Abstract
Background
Epidemiologic surveillance of COVID-19 is essential to collect and analyse data to improve public health decision making during the pandemic. There are few initiatives led by public-private alliances in Colombia and Latin America. The CoVIDA project contributed with RT-PCR tests for SARS-CoV-2 in mild or asymptomatic populations in Bogotá. The present study aimed to determine the factors associated with SARS-CoV-2 infection in working adults.
Methods
COVID-19 intensified sentinel epidemiological surveillance study, from April 18, 2020, to March 29, 2021. The study included people aged 18 years or older without a history of COVID-19. Two main occupational groups were included: healthcare and essential services workers with high mobility in the city. Social, demographic, and health-related factors were collected via phone survey. Afterwards, the molecular test was conducted to detect SARS-CoV-2 infection.
Findings
From the 58,638 participants included in the study, 3,310 (5·6%) had a positive result. A positive result was associated with the age group (18-29 years) compared with participants aged 60 or older, participants living with more than three cohabitants, living with a confirmed case, having no affiliation to the health system compared to those with social health security, reporting a very low socioeconomic status compared to those with higher socioeconomic status, and having essential occupations compared to healthcare workers.
Interpretation
The CoVIDA study showed the importance of intensified epidemiological surveillance to identify groups with increased risk of infection. These groups should be prioritised in the screening, contact tracing, and vaccination strategies to mitigate the pandemic.
Funding
The CoVIDA study was funded through donors managed by the philanthropy department of Universidad de los Andes.
Keywords: SARS-CoV-2, sentinel surveillance, risk factor, socioeconomic factors, COVID-19 RT-PCR Testing, Colombia
Research in context.
Evidence before this study
Bogotá has been the city most affected by the COVID-19 pandemic in Colombia. We searched PubMed for articles aiming to investigate social, demographic, and economic factors associated with SARS-CoV-2 infection in working adults in the Latin American region. The search strategy included the following terms: "("working adult"*" OR ""latin america"" OR "latinamerica"") AND "("SARS-CoV-2 screening"*" OR "SARS-CoV-2 testing"*" OR ""COVID-19 testing"*") AND "("social condition"*" OR "socioeconomic variable"*" OR ""socioeconomic condition"*" OR ""social vulnerability"" OR ""social vulnerabilities"") AND "("SARS-CoV-2 infection"" OR ""COVID-19"" OR ""SARS-CoV-2 positivity""). Most of the studies focused on the SARS-CoV-2 infection and social vulnerability from an ecological perspective in countries like the United States and Brazil.
Added value of this study
To our knowledge, this is one of the few studies in Colombia and Latin America to show the association between the individual risk of SARS-CoV-2 infection and conditions related to sociodemographic vulnerability. We determined associated factors with the SARS-CoV-2 positive RT-PCR test in asymptomatic or mild-symptomatic working adults in the CoVIDA study during the COVID-19 pandemic in Bogotá Colombia. Factors positively associated with SARS-CoV-2 infection were age group (18 to 29 years), living with more than three cohabitants, living with a COVID-19 confirmed case, having no affiliation to the health system, reporting a very low socioeconomic status, and having essential occupations (e.g., police, military, firefighters).
Implications of all the available evidence
Evidence suggests that socioeconomic inequalities are associated with the individual risk of SARS-CoV-2 infection. The groups with increased risk of infection should be prioritised in the intensified epidemiologic surveillance, contact tracing, and vaccination strategies. This can ultimately affect public health policy decision making and, therefore, the mitigation of the pandemic.
Alt-text: Unlabelled box
1. Introduction
Over 198 million COVID-19 cases have been confirmed globally, with around 4.2 million deaths [1], as of August 2, 2021. In Latin America, one of the epicentres of the pandemic, more than 40.9 million cases have been confirmed [2], and despite strong non-pharmacological measures being implemented, the pandemic remained out of control in the largest urban centres during 2020 and the first third of 2021 [3,4]. Since the COVID-19 pandemic was declared, Colombia has had three pandemic peaks. The number of cases has continued to increase, with more than 4.9 million confirmed cases and over 120,000 deaths [5].
Bogotá is the largest most populated city in Colombia, with over 7 million inhabitants, accounting for 15% of the Colombian population (over 50 million inhabitants). Bogotá has been the most affected city by the pandemic in the country, accounting for 1 351 273 confirmed cases (29·6% of the confirmed cases in Colombia) and 25,470 deaths [6]. Geographically, Bogotá is divided into 20 localities, and the healthcare network is organised on four integrated subnets. Within these subnets, there are 40 high-complexity private hospitals and 22 high-complexity public hospitals [7].
Bogotá has a 41.8% of informal employment [8], with high mobility throughout the city [9] and some essential workers did not suspend their activities during the pandemic. These conditions can create scenarios of a higher risk of infection in this population. However, few studies have investigated the individual risk of having the SARS-CoV-2 infection and its association with social, economic, and demographic vulnerability factors [10], [11]. Identifying transmission patterns and associated factors of SARS-CoV-2 infection can contribute to implementing strategies to mitigate the pandemic in Colombia.
The CoVIDA study is an initiative led by Universidad de los Andes in Bogotá in collaboration with 71 allies in both the public and the private sectors, including the Universidad Nacional de Colombia (National University of Colombia), Secretaría Distrital de Salud de Bogotá (District Health Department of Bogotá), and Hospital Universitario Fundación Santa Fe de Bogotá (University Hospital of Fundación Santa Fe de Bogotá). Based at a private university, CoVIDA made available scientific, technical, and academic resources to support the COVID-19 epidemiologic community-based intensified sentinel surveillance and informed public health policy as the pandemic evolved in the city of Bogotá and the towns nearby. CoVIDA developed the capacity to RT-PCR test for SARS-CoV-2 and provided real-time information for local authorities and policymakers in the city.
We aimed to investigate associated factors with SARS-CoV-2 positive tests in asymptomatic or mild symptomatic working adults in the CoVIDA study during the COVID-19 pandemic in Bogotá, Colombia, April 2020 to March 2021.
2. Methods
2.1. Study Design and Sampling
The CoVIDA project was an intensified sentinel epidemiological surveillance study created in collaboration with the District Health Department of Bogotá as a complementary strategy for surveillance of COVID-19. The study included asymptomatic or mildly symptomatic people aged 18 years or older without a history of a COVID-19 positive test. The Universidad de los Andes assigned 60 000 RT-PCR tests to the CoVIDA project to amplify the testing capacity of Bogota's health department. Priority was given to two main groups working during the pandemic: (a) healthcare frontline workers and personnel from all networks of health services in Bogotá, including 14 public hospitals, seven private hospitals, health departments from six nearby towns, and two hospitals in other municipalities near Bogotá; and (b) essential services workers with high mobility in the city, including those in transportation, public markets, food stores, food delivery, construction, cleaning and other home services, education, informal occupations, police, military forces, firefighting, and the justice system. Also, the study included participants who were part of the contact tracing strategy of the CoVIDA study.
Recruitment and sampling were conducted through strategic alliances with the District Health Department of Bogotá, the District Mobility Department of Bogotá (Secretaría Distrital de Movilidad de Bogotá) and the human resources departments of allied institutions included in the study (healthcare and non-healthcare such as public/private drivers, private security, police, military among the other occupation groups). These allies were chosen based on their willingness to participate and based on their workers' occupations. These workers provided essential services during the pandemic lockdowns.
Healthcare workers were classified into two risk groups, according to the information provided by the human resources department of each allied healthcare institution: (a) high risk, including workers from intensive care units, emergency rooms, hospitalisation and other areas managing probable or confirmed COVID-19 patients; and (b) low risk, including workers with no contact with COVID-19 patients, and administrative and non-healthcare personnel. All high-risk participants were included in the study, while low-risk participants were randomly selected through simple random sampling until the sample size was completed (maximum 2000 RT-PCR tests per institution). Each of these institutions belonged to one of the four integrated subnets of the city's healthcare network. Given that these subnets had a similar number of workers, we decided to use an average estimate of workers to define the number of tests for each hospital (2000 RT-PCR).
Essential services workers with high mobility in the city were identified based on the lists provided by the human resources department from allied institutions. All participants from this group were randomly selected through simple random sampling until the sample size was completed (same number as in the healthcare workers group due to logistical reasons and to obtain an even distribution of the available tests). In this group, we also performed a public campaign to the targeted occupations through various communication channels (mass information media, social networks, and announcements in public spaces such as public transportation systems) to convene individuals to participate and attend to the CoVIDA testing sites. Also, the CoVIDA project applied a contact tracing strategy, and all the close contacts were included in the study.
Ethics approval was obtained from the ethics committee of Universidad de los Andes (2020; Approval No. 1181).
2.2. Procedures and Data Collection
Data collection started on April 18, 2020, and finished on March 29, 2021. All participants were invited via a telephone call. At enrolment, participants consented to the use of information for research and agreed to confidentiality and privacy policies and terms. After giving their informed consent, each participant completed a questionnaire via telephone about sociodemographic factors and COVID-19 preventive measures and attitudes.
For participants from the healthcare allied institutions, the healthcare staff performed nasopharyngeal swab sampling (previously trained by the CoVIDA project) within the healthcare institutions. The CoVIDA project provided testing kits. Also, nasopharyngeal swab samples transportation, molecular analyses and reporting of results was performed by the CoVIDA project.
The rest of the participants were tested through a drive-thru/walk-thru model in the case of being asymptomatic or through a home visit model to report COVID-19-related symptoms. Performance of the drive/walk-thru model implemented by the CoVIDA project was described elsewhere [12]. Testing sites were distributed across the city's healthcare network to allow maximum availability for participants (see Appendix 1). RT-PCR swab sampling was taken on average three days after the questionnaire was completed.
The RT-PCR molecular test was performed to detect SARS-CoV-2 infection according to the recommended international protocols [13] and the U-TOP™ COVID-19 detection kit (Seasun Biomaterials, Daejeon, Korea) according to the manufacturer's instructions. Participants were informed of their test results via telephone or email and provided with health recommendations. If participants tested positive, they were followed up for symptoms every 3 or 5 days for 14 days, and contact tracing (test, track, and isolate strategy) was implemented as the capacity of the CoVIDA contact centre would allow. If participants tested negative, they were followed up with for symptoms every seven days for 21 days. During follow-up, those who reported related COVID-19 symptoms were tested for a second time (see Appendix 2). Recommendations given to participants were based on national and international guidelines for COVID-19 prevention and management.
2.3. Data Analysis
The primary outcome was a positive result of the RT-PCR test for SARS-CoV-2 infection, which was used as the dependent variable. Descriptive analyses of variables were performed using 'Pearson's chi-squared test, presenting relative and absolute frequencies. Logistic regression was conducted to estimate the association between the SARS-CoV-2 infection and the individual's social and demographic factors. The risk of SARS-CoV-2 infection and associated factors was estimated using a hierarchical conceptual model with backward elimination of variables. At each level of the analysis model, the variables with a p-value ≤ 0.20 were retained in the model. In the final model, the date on which the test was taken (epidemiological week) was used as a covariate in the adjusted logistic regression model. A test for trends was performed between the positive test result and the socioeconomic strata. We performed a complete case analysis. Missing values accounted for less than 3·7% on average. Data analyses were performed using Stata software (Version 16.1) for Windows.
2.4. Role of the Funding Source
The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all data in the study and had the final responsibility for the decision to submit it for publication.
3. Results
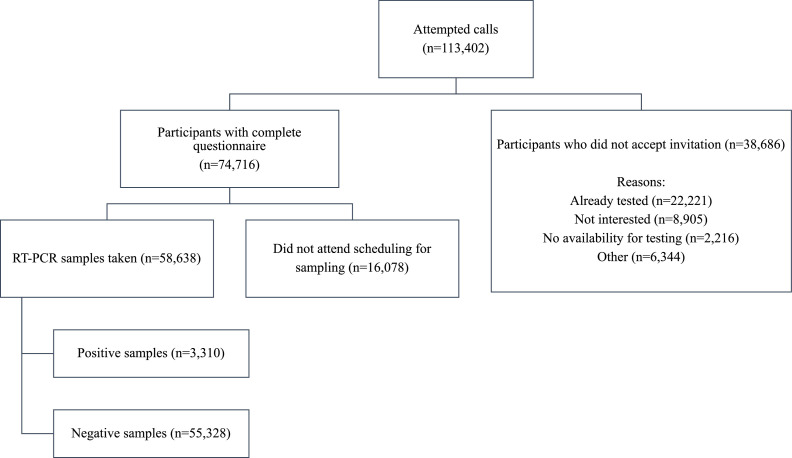
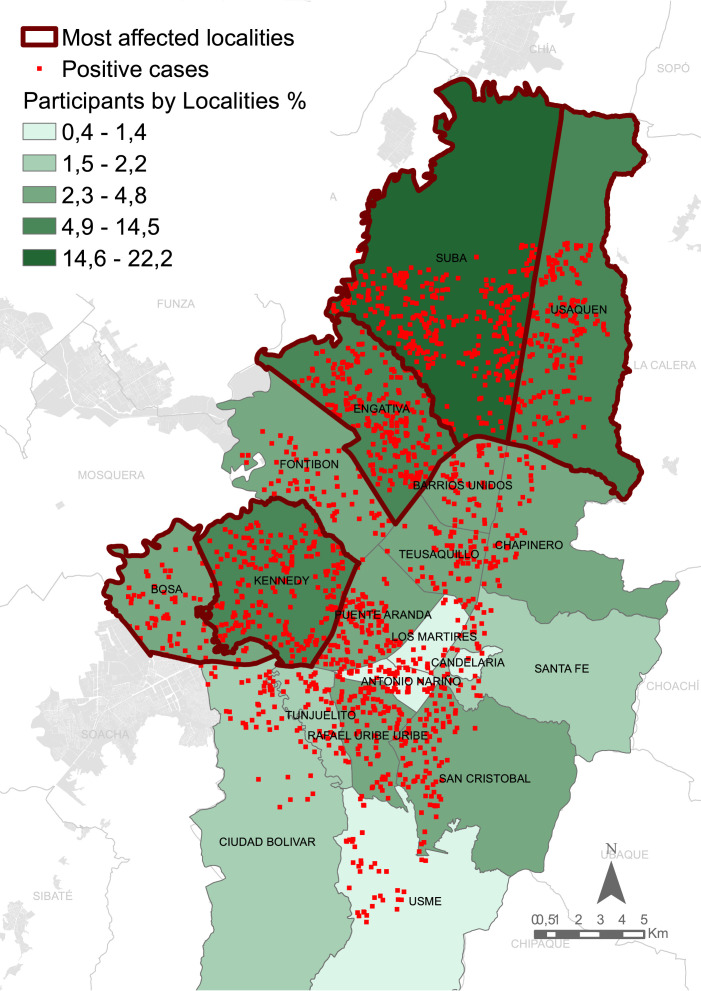
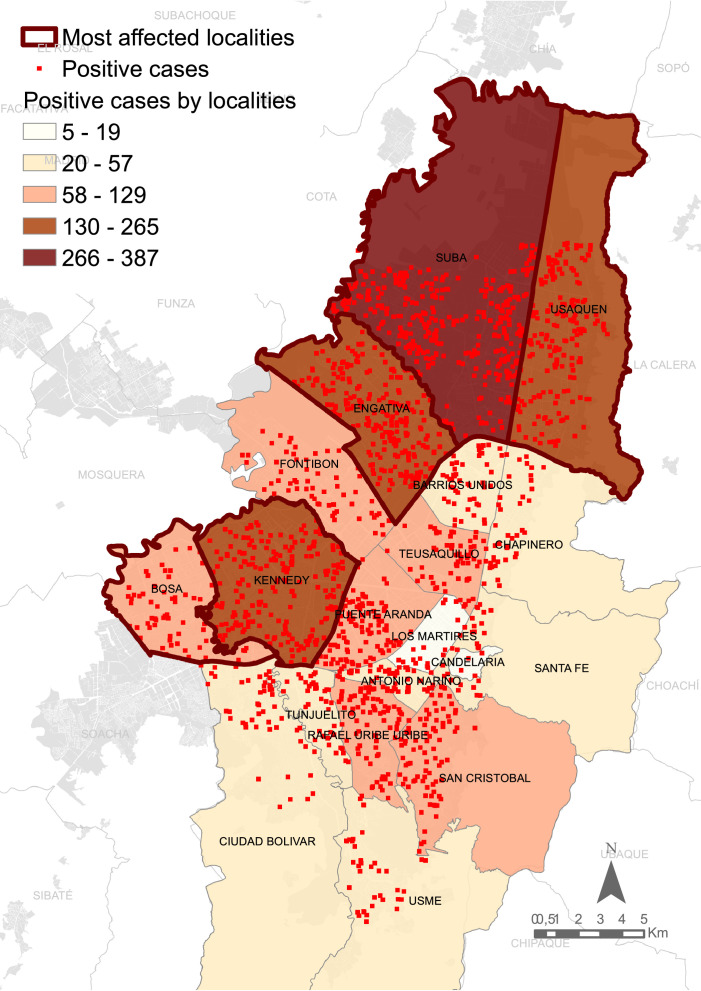
Of the 113,402 people who were initially contacted via telephone, 74,716 completed the study questionnaire. Included in the analysis were 58,638 participants who completed the questionnaire and provided the nasopharyngeal swab sample. The number of participants with a positive RT-PCR test result was 3,310 (5·6%; see Figure 1). The participants were geographically distributed homogeneously across the city (see Figure 2). The distribution of positive cases across the city is presented in Figure 3.
Figure 1.
Flowchart of participant selection and inclusion.
Figure 2.
Distribution of study participants in each locality of Bogotá, Colombia.
Figure 3.
Distribution of participants with a positive RT-PCR test result for SARS-CoV-2 infection in each locality of Bogotá, Colombia.
Table 1 shows the sociodemographic and health characteristics of individuals in the study sample. Over 60% of the participants were 30 to 59 years old (n = 35,347). The most common occupations were those in general service with contact with customers (21·6%; n = 12,665), essential office workers (19·8%; n = 11,602), and health workers (13·9%; n = 8,192). Of the total number of participants, 70·3% (n = 41,247) reported low-low to middle-low socioeconomic status.
Table 1.
Sociodemographic and Health Characteristics of the Study Sample
| SARS-CoV-2 test result | ||||||
|---|---|---|---|---|---|---|
| Negative (n = 55,328) | Positive (n = 3,310) | |||||
| n | Number | % | Number | % | pa | |
| Sociodemographic characteristics | ||||||
| Age (years) | ||||||
| 18–29 | 17,800 | 16,699 | 93·8 | 1,101 | 6·2 | <0·001 |
| 30–59 | 35,347 | 33,457 | 94·6 | 1,890 | 5·4 | |
| > 60 | 5,096 | 4,790 | 94·0 | 306 | 6·0 | |
| Sex | ||||||
| Female | 29,800 | 28,155 | 94·5 | 1,645 | 5·5 | 0·183 |
| Male | 28,812 | 27,147 | 94·2 | 1,665 | 5·8 | |
| Ethnic minority b | ||||||
| No | 57,562 | 54,303 | 94·4 | 3,259 | 5·6 | 0·194 |
| Yes | 1,076 | 1,025 | 95·3 | 51 | 4·7 | |
| Immigrant | ||||||
| No | 57,423 | 54,213 | 94·4 | 3,210 | 5·6 | <0·001 |
| Yes | 1,215 | 1,115 | 91·7 | 100 | 8·3 | |
| Use of protective elements, type of occupation, and contact with COVID-19 | ||||||
| Frequency of hand washing (times per day) | ||||||
| < 10 | 36,140 | 33,974 | 94·0 | 2,166 | 6·0 | <0·001 |
| ≥ 10 | 21,377 | 20,308 | 95·0 | 1,069 | 5·0 | |
| Duration of hand washing (seconds) | ||||||
| < 20 | 19,415 | 18,299 | 94·3 | 1,116 | 5·7 | 0·203 |
| ≥ 20 | 38,102 | 35,983 | 94·4 | 2,119 | 5·6 | |
| Use of hand sanitizer | ||||||
| Yes | 52,241 | 49,358 | 94·5 | 2,883 | 5·5 | <0·001 |
| No | 5,260 | 4,908 | 93·3 | 352 | 6·7 | |
| Use of facemask during the day | ||||||
| Always | 44,808 | 42,276 | 94·4 | 2,532 | 5·6 | <0·001 |
| Sometimes | 11,744 | 11,135 | 94·8 | 609 | 5·2 | |
| Never | 948 | 854 | 90·1 | 94 | 9·9 | |
| Number of cohabitants | ||||||
| > 3 | 23,604 | 22,025 | 93·3 | 1,579 | 6·7 | <0·001 |
| ≤ 3 | 35,034 | 33,303 | 95·1 | 1,731 | 4·9 | |
| Occupation | ||||||
| Health worker | 8,192 | 7,932 | 96·8 | 260 | 3·2 | <0·001 |
| Essential office work | 11,602 | 11,065 | 95·4 | 537 | 4·6 | |
| Police/military/firefighter | 1,623 | 1,475 | 90·9 | 148 | 9·1 | |
| Public/private driver | 4,444 | 4,171 | 93·9 | 273 | 6·1 | |
| Construction worker | 671 | 626 | 93·3 | 45 | 6·7 | |
| Contact with costumers/general service | 12,665 | 11,747 | 92·8 | 918 | 7·2 | |
| Teacher/auxiliar/student | 7,035 | 6,658 | 94·6 | 377 | 5·4 | |
| Other occupation c | 6,914 | 6,602 | 95·5 | 312 | 4·5 | |
| Informal employment/ looking for a job | 5,492 | 5,052 | 91·9 | 440 | 8·1 | |
| Use of public transportation | ||||||
| Public transport | 14,078 | 13,409 | 95·3 | 669 | 4·7 | <0·001 |
| Private transport/walking | 20,380 | 19,528 | 95·8 | 852 | 4·2 | |
| Living with a COVID-19 confirmed case | ||||||
| Yes | 4,405 | 3,883 | 88·2 | 522 | 11·8 | <0·001 |
| No | 50,627 | 48,225 | 95·3 | 2,402 | 4·7 | |
| Socioeconomic characteristics | ||||||
| Type of health care insurance | ||||||
| Contributive, special, exception | 51,385 | 48,824 | 95·0 | 2,561 | 5·0 | <0·001 |
| Subsidiary | 4,269 | 3,823 | 89·6 | 446 | 10·4 | |
| No affiliated, no determined | 2,984 | 2,681 | 89·9 | 303 | 10·1 | |
| Socioeconomic strata d | ||||||
| High | 2,239 | 2,187 | 97·7 | 52 | 2·3 | <0·001 |
| Middle-high | 3,757 | 3,651 | 97·2 | 106 | 2·8 | |
| Middle | 10,856 | 10,497 | 96·7 | 359 | 3·3 | |
| Middle-low | 24,061 | 22,636 | 94·1 | 1,425 | 5·9 | |
| Low | 14,632 | 13,644 | 93·2 | 988 | 6·8 | |
| Low-low | 2,554 | 2,245 | 87·9 | 309 | 12·1 | |
Pearson's chi-squared test. N=58,638
Ethnic groups: Indigenous, Black, Mulatto, and Gypsy.
other occupations: cooks, musicians, technicians, veterinarians, among others.
Socioeconomic strata as defined by the National Department of Statistics (DANE) of Colombia: 1 (very low strata) to 6 (high strata).
At least one COVID-19 related symptom was reported by 11·9% of participants (n = 7,006). Among these asymptomatic participants, 3·8% had a positive test result; 18·9% of symptomatic participants had a positive test result. Among those participants with a positive test result, 40·2% (n = 1,329) reported having experienced at least one COVID-19 related symptom in the last 14 days. The most common symptoms reported by the participants with a positive test were dry cough (25·0%; n = 828), sore throat (22·3%; n = 739), anosmia/dysgeusia (21·0%; n = 695), and tiredness (19·7%; n = 652; see Table 2).
Table 2.
Frequency of Symptoms Reported by the Participants With a Positive RT-PCR Test Result for SARS-CoV-2 Infection
| n | % | |
|---|---|---|
| Dry cough | 828 | 25·0 |
| Sore throat | 739 | 22·3 |
| Anosmia/dysgeusia | 695 | 21·0 |
| Tiredness | 652 | 19·7 |
| Fever | 418 | 12·6 |
| Diarrhea | 385 | 11·6 |
| Shortness of breath | 335 | 10·1 |
| At least one COVID-19 related symptom | 1,329 | 40·2 |
Table 3 presents the unadjusted and adjusted analysis of the risk of SARS-CoV-2 infection (positive RT-PCR test) in the study sample. The final analysis model showed a positive association between the SARS-CoV-2 infection and the 18 to 29 age group (OR = 1.22, 95% CI [1·05, 1·41]) compared to participants aged 60 or more, living with more than three cohabitants (OR = 1·27, 95% CI [1·17, 1·36]) compared to participants living in a household with less than three inhabitants, living with a COVID-19 confirmed case (OR = 2·21, 95% CI [1·99, 2·46]) compared to participants that did not have close contact with a COVID-19 confirmed case, having no affiliation to the health system (OR = 1·58, 95% CI [1·38, 1·82]) compared to participants affiliated to the health and social security system, and reporting low-low (OR = 3·91, 95% CI [2·86, 5·35]) or low (OR = 2·55, 95% CI [1·91, 3·40]) socioeconomic status compared to participants living in higher socioeconomic strata. The socioeconomic strata showed an inverse association with the SARS-CoV-2 infection, with lower strata having higher odds of infection. Police, military, and firefighters' occupations showed the highest odds of infection (OR = 2·27, 95% CI [1·80, 2·86]) followed by construction workers (OR = 1·90, 95% CI [1·35, 2·68]) compared to healthcare workers.
Table 3.
Logistic Regression Presenting the Crude and Adjusted Risk of SARS-CoV-2 Infection (Positive RT-PCR Test Result) for the Study sample
| Unadjusted OR | 95% CI | pa | Adjusted OR | 95% CI | pa | |
|---|---|---|---|---|---|---|
| Sociodemographic characteristics | ||||||
| Age (years) | ||||||
| 18–29 | 1·03 | [0·90, 1·17] | 0·001 | 1·22 | [1·05, 1·41] | 0·098 |
| 30–59 | 0·88 | [0·78, 1·00] | 1·06 | [0·92, 1·21] | ||
| > 60 | ·· | ·· | ·· | ·· | ||
| Prefer not to answer | 0·53 | [0·30, 0·93] | 0·40 | [0·21, 0·74] | ||
| Sex | ||||||
| Female | ·· | ·· | 0·175 | ·· | ·· | 0·305 |
| Male | 1·04 | [0·97, 1·12] | 1·01 | [0·94, 1·09] | ||
| Ethnic minority b | ||||||
| No | 1·20 | [0·91, 1·60] | 0·183 | 1·32 | [0·99, 1·77] | 0·016 |
| Yes | ·· | ·· | ·· | ·· | ||
| Immigrant | ||||||
| No | ·· | ·· | <0·001 | ·· | ·· | 0·506 |
| Yes | 1·51 | [1·23, 1·86] | 1·12 | [0·89, 1·40] | ||
| Use of protective elements, type of occupation, and contact with COVID-19 | ||||||
| Frequency of hand washing (times per day) | ||||||
| < 10 | ·· | ·· | <0·001 | ·· | ·· | 0·159 |
| ≥ 10 | 0·82 | [0·76, 0·89] | 0·99 | [0·91, 1·07] | ||
| Do not know / no answer | 1·12 | [0·88, 1·42] | 0·90 | [0·64, 1·28] | ||
| Duration of hand washing (seconds) | ||||||
| < 20 | ·· | ·· | 0·216 | ·· | ·· | 0·108 |
| ≥ 20 | 0·96 | [0·89, 1·04] | 1·05 | [0·97, 1·14] | ||
| Do not know / no answer | ·· | ·· | ·· | ·· | ||
| Use of hand sanitizer | ||||||
| Yes | 0·81 | [0·72, 0·91] | 0·001 | * | * | * |
| No | ·· | ·· | * | * | ||
| Use of facemask during the day | ||||||
| Always | 0·54 | [0·43, 0·67] | <0·001 | * | ||
| Sometimes | 0·49 | [0·39, 0·62] | * | * | ||
| Never | ·· | ·· | * | * | ||
| Number of cohabitants | ||||||
| > 3 | 1·37 | [1·28, 1·47] | <0·001 | 1·27 | [1·17, 1·36] | <0·001 |
| ≤ 3 | ·· | ·· | ·· | ·· | ||
| Occupation | ||||||
| Health worker | ·· | ·· | <0·001 | ·· | ·· | 0·004 |
| Essential office work | 1·48 | [1·27, 1·72] | 1·37 | [1·17, 1·61] | ||
| Police/military/firefighter | 3·06 | [2·48, 3·77] | 2·27 | [1·80, 2·86] | ||
| Public/private driver | 1·99 | [1·67, 2·37] | 1·43 | [1·17, 1·74] | ||
| Construction worker | 2·19 | [1·58, 3·04] | 1·90 | [1·35, 2·68] | ||
| Contact with costumers/general service | 2·38 | [2·07, 2·74] | 1·15 | [1·30, 1·77] | ||
| Teacher/auxiliar/student | 1·72 | [1·47, 2·02] | 1·13 | [0·94, 1·35] | ||
| Other occupation c | 1·44 | [1·21, 1·70] | 1·28 | [1·07, 1·52] | ||
| Informal employment/looking for a job | 2·65 | [2·27, 3·10] | 1·61 | [1·34, 1·93] | ||
| Use of public transportation | ||||||
| Public transport | 1·14 | [1·03, 1·27] | <0·001 | 1·03 | [0·92, 1·14] | <0·001 |
| Private transport/walking | ·· | ·· | ·· | ·· | ||
| Do not know / no answer | 1.83 | [1·68, 1·99] | 1·41 | [1·27, 1·56] | ||
| Living with a COVID-19 confirmed case | ||||||
| Yes | 2·69 | [2·44, 2·98] | <0·001 | 2·21 | [1·99, 2·46] | <0·001 |
| No | ·· | ·· | ·· | ·· | ||
| Do not know / no answer | 2·40 | [2·14, 2.69] | 1·21 | [1·00, 1·45] | ||
| Socioeconomic characteristics | ||||||
| Type of health care insurance | ||||||
| Contributive, special, exception | ·· | ·· | <0·001 | ·· | ·· | <0·001 |
| Subsidiary | 2·22 | [2·00, 2·47] | 1·50 | [1·33, 1·69] | ||
| No affiliated, no determined | 2·15 | [1·90, 2·44] | 1·58 | [1·38, 1·82] | ||
| Socioeconomic strata d | ||||||
| High | ·· | ·· | <0·001 | ·· | ·· | <0·001 |
| Middle-high | 1·22 | [0·87, 1·70] | 1·15 | [0·82, 1·62] | ||
| Middle | 1·43 | [1·07, 1·93] | 1·37 | [1·02, 1·85] | ||
| Middle-low | 2·64 | [2·00, 3·50] | 2·33 | [1·75, 3·09] | ||
| Low | 3·04 | [2·29, 4·04] | 2·55 | [1·91, 3·40] | ||
| Low-low | 5·78 | [4·29, 7·81] | 3·91 | [2·86, 5·35] | ||
| Do not know / no answer | 6·38 | [4·40, 9·25] | 3·23 | [2·13, 4·89] |
= Variables not retained in the final logistic regression model (p ≥ 0·20).
p value for the Wald test in the logistic regression.
Ethnic groups: Indigenous, Black, Mulatto, and Gypsy.
Other occupations: actors, cooks, musicians, technicians, veterinarians, among others.
Socioeconomic strata as defined by the National Department of Statistics (DANE) of Colombia: 1 (very low strata) to 6 (high strata).
4. Discussion
To our knowledge, this is the largest COVID-19 intensified epidemiological sentinel surveillance study carried out in Colombia among individuals with mild or no symptoms and with a high risk of infection due to their occupation. The main findings included a mean positivity rate of 3·8% among asymptomatic and 19% among participants with mild symptoms and, among the positive cases, 6 out of 10 were asymptomatic. Also, results showed (a) 22% increased odds of SARS-CoV-2 infection in participants with ages between 18 and 29 years, (b) 27% increased odds in participants living with more than three family members, (c) 58% increased odds in participants without health insurance, (d) 121% increased odds when living with a COVID-19 confirmed case, (e) 127% increased odds in police/military/firefighters and construction workers, and (f) 291% increased odds in lower socioeconomic strata, when compared to older groups, people with less than three household members, having a healthcare affiliation, not having close contact with a COVID-19 case, being a healthcare worker, and living in high socioeconomic strata, respectively.
Unlike passive epidemiological surveillance, CoVIDA adopted a risk-based approach for the active disease surveillance model implemented. Detecting asymptomatic or mild-symptomatic cases represented logistic efforts and investments of $5·4 million in U.S. Dollars from at least 71 partners and donors, which allowed for the identification of SARS-CoV-2 transmission patterns, associated factors, and social behaviour of COVID-19 in Bogotá city. The positivity rates observed in CoVIDA are like the mean rate of 18% found in Bogotá during the same period and collected through the traditional epidemiological surveillance system of the city [14]. Also, the local health authorities reported that 4 out of 10 of the cases were asymptomatic [6]. This could be explained because traditional surveillance systems focus on symptomatic people, while CoVIDA detected cases based on the risk of exposure or contagion conditions.
With the global expansion of the COVID-19 pandemic, multiple studies have addressed the epidemiological characteristics within affected populations [15], [16], [17]. The CoVIDA study mainly included participants between 30 and 59 years of age. This age distribution is related to the working population in Bogotá [18]. In this sense, the inclusion of younger participants and mild-symptomatic or asymptomatic infection is crucial in controlling the pandemic. While people older than 60 years have a worse prognosis than younger groups [19,20], the younger population may be asymptomatic and serve as a source of virus spread [21,22]. The proportion of asymptomatic infection among positive cases has been estimated between 20% and 75% [23,24]. Other studies have shown that most patients with asymptomatic disease belonged to the younger age group [25], who, according to literature, may become superspreaders and increase the risk of transmission [26], [27], [28].
Sociodemographic characteristics and socioeconomic vulnerability represent a greater risk of infection. For example, the availability and type of healthcare insurance were associated with a higher risk of SARS-CoV-2. Specifically, health insurance status remained significant after controlling for socioeconomic strata, reinforcing the importance of having a wide access to healthcare to control virus transmission. Also, having public health insurance is aligned with a higher risk than having contributive (private) or special affiliation. In the literature, it has been found that communities with higher poverty, lower-income, and lower social security coverage have shown a higher prevalence of COVID-19 [29]. Environmental factors such as living in a neighbourhood with poor air quality, insecurity related to housing, insecurity related to transportation [30], household size, low educational level [31], [32], and public social security [33] have also been associated with a higher probability of having COVID-19 at the community level. These results are consistent with our findings, where a larger household size was also positively associated with a higher risk of SARS-CoV-2 infection. Household size may be related to household transmission because physical distancing is less likely. It is more likely that one or more household member works outside the home; therefore, the risk of infection is higher [34,35]. Also, high population density in urban areas may be determinant in the probability of spreading infectious diseases such as COVID-19, as crowded conditions can increase the probability of transmission [36].
Brazil, the country with the highest inequality index in Latin America, also has the highest number of COVID-19 cases in the region. Figueiredo et al. observed that 59·8% of the variation in the incidence of COVID-19 in the country has been attributed to income inequality and a greater number of people living in a single home. These variables also explained 57·9% of the variations in mortality in the country [37]. Similarly, in Brazil, it was found that 56·2% of the municipalities with COVID-19 confirmed cases presented a very low human development index [38]. In Colombia, no study has evaluated the individual risk for COVID-19 at a large-scale level.
Nevertheless, Cifuentes et al. analysed the association between COVID-19 related mortality and socioeconomic inequalities, such as having subsidised health insurance and people living in the very low socioeconomic strata in Colombia [10]. Their results showed that socioeconomic conditions could be associated with COVID-19 related mortality. Our study is one of the few in the country to show the association between the individual risk of SARS-CoV-2 infection and conditions related to sociodemographic vulnerability [39,40].
A living systematic review of the literature showed a SARS-CoV-2 infection rate of 11% (95% CI [7, 15]) [41]. We found a positivity rate of 3% in health workers, which contrasted with a positivity rate higher than 9% in people with occupations such as police, military, and firefighters. These results could be affected by outbreaks in military training centres, where the accommodation of many people in confined spaces favours contagion. Public services-related occupations have an increased risk of SARS-CoV-2 contagion. A study conducted among the U.S. population estimated that 18% of U.S. workers are at an increased risk of exposure due to their professions. These occupations include police officers, firefighters, postal services, education, and social services [42]. We found a positive association of SARS-CoV-2 infection among occupations other than healthcare workers. Even though the healthcare workers have increased exposure to SARS-CoV-2 according to literature [43], CoVIDA found that other highly mobile occupations also increased the risk of infection. These groups have not been prioritised in the intensified epidemiologic surveillance of the city. A possible explanation for a lower risk of infection in healthcare workers is that they may have access to better training in preventive measures and more effective personal protective equipment such as N95 respirators instead of the cloth face masks that are of frequent use by the general population [44,45].
We found that living in households with more than three cohabitants and living with a COVID-19 confirmed case increased the risk of having a positive RT-PCR test result after controlling for other sociodemographic and health characteristics. These factors have been considered to be connected with the COVID-19 infection risk in previous studies [46]. A high proportion of asymptomatic infection among the young and the impact of the number of cohabitants are especially important in countries of Latin America such as Colombia. The difficulties of isolation, limited health system capacity for asymptomatic and mild cases and the high percentage of people employed under informal conditions can lead to people choosing between isolation compliance or working for survival [47,48].
Although we did not find an association between migration status and the risk of SARS-CoV-2 infection in the final model, evidence suggests that migrants are at high risk of communicable diseases due to many factors, such as living in crowded places with no healthcare access and poor socioeconomic conditions [49,50]. Indeed, a higher prevalence of COVID-19 in migrants has been observed in regions such as Spain, sub-Saharan Africa, the Caribbean, and Latin America [51]. Despite the multivariate model used by our study not showing that being an immigrant itself represented an increased risk of SARS-CoV-2 infection (once controlling for other characteristics), we observed a higher mean positivity rate in immigrants compared to non-immigrants (8·3% versus 5·6%, respectively). This finding may be considered in light of the social vulnerability conditions that immigrants are subject to, and it could be used to inform public policy-oriented to high-risk groups.
The large sample size of the present study was a strength in the context of the community sentinel surveillance strategy and data collection period, as it allowed for studying the pandemic dynamics in the city for a year. In addition, the nature of community sentinel surveillance, including institutional and community-based surveillance, confers an advantage over other epidemiological studies. The CoVIDA study contributed to screening, diagnosis, epidemiological analysis, risk communication, and the generation of new helpful knowledge for decision making in public health during the COVID-19 pandemic. Also, the inclusion of asymptomatic and mildly symptomatic participants in our study provides information regarding these groups, considering that over 75% of infections result in an asymptomatic and mild disease.
We consider the use of self-report through telephonic interviews to be among the study's limitations, as participant's responses may be susceptible to recall bias, particularly in questions asking about the previous 14 days. In addition, participants who had a negative test and within the next 21 days became infected, but never developed symptoms, were not detected as positive. This may have underestimated the positivity rate among asymptomatic participants. Although large sample size was reached, some individuals declined to participate. This may be because the CoVIDA project was performed during the two first pandemic peaks seen in Bogota. Also, restrictions on mobility were put in place by Bogota's district government to contain the pandemic spread. Targeted quarantines, high community transmission and being tested by private healthcare providers may have influenced participation in the study (see Figure 1).
The findings of the CoVIDA study are critical to inform public policy and require an urgent integration between non-pharmacologic measures, interdisciplinary and interinstitutional collaboration, especially in highly mobile populations and asymptomatic patients with COVID-19. The groups with increased risk of infection have to be prioritised in the intensified epidemiologic surveillance, contact tracing, and vaccination strategies. Likewise, the CoVIDA study experience can contribute to the design and implementation of COVID-19 epidemiological surveillance systems or for other emerging infectious diseases with the asymptomatic transmission in low- and middle-income settings worldwide. This can ultimately affect public health policy decision making and, therefore, the mitigation of the pandemic.
Contributors
Andrea Ramirez Varela (conceptualisation, methodology, project administration, writing - original draft, writing-review & editing), Luis Jorge Hernandez (conceptualisation, writing -review & editing), Guillermo Tamayo Cabeza (data curation, formal analysis, writing - original draft), Sandra Contreras Arrieta (formal analysis, writing - original draft), Silvia Restrepo Restrepo (conceptualisation, funding acquisition, resources, writing - review & editing), Rachid Laajaj (conceptualisation, writing - review & editing), Giancarlo Buitrago Gutierrez (conceptualisation, methodology, writing - review & editing), Yenny Paola Rueda Guevera (data curation, writing - original draft), Yuldor Caballero Díaz (formal analysis, writing - original draft), Martha Vives Florez (conceptualisation, funding acquisition, resources), Elkin Osorio (conceptualisation, investigation), Ignacio Sarmiento Barbieri (formal analysis, methodology), Daniela Rodríguez Sanchez (conceptualisation, investigation), Leonardo Leon Nuñez (conceptualisation, methodology, writing-review & editing), Raquel Bernal (conceptualisation, funding acquisition, resources, writing - review & editing), Sofía Ríos Oliveros (writing - review & editing), Leonardo Salas Zapata (writing -review & editing), Marcela Guevara (conceptualisation, funding acquisition, resources), Alejandro Gaviria Uribe (conceptualisation, funding acquisition, project administration, resources, supervision), Eduardo Behrentz (conceptualisation, funding acquisition, project administration, resources, supervision).
CoVIDA working group
Fernando de la Hoz
Yessica Campaz Landazabal
Marylin Hidalgo
Paola Betancourt
Pablo Rodríguez
Andrés Felipe Patiño
Jose David Pinzón Ortiz
Declaration of Interest
The authors declare no conflicts of interest.
Data sharing statement
Individual participant data that underlie the results reported in this article, after de-identification (text, tables, figures, and appendices) will be available upon reasonable request to the editorial committee of the CoVIDA project at Universidad de los Andes. Confidentiality regarding participants personal information will be held by Universidad de los Andes. The study protocol and informed consent will be available in September 2021. All analysis and reports performed on these data must be approved by Universidad de los Andes editorial committee before a peer assessment or submission. Proposals should be directed to the following emails: srestrep@uniandes.edu.co and an-rami2@uniandes.edu.co; to gain access, data requestors will need to sign a data access agreement according to the project's publication policy.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations. Appendix 3
Funding
The CoVIDA study was funded through donors managed by the philanthropy department of Universidad de los Andes.
Acknowledgements
The CoVIDA logistic group, allies, and participants.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.lana.2021.100048.
Appendix. Supplementary materials
References
- 1.Johns Hopkins University.; 2021. COVID-19 Map - Johns Hopkins Coronavirus Resource Center.https://coronavirus.jhu.edu/map.html [cited 2021 August 2]Available from. [Google Scholar]
- 2.Johns Hopkins University; 2019. Coronavirus COVID-19. [Google Scholar]
- 3.Burki T. COVID-19 in Latin America. Lancet Infect Dis. 2020;20:547–548. doi: 10.1016/S1473-3099(20)30303-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pablos-Méndez A, Vega J, Aranguren FP, Tabish H, Raviglione MC. COVID-19 in Latin America. BMJ. 2020;370:m2939. doi: 10.1136/bmj.m2939. [DOI] [PubMed] [Google Scholar]
- 5.Instituto Nacional de Salud; 2021. COVID-19 en Colombia.https://www.ins.gov.co/Noticias/Paginas/Coronavirus.aspx [cited 2021 August 2]Available from. [Google Scholar]
- 6.Secretaría de Salud de Bogotá; 2021. Casos confirmados de COVID-19 | SALUDATA.https://saludata.saludcapital.gov.co/osb/index.php/datos-de-salud/enfermedades-trasmisibles/covid19/ Available from. [Google Scholar]
- 7.Secretaría de Salud de Bogotá; 2021. Portafolio de Servicios de la Red Hospitalaria del Distrito Capital.http://www.saludcapital.gov.co/paginas2/portafoliodeserviciosdelaredhospitalariadeldc.aspx [cited 2021 July 15] Available from. [Google Scholar]
- 8.DANE; 2021. Empleo informal y seguridad social.https://www.dane.gov.co/index.php/estadisticas-por-tema/mercado-laboral/empleo-informal-y-seguridad-social [cited 2021 July 15]Avaliable from. [Google Scholar]
- 9.Secretaría de Movilidad.; 2021. La Movilidad en Datos.https://www.movilidadbogota.gov.co/web/encuesta_de_movilidad_2019 [cited 2021 July 15]Avaliable from. [Google Scholar]
- 10.Cifuentes MP, Rodriguez-Villamizar LA, Rojas-Botero ML, Alvarez-Moreno CA, Fernández-Niño JA. Socioeconomic inequalities associated with mortality for COVID-19 in Colombia: a cohort nationwide study. J Epidemiol Community Health. 2021 doi: 10.1136/jech-2020-216275. [DOI] [PubMed] [Google Scholar]
- 11.Bambra C, Riordan R, Ford J, Matthews F. The COVID-19 pandemic and health inequalities. J Epidemiol Community Health. 2020;74:964–968. doi: 10.1136/jech-2020-214401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ramirez-Varela A., Behrentz E., Tamayo-Cabeza G, Hernández L.J., Rodríguez -Feria P., Laajaj R., et al. SARS-CoV-2 Drive/Walk-Thru screening centers in Colombia: The CoVIDA project. Infectio. 2022;26(1):33–38. doi: 10.22354/in.v26i1.991. https://www.revistainfectio.org/index.php/infectio/article/view/991 [DOI] [Google Scholar]
- 13.Corman V, Bleicker T, Brünink S, Drosten C, Landt O, Koopmans M, et al. Diagnostic detection of 2019-nCoV by real-time RT-RCR. Carité Berlin. 2020;17:1–13. doi: 10.2807/1560-7917.ES.2020.25.3.2000045. [DOI] [Google Scholar]
- 14.Observatorio de Salud de Bogotá; 2021. Muestras procesadas para COVID-19 en Bogotá D.C. SALUDATA.https://saludata.saludcapital.gov.co/osb/index.php/datos-de-salud/enfermedades-trasmisibles/covid19/ [cited 2021 May 5]Available from. [Google Scholar]
- 15.Hu B, Guo H, Zhou P, Shi ZL. Characteristics of SARS-CoV-2 and COVID-19. Nat Rev Microbiol. 2021;19:141–154. doi: 10.1038/s41579-020-00459-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 17.Salzberger B, Buder F, Lampl B, Ehrenstein B, Hitzenbichler F, Holzmann T, et al. Epidemiology of SARS-CoV-2. Infection. 2021;49:233–239. doi: 10.1007/s15010-020-01531-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.DANE; 2021. Población ocupada según su actividad económica y por cuenta propia.https://www.dane.gov.co/index.php/estadisticas-por-tema/mercado-laboral/empleo-y-desempleo/poblacion-ocupada-segun-su-actividad-economica-y-por-cuenta-propia [cited 2021 July 15]Avaliable from. [Google Scholar]
- 19.Zhao Z, Chen A, Hou W, Graham JM, Haifang L, Richman PS, et al. Prediction model and risk scores of ICU admission and mortality in COVID-19. PLoS One. 2020;15:1–14. doi: 10.1371/journal.pone.0236618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sun H, Ning R, Tao Y, Yu C, Deng X, Zhao C, et al. Risk factors for mortality in 244 older adults with COVID-19 in Wuhan, China: a retrospective study. J Am Geriatr Soc. 2020;68(6):E19–E23. doi: 10.1111/jgs.16533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Han D, Li R, Han Y, Zhang R, Li J. COVID-19: Insight into the asymptomatic SARS-COV-2 infection and transmission. Int J Biol Sci. 2020;16(15):2803–2811. doi: 10.7150/ijbs.48991. doi: 10.7150/ijbs.48991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gao Z, Xu Y, Sun C, Wang X, Guo Y, Qiu S, et al. A systematic review of asymptomatic infections with COVID-19. J Microbiol Immunol Infect. 2021;54(1):12–16. doi: 10.1016/j.jmii.2020.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yanes-Lane M, Winters N, Fregonese F, Bastos M, Perlman-Arrow S, Campbell JR, et al. Proportion of asymptomatic infection among COVID-19 positive persons and their transmission potential: a systematic review and meta-analysis. PLoS One. 2020;15(11) doi: 10.1371/journal.pone.0241536. doi: 10.1371/journal.pone.0241536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Al-Sadeq DW, Nasrallah GK. The incidence of the novel coronavirus SARS-CoV-2 among asymptomatic patients: a systematic review. Int J Infect Dis. 2020;98:372–380. doi: 10.1016/j.ijid.2020.06.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kronbichler A, Kresse D, Yoon S, Lee KH, Effenberger M, Shin JI. Asymptomatic patients as a source of COVID-19 infections: A systematic review and meta-analysis. Int J Infect Dis. 2020;98:180–186. doi: 10.1016/j.ijid.2020.06.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beldomenico PM. Do superspreaders generate new superspreaders? A hypothesis to explain the propagation pattern of COVID-19. Int J Infect Dis. 2020;96:461–463. doi: 10.1016/j.ijid.2020.05.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kault D. Superspreaders, asymptomatics and COVID-19 elimination. Med J Aust. 2020;213(10):447–448. doi: 10.5694/mja2.50835. [DOI] [PubMed] [Google Scholar]
- 28.Majra D, Benson J, Pitts J, Stebbing J. SARS-CoV-2 (COVID-19) superspreader events. J Infect. 2021;82(1):36–40. doi: 10.1016/j.jinf.2020.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hawkins D. Social determinants of COVID-19 in Massachusetts, United States: an ecological study. J Prev Med Public Health. 2020;53(4):220–227. doi: 10.3961/jpmph.20.256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rozenfeld Y, Beam J, Maier H, Haggerson W, Boudreau K, Carlson J, et al. A model of disparities: risk factors associated with COVID-19 infection. Int J Equity Health. 2020;19:126. doi: 10.1186/s12939-020-01242-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Maroko AR, Nash D, Pavilonis BT. COVID-19 and inequity: a comparative spatial analysis of New York City and Chicago hot spots. J Urban Heal. 2020;97:461–470. doi: 10.1007/s11524-020-00468-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lundon DJ, Mohamed N, Lantz A, Goltz HH, Kelly BD, Tewari AK., et al. Social determinants predict outcomes in data from a multi-ethnic cohort of 20,899 patients investigated for COVID-19. Front Public Heal. 2020;8 doi: 10.3389/fpubh.571364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Baidal JW, Wang AY, Zumwalt K, Gary D, Greenberg Y, Cormack B, et al. Social determinants of health and COVID-19 among patients. New York City Res Sq. 2020 doi: 10.21203/rs.3.rs-70959/v1. published online Sept. Available from. [DOI] [Google Scholar]
- 34.Okabe-Miyamoto K, Folk D, Lyubomirsky S, Dunn EW. Changes in social connection during COVID-19 social distancing: ‘it’s not (household) size that matters, ‘it’s who ‘you’re with. PLoS One. 2021;16(1) doi: 10.1371/journal.pone.0245009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nande A, Adlam B, Sheen J, Levy MZ, Hill AL. Dynamics of COVID-19 under social distancing measures are driven by transmission network structure. PLoS Comput Biol. 2021;17(2) doi: 10.1371/journal.pcbi.1008684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wong DWS, Li Y. Spreading of COVID-19: Density matters. PLoS One. 2020;15(12) doi: 10.1371/journal.pone.0242398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Figueiredo AM, de Figueiredo DCMM, Gomes LB, Massuda A, Gil-Garcia E, de Toledo Vianna RP, et al. Social determinants of health and COVID-19 infection in Brazil: an analysis of the pandemic. Rev Bras Enferm. 2020;73 doi: 10.1590/0034-7167-2020-0673. doi: 10.1590/0034-7167-2020-0673. [DOI] [PubMed] [Google Scholar]
- 38.de Souza CDF, Machado MF, do Carmo RF. Human development, social vulnerability and COVID-19 in Brazil: a study of the social determinants of health. Infect Dis Poverty. 2020;9:124. doi: 10.1186/s40249-020-00743-x. Avaliable from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Laajaj R, De Los Rios Rueda C, Sarmiento-Barbieri I, Aristizabal D, Behrentz E, Bernal R, et al. COVID-19 spread, detection, and dynamics in Bogota, Colombia. Nat Commun. 2021;12(4726) doi: 10.1038/s41467-021-25038-z. doi: 10.1038/s41467-021-25038-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Fernández-Niño JA, Cubillos-Novella A, Bojórquez I, Rodríguez M. Recommendations for the response against COVID-19 in migratory contexts under a closed border: the case of Colombia. Biomédica. 2020;40:68–72. doi: 10.7705/biomedica.5512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gómez-Ochoa SA, Franco OH, Rojas LZ, Reguindin PF, Roa-Díaz ZM, Wyssman BM, et al. COVID-19 in healthcare workers: a living systematic review and meta-analysis of prevalence, risk factors, clinical characteristics, and outcomes. Am J Epidemiol. 2020;190(1):161–175. doi: 10.1093/aje/kwaa191. doi: 10.1093/aje/kwaa191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Baker MG, Peckham TK, Seixas NS. Estimating the burden of United States workers exposed to infection or disease: a key factor in containing risk of COVID-19 infection. PLoS One. 2020;15 doi: 10.1371/journal.pone.0232452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo C-G, Ma W, et al. Risk of COVID-19 among frontline healthcare workers and the general community: a prospective cohort study. Lancet Public Heal. 2020;5(9):e475–e483. doi: 10.1016/S2468-2667(20)30164-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chughtai AA, Seale H, MacIntyre CR. Effectiveness of cloth masks for protection against severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(10):1–5. doi: 10.3201/eid2610.200948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Qaseem A, Etxeandia-Ikobaltzeta I, Yost J, Miller MC, Abraham GM, Obley AJ, et al. Use of N95, surgical, and cloth masks to prevent COVID-19 in healthcare and community settings: living practice points from the American College of Physicians (Version 1) Ann Intern Med. 2020;173(8):642–649. doi: 10.7326/M20-3234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Liu P, McQuarrie L, Song Y, Colijn C. Modelling the impact of household size distribution on the transmission dynamics of COVID-19. Journal of the Royal Society Interface. 2021 April 28;18(177) doi: 10.1098/rsif.2021.0036. https://10.1098/rsif.2021.0036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Trade Union Congress; 2021. Covid-19 and Insecure Work.https://www.tuc.org.uk/research-analysis/reports/covid-19-and-insecure-work [cited 2021 July 15]Available from. [Google Scholar]
- 48.International Labour Organization; 2020. Impact on the labour market and income in Latin America and the Caribbean. https://www.ilo.org/wcmsp5/groups/public/americas/ro-lima/documents/publication/wcms_756697.pdf. [Google Scholar]
- 49.Tavares AM, Fronteira I, Couto I, Machado D, Viveiros M, Abecasis AB, et al. HIV and tuberculosis co-infection among migrants in Europe: a systematic review on the prevalence, incidence and mortality. PLoS One. 2017;12(9) doi: 10.1371/journal.pone.0185526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Koh D. Migrant workers and COVID-19. Occup Environ Med. 2020;77:634–636. doi: 10.1136/oemed-2020-106626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Guijarro C, Pérez-Fernández E, González-Piñeiro B, Meléndez V, Goyanes MJ, Renilla ME, et al. Riesgo de COVID-19 en españoles y migrantes de distintas zonas del mundo residentes en España en la primera oleada de la enfermedad. Rev Clínica Española. 2020;221(5):264–273. doi: 10.1016/2Fj.rce.2020.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.