ABSTRACT
This study aims to investigate healthcare workers’ (HCWs) willingness to receive SARS-CoV-2 vaccine in Zhejiang and to discover the related influential factors. The survey was conducted in six regions of Zhejiang Province, China, and 13 hospitals and 12 Centers for Disease Control and Prevention (CDC) were incorporated into the survey research. Participants were healthcare workers and a total of 3726 questionnaires were collected online, of which 3634 (97.53%) were analyzed. The relationships between the factors and the willingness to get vaccinated against COVID-19 were computed as odds ratios (ORs) by means of multi-factor non-conditional logistic regression analysis. Of the 3634 participants, 2874 (79.09%) HCWs expressed their willingness to get vaccinated if the SARS-CoV-2 vaccine becomes available. Respondents who were younger than 50 years (OR = 1.502, 95% CI: 1.047–2.154), those who believed that they were somewhat likely (OR = 1.658, 95% CI: 1.297–2.120) or likely (OR = 1.893, 95% CI: 1.334–2.684) to get infected by SARS-COV-2 and those with a positive attitude toward the SARS-CoV-2 vaccine were more willing to get vaccinated. Furthermore, compared to doctors, nurses were more reluctant to get vaccinated. In addition, it was found that higher the education level, lower the willingness to get vaccinated. This study revealed that HCWs in Zhejiang Province had a high willingness to get vaccinated. Awareness about the vaccine’s effectiveness and safety and the disease severity should be promoted among HCWs over 50 years of age and nurses to increase the willingness to get vaccinated.
KEYWORDS: willingness, vaccine, healthcare workers, COVID-19, vaccine hesitancy
Introduction
The COVID-19 pandemic continues to incur massive human and economic losses worldwide. At the end of 2020, SARS-CoV-2 had infected over 80 million people and claimed over 1.7 million lives globally.1 The development and inoculation of SARS-CoV-2 vaccines is critical for controlling the pandemic. According to WHO, there are over 200 SARS-CoV-2 vaccines under development, of which more than 60 are in clinical development.2 Currently, China has 15 vaccines in clinical trials, among which 5 have entered phase III trials.3 About 60,000 volunteers were inoculated with these vaccine candidates. Preliminary results show that these vaccines are generally safe and only minor side effects have been observed.3,4
As of 18 February 2021, eight different vaccines have been rolled out globally: Pfizer-BioNTech,Oxford-AstraZeneca, Moderna, Sinopharm-Beijing, Gamaleya (Sputnik V), Sinovac, Sinopharm-Wuhan and Bharat Biotech (Covaxin).5 More than 184 million COVID-19 vaccination doses have been administered worldwide, which amounts to 2.36 doses for every 100 people in the total world population.6 This data is compiled from government sources by the Our World in Data project of the University of Oxford. Thus, the number of doses may not be equal to the total number of people vaccinated or fully vaccinated.
Most countries prioritize vaccine delivery to three key groups: frontline workers, clinically vulnerable groups, and older adults. By February 16, 2021, Israel had vaccinated its population faster than any other country, with 78.09 doses administered per 100 people; this was followed by United Arab Emirates, with 52.56 doses per 100 people, United Kingdom with 23.75 doses, United States with 16.51 doses, European Union with 5.07 doses, and China with 2.82 doses.6
Vaccines save millions of lives each year, but this effective measure is often challenged by individuals or groups who choose to delay or refuse vaccination.7 Vaccine hesitancy is a major barrier to herd immunity. Experts have conveyed that laying the groundwork for public acceptance of a SARS-CoV-2 vaccine is critical before the vaccine is made available. Healthcare workers (HCWs) have been fighting the pandemic from the frontline. A vaccination can not only protect their well-being but also persuade the general public, especially the reluctant population, to get vaccinated through their example.8 Therefore, investigating HCWs’ attitude toward the COVID-19 vaccination and its influencing factors will help the SARS-CoV-2 vaccine campaign.
Zhejiang Province reported the first confirmed case of COVID-19 on January 18, 2020. It is located in the south wing of the Yangtze River Delta, on the southeast coast of China, in the transition zone between Eurasia and the Northwest Pacific, which is a typical subtropical monsoon climate zone. As one of the smallest provinces in China, Zhejiang only has 11 cities, with a population of 58.5 million, and its annual gross regional product (GDP) was 6,235.2 billion yuan at the end of 2019.9 Zhejiang Province launched the level I public health emergency response on January 23, 2020. It was the first Chinese province to initiate the level I response. On March 2, 2020, Zhejiang province resorted to a level II response. By November 15, 2020, 1,291 confirmed cases and 281 asymptomatic cases had been reported in Zhejiang. In this study, participants were HCWs who have been fighting the COVID-19 pandemic from Centers for Disease Control and Prevention (CDC) and general public hospitals in Zhejiang province of China. We aimed to assess the willingness to receive the SARS-CoV-2 vaccination among HCWs in Zhejiang, and we also tried to have an in-depth understanding of the underlying factors affecting the decision toward getting vaccinated, especially the factors related to vaccine hesitancy. Our study may help policy-makers formulate more accurate immunization strategies.
Materials and methods
Participants
Area: The survey was conducted in 6 of the 11 cities of Zhejiang Province: Hangzhou, Wenzhou, Jiaxing, Jinhua, Lishui, and Zhoushan. We randomly selected one county in each city.
Institution: Among all medical institutions, hospitals and CDCs were selected as research subjects. There is one municipal CDC in each city and one county-level CDC in each county. The municipal CDC and the county-level CDC were chosen in selected area. Additionally, each selected city has multiple public and private hospitals. We picked general public hospitals as survey targets because in China, public hospitals have more staff and bigger scale, and COVID-19 patients have been exclusively diagnosed and treated in general public hospitals. Considering that the largest public hospital often leads local mainstream opinions, in the selected area mentioned above, we picked the largest municipal public general hospital in each city and the largest county-level public general hospital in each county. Hangzhou as the provincial capital of Zhejiang Province, has more public hospitals than other cities, one additional provincial hospital was chosen. In total, there were 13 hospitals and 12 CDCs designated.
Participant: Participants were HCWs from the selected CDCs and hospitals, who participated in the survey and voluntarily completed the questionnaire. Informed consent was obtained from all healthcare workers before conducting the survey. No personal identification information was collected or stored (see Figure 1).
Figure 1.
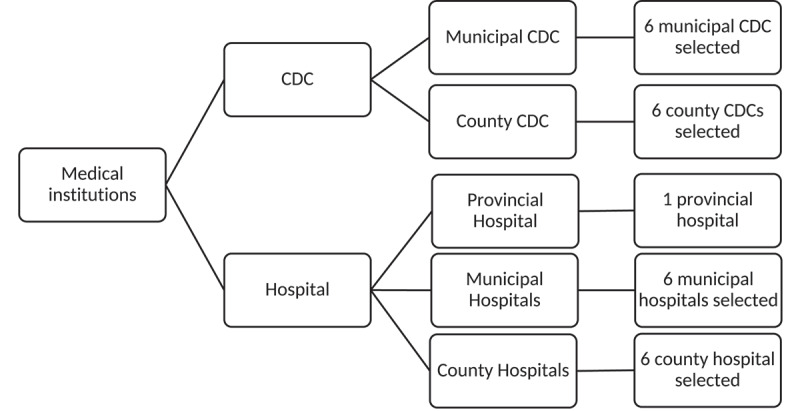
Sampling flow chart of survey participants in Zhejiang Province, China
A total of 3726 filled questionnaires were collected online (via WJX.com). Of these, 92 (2.47%) were excluded because of missing information; the remaining 3634 (97.53%) were used for data analysis.
Procedure
The study was conducted between September 15 and 20, 2020, and the procedures were in accordance with the Declaration of Helsinki principles. A questionnaire survey method was adopted and a set of questionnaires were administered online.
Questionnaire
The overall willingness-related question was, “Are you going to get vaccinated if the SARS-CoV-2 vaccine becomes available?” Additionally, the questionnaire consisted of other two sections, as follows:
Demographic information: including gender, age, medical department, educational background, designation, work experience, and medical history (including history of chronic diseases such as cardiovascular, cerebrovascular, and kidney diseases).
- Responses about attitude to COVID-19, as well as attitude to SARS-CoV-2 vaccine, including three parts of vaccine hesitancy related items.
- Attitude toward COVID-19 including perceptions of COVID-19 severity and self-assessment of vulnerability to SARS-COV-2 infection, were gathered. Questions such as “Do you think COVID-19 can cause serious damage?” and “How likely do you believe you are to get infected with SARS-COV-2?” was used to gauge HCWs’ attitude toward COVID-19 severity and to measure the perceived vulnerability, respectively.
- Attitudes toward SARS-CoV-2 vaccine including the necessity of the vaccination, vaccine safety, effectiveness, as well as vaccination outcome expectations.
- Acceptable vaccine pricing.
The reliability of the vaccine-related items was evaluated according to Cronbach’s coefficient and the alpha coefficient value was 0.799.
Statistical analysis
EpiData was used for data input and database development. Epi Info 7 and SPSS (Version 22.0) were used for data analysis. Qualitative data were described using numbers and/or proportion, and the differences were compared using the Chi-square test. We used a multi-factor logistic regression analysis model [Forward (STEP): LR] for influential factor exploration, leaving behind statistically significant Odds rations (OR). Single factors that were found to be statistically significant using a Chi-square test or were considered professionally essential were included as independent variables in the model. OR showed the strength of the association between these factors and the willingness to get vaccinated. Statistical significance was set at p < .05.
Furthermore, we used a collinearity diagnosis module in linear regression to perform a collinearity diagnosis. According to the judgment of the independent variable tolerance and the variance inflation factors (VIF), there is no collinearity.
Results
Demographic characteristics of the participants
As shown in Table 1, of the 3634 HCWs, 2874 (79.09%) expressed their willingness to get vaccinated if the SARS-COV-2 vaccine became available, while 760 (20.91%) were reluctant. The median age of HCWs in this survey was 34 years (interquartile range [IQR]: 28–41 years), with 2814 (77.44%) females. There were 3202 (88.11%) participants from hospitals and 432 (11.89%) from CDCs. Among them, 1841 (50.66%) were nurses and 1123 (30.90%) were doctors, followed by 373 (10.26%) health technicians and 297 (8.17%) others (administrators, volunteers, etc.). The median duration of work experience was 10 years (IQR: 5–19 years). Most HCWs had a bachelor’s degree or a higher level of education, while 485 (13.35%) had junior college diplomas or lower. A total of 662 (18.22%) participants indicated they could have come in close contact with COVID-19 patients at work. A total of 297 (8.17%) HCWs had preexisting medical conditions, such as cardiovascular diseases and diabetes.
Table 1.
Demographic characteristics of survey participants in Zhejiang Province, China (September 2020; N = 3634)
| Characteristics | Willingness to receive SARS-CoV-2 vaccine |
p-value | ||
|---|---|---|---|---|
| Total (N) |
Yes (N, %) |
No or uncertain (N, %) | ||
| Gender | <0.001 | |||
| Male | 820 | 689 (84.02%) | 131 (15.98%) | |
| Female | 2814 | 2185 (77.65%) | 629 (22.35%) | |
| Age group | <0.001 | |||
| ≥50 years old | 432 | 375 (86.81%) | 57 (13.19%) | |
| < 50 years old | 3202 | 2499 (78.04%) | 703 (21.96%) | |
| Education | <0.001 | |||
| Associate’s degree or lower | 485 | 422 (87.01%) | 63 (12.99%) | |
| Bachelor’s degree | 2625 | 2060 (78.48%) | 565 (21.52%) | |
| Master’s degree | 447 | 344 (76.96%) | 103 (23.04%) | |
| PhD | 77 | 48 (62.34%) | 29 (37.66%) | |
| Profession | <0.001 | |||
| Doctors | 1123 | 929 (82.72%) | 194 (17.28%) | |
| Health technicians | 373 | 293 (78.55%) | 80 (21.45%) | |
| Nurses | 1841 | 1400 (76.05%) | 441 (23.95%) | |
| Others | 297 | 252 (84.85%) | 45 (15.15%) | |
| Institution | <0.001 | |||
| Hospital | 3202 | 2499 (78.04%) | 703 (21.96%) | |
| CDC | 432 | 375 (86.81%) | 57 (13.19%) | |
| Close contact with COVID-19 patients at work | 0.800 | |||
| Yes | 662 | 526 (79.46%) | 136 (20.54%) | |
| No | 2972 | 2348 (79.00%) | 624 (21.00%) | |
| Work experience | 0.754 | |||
| ≤ 5 years | 1044 | 837 (80.17%) | 207 (19.83%) | |
| 6–10 years | 933 | 730 (78.24%) | 203 (21.76%) | |
| 11–20 years | 901 | 710 (78.80%) | 191 (21.20%) | |
| >20 years | 756 | 597 (78.97%) | 159 (21.03%) | |
| Preexisting medical conditions | 0.006 | |||
| Yes | 3337 | 2652(79.47%) | 685 (20.53%) | |
| No | 297 | 222(74.75%) | 75 (25.25%) | |
Note: COVID-19, coronavirus disease 2019;
Attitude toward COVID-19 and SARS-CoV-2 vaccine
Attitude toward COVID-19
The first two items in Table 2 presents the participants’ perceptions of COVID-19 severity and self-assessment of vulnerability to SARS-COV-2 infection. Questions such as “Do you think COVID-19 can cause serious damage?” were used to gauge HCWs’ attitude toward COVID-19 severity. A total of 2438 participants believed it could be very serious, of which 1979 (81.17%) were willing to receive the vaccines. Similarly, questions such as “How likely do you believe you are to get infected with SARS-COV-2?” were used to measure the vulnerability. Over 2700 respondents believed that they were “likely” or “somewhat likely” to be infected by the virus; therefore, more than 80% of them present their willingness to get vaccinated.
Table 2.
Attitude to COVID-19 and SARS-CoV-2 vaccine of survey participants in Zhejiang Province, China (September 2020; N = 3634)
| Questionnaire item | Willingness to receive SARS-CoV-2 vaccine |
p-value | ||
|---|---|---|---|---|
| Total (N) |
Yes (N, %) |
No or uncertain (N, %) | ||
| Do you think COVID-19 can cause serious damage | <0.001 | |||
| Very Serious | 2438 | 1979 (81.17%) | 459 (18.83%) | |
| Serious | 1125 | 854 (75.91%) | 271 (24.09%) | |
| Average | 63 | 39 (61.90%) | 24 (38.10%) | |
| Not Serious or uncertain | 8 | 2 (25.00%) | 6 (75.00%) | |
| How likely do you believe you are to get infected with SARS-COV-2 | <0.001 | |||
| Not Likely | 701 | 533 (76.03%) | 168 (23.97%) | |
| Somewhat Likely | 2214 | 1784 (80.58%) | 430 (19.42%) | |
| Likely | 490 | 403 (82.24%) | 87 (17.76%) | |
| Uncertain | 229 | 154 (67.25%) | 75 (32.75%) | |
| Do you agree that getting vaccinated against COVID-19 is important to protect you from COVID-19 | <0.001 | |||
| No or Uncertain | 697 | 312 (44.76%) | 385 (55.24%) | |
| Yes | 2937 | 2562 (87.23%) | 375 (12.77%) | |
| SARS-CoV-2 vaccine approved by the Government is safe | <0.001 | |||
| Disagree or Neutral | 823 | 399 (48.48%) | 424 (51.52%) | |
| Agree | 2811 | 2475 (88.05%) | 336 (11.95%) | |
| SARS-CoV-2 vaccine approved by the Government is effective | <0.001 | |||
| Disagree or Neutral | 922 | 467 (50.65%) | 455 (49.35%) | |
| Agree | 2712 | 2407 (88.75%) | 305 (11.25%) | |
| Do you believe vaccination can control the COVID-19 pandemic | <0.001 | |||
| No | 1119 | 616 (55.05%) | 503 (44.95%) | |
| Yes | 2515 | 2258 (89.78%) | 257 (10.22%) | |
| What is your highest acceptable total price for vaccination | <0.001 | |||
| Less than 100 yuan | 1086 | 853 (78.55%) | 233 (21.45%) | |
| 101–500 yuan | 1860 | 1468 (78.92%) | 392 (21.08%) | |
| 500–1000 yuan | 552 | 445 (80.62%) | 107 (19.38%) | |
| More than 1000 yuan | 136 | 108 (79.41%) | 28 (20.59%) | |
Note: COVID-19, coronavirus disease 2019;
Attitude toward SARS-CoV-2 vaccine
Majority of HCWs (2937/3634) believed that a vaccine would be an important tool to protect them from COVID-19. More than 70% of the participants agreed that SARS-CoV-2 vaccine approved by the National Medical Products Administration would be safe (2811) and effective (2712), but 11% of them were still unwilling or hesitant to be vaccinated. However, up to two thirds of respondents did not think that the vaccine could thwart the progress of the pandemic.
Acceptable total price of vaccine
Over 2900 HCWs suggested that acceptable vaccine prices should be under 500 yuan (RMB), while few participants agreed to a price of over 1000 yuan (RMB). Interestingly, regardless of the price range, the proportion of respondents willing to vaccinate were always around 80%.
Factors associated with willingness
The following factors were incorporated into the multivariable logistic regression: gender, institution, close contact with COVID-19 patient, preexisting condition, perception of severity, the price of vaccine, education, profession, perception of vulnerability and the attitude toward vaccination. Among these, the first six variables were not statistically significant.
Multivariate logistic regression analysis (see Table 3) revealed that factors predicting the willingness to receive SARS-CoV-2 vaccine were age and perceptions of vulnerability. Additionally, younger HCWs were more willing to get vaccinated (OR = 1.502, 95% confidence interval [CI]: 1.047–2.154) than those over 50 years old. Participants who believed that they were somewhat likely (OR = 1.658, 95% CI: 1.297–2.120) or likely (OR = 1.893, 95% CI: 1.334–2.684) to get infected with SARS-COV-2 were also more willing to get vaccinated.
Table 3.
Factors related to the willingness to receive SARS-CoV-2 vaccine of the survey participants (N = 3634)
| Factors | B | S.E. | Wald | p-value | Odds Ratio (95% CI) |
|---|---|---|---|---|---|
| Age group | |||||
| ≥50 years old (Ref.) | |||||
| < 50 years old | 0.401 | 0.184 | 4.887 | 0.027** | 1.502 (1.047–2.154) |
| Education | |||||
| Associate’s degree or lower (Ref.) | |||||
| Bachelor’s degree | 1.141 | 0.177 | 41.678 | <0.001** | 0.319 (0.226–0.452) |
| Master’s degree | 1.530 | 0.229 | 44.595 | <0.001** | 0.217 (0.138–0.339) |
| PhD | 1.819 | 0.338 | 29.040 | <0.001** | 0.162 (0.084–0.314) |
| Profession | |||||
| Doctors (Ref.) | |||||
| Health technicians | 0.311 | 0.180 | 2.980 | 0.084 | 0.733 (0.515–1.043) |
| Nurses | 0.364 | 0.130 | 7.842 | 0.005** | 0.695 (0.538–0.896) |
| Others | 0.086 | 0.221 | 0.151 | 0.698 | 1.089 (0.707–1.679) |
| How likely do you think you are to get infected with SARS-COV-2 | |||||
| Not Likely (Ref.) | |||||
| Somewhat Likely | 0.506 | 0.125 | 16.310 | <0.001** | 1.658 (1.297–2.120) |
| Maybe | 0.638 | 0.178 | 12.795 | <0.001** | 1.893 (1.334–2.684) |
| Uncertain | 0.139 | 0.204 | 0.468 | 0.494 | 0.870 (0.584–1.297) |
| SARS-CoV-2 vaccine approved by the Government is safe | |||||
| Disagree or Neutral (Ref.) | |||||
| Agree | 1.090 | 0.142 | 58.984 | <0.001** | 2.975 (2.253–3.930) |
| SARS-CoV-2 vaccine approved by the Government is effective | |||||
| Disagree or Neutral (Ref.) | |||||
| Agree | 0.581 | 0.144 | 16.320 | <0.001** | 1.788 (1.349–2.370) |
| Do you believe vaccination can control the COVID-19 pandemic | |||||
| No (Ref.) | |||||
| Yes | 1.014 | 0.112 | 82.377 | <0.001** | 2.755 (2.214–3.429) |
| Do you agree that getting vaccinated against COVID-19 is important to protect you from COVID-19 | |||||
| No or Uncertain (Ref.) | |||||
| Yes | 1.150 | 0.118 | 95.336 | <0.001** | 3.157 (2.507–3.977) |
Note: COVID-19, coronavirus disease; CI, confidence interval; **p < 0.05
The following factors were eliminated by the multivariate logistic regression model: gender, institution, close contact with COVID-19 patient, preexisting condition, perception of severity, price of vaccine.
Respondents with a positive attitude (trust that the vaccine would be safe and effective) toward the vaccination against COVID-19 were more willing to get vaccinated. However, in comparison to doctors, nurses were more reluctant to get vaccinated; additionally, it was observed that higher the education level, the lower the willingness to get vaccinated. ORs and 95% CIs are presented in Table 4.
Discussion
We conducted a study on the vaccination intentions 3634 HCWs, both from hospitals and CDCs, with respect to the SARS-CoV-2 vaccine. To the best of our knowledge, our study is the largest survey of HCWs’ vaccination willingness in China.
In the battle against COVID-19, HCWs deal with challenges every day. They are exposed to infection through treatment, nursing, epidemiological investigation, control, and prevention.10,11 Many were infected and several sacrificed their lives during this global pandemic.11 Some of them suffered stress, anxiety, and depression.10 In addition, patients and family members may be less vigilant around HCWs and are more susceptible to infection if HCWs become infected.12 Hence, HCWs must be protected from illness to prevent absenteeism during a pandemic and protect those they come in contact with.13 We found that compared to previous surveys conducted among the general public in Europe (73.9%) and the US (69%),14,15 the healthcare workers in our research had a higher willingness (79.09%) to get vaccinated; however, HCWs showed slightly lower vaccination intentions than the general public.16,17 As a newly developed vaccine, SARS-CoV-2 vaccine had a significantly higher acceptance rate than the A (H1N1) vaccine rate 10 years ago.13,18 The positive attitude toward vaccination might reflect the degree of trust in the government.16 It also indicates that HCWs believed COVID-19 pandemic was much sterner than the new influenza subtype pandemic.
Contrary to our expectations, although the HCWs from the hospitals and CDCs showed significant differences in single factor analysis, no statistical significance was observed after conducting a multivariable logistic regression analysis. Interestingly, our results revealed that nurses had a lower willingness to get vaccinated against COVID-19 than doctors. This result is consistent with some previous surveys on influenza vaccination willingness. Compared to doctors, nurses have a higher risk of exposure, as they engage in activities such as taking swabs, drawing blood, sputum suction, etc.19 Arda et al.13 suggested that nursing staff are less willing to be vaccinated because of misconceptions regarding the vaccine’s general effectiveness. Existing literature points out that the low willingness among nurses to be vaccinated may be related to their knowledge level. Despite their training, HCWs do not seem to understand that they can be a transmitting agent of the infection at work.12 However, we also found that higher levels of education lower their willingness to inoculate themselves. This is inconsistent with the results from Nature.20 Another previous study pointed out that the vaccination intention of doctors and nurses might be related to their income, marital status, positions, etc.21 Therefore, the difference in vaccination willingness between these two professionals needs to be studied further so that decision makers can formulate more targeted vaccination strategies.
In our multivariate analysis, another influential demographic aspect is age. Unlike previous studies, we found that the willingness to get vaccinated among HCWs over 50 years of age is lower than that among younger workers. In Zhejiang, many medical staff over 50 years had experienced the SARS outbreak in 2003, the H1N1 pandemic in 2009, and the H7N9 avian influenza outbreak in 2013. Except A (H1N1), the spread of the other two new infectious diseases was controlled without a vaccine. This may also lower their willingness to get vaccinated. Even though vaccination history has a positive effect on the willingness to be vaccinated,12,13 after remaining uninfected through during multiple epidemics, some people may overestimate their immunity.12 COVID-19 is evidently different from the viruses of previous epidemics. It spreads faster and is infectious during the incubation period. The initial symptoms are not apparent, making it difficult even for experienced doctors to make an early diagnosis.22 Therefore, the target population involved in public vaccines and health education should be treated differently according to their different experiences. For those who underestimate the role of vaccines, we should focus on making them aware of the dangers of diseases and the necessity of vaccines.
According to SAGE vaccine hesitancy working group, vaccine hesitancy is mainly affected by three factors: complacency, confidence, and convenience.23 These factors vary in different populations, as well as for different type of vaccines. As a relatively special group, HCWs have a stronger medical background, and are thus more cautious with a new vaccine before its safety, effectiveness, and long-term impact on the immune system are fully understood. Complacency refers to the lower perceived risks of vaccine-preventable diseases, where vaccination is not considered a necessary preventive method.23 In our research, we found that vaccine heritage is more common in those who believe that the severity of the disease is low and that they are unlikely to be infected. Most people who are willing to be vaccinated believe that the SARS-CoV-2 vaccine is an important way to protect themselves. Confidence refers to the trust in the safety and effectiveness of vaccines, in the health system that provide vaccine services, and vaccination policy-makers.23 According to our results, more than half of those hesitant about the vaccine, were worried about the safety (424/760) and effectiveness (455/760) of the vaccine, and did not believe that vaccines could control the COVID-19 pandemic. HCWs are not only the target population for vaccination, but also a trusted source of vaccine information.24 They are also considered to be the most effective interveners to deal with hesitation to vaccinate.25 Many studies have found that recommendations from the medical staff are particularly effective in improving the vaccination rate. The hesitation to vaccinate among HCWs and the lack of knowledge about vaccines may undermine the confidence of the population in the vaccines.26 Due to time constraints caused by work shifts, increased workload, and lack of training resources, HCWs do not have enough training to resolve of the doubts of vaccine hesitators, and some HCWs even agree to delay vaccination.26 Studies have also found that compared to the information provided by vaccine suppliers, HCWs display higher trust in the information provided by the government health department.24 Therefore, as the most effective intervener, it is necessary train HCWs more, about the vaccination, and provide them with more information from government departments.
The government played a certain role in affecting the willingness of getting vaccinated.27 It is unclear whether its role has a positive or negative impact. As early emergency response and non-pharmaceutical interventions, such as isolation and quarantine, have brought the epidemic under control, the urgency and necessity of vaccinations seems to have declined. In dealing with a new viral infectious disease, the role of vaccines is clear and positive in control and prevention. It requires reasonable guidance from the government and public health personnel. Public health agencies should develop a robust SARS-COV-2 vaccine educational campaign by leveraging traditional and modern social media, with a focus on involving influencers and targeting misinformation.8
It is also noteworthy that, although the price of vaccines acceptable to most people is below 500 yuan (about 77 US dollars), the price of the vaccine is not a factor influencing the willingness to inoculate oneself. Although China is a developing country, as an economically developed coastal area, the income of HCWs in Zhejiang Province is stable and relatively high. Thus, they are not particularly concerned with price factors.28
This study has some limitations. First, although in our survey, we chose the institutions randomly, the participants were recruited through a convenient sampling procedure by filling a voluntary online survey; such survey methods may have recruitment bias and certain deviations. For example, half of the respondents were nurses. However, the findings of this study are consistent with similar previous studies, and we can assume that the representativeness of the sample is reasonable. Second, our survey was conducted before the vaccination process began. Thus, with the progress of vaccine research and development in many countries, the safety and effectiveness of vaccines reported will continue to influence healthcare workers’ willingness to get vaccinated. Moreover, this research was only conducted in Zhejiang Province, and the demographic information of the sample may not be generalizable to all populations. This factor should be considered carefully when applying our research results.
In conclusion, HCWs in Zhejiang Province had a high willingness (79.09%) to get vaccinated if the SARS-CoV-2 vaccine became available. Factors associated with willingness are age, education level, profession, perceptions of vulnerability, and attitude toward vaccinations. Complacency of health, distrust of vaccine safety and effectiveness, and underestimating the necessity of the vaccination were important factors that influenced HCWs’ vaccine hesitancy. Training and health education about the vaccine’s effectiveness and safety and regarding the disease severity should be provided to HCWs over 50-years of age, and among nurses, to increase their willingness to be vaccinated. The scientific data on vaccine safety and effectiveness, provided by government departments, should be shared as soon as possible to increase the healthcare workers’ confidence about vaccinations. Improving healthcare workers’ inoculation willingness would provide a good demonstration effect for the public and help improve the vaccination rate among the general public for the ongoing COVID-19 pandemic.
Acknowledgments
The authors express their gratitude to all personnel working on COVID-19 control and prevention at all levels of hospitals, CDC, and other medical institutions in Zhejiang Province. We also would like to thank Editage (www.editage.cn) for English language editing.
Funding Statement
This work was supported by the Medical Science and Technology Project of Zhejiang Province under Grant number [2021KY950]; the Medical and Health Technology Project of Hangzhou Municipality under Grant number [A20200591]; and the Science and Technology Project of Hangzhou Municipality under Grant number [20202013A02].
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- 1.World Health Organization . WHO coronavirus disease (COVID-19) dashboard. 2020. [cited 2020 Dec 28]. Available from: https://covid19.who.int/
- 2.World Health Organization . WHO COVID-19 vaccines. 2020. [cited 2021 Feb 19]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines
- 3.National Health Commission of the People’s Republic of China . China at forefront of global COVID-19 vaccine development: official. [cited 2020 Dec 22]. Available from:http://en.nhc.gov.cn/2020-12/22/c_82524.htm
- 4.Zhang ZH, Wang XY.. Trials of China’s vaccines make major progress. China daily. [cited 2020 Dec 1]. Available from:https://www.chinadaily.com.cn/a/202010/21/WS5f8f6b55a31024ad0ba7fe52.html
- 5.Our world in data . Coronavirus (COVID-19) Vaccinations. [cited 2021 Feb 19]. Available from:https://ourworldindata.org/covid-vaccinations
- 6.Zimmer C, Corum J, Wee SL. Coronavirus vaccine tracker. [cited 2021 Feb 19]. Available from:https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html
- 7.Larson HJ, Jarrett C, Eckersberger E, Smith DM, Paterson P. Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007-2012. Vaccine. 2014;32:2150–59. doi: 10.1016/j.vaccine.2014.01.081. [DOI] [PubMed] [Google Scholar]
- 8.DeRoo SS, Pudalov NJ, Fu LY. Planning for a COVID-19 vaccination program. JAMA. 2020;323:2458–59. doi: 10.1001/jama.2020.8711. [DOI] [PubMed] [Google Scholar]
- 9.Zhejiang Province Government . General situation of Zhejiang Province. [cited 2021 Feb 19]http://www.zj.gov.cn/col/col1229216136/index.html
- 10.Shreffler J, Petrey J, Huecker M. The impact of COVID-19 on healthcare worker wellness: a scoping review. West J Emerg Med. 2020;21:1059–66. doi: 10.5811/westjem.2020.7.48684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Schwartz J, King -C-C, Yen M-Y, Schwartz J, Cc K, My Y. Protecting health care workers during the COVID-19 coronavirus outbreak –lessons from Taiwan’s SARS response. Clin Infect Dis. 2020;71:858–60. doi: 10.1093/cid/ciaa255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Claire B, Setbon M, Zylberman P, Flahault A. Healthcare worker compliance with seasonal and pandemic influenza vaccination. Influenza Other Respir Viruses. 2013;7:97–104. doi: 10.1111/irv.12088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arda B, Raika D, Yamazhan T, Sipahi OR, Tasbakan M, Pullukçu H, Erdem E, Ulusoy S. Did the pandemic have an impact on influenza vaccination attitude? a survey among health care workers. BMC Infect Dis. 2011;11:87. doi: 10.1186/1471-2334-11-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reiter PL, Pennell ML, Katz ML. Acceptability of a COVID-19 vaccine among adults in the United States: how many people would get vaccinated? Vaccine. 2020;38:6500–07. doi: 10.1016/j.vaccine.2020.08.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Neumann-Bohme S, Varghese NE, Sabat I, Barros PP, Brouwer W, Van Exel J, Schreyogg J, Stargardt T. Once we have it, will we use it? A European survey on willingness to be vaccinated against COVID-19. Eur J Health Econ. 2020;21:977–82. doi: 10.1007/s10198-020-01208-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chen MS, Li YJ, Chen JS, Wen ZY, Feng FL, Zou HC, Fu CX, Chen L, Shu YL, Sun CJ. An online survey of the attitude and willingness of Chinese adults to receive COVID-19 vaccination. Hum Vaccin Immunother. 2021Jan;31:1–10. Online ahead of print. doi: 10.1080/21645515.2020.1853449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang JH, Jing RZ, Lai XZ, Zhang HJ, Lyu Y, Knoll MD, Fang H. Acceptance of COVID-19 vaccination during the COVID-19 pandemic in China. Vaccines (Basel). 2020;8:482. doi: 10.3390/vaccines8030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Tawfiq JA. Willingness of health care workers of various nationalities to accept H1N1 (2009) pandemic influenza A vaccination. Ann Saudi Med. 2012;32:64–67. doi: 10.5144/0256-4947.2012.64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vírseda S, Restrepo MA, Arranz E, Magán-Tapia P, Fernández-Ruiz M, Cámara AGDL, Aguado JM, López-Medrano F. Seasonal and Pandemic A (H1N1) 2009 influenza vaccination coverage and attitudes among health-care workers in a Spanish University Hospital. Vaccine. 2010;28:4751–57. doi: 10.1016/j.vaccine.2010.04.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lazarus JV, Ratzan SC, Palayew A, Gostin LO, Larson HJ, Rabin K, Kimball S, El-Mohandes A. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. 2020;20:1–4. doi: 10.1038/s41591-020-1124-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Doebbeling BN, Edmond MB, Davis CS, Woodin JR, Zeitler RR. Influenza vaccination of health care workers: evaluation of factors that are important in acceptance. Prev Med. 1997;26:68–77. doi: 10.1006/pmed.1996.9991. [DOI] [PubMed] [Google Scholar]
- 22.Sun YX, Koh V, Marimuthu K, Ng OT, Young B, Vasoo S, Chan M, Lee VHM, De PP, Barkham T, et al. Epidemiological and clinical predictors of COVID-19. Clin Infect Dis. 2020;71:786–92. doi: 10.1093/cid/ciaa322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.MacDonald NE. SAGE working group on vaccine hesitancy. Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33:4161–64. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 24.Karafillakis E, Dinca I, Apfel F, Cecconi S, Wurz A, Takacs J, Suk J, Celentano LP, Kramarz P, Larson HJ. Vaccine hesitancy among healthcare workers in Europe: a qualitative study. Vaccine. 2016;34:5013–20. doi: 10.1016/j.vaccine.2016.08.029. [DOI] [PubMed] [Google Scholar]
- 25.Paterson P, Meurice F, Stanberry LR, Glismann S, Rosenthal SL, Larson HJ. Vaccine hesitancy and healthcare providers. Vaccine. 2016;34:6700–06. doi: 10.1016/j.vaccine.2016.10.042. [DOI] [PubMed] [Google Scholar]
- 26.Wei Z, Fu CX. Progress on vaccine hesitancy and its influential factors. Prog in Microbiol Immunol. 2019;47:74–78. doi: 10.13309/j.cnki.pmi.2019.05.014. [DOI] [Google Scholar]
- 27.Peretti-Watel P, Seror V, Cortaredona S, Launay O, Raude J, Verger P, François B, Legleye S, L’Haridon O, Ward J. A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicization. Lancet Infect Dis. 2020;20:769–70. doi: 10.1016/s1473-3099(20)30426-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, Seriawan AM, Rajamoorthy Y, Sofyan H, Vo TQ, et al. Willingness-to-pay for a COVID-19 vaccine and its associated determinants in Indonesia. Hum Vaccin Immunother. 2020;16:3074–80. doi: 10.1080/21645515.2020.1819741. [DOI] [PMC free article] [PubMed] [Google Scholar]


