Abstract
Objective:
To evaluate the precision and reproducibility of a protocol to perform rapid voxel-based superimposition of the mandible in growing patients using CBCT.
Materials and Methods:
The sample comprised two cone-beam computed tomography scans taken at least 1 year apart from each of 24 growing patients. Voxel-based superimposition was performed by two examiners independently. The internal part of the symphysis extending to the first molar was used as the reference. The superimposition process took approximately 5 minutes. Once the mandibles were superimposed, surface models were created and root mean square (RMS) changes were obtained by means of iterative closest point. To evaluate precision, differences in three areas were measured between time point 1 (T1) and time point 2 (T2) superimposed. To evaluate reproducibility between different examiners, the distances between T2 superimposed by each operator were measured in five different areas. Descriptive statistics were used to evaluate the precision of the superimposition and the interexaminer reproducibility measurements for each case were reported individually.
Results:
The superimposition mean error between T1 and T2 for the right and left sides of the mandible and chin were 0.23 mm, 0.25 mm, and 0.33 mm, respectively. Interexaminer reproducibility error was ≤0.3 mm in 20 of 24 cases for measurements near the registration area. In the ramus area, two cases had errors >1 mm (1 mm–1.3 mm).
Conclusion:
The rapid superimposition was precise for assessing dentoalveolar changes and structures close to the registration area. However, evaluation of the condyles and ramus area had limitations and needs improvement.
Keywords: Cone-beam CT, Three-dimensional image, CBCT superimposition, 3D image registration
INTRODUCTION
Facial growth has been extensively studied since the development of the cephalostat using cephalometric tracing techniques and superimposition.1,2 Tracings performed at two different time points can be superimposed to assess the changes. Depending on which structures are used for superimposition, different features of growth can be studied. For example, superimposition on the cranial base demonstrates overall facial growth. It is also of interest to study growth of the mandible individually by superimposing sequential images of the mandible. Options for superimposition are “best fit” or the mandibular symphysis to assess mandibular growth.3 However, lateral cephalometry has several limitations including 2D appreciation of a 3D structure, magnification, overlapping of osseous structures, patient positioning errors, and errors related to tracing.4–6
The introduction of cone-beam computed tomography (CBCT)7 has had great impact on the imaging field. CBCT allows a three-dimensional (3D) appreciation of the subject without the overlapping of different structures or magnification. Positional errors in CBCT can also be corrected by adjusting the head orientation digitally after the scan has been taken. The challenge that arose with this new technology was being able to superimpose CBCT scans from different time points. Three main techniques have been used: (1) landmark-based, (2) surface-based, and (3) voxel-based. The latter technique is considered the best one as it does not rely on landmark identification or creation of a surface model by the segmentation process as needed in the two other superimposition methods.8 In voxel-base superimposition, the intensity of the voxels of two different CBCT images are read, compared, and matched. One image retains the same orientation while the other moves to match the first image. This method was first described in dentistry by Cevidanes et al.9,10 for nongrowing and growing patients. More recently, a faster method for voxel-based superimposition of the cranial base was introduced by Mah and Cho11 and validated by Weissheimer et al.12 For these cases, the cranial base (nongrowing) or anterior cranial base (growing) were used as references. The result of this type of superimposition demonstrates overall facial changes after therapy or growth. This technique is similar to the sella-nasion superimposition used with 2D images.
Mandibular regional superimposition is very important to assess local changes and bone remodeling. This could be used to evaluate skeletal, alveolar, and dental changes that occur due to growth or from treatment. The literature is limited on the topic of 3D mandibular superimposition. Only one study has been published assessing the quality of superimposition for both nongrowing13 and growing14 patients. Therefore, this research aimed to test the precision and reproducibility of a rapid protocol to perform a voxel-based superimposition of the mandible in growing patients using CBCT.
MATERIALS AND METHODS
This study was approved by the Institutional Review Board of Virginia Commonwealth University No. HM20006211. Two CBCT scans from each of 24 growing patients that were taken at least 1 year apart (T1 to T2 average time = 16.0 ± 2.9 months), were used for this retrospective study (Table 1). The CBCT scans were obtained using an i-CAT scanner (Imaging Sciences International, Hatfield, Pa) set at 120 kVp, 8 mA, large field of view, scan time of 40 seconds, and 0.3-mm voxel size. The images were reconstructed with 0.3-mm slice thickness and exported as digital imaging and communications in medicine (DICOM) files. The sample was obtained from the database of the Department of Orthodontics of Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil. They were originally used to assess the effects of rapid palatal expansion.
Table 1.
Demographics of the Population
|
|
Descriptive Statistics |
|||
| Minimum |
Maximum |
Mean |
Standard Deviation |
|
| Age | 7.4 | 13.8 | 10.8 | 1.7 |
| Interval between CBCTs | 13 | 27 | 16.0 | 2.9 |
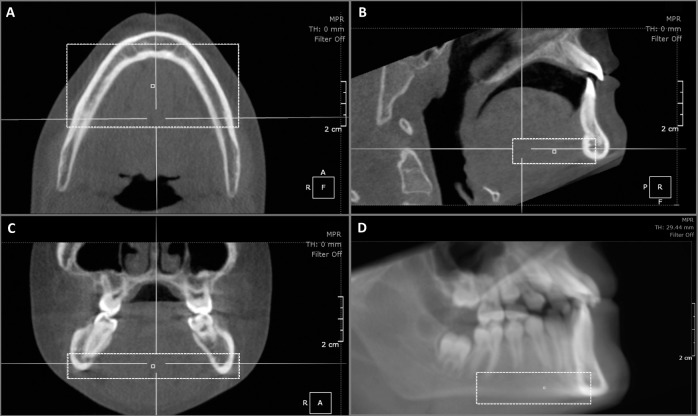
The DICOM files were imported and organized into the OnDemand 3D software program data base (Cybermed v1.0.10.5261, Seoul, Korea). First, T1 and T2 CBCT images were cropped to include all of the mandible but not the cranial base. The T1 image was then reoriented with the base of the mandible parallel to the floor (Figure 1). Two calibrated examiners then performed the regional superimposition independently. T1 and T2 CBCT images were opened using the Fusion tab found within the software. This module allowed each examiner to manually move the T2 CBCT as close as possible to the T1 CBCT position and also allowed the examiner to do an automatic, voxel-based superimposition. At first, an automated superimposition was done without defining any specific area of interest and T2 CBCT with a new orientation was exported. After that, a second superimposition was done using an area encompassing from the internal part of the symphysis to the distal aspect of the first molars at the level of basal bone as a reference for mandibular registration (Figure 2). The T2 superimposed (T2S) with the final orientation was saved. The second calibrated operator performed the same steps, and the differences were used to assess the reliability of the superimposition technique between examiners. Each examiner superimposition process took approximately 5 minutes.
Figure 1.
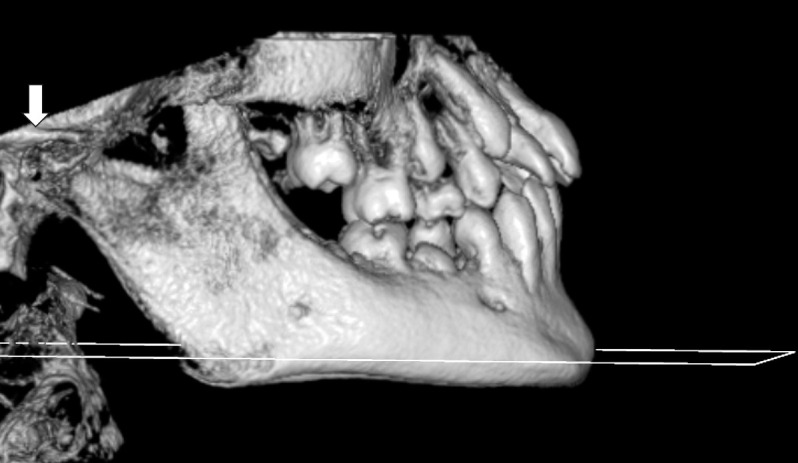
Orientation of the CBCT scan with the lower mandible border parallel to the floor. Arrow shows that the condyles were included in the crop.
Figure 2.
Area used to refine the superimposition (box). Reconstruction of the CBCT scan in axial (A), sagittal (B) and coronal (C) views of the mandible. The limits were: posterior limit – distal of the first molar, anterior limit – middle of the mandibular symphysis, inferior limit – including all the lower border of the mandible, superior limit – apical third of the roots, lateral limits – including all the external cortical area of the mandible (D).
After both examiners superimposed the CBCT scans, the three images (T1 and T2 superimposed by examiner 1 and T2 superimposed by examiner 2) were segmented using the 3D Picker tool inside the 3D module. All the segmentations were standardized at 554–555 grey levels and exported as .stl (Standard Tessellation Language) files using the software parameters of 0.005 and a smooth of 1.
One examiner imported all three STL files into VAM software (Canfield Scientific, Fairfield, NJ) and measured the distances between the surfaces with an iterative closest point technique. This technique measured the smallest distance between two surfaces, providing the root mean square (RMS) of the changes.
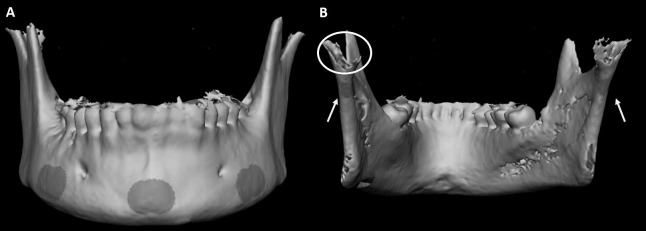
The study aimed to measure areas that are less likely to change and not highly influenced by alveolar changes or growth. To evaluate precision of the method, three areas (the basal bone at the mandibular symphysis and areas distal to the mental foramina on each side) were measured between T1 and T2 superimposed from one of the examiners (Figure 3A). These areas were named chin, left mandible, and right mandible. There were no distances between specific landmarks measured with this technique. Instead, the VAM software established the closest distance of the selected area in the T2 model from the T1 model and provided one RMS distance for the whole measured surface that was used for the statistical report. To evaluate precision and reproducibility between different examiners, the distances between T2 superimposed by each operator were measured. A mean value of 0 would be considered ideal. In addition to the three areas, measurements were done in the posterior part of the ramus on the left and right sides (Figure 3B). The measurements were repeated for 10 cases by the same operator after 1 month to test intraexaminer reproducibility. The results were exported to an Excel spreadsheet. Figure 4 shows a flowchart with the steps.
Figure 3.
Areas used for measurement. A – left mandible, chin and right mandible. B – Arrows pointing to the left and right posterior mandible. Circle showing the lack of quality in the condylar segmentation.
Figure 4.
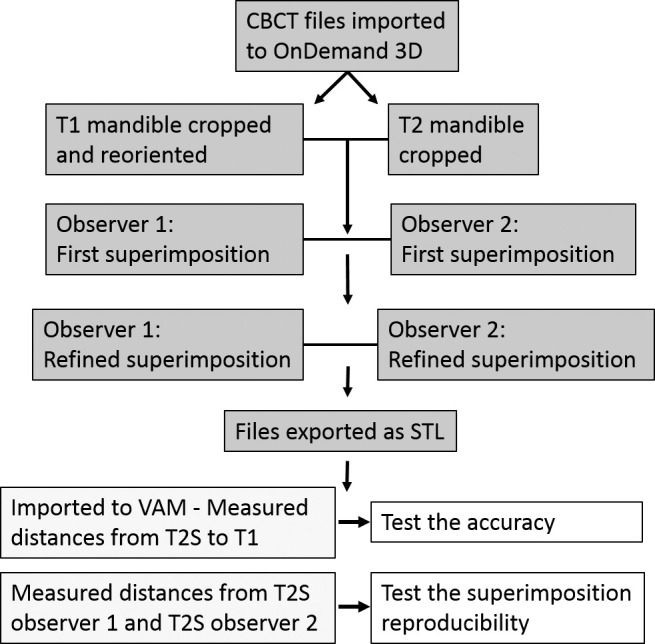
Flowchart of the method.
Statistical analyses were done using SPSS 22.0 (IBM Corp, Armonk, NY). Intraexaminer agreement for the measurements was assessed by means of intraclass correlation coefficients (ICCs). Descriptive statistics were used to evaluate the precision of the superimpositions. Measurements for interexaminer reproducibility for each of the 24 cases are shown individually.
RESULTS
Table 2 shows the ICC results for intraexaminer agreement of the measurements. All the results were higher than 0.95. The precision of the mandibular superimposition method is shown in Table 3. Descriptive statistics for measurements made between T2S and T1 for the 24 cases show that the overall superimposition mean error for the chin and left and right sides of the mandible were 0.23 mm, 0.25 mm, and 0.33 mm, respectively. None of the cases had an error greater than 0.85 mm.
Table 2.
Intraclass Correlation Coefficients and Confidence Interval for Repeated Measurements of 10 Patients
|
|
Intraclass Correlation |
95% Confidence Interval |
| Right mandible | 0.97 | 0.89–0.99 |
| Chin | 0.95 | 0.81–0.99 |
| Left mandible | 0.97 | 0.88–0.99 |
| Right ramus | 0.98 | 0.93–1.00 |
| Left ramus | 0.97 | 0.88–0.99 |
Table 3.
Descriptive Values for Differences Between Superimposition of T2 and T1 (mm)
|
|
Descriptive Statistics |
|||
| Minimum |
Maximum |
Mean |
Standard Deviation |
|
| Right mandible | 0.05 | 0.68 | 0.23 | 0.18 |
| Chin | 0.12 | 0.85 | 0.33 | 0.18 |
| Left mandible | 0.06 | 0.81 | 0.25 | 0.18 |
Table 4 shows a case-by-case analysis of interexaminer reproducibility. Twenty of the 24 cases had reproducibility errors ≤0.3 mm (voxel-size) for measurements at the chin and left and right sides of the mandible.
Table 4.
Case-by-case Analysis Showing Reproducibility of the Superimposition (mm)
| Case |
Right Mandible |
Chin |
Left Mandible |
Right Ramus |
Left Ramus |
| 01 | 0.30 | 0.23 | 0.69 | 1.06 | 0.50 |
| 02 | 0.09 | 0.19 | 0.07 | 0.74 | 0.81 |
| 03 | 0.16 | 0.23 | 0.21 | 0.16 | 0.28 |
| 04 | 0.11 | 0.04 | 0.05 | 0.43 | 0.37 |
| 05 | 0.20 | 0.15 | 0.14 | 0.63 | 0.60 |
| 06 | 0.08 | 0.12 | 0.03 | 0.23 | 0.24 |
| 07 | 0.13 | 0.12 | 0.03 | 1.18 | 1.30 |
| 08 | 0.02 | 0.03 | 0.02 | 0.02 | 0.03 |
| 09 | 0.08 | 0.03 | 0.04 | 0.35 | 0.56 |
| 10 | 0.14 | 0.11 | 0.08 | 0.29 | 0.05 |
| 11 | 0.04 | 0.06 | 0.13 | 0.13 | 0.20 |
| 12 | 0.22 | 0.44 | 0.13 | 0.68 | 0.56 |
| 13 | 0.05 | 0.07 | 0.02 | 0.51 | 0.93 |
| 14 | 0.24 | 0.17 | 0.03 | 0.28 | 0.20 |
| 15 | 0.15 | 0.23 | 0.15 | 0.25 | 0.52 |
| 16 | 0.06 | 0.21 | 0.19 | 0.33 | 0.38 |
| 17 | 0.03 | 0.10 | 0.05 | 0.14 | 0.09 |
| 18 | 0.41 | 0.26 | 0.46 | 0.11 | 0.91 |
| 19 | 0.04 | 0.21 | 0.20 | 0.33 | 0.08 |
| 20 | 0.03 | 0.10 | 0.17 | 0.37 | 0.32 |
| 21 | 0.11 | 0.29 | 0.36 | 0.48 | 0.61 |
| 22 | 0.50 | 0.30 | 0.10 | 0.54 | 0.56 |
| 23 | 0.19 | 0.13 | 0.20 | 0.29 | 0.14 |
| 24 | 0.06 | 0.02 | 0.03 | 0.24 | 0.07 |
DISCUSSION
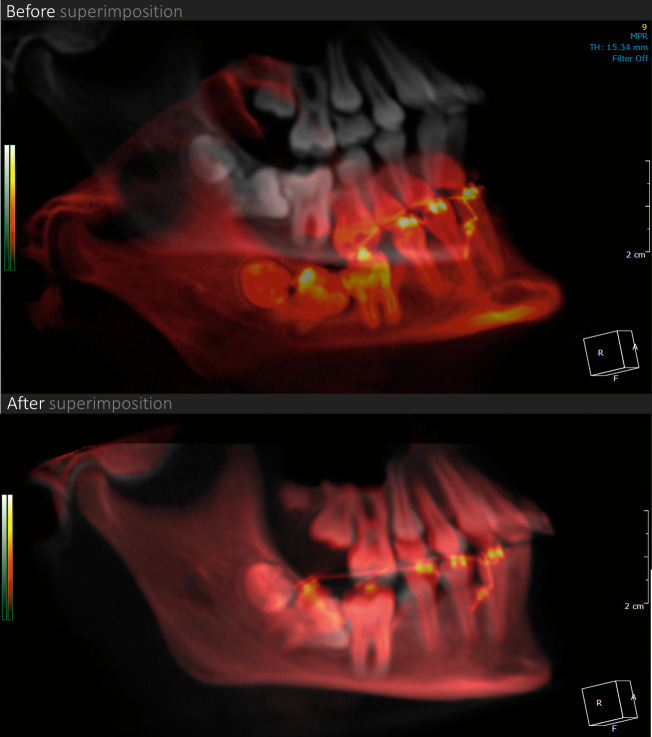
This study presented a voxel-based mandibular superimposition method for growing patients. Koerich et al.13 validated the same technique for mandibular superimposition for nongrowing patients. They evaluated 15 subjects, and the results were reported in RMS with the mean error being approximately 0.10 mm. Interexaminer reliability for 10 out of 15 cases had ideal reproducibility (mean displacement was 0) while the other 5 cases had differences <0.03 mm. In the current study, the mean error for precision was smaller than 0.33 mm, with variation at the chin up to 0.88 mm. This could be explained by the remodeling that occurs in that area, thereby contributing to the higher difference compared with nongrowing patients. The interexaminer reproducibility error was also higher than for the nongrowing patients. Most of the cases (20 out of 24) had reproducibility errors ≤0.3 mm for measurements near the registration area. However, two cases (1 and 7) had errors up to 1.3 mm in the ramus region. Ruellas et al.14 found that condyle errors were <1.94 mm for most of their cases. In the current study, the best results were found for structures near the registration area, suggesting that the method is reliable for evaluating dentoalveolar changes (Figure 5). On the other hand, it has limitations for assessment of growth or treatment changes in the condyles and the ramus.
Figure 5.
Example of mandibular regional superimposition. Pretreatment CBCT (grey) and treatment progress CBCT (red) superimposed to show the effects of orthodontic treatment in a 13-year-old patient with two molars retained and impacted.
Surface-based superimposition could be an alternative to the method used in this study. As mentioned before, voxel-based techniques read the intensity of the voxels and apply the changes to each of the CBCT slices. On the other hand, surface-based techniques try to match the models created from the DICOM files. This match is based on the principle of closest distance between structures.8 Ahmad et al.15 used surface-based superimposition of the mandible in nongrowing patients to assess mandibular alveolar resorption. That study, however, did not present data to support whether the superimposition method was accurate or reproducible. Surface-based techniques also have limitations. They can be used to assess superficial changes but do not allow for evaluation of internal structures such as tooth roots, the mandibular canal, and bone thickness directly in the multiplanar slice-views. They require extra time for segmentation of the structures. Also, the segmentation process can be affected by beam-hardening artifacts16 such as gutta-percha, braces, temporary anchorage devices, and skeletal anchorage systems. Surface-based techniques require creating an additional file and an extra step in the superimposition process.8 Usually, voxel-based techniques are easier and faster to process. However, for this particular case of mandibular superimposition in growing patients, future studies could address the reproducibility of the surface-based technique.
To perform mandibular superimposition in nongrowing patients, Koerich et al.13 moved the T2 mandible close to T1 and proceeded with the automatic registration provided by the software. The process took 10–15 seconds. In the present study, that same technique did not work well. Extra steps were required to ensure the best outcome, and the time to process the superimpositions was approximately 5 minutes when done by experienced examiners. After initial alignment, use of the Region of Interest tool provided by the software was required. This tool delineates a chosen area of the CBCT and, instead of using all the voxels from the image equally for the registration, priority is given to the voxels inside the selected region of interest.
To select the appropriate technique before starting the study, several methods were tested including (1) not selecting any region of interest, (2) selecting the external and internal part of the symphysis, (3) selecting the internal part of the symphysis only, and (4) selecting the internal part of the symphysis extended to the first molar area (Figure 2). Selection of the symphysis was derived from Bjork's17 study wherein he stated that the internal part of the symphysis was stable during growth. However, the results in 3D were very poor using this method. Bjork17 also stated that the mandibular canal and the lower border of the developing molar germs also could be considered stable structures to be used for superimposition. Those options were not tested in the current study because the software does not allow two independent areas to be used as a reference simultaneously. In addition, according to Pluim et al.18 and Ruellas et al.,14 the voxel-based technique has problems matching voxels from very small areas, such as the mandibular canal and molar germs. The fourth method, using the internal part of the symphysis extended to the first molar area, showed better preliminary results. In other words, the method used was a mandibular superimposition using part of the mandibular basal area and chin as references. This would explain the superior results found in the chin and lateral areas of the mandible compared with the posterior area.
Some of the limitations of this study were the age of the sample and the time interval between T1 and T2. There was a wide range of ages between 7.4 to 13.8 years at the time of the first scan. Also, it was not possible to confirm whether this technique would work if the scans were taken more than 3 years apart or that perfect 3D mandibular superimposition is even feasible for growing patients. Another limitation was the way measurements were done. The iterative closest point tends to underestimate overall changes.19 On the other hand, if a landmark technique were used for measurements, the error of placing the landmarks would also exist.20
Measurements in the posterior area of the mandible were made because, although changes in the chin were noted to be small, the effect in a distant area such as the condyles could be greater. Ideally, measurements done in the posterior part of the ramus should be done on the posterosuperior area of the condyle. By doing that, measurements would be done in the two extremes of the mandible (anterior part of the chin and posterior part of the condyle). However, the automated segmentation process does not allow for perfect segmentation of the condyles (Figure 3B). Therefore, the closest area that could be automatically segmented was chosen. Segmentation of the condyles would require manual steps, and this could add error to the study. Measurements in the posterior area of the mandible were not done between T2 superimposed to T1 because of the extensive growth that would be expected there.
Superimposition done in 3D is much more challenging than in 2D. A lot more information is provided by CBCT and, consequently, it is easier to recognize error. When T2 is moved to match T1, small rotations and translations in three different planes of space can affect the accuracy of the final superimposition. The magnitude of the error tends to increase as the distance from the reference area (chin) increases. The difficulty in superimposing 3D images for growing patients suggests that previous work done in 2D is likely to have been oversimplified and may not be appropriate as the standard.
CONCLUSION
The method of mandibular superimposition in 3D for growing subjects was not time-consuming and was considered precise for assessing dentoalveolar changes and structures close to the registration area.
ACKNOWLEDGMENT
The authors thank Cybermed Inc. for providing the software for this research. This study was supported by the A. D. Williams Funds (award number UL1RR031990) from the National Center for Research Resources and NIH Roadmap for Medical Research, National Institutes of Health.
REFERENCES
- 1.Björk A, Skieller V. Normal and abnormal growth of the mandible. A synthesis of longitudinal cephalometric implant studies over a period of 25 years. Eur J Orthod. 1983;5:1–46. doi: 10.1093/ejo/5.1.1. [DOI] [PubMed] [Google Scholar]
- 2.Björk A, Skieller V. Facial development and tooth eruption: An implant study at the age of puberty. Am J Orthod. 1972;62:339–383. doi: 10.1016/s0002-9416(72)90277-1. [DOI] [PubMed] [Google Scholar]
- 3.Gu Y, McNamara JA., Jr Cephalometric superimpositions. Angle Orthod. 2008;78:967–976. doi: 10.2319/070107-301.1. [DOI] [PubMed] [Google Scholar]
- 4.de Paula LK, Solon-de-Mello PdA, Mattos CT, Ruellas AC, Sant'Anna EF. Influence of magnification and superimposition of structures on cephalometric diagnosis. Dental Press J Orthod. 2015;20(2):29–34. doi: 10.1590/2176-9451.20.2.029-034.oar. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Baumrind S, Frantz RC. The reliability of head film measurements: 1. Landmark identification. Am J Orthod. 1971;60:111–127. doi: 10.1016/0002-9416(71)90028-5. [DOI] [PubMed] [Google Scholar]
- 6.Baumrind S, Frantz RC. The reliability of head film measurements: 2. Conventional angular and linear measures. Am J Orthod. 1971;60:505–517. doi: 10.1016/0002-9416(71)90116-3. [DOI] [PubMed] [Google Scholar]
- 7.Mozzo P, Procacci C, Tacconi A, Martini PT, Andreis IA. A new volumetric CT machine for dental imaging based on the cone-beam technique: preliminary results. Eur Radiol. 1998;8:1558–1564. doi: 10.1007/s003300050586. [DOI] [PubMed] [Google Scholar]
- 8.Almukhtar A, Ju X, Khambay B, McDonald J, Ayoub A. Comparison of the accuracy of voxel-based registration and surface based registration for 3D assessment of surgical change following orthognathic surgery. PLoS One. 2014;9(4):e93402. doi: 10.1371/journal.pone.0093402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cevidanes LHS, Bailey LJ, Tucker GR, et al. Superimposition of 3D cone-beam CT models of orthognathic surgery patients. Dentomaxillofac Radiol. 2005;34:369–375. doi: 10.1259/dmfr/17102411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cevidanes LH, Heymann G, Cornelis MA, DeClerck HJ, Tulloch JFC. Superimposition of 3-dimensional cone-beam computed tomography models of growing patients. Am J Orthod Dentofacial Orthop. 2009;136:94–99. doi: 10.1016/j.ajodo.2009.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi J, Mah J. A new method for superimposition of CBCT volumes. J Clin Orthod. 2010;44:303–312. [PubMed] [Google Scholar]
- 12.Weissheimer A, Menezes LM, Koerich L, Pham J, Cevidanes LHS. Fast three-dimensional superimposition of cone beam computed tomography for orthopaedics and orthognathic surgery evaluation. Int J Oral Maxillofac Surg. 2015;44:1188–1196. doi: 10.1016/j.ijom.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Koerich L, Burns D, Weissheimer A, Claus JDP. Three-dimensional maxillary and mandibular regional superimposition using cone beam computed tomography: a validation study. Int J Oral Maxillofac Surg. 2016;45:662–669. doi: 10.1016/j.ijom.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 14.Ruellas AC, Yatabe MS, Souki BQ, et al. 3D Mandibular superimposition: comparison of regions of reference for voxel-based registration. PLoS ONE. 2016;11(6):e0157625. doi: 10.1371/journal.pone.0157625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ahmad R, Abu-Hassan MI, Li Q, Swain MV. Three dimensional quantification of mandibular bone remodeling using standard tessellation language registration based superimposition. Clin Oral Implants Res. 2013. 24):1273–1279. [DOI] [PubMed]
- 16.Schulze R, Heil U, Gross D, et al. Artefacts in CBCT: a review. Dentomaxillofac Radiol. 2011;40:265–273. doi: 10.1259/dmfr/30642039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Björk A. Prediction of mandibular growth rotation. Am J Orthod. 1969;55(6):585–599. doi: 10.1016/0002-9416(69)90036-0. [DOI] [PubMed] [Google Scholar]
- 18.Pluim JP, Maintz JB, Viergever MA. Mutual-information-based registration of medical images: a survey. IEEE Trans Med Imaging. 2003;22:986–1004. doi: 10.1109/TMI.2003.815867. [DOI] [PubMed] [Google Scholar]
- 19.Jabar N, Robinson W, Goto TK, Khambay BS. The validity of using surface meshes for evaluation of three-dimensional maxillary and mandibular surgical changes. Int J Oral Maxillofac Surg. 2015;44:914–920. doi: 10.1016/j.ijom.2015.02.005. [DOI] [PubMed] [Google Scholar]
- 20.Lemieux G, Carey JP, Flores-Mir C, et al. Precision and accuracy of suggested maxillary and mandibular landmarks with cone-beam computed tomography for regional superimpositions: an in vitro study. Am J Orthod Dentofacial Orthop. 2016;149(1):67–75. doi: 10.1016/j.ajodo.2015.06.025. [DOI] [PubMed] [Google Scholar]