Abstract
Chimeric antigen receptor (CAR) T-cell therapy is an emerging highly effective treatment for refractory haematological malignancies. Unfortunately, its therapeutic benefit may be hampered by treatment-related toxicities, including neurotoxicity. Early aggressive treatment is paramount to prevent neurological sequelae, yet it potentially interferes with the anti-cancer action of CAR T-cells. We describe four CAR T-cells infused patients who presented with reiterative writing behaviours, namely paligraphia, as an early manifestation of neurotoxicity, and eventually developed frontal predominant encephalopathy (one mild, three severe). Paligraphia may represent an early, specific, and easily detectable clinical finding of CAR T-cell therapy-related neurotoxicity, potentially informing its management.
Keywords: B-cell lymphoma, Immune effectors cell-associated neurotoxicity syndrome (ICANS), Cytokine release syndrome (CRS), CAR-T therapy, Cytokine storm-associated encephalopathy (CySE), Anakinra
Introduction
Chimeric antigen receptor (CAR) T-cell therapy is emerging as a highly effective treatment for refractory haematological malignancies [1]. Unfortunately, its therapeutic benefit may be hampered by treatment-related toxicities consisting in cytokine release syndrome (CRS) and neurotoxicity, namely immune effector cell-associated neurotoxicity syndrome (ICANS) [2]. The former is a well-known life-threatening systemic inflammatory syndrome resulting from the activation of the infused T cells and consequent release of circulating cytokines, which usually manifests with fever, hypoxia and hypotension [2]. Conversely, the biological underpinnings of ICANS have not been fully elucidated, yet a clear relationship between CRS and neurotoxicity has been observed [3–5] likely involving cytokine-mediated neuroinflammatory mechanisms [6]. Clinical manifestations of ICANS are heterogeneous and may have a progressive or fluctuating course, ranging from mild cognitive slowing, headache and tremor, to language disorders, seizure, motor deficits and encephalopathy, potentially leading to akinetic mutism and death [2, 3]. Steroids are currently the first-line therapy for ICANS, despite potential interference with CAR T-cell anti-tumour action [2, 5, 7, 8]. Hence, it is paramount to identify early clinical and instrumental findings of neurotoxicity to detect early stages of ICANS, define the prognosis and guide the appropriate treatment.
Methods
We collected data from CAR T-cell therapy candidates affected by refractory advanced diffuse large B cell lymphoma (DLBCL) at Institute of Haematology “Seragnoli” (Advanced Cell Therapy Program, IRCCS AOU Bologna, Italy) from September 2019 to March 2021. Twenty-eight patients were evaluated through a comprehensive neurological screening for both clinical and research purposes (neurological examination, EEG, brain MRI, nerve conduction study, neuropsychological tests) 15–30 days before infusion to exclude CNS involvement and start prophylactic anti-seizure medication (levetiracetam 750 mg twice a day), which then was gradually tapered and discontinued [9]. From the day of CAR T-cells infusion, patients were hospitalized for at least 15 days and underwent neurological examinations and EEG every other day to monitor any development of neurotoxicity. CRS and ICANS were assessed and graded based on the Consensus published by Lee et al. [2], using the Immune Effector Cell-associated Encephalopathy (ICE) score at each visit. Whenever a patient developed ICANS, daily neurological evaluation and further diagnostic tests guided by neurological manifestations were performed. We observed nine cases of ICANS (five mild: ≤ 2 grade; and four severe: ≥ 3 grade), among whom we report four cases who presented with a similar writing disorder, paligraphia, as an early neurotoxicity sign.
Results
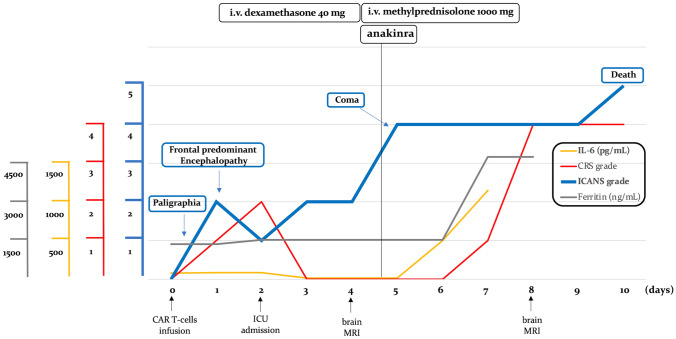
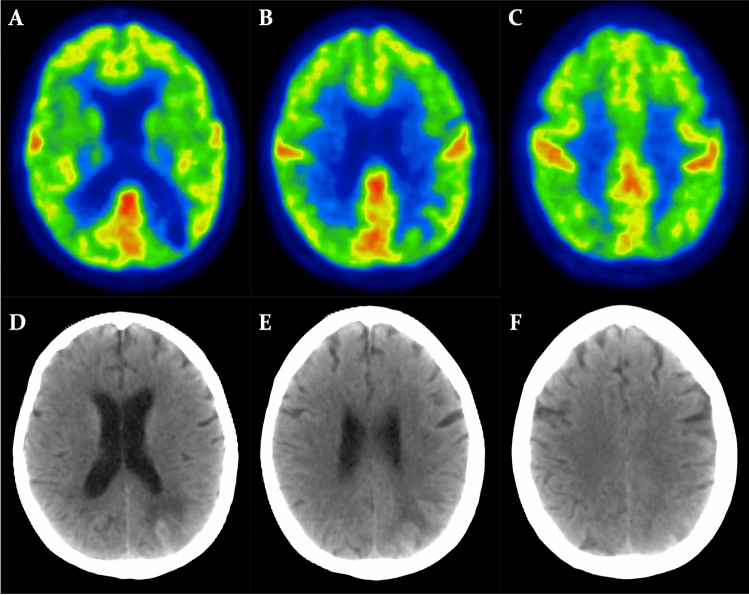
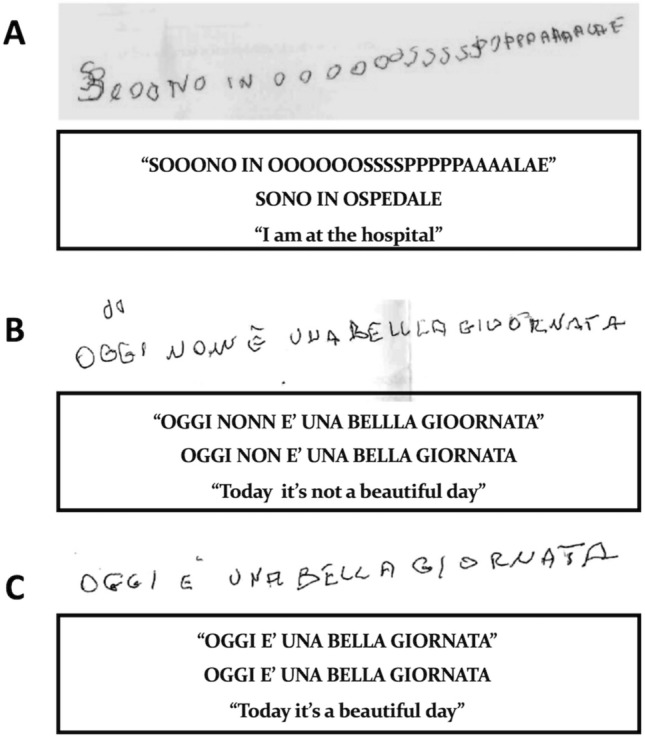
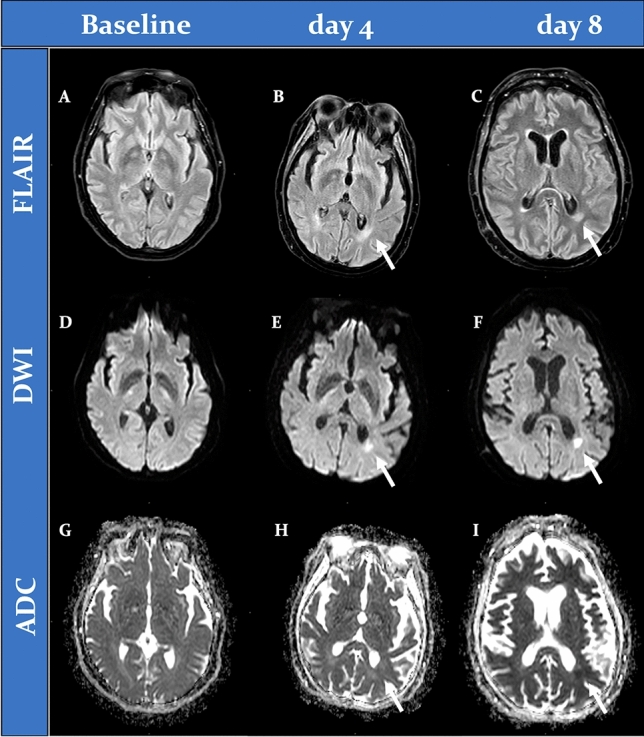
Four patients (three females) with a mean age of 66.5 years (range: 65–68 years) were included in the study. Demographics, CRS and ICANS disease course, neurological clinical and investigative findings, and immunotherapies are summarized in Table 1. The illustrative case of patient 1 is shown in Fig. 1. Neurological screening evaluations were unrevealing in all patients, except for patient 4 who showed a pre-existent multi-domain mild cognitive impairment (Mini-Mental Status Examination score = 24). All patients received lymphodepletion with cyclophosphamide and fludarabine as recommended [10] and then were infused with either axicabtagene ciloleucel (pts 1 and 4) or tisagenlecleucel (pts 2 and 3). All patients developed CRS within 24 h since CAR T-cells infusion, with a mean duration of 19 days (range 5–59), and three patients (pts 1–3) required tocilizumab administration. Patients 3 and 4 developed neurotoxicity following CRS, whereas patient 1 and 2 showed neurological manifestations accompanying the systemic hyperinflammatory state. Neurotoxicity developed with a mean onset of 2.3 days (range 1–4 days) after CAR T-cell therapy. A writing disorder was observed as the earliest neurological manifestation in all patients, either as an isolated sign (pt1) or accompanied by other symptoms. The disorder was characterized by repetition of written letters associated with mild apraxia (Fig. 2). This peculiar writing disturbance rapidly evolved into more complex agraphia as the neurotoxicity worsened, sometimes resulting in illegible scrawls. Notably, a frontal predominant encephalopathy, characterized by a combination of ideomotor slowing, echolalia, perseveration, difficulties in Luria’s test, frontal release signs and fluency slowing, was observed in all cases. Additional signs were variably associated, including headache, mild aphasia, apraxia, dyscalculia and myoclonic tremor. Rapid clinical deterioration required transfer to ICU in three patients (pts 1–3). Lumbar puncture was not performed because all patients had severe thrombocytopenia. EEG revealed diffuse slowing in all patients, with occasional focal discharges in two cases (pts 1 and 3), yet no clinical seizure was observed. Brain MRI was unrevealing, apart from patient 1 where it showed multiple small T2 hyperintensity in the white matter related to focal vasogenic, and eventually cytotoxic, oedema (one exemplifying lesion is shown in Fig. 3). Brain 18-[18F]FDG positron emission tomography (FDG-PET) was performed in three patients and demonstrated diffuse hypometabolism with frontal predominance, consistently with the clinical presentation (Fig. 4). Patients were treated with intravenous steroid administration and anti-cytokine monoclonal antibodies after steroid failure (Table 1). Patients 3 and 4 achieved complete clinical recovery and EEG abnormality resolution following steroids. Patient 2 was treated with siltuximab (anti-interleukin-6), intravenous methylprednisolone and anakinra (anti-inteleukin-1). She developed a spontaneous left parietal intraparenchymal haematoma with associated subarachnoid haemorrhage on the 20th day (Fig. 4), likely due to severe thrombocytopaenia and altered coagulation. Gradually, patient’s neurological and general condition ameliorated, with mild dysexecutive signs as neurological sequelae. Unfortunately, she died from haematological relapse few months after CAR T-cell therapy. Patient 1 experienced progressive worsening of her general (CRS grade 4) and neurological condition until deep coma state with preserved midbrain reflexes and no associated neurological focal signs; thus, she was sedated and placed on invasive mechanical ventilation with supportive care. Despite aggressive immunotherapies (intravenous steroids and anakinra), her condition deteriorated, leading to death on the 10th day since reinfusion (Fig. 1). Her family declined autopsy.
Table 1.
Demographics and disease course
| Pt | Age (y), Sex | CRS start/enda (max grade) | ICANS start/enda (max grade) | ICANS neurological manifestationsa | Investigative findingsa (EEG, MRI, 18F-PET) | Treatment | Follow-upa |
|---|---|---|---|---|---|---|---|
| 1 | 65, F | + 0, + 10 (grade 4) | + 0, + 10 (grade 5) | Paligraphia (+ 0), confusion, ideo-motor apraxia, echolalia, frontal release signs, coma (+5) |
EEG: diffuse slowing at 4-5 Hz, left frontal discharges (+ 1) -Brain MRI: multiple white matter hyperintensity (+ 8) |
-Dexamethasone (+ 1), -High-dose intravenous methylprednisolone (+ 4), -Anakinra (+ 4) |
Death related to CAR T-cell therapy toxicity and sepsis (+ 10) |
| 2 | 65, F | + 0, + 59 (grade 4) | + 0, + 51 (grade 4) | Paligraphia (+ 0), perseveration, difficulties in Luria’s test, frontal release signs, fluency slowing, postural myoclonic tremor, severe encephalopathy (+ 7) |
EEG: diffuse slowing at 5 Hz (+ 2) -Brain MRI: normal (+ 5) -Brain FDG-PET: diffuse bilateral hypometabolism with frontal predominance (+ 39) |
-High-dose intravenous methylprednisolone (+ 7), -Siltuximab (+ 7), -Anakinra (+ 14) |
Mild dysexecutive signs (+ 59) Death related to cancer relapse (+ 180) |
| 3 | 68, F | + 0, + 7 (grade 3) | + 2, + 20 (grade 3) | Paligraphia (+ 2), ideo-motor slowing, postural myoclonic tremor, aphasia, frontal release signs, perseveration, dyscalculia |
EEG: diffuse slowing at 6 Hz with isolated posterior discharges (+ 3) -Brain MRI: normal (+ 9) -Brain FDG-PET: diffuse hypometabolism with posterior sparing (+ 9) |
-Dexamethasone (+ 3), -High-dose intravenous methylprednisolone (+ 5) |
Complete neurological recovery (+ 30) |
| 4 | 68, M | + 0, + 7 (grade 1) | + 3, + 12 (grade 2) | Paligraphia (+ 4), ideo-motor slowing, aphasia nominum, fluency slowing, frontal release signs, postural myoclonic tremor |
EEG: diffuse slowing at 6 Hz (+ 4) Brain MRI: normal (+ 6) Brain FDG-PET: diffuse hypometabolism with posterior sparing (+ 6) |
-Dexamethasone (+ 3) | Complete neurological recovery (+ 30) |
aWe refer to CAR T-cells infusion as day “0”, and to all events occurred subsequently as “plus day”
Immunotherapies were administered at the following regimens: intravenous dexamethasone (10 mg q6-8 h), high-dose intravenous methylprednisolone (1000 mg daily for 5 days), intravenous siltuximab (11 mg/kg), and subcutaneous anakinra (100 mg q12h for 7 days)
CRS cytokine release syndrome. ICANS immune effector-associated neurotoxicity syndrome. EEG electroencephalography. MRI magnetic resonance imaging. CT computed tomography. FDG-PET [18F]FDG positron emission tomography
Fig. 1.
Disease course in case 1. Neurological manifestations, ICANS severity, CRS severity, serum IL-6 and ferritin levels, timing of treatments and diagnostic investigations during disease course. ICANS and CRS severity were graded according to the consensus by Lee et al. [2] ICE score modified during disease course as follows: day0 = 10; day1 = 3 day2 = 7; day3 = 4; day5 till death = 0. ICANS immune effector cell-associated neurotoxicity syndrome. CRS cytokine release syndrome. ICE score immune effector cell-associated encephalopathy score
Fig. 2.
Writing findings in ICANS patients. Within the black box, the faithful drafting of the Italian sentence written by the patients is reported, followed by the same Italian sentence reported with no letter repetitions and then its English translation. Rewriting of letters produced by patient 1 at ICANS onset (A) and by patient 3 at ICANS onset (B) and after complete clinical resolution (C). ICANS immune effector cell-associated neurotoxicity syndrome
Fig. 3.
Brain MRI findings in case 1. Axial 1.5 Tesla brain MRI. Unremarkable baseline brain MRI (A, D, G). Left parietal periventricular T2-weighted hyperintensity (white arrows) with radiological features initially consistent with vasogenic oedema [↑DWI (E); ↑/ = ADC (H)], and then with cytotoxic oedema [↑DWI (F); ↓ADC (I)]. FLAIR fluid-attenuated inversion recovery; DWI diffusion-weighted image; ADC apparent diffusion coefficient
Fig. 4.
Brain FDG-PET findings in case 2. Matched axial brain FDG-PET (A,B,C) and CT scan (D,E,F) showing diffuse bilateral hypometabolism with frontal predominance. Additionally, a focal area of severe hypometabolism (A, B), resulting from a spontaneous parenchymal haematoma associated with subarachnoid haemorrhage (D, E), is observable in the left parietal lobe. FDG-PET [18F]FDG positron emission tomography. CT computed tomography
Discussion
Here, we describe four patients treated with CAR T-cell therapy presenting with a writing disorder, namely paligraphia, as an early manifestation of neurotoxicity. In all cases, paligraphia was followed by a rapid neurological deterioration with frontal predominant encephalopathy that required transfer to ICU for three patients. In previous studies, neurotoxicity was observed with a mean onset of 5 days after infusion, even though it developed within 24 h since reinfusion in a subgroup of patients [7, 11], as we observed in two cases, requiring early management. Despite the use of specific aggressive treatment, one of our cases died from CAR T-cell therapy-related toxicity, while another one because of CAR T-cell therapy failure (disease progression). Accordingly, severe neurotoxicity is a well-known potentially fatal complication of CAR T-cell therapy that is likely antagonized by aggressive early treatment. Thus, clinical or instrumental markers to identify early and reliably patients at higher risk of experiencing severe neurotoxicity is an urgent need in CAR T-cell therapy to ensure close monitoring and prompt interventions without overtreating.
Speech disorders are considered recurrent early findings, even though they are neither specific nor predictive of severity [2, 3, 9]. Conversely, akinetic mutism, a neurological manifestation resulting from frontal-subcortical dysfunction, is quite specific to ICANS, but usually develops over days and it is not always present as in our cases. Agraphia has been previously reported as a neurotoxicity manifestation [9], yet it has been generally defined as a handwriting impairment. Notably, our cases presented with paligraphia, a writing disorder that has been described anecdotally in literature, mostly in patients with Gilles de la Tourette syndrome [12] and it has never been reported in ICANS to the best of our knowledge. Paligraphia is defined as a reiterative agraphia characterized by rewriting phrases, words, or letters produced by the patient [13]. Paligraphia occurs mostly in words containing double letters and circular-shaped letters [14]. It is considered as an apraxic disorder and reflects a difficulty in programming or generating the appropriate motor skilled commands for writing production [13]. Dysfunctions of the frontal and dominant parietal lobes are suggested as putative mechanisms [14]. Currently, research on apraxic agraphia, especially paligraphia, is limited by the uncommonness of this phenomenon. Nonetheless, when this feature is accompanied with perseverative behaviours, as in our patients, this is thought to broadly localize to the frontal lobes [15]. Notably, all our patients eventually developed a frontal predominant encephalopathy [3, 4], which was also supported by brain FDG-PET findings in three patients. Taken together, these data suggest that paligraphia may be an early manifestation of frontal lobe dysfunction. Additionally, in our cohort paligraphia was present in three out of four severe ICANS (75%) and only in one out of five mild ICANS (20%), with no cases of death related to neurotoxicity (grade 5) observed among patients who did not present paligraphia. This observation, although not statistically significant, suggests that paligraphia could be more specific to severe ICANS and thus, when present, potentially predicts neurotoxicity severity.
Even though we described only four patients, they were selected from a pool of extensively investigated CAR T-cells infused patients, allowing us to monitor day by day the dynamic evolution of neurotoxicity and to detect paligraphia in most of the observed cases of severe ICANS, suggesting this neurological manifestation may be relatively common in these patients. Serial neurological examinations and the use of specific tools may help in both detection of early writing dysfunction and its monitoring [2].
Instrumental distinctive findings in ICANS are also currently lacking [2], [3], [9]. Brain MRI is usually normal, even though non-specific parenchymal alterations are described, including thalami, brainstem and cerebral white matter oedema, while EEG usually reveals diffuse slowing with frontal abnormalities, as observed in our first patient [16]. More advanced functional studies, such as brain FDG-PET, could be implemented in this setting.
Interestingly, we recently reviewed encephalopathies related to several cytokine storm disorders, including CAR T-cells and COVID-19-associated ones, revealing that electro-clinical frontal lobe dysfunction, among other shared clinical and investigative findings, is a recurrent manifestation across these conditions [17–19]. Therefore, we suggested that cytokine-mediated neuroinflammation might represent a common overarching mechanism resulting in encephalopathy and we proposed a unifying term that is cytokine storm-associated encephalopathy (CySE) [18].
Conclusions
CAR T-cell therapy is a revolutionary treatment that has been showing efficacy in a growing number of refractory haematological cancers. Therefore, related neurological complications are expected to be observed more and more in clinical practice. Paligraphia may represent an early, specific and easily detectable neurological manifestation, yet may be overlooked during regular visit if not specifically investigated. Future studies on larger numbers of patients are needed to confirm paligraphia as a distinctive, and possibly predictive, sign of a more severe ICANS.
Acknowledgements
We would like to thank Cecilia Baroncini who edited the English text.
Author contributions
UP, GA: drafting the manuscript; conception and design of the study; acquisition and analysis of data. RDA, RR, MN, FR, SM, RS; SS, AF, LS, LF, BC, MD, FB, PZ, PC: acquisition and analysis of data; revision of the manuscript for content. AS, MG: conception and design of the study, acquisition and analysis of data; revision of the manuscript for content. All the authors contributed to the article and approved the submitted version.
Funding
The authors declare that they have nothing to report.
Data availability
The authors take full responsibility for the data, the analysis, and interpretation of the research, and they have full access to all of the data.
Code availability
Not applicable.
Declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical standards
All investigations were carried out according to the Declaration of Helsinki.
Consent to participate
Written informed consent was collected from the patient for the inclusion of deidentified clinical data in a scientific publication, in accordance with the Declaration of Helsinki.
Consent for publication
All authors agreed with this final version.
Footnotes
Umberto Pensato and Giulia Amore contributed equally to this work.
References
- 1.Singh AK, McGuirk JP. CAR T cells: continuation in a revolution of immunotherapy. Lancet Oncol. 2020;21:e168–e178. doi: 10.1016/S1470-2045(19)30823-X. [DOI] [PubMed] [Google Scholar]
- 2.Lee DW, Santomasso BD, Locke FL, et al. ASTCT consensus grading for cytokine release syndrome and neurologic toxicity associated with immune effector cells. Biol Blood Marrow Transplant. 2019;25:625–638. doi: 10.1016/j.bbmt.2018.12.758. [DOI] [PubMed] [Google Scholar]
- 3.Rubin DB, Danish HH, Ali AB, et al. Neurological toxicities associated with chimeric antigen receptor T-cell therapy. Brain. 2019;142:1334–1348. doi: 10.1093/brain/awz053. [DOI] [PubMed] [Google Scholar]
- 4.Santomasso BD, Park JH, Salloum D, et al. Clinical and biological correlates of neurotoxicity associated with CAR T-cell therapy in patients with B-cell acute lymphoblastic leukemia. Cancer Discov. 2018;8:958–971. doi: 10.1158/2159-8290.CD-17-1319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rice J, Nagle S, Randall J, Hinson HE. Chimeric antigen receptor T cell-related neurotoxicity: mechanisms, clinical presentation, and approach to treatment. Curr Treat Options Neurol. 2019;21:40. doi: 10.1007/s11940-019-0580-3. [DOI] [PubMed] [Google Scholar]
- 6.Gust J, Hay KA, Hanafi LA, et al. Endothelial activation and blood-brain barrier disruption in neurotoxicity after adoptive immunotherapy with CD19 CAR-T cells. Cancer Discov. 2017;7:1404–1419. doi: 10.1158/2159-8290.CD-17-0698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tallantyre EC, Evans NA, Parry-Jones J, Morgan MPG, Jones CH, Ingram W. Neurological updates: neurological complications of CAR-T therapy. J Neurol. 2020;268(4):1544–1554. doi: 10.1007/s00415-020-10237-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Strati P, Ahmed S, Furqan F, et al. Prognostic impact of corticosteroids on efficacy of chimeric antigen receptor T-cell therapy in large B-cell lymphoma. Blood. 2021;137:3272–3276. doi: 10.1182/blood.2020008865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neelapu SS, Tummala S, Kebriaei P, et al. Chimeric antigen receptor T-cell therapy - assessment and management of toxicities. Nat Rev Clin Oncol. 2018;15:47–62. doi: 10.1038/nrclinonc.2017.148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yakoub-Agha I, Chabannon C, Bader P, et al. Management of adults and children undergoing chimeric antigen receptor T-cell therapy: best practice recommendations of the European Society for Blood and Marrow Transplantation (EBMT) and the Joint Accreditation Committee of ISCT and EBMT (JACIE) Haematologica. 2020;105:297–316. doi: 10.3324/haematol.2019.229781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gust J, Taraseviciute A, Turtle CJ. Neurotoxicity associated with CD19-targeted CAR-T cell therapies. CNS Drugs. 2018;32:1091–1101. doi: 10.1007/s40263-018-0582-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cavanna AE, Ali F, Rickards H. Paligraphia and written jocularity in gilles de la tourette syndrome. Mov Disord. 2011;26:930–931. doi: 10.1002/mds.23495. [DOI] [PubMed] [Google Scholar]
- 13.Tiu JB, Carter AR. Agraphia. StatPearls; 2020. [PubMed] [Google Scholar]
- 14.Rapcsak SZ, Beeson PM. Agraphia. In: Ramachandran VS, editor. Encyclopedia of the human Brain. Academic Press; 2002. pp. 71–86. [Google Scholar]
- 15.Reber J, Tranel D. Chapter 8 - Frontal lobe syndromes. In: D’Esposito M, Grafman JH, editors. Handbook of clinical neurology. Elsevier; 2019. pp. 147–164. [DOI] [PubMed] [Google Scholar]
- 16.Rubin DB, Al Jarrah A, Li K, et al. Clinical predictors of neurotoxicity after chimeric antigen receptor T-Cell therapy. JAMA Neurol. 2020;77(12):1536–1542. doi: 10.1001/jamaneurol.2020.2703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muccioli L, Pensato U, Cani I, Guarino M, Cortelli P, Bisulli F. COVID-19-Associated Encephalopathy and Cytokine-Mediated Neuroinflammation. Ann Neurol. 2020;88(4):860–861. doi: 10.1002/ana.25855. [DOI] [PubMed] [Google Scholar]
- 18.Pensato U, Muccioli L, Cani I, Janigro D, Zinzani PL, Guarino M, Cortelli P, Bisulli F. Brain dysfunction in COVID-19 and CAR-T therapy: cytokine storm-associated encephalopathy. Ann Clin Transl Neurol. 2021;8(4):968–979. doi: 10.1002/acn3.51348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pilotto A, Masciocchi S, Volonghi I, De Giuli V, Caprioli F, Mariotto S, Ferrari S, Bozzetti S, Imarisio A, Risi B, Premi E, Benussi A, Focà E, Castelli F, Zanusso G, Monaco S, Stefanelli P, Gasparotti R, Zekeridou A, McKeon A, Ashton NJ, Blennov K, Zetterberg H, Padovani A (2021) SARS-CoV-2 encephalitis is a cytokine release syndrome: evidences from cerebrospinal fluid analyses. Clin Infect Dis ciaa1933. 10.1093/cid/ciaa1933 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors take full responsibility for the data, the analysis, and interpretation of the research, and they have full access to all of the data.
Not applicable.