Abstract
Objective:
To compare the effectiveness of comprehensive fixed appliance treatments implemented in combination with Forsus or intermaxillary elastics in Class II subdivision subjects.
Materials and Methods:
Twenty-eight Class II subdivision patients were allocated to two groups using matched randomization: Forsus group (mean age, 14.19 ± 1.02 years) and elastics group (mean age, 13.75 ± 1.16 years). Patients received fixed appliance therapy in combination with either Forsus or intermaxillary elastics. The study was conducted on lateral cephalograms and digital models acquired before orthodontic treatment and 10–12 weeks after the fixed appliances were removed.
Results:
The treatment phase comprising the use of Forsus (4.53 ± 0.91 months) was significantly shorter compared with elastics application (6.85 ± 1.08 months). This was also true for comparing duration of overall comprehensive treatment in both groups. Extrusion and palatal tipping of maxillary incisors and clockwise rotation of the occlusal plane were greater in the elastics group (P < .05). The mandibular incisors were proclined in both groups (P < .001), but no significant difference was observed between groups (P > .05). The mandibular incisors showed intrusion in the Forsus group and extrusion in the elastics group; the difference between groups was significant (P < .05). Overbite was decreased in both groups (P < .001) in similar amounts. Improvement in overjet, mandibular midline deviation, and correction of molar relationship on the Class II side were greater in the Forsus group (P < .05).
Conclusion:
Forsus is more effective for correcting Class II subdivision malocclusion in a shorter treatment period with minimal patient compliance required.
Keywords: Class II subdivision, Intermaxillary elastics, Fixed functional appliance
INTRODUCTION
Angle Class II subdivision classification describes a type of asymmetric malocclusion wherein the molar occlusion is Class II on one side and Class I on the other. Unilateral distal positioning of the mandibular first molar seems to be the major contributing factor in this malocclusion,1–4 while mesial positioning of the maxillary molars,1,3–5 asymmetric mandible,6–8 posterior position of the glenoid fossa,9 and functional mandibular shift9 can also be responsible for the Class II molar relationship in this type of occlusal disharmony.
The treatment of Class II subdivision malocclusion includes a variety of alternatives such as (a) nonextraction protocols with tip-back mechanics,10 intermaxillary elastics,11,12 extraoral appliances,13 and fixed functional appliances14,15; (b) extraction treatments with one, three, or four premolar extraction protocols11,12,16; and (c) orthognathic surgery.17 However, treatment trends over the past 15 years show that elastics and fixed functional appliance usage have increased from 20% to 38% and from 0% to about 15%, respectively, while the rates of orthognathic surgery and extraction treatment decreased for these patients.18
The Forsus Fatigue Resistance Device (Forsus; 3M Unitek, Monrovia, Calif) is a fixed functional appliance that has received increasing interest as an effective and noncompliant option for Class II Division 1 treatment. Unfortunately, only a case report on the treatment of Class II subdivision malocclusion with Forsus has been published.14 Although intermaxillary elastics and fixed functional appliance are the most common means of resolving this problem,18 no statistical analysis comparing the effectiveness of the aforementioned methods has previously been performed.
The aim of this study was to compare by means of lateral cephalograms and study models the treatment effects of the Forsus Fatigue Resistant Device vs intermaxillary elastics in combination with fixed appliances for correction of Class II subdivision malocclusion.
MATERIALS AND METHODS
Patients with the following characteristics were included in this study: (1) Angle Class II subdivision malocclusion in the permanent dentition, based on the presence of Class I molar relationship on one side and at least end-to-end Class II molar relationship on the other; (2) absence of severe crowding; (3) normal or slightly increased overbite; (4) mild or moderately increased overjet; (5) maxillary midline coincident with facial midline; (6) mandibular midline deviation to the Class II side; and (7) no functional lateral mandibular shift during closure (determined by clinical examination). Matched randomization was used for allocation of patients to the two study groups.19 Subjects were divided into 17 pairs. Patients within each pair were selected so that they had a similar degree of malocclusion (based on overjet, molar relationship, and crowding). One of the patients in each pair, randomly selected through tossing a coin, received fixed appliance treatment with the Forsus group (Forsus FRD) whereas the other patient received fixed appliance treatment with intermaxillary elastics (elastics group). The study protocol was approved by the Ethics Committee of the School of Medicine, Ege University.
All patients underwent a nonextraction treatment protocol with 0.018-inch preadjusted fixed appliances. Overall treatment consisted of leveling and aligning, followed by Forsus FRD or intermaxillary elastics, and detailing. When maxillary and mandibular 0.017 × 0.025-inch stainless steel archwires were inserted, elastics usage was initiated in the elastics group while Forsus FRDs were attached to the maxillary first molars (through the EZ 2 module) and mandibular arches in the Forsus group.
In the elastics group, Class II elastics (1/4-inch, 6-ounce) extending from the maxillary canine to the mandibular second molar were applied on the Class II side, while triangular elastics (1/4-inch, 6-ounce) attached to the maxillary canine, mandibular first premolar, and mandibular second molar were worn on the Class I side (Figure 1). Forsus springs were fitted onto mandibular archwires between the canine and first premolar bracket on the Class I side and between the first and second premolars on the Class II side (Figure 2). A split crimp was added on the push rod only on the Class II side at 4–6-week intervals as needed.
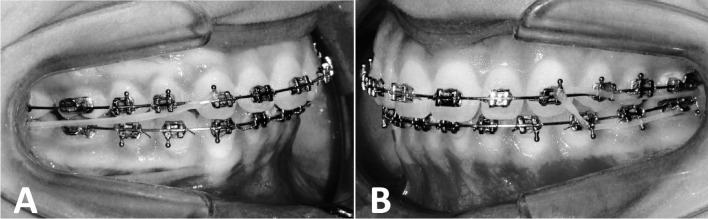
Figure 1.
Application of elastics on (A) Class II side and (B) Class I side.
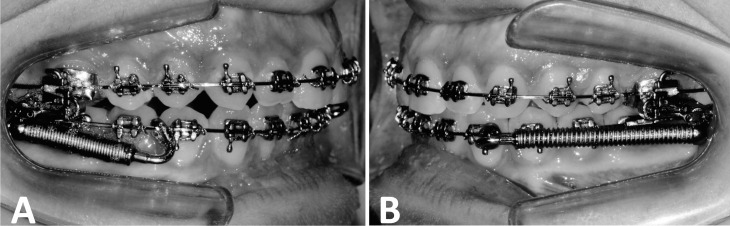
Figure 2.
Application of Forsus on (A) Class II side and (B) Class I side.
The active phase with Forsus and intermaxillary elastics was undertaken until the Class II molar relation was corrected to a Class I. In the subsequent detailing/finishing phase, elastics for interdigitation were used when indicated. After debonding, lingual fixed retainers were bonded to the anterior teeth.
The study was conducted on lateral cephalograms and digital models acquired before treatment (T1) and 10–12 weeks after fixed-appliance removal (T2). Appraisal of all cephalometric radiographs and digital models were carried out by one examiner in a blinded manner. Cephalometric measurements were made using Dolphin Imagining 11.0 Software (Dolphin Imaging and Management Solutions, Chatsworth, Calif) (Figure 3). Model measurements were done using Orthomodel 2.0.206 Software (Orthomodel, Istanbul, Turkey). Molar relationship was evaluated in terms of difference from the mesiobuccal cusp tip of the maxillary first molar to the mesiobuccal groove of the mandibular first molar. While a perfect Class I molar relationship was represented by exact coincidence of the aforementioned landmarks, positive values designated a Class II relationship and negative appraisals meant Class III discrepancy.
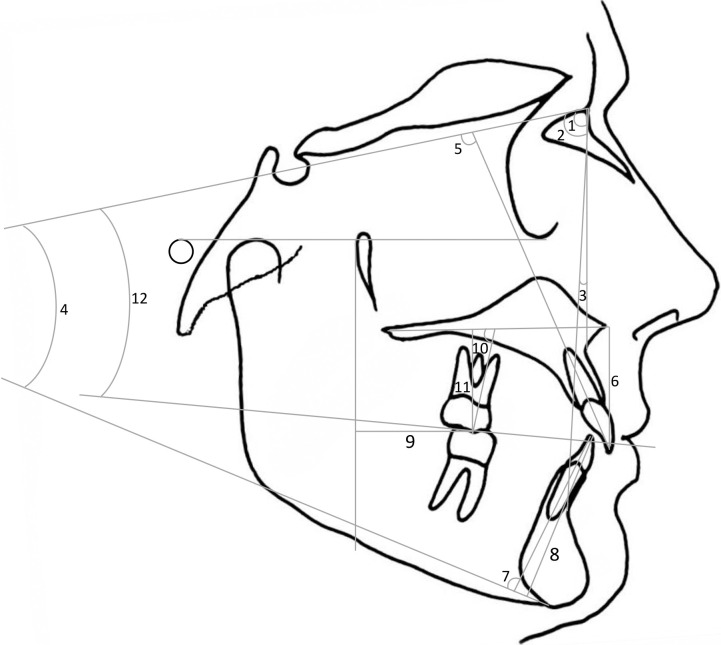
Figure 3.
Skeletal and dental cephalometric measurements: (1) SNA angle; (2) SNB angle; (3) ANB angle; (4) SN-GoGn angle; (5) U1-SN angle; (6) U1 vertical; (7) IMPA; (8) L1 vertical; (9) U6-horizontal; (10) U6-PP angle; (11) U6-vertical; (12) SN-occlusal plane angle.
Statistical Analysis
To determine interrater reliability, 20 randomly selected cephalograms were retraced and remeasured at 2-week intervals. According to the power analysis with 0.05 level and 80% power (based on a 1.32-mm standard deviation and a 1.5-mm detectable difference for midline correction),15 the needed minimum sample size was 12 for each group.
The normality test of Shapiro-Wilks and Levene's variance homogeneity test were applied to the data. The data was normally distributed, and there was homogeneity of variance among the groups. Thus, statistical evaluation of cephalometric values between groups was performed using parametric tests. The paired t-test was used for significance of mean changes in both groups. An independent t-test was performed for comparing initial measurements of the groups at T1 and comparing mean changes in both groups. The data were analyzed using SPSS software (version 16.0, SPSS Inc, Chicago, Ill). Statistical significance was set at P < .05.
RESULTS
Two patients were removed from the elastics groups due to poor cooperation on elastics wear. Also, after leveling and alignment, the Class II molar relationship turned into a Class I in one of the Forsus patients. These and the corresponding patients in the other group were excluded from the final analysis to maintain the 1:1 intergroup ratio. Thus, 28 patients were included in the final assessment. Intraclass correlation coefficients ranged from 0.936 to 0.981 for cephalometric measurements and from 0.976 to 0.992 for model measurements. Eleven female and three male patients with a mean age of 14.19 ± 1.02 years constituted the Forsus group, while the elastics group consisted of nine females and five males with a mean age of 13.75 ± 1.16 years.
The mean treatment lengths for Forsus and subsequent multibracket phase were 4.53 ± 0.91 months and 4.05 ± 0.43 months, respectively. While the mean treatment length with intermaxillary elastics was 6.85 ± 1.08 months, the subsequent multibracket phase took 4.32 ± 0.57 months. Duration of comprehensive treatment for the Forsus and elastics groups were 17.42 ± 0.85 months and 20.74 ± 1.01 months, respectively. The mean treatment time was significantly shorter with Forsus compared with elastics (P < .001). This was also true in comparing overall comprehensive treatments between groups. Pre-and posttreatment measurements are shown in Table 1. At T1, there were no statistically significant differences between the two groups for any of the variables, except for L1-MP (mm) and Occ-SN (P < .05); thus both groups were comparable in terms of malocclusion severity.
Table 1.
Means and Standard Deviations for the Cephalometric and Model Measurements
|
|
Forsus Group |
Elastics Group |
||
| T1 (Mean ± SD) |
T2 (Mean ± SD) |
T1 (Mean ± SD) |
T2 (Mean ± SD) |
|
| Cephalometric measurements | ||||
| SNA (°) | 78.25 ± 3.02 | 78.03 ± 2.98 | 79.81 ± 2.65 | 80.11 ± 2.74 |
| SNB (°) | 74.18 ± 2.63 | 74.71 ± 2.51 | 75.47 ± 2.84 | 75.89 ± 2.73 |
| ANB (°) | 4.07 ± 1.44 | 3.32 ± 1.38 | 4.34 ± 1.57 | 4.22 ± 1.49 |
| SN-GoGn (°) | 32.75 ± 3.59 | 32.94 ± 3.35 | 31.59 ± 3.88 | 32.51 ± 4.12 |
| U1-SN (°) | 106.49 ± 6.25 | 102.85 ± 5.17 | 108.58 ± 7.52 | 102.91 ± 6.22 |
| U1-PP (mm) | 29.85 ± 2.63 | 30.93 ± 2.55 | 30.15 ± 3.06 | 32.06 ± 2.81 |
| L1-MP (°) | 93.24 ± 7.22 | 98.41 ± 8.09 | 97.53 ± 6.62 | 101.81 ± 7.45 |
| L1-MP (mm) | 40.21 ± 2.63 | 39.72 ± 2.71 | 38.09 ± 1.45 | 38.67 ± 1.91 |
| U6-PTV (mm) | 14.75 ± 3.02 | 13.88 ± 3.45 | 15.00 ± 3.35 | 14.86 ± 3.51 |
| U6-PP (°) | 78.52 ± 4.77 | 76.23 ± 5.09 | 75.66 ± 5.01 | 73.69 ± 5.28 |
| U6-PP (mm) | 28.58 ± 3.87 | 29.01 ± 3.68 | 26.19 ± 4.04 | 26.58 ± 4.18 |
| Occ/SN (°) | 15.05 ± 2.85 | 16.05 ± 2.99 | 17.74 ± 3.04 | 19.62 ± 1.36 |
| Overjet | 5.72 ± 1.08 | 2.36 ± 0.83 | 4.51 ± 1.11 | 2.08 ± 0.88 |
| Overbite | 3.85 ± 0.97 | 1.63 ± 0.86 | 3.77 ± 0.88 | 2.31 ± 0.94 |
| Model measurements | ||||
| Molar relation (Cl II side) | 4.06 ± 1.04 | 0.94 ± 0.61 | 4.04 ± 1.02 | 1.84 ± 0.49 |
| Molar relation (Cl I side) | 0.09 ± 0.21 | −0.25 ± 0.36 | 0.15 ± 0.22 | −0.11 ± 0.29 |
| Midline deviation | 2.43 ± 0.96 | 0.29 ± 0.85 | 2.28 ± 1.04 | 0.55 ± 0.91 |
The significance of intragroup changes and intergroup differences are presented in Table 2. Both groups showed no statistically significant skeletal changes, except for the SN-GoGn angle in the elastics group, which exhibited a significant increase (P < .05). However, the difference in the SN-GoGn angle between the two groups was nonsignificant (P > .05). In both groups, palatal tipping and extrusion of the maxillary incisors—as well as clockwise rotation of the occlusal plane—were statistically significant, and these changes were greater in the elastics group (P < .05). Mandibular incisors were proclined in both groups (P < .001), but no significant difference was observed between groups (P > .05). Moreover, these teeth showed significant intrusion in the Forsus group and significant extrusion in the elastics group; the difference between the two groups for the L1-MP distance was significant (P < .05). Changes in overjet and overbite were statistically significant: the Forsus sample showed significantly greater improvement in overjet (P < .05).
Table 2.
Mean Changes in Each Group and Comparison Between Groups
|
|
Forsus Group |
Elastics Group |
Intergroup Difference | ||||
| Mean |
SD |
P
|
Mean |
SD |
P
|
P
|
|
| Cephalometric measurements | |||||||
| SNA (°) | −0.22 | 1.05 | .447 | 0.30 | 1.12 | .335 | .216 |
| SNB (°) | 0.53 | 0.93 | .053 | 0.42 | 0.88 | .097 | .750 |
| ANB (°) | −0.75 | 1.31 | .052 | −0.12 | 0.72 | .544 | .127 |
| SN-GoGn (°) | 0.19 | 1.03 | .502 | 0.92 | 1.17 | .011* | .092 |
| U1-SN (°) | −3.64 | 1.64 | <.001** | −5.67 | 1.96 | <.001** | .006* |
| U1-PP (mm) | 1.08 | 0.95 | .001* | 1.91 | 0.69 | <.001** | .014* |
| L1-MP (°) | 5.17 | 1.43 | <.001** | 4.28 | 1.21 | <.001** | .087 |
| L1-MP (mm) | −0.49 | 0.83 | .046* | 0.58 | 0.99 | .047* | .005* |
| U6-PTV (mm) | −0.87 | 1.77 | .089 | −0.14 | 1.82 | .778 | .292 |
| U6-PP (°) | −2.29 | 4.03 | .053 | −1.97 | 3.51 | .056 | .824 |
| U6-PP (mm) | 0.43 | 0.78 | .060 | 0.39 | 0.92 | .137 | .902 |
| Occ/SN (°) | 1.00 | 0.96 | .002* | 1.88 | 1.21 | <.001** | .043* |
| Overjet | −3.36 | 1.02 | <.001** | −2.43 | 0.96 | <.001** | .020* |
| Overbite | −2.22 | 0.45 | <.001** | −1.76 | 0.78 | <.001** | .067 |
| Model measurements | |||||||
| Molar relation (Cl II side) | −3.12 | 0.72 | <.001** | −2.20 | 1.01 | <.001** | .01* |
| Molar relation (Cl I side) | −0.34 | 0.69 | .088 | −0.26 | 0.50 | .074 | .728 |
| Midline deviation | −2.14 | 0.41 | <.001** | −1.73 | 0.55 | <.001** | .034* |
P < .05; ** P < .001.
In both groups, the midline deviation was decreased, and there were significant changes in molar relationship on the Class II side (P < .001). Improvements in the aforementioned parameters were greater in the Forsus group (P < .05). The molar relationship on the Class II side was corrected toward Class I, while the Class I side exhibited a nonsignificant change toward a Class III molar relationship. After treatment, a Class I molar relationship was seen in 12 (85%) and 10 (71%) of the subjects in the Forsus and elastics groups, respectively.
DISCUSSION
There is only one study in the literature reporting the statistical outcome of functional treatment of Class II subdivision malocclusion.15 In that study, Bock et al.15 retrospectively evaluated the effectiveness of Class II subdivision Herbst treatment by means of study models. On the other hand, Cassidy et al.18 compared the treatment results of groups classified according to midline relationships, in terms of overall occlusal outcomes, and incisor inclinations. However, it was difficult to draw a strong conclusion about any treatment method in that study because a variety of treatment strategies, including headgear, elastics, fixed functional appliances, and surgical intervention, were used in each group. In addition, many patients received a combination of these treatment approaches.18 The present study is the first to compare therapeutic changes induced by Forsus with those brought about by intermaxillary elastics in Class II subdivision treatment, while Jones et al.20 compared the same treatment modalities in patients who had bilateral Class II molar relationship. Therefore, direct comparison with results from previous studies was not possible.
Although intermaxillary elastic usage is the most common method of correcting Class II subdivision, the major drawback with elastics is the intense need of patient compliance, which was also true for the current study. This feature was reflected as a longer treatment duration in the elastics group compared with the treatment using Forsus, which required less patient cooperation. Although it has been reported that unexpected breakages can occur with Forsus,14 it was relatively well accepted by our patients with some initial discomfort, and no breakage occurred.
Extrusion and palatal tipping of the maxillary incisors and clockwise rotation of the occlusal plane were significantly greater in the elastics group than in the Forsus group. Also, there was a significant extrusion of mandibular incisors and clockwise rotation of the mandible in the elastics group. These findings can be explained by the vertical component of elastics attachment points, as reported previously.21,22 In the Forsus group, the mandibular incisors were intruded, a finding that agreed with previous studies.23–27 A main expected effect, protrusion of mandibular incisors, took place in both groups, but in similar amounts. This result was not in accordance with the Cassidy et al18 report. The authors explained that the mandibular incisors were proclined more when fixed functional appliances were used, compared with elastics only.18 However, this was not supported with statistical data. Considering that treatment length influences the L1-MP angle in the compliance-free Class II correction protocol,23 our finding that Forsus did not appear to create greater incisor proclination may be associated with the shorter treatment time in the Forsus group.
In both groups, no significant change was observed related to the maxillary molars, which is a finding that agrees with the Jones et al.20 study, reporting nonsignificant positional changes of these teeth at the end of comprehensive treatment. This could be attributed to the relapse that occurred in the detailing phase of treatment that can negate the distalization or distal tipping effects of Forsus and elastics on the maxillary molars. This pattern could also hold true for vertical movement of the maxillary molars, which could have been intruded with Forsus and then rebounded after spring removal, as reported previously.26
In both treatment protocols, improvement in overjet, mandibular midline deviation, and molar relationship were induced mainly by dentoalveolar changes without any statistically significant skeletal modifications, the lack of which could have been due to the intercuspation of teeth on the Class I side. This, in turn, might have impaired the horizontal force vectors that encourage mandibular advancement. Additionally, a probable reason that applies especially to the Forsus group can be the short term application (on average, 4.5 months) of the Forsus device.
Previous studies have revealed that ideal correction of molar relationship and midline deviation is challenging and often not achieved.13,15,18 During Herbst treatment of Class II subdivision, nearly all subjects were treated to an overcorrected Class I or Class III molar relationship, whereas after subsequent multibracket treatment, bilateral Class I or a super Class I molar relationship was seen in 72% of the subjects and a mean midline deviation of 0.4 mm was noted.15 Also, Cassidy et al.18 found that in 70% of the patients, treatment was finished within 1 mm of the Class I target. According to our finding, improvements in molar relationship and mandibular midline deviation in both groups was a result of the anterior movement of the mandibular dentition as a unit, especially on the Class II side. Furthermore, the decrease in overjet was associated with significant retroclination of the maxillary incisors and proclination of the mandibular incisors. While a Class I molar relationship was the treatment goal for both groups, after debonding, a slight relapse occurred in the corrected molar relationship, midline deviation, and overjet. However, it appeared that fixed appliance treatment with Forsus has shown less relapse in terms of the aforementioned parameters, compared with using intermaxillary elastics. Thus after treatment, the ratio of patients who exhibited Class I molar relationship in the Forsus group (85%) was greater than both the percentage of patients with Class I molar relationship in the elastics group (71%) and the success ratio reported in previous studies.15,18 On the other hand, it should be noted that the significant intergroup differences detected cannot be regarded as clinically meaningful because of their small magnitude. Also, when considered in terms of smile esthetics, a midline correction difference of 0.4 mm between the methods used herein seems trivial when we consider that midline shifts of 1 mm is the dissonance limit that is well tolerated.28
CONCLUSIONS
Class II subdivision treatment using Forsus was more successful than elastics in terms of correcting the unilateral Class II molar relationship, overjet, and mandibular midline deviation.
Forsus is a valuable option for the correction of Class II subdivision malocclusion, providing a shorter treatment period, requiring minimal patient compliance compared with intermaxillary elastics, while Class II subdivision treatment using elastics presents the most affordable modality.
REFERENCES
- 1.Alavi DG, BeGole EA, Schneider BJ. Facial and dental arch asymmetries in Class II subdivision malocclusion. Am J Orthod Dentofacial Orthop. 1988;93:38–46. doi: 10.1016/0889-5406(88)90191-6. [DOI] [PubMed] [Google Scholar]
- 2.Rose MR, Sadowsky C, BeGole EA, Moles R. Mandibular skeletal and dental asymmetry in Class II subdivision malocclusion. Am J Orthod Dentofacial Orthop. 1994;105:489–495. doi: 10.1016/S0889-5406(94)70010-9. [DOI] [PubMed] [Google Scholar]
- 3.Janson GRP, Metaxas A, Woodside DG, de Freitas MR, Pinzan A. Three-dimensional evaluation of skeletal and dental asymmetries in Class II subdivision malocclusions. Am J Orthod Dentofacial Orthop. 2001;119:406–418. doi: 10.1067/mod.2001.113267. [DOI] [PubMed] [Google Scholar]
- 4.Azevedo ARP, Janson G, Henriques JFC, de Freitas MR. Evaluation of asymmetries between subjects with Class II subdivision and apparent facial asymmetry and those with normal occlusion. Am J Orthod Dentofacial Orthop. 2006;129:376–383. doi: 10.1016/j.ajodo.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Janson G, de Lima KJRS, Woodside DG, Metaxas A, de Freitas MR, Henriques JFC. Class II subdivision malocclusion types and evaluation of their asymmetries. Am J Orthod Dentofacial Orthop. 2007;131:57–66. doi: 10.1016/j.ajodo.2005.02.031. [DOI] [PubMed] [Google Scholar]
- 6.Kurt G, Uysal T, Sisman Y, Ramoglu SI. Mandibular asymmetry in Class II subdivision malocclusion. Angle Orthod. 2008;78:32–37. doi: 10.2319/021507-73.1. [DOI] [PubMed] [Google Scholar]
- 7.Sanders DA, Rigali PH, Neace WP, Uribe F, Nanda R. Skeletal and dental asymmetries in Angle Class II subdivision malocclusion using cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2010;138:542.e1–e20. doi: 10.1016/j.ajodo.2010.02.027. [DOI] [PubMed] [Google Scholar]
- 8.Minich CM, Araújo EA, Behrents RG, Buschang PH, Tanaka OM, Kim KB. Evaluation of skeletal and dental asymmetries in Angle Class II subdivision malocclusion with cone-beam computed tomography. Am J Orthod Dentofacial Orthop. 2013;144:57–66. doi: 10.1016/j.ajodo.2013.02.026. [DOI] [PubMed] [Google Scholar]
- 9.Li J, He Y, Wang Y, et al. Dental, skeletal asymmetries and functional characteristics in Class II subdivision malocclusions. J Oral Rehabil. 2015;42:588–599. doi: 10.1111/joor.12303. [DOI] [PubMed] [Google Scholar]
- 10.Shroff B, Lindauer SJ, Burstone CJ. Class II subdivision treatment with tip-back moments. Eur J Orthod. 1997;19:93–101. doi: 10.1093/ejo/19.1.93. [DOI] [PubMed] [Google Scholar]
- 11.Wertz RA. Diagnosis and treatment planning of unilateral Class II malocclusions. Angle Orthod. 1975;45:85–94. doi: 10.1043/0003-3219(1975)045<0085:DATPOU>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 12.Burstone CJ. Diagnosis and treatment planning of patients with asymmetries. Semin Orthod. 1998;4:153–164. doi: 10.1016/s1073-8746(98)80017-0. [DOI] [PubMed] [Google Scholar]
- 13.Smith SS, Alexander RG. Orthodontic correction of a Class II Division 1 subdivision right open bite malocclusion in an adolescent patient with a cervical pull face-bow headgear. Am J Orthod Dentofacial Orthop. 1999;116:60–65. doi: 10.1016/s0889-5406(99)70303-3. [DOI] [PubMed] [Google Scholar]
- 14.Ross AP, Gaffey BJ, Quick AN. Breakages using a unilateral fixed functional appliance: a case report using the Forsus TM Fatigue Resistant Device. J Orthod. 2007;34:2–5. doi: 10.1179/146531207225021852. [DOI] [PubMed] [Google Scholar]
- 15.Bock NC, Reiser B, Ruf S. Class II subdivision treatment with Herbst appliance. Angle Orthod. 2013;83:327–333. doi: 10.2319/052912-449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Janson G, Dainesi EA, Henriques JFC, de Freitas MR, de Lima KJ. Class II subdivision treatment success rate with symmetric and asymmetric extraction protocols. Am J Orthod Dentofacial Orthop. 2003;124:257–264. doi: 10.1016/s0889-5406(03)00406-2. [DOI] [PubMed] [Google Scholar]
- 17.Janson M, Janson G, Sant'Ana E, Simao TM, de Freitas MR. An orthodontic-surgical approach to Class II subdivision malocclusion treatment. J Appl Oral Sci. 2009;17:266–273. doi: 10.1590/S1678-77572009000300026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cassidy SE, Jackson SR, Turpin DL, Ramsay DS, Spiekerman C, Huang GJ. Classification and treatment of Class II subdivision malocclusions. Am J Orthod Dentofacial Orthop. 2014;145:443–451. doi: 10.1016/j.ajodo.2013.12.017. [DOI] [PubMed] [Google Scholar]
- 19.Torgerson DJ, Torgerson CJ. Designing Randomised Trials in Health, Education and the Social Sciences. New York: Palgrave MacMillan;; 2008. [Google Scholar]
- 20.Jones G, Buschang PH, Kim KB, Oliver DR. Class II non-extraction patients treated with the Forsus Fatigue Resistant Device versus intermaxillary elastics. Angle Orthod. 2008;78:332–338. doi: 10.2319/030607-115.1. [DOI] [PubMed] [Google Scholar]
- 21.Proffit WR, Fields HW. Contemporary Orthodontics. St. Louis: Mosby;; 2000. [Google Scholar]
- 22.Nelson B, Hansen K, Hägg U. Class II correction in patients treated with Class II elastics and with fixed functional appliances: a comparative study. Am J Orthod Dentofacial Orthop. 2000;118:142–149. doi: 10.1067/mod.2000.104489. [DOI] [PubMed] [Google Scholar]
- 23.Miller RA, Tieu L, Flores-Mir C. Incisor inclination changes produced by two compliance-free Class II correction protocols for the treatment of mild to moderate Class II malocclusions. Angle Orthod. 2013;83:431–436. doi: 10.2319/062712-528.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aras A, Ada E, Saracoglu H, Gezer NS, Aras I. Comparison of treatments with the Forsus Fatigue Resistant Device in relation to skeletal maturity: a cephalometric and magnetic resonance imaging study. Am J Orthod Dentofacial Orthop. 2011;140:616–625. doi: 10.1016/j.ajodo.2010.12.018. [DOI] [PubMed] [Google Scholar]
- 25.Franchi L, Alvetro L, Giuntini V, Masucci C, Defraia E, Bacetti T. Effectiveness of comprehensive fixed appliance treatment used with the Forsus Fatigue Resistant Device in Class II patients. Angle Orthod. 2011;81:678–683. doi: 10.2319/102710-629.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cacciatore G, Alvetro L, Defraia E, Ghislanzoni LTH, Franchi L. Active-treatment effects of the Forsus fatigue resistant device during comprehensive Class II correction in growing patients. Korean J Orthod. 2014;44:136–142. doi: 10.4041/kjod.2014.44.3.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cacciatore G, Ghislanzoni LTH, Alvetro L, Giuntini V, Franchi L. Treatment and posttreatment effects induced by the Forsus appliance: a controlled clinical study. Angle Orthod. 2014;84:1010–1017. doi: 10.2319/112613-867.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pinho S, Ciriaco C, Faber J, Lenza MA. Impact of dental asymmetries on the perception of smile esthetics. Am J Orthod Dentofacial Orthop. 2007;132:748–753. doi: 10.1016/j.ajodo.2006.01.039. [DOI] [PubMed] [Google Scholar]