Abstract
Models of non-suicidal self-injury (NSSI) posit that individuals use NSSI to influence others, but this remains largely untested. We used ambulatory assessment to test the interpersonal function of NSSI in the daily lives of 51 women with DSM-5 NSSI disorder. Participants reported NSSI events, urges, motives, and positive/negative interpersonal events (IPEs) for 14 days, providing five semi-random daily assessments and event-related NSSI reports. We analyzed 3,498 data-points, including 155 NSSI events, using multilevel models. We observed a positive concurrent association between the number of negative IPEs and NSSI engagement. Additionally, perceived distress of negative IPEs was positively associated with concurrent NSSI events and urges, and predicted later events. We saw no reduction in negative or increase in positive IPEs following NSSI. In a trait-level interview, participants endorsed interpersonal motives only minimally, but indicated that others often trigger NSSI. In daily life, participants rarely endorsed the motive ‘get help/attention’. The results suggest that negative IPEs trigger NSSI, but that individuals in this sample rarely used NSSI for interpersonal motives and did not experience interpersonal reinforcement of NSSI. We discuss limitations of and possible solutions for under-reporting of interpersonal motives and benefits of studying interpersonal triggers (rather than outcomes) in future studies.
Keywords: Non-suicidal self-injury, interpersonal, function, reinforcement, ambulatory assessment, daily life
Introduction
Non-suicidal self-injury (NSSI) refers to the intentional, self-inflicted damage of body tissue without suicidal intent and is a prevalent, trans-diagnostic phenomenon that is recognized as a nosological entity in the DSM-5 (APA, 2013). NSSI can take many forms, for instance cutting or burning the skin or hitting oneself. NSSI afflicts approximately 5.5% of the adult population and prevalence peaks in adolescence with rates as high as 17.2% during this developmental period (e.g., Swannell et al., 2014). Beyond the mental health burden itself, NSSI is predictive of future suicide attempts (Victor & Klonsky, 2014) and creates substantial health care and economic costs related to productivity loss, increased morbidity, and mortality (e.g., Kinchin et al., 2017).
Given marked negative outcomes associated with NSSI, the field has produced several theoretical models aiming to explain why people self-injure. Most models posit an affect regulation function of NSSI, including the Experiential Avoidance Model (Chapman et al., 2006), the Four-Function Model (Nock & Prinstein, 2004), and the Benefits and Barriers Model (Hooley & Franklin, 2018). NSSI for the purpose of negative affect regulation has been researched in depth and is the most common self-reported motive for NSSI (Edmondson et al., 2016). Laboratory studies support this picture (Ammerman et al., 2018), as does an emerging body of daily-life evidence (see Hepp et al., 2020 for a review).
Interpersonal functions of NSSI are less researched. The Four-Function Model (Nock & Prinstein, 2004) suggests two interpersonal functions: Interpersonal positive reinforcement, which comprises NSSI aiming to elicit positive behavior from others, and interpersonal negative reinforcement, which includes NSSI aiming to reduce unwanted behavior from others or unwanted interactions, for instance ending a conflict. Similarly, the Benefits and Barriers Model (Hooley & Franklin, 2018) suggests that some NSSI is used to generate peer group affiliation and to communicate distress or strength to others. In a systematic review of 152 studies, Edmondson et al. (2016) found that 87% of studies using self-report questionnaires found evidence for interpersonal functions, for instance seeking help from others. Adding to this, a recent meta-analysis of 46 studies found that NSSI with the goal of communicating distress or increasing support from others was endorsed by 32–56% of individuals, though most participants endorsed more than one function (Taylor et al., 2018).
Beyond cross-sectional self-report studies, few studies have assessed interpersonal functions of NSSI. Laboratory evidence appears to be lacking altogether, and the daily-life evidence on interpersonal functions of NSSI is sparse, as summarized in a recent review (Hepp et al., 2020). Only four of the 35 reviewed studies assessed interpersonal motives for NSSI in the moment (i.e. asking participants why they self-harmed right after it happened), and found endorsement of interpersonal functions in less than 15% of events. Beyond these, only three studies have explicitly tested the interpersonal function of NSSI in daily life. Two studies suggest that the probability of experiencing negative interpersonal events (IPEs) is increased prior to NSSI or on days with NSSI (Snir et al., 2015; Turner et al., 2016), but only one of these demonstrated a decrease following NSSI, suggesting negative reinforcement (Snir et al., 2015). Turner et al. (2016) further assessed the association between NSSI and social support and found that support increased on days following NSSI that was revealed to another person, suggesting positive reinforcement. Lastly, a study assessing NSSI in adolescents found no evidence of positive interpersonal reinforcement, but decreased feelings of attachment to the mother after NSSI (König et al., 2020).
In sum, evidence for interpersonal functions of NSSI is sparse despite being included in leading theoretical models (Hooley & Franklin, 2018; Nock & Prinstein, 2004). Cross-sectional studies suggest that participants endorse interpersonal motives retrospectively, but daily-life studies have shown that participants rarely report interpersonal motives when asked directly after engaging in NSSI. Moreover, daily-life evidence on negative interpersonal reinforcement is limited to only two studies (Snir et al., 2015; Turner et al., 2016), as are examinations of positive interpersonal reinforcement (König et al., 2020; Turner et al., 2016). The present study sought to fill this gap and provide a test of both self-reported and inferred interpersonal functions of NSSI in daily life.
The present study
The aim of the present study was to test the interpersonal function of NSSI as posited by the Four-Function Model (Nock & Prinstein, 2004) using ambulatory assessment (AA). Interpersonal negative reinforcement of NSSI suggests that negative IPEs occur prior to NSSI and decrease after NSSI, contributing to an increased likelihood of using NSSI to reduce negative IPEs in the future. Based on this, we derived the following hypotheses. Hypothesis 1: Negative IPEs at t-1 predict a greater probability of engaging in NSSI at t0. Hypothesis 2: NSSI at t0 predicts a lower number of negative IPEs at t1. Additionally, interpersonal positive reinforcement suggests that the probability of experiencing positive IPEs, such as support or comfort from others, increases after NSSI. Therefore, we hypothesized that NSSI at t0 predicts a greater number of positive IPEs at t1 (Hypothesis 3).
Method
Participants
We recruited participants via flyers at local clinics, our institution patient waitlist, and Facebook groups on NSSI-related topics. Only women were recruited to reduce heterogeneity, as the parent study assessed biological markers (see Störkel et al., 2021). Data were collected between April 2017 and November 2018. The total sample included 51 women (M age = 23.92 years, SD = 6.72, range = 18–45) who met criteria for DSM-5 NSSI-disorder, reporting repeated (≥ 1/week) NSSI acts that damaged body tissue for the past three months or more. Exclusion criteria were substance dependence in the past 6 months, lifetime developmental disorders or schizophrenia, current pregnancy, and current injuries unrelated to NSSI.1
Participants reported frequent past-month NSSI (M=10.36 events, SD=6.44, range=3–32) and past-year NSSI (M=124.41 events, SD=104.08, range=5.5–624) on the Self-Injurious Thoughts and Behavior Interview (SITBI-G, Fischer et al., 2014). To assess further psychopathology, we used the Structured Clinical Interview for DSM-IV (SCID-I, First et al., 1995) and the BPD section of the International Personality Disorder Examination (IPDE, Loranger et al., 1997). All participants met criteria for at least one mental disorder, the most common being major depression (n=33, 64.71%) and borderline personality disorder (n=32, 62.75%). The majority of participants (n=30, 58.82%) reported long-term use of psychiatric medication, most commonly antidepressants (n=30, 58.82%) and atypical antipsychotics (n=14, 27.45%). See Table S1 in the supplement for additional demographic and clinical characteristics.
Procedure
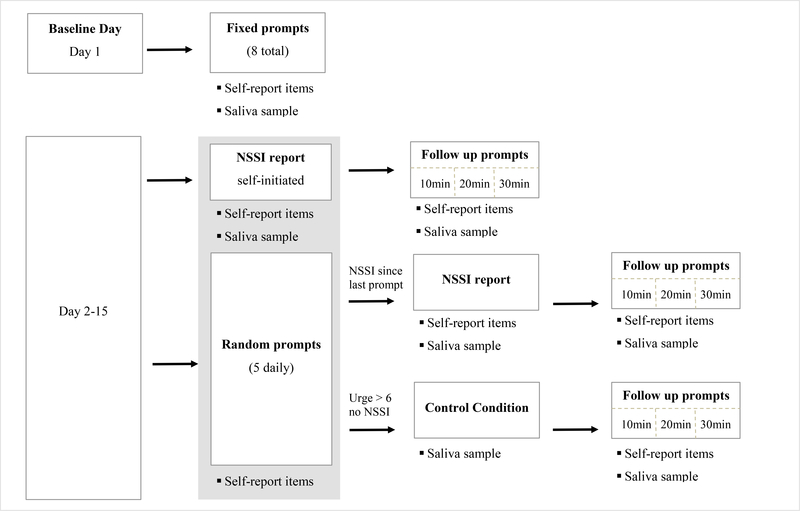
Following a description of the study protocol, participants provided written informed consent for the study, which was approved by the ethics committee of the Medical Faculty Mannheim, Heidelberg University (2014–601N-MA). Participants then completed an in-person or online (via the secure platform Patientus, jameda GmBH, Munich, Germany) orientation session, including clinical interviews and an introduction to the smartphone application (movisensXS, Version 0.7.4682, movisens GmbH, Karlsruhe, Germany), which was provided on study smartphones. Study smartphones were mailed to participants who completed the orientation session online. Additionally, we sent an email with video instructions on how to use the smartphone app to these participants, so they could refer back to the video after completing the online orientation session. Participants who received the instructions online did not report any problems with the app, which suggests that using an online orientation session and using instructional videos may be a feasible avenue in AA NSSI research. Following this, participants completed a 15-day AA assessment period (including a baseline day and 14 days of regular AA protocol). Figure 1 illustrates the different types of prompts that were included (also see Störkel et al., 2021). Participants completed five semi-random prompts per day (scheduled at least two hours apart during participants’ normal waking hours), and were asked to self-initiate additional reports as soon as possible following NSSI. We included self-initiated prompts for NSSI events (and follow-up prompts for these) as we were interested in the psychological processes that unfold right after NSSI. If NSSI events were only assessed during random prompts, the time lag between the actual NSSI event and the reporting of that event during the next random prompt would be substantial (on average 2 hours in our sampling scheme). Therefore, including self-initiated prompts allowed for a much higher temporal resolution. In addition to the self-initiated prompts, we included five semi-random prompts per day to capture psychological processes during the whole day on both NSSI and non-NSSI days. The combined sampling scheme has the benefit of capturing NSSI events as close in time as possible (self-initiated prompts) and ensures that no NSSI events get lost if participants forget to self-initiate a report, as they would be prompted to report them during the next random prompt. Participants took on average 87.75 seconds (SD = 57.61) to complete a random prompt. The design included no “skip-out” options, that is, participants always saw the total number of items and there were no item filters. IPEs were only assessed during random prompts and self-initiated NSSI reports outside the baseline day. For further detail on all prompt types and variables, see the online supplement. Following participation, participants received 100€ for compensation, with an additional bonus of 50€ for ≥ 80% compliance. As an additional incentive, participants had the option to receive a personalized plot with their study data after completing the study, which many of them indicated to us was a motivating factor for high adherence to the study protocol.
Figure 1.
Overview of all prompt types included in the parent study. Prompts where interpersonal events were assessed are shaded in grey, only these were used for the current analyses. For further detail, see Störkel et al. (2020) and supplement.
Material
NSSI Interview:
During the orientation session, a trained Master’s level psychologist administered the SITBI-G (Fischer et al., 2014), a semi-structured interview that assesses motives of and triggers for NSSI on a scale from 0 (“low/little”) to 4 (“very much/severe”). NSSI frequency, severity, and methods were also assessed via the SITBI-G. Scores for SITBI-G motives and triggers are presented in Table 1.
Table 1.
Triggers and motives for NSSI at the trait and momentary levels.
| M/n | SD/% | |
|---|---|---|
| SITBI-G NSSI triggers | ||
| mental state at the time | 3.40 | 0.76 |
| problems with family | 2.81 | 1.16 |
| problems with work/school | 2.76 | 1.15 |
| problems with peers | 1.99 | 1.33 |
| problems with relationships | 1.95 | 1.57 |
| problems with friends | 1.72 | 1.31 |
| SITBI-G NSSI motives | ||
| as a way to get rid of bad feelings | 3.37 | 1.02 |
| because you were feeling numb and empty | 2.80 | 1.29 |
| to get out of doing something or to get away from others | 1.36 | 1.22 |
| to communicate with someone else or to get attention | 0.91 | 1.20 |
| Momentary NSSI motives | ||
| To reduce aversive tension or overwhelming emotions | 99 | 63.9% |
| Self-hatred/ self-contempt | 59 | 38.1% |
| To feel something (other than nothing) | 31 | 20.0% |
| To get help/ attention from others | 8 | 5.2% |
Note. SITBI-G triggers and motives asses on a scale from 0 “low/little” to 4 “very much/severe”. Momentary motives were assessed dichotomously (present/absent) whenever NSSI was reported.
In 45.8 % of NSSI events participants chose more than one motive.
NSSI events.
Participants were instructed to self-initiate an AA assessment whenever they self-injured, by clicking a button on the smartphone app that said “I have hurt myself.” Additionally, participants were asked during all random reports: “Since the last prompt I have answered, I have hurt myself” (1= yes, 0 = no).
NSSI urges.
Urge was assessed with the single item “During the last 15 minutes, the urge to hurt myself was” on a visual analog scale from 0 (“no urge at all”) to 10 (“I can hardly contain it”).
NSSI motives.
Whenever participants reported NSSI, motives were assessed. Participants selected all that apply from the following: “I wanted to reduce aversive tension or overwhelming emotions,” “I wanted to express my self-hatred/self-contempt,” “I wanted to feel something (other than nothing),” “I wanted help/attention of others,” “I had another reason,” and “I don’t know why I self-harmed.”2 Endorsement frequencies are presented in Table 1.
Interpersonal events.
Participants reported significant positive and negative IPEs during random prompts (“Since the last beep, someone... “) and during self-initiated NSSI prompts (“Before I self-harmed, someone...”). We presented participants with five positive and five negative items that we piloted previously (for further detail, see online supplement). Individual items are presented in Table 2. Participants were instructed to select all items that applied. If any event was endorsed, participants were asked whether “What the person did was a reaction to my last NSSI” (“yes”/”no”/”don’t know”) and “What the person did distressed me” (0= “not at all” to 5= “very deeply”).
Table 2.
Frequency of endorsement of interpersonal events by prompt type and Chi-square tests comparing frequencies between prompt types.
| NSSI prompts (Before I self-harmed, s/o...) | Random prompts (Since the last prompt, s/o...) | ||||
|---|---|---|---|---|---|
|
|
|
|
|||
| n | % of prompts | n | % of prompts | Chi-square test | |
| Negative Events | |||||
| ...criticized me | 13 | 9.49 | 236 | 7.02 | χ2(1)=1.71 |
| ...rejected/excluded me | 19 | 13.87 | 186 | 5.53 | χ2(1)=18.81*** |
| ...ignored my needs or feelings | 24 | 17.52 | 216 | 6.43 | χ2(1)=28.52*** |
| ...behaved angry/ aggressive towards me | 14 | 10.22 | 141 | 4.20 | χ2(1)=12.85*** |
| ...let me down/ disappointed me | 23 | 16.79 | 221 | 6.58 | χ2(1)=23.97*** |
| ...none of the above | 90 | 65.69 | 2847 | 84.71 | χ2(1)=22.28*** |
| Positive Events | |||||
| ...supported/ helped me | 3 | 2.19 | 401 | 11.93 | χ2(1)=11.28*** |
| ...showed me affection | 10 | 7.30 | 664 | 19.76 | χ2(1)= 11.62*** |
| ...respected my needs or feelings | 6 | 4.38 | 454 | 13.51 | χ2(1)=8.60** |
| ...gave me their attention or time | 18 | 13.14 | 892 | 26.54 | χ2(1)=10.37** |
| ...was interested in me, understood me | 12 | 8.76 | 685 | 20.38 | χ2(1)=9.67** |
| ...none of the above | 110 | 80.29 | 2073 | 61.68 | χ2(1)=28.91*** |
Note.n=137 NSSI reports and n=3361 random prompts.
p<.05
p<.01
p<.001
Data analysis
Data were analyzed using multi-level models (MLMs), treating prompts as nested within persons. We modelled random intercepts per person and random slopes for momentary-level predictors. Analyses were conducted in R using the package lme4. We used the function lmer for linear MLMs, glmer with a logit link function for logistic MLMs, and glmer with a log link for count outcomes. Significance tests were conducted using the package lmerTest. All models adjusted for the person mean of the predictor variable (i.e. mean number of negative IPEs for each individual, mean distress reported by each individual) to disaggregate within- from between-person effects. All models further included a covariate for the time since wake (in hours), as NSSI was more likely to occur toward the end of the individual day. Momentary predictors were centered on the person mean, and person-level predictors were centered on the grand mean. Lagged analyses did not include lags across days (e.g., the last prompt of day 2 was not treated as a lagged prompt for the first prompt of day 3).
Results
Descriptive results
Random prompt compliance was high (92.04%) and resulted in a total of 3,498 observations included in the present analysis. On average, participants reported 3.04 NSSI events per person (SD=2.45; range 0–15), totaling 155 events. Endorsement rates for trait-level motives and triggers assessed using the SITBI-G (Fischer et al., 2014) are presented in Table 1. Problems with family were the second most endorsed trigger for NSSI and problems with all remaining interaction partners (peers, friends, partners) were endorsed to a moderate degree with average endorsement ranging around 2 (0=“low/little”, 4=“very much/severe”). The two interpersonal motives for NSSI (“to get out of doing something or to get away from others”, “to communicate with someone or get attention”) were endorsed at very low levels. In addition to these trait measures, we assessed NSSI motives at the momentary level. Of note, the interpersonal motive, “to get help/attention from others,” was only endorsed for eight NSSI events (5.16%).
Negative IPEs were endorsed on 15.3% of all random prompts and positive IPEs were endorsed on 38.3%. Of prompts where NSSI was reported, participants endorsed negative IPEs on 34.3% and positive IPEs on 19.7%. Table 2 presents endorsement rates for the specific types of negative and positive IPEs during NSSI and random prompts and a comparison of their frequency based on chi-square tests. Importantly, almost all negative IPEs were significantly more likely to be endorsed during NSSI prompts than random prompts, and all positive IPEs were significantly more likely to be endorsed during random prompts than NSSI prompts.
When negative or positive IPEs occurred, participants rarely reported that what their interaction partner did was a reaction to their most recent NSSI. Participants indicated this for only 1.11% of negative events and 1.81% of positive events. Additionally, participants reported how distressing the IPEs were. On average, participants rated the distress level of negative IPEs during random prompts significantly lower (M=3.09, SD=1.42) than for events directly preceding NSSI (M=3.77, SD=1.16, t(47.44)=3.47, p=001).
Hypothesis 1
To test whether negative IPEs are positively associated with the probability of subsequent engagement in NSSI, we conducted two generalized MLMs using a logit link function with momentary NSSI (yes/no) as the binary outcome variable. The first model included the concurrent and lagged sum of negative IPEs and covariates. We included the concurrent prompts because the self-initiated NSSI prompts asked individuals about negative IPEs occurring ‘right before’ any reported NSSI. Therefore, temporal precedence was present for NSSI prompts such that any reported negative interpersonal event preceded NSSI. The second model included the concurrent and lagged distress caused by negative IPEs as predictors.
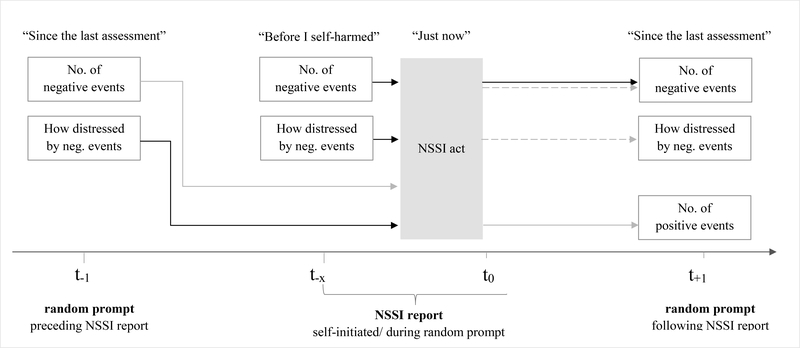
Results indicated that a higher number of negative IPEs in the current moment (at t0) predicted a higher probability of reporting NSSI at that prompt (OR=1.54, 95% CI=[1.24, 1.91], p<.001). In contrast, a higher number of negative IPEs at t-1 did not significantly predict NSSI at t0 (OR=1.11, 95% CI=[0.77, 1.60],p=.565)3. Results from model 2 showed that higher distress from negative events at t0 and at t-1 positively predicted NSSI at t0 (distress at t0: OR=1.37, 95% CI=[1.20, 1.58], p<.001; distress t-1: OR=1.21; 95% CI=[1.01, 1.45], p=.040). For detailed results including effects for all covariates, see Tables S2-S3. Results are illustrated in Figure 2.
Figure 2.
Illustration of findings. Solid black arrows indicate significant positive associations. Solid grey arrows indicate hypothesized, but non-significant positive associations. Dotted grey arrows indicate hypothesized but non-significant negative associations.
Hypothesis 2
To test the hypothesis that NSSI would be negatively associated with the number of subsequent negative IPEs, we conducted two MLMs. The first, a generalized MLM using a log link function, included the number of negative IPEs reported since the last prompt as the outcome variable from a Poisson distribution. The second model was a linear MLM with the distress of negative IPEs reported since the last prompt as the outcome. Predictors in both models included NSSI at t-1. Results indicated that NSSI was not significantly associated with either the number of negative IPEs reported in the subsequent moment (Incidence Rate Ratio [IRR]=0.73, 95% CI=[0.25, 2.09], p=.555) nor their distress following negative IPEs (β=0.01, 95% CI=[−0.02, 0.05], p=.488)4. See Tables S4-S5 and Figure 2.
Hypothesis 3
To test the hypothesis that NSSI would be positively associated with the number of subsequent positive IPEs, we conducted a generalized MLM. The model mirrored that for hypothesis 2 but with positive IPEs as the outcome. Results indicated that NSSI at t0 was not significantly associated with the number of positive IPEs at t1 (IRR=0.91, 95% CI=[0.58, 1.43], p=.679). See Table S6 and Figure 2.
Exploratory analyses
NSSI urges: Previous studies suggest that negative IPEs are not only associated with NSSI acts but also with urges for NSSI and that most acts are preceded by urges (Hepp et al., 2020). Negative IPEs may thus precede urges that do not necessarily lead to acts of self-harm. In an exploratory linear MLM, we tested whether the sum of negative IPEs predicts concurrent or subsequent NSSI urges. As for NSSI acts, the sum of negative IPEs were positively associated with concurrent urges (β=0.26, 95% CI=[0.19, 0.33], p<.001) but not subsequent urges (β=0.03, 95% CI=[−0.01, 0.08], p=.125; see Table S7). In a second MLM, we tested whether distress caused by negative IPEs predicted concurrent or subsequent NSSI urges. The degree of distress resulting from negative events was positively associated with concurrent urges (β=0.23 95% CI=[0.19, 0.27], p< .001) but not subsequent urges (β=0.02, 95% CI=[−0.02, 0.05], p=436; Table S8).
Day level analyses:
Consistent with Turner et al. (2016), we conducted additional analyses to determine whether associations between NSSI and IPEs might be better captured at the day level of analysis (see supplement for details and results in Tables S9-S10). We conducted two linear MLMs using the average number of negative/positive IPEs reported in a day as the outcome. The predictors of interest were whether NSSI was reported during the concurrent or lagged day (coded 0 or 1). NSSI on any given day was positively associated with the average number of negative IPEs reported on the same day (β=0.08, 95% CI=[0.02, 0.13],p=.005), but not the next day (β=0.00, 95% CI=[−0.06, 0.05], p=.904). We observed no significant association between positive IPEs and NSSI on the same day (β=−0.06, 95% CI=[−0.11, 0.00], p=.062) or the next day (β=0.03, 95% CI=[−0.03, 0.09], p=.263).
Discussion
We tested the interpersonal function of NSSI as proposed in the Four-Function Model (Nock & Prinstein, 2004) in the daily lives of 51 women with NSSI disorder over a period of two weeks. Using the SITBI-G (Fischer et al., 2014), we assessed participants’ trait-level motives and triggers for NSSI. Participants showed only weak endorsement of interpersonal negative reinforcement motives at the trait level (“to get out of doing something/away from others”) and rarely endorsed positive interpersonal reinforcement motives (“to get attention”) at both the trait and momentary levels..
In contrast to the weak endorsement of interpersonal motives, participants strongly endorsed interpersonal triggers for NSSI (especially family members) in the SITBI-G and reported a significantly higher number of interpersonal problems as having occurred ‘right before’ NSSI (see Figure 2) than during other assessments. Compared to previous studies, we included a substantially broader set of IPEs and observed that participants most often endorsed ‘someone ignored my needs or feelings’ and ‘someone let me down or disappointed me’ as preceding NSSI.
Using a logistic MLM, we found that the number of negative IPEs that occurred directly before NSSI was positively associated with the probability of engaging in NSSI at that time-point. Going further back in time and considering the last random assessment preceding NSSI did not reveal a significant association. The same pattern emerged in an exploratory analysis for NSSI urges. These results differ somewhat from findings by Snir et al. (2015), who sampled at a similar frequency (also including five semi-random daily prompts), and found elevated rejection in the prompts preceding NSSI events. However, their sample included individuals with BPD and avoidant personality disorder, both of which are characterized by increased reactivity to rejection. This could explain why Snir and colleagues (2015) observed a significant association between rejection and NSSI across a longer timeframe in their study, while we only observed this association with events that occurred immediately prior to NSSI. However, when considering the perceived distress caused by negative events rather than just the number of events that occurred, we observed significant associations with concurrent and later NSSI acts. In other words, negative IPEs that occurred around two hours earlier did not predict NSSI engagement, but negative IPEs that were perceived as highly distressing did. The same was observed for NSSI urges. It is possible that increased distress caused by negative IPEs also underlies the increased prevalence of negative IPEs preceding NSSI that was demonstrated by Snir et al. (2015), but additional studies are needed to clarify the types and intensities of interpersonal events that precede NSSI and further specify the time window for this association.
Next, we tested whether interpersonal problems decreased following NSSI, as this would facilitate interpersonal negative reinforcement. We found no significant association between NSSI at t0 and the number of or the perceived distress caused by negative IPEs at t1. This contrasts findings by Snir et al. (2015), who observed a decrease in rejection following NSSI, and is inconsistent with the idea of NSSI eliciting interpersonal negative reinforcement (Nock & Prinstein, 2004). Likewise, we found no association between NSSI and a subsequent increase in positive events, as would be implied by interpersonal positive reinforcement. This was consistent with another source of data from our study: whenever participants reported IPEs, we asked whether they saw the other person’s behavior as a reaction to their last NSSI. Participants rarely endorsed this (only 1.81% of positive events). It somewhat contrasts findings by König et al. (2020) who found decreased feelings of attachment to participants’ mothers following NSSI in an adolescent sample. However, the present study is not directly comparable because i) the samples are different, ii) König et al. used a higher frequency sampling approach with hourly prompts, and iii) feeling attached is conceptually different from the positive behaviors by others we assessed.
Because a previous study found that positive IPEs did not increase immediately following NSSI, but only the next day (Turner et al., 2016), we conducted exploratory day-level analyses. Turner and colleagues (2016) found a positive association between the level of conflict in a day and the likelihood for NSSI that day, and we replicated this finding. They also found that conflict did not decrease on days following NSSI (including NSSI revealed to others), which we also replicated. Contrasting findings by Turner et al., we did not see an increase in positive IPEs on days following NSSI, whereas they observed increased support following NSSI days.
Limitations and future directions
First, the generalizability of results is limited to younger women with DSM-5 NSSI disorder, as we excluded men and restricted the age range (18–45 years) to reduce sample heterogeneity in light of the biological component of the parent study (Störkel et al., 2021). This reflects a problem of the field of AA NSSI research at large (see Hepp et al., 2020) – a selective focus on studying younger white women, resulting in a clear need for the assessment of more diverse samples.
A second limitation is the possibility of under-reporting of interpersonal motives because of social desirability. The way interpersonal motives are phrased in the SITBI-G and the momentary motive ‘to get help/attention’ could have suggested to participants that their NSSI was a manipulative means of getting attention from others. This is one of the central stigmas surrounding NSSI, and a fear of propagating it could have resulted in under-reporting of interpersonal motives. We relied on the SITBI-G as an established measure to assess NSSI motives, but suggest that future studies include additional, less stigmatizing items to assess interpersonal motives (e.g., ‘to cope with interpersonal stress’). Moreover, the fact that we only assessed interpersonal motives with one AA item restricts conclusions for momentary interpersonal motives. For instance, participants may have engaged in NSSI for interpersonal reasons other than seeking help/attention but were unable to reflect this on the AA surveys. Additionally, as detailed in Table 2, for the majority of NSSI events (65.69%), participants reported that none of the negative IPEs we assessed preceded the event. Participants may have experienced other negative IPEs which we did not assess, or may have experienced other triggers for NSSI of an intrapersonal nature.
A third limitation is that we did not assess whether NSSI was revealed to another person. Turner et al. (2016) found that interpersonal reinforcement of NSSI only occurred for events that were revealed to another person and, conceptually, someone else being aware that NSSI took place is a prerequisite for interpersonal reinforcement. We intended to implicitly assess whether NSSI was revealed to another person by asking participants whether another person reacted to it. However, responding “no” to the question we used (“Was the interpersonal event a reaction to the last NSSI?”) could mean several different things. It could indicate that (a) the interaction partner did not know about the participant’s NSSI act (it was not revealed to them), or (b) the interaction partner did know about the NSSI act, but did not react to it, or (c) that the interaction partner’s reaction was not attributed to NSSI by the participant. Consequently, an additional direct assessment of NSSI revelation in combination with a question asking participants whether they perceived an interaction partner’s behavior as a reaction to their latest NSSI would be ideal in future studies.
Fourth, the way that we aimed to establish temporal precedence of IPEs prior to NSSI may have introduced limitations. Whenever participants reported NSSI during NSSI prompts, we asked them to report whether any IPEs happened ‘right before’ the NSSI event. This suggests temporal precedence of IPEs prior to NSSI. However, it is possible that negative events occurred much earlier in the day and triggered NSSI despite not occurring ‘right before’ the NSSI event. For instance, an individual may feel rejected by their partner in the morning, resulting in sustained negative affect or self-loathing throughout the day that ultimately culminates in NSSI. In this instance, they might indicate affect regulation or self-loathing as the motive for NSSI and no IPEs occurring ‘right before’ NSSI, despite the initial trigger being rejection. Moreover, despite asking participants to report IPEs that occurred ‘right before’ NSSI engagement, these IPEs were still assessed at the same occasion as the NSSI event. Therefore, the time lag was only established based on the way the item was phrased, rather than being incorporated in the study design. It is therefore possible that these reports are biased, given that participants were asked to complete these reports directly following NSSI while they may have still experienced substantial distress.
A final limitation that affects the present study and previous work on interpersonal NSSI is the question of specificity of interpersonal events. By only assessing interpersonal stressors, it remains unclear whether the specific interpersonal nature of the stressor was predictive of NSSI or whether other types of stressors (e.g., a job demand or financial trouble) would produce similar results. Therefore, future studies should consider comparing interpersonal stressors to other types to stressors with regard to predicting NSSI.
Conclusion
In sum, results implicate negative IPEs as a trigger for NSSI and suggest that assessing the level of distress caused by IPEs is an important extension to assessing their incidence. Only negative IPEs with high levels of associated distress, but not mere incidence of negative events, predicted subsequent NSSI. At the same time, we found no evidence for positive or negative interpersonal reinforcement following NSSI, which questions the role of these processes in the maintenance of NSSI. Overall, we found only limited evidence for interpersonal functions of NSSI, as individuals rarely endorsed these as self-reported motives. However, conclusions on motives are likely limited by the restricted assessment of interpersonal motives and possible under-reporting due to social desirability. Future studies may benefit from assessing IPEs as triggers of NSSI and a careful assessment of interpersonal motives using non-stigmatizing items. A careful assessment of the quality of IPEs, for instance how distressing they are, with whom they occur, or even cognitive aspects such as whether they violate prior beliefs (e.g., betrayal by a trusted person) may help further elucidate which IPEs are the most potent triggers of distress and NSSI, to ultimately inform prevention and treatment approaches.
We note that the empirical evidence on interpersonal functions of NSSI is still limited, as this is only the fourth study to directly test it. Therefore, any clinical implications must be considered preliminary. Yet, so far, studies have found little evidence for interpersonal reinforcement following NSSI, suggesting that the behavior is unlikely to be substantially maintained by outside attention from others. Therefore, rather than focusing on the role of parental, spousal, or peer behavior in response to NSSI, clinicians may better help their patients by helping them identify interpersonal triggers of NSSI and how the distress resulting from negative interpersonal events can be regulated so that NSSI does not occur.
Supplementary Material
We tested the interpersonal function of NSSI using 15 days of ambulatory assessment
Negative interpersonal events were elevated pre NSSI but did not decrease post NSSI
Distressfulness of interpersonal events predicted concurrent and subsequent NSSI
Positive interpersonal events did not increase post NSSI
NSSI was not interpersonally reinforced but sometimes interpersonally triggered
Acknowledgments
This research was supported by the Young Investigator Award of the Central Institute of Mental Health Mannheim awarded to Inga Niedtfeld. Andrea M. Wycoff and Lindsey K. Freeman were supported by the National Institutes of Health (F31 AA027958, Wycoff; T32 AA013526, Sher).
Footnotes
Data and R code available at: https://osf.io/uqmky/?view_only=c8afefb640354a6286c3c7f70d8dda46
We applied additional exclusion criteria related to the collection of saliva samples (see Störkel et al., 2021).
Participants responded to additional questions following endorsement of NSSI (method, severity, painfulness, pleasantness of pain, momentary affect, dissociative symptoms), but these items were not included in the analyses for present study (see Störkel et al., 2021 and the online supplement for further details).
Using a dichotomous variable that codes whether any negative IPE occurred (coded 1) or none occurred (coded 0) produced the same results as the sum score.
Again, using a dichotomous indicator of whether any negative IPE occurred produced the same results.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders: DSM-5™. American Psychiatric Asociation. [Google Scholar]
- Ammerman BA, Berman ME, & McCloskey MS (2018). Assessing non-suicidal self-injury in the laboratory. Archives of Suicide Research, 22(2), 193–223. 10.1080/13811118.2017.1319312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman AL, Gratz KL, & Brown MZ (2006). Solving the puzzle of deliberate self-harm: The experiential avoidance model. Behaviour research and therapy, 44(3), 371–394. [DOI] [PubMed] [Google Scholar]
- Edmondson AJ, Brennan CA, & House AO (2016). Non-suicidal reasons for self-harm: A systematic review of self-reported accounts. Journal of Affective Disorders, 191, 109–117. 10.1016/j.jad.2015.11.043 [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JB (1995). Structured Clinical Interview for DSM-IVAxis I disorders - patient ed. (SCID-I/P, version 2). Biometrics Research Department, New York State Psychiatric Institute. [Google Scholar]
- Fischer G, Ameis N, Parzer P, Plener PL, Groschwitz R, Vonderlin E, Kolch M, Brunner R, & Kaess M (2014). The German version of the self-injurious thoughts and behaviors interview (SITBI-G): a tool to assess non-suicidal self-injury and suicidal behavior disorder. BMC psychiatry, 14(1), 265. 10.1186/s12888-014-0265-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hepp J, Carpenter RW, Störkel LM, Schmitz SE, Schmahl C, & Niedtfeld I (2020). A systematic review of daily life studies on non-suicidal self-injury based on the four-function model. Clinical Psychology Review, 82, 101888. 10.1016/j.cpr.2020.101888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooley JM, & Franklin JC (2018). Why do people hurt themselves? A new conceptual model of nonsuicidal self-injury. Clinical Psychological Science, 6(3), 428–451. 10.1177/2167702617745641 [DOI] [Google Scholar]
- Kinchin I, Doran CM, Hall WD, & Meurk C (2017). Understanding the true economic impact of self-harming behaviour. The Lancet Psychiatry, 4(12), 900–901. 10.1016/S2215-0366(17)30411-X [DOI] [PubMed] [Google Scholar]
- Konig J, Klier J, Parzer P, Santangelo P, Resch F, Ebner-Priemer U, & Kaess M (2020). High-frequency ecological momentary assessment of emotional and interpersonal states preceding and following self-injury in female adolescents. European Child & Adolescent Psychiatry, 1–10. 10.1007/s00787-020-01626-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loranger AW, Janca A, & Sartorius N (1997). Assessment and diagnosis of personality disorders: The ICD-10 international personality disorder examination (IPDE). Cambridge University Press. [Google Scholar]
- Nock MK, & Prinstein MJ (2004). A functional approach to the assessment of self-mutilative behavior. Journal of Consulting and Clinical Psychology, 72(5), 885–890. 10.1037/0022-006X.72.5.885 [DOI] [PubMed] [Google Scholar]
- Snir A, Rafaeli E, Gadassi R, Berenson K, & Downey G (2015). Explicit and inferred motives for nonsuicidal self-injurious acts and urges in borderline and avoidant personality disorders. Personality Disorders: Theory, Research, and Treatment, 6(3), 267–277. 10.1037/per0000104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Störkel LM, Karabatsiakis A, Hepp J, Kolassa I-T, Schmahl C, & Niedtfeld I (2021). Salivary beta-endorphin in non-suicidal self-injury: An ambulatory assessment study. Neuropsychopharmacology, Advance online publication. 10.1038/s41386-020-00914-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swannell SV, Martin GE, Page A, Hasking P, & St John NJ (2014). Prevalence of nonsuicidal self- injury in nonclinical samples: Systematic review, meta- analysis and meta-regression. Suicide and Life- Threatening Behavior, 44(3), 273–303. 10.1111/sltb.12070. [DOI] [PubMed] [Google Scholar]
- Taylor PJ, Jomar K, Dhingra K, Forrester R, Shahmalak U, & Dickson JM (2018). A meta-analysis of the prevalence of different functions of non-suicidal self-injury. Journal of Affective Disorders, 227, 759–769. 10.1016/j.jad.2017.11.073 [DOI] [PubMed] [Google Scholar]
- Turner BJ, Cobb RJ, Gratz KL, & Chapman AL (2016). The role of interpersonal conflict and perceived social support in nonsuicidal self-injury in daily life. Journal of abnormal psychology, 125(4), 588–598. 10.1037/abn0000141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victor SE, & Klonsky ED (2014). Correlates of suicide attempts among self-injurers: A meta-analysis. Clinical Psychology Review, 34(4), 282–297. 10.1016/j.cpr.2014.03.005 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.