Abstract
Coronavirus disease-19 (COVID-19) pandemic is associated with high morbidity and mortality. COVID-19, which is caused by the Severe Acute Respiratory Syndrome Coronavirus-2 (SARS CoV-2), affects multiple organ systems through a myriad of mechanisms. Afflicted patients present with a vast constellation of symptoms, from asymptomatic disease to life-threatening complications. The most common manifestations pertain to mild pulmonary symptoms, which can progress to respiratory distress syndrome and venous thromboembolism. However, in patients with renal failure, life-threatening cardiac abnormalities can ensue. Various mechanisms such as viral entry through Angiotensin receptor (ACE) affecting multiple organs and thus releasing pro-inflammatory markers have been postulated. Nevertheless, the predictors of various presentations in the affected population remain elusive. An ameliorated understanding of the pathology and pathogenesis of the viral infection has led to the development of variable treatment options, with many more that are presently under trial. This review article discusses the pathogenesis of multiple organ involvement secondary to COVID-19 infection in infected patients.
Highlights
-
•
This review sheds light on the pathogenesis of multi-organ involvement secondary to COVID-19 infection.
-
•
The predictors of various presentations in the affected population are not clear at present. A better understanding of the pathology and pathogenesis of the viral infection will be pivotal in the development of variable treatment options.
-
•
Various proposed mechanisms such as viral entry through Angiotensin receptor (ACE) affecting multiple organs, releasing pro-inflammatory markers and cytokines inducing hypercoagulable state and cytokine storm syndrome have been postulated.
1. Introduction
The Coronavirus disease pandemic (COVID-19) caused by Severe Acute Respiratory Syndrome Coronavirus-2 (SARS CoV-2) has affected over 185 countries with a reported total number of 2,790,986 cases and 195,920 deaths [1]. The United States is one among the countries leading in COVID-19 associated infections and death rates [2]. The symptomatology associated with COVID-19 is variable from asymptomatic cases to multiorgan dysfunction and death [3]. Due to severe systemic inflammatory response from cytokine release, COVID-19 leads to end-organ damage and multiorgan failure (MOF) [3,4]. Understanding the underlying pathophysiology of COVID-19 for each organ system is critical for developing new therapies and improving management. We aim to do a systematic review of the literature to understand the pathophysiology of multiorgan involvement.
1.1. Multiorgan failure secondary to COVID-19
The multiorgan failure associated with COVID-19 is secondary to severe systemic inflammatory syndrome [3,4]. Studies have shown a strong association between ACE receptor and COVID-19 induced severe inflammatory response [5]. TMPRSS-2 is a serine protease involved in receptor-mediated endocytosis of SARS-CoV-2 [[6], [7], [8]]. The binding of SARS-CoV-2 virus results in the downregulation of ACE2 receptors, which means that angiotensin II levels begin to elevate. This elevation leads to a plethora of downstream effects on cytokine signaling, vascular homeostasis, and the coagulation cascade [5]. Cytokine storms can manifest as lymphopenia and elevated serum markers of inflammation including D-dimer, IL-6, ferritin and C-reactive protein (CRP) that can lead to multi organ failure [9].
1.2. Acute respiratory distress syndrome
Angiotensin-converting enzyme 2 (ACE2) receptor facilitate SARS-CoV-2 cell entry by providing a direct binding site for the S proteins of SARS-CoV-2 and promotes cleavage of angiotensin (Ang) I to produce Ang-(1–9) [10]. ACE2 receptors are widely expressed in the human body such as in nasal mucosa, bronchus, lung, heart, esophagus, kidney, stomach, bladder, and ileum which are all potential targets for COVID19 [11]. Once the virus enters, it induces ACE2 downregulation and shedding [10]. This is the primary mode of entry for SARS-COV2 and affects different organ systems. The ACE2 receptor expressed in the human airway epithelium is converted to active soluble ACE2 (sACE2) by disintegrin and metalloprotease 17.
Downregulation of ACE2 receptors is compensated by overproduction of angiotensin II (Ang II) by ACE which stimulates angiotensin II type 1a receptor that increases lung vascular permeability leading to acute lung injury and induces acute respiratory distress syndrome (ARDS) function [8]. Lung tissue has high RAS activity, enhanced during hypoxic state, and is the leading site of Ang II synthesis. Ang II is a pulmonary vasoconstrictor, resulting in pulmonary hypertension [5], and can also promote the occurrence of pulmonary edema and impair lung function [8].
In response to viral entry, the innate and adaptive immune system response secrete cytokines and inflammatory markers (see coagulopathy section) to combat the virus, specifically, increased production of cytokines interleukin-6 (IL-6), early induction of CXCL10, interleukin-2 (IL-2) and decreased production or absence of interleukin-10 (IL-10) which in turn promotes acute lung injury [12]. The viral overload and delayed type I interferon signaling further precipitate lung injury by accumulation of monocyte/macrophages that release cytokine/chemokine in the extracellular matrix and further attract accumulation of inflammatory cells induced inflammatory response and cell injury [12]. Excessive neutrophil can induce lung injury and CD8, cytotoxic T cells, contribute to lung damage from cytokines [12].
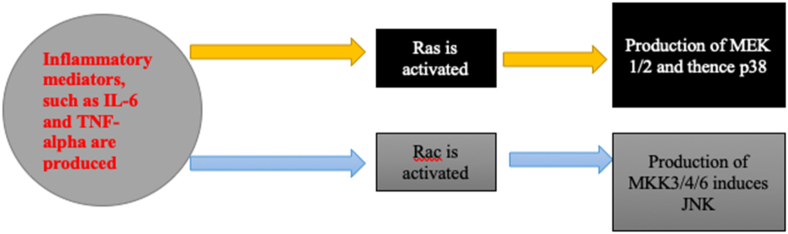
1.2.1. SARS-CoV-2 coagulopathy and thromboembolism
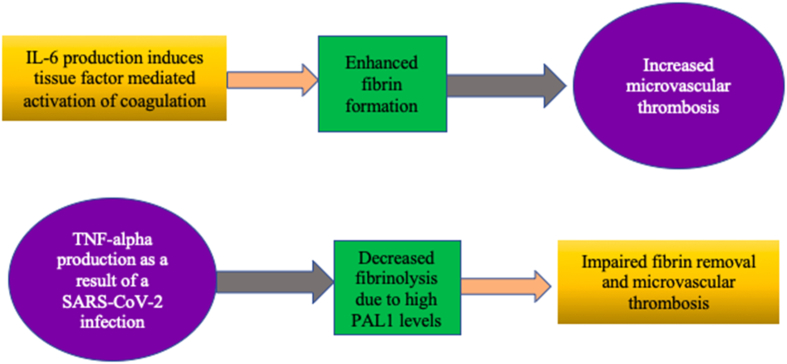
COVID-19 induced coagulopathy has been reported in many case reports ranging from immune thrombocytopenic purpura, deep venous thrombosis, carotid artery thrombus, pulmonary embolism, and disseminated intravascular coagulation (DIC) [10,[13], [14], [15], [16]]. Severe COVID-19 infection was associated with a more procoagulant state with higher rates of pulmonary embolism [9]. However, a meta-analysis by Mir et al. did not reveal any worsening in mortality in such critically ill patients with pulmonary embolism [17] The procoagulant state of COVID-19 infection is related with the inflammatory response of cytokines and tissue injury. Proteins expressed via SARS-CoV-2 virus likely delay the Type 1 IFN (interferon) release allowing fast viral replication, thus a dysregulated release of IFN-1 emerges [7]. As a result, proinflammatory cytokines, for example IL-6 and TNF-alpha stimulate neutrophils (PMNs) and monocytes thereby inciting a hyperinflammatory response, vascular leakage, and endothelial dysfunction [7]. Activated endothelial cells stimulate tissue factors and the extrinsic pathway whereas activated PMNs secrete neutrophil extracellular traps (NETs), which contain DAMPs that lead to activation of the intrinsic pathway via factor II. Further, combined activation of the intrinsic and extrinsic pathway coupled with reduced plasminogen activator inhibitor-1 (PAI-1) levels in ARDS resulting widespread thrombosis, a story similarly seen in the previous SARS-CoV-1 induced thrombosis [[18], [19], [20], [21]]. In addition, the upregulation of the Ang II-AT-1R axis, which promotes PAI-1 expression, the sequestration of platelets, and hypoxemia releasing a variety of hypoxia-inducible factors (HIF-1) add fuel to the impaired state [[22], [23], [24]]. High D-dimers observed in COVID-19 are representative of this dysfunctional coagulation activity requiring fibrin breakdown (Fig. 1).
Fig. 1.
Pathogenesis of the procoagulant state secondary to COVID-19.
1.2.2. COVID and pulmonary disease
COVID-19 infection is associated with acute respiratory distress syndrome from severe inflammatory response [16]. Burst of proinflammatory cytokines initiate alveolar injury, pulmonary edema, and reduced oxygenation within pulmonary vessels. This hypoxic state leads to pulmonary vasoconstriction, increased vascular permeability with an influx of inflammatory cells within the lung parenchyma, thereby reducing surfactant levels and atelectasis. A right-to-left shunt ensues a ventilation/perfusion mismatch with an increased physiological dead space [[25], [26], [27]]. As a result of hypoxic lung injury, viral replication follows unopposed activation of Angiotensin II [28].
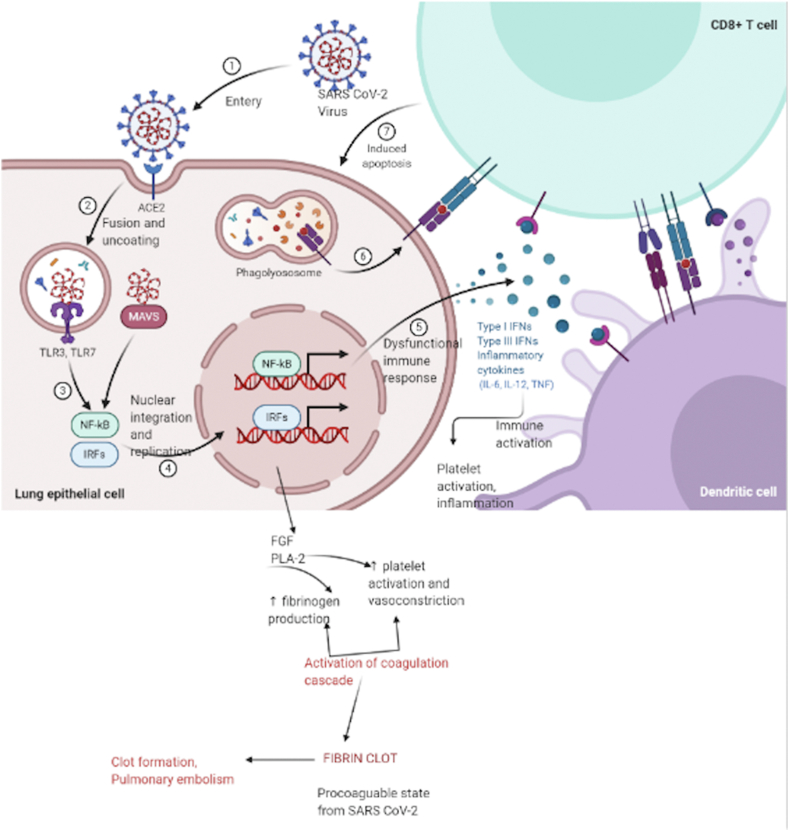
The elevations in Ang II and decreased ACE II expression post viral entry contribute to generation of reactive oxygen species through nuclear factor kappa light chain (NFkB) activation [24] (Fig. 2). The expression of inflammatory genes further lead to generation of proinflammatory cytokines like tumor necrosis factor alpha (TNF-alpha), interleukin-1 (IL-1), and IL-6. The cytokine surge contributes to endothelial dysfunction via uncoupled nitrous oxide (eNOS), increased endothelin-1(ET-1) levels, reactive thrombocytosis, and formation of emboli which lodge into pulmonary vessels causing acute hypoxic changes [29,30]. Oxygen deficient states also cause activation of hypoxia inducible factors (HIF1-alpha, enacting angiogenesis, elevated levels of fibrinogen, and consumption of clotting factors. Further, levels of PAL-1 lead to reduced depletion of fibrin causing perfusion deficiency and pulmonary dysfunction [4,31].
Fig. 2.
The mechanisms underlying SARS-CoV-2 induced ARDS [1] a hypothetical model of SARCoV-2 virus demonstrating infectious pathways to cell entery, induce inflammation, ARDS and procoagulation state. SARS CoV-2; Severe Acute Respiratory Syndrome Coronavirus-2, IL-6; Interleukin −6, TNFα; Tumor necrosis alpha, IL 1-β; Interleukin 1-beta, ACE II; Angiotensin converting enzyme II, Ang II; Angiotensin II (Created with BioRender.com).
1.3. Acute kidney injury
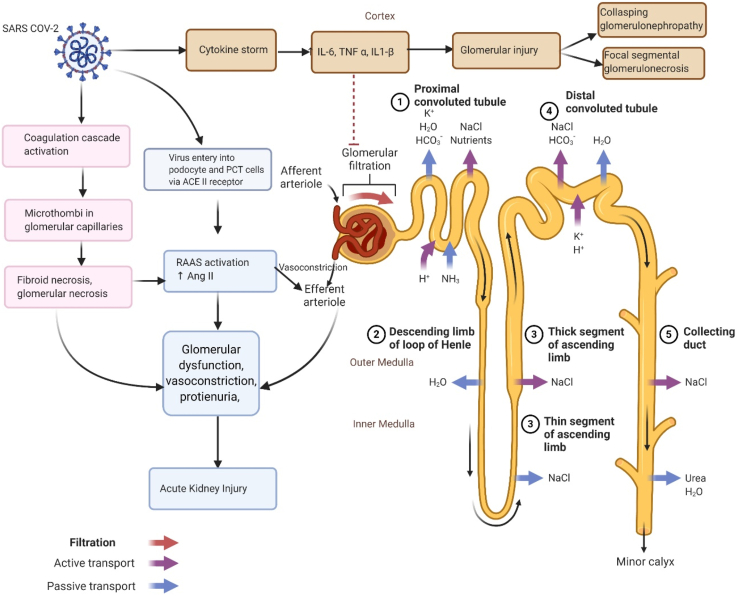
The mechanisms involved in heralding the onset of acute kidney injury (AKI) remain elusive, but a concoction of factors, such as hemodynamic changes, fluid overload, right heart failure, and cytokine-storm, might be at play in eliciting AKI [13]. The mechanistic features underlying AKI are therefore the subject of extensive medical research, and we hereby detail a schematic representation of the etiology underlying AKI.
Cytokines produced as part of a SARS-CoV-2 response, such as IL-6, upregulates the expression of sodium hydrogen exchangers. As a result, the adenosine triphosphatase (ATPase) molecules undergo hypertrophy. Complementing this tubular ATPase hypertrophy is hypoxia, which routinely results as a ramification of ARDS [25]. The hypoxia results in increased aldosterone retention, which consequently increases water retention, worsening renal failure. It is imperative to note, also, that AKI portends worse outcomes if it is superimposed on an existing chronic kidney disease (CKD) [13]. Increased acid secretion levels eventually lead to increased intraglomerular pressure, thereby damaging the filtration barrier. To compensate, tubular fibroblasts release mediators, such as NFKB and ETS-1, which culminate in tubular atrophy, inflammation, and fibrosis) [13]. The summary for mechanisms of AKI is shown in Fig. 3.
Fig. 3.
Pathogenesis underlying the acute kidney injury (AKI) seen in SARS-CoV-2. SARS CoV-2; Severe Acute Respiratory Syndrome Coronavirus-2, IL-6; Interleukin −6, TNFα; Tumor necrosis alpha, IL 1-β; Interleukin 1-beta, ACE II; Angiotensin converting enzyme II, Ang II; Angiotensin II (Created with BioRender.com).
1.3.1. Cardiovascular complications: heart failure, STEMI, arrhythmias, and cardiac tamponade
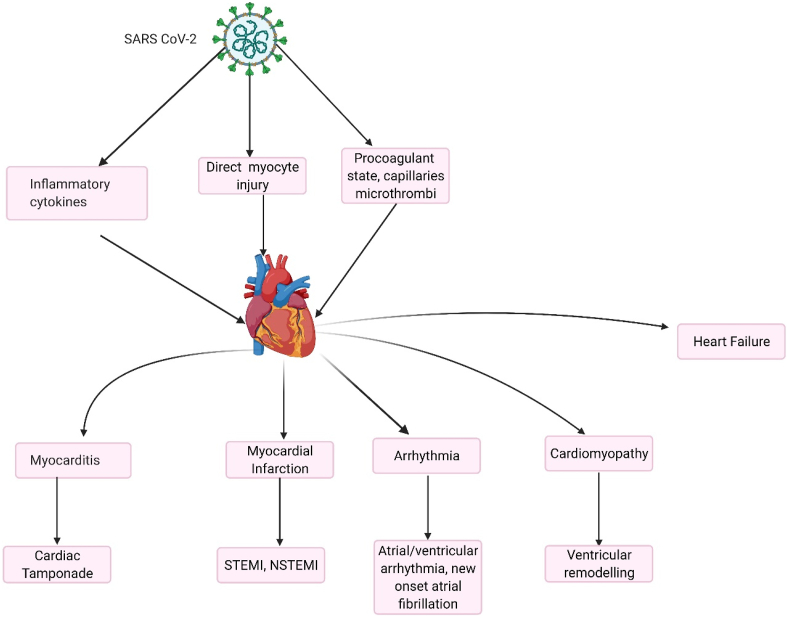
COVID-19 can cause cardiac complications such as myocarditis. Clinically, patients might present with chest pain, dyspnea, arrhythmias, and acute coronary syndrome (ACS) [17]. Distinguishing between ACS and myocarditis in an acute setting might be challenging. A proposed mechanism that explains myocarditis is elucidated. In addition to the mentioned cardiovascular side effects, SARS-CoV-2 also causes heart failure, pericarditis, cardiac tamponade, arrhythmias and thromboembolic events. It is presently understood that electrolyte disturbances, coupled oxidation of the Ca2+/Calmodulin-dependent protein kinase 2 is responsible for the arrhythmias seen amid a SARS-CoV-2 infection [26].
Similarly, the exorbitant increase in the production of IL-6 upregulates the expression of vascular endothelial growth factor (VEGF) resulting in increased vessel permeability and effusion that may progress to cardiac tamponade [32]. Additionally, due to deranged coagulation profiles and increased circulating levels of angiotensin II, downstream pathways involving endothelial dysfunction and oxidative stress herald the onset of thromboembolic events [3].
The stimulation of these pathways lead to increased production of mononuclear infiltrates, which are directed towards the myocardium, and might result in subsequent myocarditis [33]. The elevated troponin levels among patients with COVID-19 might be a result of demand ischemia rather than myocarditis itself [11]). It is therefore of clinical relevance that the troponin levels are not used exclusively, but instead in conjunction with the overall clinical picture, to yield a diagnosis of myocarditis. The graphic representation of cardiovascular pathology is in Fig. 4.
Fig. 4.
Cardiovascular pathology of COVID-19. SARS CoV-2; Severe Acute Respiratory Syndrome Coronavirus-2STEMI; ST-elevation myocardial Infarction, NSTEMI; Non-ST elevation myocardial infarction (Created with BioRender.com).
Both above detailed pathways lead to increased production of mononuclear infiltrates, which are directed towards the myocardium, leading to myocarditis [33]. Fig. 5. In study by Deng et al. troponemia in myocarditis suspect can be a demand for ischemia in the setting of COVID-19 rather than myocarditis itself [11]. It is therefore of clinical relevance that the troponin levels are not used exclusively, but instead in conjunction with the overall clinical picture, to yield a diagnosis of myocarditis.
Fig. 5.
Pathogenesis of myocarditis in COVID-19 infection.
1.4. Gastrointestinal
The colon and small intestine have higher expression of ACE2 receptors mainly in the endothelium and the vascular smooth muscle cells [34]. SARS-CoV-2 is associated with infiltration of plasma cells and lymphocytes in the lamina propria of stomach, duodenum and rectum that promotes interstitial edema. ACE2 receptor is also associated with neutral amino acid transporters in the gastrointestinal tract and plays an essential role. In patients with amino acid malnutrition, ACE2 promotes intestinal inflammation. ACE2 plays a significant role in amino acid homeostasis and maintaining intestinal microbiota [34]. Downregulation or alteration of ACE2 is associated with colitis, by promoting intestinal inflammation and diarrhea suggesting that SARS-Co-2 entry via ACE2 receptor may alter its activity. The proposed model is that COVID19 uses ACE2 and TMPRSS22 to enter the gut [35].
The entry of SARS-CoV-2 into the host cell begins by the binding of viral spike glycoprotein with ACE2 protein followed by processing of the spike glycoprotein by TMPRSS2 leading to membrane fusion, and recent evidence suggests an additive effect of TMPRSS4 in viral entry [35]. TMPRSS serine proteases facilitate virus infection by inducing S cleavage and exposing the fusion peptide for efficient viral entry in gastrointestinal (GI) tract [35] Inflammatory response induced by SARS-CoV-2 can also lead to direct injury of GI tract, destroying absorptive enterocytes, potentially leading to malabsorption, unbalanced intestinal secretion, and enteric nervous system [[34], [58]]. Additionally, hyperinflammation and dysregulated immune responses lead to cytokine surge which may culminate in widespread injury and serious complications like paralytic ileus and hemorrhagic colitis [22,36].
1.4.1. Neurologic manifestation
Significant neurologic complications such as increased risk for ischemic and hemorrhagic stroke have become increasingly associated with COVID-19. There are many case reports and observational studies demonstrating that these patients presented with stroke often in the early stages of their illness [37,38]. Cytokine release induced hypercoagulability (as evidenced by remarkable D-Dimer elevation) contributes to significant downstream thrombus formation. Hypoxemia leading to intracellular acidosis and down-stream production of oxygen free radicals, compounded by the influx of proinflammatory cytokines, may lead to neuronal tissue ischemia. It is known that inflammation contributes significantly to atherosclerosis and increases the instability of plaques, predisposing to stroke [39].
When SARS-CoV-2 binds with ACE II receptors, patients with underlying hypertension may additionally be affected by extremes of high blood pressure, putting them at risk for intracerebral hemorrhage. Some patient cohorts have also been shown to present with thrombocytopenia, further increasing risk of intracerebral bleeding [40].
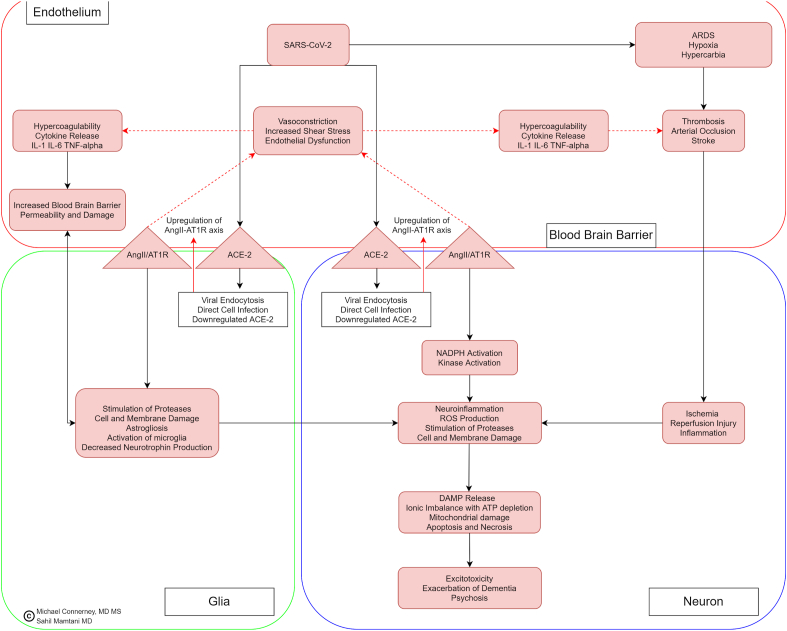
Inflammatory response and cytokine storm can affect the central nervous system by inducing toxic metabolic encephalopathy. In one confirmed case, a patient presented with fever and cough, which later progressed to acute necrotizing encephalopathy related to the cytokine storm [38]. There are also case reports of meningitis, confirmed by detection of the virus within the CSF, and hippocampal sclerosis leading to post-convulsive encephalopathy from COVID-19 [41] (Fig. 6).
Fig. 6.
Neurologic involvement in COVID-19.
SARS-CoV-2 binding to ACE-2 Receptors followed by viral endocytosis causes upregulation of Ang II/AT-1R; this results in endothelial dysfunction which includes vasoconstriction and increased shear stress. Endothelial dysfunction leads to cytokine release, including Il-1, Il-6 and TNF-alpha, culminating in increased blood brain barrier permeability. This increased inflammatory cytokine activity leads to hypercoagulability. The hypercoagulable state leading to stroke compounded by ARDS hypoxemia leads to downstream neuronal ischemia, inflammation, and necrosis secondary to reperfusion injury [[42], [43], [44], [45], [46], [47]]. Ang-II/AT1R upregulation related enzymatic activity within both glial cells and neurons, in addition to ischemia and reperfusion injury, leads to reactive oxygen species production, stimulation of proteases, with cell and membrane damage as a result [[48], [49], [50], [51], [52]]. Apoptosis of neurons occurs because of DAMP release from cell membrane damage, ATP depletion, and mitochondrial damage [[53], [54], [55], [57], [58]].
The downstream effects of this neuro-inflammatory process and excitotoxicity may manifest as altered mental status including psychosis and exacerbation of existing dementia.
1.5. Future directions
This review gives a potential pathophysiological mechanism behind SARS-CoV-2 infection for every system that it involves. The evidence behind these mechanisms is based on experience with similar coronaviruses and other viral infections of the same class, as well as clinical characteristics, laboratory findings, and postmortem pathological reports of COVID-19 patients around the world. The main concern is the exact contribution of risk factors to disease progression in different age, sex and race groups. Additionally, more studies are needed to understand the main drivers of COVID-19 and their molecular mechanisms of action especially in different age groups, which would help for appropriate risk stratification and therapeutic strategies. From our understanding of the published studies and evidence, immunomodulatory therapies are more likely to be equally and also very effective than just targeting virus at different stages of cycle in humans. Furthermore, treatment approaches may be further tailored to support immune response earlier during disease progression to enhance an efficient antiviral response and also to prevent progression of the disease into multi system inflammatory syndrome.
2. Conclusion
COVID-19 has been related as a respiratory illness, however through our extensive review of systems it can now be considered as a complex multisystem disorder. Moreover, there is a need to better understand the varied presentation of symptoms and organ involvement in different populations, nevertheless with the emerging epidemiology and basic science evidence, there has been some understanding of susceptibility of the infection and its outcomes. Even with initiation of mass vaccination drive of COVID vaccines the SARS-CoV-2 infection is expected to continue to be a burden to the healthcare sector and also to the country's economy. Hence there is need for more prospective studies to better understand this disease and varied involvements of the organs in different patients so that an effective therapy can be directed.
Ethical approval
Research studies involving patients require ethical approval. Please state whether approval has been given, name the relevant ethics committee and the state the reference number for their judgement.
NA.
Author contribution
TM, YS, TA: conceived the idea, designed the study, and drafted the manuscript. DS, JK, WU, SM: conducted literature search and created the illustrations. HR, SY, SL: revised the manuscript critically and refined the illustrations. TM, YS, TA, MCA: revised the final version of the manuscript critically and gave the final approval. YS conceived the idea and led this project.
Guarantor
The Guarantor is the one or more people who accept full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Talal Almas.
Financial conflict
None.
Declaration of competing interest
None.
Contributor Information
Talal Almas, Email: talalalmas.almas@gmail.com.
Yasar Sattar, Email: mdyasarsattar@gmail.com.
References
- 1.Amawi H., Abu Deiab G.I., Aa A.A., Dua K., Tambuwala M.M. COVID-19 pandemic: an overview of epidemiology, pathogenesis, diagnostics and potential vaccines and therapeutics. Ther. Deliv. 2020;11:245–268. doi: 10.4155/tde-2020-0035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Weinberger D.M., Chen J., Cohen T., Crawford F.W., Mostashari F., Olson D., Pitzer V.E., Reich N.G., Russi M., Simonsen L., Watkins A., Viboud C. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, march to may 2020. JAMA Intern Med. 2020;180:1336–1344. doi: 10.1001/jamainternmed.2020.3391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Siddiqi H.K., Mehra M.R. COVID-19 illness in native and immunosuppressed states: a clinical-therapeutic staging proposal. J. Heart Lung Transplant. 2020;39:405–407. doi: 10.1016/j.healun.2020.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang T., Du Z., Zhu F., Cao Z., An Y., Gao Y., Jiang B. Comorbidities and multi-organ injuries in the treatment of COVID-19. Lancet (London, England) 2020;395:e52. doi: 10.1016/S0140-6736(20)30558-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Budhiraja R., Tuder R.M., Hassoun P.M. Endothelial dysfunction in pulmonary hypertension. Circulation. 2004;109:159–165. doi: 10.1161/01.CIR.0000102381.57477.50. [DOI] [PubMed] [Google Scholar]
- 6.Shieh W.J., Hsiao C.H., Paddock C.D., Guarner J., Goldsmith C.S., Tatti K., Packard M., Mueller L., Wu M.Z., Rollin P., Su I.J., Zaki S.R. Immunohistochemical, in situ hybridization, and ultrastructural localization of SARS-associated coronavirus in lung of a fatal case of severe acute respiratory syndrome in Taiwan. Hum. Pathol. 2005;36:303–309. doi: 10.1016/j.humpath.2004.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Millet J.K., Whittaker G.R. Host cell entry of Middle East respiratory syndrome coronavirus after two-step, furin-mediated activation of the spike protein. Proc. Natl. Acad. Sci. U. S. A. 2014;111:15214–15219. doi: 10.1073/pnas.1407087111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoffmann M., Kleine-Weber H., Schroeder S., Krüger N., Herrler T., Erichsen S., Schiergens T.S., Herrler G., Wu N.-H., Nitsche A. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;12(12) doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ruan Q., Yang K., Wang W., Jiang L., Song J. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46:846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fu Y., Cheng Y., Wu Y. Understanding SARS-CoV-2-mediated inflammatory responses: from mechanisms to potential therapeutic tools. Virol. Sin. 2020;35:266–271. doi: 10.1007/s12250-020-00207-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jin Y., Yang H., Ji W., Wu W., Chen S., Zhang W., Duan G. 2020. Virology, Epidemiology, Pathogenesis, and Control of COVID-19. Viruses12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yuki K., Fujiogi M., Koutsogiannaki S. COVID-19 pathophysiology: a review. Clin. Immunol. 2020;215:108427. doi: 10.1016/j.clim.2020.108427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Helms J., Tacquard C., Severac F., Leonard-Lorant I., Ohana M., Delabranche X., Merdji H., Clere-Jehl R., Schenck M., Fagot Gandet F., Fafi-Kremer S., Castelain V., Schneider F., Grunebaum L., Angles-Cano E., Sattler L., Mertes P.M., Meziani F., Group C.T. High risk of thrombosis in patients with severe SARS-CoV-2 infection: a multicenter prospective cohort study. Intensive Care Med. 2020;46:1089–1098. doi: 10.1007/s00134-020-06062-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lillicrap D. Disseminated intravascular coagulation in patients with 2019-nCoV pneumonia. J. Thromb. Haemostasis : JTH. 2020;18:786–787. doi: 10.1111/jth.14781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oxley T.J., Mocco J., Majidi S., Kellner C.P., Shoirah H., Singh I.P., De Leacy R.A., Shigematsu T., Ladner T.R., Yaeger K.A., Skliut M., Weinberger J., Dangayach N.S., Bederson J.B., Tuhrim S., Fifi J.T. Large-vessel stroke as a presenting feature of covid-19 in the young. N. Engl. J. Med. 2020;382:e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zulfiqar A.A., Lorenzo-Villalba N., Hassler P., Andres E. Immune thrombocytopenic purpura in a patient with covid-19. N. Engl. J. Med. 2020;382:e43. doi: 10.1056/NEJMc2010472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72314 cases from the Chinese center for disease control and prevention. J. Am. Med. Assoc. 2020;323:1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 18.Gralinski L.E., Bankhead A., 3rd, Jeng S., Menachery V.D., Proll S., Belisle S.E., Matzke M., Webb-Robertson B.J., Luna M.L., Shukla A.K., Ferris M.T., Bolles M., Chang J., Aicher L., Waters K.M., Smith R.D., Metz T.O., Law G.L., Katze M.G., McWeeney S., Baric R.S. Mechanisms of severe acute respiratory syndrome coronavirus-induced acute lung injury. mBio. 2013;4 doi: 10.1128/mBio.00271-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Keragala C.B., Draxler D.F., McQuilten Z.K., Medcalf R.L. Haemostasis and innate immunity - a complementary relationship: a review of the intricate relationship between coagulation and complement pathways. Br. J. Haematol. 2018;180:782–798. doi: 10.1111/bjh.15062. [DOI] [PubMed] [Google Scholar]
- 20.Jackson S.P., Darbousset R., Schoenwaelder S.M. Thromboinflammation: challenges of therapeutically targeting coagulation and other host defense mechanisms. Blood. 2019;133:906–918. doi: 10.1182/blood-2018-11-882993. [DOI] [PubMed] [Google Scholar]
- 21.Lippi G., Adcock D., Favaloro E.J. Understanding the "philosophy" of laboratory hemostasis. Diagnosis (Berl) 2019;6:223–226. doi: 10.1515/dx-2018-0099. [DOI] [PubMed] [Google Scholar]
- 22.Morrell C.N., Aggrey A.A., Chapman L.M., Modjeski K.L. Emerging roles for platelets as immune and inflammatory cells. Blood. 2014;123:2759–2767. doi: 10.1182/blood-2013-11-462432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ozolina A., Sarkele M., Sabelnikovs O., Skesters A., Jaunalksne I., Serova J., Ievins T., Bjertnaes L.J., Vanags I. Activation of coagulation and fibrinolysis in acute respiratory distress syndrome: a prospective pilot study. Front. Med. 2016;3:64. doi: 10.3389/fmed.2016.00064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Evans C.E. Hypoxia and HIF activation as a possible link between sepsis and thrombosis. Thromb. J. 2019;17:16. doi: 10.1186/s12959-019-0205-9. 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim J.M., Heo H.S., Ha Y.M., Ye B.H., Lee E.K., Choi Y.J., Yu B.P., Chung H.Y. Mechanism of Ang II involvement in activation of NF-kappaB through phosphorylation of p65 during aging. Age (Dordr) 2012;34:11–25. doi: 10.1007/s11357-011-9207-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thompson B.T., Chambers R.C., Liu K.D. Acute respiratory distress syndrome. N. Engl. J. Med. 2017;377:562–572. doi: 10.1056/NEJMra1608077. [DOI] [PubMed] [Google Scholar]
- 27.Luks A.M., Swenson E.R. COVID-19 lung injury and high altitude pulmonary edema: a false equation with dangerous implications. Ann Am Thorac Soc. 2020;2020 doi: 10.1513/AnnalsATS.202004-327FR. [DOI] [PubMed] [Google Scholar]
- 28.Perlman S., Netland J. Coronaviruses post-SARS: update on replication and pathogenesis. Nat. Rev. Microbiol. 2009;7:439–450. doi: 10.1038/nrmicro2147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nakamura-Utsunomiya A., Tsumura M., Okada S., Kawaguchi H., Kobayashi M. Downregulation of endothelial nitric oxide synthase (eNOS) and endothelin-1 (ET-1) in a co-culture system with human stimulated X-linked CGD neutrophils. PloS One. 2020;15 doi: 10.1371/journal.pone.0230665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Xu J., Sun Y., Lu J. Knockdown of long noncoding RNA (lncRNA) AK094457 relieved angiotensin II induced vascular endothelial cell injury. Med. Sci. Mon. Int. Med. J. Exp. Clin. Res. 2020;26 doi: 10.12659/MSM.919854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhao X., Jin Y., Li H., Wang Z., Zhang W., Feng C. Hypoxia-inducible factor 1 alpha contributes to pulmonary vascular dysfunction in lung ischemia-reperfusion injury. Int. J. Clin. Exp. Pathol. 2014;7:3081–3088. [PMC free article] [PubMed] [Google Scholar]
- 32.Purohit A., Rokita A.G., Guan X., Chen B., Koval O.M., Voigt N., Neef S., Sowa T., Gao Z., Luczak E.D., Stefansdottir H., Behunin A.C., Li N., El-Accaoui R.N., Yang B., Swaminathan P.D., Weiss R.M., Wehrens X.H., Song L.S., Dobrev D., Maier L.S., Anderson M.E. Oxidized Ca(2+)/calmodulin-dependent protein kinase II triggers atrial fibrillation. Circulation. 2013;128:1748–1757. doi: 10.1161/CIRCULATIONAHA.113.003313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Liu K., Fang Y.Y., Deng Y., Liu W., Wang M.F., Ma J.P., Xiao W., Wang Y.N., Zhong M.H., Li C.H., Li G.C., Liu H.G. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin. Med. J. 2020;133:1025–1031. doi: 10.1097/CM9.0000000000000744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhang H., Li H.B., Lyu J.R., Lei X.M., Li W., Wu G., Lyu J., Dai Z.M. Specific ACE2 expression in small intestinal enterocytes may cause gastrointestinal symptoms and injury after 2019-nCoV infection. Int. J. Infect. Dis. 2020;96:19–24. doi: 10.1016/j.ijid.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Patel K.P., Patel P.A., Vunnam R.R., Hewlett A.T., Jain R., Jing R., Vunnam S.R. Gastrointestinal, hepatobiliary, and pancreatic manifestations of COVID-19. J. Clin. Virol. : the official publication of the Pan American Society for Clinical Virology. 2020;128:104386. doi: 10.1016/j.jcv.2020.104386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Qin C., Zhou L., Hu Z., Zhang S., Yang S., Tao Y., Xie C., Ma K., Shang K., Wang W., Tian D.S. Dysregulation of immune response in patients with coronavirus 2019 (COVID-19) in wuhan, China. Clin. Infect. Dis. : an official publication of the Infectious Diseases Society of America. 2020;71:762–768. doi: 10.1093/cid/ciaa248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Avula A., Nalleballe K., Narula N., Sapozhnikov S., Dandu V., Toom S., Glaser A., Elsayegh D. COVID-19 presenting as stroke. Brain Behav. Immun. 2020;87:115–119. doi: 10.1016/j.bbi.2020.04.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ntaios G., Michel P., Georgiopoulos G., Guo Y., Li W., Xiong J., Calleja P., Ostos F., González-Ortega G., Fuentes B., Alonso de Leciñana M., Díez-Tejedor E., García-Madrona S., Masjuan J., DeFelipe A., Turc G., Gonçalves B., Domigo V., Dan G.A., Vezeteu R., Christensen H., Christensen L.M., Meden P., Hajdarevic L., Rodriguez-Lopez A., Díaz-Otero F., García-Pastor A., Gil-Nuñez A., Maslias E., Strambo D., Werring D.J., Chandratheva A., Benjamin L., Simister R., Perry R., Beyrouti R., Jabbour P., Sweid A., Tjoumakaris S., Cuadrado-Godia E., Campello A.R., Roquer J., Moreira T., Mazya M.V., Bandini F., Matz K., Iversen H.K., González-Duarte A., Tiu C., Ferrari J., Vosko M.R., Salzer H.J.F., Lamprecht B., Dünser M.W., Cereda C.W., Quintero Á B.C., Korompoki E., Soriano-Navarro E., Soto-Ramírez L.E., Castañeda-Méndez P.F., Bay-Sansores D., Arauz A., Cano-Nigenda V., Kristoffersen E.S., Tiainen M., Strbian D., Putaala J., Lip G.Y.H. Characteristics and outcomes in patients with COVID-19 and acute ischemic stroke: the global COVID-19 stroke registry. Stroke. 2020;51:e254–e258. doi: 10.1161/STROKEAHA.120.031208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ramji D.P., Davies T.S. Cytokines in atherosclerosis: key players in all stages of disease and promising therapeutic targets. Cytokine Growth Factor Rev. 2015;26:673–685. doi: 10.1016/j.cytogfr.2015.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chan J.F., Yuan S., Kok K.H., To K.K., Chu H., Yang J., Xing F., Liu J., Yip C.C., Poon R.W., Tsoi H.W., Lo S.K., Chan K.H., Poon V.K., Chan W.M., Ip J.D., Cai J.P., Cheng V.C., Chen H., Hui C.K., Yuen K.Y. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet (London, England) 2020;395:514–523. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Poyiadji N., Shahin G., Noujaim D., Stone M., Patel S., Griffith B. COVID-19-associated acute hemorrhagic necrotizing encephalopathy: imaging features. Radiology. 2020;296:E119–E120. doi: 10.1148/radiol.2020201187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moriguchi T., Harii N., Goto J., Harada D., Sugawara H., Takamino J., Ueno M., Sakata H., Kondo K., Myose N., Nakao A., Takeda M., Haro H., Inoue O., Suzuki-Inoue K., Kubokawa K., Ogihara S., Sasaki T., Kinouchi H., Kojin H., Ito M., Onishi H., Shimizu T., Sasaki Y., Enomoto N., Ishihara H., Furuya S., Yamamoto T., Shimada S. A first case of meningitis/encephalitis associated with SARS-Coronavirus-2. Int. J. Infect. Dis. 2020;94:55–58. doi: 10.1016/j.ijid.2020.03.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Farha S. COVID-19 and pulmonary hypertension. Cleve. Clin. J. Med. 2020;2020 doi: 10.3949/ccjm.87a.ccc021. [DOI] [PubMed] [Google Scholar]
- 44.Bikdeli B., Madhavan M.V., Jimenez D., Chuich T., Dreyfus I., Driggin E., Nigoghossian C., Ageno W., Madjid M., Guo Y., Tang L.V., Hu Y., Giri J., Cushman M., Quere I., Dimakakos E.P., Gibson C.M., Lippi G., Favaloro E.J., Fareed J., Caprini J.A., Tafur A.J., Burton J.R., Francese D.P., Wang E.Y., Falanga A., McLintock C., Hunt B.J., Spyropoulos A.C., Barnes G.D., Eikelboom J.W., Weinberg I., Schulman S., Carrier M., Piazza G., Beckman J.A., Steg P.G., Stone G.W., Rosenkranz S., Goldhaber S.Z., Parikh S.A., Monreal M., Krumholz H.M., Konstantinides S.V., Weitz J.I., Lip G.Y.H. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J. Am. Coll. Cardiol. 2020;75:2950–2973. doi: 10.1016/j.jacc.2020.04.031. Global Covid-19 Thrombosis Collaborative Group EbtINE, the Iua SbtESCWGoPC & Right Ventricular F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Branchford B.R., Carpenter S.L. The role of inflammation in venous thromboembolism. Front Pediatr. 2018;6:142. doi: 10.3389/fped.2018.00142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Channappanavar R., Fehr A.R., Vijay R., Mack M., Zhao J., Meyerholz D.K., Perlman S. Dysregulated type I interferon and inflammatory monocyte-macrophage responses cause lethal pneumonia in SARS-CoV-infected mice. Cell Host Microbe. 2016;19:181–193. doi: 10.1016/j.chom.2016.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cheng H., Wang Y., Wang G.Q. Organ-protective effect of angiotensin-converting enzyme 2 and its effect on the prognosis of COVID-19. J. Med. Virol. 2020;92:726–730. doi: 10.1002/jmv.25785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Contou D., Pajot O., Cally R., Logre E., Fraissé M., Mentec H., Plantefève G. Pulmonary embolism or thrombosis in ARDS COVID-19 patients: a French monocenter retrospective study. PloS One. 2020;15 doi: 10.1371/journal.pone.0238413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.de Barry O., Mekki A., Diffre C., Seror M., El Hajjam M., Carlier R.Y. Arterial and venous abdominal thrombosis in a 79-year-old woman with COVID-19 pneumonia. Radiol Case Rep. 2020;15:1054–1057. doi: 10.1016/j.radcr.2020.04.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Deng Q., Hu B., Zhang Y., Wang H., Zhou X., Hu W., Cheng Y., Yan J., Ping H., Zhou Q. Suspected myocardial injury in patients with COVID-19: evidence from front-line clinical observation in Wuhan, China. Int. J. Cardiol. 2020;311:116–121. doi: 10.1016/j.ijcard.2020.03.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fanelli V., Fiorentino M., Cantaluppi V., Gesualdo L., Stallone G., Ronco C., Castellano G. Acute kidney injury in SARS-CoV-2 infected patients. Crit. Care. 2020;24:155. doi: 10.1186/s13054-020-02872-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Gattinoni L., Coppola S., Cressoni M., Busana M., Rossi S., Chiumello D. COVID-19 does not lead to a "typical" acute respiratory distress syndrome. Am. J. Respir. Crit. Care Med. 2020;201:1299–1300. doi: 10.1164/rccm.202003-0817LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kennedy C., Leak A. Eosinophilic fasciitis with erosive arthritis. Clin. Exp. Dermatol. 1982;7:469–476. doi: 10.1111/j.1365-2230.1982.tb02462.x. [DOI] [PubMed] [Google Scholar]
- 54.Lakkireddy D.R., Chung M.K., Gopinathannair R., Patton K.K., Gluckman T.J., Turagam M., Cheung J., Patel P., Sotomonte J., Lampert R., Han J.K., Rajagopalan B., Eckhardt L., Joglar J., Sandau K., Olshansky B., Wan E., Noseworthy P.A., Leal M., Kaufman E., Gutierrez A., Marine J.E., Wang P.J., Russo A.M. Guidance for cardiac electrophysiology during the COVID-19 pandemic from the heart rhythm society COVID-19 task force; electrophysiology section of the American college of cardiology; and the electrocardiography and arrhythmias committee of the council on clinical cardiology, American heart association. Circulation. 2020;141:e823–e831. doi: 10.1161/CIRCULATIONAHA.120.047063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Millet J.K., Whittaker G.R. Host cell entry of Middle East respiratory syndrome coronavirus after two-step, furin-mediated activation of the spike protein. Proc. Natl. Acad. Sci. U. S. A. 2014;111:15214–15219. doi: 10.1073/pnas.1407087111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Stefanini T., Calvosa S., Fiocchi R., Lagana G. [Hemodynamic changes in elderly patients after Ender nailing procedures] Chir. Organi Mov. 1982;68:201–205. [PubMed] [Google Scholar]
- 58.Almas Talal. The many faces of coronavirus disease 2019: COVID-19 and the liver. Ann. Med. Surg. (Lond.) 2021;64:102224. doi: 10.1016/j.amsu.2021.102224. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]