ABSTRACT
Background: Refugees may be particularly vulnerable to the adverse effects of the COVID-19 pandemic on mental health due to their traumatic pasts and the challenges of the postmigration environment.
Objective: To evaluate the prevalence of COVID-19 related stressors and their relationship to key mental health and functioning outcomes in a resettled refugee sample.
Method: N = 656 refugees and asylum seekers living in Australia completed a survey in June 2020 to index their mental health (posttraumatic stress disorder (PTSD), depression, health anxiety and disability) and COVID-19 experiences. The relationship between COVID-19 stressors and mental health was examined using a series of hierarchical linear regression models while controlling for other key demographic factors.
Results: Refugees’ most prevalent stressors related to worries of being infected by COVID-19 or the risk COVID-19 posed to others, which predicted health anxiety and PTSD. Social-related difficulties predicted depression and disability symptoms. Accessing and trusting information from authorities were the least prevalent stressors and were not significantly associated with mental health outcomes; neither was accessing basic supplies and financial support. Fears relating to the future such as concerns about visa application processes predicted health anxiety and disability. Crucially, the strongest predictor of all mental health outcomes was COVID-19 serving as a reminder of difficult past events.
Conclusions: Refugees may be uniquely affected by COVID-19 because the pandemic serves as a reminder of their past conflict and persecution trauma. It is critical that mental health strategies accommodate the specific needs of refugees during the COVID-19 pandemic.
KEYWORDS: COVID-19, refugees, trauma, PTSD, depression, health anxiety, disability, stressors
HIGHLIGHTS
Resettled refugees report significant COVID-19 stressors, including being reminded of past traumatic events, which had strong associations with increased PTSD, depression, health anxiety and disability symptoms.
Abstract
Antecedentes: Los refugiados pueden ser particularmente vulnerables a los efectos adversos de la pandemia del COVID-19 en la salud mental a consecuencia de sus pasados traumáticos y los desafíos del ambiente post migración.
Objetivo: Evaluar la prevalencia de los estresores relacionados al COVID-19 y su relación a resultados claves funcionamiento y salud mental claves en una muestra de refugiados reubicados.
Método: N = 656 refugiados y personas en búsqueda de asilo que viven en Australia completaron una encuesta en junio de 2020 para identificar su salud mental (trastorno de estrés postraumático (TEPT), depresión, ansiedad de salud y discapacidad) y las experiencias de COVID-19. Fueron examinadas la relación entre los estresores de COVID-19 y la salud mental usando una serie de modelos de regresión lineal jerárquica mientras se controlaron otros factores demográficos claves.
Resultados: Los estresores más prevalentes de los refugiados se relacionaban con la preocupación de infectarse de COVID-19 o el riesgo del COVID-19 hacia otros, lo cual predijo la ansiedad de salud y TEPT. Las dificultades sociales predijeron los síntomas de depresión y discapacidad. Acceder y confiar en la información proporcionada por las autoridades fueron los estresores menos prevalentes y no se asociaron significativamente a los resultados de salud mental; tampoco lo fue el acceder a insumos básicos y apoyo financiero. Los temores asociados al futuro tales como preocupaciones sobre los procesos de aplicación a la visa predijeron la ansiedad de salud y discapacidad. De manera crucial, el predictor más fuerte de todos los resultados de salud mental fue el COVID-19 sirviendo como un recordatorio de los eventos pasados difíciles.
Conclusiones: Los refugiados pueden estar afectados de forma única por el COVID-19 porque la pandemia sirve como un recordatorio de sus conflictos pasados y trauma de persecución. Es crítico que las estrategias de salud mental se acomoden a las necesidades específicas de los refugiados durante la pandemia del COVID-19.
PALABRAS CLAVE: COVID-19, refugiados, trauma, TEPT, depresión, ansiedad de salud, discapacidad, estresores
Short abstract
背景: 由于过去的创伤和移民后环境的挑战, 难民可能特别容易受到 COVID-19 疫情对心理健康的不利影响。
目的: 评估重新定居的难民样本中 COVID-19 相关应激源的流行率及其与关键心理健康和功能结果的关系。
方法: N= 656 名居住在澳大利亚的难民和寻求庇护者于 2020 年 6 月完成了一项调查, 以表征其心理健康 (创伤后应激障碍 (PTSD), 抑郁, 健康焦虑和残疾) 和 COVID-19 经历。使用一系列控制了其他关键人口统计因素的分层线性回归模型考查 COVID-19 应激源与心理健康之间的关系。
结果: 难民最普遍的应激源与担心感染 COVID-19 或 COVID-19 对其他人构成的风险有关, 这预测了健康焦虑和 PTSD。社交相关困难预测了抑郁和残疾症状。获取和信任官方信息是最不常见的应激源, 并且与心理健康结果无显著关联; 获取基本用品和财政支持也不显著。对未来的担忧 (例如对签证申请流程的担忧) 预测了健康焦虑和残疾。至关重要的是, 所有心理健康结果的最强预测指标是 COVID-19起到过去困难事件的提示物的作用。
结论: 难民可能会受到 COVID-19 的独特影响, 因为疫情提醒他们过去的冲突和迫害创伤。在 COVID-19 疫情期间, 心理健康策略满足难民的特定需求至关重要。
关键词: COVID-19, 难民, 创伤, PTSD, 抑郁, 健康焦虑, 残疾, 应激源
The COVID-19 pandemic is a major global human crisis with substantial health, mental health and psychosocial consequences (Breslau et al., 2021; Dawel et al., 2020; Holmes et al., 2020; Pan et al., 2021; Pfefferbaum & North, 2020; Pierce et al., 2020). It has been suggested that refugees and asylum-seekers may be among the most vulnerable to the mental health effects of COVID-19 (Holmes et al., 2020; Júnior et al., 2020; Mukumbang, Ambe, & Adebiyi, 2020; Rees & Fisher, 2020), but few studies to date have explicitly investigated how refugees or forcibly displaced populations have responded to the COVID-19 pandemic. Specifically studying refugee populations is critical because the refugee experience is characterized by a number of factors that may exacerbate the impact of COVID-19. Firstly, refugees are highly trauma exposed, and commonly report experiencing extreme human rights violations like torture, conflict, violence, persecution and the traumatic loss of loved ones (Li, Liddell, & Nickerson, 2016; Nickerson et al., 2019; Steel et al., 2009). Second, people with a refugee background or who are displaced typically live in situations of varying instability including with insecure visa status (Nickerson et al., 2019), employment or housing (Li et al., 2016), and report significant daily or post-migration stressors such as social isolation, discrimination and communication difficulties (Chen, Hall, Ling, & Renzaho, 2017; Li et al., 2016). Refugee mental health models and empirical evidence suggest that while exposure to trauma has an adverse effect on mental health, this association is mediated by the degree of these daily stressors common to refugees (Miller & Rasmussen, 2010, 2017). Indeed, refugees report higher rates of psychological disorders compared to non-refugee community populations. For example, around one in three refugees will be diagnosed with posttraumatic stress disorder (PTSD) or depression in their lifetime (Fazel, Wheeler, & Danesh, 2005; Steel et al., 2009), compared to 6.4% and 4.1% respectively in the general Australian population (Australian Bureau of Statistics [ABS], 2007). The combination of exposure to trauma, significant post-migration stressors and high levels of pre-existing mental health issues may influence the impact of the COVID-19 pandemic on refugees.
Research conducted around the world has demonstrated that mental health has generally deteriorated because of COVID-19 (Breslau et al., 2021; Dawel et al., 2020; Pan et al., 2021; Pierce et al., 2020). An Australian study suggests that it is the social and economic impact of COVID-19 (rather than exposure to COVID-19 itself) that had a deleterious effect on the mental health of the general Australian community (especially elevated rates of depression and anxiety) (Dawel et al., 2020). This accords with another study conducted in the United States that reported pre-existing social and economic problems predicted poor mental health outcomes during COVID-19 (Breslau et al., 2021). The studies conducted with trauma-exposed populations have been smaller in number and size. One study found that childhood trauma exposure predicted increased PTSD symptom severity following the onset of the COVID-19 pandemic (Seitz, Bertsch, & Herpertz, 2021). In the case of refugees, it has been hypothesized that COVID-19 and its public health response may be reminiscent of prior conflict, persecution, or deprivation-related traumatic events commonly reported by refugees (Mollica, McInnes, Pool, & Tor, 1998; Steel et al., 2009), giving rise to distressing memories that may have mental health implications (Hoagland & Randrianarisoa, 2021; Rees & Fisher, 2020).
The relationship between COVID-19 stressors and mental health has not yet been examined in refugee groups. On top of prior trauma and visa insecurity, refugees may also experience specific difficulties as a result of COVID-19. Resettled refugees may face problems accessing regular health or settlement support services during COVID-19 (Aragona et al., 2020; Hoagland & Randrianarisoa, 2021; Júnior et al., 2020) or engaging in social initiatives important for building connections in their new communities (Culos, Rajwani, McMahon, & Robertson, 2020) and supporting their mental wellbeing (Nickerson et al., 2019). Fears relating to COVID-19 infection may also be elevated in refugee and culturally and linguistically diverse (CALD) communities in general due to barriers to accessing in-language public health services and resources (Júnior et al., 2020). Relatedly, refugees may have difficulty trusting Government advice given their past experiences of persecution by the hands of authorities. Resettled refugees may also be particularly vulnerable to deteriorating mental health due to employment loss or decline as a result of COVID-19 public health measures to contain the spread of the virus, and are considered to be at increased risk of homelessness and destitution (Kluge, Jakab, Bartovic, D’Anna, & Severoni, 2020).
Accordingly, it is essential to understand the mental health effects of exposure to COVID-19 events and stressors on refugees to assist practitioners and service providers to respond to the specific needs of refugees during the pandemic. This study addresses this question by examining the prevalence of COVID-19 stressors (e.g. worry about being infected with COVID-19) or events (e.g. being diagnosed with COVID-19) in a large sample of resettled refugees and asylum seekers living in Australia with high levels of psychopathology including PTSD, depression and generalized anxiety symptoms. The goal of this study was to examine which COVID-19 stressors were specifically associated with depression, PTSD and disability outcomes in refugees. These outcomes were selected as the most common mental health disorders examined in refugee populations, In addition, we examined health anxiety as a mental health outcome due to emerging evidence of its particular relevance to understanding psychological responses to COVID-19 (Newby et al., 2020).
1. Methods
1.1. Participants
Participants were adult refugees and asylum seekers residing in Australia who had participated in the Refugee Adjustment Study (RAS) – a large online study of refugee mental health and adjustment (Nickerson et al., 2019). The RAS sample comprised over 1,012 refugees from Arabic, Farsi, Tamil or English-speaking backgrounds who had arrived in Australia within the last 10 years and were initially recruited via advertising placed at refugee services across Australia, online advertising via social media and snowball sampling methods (Nickerson et al., 2019). Inclusion criteria were having a refugee or asylum seeker background, being over 18 years old, having arrived in Australia after January 2011, and literacy in Arabic, Farsi, Tamil or English.
To measure the acute effects of COVID-19, all RAS participants were invited to complete a COVID-19-related survey in June 2020. A total of 656 participants responded to the survey within the timeframe with N = 604 (92.2%) completing online and N = 55 (7.8%) completing a pen and paper version returned by post. This represents an overall response rate of 65.1%. We note that a further N = 42 participants clicked on the survey link but did not proceed with completing the survey and 3 participants who completed the pen and paper survey did not provide clear consent to participate. These participants were not included in the final sample of N = 656. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. All procedures involving human subjects were approved by the Human Research Ethics Committee at University of NSW Sydney; HC180627. Written informed consent was obtained from all subjects. Participants received an AUD$25 shopping voucher as reimbursement.
1.2. COVID-19 situation in Australia at the time of the survey, June 2020
At the time of data collection (June 2020), Australia was emerging from its first COVID-19 lockdown. By 30 June 2020, there were 7,834 total cases in the Australian community and 104 deaths, with case numbers rising in Melbourne, Victoria (Australian Government Department of Health, 2020). Even though rates of infection and deaths were relatively lower compared to many other countries (https://covid19.who.int/), anxiety and uncertainty around COVID-19 was extremely high in the Australian community (Newby et al., 2020).
1.3. Measures
All measures were collected during the COVID-19 survey with the exception of pre-migration trauma exposure, which was measured in the original RAS survey. Measures were translated and back-translated into study languages by accredited translators using World Health Organization (WHO) recommended procedures (World Health Organisation [WHO], n.d.); see (Nickerson et al., 2019).
1.3.1. Demographic measures
Key demographic measures were collected from participants including sex, age, country-of-origin, time in Australia and visa status. Pre-migration PTE exposure (drawn from original RAS survey) was measured via the Harvard Trauma Questionnaire (HTQ; (Mollica et al., 1992)), which indexes exposure to 16 potentially traumatic event types (experienced, witnessed) commonly reported by refugees (e.g. deprivation, forced separation, witnessing murder of loved ones, torture).
1.3.2. COVID-19 events and stressors measure
A measure indexing exposure to COVID-19 related events and worries for refugees was developed for this study. The structure of this measure drew on emerging COVID-19 mental health measures (Armour, McClinchey, Butter, McAloney-Kocaman, & McPherson, 2020; Conway, Woodard, & Zubrod, 2020; Freedman, Greene, & Armour, 2020; McLean & Cloitre, 2020), guided by WHO advice on COVID-19 survey development (WHO, 2020), as well as input from expert refugee practitioners, refugee community representatives, researchers and service providers in Australia. The first section of the measure focused on exposure to COVID-19 events encompassing 5 health-related events (i.e. experiencing COVID-19 symptoms, being tested for COVID-19, being diagnosed with COVID-19, being hospitalized with COVID-19, having a family member or close other die from COVID-19) and one item specifying the experience of employment loss or reduced work because of COVID-19. Frequencies of each event type were computed to measure relative prevalence.
The second section of the scale measured the extent to which COVID-19 related stressors were a problem for participants on a 5-point Likert scale (1 = No problem; 2 = A little bit of a problem; 3 = A moderately serious problem; 4 = A serious problem; 5 = A very serious problem). The structure of this scale was similar to that of the Post-Migration Living Difficulties Checklist, a measure commonly used to index stressors encountered by refugees in the postmigration environment (Steel, Silove, Bird, McGorry, & Mohan, 1999). The COVID-19 stressor subscale consisted of 5 Stressor Categories and 18 items. These 5 categories were as follows: (1)) COVID-19 infection stressors (e.g. ‘Worry about being infected by COVID-19’ α = .88); (2) Social stressors due to COVID-19 (‘Having to remain at home because of COVID-19’ α = .74); (3) Stressors relating to accessing practical support during COVID-19 (e.g. ‘Difficulty accessing emergency support through the Government’s COVID-19 measures’, α = .82); (4) Difficulties with relating to and trusting authorities (e.g. ‘Difficulty trusting information provided by authorities about COVID-19’, α = .83); and (5) Fears relating to the future (‘Worry that my visa application will be negatively affected by COVID-19’, α = .68). A complete overview of which items were grouped under the 5 themes is presented in Table S1. The overall internal consistency of the COVID-19 stressor subscale was strong (Cronbach α = .93). To obtain a count of COVID-19 related stressors we considered each stressor to be present if the item was rated as a moderately serious problem or higher (i.e. a score of 3 or above). Means were generated for each stressor category to be used in statistical models.
Finally, in recognition that experiences associated with COVID might trigger reminders of past traumatic/stressful events in this highly traumatized refugee cohort, we created a COVID-19 trauma reminder item. This item indexed the degree of problems experienced because of ‘the COVID-19 pandemic reminding me of difficult or stressful experiences from my past’.
1.3.3. Key mental health outcomes – mental health and disability
We assessed depression, PTSD, health anxiety symptoms and mental health-related disability as the key mental health outcomes in the sample. Depression (DSM-5) was assessed via the Patient Health Questionnaire (PHQ) which comprises nine items measuring the frequency of depression symptoms over the previous 2 weeks (Kroenke, Spitzer, Williams, & The, 2001). Responses are provided on a 4-point scale ranging 0 = Not at all to 4 = Nearly every day. Internal consistency was strong in this sample (α = .93). PTSD symptoms (DSM-5) were assessed with the Posttraumatic Diagnostic Scale (PDS), with 20 items indexing symptoms over the previous 2 weeks (Foa, Cashman, Jaycox, & Perry, 1997; Foa et al., 2016), with responses being provided on a 4-point scale ranging 0 = not at all or only 1 time, to 3 = five or more times per week or almost always. Internal consistency was very strong in this sample (α = .97). Health anxiety symptoms were assessed using the Bodily Preoccupation Scale of the Illness Attitude scale (Hedman-Lagerlöf, Tyrer, Hague, & Tyrer, 2019; Weck, Bleichhardt, & Hiller, 2010). It comprises three items measuring attention to and worry about bodily sensations, with responses provided on a 5-point scale ranging 0 = no to 4 = most of the time. Internal consistency was good for our sample (α = .83). Functioning was measured by the World Health Organization Disability Assessment Schedule 2.0 (WHO, 2000), which measures difficulties in performing daily activities over the previous 30 days on a 5-point scale (0 = Not at all to 5 = Extremely or cannot do). Internal consistency was strong (α = 0.94). Means for each measure were computed to represent symptom severity, with the exception of the WHODAS, where responses were summed across items in accordance with protocols (WHO, 2000).
Probable diagnosis was also determined for depression, PTSD, health anxiety, as well as generalized anxiety disorder (GAD) to gauge the degree of psychopathology in the sample for reporting purposes. For PTSD, this was determined by algorithm where symptoms were considered present if rated at least 1 (once a week/at least once in a while) (Foa, 1996). Probable PTSD diagnosis (DSM-5) was determined if participants met the threshold of at least one re-experiencing symptom, at least one avoidance symptom, at least two negative alterations in mood and cognition symptoms, and at least two hyperarousal symptoms, and experienced for more than 1 month. For depression, symptoms were considered present if rated at least 2 (more than half the days) according to the PHQ. Diagnosis was determined if participants endorsed the item of ‘feeling little interest or pleasure in doing things or ‘feeling down, depressed or hopeless’ and at least 4 more symptoms. For health anxiety, a summed score of at least 6 on the Bodily Preoccupation Scale of the Illness Attitude scale represented probable health anxiety diagnosis as previously validated (Hedman-Lagerlöf et al., 2019; Weck et al., 2010). We additionally assessed the probable diagnosis of generalized anxiety disorder, measured by the GAD-7 (Spitzer, Kroenke, Williams, & Lowe, 2006), which is a 7 item measure indexing anxiety symptoms in the past 2 weeks with responses provided on a 4 point scale ranging from 0 = Not at all to 3 = Nearly every day (internal consistency was strong, α = 0.95). A validated cut-off score of 10 or more was used to reflect probable GAD diagnosis (Spitzer et al., 2006).
1.4. Statistical analysis
We conducted four hierarchical linear regression models with three steps to examine the relationship between specific COVID-19 stressors and four key mental health outcomes. In the first step, we entered demographic and situational factors known to influence mental health in refugee and general populations; sex, age, language group, trauma exposure, visa status and time in Australia. At the second step, we entered the five COVID-19 stressor categories; infection stressors, social stressors, accessing support stressors, trusting authority stressors and fears relating to the future (see Table S1). At the third step, we entered the COVID-19 trauma reminder item as we predicted COVID-19 would serve to trigger distress in this highly traumatized refugee sample. Participants were not required to answer every question. As a result, there is some missing data across measures (<5%) and participants with missing data were excluded from regression analyses. The significance of each model and for individual predictors was determined at p < .0125 (Bonferroni-corrected p-value reflecting four models tested).
2. Results
2.1. Participant characteristics
Participant characteristics are presented in Table 1. There was an equal distribution of males/females, and participants were aged 42.85 years (SD = 12.22) on average. Most respondents completed the survey in Arabic (78.4%, N = 514), and the majority were originally from Iraq (58.7%, N = 385) and Syria (16.9%, N = 111). The average time in Australia was 4.64 years (SD = 1.7), and the majority of the sample held a secure visa (86.2%). Most participants were married or living with a partner (76.9%), and over half of the sample were unemployed (52.6%). Pre-migration trauma exposure rates were high, averaging 3.88 (SD = 4.08) different event types (range 0–16). In terms of mental health, rates of probable psychological disorder were high for this cohort: 32.9% of the sample met DSM-5 criteria for probable PTSD; 17.3% met DSM-5 criteria for probable depression, 23.3% met criteria for health anxiety (Hedman-Lagerlöf et al., 2019; Weck et al., 2010) and 19.8% met criteria for probable generalized anxiety disorder. We note that these rates of psychiatric disorders are higher than the general Australian population (PTSD – 6.4%, depressive episode – 4.1%, generalized anxiety disorder – 2.7%; (Slade, Johnston, Oakley-Browne, Andrews, & Whiteford, 2007), and reflect the elevated rates of psychiatric disorders in conflict-affected and displaced populations that are generally reported (Steel et al., 2009).
Table 1.
Participant characteristics. Percentages are reported as valid %
| N/mean | %/SD | ||
|---|---|---|---|
| Sex | |||
| Female | 323 | 49.2% | |
| Male | 333 | 50.8% | |
| Age (yrs) | 42.85 | 12.22 | |
| Language | |||
| Arabic | 514 | 78.4% | |
| Farsi | 65 | 9.9% | |
| Tamil | 18 | 2.7% | |
| English | 59 | 9.0% | |
| Country-of-origin | |||
| Iraq | 385 | 61.3% | |
| Syria | 111 | 17.7% | |
| Iran | 67 | 10.7% | |
| Sri Lanka | 20 | 3.2% | |
| Afghanistan | 10 | 1.6% | |
| Other | 35 | 4.5% | |
| Visa status | |||
| Secure | 561 | 86.2% | |
| Insecure | 90 | 13.8% | |
| Time in Australia (yrs) | 4.64 | 1.70 | |
| Employment | |||
| Employed | 209 | 31.9% | |
| Unemployed | 345 | 52.6% | |
| Studying | 102 | 15.5% | |
| Marital status | |||
| Married or de facto | 503 | 76.9% | |
| Single | 113 | 17.3% | |
| Separated or divorced | 21 | 3.2% | |
| Deceased spouse | 17 | 2.6% | |
| PTE exposure (event type count) | 3.88 | 4.08 | |
| PTSD | |||
| Probable PTSD diagnosis (DSM-5) | 183 | 32.9% | |
| PTSD symptom severity (PDS-5) | 0.61 | 0.70 | |
| Depression | |||
| Probable Depression diagnosis (DSM-5) | 106 | 17.3% | |
| Depression symptom severity (PHQ-9) | 0.80 | 0.67 | |
| Anxiety | |||
| Probably GAD diagnosis (DSM-5) | 122 | 19.8% | |
| Anxiety symptom severity (GAD-7) | 0.85 | 0.79 | |
| Health anxiety | |||
| Probable health anxiety diagnosis (BSQ) | 144 | 23.3% | |
| Health anxiety symptom severity (BSQ) | 1.09 | 0.90 | |
| Disability (WHO-DAS 12) | 12.19 | 10.07 | |
| COVID-19 stressors | |||
| Infection stressors | 2.99 | 1.23 | |
| Social stressors | 2.21 | 0.90 | |
| Accessing support stressors | 1.66 | 1.33 | |
| Trusting authority stressors | 1.53 | 0.79 | |
| Fears relating to the future | 2.11 | 1.14 | |
| Reminders of difficult past experiences | 2.33 | 1.32 | |
2.2. Exposure to COVID-19 events
The frequency of COVID-19 events is presented in Figure 1. Around one in five of our sample reported experiencing employment loss or decline due to COVID-19. Health-related COVID-19 events were relatively less prevalent. Less than 1% had been diagnosed with COVID-19 and 1.4% had experienced a loved one dying from COVID-19 (in Australia or overseas).
Figure 1.
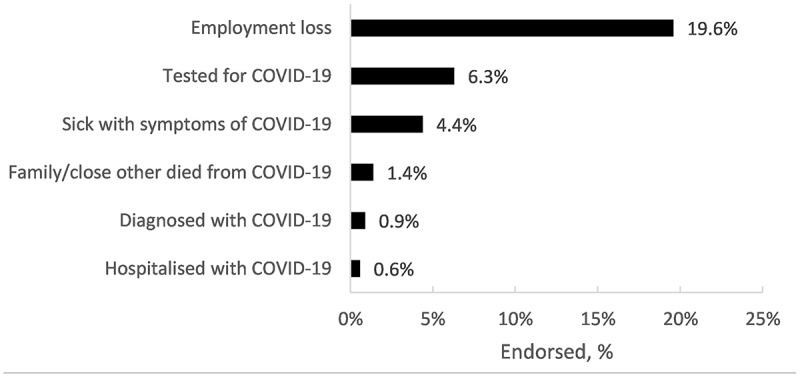
Prevalence of COVID-19 health and employment-related events (N = 656)
2.3. Exposure to COVID-19 related stressors
The frequency of COVID-19 stressors is presented in Figure 2. The most prevalent stressors were related to COVID-19 infection, including worries about being infected (66.5%), of a loved one being infected (72.1%) or infecting others (47.7%) being most commonly reported. Social stressors as a consequence of the COVID-19 pandemic were also common, including school closures (46.7%), reduced social activities (46.6%), and having to remain at home (41.3%). The COVID-19 pandemic serving as a reminder of past trauma was endorsed by 41.1% of the sample. Difficulties in accessing resources, emergency support, or information relating to COVID-19 were reported relatively less frequently (range 13.5–28.3%). Difficulties trusting information about COVID-19 from authorities and implementing COVID-19 public health advice was reported by 11.7% and 16.7% of the sample respectively.
Figure 2.
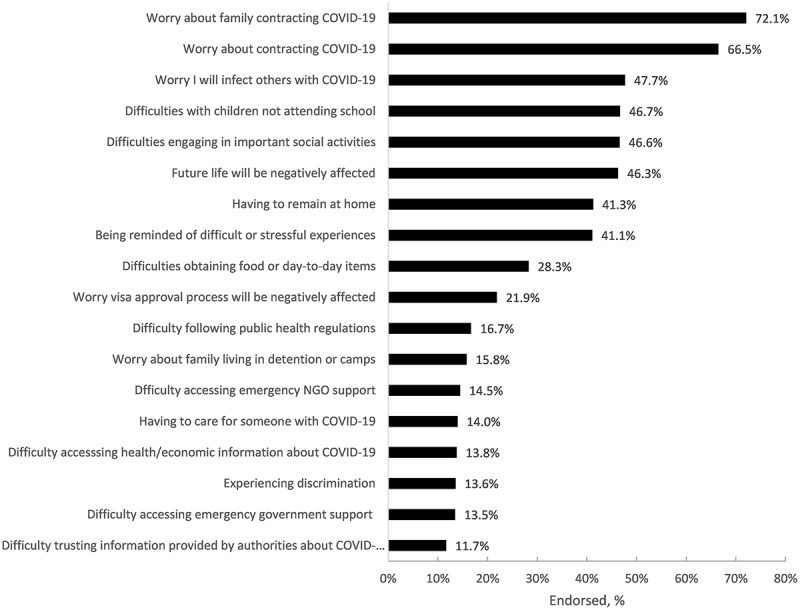
Prevalence of COVID-19 stressors, endorsed at a moderately serious or higher level (N = 656)
2.4. Multivariate regressions
Associations between COVID-19 worries and mental health and functioning were tested using multivariate regression models. First, bivariate correlations between continuous independent and dependent variables are provided in Table S2. These indicate there are significant correlations between COVID-19 stressor categories and mental health outcomes. Second, the three step hierarchical regression models were significant for PTSD, health anxiety, depression and disability (see Table 2 which presents the abbreviated model; the full-model for each Step is presented in Table S3). Worries related to contracting COVID-19 (for the self, for family or risk of infecting others) predicted PTSD and health anxiety symptoms as expected, and remained significant at the 3rd step for health anxiety. Social-related difficulties due to COVID-19 specifically predicted increased depression symptoms and disability outcomes. While fear relating to the future (including visa application processes and future life in Australia) was associated with increased health anxiety symptoms and disability at Step 2, this factor was not significant at Step 3. The degree to which COVID-19 reminded participants of their past trauma was strongly associated with elevated PTSD, health anxiety, depression and disability symptoms.
Table 2.
Hierarchical regression models featuring COVID-19 stressor categories as predictor variables. Bold predictors are significant at p < .0125 (Bonferroni-corrected). Full model with all steps presented in Table S2
| PTSD symptoms |
Health anxiety symptoms |
Depression symptoms |
Disability |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| F(14,500) = 25.75, p < .001, AdjR2 = .40 |
F(14,517) = 16.91, p < .001, AdjR2 = .30 |
F(14,512) = 19.47, p < .001, AdjR2 = .33 |
F(14,509 = 12.78, p < .001, AdjR2 = .24 |
||||||||||||||
| B (SE) | β | sig | 95% CI | B (SE) | β | sig | 95% CI | B (SE) | β | sig | 95% CI | B (SE) | β | sig | 95% CI | ||
| Step 1 | |||||||||||||||||
| Female | 0.17 (0.06) | 0.13 | 0.002* | 0.06,0.29 | 0.12 (0.08) | 0.07 | 0.134 | −0.04,0.27 | 0.12 (0.06) | 0.08 | 0.044 | 0.003,0.24 | 1.87 (0.86) | 0.09 | 0.030* | 0.19,3.56 | |
| Age | 0.00 (0.002) | −0.003 | 0.944 | −0.01, 0.00 | 0.003(0.003) | 0.04 | 0.339 | −0.003,0.01 | 0.00 (0.002) | −0.01 | 0.910 | −0.01,0.1 | 0.10 (0.04) | 0.12 | 0.005* | 0.03,0.17 | |
| Language (Arabic = reference) | |||||||||||||||||
| English | 0.16 (0.12) | 0.07 | 0.132 | −0.05,0.37 | 0.06 (0.14) | 0.02 | 0.686 | −0.22,0.34 | 0.06 (0.11) | 0.03 | 0.573 | −0.15,0.28 | −1.81 (1.57) | −0.05 | 0.251 | −4.89,1.28 | |
| Farsi | 0.02 (0.13) | 0.01 | 0.866 | −0.24,0.28 | 0.02 (0.18) | 0.01 | 0.901 | −0.33,0.37 | 0.14 (0.14) | 0.06 | 0.303 | −0.13,0.41 | −4.24 (1.98) | −0.13 | 0.033* | −8.14,-0.35 | |
| Tamil | −0.21 (0.21) | −0.05 | 0.322 | −0.63,0.21 | −0.10 (0.29) | −0.02 | 0.728 | −0.67,0.47 | −0.02 (0.22) | −0.01 | 0.938 | −0.45,0.42 | −4.18 (3.30) | −0.06 | 0.206 | −10.66,2.30 | |
| Time in Aus (yrs) | 0.05 (0.02) | 0.13 | 0.018 | 0.01,0.10 | 0.07 (0.03) | 0.14 | 0.02* | 0.01,0.13 | 0.04 (0.02) | 0.10 | 0.065 | −0.003,0.09 | 0.41 (0.34) | 0.07 | 0.230 | −0.26, 1.07 | |
| PTE exposure | 0.07 (0.01) | 0.37 | <.001* | 0.05,0.08 | 0.05 (0.01) | 0.24 | <.001* | 0.03,0.07 | 0.05 (0.01) | 0.29 | <.001* | 0.04,0.07 | 0.73 (0.11) | 0.29 | <.001* | 0.51,0.95 | |
| Visa insecurity | 0.11 (0.12) | 0.05 | 0.365 | −0.13,0.34 | −0.13 (0.16) | −0.05 | 0.417 | −0.45,0.19 | 0.22 (0.12) | 0.11 | 0.071 | −0.02,0.46 | 2.83 (1.79) | 0.10 | 0.115 | −0.70, 6.35 | |
| Step 2 | |||||||||||||||||
| Infection stressors | 0.08 (0.03) | 0.13 | 0.010a | 0.02,0.13 | 0.16 (0.04) | 0.22 | <.001* | 0.08,0.24 | 0.05 (0.03) | 0.08 | 0.138 | −0.15,0.11 | 0.26 (0.46) | 0.03 | 0.573 | −0.64,1.16 | |
| Social stressors | 0.09 (0.05) | 0.11 | 0.074 | −0.01,0.18 | 0.14 (0.07) | 0.14 | 0.029 | 0.01,0.27 | 0.14 (0.05) | 0.18 | 0.006* | 0.04,0.24 | 2.11 (0.75) | 0.19 | 0.005* | 0.65,3.58 | |
| Accessing support stressors | 0.07 (0.05) | 0.09 | 0.133 | −0.02,0.17 | −0.08 (0.07) | −0.08 | 0.242 | −0.21,0.05 | 0.08 (0.05) | 0.10 | 0.118 | −0.02,0.18 | 0.11 (0.75) | 0.01 | 0.888 | −1.37,1.58 | |
| Trusting authority stressors | 0.10 (0.05) | 0.11 | 0.039 | 0.01,0.20 | 0.14 (0.06) | 0.12 | 0.036 | 0.01,0.26 | 0.04 (0.05) | 0.04 | 0.456 | −0.06,0.14 | 1.33 (0.74) | 0.11 | 0.073 | −0.13,2.79 | |
| Fears relating to the future | 0.07 (0.04) | 0.11 | 0.057 | −0.01,0.14 | 0.14 (0.05) | 0.18 | 0.003 | 0.05,0.24 | 0.07 (0.04) | 0.11 | 0.065 | −0.004,0.14 | 1.41 (0.55) | 0.16 | 0.011 | 0.33, 2.50 | |
| Step 3 | |||||||||||||||||
| COVID-19 reminding of difficult past experiences | 0.15 (0.03) | 0.27 | <0.001*a | 0.09,0.20 | 0.17 (0.04) | 0.25 | <0.001* | 0.10,0.24 | 0.11 (0.03) | 0.20 | <0.001* | 0.05,0.17 | 1.17 (0.43) | 0.16 | 0.007* | 0.32, 2.01 | |
*Remains or becomes significant at Step 3.
3. Discussion
This study examined the prevalence of COVID-19 related stressors and their relationship to mental health outcomes in a cohort of refugees with high rates of psychiatric disorders including PTSD, depression and anxiety. Despite not being the most prevalent concern (41.1%), difficulties experienced because of COVID-19 triggering memories of past traumatic events was the strongest predictor of PTSD, health anxiety, depression and disability in this refugee cohort. This was over and above the contribution of other significant factors known to affect mental health outcomes in refugees including quantum of trauma exposure (Steel et al., 2009), visa insecurity (Nickerson et al., 2019) and other important COVID-19 stressors. It has been posited that reminders of past events could be an important determinant of mental health in refugees during COVID-19 (Rees & Fisher, 2020), and may differentiate reactions of refugees from non-refugee populations to the pandemic. Reports from data collected in Australia, Egypt, Sweden and other countries by Red Cross/Red Crescent suggest that being reminded of past trauma is a critical factor determining refugee community response to the pandemic (Hoagland & Randrianarisoa, 2021). This may be because COVID-19 responses to prevent disease transmission may share characteristics with refugee traumatic experiences. For example, memories of living in situations of political terror or in immigration detention may be triggered by a heightened role of government, social isolation strategies and quarantine measures that are enacted during COVID-19. Problems sourcing basic supplies or accessing services during the COVID-19 lock-down could remind refugees of previous difficulties accessing essential goods during situations of conflict or civil unrest. These findings underscore the importance of practitioners and service providers being aware of the significance of COVID-19 for refugees, and its impact on mental health. Access to mental health services are critical to ensure that these effects are mitigated and that refugees are psychologically supported to cope with the pandemic. At the same time, refugees may also have strategies and support networks in place to assist them in navigating the uncertainty associated with COVID-19 due to having to overcome similar difficulties in the past (Hoagland & Randrianarisoa, 2021).
The most prevalent stressors related to worries about self or family contracting COVID-19 or worry about spreading COVID-19 to others. Given these worries reflect fear of being harmed or harming others with COVID-19, it is not surprising that COVID-19 infection stressors predicted increased health anxiety and PTSD symptoms. Elevated health anxiety has been reported in the general Australian population during COVID-19, particularly amongst those with pre-pandemic mental illness (Newby et al., 2020). The link between COVID-19 infection stressors and health anxiety is critical for refugees as those who experience high health anxiety may be at risk of social withdrawal, excessive symptom checking or hygiene practices and increased media engagement regarding COVID-19, which may exacerbate psychological distress. While refugees were concerned with being personally infected, they also demonstrated high levels of fear for family and worry about infecting others. This might reflect the fact that many refugees come from collectivistic cultural backgrounds, which cultivate a sense of self that is interdependent with others, particularly their families (Liddell et al., 2021). High prevalence of this particular stressor may also reflect the fact that many refugees may be concerned about their family members living in their home countries or other contexts (e.g. refugee camps) where vulnerability to COVID-19 is increased. For example, Iran was an early global hotspot for COVID-19, with the number of cases and deaths in Iran, Iraq, Syria, Afghanistan and Sri Lanka where the participants were from continuing to climb at the time of the survey (June 2020; https://covid19.who.int/). It is also notable that health anxiety has rarely been reported in refugees, where research studies have tended to focus on PTSD, depression, or grief. The results of this study suggest that health anxiety is an important disorder that should be considered in refugee populations in future research.
Social difficulties experienced as a consequence of COVID-19 – which included staying at home or engaging in social activities – were associated with increased depression and disability symptoms in this refugee sample. While social isolation as a consequence of restrictions to curb COVID-19 community transmission has been linked to poorer mental health in the general community (Dawel et al., 2020; McGinty, Presskreischer, Han, & Barry, 2020), refugees may be particularly vulnerable to this adverse effect. Resettled refugees often experience significant isolation and loneliness (Chen et al., 2017; Nickerson et al., 2019), which diminishes mental wellbeing (Wu et al., 2021). However, studies have found that social support from within a refugee’s own community is related to lower PTSD symptoms (Schweitzer, Melville, Steel, & Lacherez, 2006), and higher levels of structural social capital (i.e. membership of groups) appears to be protective against the adverse effect of insecure visa status on depression and suicidality in refugee communities (Nickerson et al., 2019). Indeed, factors that contribute to increased social inclusion have been associated with stronger psychological adaptation in refugees settled in Germany (von Haumeder, Ghafoori, & Retailleau, 2019). The combination of pre-existing isolation, elevated depression symptoms which engenders social withdrawal (Nickerson et al., 2019), the inability to engage in crucial social-based coping strategies due to COVID-19 restrictions and ongoing separation from family (Liddell et al., 2021), may have particularly potent consequences for the mental health and functioning in refugee populations during COVID-19.
We did not observe significant links between difficulties trusting authorities or accessing basic needs/support and mental health outcomes in this study. Trust-related stressors appeared to be less prevalent (at 11.7%) relative to other COVID-19 stressors. This is somewhat surprising given refugees have commonly endured persecution and threats to their life at the hands of authorities in their home countries, which has been previously linked to reduced interpersonal trust (Nickerson et al., 2019). Other reports are suggesting that trust in Government has increased during COVID-19 in the general Australian community (Markus, 2020), and evidence from newly arrived refugees to Australia with secure visas (which constituted 86.2% of the our sample) suggests they have high trust in government and essential services like police (Culos et al., 2020). Difficulties accessing services, basic resources, and financial support were moderately prevalent, but did not predict mental health outcomes in this study. A recent report indicates that barriers to acquiring essential items or accessing basic services during COVID-19 increased psychological distress, particularly amongst migrants with temporary or undocumented status (Hoagland & Randrianarisoa, 2021). Our study controlled for visa status, and so it is possible this barrier particularly impacts those with insecure visa status and will need to be more closely examined in future studies. We also did not measure access to services, including health and settlement support services, which is a limitation of this study. It is critical to understand the relationships between trust and access with mental health in more detail in order to ensure refugee communities fully engage in public health practices that will protect them from COVID-19.
Finally, we observed that future-related fears concerning visa security and settlement in Australia were significant predictors of health anxiety and disability in this cohort. It is somewhat surprising that this stressor did not predict depression, as past research has shown a sense of a constricted future is related to hopelessness and suicidality in refugees (Procter, Kenny, Eaton, & Grech, 2018). It is concerning that future-related fears due to COVID-19 predicts increased disability as it is crucial that functioning is maintained in order to navigate COVID-19 related stressors. Government authorities and services could play a role in reassuring refugees regarding the impact of COVID-19 on visa or citizenship applications, in order to assuage the worst mental health impacts of these stressors.
3.1. Implications
It is important that health and mental health professionals are aware of the specific risks faced by resettled refugees during COVID-19, particularly in relation to the strong association between past trauma reminders and higher mental health symptoms. Refugee and migrant services remain an important avenue of support for refugees during COVID-19, and have been working during the pandemic to address the problem of increased social isolation in refugees (Hoagland & Randrianarisoa, 2021). These findings also highlight the importance of public health messages that specifically target culturally and linguistically diverse members of the community, as well as those with limited literacy (McCaffery et al., 2020), in order to strengthen participation in COVID-19 public health preventative programmes, including vaccine uptake. Governments need to ensure resettled refugees have equal access to COVID-19 emergency measures in order to protect against worsening mental health outcomes that may flow from financial stress and reduced employment.
3.2. Limitations
Limitations include the fact that the data were collected from a large convenience sample who were participants in an ongoing study that did not implement representative sampling. This may limit the generalizability of the findings of this study to all resettled refugees in Australia. The original sample was recruited via advertising and snowball sampling methods (Nickerson et al., 2019). Overall, our sample is comparable in terms of gender, age and proportion of arrivals from Iran and Sri Lanka to a nationally representative study of refugees who arrived in Australia in 2013 – the Building a New Life in Australia (BNLA) study (Australian Government Department of Services, 2017). However, our sample over-represents Arabic-speaking refugees from Iraq and Syria, and under-represents refugees from Afghanistan compared to the BNLA study. Furthermore, 65% of invited participants from the Refugee Adjustment Study completed the COVID-19 survey outlined in this study. This lower completion rate may be due participants having a short (1 month) time frame to complete the survey, or that they were invited during a particularly stressful time as Australia was emerging from its first COVID-19 wave. We acknowledge that the lower completion rate may have over-sampled participants with either higher levels of psychological symptoms (i.e. more distressed participants were motivated to take part) or lower levels of psychological symptoms (i.e. individuals with good functioning were more motivated to take part). Given the relatively low rates of exposure to COVID-19 health events in Australia at the time of data collection, these findings may not generalize to refugees in other settings outside Australia. However, we note that uncertainty and anxiety around COVID-19 was exceptionally high in the Australian community despite low rates of infection (Newby et al., 2020). This data is cross-sectional; longitudinal studies that examine changes in psychological symptoms over time will be critical to unpacking the key determinants of mental health outcomes in refugees during COVID-19. We acknowledge that there may be other psychological and mental health outcomes relevant to refugees that were not examined in this study (e.g. prolonged grief). Finally, our COVID-19 experiences and stressors measures were developed specifically for this study, but were derived from other emerging COVID-19 (Armour et al., 2020; Conway et al., 2020; Freedman et al., 2020; McLean & Cloitre, 2020) and refugee stressor measures (Steel et al., 1999).
4. Conclusions
COVID-19 represents a major life stressor for all humans, but the pandemic may render groups like refugees particularly vulnerable to negative mental health consequences due to their traumatic pasts and high rates of mental health issues. Findings from this study provide evidence for mental health practitioners, service providers and policy makers to ensure that COVID-19 strategies are inclusive and respond to the needs of vulnerable groups like resettled refugees.
Supplementary Material
Acknowledgments
The authors wish to thank the participants in this study. The authors acknowledge the contribution of Australian Red Cross and Settlement Services International (SSI) to this study. We also acknowledge the assistance of A/Prof Jill Newby in relation to the measurement of health anxiety.
Funding Statement
This work was supported by an Australian Research Council Linkage Project [AN, BL, MOD, VM, TM; LP160100670] and a Career Advancement Award to Belinda Liddell from the University of New South Wales Sydney.
Disclosure statement
Author Vicki Mau is employed at Australian Red Cross. Authors Tadgh McMahon and Greg Benson are employed at Settlement Services International (SSI). The remaining authors have nothing to disclose.
Data availability statement
The data that support the findings of this study are available on request from the corresponding author, BL. The data are not publicly available due to the de-identified data possibly containing information that could compromise the privacy and safety of the research participants.
Supplementary material
Supplemental data for this article can be accessed here.
References
- Aragona, M., Barbato, A., Cavani, A., Costanzo, G., & Mirisola, C. (2020). Negative impacts of COVID-19 lockdown on mental health service access and follow-up adherence for immigrants and individuals in socio-economic difficulties. Public Health, 186, 52–12. doi: 10.1016/j.puhe.2020.06.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armour, C., McClinchey, E., Butter, S., McAloney-Kocaman, K., & McPherson, K. E. (2020). Understanding the longitudinal psychosocial impact of the COVID-19 pandemic in the United Kingdom; A methodological overview of The COVID-19 psychological wellbeing study [Preprint]. doi: 10.1007/s10862-020-09841-4 [DOI] [PMC free article] [PubMed]
- Australian Bureau of Statistics . (2007). National survey of mental health and wellbeing: Summary of results 2007. Australia: Australian Government. Retrieved from https://www.abs.gov.au/statistics/health/mental-health/national-survey-mental-health-and-wellbeing-summary-results/latest-release [Google Scholar]
- Australian Government Department of Health . (2020). Coronavirus (COVID-19) at a glance for 30 June 2020. Australia: Australian Government. Retrieved from https://www.health.gov.au/resources/collections/coronavirus-covid-19-at-a-glance-infographic-collection [Google Scholar]
- Australian Government Department of Services . (2017). Building aNew Life in Australia (BNLA): The longitudinal study of humanitarian migrants ─ Findings from the first three waves. Australia: Australian Government. Retrieved from https://www.dss.gov.au/our-responsibilities/families-and-children/programmes-services/building-a-new-life-in-australia-bnla-the-longitudinal-study-of-humanitarian-migrants
- Breslau, J., Finucane, M. L., Locker, A. R., Baird, M. D., Roth, E. A., & Collins, R. L. (2021). A longitudinal study of psychological distress in the United States before and during the COVID-19 pandemic. Preventive Medicine, 143, 143. doi: 10.1016/j.ypmed.2020.106362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen, W., Hall, B. J., Ling, L., & Renzaho, A. M. (2017). Pre-migration and post-migration factors associated with mental health in humanitarian migrants in Australia and the moderation effect of post-migration stressors: Findings from the first wave data of the BNLA cohort study. The Lancet Psychiatry, 4(3), 218–229. doi: 10.1016/S2215-0366(17)30032-9 [DOI] [PubMed] [Google Scholar]
- Conway, L. G. I., Woodard, S. R., & Zubrod, A. (2020). Social psychological measurements of COVID-19: Coronavirus perceived threat, government response, impacts, and experiences questionnaires preprint.
- Culos, I., Rajwani, H., McMahon, T., & Robertson, S. (2020). Foundations for belonging: A snapshot of newly arrived refugees. Sydney, Australia: Settlement Services International/Institute for Culture and Society, Western Sydney University. [Google Scholar]
- Dawel, A., Shou, Y., Smithson, M., Cherbuin, N., Banfield, M., Calear, A. L., & Batterham, P. J. (2020). The effect of COVID-19 on mental health and wellbeing in a representative sample of Australian adults. Frontiers in Psychiatry, 11, 579985. doi: 10.3389/fpsyt.2020.579985 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazel, M., Wheeler, J., & Danesh, J. (2005). Prevalence of serious mental disorder in 7000 refugees resettled in western countries: A systematic review. Lancet, 365(9467), 1309–1314. doi: 10.1016/S0140-6736(05)61027-6 [DOI] [PubMed] [Google Scholar]
- Foa, E. (1996). Posttraumatic diagnostic manual. Minneapolis, MN: National Computer Systems. [Google Scholar]
- Foa, E. B., Cashman, L., Jaycox, L., & Perry, K. (1997). The validation of a self-report measure of posttraumatic stress disorder: The posttraumatic diagnostic scale. Psychological Assessment, 9(4), 445–451. doi: 10.1037/1040-3590.9.4.445 [DOI] [Google Scholar]
- Foa, E. B., McLean, C. P., Zang, Y., Zhong, J., Powers, M. B., Kauffman, B. Y., & Knowles, K. (2016). Psychometric properties of the posttraumatic diagnostic scale for DSM-5 (PDS-5). Psychological Assessment, 28(10), 1166–1171. doi: 10.1037/pas0000258 [DOI] [PubMed] [Google Scholar]
- Freedman, S., Greene, T., & Armour, C. (2020). Coronavirus experiences and concerns measure (Unpublished). [Google Scholar]
- Hedman-Lagerlöf, E., Tyrer, P., Hague, P., & Tyrer, H. (2019). Health anxiety. British Medical Journal, 364, I1774. doi: 10.1136/bmj.l774 [DOI] [PubMed] [Google Scholar]
- Hoagland, N., & Randrianarisoa, A. (2021). Locked down and left out. Australia: Red Cross Red Cresent Global Migration Lab. Retrieved from https://www.redcross.org.au/getmedia/3c066b6d-a71f-46b8-af16-2342ff304291/EN-RCRC-Global-Migration-Lab-Locked-down-left-out-COVID19.pdf.aspx [Google Scholar]
- Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., & Bullmore, E. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: A call for action for mental health science. The Lancet Psychiatry, 7(6), 547–560. doi: 10.1016/S2215-0366(20)30168-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Júnior, J. G., De Sales, J. P., Moreira, M. M., R, P. W., Lima, C. K. T., & Neto, M. L. R. (2020). A crisis within the crisis: The mental health situation of refugees in the world during the 2019 coronavirus (2019-nCoV) outbreak. Psychiatry Research, 288(113000), 113000. doi: 10.1016/j.psychres.2020.113000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kluge, H. H. P., Jakab, Z., Bartovic, J., D’Anna, V., & Severoni, S. (2020). Refugee and migrant health in the COVID-19 response. Lancet, 395(10232), 1237–1239. doi: 10.1016/S0140-6736(20)30791-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke, K., Spitzer, R. L., & Williams, J. B. (2001). 9 The PHQ-: Validity of a brief depression severity measure. Journal of General Internal Medicine, 16(9), 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, S. S., Liddell, B. J., & Nickerson, A. (2016). The relationship between post-migration stress and psychological disorders in refugees and asylum seekers. Current Psychiatry Reports, 18(9), 82. doi: 10.1007/s11920-016-0723-0 [DOI] [PubMed] [Google Scholar]
- Liddell, B. J., Byrow, Y., O’Donnell, D. A., Mau, V., Batch, N., McMahon, T., … Nickerson, A. (2021). Mechanisms underlying the mental health impact of family separation on resettled refugees. The Australian and New Zealand Journal of Psychiatry, 55, 699–710. doi: 10.1177/0004867420967427 [DOI] [PubMed] [Google Scholar]
- Markus, A. (2020). Mapping social cohesion: The scalon foundation surveys. Scalon Foundation Research Institute. [Google Scholar]
- McCaffery, K. J., Dodd, R. H., Cvejic, E., Ayre, J., Isautier, J., Copp, T., … Wolf, M. (2020). Health literacy and disparities in COVID-19–related knowledge, attitudes, beliefs and behaviours in Australia. Public Health Research & Practice, 30(4), e30342012. doi: 10.17061/phrp30342012 [DOI] [PubMed] [Google Scholar]
- McGinty, E. E., Presskreischer, R., Han, H., & Barry, C. L. (2020). Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA, 324(1), 93–94. doi: 10.1001/jama.2020.9740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean, P., & Cloitre, M. (2020). Coronavirus stressor survey (Unpublished measure). [Google Scholar]
- Miller, K. E., & Rasmussen, A. (2010). War exposure, daily stressors, and mental health in conflict and post-conflict settings: Bridging the divide between trauma-focused and psychosocial frameworks. Social Science & Medicine, 70(1), 7–16. doi: 10.1016/j.socscimed.2009.09.029 [DOI] [PubMed] [Google Scholar]
- Miller, K. E., & Rasmussen, A. (2017). The mental health of civilians displaced by armed conflict: An ecological model of refugee distress. Epidemiology and Psychiatric Sciences, 26(2), 129–138. doi: 10.1017/S2045796016000172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mollica, R., Caspi-Yavin, Y., Bollini, P., Truong, T., Tor, S., & Lavelle, J. (1992). The Harvard trauma questionnaire; Validating a cross cultural instrument for measuring torture, trauma, and post-traumatic stress disorder in Indochina refugees. The Journal of Nervous and Mental Disease, 180(2), 111–116. doi: 10.1097/00005053-199202000-00008 [DOI] [PubMed] [Google Scholar]
- Mollica, R. F., McInnes, K., Pool, C., & Tor, S. (1998). Dose-effect relationships of trauma to symptoms of depression and post-traumatic stress disorder among Cambodian survivors of mass violence. British Journal of Psychiatry, 173(6), 482–488. doi: 10.1192/bjp.173.6.482 [DOI] [PubMed] [Google Scholar]
- Mukumbang, F. C., Ambe, A. N., & Adebiyi, B. O. (2020). Unspoken inequality: How COVID-19 has exacerbated existing vulnerabilities of asylum-seekers, refugees, and undocumented migrants in South Africa. International Journal for Equity in Health, 19(141). doi: 10.1186/s12939-020-01259-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newby, J. M., O’Moore, K., Tang, S., Christensen, H., Faasse, K., & Francis, J. M. (2020). Acute mental health responses during the COVID-19 pandemic in Australia. PLoS One, 15(7), e0236562. doi: 10.1371/journal.pone.0236562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickerson, A., Byrow, Y., O’Donnell, M., Mau, V., McMahon, T., Pajak, R., & Liddell, B. J. (2019). The association between visa insecurity and mental health, disability and social engagement in refugees living in Australia. European Journal of Psychotraumatology, 10(1), 1688129. doi: 10.1080/20008198.2019.1688129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nickerson, A., Liddell, B. J., Keegan, D., Edwards, B., Felmingham, K., Forbes, D., & Bryant, R. A. (2019). Longitudinal association between trust, psychological symptoms and community engagement in resettled refugees. Psychological Medicine, 49(10), 1661–1669. doi: 10.1017/S0033291718002246 [DOI] [PubMed] [Google Scholar]
- Pan, K.-Y., Kok, A. A. L., Eikelenboom, M., Horsfall, M., Jorg, F., Luteijn, R., & Penninx, B. W. J. H. (2021). The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: A longitudinal study of three Dutch case-control cohorts. The Lancet Psychiatry, 8(2), 121–129. doi: 10.1016/S2215-0366(20)30491-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfefferbaum, B., & North, C. S. (2020). Mental health and the COVID-19 pandemic. New England Journal of Medicine, 383(6), 510–512. doi: 10.1056/NEJMp2008017 [DOI] [PubMed] [Google Scholar]
- Pierce, M., Hope, H., Ford, T., Hatch, S., Hotopf, M., John, A., & Abel, K. M. (2020). Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry, 7(10), 883–892. doi: 10.1016/S2215-0366(20)30308-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Procter, N., Kenny, M., Eaton, H., & Grech, C. (2018). Lethal hopelessness: Understanding andresponding to asylum seeker distress and mental deterioration. International Journal of Mental Health Nursing, 27(1), 448–454. doi: 10.1111/inm.12325 [DOI] [PubMed] [Google Scholar]
- Rees, S., & Fisher, J. (2020). COVID-19 and the mental health of people from refugee backgrounds. International Journal of Health Services, 50(4), 415–417. doi: 10.1177/0020731420942475 [DOI] [PubMed] [Google Scholar]
- Schweitzer, R., Melville, F., Steel, Z., & Lacherez, P. (2006). Trauma, post-migration living difficulties, and social support as predictors of psychological adjustment in resettled Sudanese refugees. Australian and New Zealand Journal of Psychiatry, 40(2), 179–188. doi: 10.1080/j.1440-1614.2006.01766.x [DOI] [PubMed] [Google Scholar]
- Seitz, K. I., Bertsch, K., & Herpertz, S. C. (2021). A prospective study of mental health during the COVID-19 pandemic in childhood trauma–exposed individuals: Social support matters. Journal of Traumatic Stress, 34(3), 477–486. doi: 10.1002/jts.22660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade, T., Johnston, A., Oakley-Browne, M., Andrews, G., & Whiteford, H. (2007). National survey of mental health and wellbeing: Methods and key findings. Australian and New Zealand Journal of Psychiatry, 2009(43), 594–605. doi: 10.1080/00048670902970882 [DOI] [PubMed] [Google Scholar]
- Spitzer, R. L., Kroenke, K., Williams, J. B., & Lowe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. doi: 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Steel, Z., Chey, T., Silove, D., Marnane, C., Bryant, R. A., & van Ommeren, M. (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. JAMA, 302(5), 537–549. doi: 10.1001/jama.2009.1132 [DOI] [PubMed] [Google Scholar]
- Steel, Z., Silove, D., Bird, K., McGorry, P., & Mohan, P. (1999). Pathways from war trauma to posttraumatic stress symptoms among tamil asylum seekers, refugees, and immigrants. Journal of Traumatic Stress, 12(3), 421–435. doi: 10.1023/A:1024710902534 [DOI] [PubMed] [Google Scholar]
- von Haumeder, A., Ghafoori, B., & Retailleau, J. (2019). Psychological adaptation and posttraumatic stress disorder among Syrian refugees in Germany: A mixed-methods study investigating environmental factors. European Journal of Psychotraumatology, 10(1), 1686801. doi: 10.1080/20008198.2019.1686801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weck, F., Bleichhardt, G., & Hiller, W. (2010). Screening for hypochondriasis with the illness attitude scales. Journal of Personality Assessment, 92(3), 260–268. doi: 10.1080/00223891003670216 [DOI] [PubMed] [Google Scholar]
- World Health Organisation . Regional Office for Europe. (2020). Survey tool and guidance: Rapid, simple, flexible behavioural insights on COVID-19. Denmark. Retrieved from https://apps.who.int/iris/handle/10665/333549 [Google Scholar]
- World Health Organisation . (n.d.). Process of translation and adaptation of instruments. Geneva: WHO. [Google Scholar]
- World Health Organization . 2000. World Health Organization Disability Assessment Schedule II (WHO-DAS II). Retrieved from http://www.who.int/icidh/whodas/
- Wu, S., Renzaho, A. M. N., Hall, B. J., Shi, L., Ling, L., & Chen, W. (2021). Time-varying associations of pre-migration and post-migration stressors in refugees’ mental health during resettlement: A longitudinal study in Australia. The Lancet Psychiatry, 8(1), 36–47. doi: 10.1016/S2215-0366(20)30422-3 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author, BL. The data are not publicly available due to the de-identified data possibly containing information that could compromise the privacy and safety of the research participants.


