Abstract
Background
The COVID-19 pandemic has had considerable behavioral health implications globally. One subgroup that may be of particular concern is U.S. veterans, who are susceptible to mental health and substance use concerns. The current study aimed to investigate changes in alcohol use and binge drinking before and during the first year of the pandemic among U.S. veterans, and how pre-pandemic mental health disorders, namely posttraumatic stress disorder (PTSD), and COVID-19-related factors like loneliness, negative reactions to COVID-19, and economic hardship influenced alcohol use trends.
Methods
1230 veterans were recruited in February 2020 as part of a larger survey study on veteran health behaviors. Veterans were asked to complete follow-up assessments throughout the pandemic at 6, 9, and 12- months.
Results
Overall, veterans reported a significant decrease in alcohol use (IRR = 0.98) and binge drinking (IRR = 0.11) However, women, racial/ethnic minority veterans, and those with pre-existing PTSD exhibited smaller decreases in alcohol use and binge drinking and overall higher rates of use compared to men, White veterans, and those without PTSD. Both economic hardship and negative reactions to COVID-19 were associated with greater alcohol and binge drinking whereas loneliness showed a negative association with alcohol use and binge drinking.
Conclusions
Veterans reported decreases in alcohol use and binge drinking throughout the pandemic, with heterogeneity in these outcomes noted for higher risk groups. Special research and clinical attention should be given to the behavioral health care needs of veterans in the post-pandemic period.
Keywords: Trauma, Longitudinal, Active duty, Veterans administration, Drug use, COVID-19
1. Introduction
American veterans from the conflicts in Iraq and Afghanistan are at high-risk of alcohol misuse, which can lead to the development of alcohol use disorders. One in ten veterans seeking care at the Veterans Affairs Healthcare System (VA) meet criteria for alcohol use disorder, and estimates of high-risk drinking in community samples of veterans range from 12% to 40%, or upwards of 1 million veterans (Calhoun et al., 2008, Eisen et al., 2012, Seal et al., 2011). Heavy drinking puts veterans at risk of both short- and long-term consequences, such as relational, behavioral, physical health, and occupational problems. Complicating this, veterans from these conflicts have a high prevalence of co-occurring alcohol use disorders and mental health disorders, such as posttraumatic stress disorder (PTSD) (Seal et al., 2011), which is among the most commonly occurring mental health disorder among veterans (Trivedi et al., 2015). Between 11% and 20% of veterans with alcohol use disorders are diagnosed with PTSD and upwards of 69% of those seeking treatment for substance use disorders also have a PTSD diagnosis (Seal et al., 2011, McDevitt-Murphy et al., 2010). However, only about half of veterans with alcohol use disorders and mental health disorders seek behavioral health services from the VA or elsewhere (Schell and Marshall, 2008, U.S Department of Veterans Affairs, 2018). Given the high prevalence of co-occurring disorders, veterans are a population at high-risk for experiencing exacerbation of mental health symptoms and increases in alcohol use during the current COVID-19 pandemic which could bring greater attention to the mental health care needs of veterans.
Current research reports heightened feelings of anxiety, distress, and traumatic stress among adults during the pandemic (Gallagher et al., 2020, Liu et al., 2020, Rajkumar, 2020). Several pandemic-related hardships are thought to contribute to the observed rises in mental health and substance use symptomology, including negative reactions to COVID-19 (e.g., stress related to the pandemic, problems sleeping, relationships impacted), economic hardship (e.g., disruption in employment), and loneliness (Fitzpatrick et al., 2020, McGinty et al., 2020, Witteveen and Velthorst, 2020). Alcohol use behaviors may be increasing among the global population as well, with individuals reporting or experiencing COVID-19-specific factors such as negative reactions to COVID-19, loneliness, economic and financial hardship, and pre-pandemic mental health disorders being at particular high-risk for detrimental short- and long-term consequences (Pollard, Tucker, & Green, 2020). Prior work also notes that some groups, such as women, members of racial/ethnic minority groups, and individuals with pre-existing mental health problems are at greater risk of experiencing long-term problems during this high stress time (Özdin & Bayrak Özdin, 2020). While the COVID-19 pandemic has had considerable implications for behavioral health within the general population (Ettman et al., 2020b, Gallagher et al., 2020, Pollard et al., 2020, Rajkumar, 2020), veterans may be at particular risk. Veterans already face unique, context-specific, risks related to their deployment and subsequent reintegration into civilian life (Derefinko, Hallsell, Isaacs, Salgado Garcia, Colvin, Bursac, McDevitt-Murphy, Murphy, Little, & Talcott, 2018), placing them at risk of poor long-term behavioral, social, and economic outcomes. In addition, veterans are a group at-risk for heavy alcohol use behaviors (Hoge et al., 2006, Seal et al., 2011) and have high rates of mental health problems (Hoge et al., 2006, Trivedi et al., 2015). Pre-pandemic mental health problems among veterans may influence substance use behaviors during the pandemic (and thereafter), perhaps to cope with the added stress of the pandemic or exacerbation of mental health symptoms (Rogers, Shepherd, Garey, & Zvolensky, 2020). Prior work reports that veterans who have experienced some type of stressful life event are at heightened risk of mental health and substance use problems (Aronson et al., 2020), and such pre-existing conditions can have substantial implications for psychological outcomes during subsequent stressful events, like COVID-19 (Alonzi et al., 2020, Kim et al., 2020). As with the general population, there is also some research indicating that COVID-19 has disproportionately affected women and racial/ethnic minority veterans (Rentsch et al., 2020, Tsai et al., 2021).
There is a clear need to understand the extent to which the COVID 19 pandemic has influenced substance use among American veterans, a high-risk population for substance use disorders. Unfortunately, little is known regarding veterans’ ability to manage alcohol use during this exceptionally stressful life event. For the first aim of the current study, we examined changes in alcohol use (including days of alcohol use and binge drinking) from a month prior to the outbreak of the pandemic in the United States through the first year of the pandemic. For the second aim, we assessed how changes in alcohol and binge drinking use differed for veterans screening for pre-pandemic PTSD. Finally, in an effort to understand how COVID-19-specific factors influence alcohol use and binge drinking trajectories, we also considered the time varying effects of negative reactions to COVID, loneliness, and economic hardship. As an exploratory aim, and given recent research indicating disparities during the COVID-19 pandemic, we assessed potential differences in alcohol use trajectories across sex (men vs. women) and race/ethnicity.
2. Methods
2.1. Procedures
Veterans aged 18 to 40 that had separated from the Air Force, Army, Marine Corps, and Navy were recruited in February 2020 as part of a large survey study of veteran attitudes and health behavior. Advertisements were displayed on social media websites (Facebook, Instagram) and military-specific social media websites and listservs (RallyPoint, We Are the Mighty). Participants consented to the study, which was approved by the local Institutional Review Board, and completed a 30-minute survey on a secure website. They were given a $20 Amazon gift card for participation.
As with most online studies with widespread advertising, many potential participants clicked on the online ads, but most either did not pursue participation or were ineligible. Of the 5776 individuals who clicked on ads and reached the online consent form, 2750 (48%) did not pursue past the initial consent page. Ninety-four (2%) were screened and found to be ineligible (i.e., not within age range, not a US veteran). An additional 1077 (19%) attempted to access the study once it was no longer accepting participants. Thus, 1855 (32%) consented to be a part of the study and completed the survey. We ran a series of internal checks to remove participants where it was unclear they were actually veterans, such as endorsing inconsistent responses between items within and across surveys (e.g., branch, rank, pay grade matches), where it was clear the participant was carelessly responding to items (e.g., completing the survey too quickly or selecting the same response option throughout), and where they attempt to access the survey multiple times (e.g., reviewing IP addresses). These checks removed 625 individuals from the sample. When it was unclear if a participant was a veteran or was responding carelessly, we opted to drop them, which is a conservative approach that may be necessary in online studies with no face-to-face contact with participants.
The final sample was composed of 1230 veteran participants at baseline (see Table 1 ). Participants were invited to complete three follow-up surveys over the course of the pandemic. They were sent follow-up surveys via email at 6-months (August 2020; N = 1025; 83.3% retention from baseline), 9-months (November 2020; N = 1006; 81.8% retention from baseline), and 12-months (February 2021; N = 1005; 81.7% retention from baseline). Participants were given a $30, $40, and $50 Amazon gift card for the 6-, 9-, and 12-month surveys, respectively.
Table 1.
Demographic characteristics pre-COVID-19.
| Variable | M(SD) or N(%) |
|---|---|
| Age | 34.5 (3.67) |
| Sex (men) | 1091 (88.7%) |
| Race/ethnicity | |
| White | 975 (79.3%) |
| Hispanic/Latino/a | 134 (10.9%) |
| Black | 90 (7.3%) |
| Asian | 13 (1.1%) |
| Multiracial/other | 18 (1.5%) |
| Combat scale | 5.02 (2.35) |
| Mental Health (positive screen) | |
| PTSD | 397 (32.3%) |
| COVID-19 Time-varying Co-variates | |
| Negative reactions to COVID-19 | 1.22 (0.49) |
| Loneliness | 48.8 (7.07) |
| Economic hardship | 477 (38.8%) |
| Days of Substance Use | |
| Alcohol use Time 1 (past month) | 11.1 (5.98) |
| Alcohol use Time 2 (past month) | 8.82 (6.05) |
| Alcohol use Time 3 (past month) | 9.54 (5.0) |
| Alcohol use Time 4 (past month) | 9.13 (5.02) |
| Binge drinking Time 1 (past month) | 4.99 (4.02) |
| Binge drinking Time 2 (past month) | 3.39 (3.14) |
| Binge drinking Time 3 (past month) | 2.33 (2.24) |
| Binge drinking Time 4 (past month) | 2.42 (2.66) |
Note: PTSD = Posttraumatic Stress Disorder.
Continuous variable ranges: all alcohol use and binge drinking variables are past 30-day, range 0–30; negative reactions to COVID-19 (0–4); loneliness (20–80); economic hardship (0–1); combat scale (0–12).
2.2. Measures
2.2.1. Socio-demographic factors
Participants self-reported sex (male, female), race/ethnicity, and age, which were included as covariates in models. We also controlled for severity of combat exposure using a composite measure of 11 items from prior work with veterans (e.g., witnessing an accident resulting in serious injury or death; engaging in hand-to-hand combat) (Schell & Marshall, 2008) and an additional item of ever feeling like they were in great danger of being killed. Nearly all (96.1%) experienced combat. A summed score of self-reported adverse childhood experiences (Felitti et al., 1998) were used. Four items from the original Adverse Childhood Experiences Study were used that covered experiences of sexual, physical, emotional abuse, and neglect. Participants responded with “yes” or “no” to each item.
2.2.2. Posttraumatic stress disorder
PTSD symptom severity was assessed using the 20-item Posttraumatic Stress Disorder Checklist for DSM-5 (PCL-5; Bovin et al., 2016) at baseline, where participants indicated how often they were bothered by 20 PTSD symptoms in the past month from not at all (0) to extremely (4). The PCL-5 yields a total sum score from 0 to 80 and had a reliability estimate of α = 0.91 in the current sample. We used the clinical cutoff score of 33 to determine if a participant met criteria for probable PTSD (Bovin et al., 2016).
2.2.3. Negative reactions to COVID-19
On the 6- and 9-month survey participants were asked how often they felt negative reactions to the pandemic related to emotional, stress, sleep, and relationships using nine items from prior work (Johns Hopkins Bloomberg School of Public Health, 2020). Items such as “was stressed by the restrictions on leaving home” and “felt that your social relationships were suffering” when considering the pandemic over the past three months were rated from 0 “not at all” to 4 “a great deal.” Higher scores on the composite measure suggested greater negative reactions to the pandemic.
2.2.4. Loneliness
At the three follow-up time points, loneliness was measured with the 20-item UCLA Loneliness Scale (Russell, 1996). The scale assessed general loneliness by asking participants questions such as “do you feel alone,” “How often do you feel close to people,” and “How often do you feel left out” (1 = never to 4 = always). A sum score was calculated ranging from 20 to 80, with a reliability of α = 0.82 across the three survey waves.
2.2.5. Economic hardship
Economic hardship was conceptualized by experiencing disruptions in employment during the pandemic. Two items from the Epidemic-Pandemic Impact Inventory (Grasso, Briggs-Gowan, Ford, & Carter, 2020) assessed disruptions in employment at 6-, 9-, and 12-months. Participants indicated if they (1) were laid off from a job or had to close their own business or (2) had to reduce work hours or were furloughed due to the pandemic. Participants were coded as having experienced economic hardship if they indicated a positive response to either of these items.
2.2.6. Alcohol use and binge drinking
Days of alcohol use and binge drinking (i.e., drinking five or more drinks on a day if male sex, drinking four or more drinks on a day if female sex) were assessed by asking each participant to indicate how many days they drank and the how many days they binge drank in the past month (i.e., past 30 days).
2.3. Analytic plan
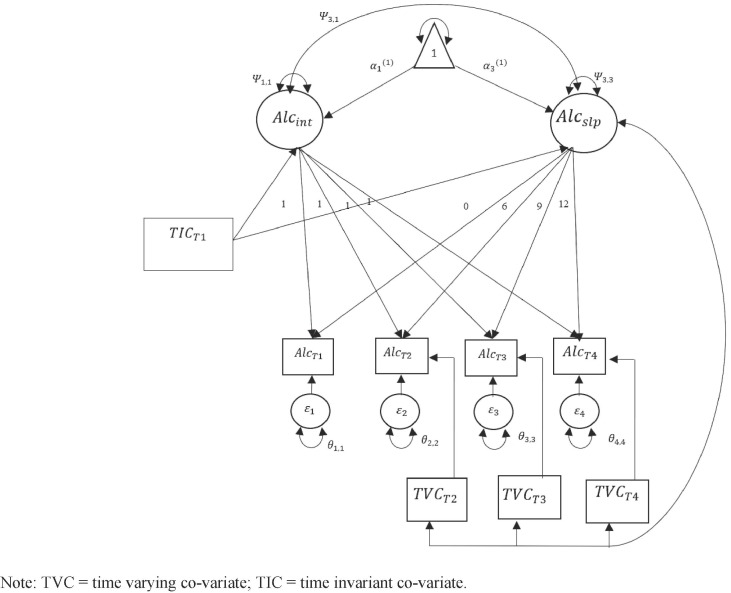
To address the first aim of understanding changes in alcohol use before and after the initial stay-at-home orders in the U.S. (implemented in March 2020), we estimated a series of latent growth models (Grimm, Ram, & Estabrook, 2016). Specifically, we estimated a separate growth model for days of alcohol use and days of binge drinking in the past 30 days. Because all observed variables used in the growth model were count variables, we used a negative binomial distribution. To ensure a negative binomial model was the best fitting model, we used the dispersion parameter. If the dispersion parameter is significantly different from zero, a negative binomial model should be used; if it is not different from zero, a Poisson model should be used (Grimm et al., 2016). For our latent growth model, we first estimated an unconditional model to understand the functional form of the data. During this step, we also tested for random (versus) fixed slopes using the negative two loglikelihood ratio test. Next, we entered our demographic covariates including sex, age, race/ethnicity (white vs. racial/ethnic minority), a summed score of combat severity, and adverse childhood experiences. All continuous variables were grand mean centered. Next, to address the second aim, we entered the dichotomous indicator for probable PTSD onto the intercepts and slopes of our growth models. Finally, to address our third aim, we entered our time varying covariates into the model. At each time point, we regressed each of our time varying co-variates onto the contemporaneously observed alcohol use variables (see Fig. 1 for conceptual model). This allowed us to determine the effect of negative reactions to COVID-19 (note: this was only assessed at the 6- and 9-month time points and not at the 12-month follow-up), loneliness, and economic hardship on alcohol use and binge drinking over time, above and beyond the effects of the underlying growth model and our time invariant co-variates. To do this, we first introduced time-varying covariates as constrained predictors (e.g., effects are constrained to be equal over time) and tested this model against one where time-varying covariates were unconstrained (e.g., freely estimated at each time point). We used difference in negative two log likelihood ratio tests to determine if constrained versus freely estimated model fit the data best. Doing this allowed us to test if each of our time varying covariates had consistent, stronger, or weaker influences over time.
Fig. 1.
Conceptual model using time varying and time invariant co-variates to predict alcohol use and binge drinking.
3. Results
3.1. Changes in alcohol use
To address our first aim, we initially estimated a series of unconditional latent growth models for days of alcohol use and days of binge drinking. Results of our model building process can be found in the Supplementary materials. Final model results are reported in Table 2 . Effects of time invariant predictors are presented as Incident Rate Ratios (IRR), the exponentiated value of the log-mean beta estimate. Effects of time varying predictors are presented as traditional beta estimates.
Table 2.
Final model of time invariant and time varying co-variates on changes in alcohol use and binge drinking among veterans.
| Time invariant co-variates | Days of alcohol use |
Days of binge drinking |
||
|---|---|---|---|---|
| IRR [95% CI] |
IRR [95% CI] |
|||
| Intercept | Slope | Intercept | Slope | |
| Control variables | ||||
| Age | 1.01 [1.00, 1.02] | 1.00 [0.99, 1.02] | 1.00 [0.99, 1.01] | 0.99 [0.97, 1.02] |
| Sex (female) | 1.90 [1.76, 2.04] | 1.00 [0.99, 1.01] | 2.05 [1.87, 2.23] | 1.00 [0.98, 1.02] |
| Race/ethnicity (racial/ethnic minority) | 0.80 [0.73, 0.88] | 1.02 [1.01, 1.03] | 0.57 [0.50, 0.65] | 1.04 [1.02, 1.05] |
| Combat severity | 1.04 [1.02, 1.05] | 0.99 [0.97, 1.00] | 1.04 [1.02, 1.05] | 0.99 [0.98, 1.00] |
| Adverse childhood experiences | 1.00 [0.98, 1.2] | 1.03 [1.02, 1.04] | 1.05 [1.03, 1.07] | 1.00 [1.00, 1.01] |
| Mental health | ||||
| PTSD positive screen | 1.09 [1.01, 1.17] | 1.02 [1.01, 1.04] | 1.24 [1.13, 1.36] | 1.00 [0.99, 1.01] |
| Time varying covariates | B [95% CI] | B [95% CI] | ||
| Negative reactions to COVID-19 | ||||
| Time 2 | 0.29 [0.23, 0.35] | 0.39 [0.32, 0.46] | ||
| Time 3 | 0.10 [0.04, 0.16] | 0.39 [0.32, 0.46] | ||
| Time 4 | – | – | ||
| Loneliness | ||||
| Time 2 | −0.02 [−0.016, −0.012] | −0.004 [−0.007, −0.002] | ||
| Time 3 | −0.01 [−0.012, −0.006] | −0.01 [−0.01, −0.005] | ||
| Time 4 | −0.01 [−0.01, −0.006] | 0.01 [0.007, 0.02] | ||
| Economic hardship | ||||
| Time 2 | 0.004 [−0.03, 0.04] | 0.12 [0.04, 0.19] | ||
| Time 3 | 0.004 [−0.03, 0.04] | 0.03 [−0.06, 0.12] | ||
| Time 4 | 0.004 [−0.03, 0.04] | 0.11 [0.01, 0.21] | ||
| Growth parameters | IRR [95% CI] | IRR [95% CI] | ||
| Intercept | 21.8 [19.0, 25.1] | 10.2 [9.46, 12.4] | ||
| Slope | 0.99 [0.97, 1.01] | 0.88 [0.86, 0.90] | ||
| Residual Variance B [95% CI] | ||||
| Intercept | 0.07 [0.05, 0.09] | 0.10 [0.08, 0.12] | ||
| Slope | 0.05 [0.03, 0.08] | 0.02 [−0.03, 0.04] | ||
| Model fit criteria | ||||
| AIC | 20629.113 | 14317.311 | ||
| BIC | 20744.741 | 14437.757 | ||
| aBIC | 20668.521 | 14358.360 | ||
Note: bold indicates confidence interval does not include 0 or 1.
AIC = Akaike information criteria; BIC = Bayesian information criteria; aBIC = sample size adjusted Bayesian information criteria. Effects of time invariant co-variates are represented by Incident Rate Ratios (IRR), which is the exponentiated value of the log mean effect. Effects of the time varying co-variates are represented by traditional beta (B) coefficients, and represent the effect of the time varying co-variate on the contemporaneous outcome above the underlying growth model.
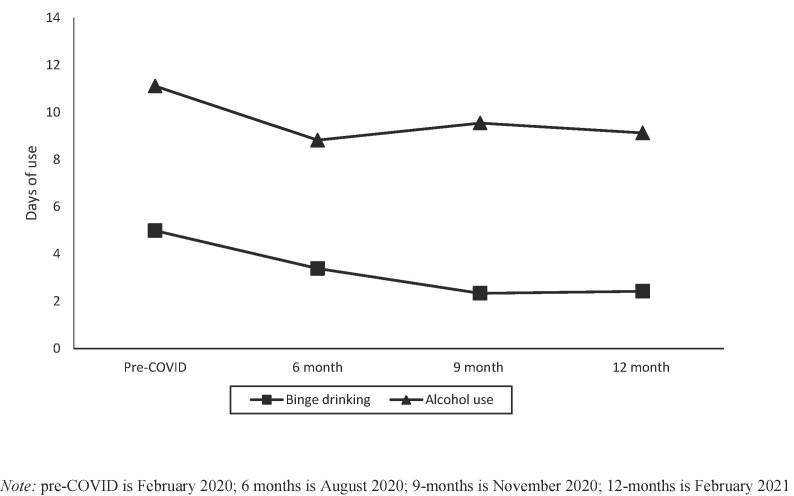
3.1.1. Alcohol use
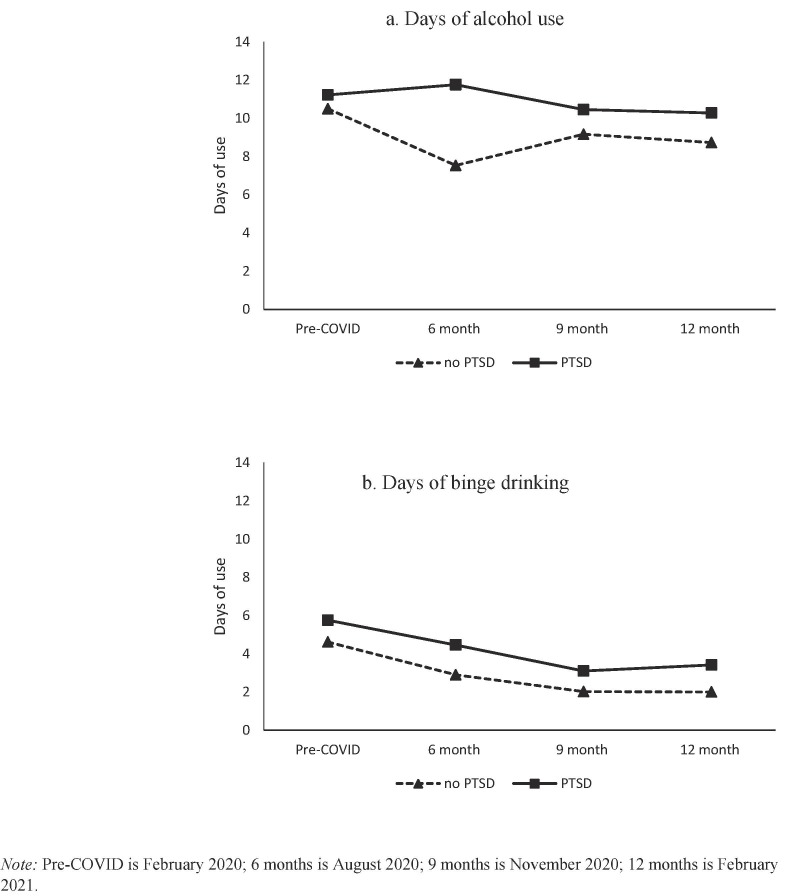
In the unconditional model (see Supplemental Table 1), the dispersion parameter was significantly different from zero (. Results of the unconditional model indicated a decrease in past month alcohol use among veterans (see Fig. 2 ). Looking more closely, veterans reported, on average, slightly over 11 days of past 30-day alcohol use in February 2020 prior to the initial stay-at-home orders. Over the first six months of the pandemic, veterans reported 8.8 days of alcohol use with this average slightly increasing to nearly 10 days and leveling off during the second half of the year. In our final model (see top of Table 2) we added pre-pandemic PTSD, demographic co-variates, and our time-varying co-variates to the model. Pre-pandemic PTSD predicted greater pre-pandemic alcohol use and a less steep decline in alcohol use. In other words, those with probable PTSD at baseline started higher in past 30-day alcohol use but decreased their drinking to a lesser extent during the first year of the pandemic. Fig. 3 a shows mean level drinking for those with and without positive screening criteria for PTSD.
Fig. 2.
Changes in alcohol use and binge drinking before and following COVID-19 among veterans.
Fig. 3.
Changes in alcohol use and binge drinking across veterans who screened for probable PTSD, pre-COVID-19.
We also noted some differences by sex, race/ethnicity, and combat severity. Women veterans and higher combat severity were associated with higher starting points but no discernable difference across change in alcohol use. However, racial and ethnic minority veterans reported lower pre-pandemic alcohol use, but during the follow up period showed a less steep decline in alcohol use, compared to white veterans.
In terms of our time varying covariates (see middle of Table 2), the best fitting model for past 30-day alcohol use was allowing negative reactions to COVID-19 to be freely estimated with loneliness and economic hardship constrained to be equal over time (model fitting results can be found in Supplemental Table 2). Results indicated that negative reactions to COVID-19 had a positive effect on past-30-day alcohol use, whereas loneliness had a negative effect on alcohol use during the entire follow-up period. Economic hardship did not emerge as a significant predictor.
3.1.2. Binge drinking
In the unconditional model for binge drinking, the dispersion parameter was significantly different from zero (. Results from the unconditional model revealed a significant decrease in binge drinking. Specifically, veterans reported binge drinking five days in the past 30-days during February 2020 pre-COVID-19, which reduced by more than half (2.3 days) throughout the 12-month follow-up period (see Fig. 2). In our final model (see Fig. 2b), where we added pre-pandemic PTSD screen, demographic covariates, and time varying co-variates, a similar pattern to alcohol use days emerged such that women veterans and experiencing higher combat severity were associated with greater pre-pandemic binge drinking, with no differences on the change factor. Racial/ethnic minority veterans reported fewer binge drinking days pre-COVID-19, and showed a less steep decrease in binge drinking during the year. Further, veterans screening for PTSD reported greater binge drinking days pre-pandemic (intercept), but no effect on the slope, indicating those with PTSD started higher and remained higher – with no differences in change over the first year of the pandemic. In terms of our time varying covariates, the best fitting model was constraining negative reactions to COVID-19 to be equal and allowing both loneliness and economic hardship to be freely estimated. Results revealed a slightly different pattern than alcohol use. For example, negative reactions to COVID-19 had a positive effect on binge drinking. However, loneliness started out at the 6- and 9-month time points having a negative effect on binge drinking, but at the 12-month mark, this changed and loneliness was associated with greater binge drinking. Finally, economic hardship was positively associated with binge drinking during the first 6 months of the pandemic and again at the 12-month follow up.
4. Discussion
The COVID-19 pandemic has taken a toll on the psychological well-being of many people across the world. However, prior work has noted that some groups, such as women, people from racial/ethnic minority groups, and individuals with pre-existing mental health problems are at greater risk of experiencing long-term problems during this high stress time (Özdin and Bayrak Özdin, 2020, Rentsch et al., 2020, Tsai et al., 2021). One group of individuals that reported heightened substance use and mental health problems pre-pandemic are American veterans (Seal et al., 2011, Trivedi et al., 2015), which makes them an important group to examine in longitudinal research over the course of the pandemic. The current study is among the first to report on changes in frequency of alcohol use and binge drinking over one year of the pandemic for veterans. Further, our study notes incremental differences in changes in alcohol use considering important demographics (sex, racial/ethnic minority status), pre-pandemic PTSD, and COVID-19-specific factors such as loneliness, negative reactions to COVID-19, and economic hardship.
Overall, the current study shows marked decreases in frequency of alcohol use and binge drinking over the one-year study period. This is in line with some prior theoretical and empirical work noting decreases in alcohol consumption during the pandemic. For example, Rehm et al. (2020) posited that, in the immediate months following the COVID-19 pandemic, alcohol use would decrease due to potential economic burdens, decreased physical activity, and an inability to frequent bars and restaurants due to stay-at-home orders. However, our results, and this theory, are in contrast to some reports of increased alcohol consumption following the COVID-19 pandemic. Pollard et al. (2020) noted a significant increase in alcohol consumption during the pandemic; however, this increase only represented one additional drink per month. Others have attempted to capture changes in alcohol use during the pandemic, but many of these studies have relied on retrospective reports of their use prior to the pandemic, thus neglecting proper temporal order (Vanderbruggen et al., 2020). Our study includes both a pre-pandemic time point as well as 6-, 9-, and 12-month follow-up periods, lending to more accurate and appropriate description of substance use trends among American veterans during COVID-19.
The current study does, however, indicate heterogeneity in substance use based on some demographic, mental health, and COVID-19-specific factors. For instance, results indicated that women veterans tended to have higher pre-pandemic alcohol use and binge drinking with no effect on the slope, indicating that women started higher and stayed higher on alcohol use and binge drinking compared to their male counterparts. This is in slight contrast to prior work on alcohol use, with some studies reporting increases in alcohol use among non-veteran women during the pandemic (Pollard et al., 2020). While our sample, as a whole, reported decreases in alcohol use and binge drinking over the study period, individuals screening positive for PTSD showed consistently higher rates of drinking over the study period. The results from the current study are not uncommon, as some previous work notes that individuals with pre-pandemic mental health problems reported increased substance use. This may imply that individuals struggling with PTSD may require greater outreach efforts as in person services return.
Our results also showed that racial/ethnic minority veterans reported lower pre-pandemic alcohol use and binge drinking, but a less steep decline over the course of the pandemic, compared to white veterans. This indicates that, while racial/ethnic minority veterans may have started lower in alcohol consumption, they did not show a similar decrease in alcohol use or binge drinking over the first year of the pandemic. These results may be partially explained by a growing literature noting disparities around the COVID-19 pandemic. For example, previous work notes higher mortality rate and higher COVID-19 positive tests among racial/ethnic minority veterans (Rentsch et al., 2020). Others have noted, in a representative U.S. sample, Hispanic and Black adults reported a higher prevalence of substance use during the pandemic compared to White respondents (Czeisler et al., 2020). However, these estimates were cross sectional in nature and do not assess changes in substance use. Our results point to a common story around the pandemic; individuals from racial/ethnic minority backgrounds are being affected differently compared to their White peers, and this appears to apply to veterans. These results may indicate structural barriers, such as less access to psychological services during the pandemic and, potentially, long-term healthcare disparities once cities and agencies begin to reopen to full capacity. While our study does not assess access to care, similar results have been reported such that racial/ethnicity minority populations reported greater health care disparities such as lower levels of access to mental health services and telehealth care during the pandemic (Ruprecht et al., 2021). While our sample provides important insight into the effect of the pandemic on racial/ethnic minority veterans in general, we did not have a diverse enough sample to explore such effects within specific racial/ethnic minority groups, which represents an essential area for further work.
Our results also shed light on important COVID-specific factors such as negative reactions to COVID, loneliness, and economic hardship. Not surprisingly, individuals reporting greater negative reactions to COVID-19 reported more alcohol use and binge drinking during the first 9 months of the pandemic. Fear and anxiety about the virus itself as well as the economic effects of local and national shutdowns may have influenced psychological well-being. In fact, an early study of COVID-19 in March of 2020 reported that 15% of individuals in the U.S. had already reduced wages or work hours, and nearly 40% of Americans reported COVID-19-related financial stress (Ettman et al., 2020a, Nelson et al., 2020). By August of 2020, there were over 57 million Americans who had filed for unemployment since the start of the pandemic (Kelly, 2020). Without even considering the current pandemic, there are a myriad of studies noting that lower income, economic volatility, and financial hardship are strongly associated with worse mental health and substance use outcomes (Karanikolos et al., 2013, Nandi et al., 2012). Our study provides further support for the effects of economic hardship during the COVID-19 pandemic on substance use such that those who reported losing their job, being furloughed, or experienced reduced work hours reported increased binge drinking and alcohol use.
In general, loneliness was associated with lower alcohol use over the one-year study period. Recent work assessing loneliness on a variety of behavioral health outcomes notes that individuals reporting higher loneliness also reported worsening mental health symptoms (particularly depression) throughout the COVID-19 period (Creese et al., 2021). In a recent narrative review, Ingram et al. (2020) reported, across 41 studies, that loneliness is associated with poor mental health and greater substance use problems. Our results are in contrast to these studies and recent work noting that loneliness due to COVID-19 is associated with worse outcomes across a variety of domains (Creese et al., 2021, McGinty et al., 2020). However, some recent work among a representative sample of American adults noted no change in loneliness during the pandemic and, on the contrary, some groups reported decreased loneliness (Luchetti et al., 2020). Thus, it may be that, for some individuals, such as those living alone and individuals with chronic or serious conditions (e.g., heart conditions, pre-exiting medical conditions, or serious mental illness), loneliness may play more of a role in their behavioral health outcomes. One potential explanation of our results is, while the country was ordered to stay home and avoid social contact, there is some anecdotal evidence of increases in social connections during COVID, even if those connections were happening in ways other than in-person; for example, connecting with friends online or video chat (Klein, 2020, McCammon, 2020). These greater social connections may counteract effects of loneliness, especially in the early months of the pandemic. Our results did differ slightly based on the outcome being assessed, such that loneliness was associated with lower binge drinking early on, but at the one-year follow-up, loneliness was associated with greater binge drinking. Thus, it may be that cumulative loneliness influences more risky and heavy drinking practices.
4.1. Limitations
The current study should be interpreted in light of several limitations. First, all data were self-reported, lending to potential misreporting. However, numerous studies have reported on the validity of self-reported substance use and mental health conditions (e.g., Simons, Wills, Emery, & Marks, 2015). Second, results are not causal in nature. While we report on temporally ordered effects, there may be other third variables that help explain our results. We also only measured negative reactions to COVID-19 at 6- and 9-month follow-ups, thus limiting our ability to assess if these effects were carried out to one year after the pandemic hit the U.S. Finally, our results may not generalize to all veterans. We utilized a sample of veterans recruited outside of the VA and assessed for probable PTSD using self-report screening instruments. Clinical samples recruited from health care facilities with diagnosed disorders may differ in their behaviors, as might veterans who do not use social media.
4.2. Conclusions
This is the first study, to our knowledge, investigating longitudinal change in substance use among an understudied and high-risk group of veterans recruited in the community and outside of traditional health care facilities. Our results are in line with some theory noting decreases in substance use during the pandemic, but incongruent with other studies noting increases in substance use in the general population. Our results point to clear disparities among veterans during the COVID-19 pandemic. While the overall prevalence of alcohol use decreased over one year of the pandemic, some individuals, specifically women and racial/ethnic minority veterans, showed a different trajectory. This was also true of individuals who reported pre-pandemic PTSD. Our results are notable in light of the fact that veterans with co-occurring disorders are resistant to seek care, as only half of veterans with substance use disorders or mental health disorders (i.e., those who could benefit from care) actually seek care from the VA or elsewhere, and those that do often do not engage in care long enough to receive an adequate dose of treatment (Schell and Marshall, 2008, U.S Department of Veterans Affairs, 2018). Thus, it is clear that some individuals may require additional outreach or services during this high stress time.
Role of Funding Source
This research was funded by grant R01AA026575 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA), supplement R01AA026575-02S1, and a Keck School of Medicine COVID-19 Research Funding Grant awarded to Eric R. Pedersen.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.addbeh.2021.107052.
Appendix A. Supplementary data
The following are the Supplementary data to this article:
References
- Alonzi, S., La Torre, A., Silverstein, M.W., 2020. The psychological impact of preexisting mental and physical health conditions during the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy. [DOI] [PubMed]
- Aronson K.R., Perkins D.F., Morgan N.R., Bleser J.A., Vogt D., Copeland L.A., Finley E.P., Gilman C.L. The impact of adverse childhood experiences (ACEs) and combat exposure on mental health conditions among new post-9/11 veterans. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12(7):698–706. doi: 10.1037/tra0000614. [DOI] [PubMed] [Google Scholar]
- Bovin M.J., Marx B.P., Weathers F.W., Gallagher M.W., Rodriguez P., Schnurr P.P., Keane T.M. Psychometric properties of the PTSD checklist for diagnostic and statistical manual of mental disorders-fifth edition (PCL-5) in veterans. Psychological Assessment. 2016;28(11):1379–1391. doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- Creese, B., Khan, Z., Henley, W., O’Dwyer, S., Corbett, A., Vasconcelos Da Silva, M., Mills, K., Wright, N., Testad, I., Aarsland, D., Ballard, C., 2020. Loneliness, physical activity, and mental health during COVID-19: a longitudinal analysis of depression and anxiety in adults over the age of 50 between 2015 and 2020. International Psychogeriatrics, 1-10. [DOI] [PMC free article] [PubMed]
- Calhoun P.S., Elter J.R., Jones E.R., Kudler H., Straits-Troster K. Hazardous alcohol use and receipt of risk-reduction counseling among US veterans of the wars in Iraq and Afghanistan. The Journal of Clinical Psychiatry. 2008;69(11):1686–1693. doi: 10.4088/jcp.v69n1103. [DOI] [PubMed] [Google Scholar]
- Czeisler M.É., Lane R.I., Petrosky E., Wiley J.F., Christensen A., Njai R., Weaver M.D., Robbins R., Facer-Childs E.R., Barger L.K., Czeisler C.A., Howard M.E., Rajaratnam S.M.W. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report. 2020;69(32):1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derefinko, K.J., Hallsell, T.A., Isaacs, M.B., Salgado Garcia, F.I., Colvin, L.W., Bursac, Z., McDevitt-Murphy, M.E., Murphy, J.G., Little, M.A., Talcott, G.W., 2018. Substance use and psychological distress before and after the military to civilian transition. Military Medicine 183(5-6), e258-e265. [DOI] [PubMed]
- Eisen S.V., Schultz M.R., Vogt D., Glickman M.E., Elwy A.R., Drainoni M.-L.…Martin J. Mental and physical health status and alcohol and drug use following return from deployment to Iraq or Afghanistan. American Journal of Public Health. 2012;102(S1):S66–S73. doi: 10.2105/AJPH.2011.300609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman C.K., Abdalla S.M., Cohen G.H., Sampson L., Vivier P.M., Galea S. Low assets and financial stressors associated with higher depression during COVID-19 in a nationally representative sample of US adults. J Epidemiol Community Health. 2021;75(6):501–508. doi: 10.1136/jech-2020-215213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ettman, C.K., Abdalla, S.M., Cohen, G.H., Sampson, L., Vivier, P.M., Galea, S., 2020b. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open 3(9), e2019686-e2019686. [DOI] [PMC free article] [PubMed]
- Felitti V.J., Anda R.F., Nordenberg D., Williamson D.F., Spitz A.M., Edwards V., Koss M.P., Marks J.S. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick K.M., Harris C., Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychological Trauma. 2020;12(S1):S17–S21. doi: 10.1037/tra0000924. [DOI] [PubMed] [Google Scholar]
- Gallagher M.W., Zvolensky M.J., Long L.J., Rogers A.H., Garey L. The impact of covid-19 experiences and associated stress on anxiety, depression, and functional impairment in American adults. Cognitive Therapy and Research. 2020;44(6):1043–1051. doi: 10.1007/s10608-020-10143-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grasso, D.J., Briggs-Gowan, M.J., Ford, J.D., & Carter, A.S., 2020. The Epidemic – Pandemic Impacts Inventory (EPII).
- Grimm K.J., Ram N., Estabrook R. Guilford Publications; 2016. Growth modeling: Structural equation and multilevel modeling approaches. [Google Scholar]
- Hoge C.W., Auchterlonie J.L., Milliken C.S. Mental health problems, use of mental health services, and attrition from military service after returning from deployment to Iraq or Afghanistan. JAMA. 2006;295(9):1023–1032. doi: 10.1001/jama.295.9.1023. [DOI] [PubMed] [Google Scholar]
- Ingram I., Kelly P.J., Deane F.P., Baker A.L., Goh M.C.W., Raftery D.K., Dingle G.A. Loneliness among people with substance use problems: A narrative systematic review. Drug and Alcohol Review. 2020;39(5):447–483. doi: 10.1111/dar.13064. [DOI] [PubMed] [Google Scholar]
- Johns Hopkins Bloomberg School of Public Health, 2020. Mental health survey items from the COVID-19 and mental health measurement working group.
- Karanikolos M., Mladovsky P., Cylus J., Thomson S., Basu S., Stuckler D., Mackenbach J.P., McKee M. Financial crisis, austerity, and health in Europe. The Lancet. 2013;381(9874):1323–1331. doi: 10.1016/S0140-6736(13)60102-6. [DOI] [PubMed] [Google Scholar]
- Kelly, J., 2020. Jobless Claims: 57.4 Million Americans Have Sought Unemployment Benefits Since Mid-March—Over 1 Million People Filed Last Week. https://www.forbes.com/sites/jackkelly/2020/08/20/jobless-claims-574-million-americans-have-sought-unemployment-benefits-since-mid-marchover-1-million-people-filed-last-week/?sh=4637099c6d59. (Accessed May 10 2021).
- Kim J.U., Majid A., Judge R., Crook P., Nathwani R., Selvapatt N., Lovendoski J., Manousou P., Thursz M., Dhar A., Lewis H., Vergis N., Lemoine M. Effect of COVID-19 lockdown on alcohol consumption in patients with pre-existing alcohol use disorder. The Lancet Gastroenterology & Hepatology. 2020;5(10):886–887. doi: 10.1016/S2468-1253(20)30251-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein, N., 2020. Social Distancing Should Not Equal Social Isolation. https://www.psychologytoday.com/us/blog/the-intuitive-scientist/202004/social-distancing-should-not-equal-social-isolation. (Accessed May 10 2021).
- Liu C.H., Zhang E., Wong G.T.F., Hyun S., Hahm H.“. Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for U.S. young adult mental health. Psychiatry Research. 2020;290:113172. doi: 10.1016/j.psychres.2020.113172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luchetti M., Lee J.H., Aschwanden D., Sesker A., Strickhouser J.E., Terracciano A., Sutin A.R. The trajectory of loneliness in response to COVID-19. American. 2020;75(7):897–908. doi: 10.1037/amp0000690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCammon S. But Not Lonely; Despite The Coronavirus: 2020. How To Be Alone. https://www.npr.org/2020/03/17/816691923/how-to-be-alone-but-not-lonely-despite-the-coronavirus. (Accessed May 10 2021) [Google Scholar]
- McDevitt-Murphy M.E., Williams J.L., Bracken K.L., Fields J.A., Monahan C.J., Murphy J.G. PTSD symptoms, hazardous drinking, and health functioning among US OEF and OIF veterans presenting to primary care. Journal of Traumatic Stress: Official Publication of The International Society for Traumatic Stress Studies. 2010;23(1):108–111. doi: 10.1002/jts.20482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGinty, E.E., Presskreischer, R., Han, H., Barry, C.L., 2020. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. [DOI] [PMC free article] [PubMed]
- Nandi A., Prescott M.R., Cerdá M., Vlahov D., Tardiff K.J., Galea S. Economic conditions and suicide rates in New York City. American Journal of Epidemiology. 2012;175(6):527–535. doi: 10.1093/aje/kwr355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson L.M., Simard J.F., Oluyomi A., Nava V., Rosas L.G., Bondy M., Linos E. US public concerns about the COVID-19 pandemic from results of a survey given via social media. JAMA Internal Medicine. 2020;180(7):1020–1022. doi: 10.1001/jamainternmed.2020.1369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Özdin S., Bayrak Özdin Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. International Journal of Social Psychiatry. 2020;66(5):504–511. doi: 10.1177/0020764020927051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollard M.S., Tucker J.S., Green H.D. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Network Open. 2020;3(9):e2022942. doi: 10.1001/jamanetworkopen.2020.22942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar R.P. COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry. 2020;52:102066. doi: 10.1016/j.ajp.2020.102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J., Kilian C., Ferreira-Borges C., Jernigan D., Monteiro M., Parry C.D., Sanchez Z.M., Manthey J. Alcohol use in times of the COVID 19: Implications for monitoring and policy. Drug and Alcohol Review. 2020;39(4):301–304. doi: 10.1111/dar.13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rentsch C.T., Kidwai-Khan F., Tate J.P., Park L.S., King J.T., Jr, Skanderson M., Hauser R.G., Schultze A., Jarvis C.I., Holodniy M. Covid-19 by race and ethnicity: A national cohort study of 6 million United States veterans. MedRxiv. 2020 doi: 10.1371/journal.pmed.1003379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers A.H., Shepherd J.M., Garey L., Zvolensky M.J. Psychological factors associated with substance use initiation during the COVID-19 pandemic. Psychiatry Research. 2020;293:113407. doi: 10.1016/j.psychres.2020.113407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell D.W. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of Personality Assessment. 1996;66(1):20–40. doi: 10.1207/s15327752jpa6601_2. [DOI] [PubMed] [Google Scholar]
- Ruprecht M.M., Wang X., Johnson A.K., Xu J., Felt D., Ihenacho S.…Phillips II G. Evidence of social and structural COVID-19 disparities by sexual orientation, gender identity, and race/ethnicity in an urban environment. Journal of Urban Health. 2021;98(1):27–40. doi: 10.1007/s11524-020-00497-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schell, T.L., Marshall, G.N., 2008. Survey of individuals previously deployed for OEF/OIF. In T. Tanielian, & L.H. Jaycox (Eds.). Invisible wounds of war: Psychological and cognitive Injuries, their consequences, and services to assist recovery Santa Monica, CA: RAND MG-720. Available at: http://www.rand.org/pubs/monographs/2008/RAND_MG720.pdf.
- Seal K.H., Cohen G., Waldrop A., Cohen B.E., Maguen S., Ren L.i. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug Alcohol Depend. 2011;116(1-3):93–101. doi: 10.1016/j.drugalcdep.2010.11.027. [DOI] [PubMed] [Google Scholar]
- Simons J.S., Wills T.A., Emery N.N., Marks R.M. Quantifying alcohol consumption: Self-report, transdermal assessment, and prediction of dependence symptoms. Addiction Behaviour. 2015;50:205–212. doi: 10.1016/j.addbeh.2015.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trivedi R.B., Post E.P., Sun H., Pomerantz A., Saxon A.J., Piette J.D., Maynard C., Arnow B., Curtis I., Fihn S.D., Nelson K. Prevalence, comorbidity, and prognosis of mental health among US Veterans. American Journal of Public Health. 2015;105(12):2564–2569. doi: 10.2105/AJPH.2015.302836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai S., Nguyen H., Ebrahimi R., Barbosa M.R., Ramanan B., Heitjan D.F.…Jeon-Slaughter H. COVID-19 associated mortality and cardiovascular disease outcomes among US women veterans. Scientific Reports. 2021;11(1):1–10. doi: 10.1038/s41598-021-88111-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S Department of Veterans Affairs, 2018. “Profile of Post-9/11 Veterans: 2016,” briefing slides, March 2018. As of May 20, 2020: https://www.va.gov/vetdata/docs/SpecialReports/Post_911_Veterans_Profile_2016.pdf.
- Vanderbruggen N., Matthys F., Van Laere S., Zeeuws D., Santermans L., Van den Ameele S., Crunelle C.L. Self-reported alcohol, tobacco, and cannabis use during COVID-19 lockdown measures: Results from a web-based survey. European Addiction Research. 2020;26(6):309–315. doi: 10.1159/000510822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witteveen, D., Velthorst, E., 2020. Economic hardship and mental health complaints during COVID-19. Proceedings of the National Academy of Sciences 117(44), 27277-27284. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.