adult cannot hold the tandem for 10 s, they are considered at high risk of falls (Guralnik et al., 1994). Tandem stand was measured continuously (number of seconds held) and dichotomously (whether or not participant was able to hold for 10 s).
Secondary outcomes.
Falls efficacy was measured with the Tinetti Falls Efficacy Scale which measures self-report of confidence on a scale of 1 to 10 in doing each of the following 10 activities without falling: cleaning house, getting dressed and undressed, preparing simple meals, bathing, shopping, getting into or out of a chair, going up and down stairs, walking in their neighborhood, reaching into cabinets or closets, and hurrying to answer the phone (Tinetti et al., 1990). Scores range from 0 to 100 and are measured continuously. The instrument has demonstrated validity and test–retest reliability (Tinetti et al., 1990) and is a strong predictor of future falls (Hadjistavropoulos et al., 2007).
Feasibility, acceptability, and enactment: We examined feasibility with recruitment, retention, and completion rates. We measured study acceptability by examining percentages of people who stayed in each arm of the study. Participants assessed their satisfaction with the LIVE-LiFE program with a 10-item survey including overall benefit, how the program addressed specific functional goals, and whether the program required too much work or effort. Participants could pick 1 of 3 responses for each question: not at all, some, or a great deal. Finally, we measured intervention enactment by asking open-ended questions about use of what they learned in daily life.
Sample Size Calculation and Analysis of Aims
As planned, we recruited 37 participants. At the 16-week follow-up time point, we had 35 participants (23 intervention and 12 control) with outcome data to analyze. Because this was a pilot trial, we were primarily interested in feasibility and preliminary effect size estimation and had not planned to have statistical power to find significant differences between the groups.
Analytic approach: We used intention-to-treat analysis (ITT): all participants were counted in their assigned study group once assignment was made. First, we evaluated the distribution of participants’ baseline characteristics. Then, we compared the balance between the intervention and control groups, using p values from the chi-square test between groups. Next, we examined the baseline fall risk and balance for the participants, using the TUG, Tandem stand, and the Falls Efficacy Scale. For the primary aim, the outcome was improvement in the TUG and Tandem stand balance test between baseline and 16 weeks. Effect sizes were estimated based on Cohen’s d (mean difference in change between the intervention and control groups divided by the pooled standard deviation) after baseline score adjustment. We conducted general linear regression with the change of outcome variables as the dependent variable and the group assignment as the independent variable, controlling for the corresponding baseline test scores for each outcome variables. We obtained the adjusted means and pooled standard deviation of the outcome change from the general linear regression models. The difference per unit change between the intervention and control groups and their p values were also extracted from the regression model. Finally, we evaluated the 16-week satisfaction among the participants. The p values were obtained from the crude association between satisfaction content and study group assignment with linear regression. We conducted all analyses using SAS 9.4® (SAS Institute, Inc., Cary, North Carolina).
Results
The 37 participants were 77.9 (SD = 6.4) years old on average, had a broad range of educational attainment, and were 32% African American, 65% White. Thirty-five percent of the sample were men (Table 1). All participants had fallen at least once in the last year but, at baseline, had strong falls efficacy of 91 of 100 on baseline and 7.5 s (SD = 2.3) of 10 on Tandem stand time and TUG score of 17.2 (SD = 9.7).
Table 1.
Participants’ Characteristics at Study Baseline, LIVE-LiFE, N = 37.
| Total | Intervention | Control | ||
|---|---|---|---|---|
| Characteristics | N = 37 | n = 25 | n = 12 | p value |
| Age at study baseline, years | 77.9 ± 6.4 | 78.5 ± 7.3 | 76.5 ± 3.6 | .39 |
| M ± SD | ||||
| Missing | 1 | 0 | 1 | |
| Education | .11 | |||
| < 12 years | 3 (8.1) | 1 (4.0) | 2 (16.7) | |
| GED or high school (12 years) | 10 (27.0) | 5 (20.0) | 5 (41.7) | |
| More than GED or high school | 24 (64.9) | 19 (76.0) | 5 (41.7) | |
| Race | ||||
| White | 24 (64.9) | 17 (68.0) | 8 (32.0) | .56 |
| Black | 12 (32.4) | 7 (28.0) | 5 (41.7) | .41 |
| Asian | 1 (2.7) | 1 (4.0) | 0 | .48 |
| Sex | .37 | |||
| Male | 13 (35.1) | 10 (40.0) | 3 (25.0) | |
| Female | 24 (64.9) | 15 (60.0) | 9 (75.0) | |
| Income | .01a | |||
| Less than US$21,999 | 9 (24.3) | 3 (12.0) | 6 (50.0) | |
| US$22,000-US$48,999 | 14 (37.8) | 9 (36.0) | 5 (41.7) | |
| US$49,000 or more | 14 (37.8) | 13 (52.0) | 1 (8.3) | |
| Residential type | .45 | |||
| House | 28 (75.7) | 18 (72.0) | 10 (83.3) | |
| Apartment | 9 (24.3) | 7 (28.0) | 2 (16.7) | |
| Live alone | .54 | |||
| No | 15 (40.5) | 4 (33.3) | 11 (44.0) | |
| Yes | 22 (59.5) | 8 (66.7) | 14 (56.0) | |
| Total number of home hazards | 18.4 ± 8.5 | 19.0 ± 8.5 | 17.9 ± 8.6 | .49 |
| TUG time | 17.2 ± 9.7 | 17.7 ± 11.4 | 16.2 ± 4.7 | .66 |
| M ± SD | ||||
| Heel to toe stance time | 7.5 ± 3.6 | 8.2 ± 3.2 | 6.0 ± 4.1 | .30 |
| Falls Efficacy Scale (confidence) | ||||
| Summary score | 91.0 ± 12.4 | 92.0 ± 9.7 | 88.9 ± 17.0 | .49 |
Note. TUG = Timed Up and Go.
Statistically significant.
Feasibility and Acceptability Outcomes
Thirty-five of the 37 participants were retained at 16-week follow-up, resulting into a high retention rate of 95%. Figure 2 shows participants’ responses to satisfaction questions. Most participants (97%) found the length of visits appropriate. A significantly higher proportion of participants in the intervention group reported that the study helped to make their home safer compared with those in the control groups (p = .02). Sixty-eight percent of the intervention group answered the intervention had benefited them “a great deal,” 77% said it would benefit others in a similar situation “a great deal,” and 60% answered “a great deal” to it “made my home safer” and “kept me living at home.”
Figure 2.
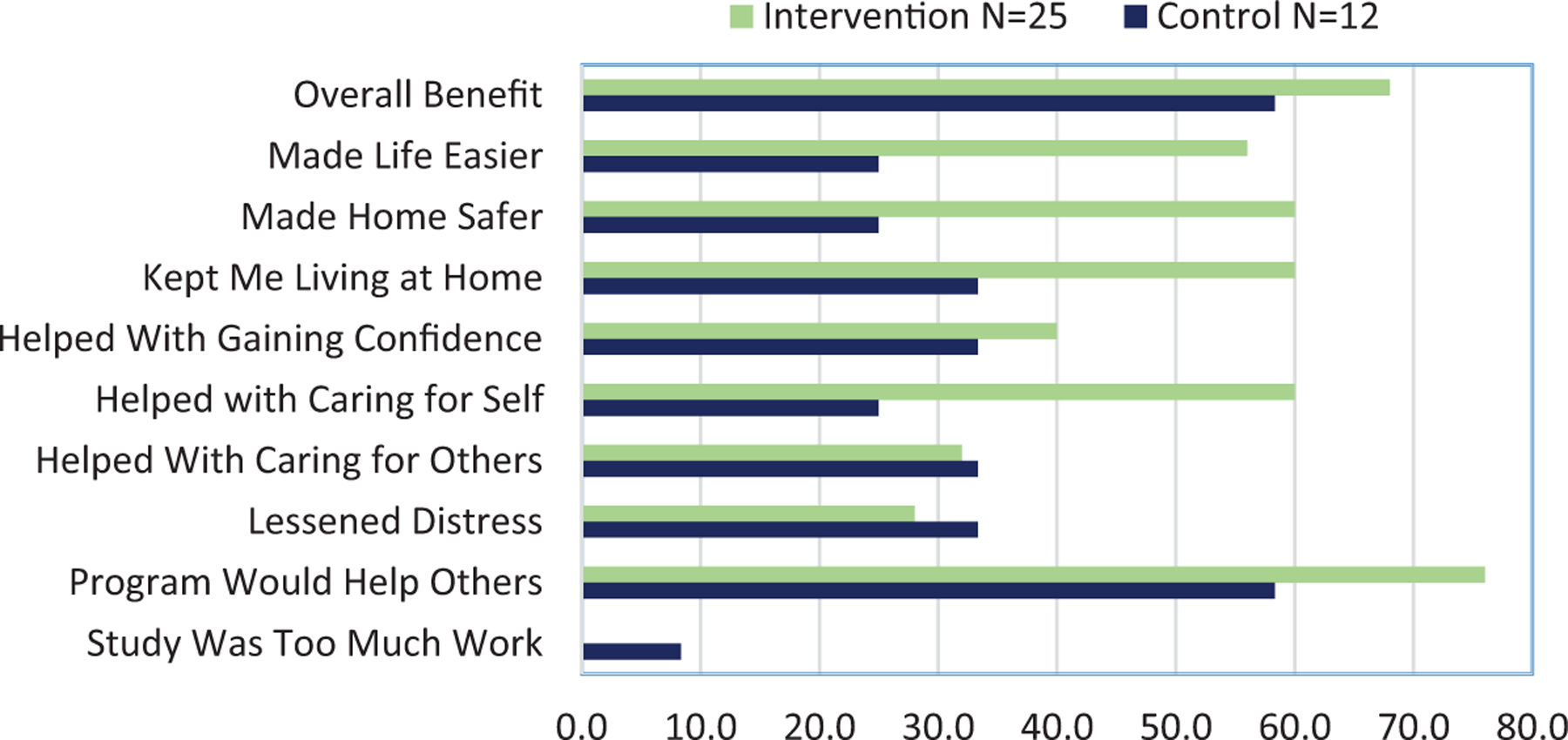
Program satisfaction survey responses by intervention and control.
Note. Percentage responding with “a great deal” for each item.
Initial Effect Sizes
All fall-related measures improved from baseline to 16-week follow-up in the intervention group but not in the control group. These improvements include the primary outcomes of TUG and the tandem stand test and secondary outcome of falls efficacy. The effect sizes evaluated by Cohen’s d range from small (TUG at 0.1) to large (Tandem at 1.1) for the physical performance measures and were moderate for subjective confidence (falls efficacy at 0.5; Table 2). There was a statistically significant difference between the groups in tandem stand time (p = .02; Table 2). Table 3 displays sample enactment quotations relating to each program component.
Table 2.
Adjusted Effects on Outcome Changes Controlling for Baseline Test Scores, N = 37.
| Mean ± SD | M ± SD | Adjusted differencea | Standardized effect sizeb | p value | |
|---|---|---|---|---|---|
| Baseline | 16 weeks | ||||
| TUG | −0.7 | −0.11 | .76 | ||
| LIVE-LiFE | 17.7 ± 11.4 | 20.4 ± 17.4 | |||
| Control | 16.2 ± 4.7 | 18.8 ± 8.5 | |||
| Heel to toe time | 3.2 | 1.13 | .02 | ||
| LIVE-LiFE | 8.2 ± 3.2 | 9.3 ± 1.6 | |||
| Control | 6.0 ± 4.1 | 5.2 ± 4.4 | |||
| Falls Efficacy Scale | 3.2 | 0.48 | .19 | ||
| LIVE-LiFE | 92.0 ± 9.7 | 93.6 ± 9.1 | |||
| Control | 88.9 ± 17.0 | 88.3 ± 15.0 | |||
Note. TUG = Timed Up and Go.
Difference (Intervention − Control) in change scores (16 weeks − Baseline) adjusted for baseline scores.
Adjusted difference divided by the pooled standard deviation.
Discussion
In this pilot study, we found that the LIVE-LiFE intervention was feasible and acceptable to most study participants. We estimated a strong effect size on one objective measure of fall risk (tandem stand time), a small effect on another (TUG), and moderate effect on falls efficacy in a group of older adults who had previously fallen compared with a control condition. The present findings are important because falls, while preventable, have interrelated risk factors that are often unaddressed. A recent Cochrane review found that the evidence base for multicomponent fall prevention trials is slim but that they “probably reduce that rate at which people fall” (Hopewell et al., 2018). This intervention, once further tested for efficacy, has the potential to add conclusively to that evidence.
There are several ways in which this pilot study is innovative. First, new knowledge on pathways to habit formation (Smith & Graybiel, 2016) tells us to build crucial strength and balance fall prevention movements into daily habits. Second, the intervention contains many of the components of the state of-the-art STRIDE fall prevention study (Reuben et al., 2017). This study refers people at fall risk to multiple services as a pragmatic trial but ours was a classic intervention trial providing the multiple components. Third, there is a long history of addressing both the individual (intrinsic) and the environment (extrinsic) factors to improve aging at home (Gitlin et al., 2006; Greenfield, 2012; Szanton et al., 2019) but few such programs directly targeted fall reduction. Because falls are a product of multiple risks, interventions need multiple components to simultaneously address these risks. Moreover, while exercise reduces falls, adherence to exercise regimes is low. This suggests the need to tailor programs and embed their components into older adults’ daily activities versus having stand-alone classes or exercise sessions.
Limitations include that it is a pilot study and is not powered for formal efficacy testing. The current findings are not generalizable to the larger population and the intervention requires additional evaluation. Also, the tandem stand improved the most, but it was also part of the actual intervention training. This improvement may be a result of the actual intervention rather than a general measure of fall risk. However, because tandem stand time is a strong predictor of falls, improving it is an important outcome. Finally, it is possible that the program satisfaction may have been improved by the home modifications. We are unable to test this as we did not have a factorial study design. Strengths of this pilot study include that it extends an already effective fall prevention intervention to include other contributing fall risk including the home environment where most falls occur. A second strength is that the intervention is tailored to each person yet replicable, standardized, and manualized. Third, given that falls are expensive for families and for Medicare, and pervasive in former fallers, this approach has the potential to save costs while improving health.
Conclusion
Addressing the person and environment to reduce the risk of falls continues to have promise. We plan to test this approach in a well-powered efficacy trial that includes fall outcomes and health care utilization.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study is funded by the Centers for Disease Control and Prevention (RF: R49CE002466). The sponsor had no role in conducting the trial, analyzing the data, or writing the paper. The sponsor’s role was limited to funding the trial.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics Statement
The Johns Hopkins Medical Institutions Internal Review Board approved this study (IRB 141297). It was registered as a clinical trial on clinicaltrials.gov (NCT03351413).
References
- Burns E, & Kakara R (2018). Deaths from falls among persons aged ≥65 years—United States, 2007–2016. Morbidity and Mortality Weekly Report, 67(18), 509–514. 10.15585/mmwr.mm6718a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casteel C, Jones J, Gildner P, Bowling JM, & Blalock SJ (2018). Falls risks and prevention behaviors among community-dwelling homebound and non-homebound older adults. Journal of Applied Gerontology, 37, 1085–1106. 10.1177/0733464816672043 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2005). Check for safety: A home fall prevention checklist for older adults. Department of Health and Human Services, Centers for Disease Control and Prevention. [Google Scholar]
- Centers for Disease Control and Prevention. (2019). Stay independent: Learn more about fall prevention. https://www.cdc.gov/steadi/pdf/STEADI-Brochure-StayIndependent-508.pdf
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. (2019). Web-based Injury Statistics Query and Reporting System (WISQARS). https://www.cdc.gov/injury/wisqars/index.html
- Christmas C, & Andersen RA (2000). Exercise and older patients: Guidelines for the clinician. Journal of the American Geriatrics Society, 48(3), 318–324. [DOI] [PubMed] [Google Scholar]
- Clemson L, Fiatarone Singh MA, Bundy A, Cumming RG, Manollaras K, O’Loughlin P, & Black D (2012). Integration of balance and strength training into daily life activity to reduce rate of falls in older people (the LiFE study): Randomised parallel trial. British Medical Journal, 345(7870), Article e4547. 10.1136/bmj.e4547 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemson L, & Munro J (2017). Conceptual model of habit reforming to improve balance and prevent falls. In Panchana NA (Ed.), Encyclopedia of geropsychology (pp. 1–10). Springer. 10.1007/978-981-287-082-7_291 [DOI] [Google Scholar]
- Clemson L, Munro J, & Singh MF (2014). Lifestyle-integrated Functional Exercise (LiFE) program to prevent falls Participant’s manual. https://ses.library.usyd.edu.au/bitstream/handle/2123/10761/LiFE%20participant%27s%20manual%20-%20prelims.pdf?sequence=1&isAllowed=y
- Dougherty BE, Flom RE, & Bullimore MA (2005). An evaluation of the Mars Letter Contrast Sensitivity Test. Optometry and Vision Science, 82(11), 970–975. 10.1097/01.opx.0000187844.27025.ea [DOI] [PubMed] [Google Scholar]
- Fick DM, Semla TP, Steinman M, Beizer J, Brandt N, Dombrowski R, & Sandhu S (2019). American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. Journal of the American Geriatrics Society, 67(4), 674–694. 10.1111/jgs.15767 [DOI] [PubMed] [Google Scholar]
- Florence CS, Bergen G, Atherly A, Burns E, Stevens J, & Drake C (2018). Medical costs of fatal and nonfatal falls in older adults. Journal of the American Geriatrics Society, 66(4), 693–698. 10.1111/jgs.15304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gitlin LN, Hauck WW, Winter L, Dennis MP, & Schulz R (2006). Effect of an in-home occupational and physical therapy intervention on reducing mortality in functionally vulnerable older people: Preliminary findings. Journal of the American Geriatrics Society, 54(6), 950–955. 10.1111/j.1532-5415.2006.00733.x [DOI] [PubMed] [Google Scholar]
- Granbom M, Clemson L, Roberts L, Hladek MD, Okoye SM, Liu M, & Szanton S (2019). Preventing falls among older fallers: Study protocol for a two-phase pilot study of the multicomponent LIVE LiFE program. Trials, 20(1), Article 2. 10.1186/s13063-018-3114-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenfield EA (2012). Using ecological frameworks to advance a field of research, practice, and policy on aging-in-place initiatives. Gerontologist, 52(1), 1–12. 10.1093/geront/gnr108 [DOI] [PubMed] [Google Scholar]
- Guirguis-Blake JM, Michael YL, Perdue LA, Coppola EL, & Beil TL (2018). Interventions to prevent falls in older adults. Journal of the American Medical Association, 319(16), 1705–1716. 10.1001/jama.2017.21962 [DOI] [PubMed] [Google Scholar]
- Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, & Wallace RB (1994). A short physical performance battery assessing lower extremity function: Association with self-reported disability and prediction of mortality and nursing home admission. Journal of Gerontology, 49(2), M85–M94. [DOI] [PubMed] [Google Scholar]
- Hadjistavropoulos T, Martin RR, Sharpe D, Lints AC, McCreary DR, & Asmundson GJ (2007). A longitudinal investigation of fear of falling, fear of pain, and activity avoidance in community-dwelling older adults. Journal of Aging and Health, 19, 965–984. 10.1177/0898264307308611 [DOI] [PubMed] [Google Scholar]
- Hopewell S, Adedire O, Copsey BJ, Boniface GJ, Sherrington C, Clemson L, & Lamb SE (2018). Multifactorial and multiple component interventions for preventing falls in older people living in the community. Cochrane Database of Systematic Reviews, 7, CD012221. 10.1002/14651858.CD012221.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malik H, Virag B, Fick F, Hunter PV, Kaasalainen S, & Dal Bello-Haas V (2020). Fall prevention program characteristics and experiences of older adults and program providers in Canada: A thematic content analysis. Journal of Applied Gerontology, 39(10), 1124–1133. 10.1177/0733464819874600 [DOI] [PubMed] [Google Scholar]
- Nyman SR, & Victor CR (2012). Older people’s participation in and engagement with falls prevention interventions in community settings: An augment to the Cochrane systematic review. Age and Ageing, 41(1), 16–23. 10.1093/ageing/afr103 [DOI] [PubMed] [Google Scholar]
- Pfeiffer E (1975). A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society, 23(10), 433–441. [DOI] [PubMed] [Google Scholar]
- Reuben DB, Gazarian P, Alexander N, Araujo K, Baker D, Bean JF, … McMahon S (2017). The strategies to reduce injuries and develop confidence in elders intervention: Falls risk factor assessment and management, patient engagement, and nurse co-management. Journal of the American Geriatrics Society, 65, 2733–2739. 10.1111/jgs.15121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoene D, Wu SM, Mikolaizak AS, Menant JC, Smith ST, Delbaere K, & Lord SR (2013). Discriminative ability and predictive validity of the timed up and go test in identifying older people who fall: Systematic review and meta-analysis. Journal of the American Geriatrics Society, 61(2), 202–208. 10.1111/jgs.12106;10.1111/jgs.12106 [DOI] [PubMed] [Google Scholar]
- Smith KS, & Graybiel AM (2016). Habit formation. Dialogues in Clinical Neuroscience, 18, 33–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sterling DA, O’Connor JA, & Bonadies J (2001). Geriatric falls: Injury severity is high and disproportionate to mechanism. The Journal of Trauma, 50(1), 116–119. [DOI] [PubMed] [Google Scholar]
- Stevens JA, & Burns E (2015). A CDC compendium of effective fall interventions: What works for community-dwelling older adults (3rd ed.). https://www.cdc.gov/homeandrecreational-safety/pdf/falls/cdc_falls_compendium-2015-a.pdf
- Szanton SL, Xue Q-L, Leff B, Guralnik J, Wolff JL, Tanner EK, … Gitlin LN (2019). Effect of a biobehavioral environmental approach on disability among low-income older adults: A randomized clinical trial. JAMA Internal Medicine, 179(2), 204–211. 10.1001/jamain-ternmed.2018.6026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tinetti ME, Richman D, & Powell L (1990). Falls efficacy as a measure of fear of falling. Journal of Gerontology, 45(6), P239–P243. [DOI] [PubMed] [Google Scholar]
- Weber M, Belala N, Clemson L, Boulton E, Hawley-Hague H, Becker C, & Schwenk M (2018). Feasibility and effectiveness of intervention programmes integrating functional exercise into daily life of older adults: A systematic review. Gerontology, 64(2), 172–187. 10.1159/000479965 [DOI] [PubMed] [Google Scholar]


