Abstract
Objective
To describe rapid implementation of telehealth during the COVID-19 pandemic and assess for disparities in video visit implementation in the Appalachian region of the United States.
Methods
A retrospective cohort of consecutive patients seen in the first 4 weeks of telehealth implementation was identified from the Neurology Ambulatory Practice at a large academic medical center. Telehealth visits defaulted to video, and when unable, phone-only visits were scheduled. Patients were divided into 2 groups based on the telehealth visit type: video or phone only. Clinical variables were collected from the electronic medical record including age, sex, race, insurance status, indication for visit, and rural-urban status. Barriers to scheduling video visits were collected at the time of scheduling. Patient satisfaction was obtained by structured postvisit telephone call.
Results
Of 1,011 telehealth patient visits, 44% were video and 56% phone only. Patients who completed a video visit were younger (39.7 vs 48.4 years, p < 0.001), more likely to be female (63% vs 55%, p < 0.007), be White or Caucasian (p = 0.024), and not have Medicare or Medicaid insurance (p < 0.001). The most common barrier to scheduling video visits was technology limitations (46%). Although patients from rural and urban communities were equally likely to be scheduled for video visits, patients from rural communities were more likely to consider future telehealth visits (55% vs 42%, p = 0.05).
Conclusion
Rapid implementation of ambulatory telemedicine defaulting to video visits successfully expanded video telehealth. Emerging disparities were revealed, as older, male, Black patients with Medicare or Medicaid insurance were less likely to complete video visits.

Telestroke was established in neurology in the mid-2000s when stroke centers expanded access to acute stroke care.1-3 Since that time, telemedicine has expanded to help overcome barriers to access, transportation, and subspecialty services.4-6 Previous studies have comprehensively identified the benefits to patients including reduced travel burden, increased access to subspecialists, and others.7-9 Telehealth has been used to address health disparities and target populations not served by conventional in-person care.10-14 Significant barriers have been identified including limitations in completing a comprehensive neurologic examination via video (e.g., deep tendon reflexes and fundoscopy), technical failures, depersonalization of the provider-patient relationship, lack of infrastructure, and reimbursement challenges.4,15
The World Health Organization declared the coronavirus disease 2019 (COVID-19) pandemic on March 11, 2020. In response, national and state recommendations led to limitation of nonessential procedures, surgeries, and clinic visits as a mitigation strategy and personal protective equipment conservation measure. The Centers for Medicare and Medicaid Services (CMS) adjusted reimbursement guidelines to expand coverage for telehealth. Almost overnight, a reorganization of health care delivery occurred in the United States and other countries to accommodate physical distancing, reduce patient exposure, and limit spread.16 Expanded policy coverage permitted health systems to broaden telehealth.17 The ensuing rapid expansion of telemedicine has introduced unique challenges as well as potential barriers in care delivery.
This study aimed to describe the impact of rapid implementation of telehealth services and assess potential disparities in care delivery experienced during the integration of this new model of care after the first 1,000 patient visits.
Methods
Intervention
In response to the COVID-19 pandemic, our academic medical center implemented restrictions to nonessential ambulatory clinic visits, elective surgeries, and outpatient procedures on March 24, 2020. A rapid transition to telehealth was instituted in our large tertiary care academic neurology practice. Before this transition, an acute Telestroke service was coordinated from our department across 21 hospitals in North Carolina. Inpatient teleneurology was not offered. No billable telemedicine services were previously offered in our ambulatory clinic. On March 24, 2020, a new scheduling and clinic workflow was instituted. All ambulatory clinic visits including new and established patients were converted to telehealth visits, except for urgent visits requiring in-person examination to prevent emergency department evaluation or hospital admission. Telehealth visit scheduling defaulted to video visits primarily using the Epic platform, and a telephone visit was scheduled only if video was not possible. Ambulatory clinical staff were repurposed to telehealth delivery, with certified medical assistants (CMAs) assigned to call all patients and offer rescheduling. CMAs received standardized training on scheduling new visit types, scripting for how to discuss the process with patients, and step-by-step instructions to guide patients through technology and software needs. If a telephone visit was ultimately scheduled, CMAs recorded the reason for not being able to schedule a video visit. All providers received training in how to conduct ambulatory video visits and were provided weekly departmental telehealth conferences led by an expert in telehealth, which included topics related to obtaining consent, troubleshooting connectivity concerns, performing a teleneurology examination, documentation, and billing. Providers were given a neurology-specific SmartPhrase to document consent and offered optional one-on-one tutorials with clinician experts.
Study Design and Setting
A retrospective cohort study was designed of consecutive patients seen via telehealth in the first 4 weeks of response to the COVID-19 pandemic in the Department of Neurology Ambulatory Practice at a large academic medical center in the southeastern United States serving the Appalachian region. The department consists of 56 faculty, 17 advanced practice providers, 24 residents (in both Child and Adult Neurology), and 5 fellows. The Ambulatory Practice serves patients of all age ranges and includes specialty sections in general neurology, pediatric neurology, movement disorders, epilepsy, neuromuscular medicine, headache medicine, neuroimmunology, stroke, behavioral neurology, and sleep medicine.
Standard Protocol Approvals, Registrations, and Patient Consents
This study was approved by the institutional review board with waiver of informed consent.
Data Availability
Anonymized data will be shared by request from any qualified investigator.
Participants
Patients seen consecutively for telehealth visits during the response to the COVID-19 pandemic were identified and included in this study.
Variables
Telehealth services are defined by the CMS as visits with a provider that uses audio or video telecommunication systems, permitting real-time communication between a provider and patient located at distant sites. Both new and established patient visits were included. Video visits were defined as visits with synchronous audio and video telecommunication used for the majority of the provider-patient encounter. Telephone visits were defined as visits with synchronous audio-only telecommunication used for the majority of the provider-patient encounter. Demographic and clinical variables were collected from the electronic medical record including patient age, sex, race, insurance status, and indication for visit as determined by the subspecialty clinic assignment.
Outcomes
After visit completion, patients were contacted by telephone to assess satisfaction with telehealth. Specifically, the following were collected: (1) the type of telehealth visit (i.e., video or phone-only visit), (2) whether the telehealth visit met the patient's needs (4 = all my needs were met, 3 = some of my needs were met, 2 = a few of my needs were met, but some were not because this was a telehealth visit, and 1 = my needs were not met because this was a telehealth visit), (3) whether the patient would want a future telehealth visit (4 = I would definitely want to do a telehealth visit, 3 = I might consider a telehealth visit, 2 = I would only consider it if required, and 1 = I would not consider a future telehealth visit), and (4) qualitative feedback was collected using a scripted open-ended question (“Please share with me any general feedback including surprises, challenges, or benefits you had from seeing your neurologist through telehealth”).
Data Sources and Measurement
Data on clinical volumes were collected and curated daily, and determination of telehealth visit type was tracked in real time. Patients were divided into 2 groups based on the telehealth visit type: video visit or phone visit. Total visit volumes were determined and displayed graphically. The proportion of telehealth video visits was calculated and trended to assess the uptake rate of video visit volume. Census bureau urban-rural classification was determined using rural-urban community area (RUCA) codes (updated in 2019). Urban was defined as a metropolitan classification (coding of 1–3), whereas rural was defined as micropolitan, small town, or rural classification (coding of 4–10). Postvisit patient feedback was gathered by scripted telephone call. Answers were preferentially provided by the patient unless language or neurologic status necessitated answers from a caregiver or family member. Qualitative data were recorded in direct quotations when able and otherwise paraphrased.
Bias
Ambulatory visit type (i.e., video or phone-only visit) was collected from the medical record and confirmed daily to reduce misclassification. The previsit barrier questionnaire and postvisit satisfaction data were collected originally for clinical operations purposes and have not been validated for research purposes. Staff and providers received standardized scripting to reduce patient reporting bias.
Statistics
Statistical analysis was conducted using Stata, version 14 (StataCorp LLC, College Station, TX). Descriptive statistics were performed to determine to assess overall ambulatory clinic volume, telehealth visit volume, video visit volume, telephone visit volume, and clinical characteristics of the cohort. To compare video visit and phone visit, the Student t test was used for continuous variables, and χ2 and Fisher exact test were used for categorical variables. Significant variables (p < 0.05) based on univariate logistic regression analysis were added to a multivariable logistic regression model to identify factors independently associated with completing a video visit.
Results
Overall Cohort
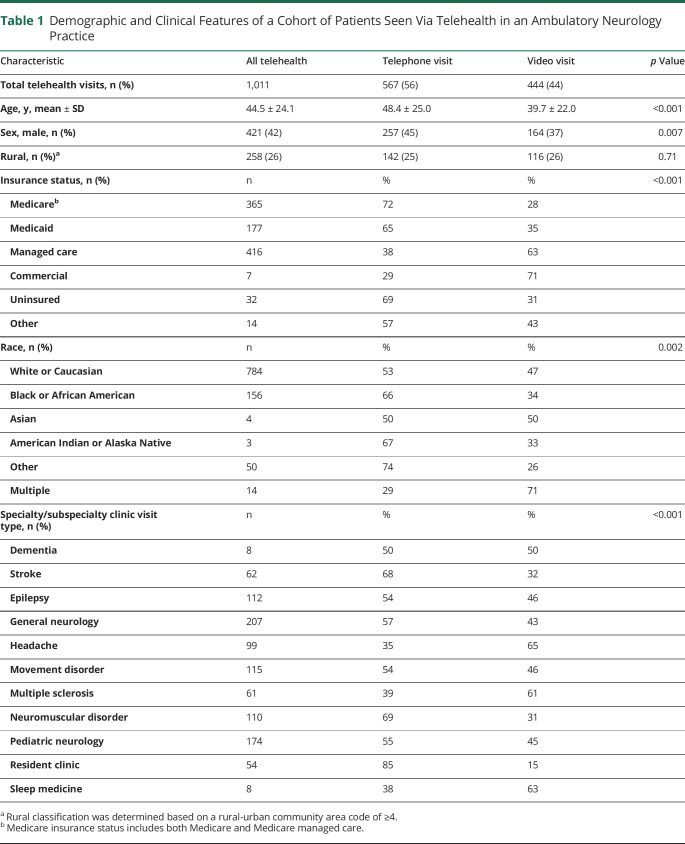
Over 1,011 telehealth patient visits were completed in the first 4 weeks of rapid implementation of ambulatory teleneurology. Patients completing telehealth visits were of mean age of 44.5 years (SD 24.1), 42% male, 78% White, 16% Black, and 26% of patients resided in a rural zip code (table 1). The most common visits were to general neurology (18%), pediatric neurology (14%), movement disorders (10%), epilepsy (10%), neuromuscular medicine (9%), headache (8%), neuroimmunology (6%), stroke (5%), and others (behavioral neurology and sleep medicine). Government insurance (e.g., Medicare, 33%; and Medicaid, 16%) and managed care insurance (37%) accounted for the majority of payers. Characteristics were comparable to patients pre-COVID, which were all in-person visits (table e-2, links.lww.com/CPJ/A186).
Table 1.
Demographic and Clinical Features of a Cohort of Patients Seen Via Telehealth in an Ambulatory Neurology Practice
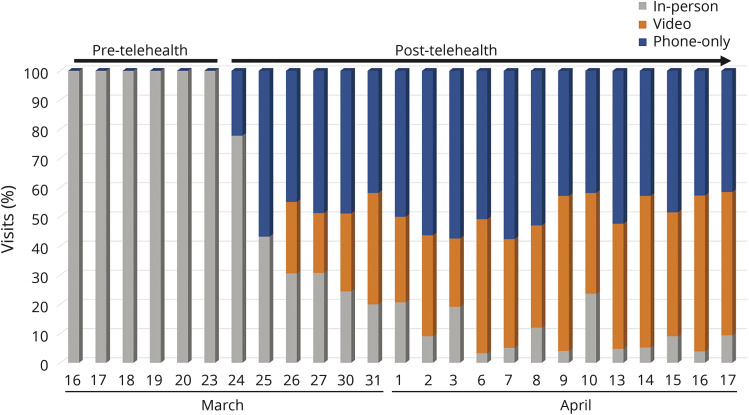
Telehealth Implementation
In-person visit volumes declined rapidly from a mean daily visits volume of 124 visits per day the month before 6.25 visits per day (range 0–14) following closure of nonessential ambulatory visits. These were urgent visits to prevent emergency department use and hospitalization. Phone visits began initially, quickly followed by escalation of video visits (figure 1). By March 26, after 3 days of instituting the standardized workflow defaulting to video visits, the rise in video and telephone visits was similar with a mean daily telehealth visit volume of 73.6 visits per day in the fourth week of implementation. The average proportion of telehealth visits over 4 weeks that were video was 47%, rising from 31% to 35% at the beginning of the program to 55% by the end of the 4-week observation period (figure e-1, links.lww.com/CPJ/A185). By the time of the 1,000th ambulatory telehealth visits, 100% of the department's providers had completed telehealth visits with an average daily visit volume at 72% of their pre-COVID levels.
Figure 1. Rise in Telehealth Services Including Video and Phone Telehealth Visits in an Ambulatory Neurology Practice.
Comparison of Video and Phone-Only Visits
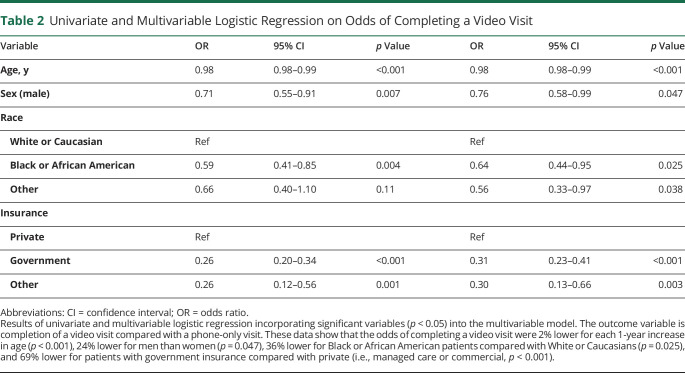
Of the first 1,011 completed telehealth visits, 44% were video visits, and 56% were phone visits (table 1). Visits initially scheduled as video visits may have been converted to telephone visit if there were concerns with connectivity. Patients who completed a video visit were younger (39.7 vs 48.4 years, p < 0.001) and more likely to be female (63% vs 55%, p < 0.007). Black or African American patients who completed a telehealth visit were more likely to use telephone, whereas White or Caucasian patients were fairly evenly split between video and telephone. Other races were not well represented in this sample. Patients with Medicare or Medicaid and uninsured patients were more likely to complete telephone-only visit (p < 0.001). Patients with commercial and managed care payers were more likely to complete a video visit. Rural patients were equally likely to complete video and telephone visits (p = 0.71). The multivariable model showed that older age (odds ratio [OR] 0.98, 95% confidence interval [CI] 0.98–0.99), male sex (OR 0.76, 95% CI 0.58–0.99), Black or African American race (OR 0.64, 95% CI 0.44–0.95), and government insurance (i.e., Medicare or Medicaid, OR 0.31, 95% CI 0.23–0.41) were independently associated with lower odds of completing a video visit (table 2).
Table 2.
Univariate and Multivariable Logistic Regression on Odds of Completing a Video Visit
Self-Reported Barriers to Video Visits
A total of 919 patients were called before their visit to schedule a telehealth visit and collect previsit data on barriers to scheduling a video visit. A voicemail was left for 189 (21%) who were not reached. Of the remaining patients (n = 730), video visits were scheduled for 43% and phone visits for 37%. The most common patient-reported barrier to scheduling a video visit was patient technology related (44% of patients), which included lack or limited access to a smartphone or home computer (n = 59), no camera for video (n = 51), no internet availability (n = 27), or other (n = 12, figure 2). Fourteen percent of patients preferred an in-person visit, whereas 9% preferred a telephone visit. Twelve percent expressed a patient barrier or concern including patient privacy due to being at work or other location that prevented video privacy (n = 15), no caregiver support (n = 13), or requesting rescheduling (n = 11). Less common barriers identified included trainee visits, which were not conducted by video (4%), language barrier requiring an interpreter (2%), provider technology error (1%), or other reason (4%). A reason was not provided for 11% of patients.
Figure 2. Self-Reported Barriers to Video Visit Adoption by Patients with Neurologic Disorders.
Patient-reported barriers were gathered by a certified medical assistant by telephone at the time of scheduling the visit. This figure demonstrates barriers to scheduling a video visit.
Patient Satisfaction
Of the 1,011 patients who were called after their visit, feedback was obtained from 276 (27%). Although there was no difference in sex, race, or urban-rural status, this group was older (47 vs 44 years, p = 0.03) and more likely to have Medicare (44% vs 33%, p < 0.007). Of these, 59% completed a telephone-only visit, 34% a video visit, and 6% reported starting with video visit converted to telephone. For all respondents, 73% reported that all clinical needs were met with the telehealth visit, 19% reported that some needs were met, 7% reported that a few needs were met, and 1% reported that their needs were not met (table 3). Patients who completed video visits were similarly likely to have all needs met compared with patients completing telephone-only visits (77% vs 71%, p = 0.34). For all respondents, 45% indicated that they would definitely consider a future telehealth visit, 28% might consider, 24% would only consider if required, and 3% would not consider a future telehealth visit. Patients who completed video visits were more likely to definitely consider a future telehealth visit compared with patients who completed a telephone-only visit (58% vs 38%, p = 0.02). A similar proportion of patients from both urban and rural communities reported that their needs were met (71% vs 80%, p = 0.27). Patients from rural communities were more likely to definitely consider a future telehealth visit compared with those from urban communities (55% vs 42%, p = 0.05). Qualitative data on patient feedback were similar to the benefits and challenges identified in the previsit barriers and are summarized in table e-1 (links.lww.com/CPJ/A186).
Table 3.
Patient Satisfaction and Feedback Collected by Telephone Call Following Completion of Video and Telephone-Only Telehealth Visits
Discussion
The expansion of telemedicine in neurology has been catalyzed by the COVID-19 pandemic. A paradigm shift has occurred in how telehealth services are incorporated into ambulatory, hospital, and other patient visits. Despite the many potential benefits of telemedicine for improving access to rural communities, this technology has the potential to widen existing health disparities, particularly in neurology where video capabilities are paramount to physical examination and patient observation. In this study, we report 2 important findings. First, rapid implementation of telemedicine services defaulting to video visits successfully expanded video telehealth. Video volumes plateaued around 50%–60% of total telehealth visits using the scripted CMA-driven video visit scheduling paradigm described here. Second, emerging disparities were revealed with older, Black, male patients with Medicare or Medicaid insurance being significantly less likely to be seen by video telecommunication.
Telemedicine offers specific advantages to patients with neurologic disease due to the presence of neurologic disability, dependence on caregivers, and transportation restrictions (e.g., epilepsy). One of the biggest potential benefits of telemedicine is expanded access to care. Telehealth has been shown to improve care in resource limited settings where there are barriers to subspecialty care and long distances to travel to see providers.18 Telemedicine, when implemented in certain settings, increases patient adherence to evidence-based guidelines, expands subspecialty services, and addresses health disparities.19 Telestroke increases access to acute care, overcomes racial and ethnic disparities, and addresses the shortage of neurologists by expanding availability of specialty care.10 However, as implementation of telehealth expands, new barriers are likely to be encountered, particularly in access to technology, availability of broadband services, and technological limitations for 2-way video conferencing that could create new disparities.20,21 In neurology as in other specialties where video capabilities are paramount to the neurologic examination, these technological barriers need to be studied, understood, and addressed.
In this study, the odds of completing a video visit were 24% lower for men than women, 36% lower for Black or African American patients compared with White or Caucasians, 69% lower for patients with government insurance, and 2% lower for each 1 year increase in age. These independent differences in video visit uptake are important in neurology. Physical observation is critical not only for the optimal care of most patients in neurology but also in establishing the provider-patient relationship and for billing services. Institutions should be aware of the disparities observed in the ability to complete video visits for older, Black, male patients with Medicare or Medicaid to understand these influences and plan appropriate resource allocation. This potential disparity could be further widened for providers, who may be unable to conduct new patient visits by telephone only, thus increasing the likelihood that patients with barriers to video visits will either be seen in person or could forego or delay a necessary evaluation. Previous studies show that men are less likely to seek care than women and are more likely to present late with more severe disease, and such barriers have the potential to accentuate this sex-based disparity.22
Older patients were more likely to experience barriers in telemedicine technology and are more likely to have government insurance, which is important for patients, health systems, and providers to recognize as reimbursement and care delivery models are determined. Before the COVID-19 pandemic, federal legislation extended coverage for telehealth in neurology through the Furthering Access to Stroke Telemedicine Act and expansion of the list of covered telehealth services by the CMS. However, broad expansion of reimbursement during COVID-19 has enabled widespread access to telehealth services, changing the way telemedicine is being implemented by health systems, used by patients, and reimbursed by payers. In this study, patients with Medicare or Medicaid insurance were 69% less likely to be seen via a video visit. Moving forward, aligning reimbursement with models of telehealth care delivery will be vital, and additional studies will be needed to investigate whether there are clinical outcome differences between telephone and video visits for appropriately selected conditions.
In this study, no difference in telehealth visit type was observed for patients in rural and urban community settings. However, differences in visit satisfaction were observed. Patients from urban and rural communities were equally likely to report that their needs were met; however, patients from rural areas were more likely to consider a future telehealth visit. One patient commented that “wait time was pretty much non-existent, not shuffled around from one waiting room to the next; sat down for 2 minutes, [provider] was there promptly and it was pretty awesome!” Patients from rural communities were more likely to consider a future telehealth visit. Many patients commented on the distance required for travel with 1 patient commenting “It's a 2-hour drive so this is much easier” and another commenting “This is the best thing in the world. It's hard to get [patient] in and out of the car, and sometimes our appointment isn't on a day that he feels like moving. We could do everything we needed with the video call.” These data support that needs of patients from urban and rural communities differ and may be met differently.
This study has several important strengths. The study incorporated consecutive ambulatory clinic visits across both general and subspecialty practices and also included pediatric patients. Data on clinical volumes were collected and curated daily, and determination of telehealth visit type was tracked in real time to avoid reliance on secondary data abstraction from large databases, enhancing the reliability of these data. The rapid integration of telehealth using a well-defined algorithm and staff scripting, with all patients contacted, and telehealth visits defaulting to video visits unless a barrier was identified, ensures that the influence of patient preference on visit type was minimal. This is confirmed by the previsit data on telehealth barriers showing patient preference as an infrequent barrier.
There are also several important limitations. Because of a statewide stay-at-home order, many visit cancellations occurred during the period of study, particularly during the first week of implementing this telehealth program. New patient visits were phased into telehealth visits as providers became comfortable with the technology. Thus, new patient visit volumes were substantially lower than pre-COVID, which could also have affected the study sample during the initiation of this program. Pre- and post-visit data were gathered on a subset of patients and may not entirely reflect the barriers encountered by all patients or providers. Patients who responded to the postvisit telephone call were similar in terms of sex, race, and urban-rural status but were older and more likely to have Medicare insurance. Demographic data were limited to those that were available in the electronic medical record. Socioeconomic data were not available and could be an important factor in access to video capabilities, internet availability, and other technology-related resources and therefore cannot exclude the possibility that the disparities identified in our research may be best explained by socioeconomic disparities. No difference in video visit uptake was observed for patients in rural vs urban communities. Although this may suggest lack of geographic disparity, urban-rural classification was determined by a RUCA code of 4 or more. Defining urban-rural status based on census data could provide a more nuanced classification.
With widespread adoption of telemedicine catalyzed by the COVID-19 pandemic, there is great potential for expansion of access to care addressing geographical, demographic, and socioeconomic barriers. However, new challenges will be faced with the way that care is delivered. Widespread adoption of telemedicine is likely to reveal new disparities that are encountered by patients. The reliance on technology is central to the delivery of telehealth care, and creative ways to overcome this barrier may be needed. Future studies are planned to explore interventions that will overcome these challenges. In this study, older, Black, male patients with government insurance were less likely to be seen for a video visit. This highlights the need for providers and health systems to monitor implementation of telemedicine services and proactively address systematic barriers in care delivery.
Appendix. Authors

Study Funding
No targeted funding reported.
Disclosure
Roy E. Strowd serves a consultant for Monteris Medical Inc, Novocure, and Nanobiotix; he receives an editorial stipend as Section Editor of the Resident and Fellow Section of Neurology® and has received research/grant support from the American Academy of Neurology, American Society for Clinical Oncology, Southeastern Brain Tumor Foundation, and Jazz Pharmaceuticals. Lauren Strauss, Rachel Graham, Kristen Dodenhoff, Allysen Schreiber, Sharon Thomson, Alexander Ambrosini, Annie Madeline Thurman, Carly Olszewski, and L. Daniela Smith report no disclosures or conflicts of interest relevant to this manuscript. Michael Cartwright received royalties from Elsevier for the textbook Neuromuscular Ultrasound. Amy Guzik reports no disclosures or conflicts of interest relevant to this manuscript. Rebecca Erwin Wells is funded by NIH grant K23AT008406-05. Heidi Munger Clary is funded by NIH grant 2KL2TR001421-05. John Malone and Mustapha Ezzeddine report no disclosures or conflicts of interest relevant to this manuscript. Pamela W. Duncan is funded by NIH grant U24NS107197-02. Charles H. Tegeler reports no disclosures or conflicts of interest relevant to this manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Schwamm LH, Holloway RG, Amarenco P, et al. A review of the evidence for the use of telemedicine within stroke systems of care: a scientific statement from the American Heart Association/American Stroke Association. Stroke 2009;40:2616–2634. [DOI] [PubMed] [Google Scholar]
- 2.Powers WJ, Rabinstein AA, Ackerson T, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Atroke Association. Stroke 2018;49:e46–e110. [DOI] [PubMed] [Google Scholar]
- 3.Adeoye O, Nyström KV, Yavagal DR, et al. Recommendations for the establishment of stroke systems of care: a 2019 update: a policy statement from the American Atroke Association. Stroke 2019;50:e187–e210. [DOI] [PubMed] [Google Scholar]
- 4.Hatcher-Martin JM, Adams JL, Anderson ER, et al. Telemedicine in neurology: Telemedicine Work Group of the American Academy of Neurology update. Neurology 2020;94:30–38. [DOI] [PubMed] [Google Scholar]
- 5.Guzik AK, Switzer JA. Teleneurology is neurology. Neurology 2020;94:16–17. [DOI] [PubMed] [Google Scholar]
- 6.George BP, Reminick JI, Scoglio NJ, et al. Telemedicine in leading US neurology departments. Neurohospitalist 2012;2:123–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kruse CS, Krowski N, Rodriguez B, Tran L, Vela J, Brooks M. Telehealth and patient satisfaction: a systematic review and narrative analysis. BMJ Open 2017;7:e016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wechsler LR, Tsao JW, Levine SR, et al. Teleneurology applications: report of the telemedicine work group of the American Academy of Neurology. Neurology 2013;80:670–676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wechsler LR. Advantages and limitations of teleneurology. JAMA Neurol 2015;72:349–354. [DOI] [PubMed] [Google Scholar]
- 10.Lyerly MJ, Wu TC, Mullen MT, et al. The effects of telemedicine on racial and ethnic disparities in access to acute stroke care. J Telemed Telecare 2016;22:114–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khairat S, Haithcoat T, Liu S, et al. Advancing health equity and access using telemedicine: a geospatial assessment. J Am Med Inform Assoc 2019;26:796–805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leath B, Dunn LW, Alsobrook A, Darden ML. Enhancing rural population health care access and outcomes through the Telehealth EcoSystem model. Online J Public Health Inform 2018;10:e218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Marcin JP, Shaikh U, Steinhorn RH. Addressing health disparities in rural communities using telehealth. Pediatr Res 2016;79:169–176. [DOI] [PubMed] [Google Scholar]
- 14.Sauers-Ford HS, Marcin JP, Underwood MA, et al. The use of telemedicine to address disparities in access to specialist care for neonates. Telemed J E Health 2019;25:775–780. [DOI] [PubMed] [Google Scholar]
- 15.Hassan A, Dorsey ER, Goetz CG, et al. Telemedicine use for movement disorders: a global survey. Telemed J E Health 2018;24:979–992. [DOI] [PubMed] [Google Scholar]
- 16.Mann DM, Chen J, Chunara R, Testa PA, Nov O, Mann D. COVID-19 transforms health care through telemedicine: evidence from the field. J Am Med Inform Assoc Epub 2020 Apr 20. doi: 10.1093/jamia/ocaa072/5824298. [DOI] [PMC free article] [PubMed]
- 17.Hollander JE, Carr BG. Virtually perfect? Telemedicine for COVID-19. N Engl J Med 2020;382:1679–1681. [DOI] [PubMed] [Google Scholar]
- 18.Ray KN, Demirci JR, Bogen DL, Mehrotra A, Miller E. Optimizing telehealth strategies for subspecialty care: recommendations from rural pediatricians. Telemed J E Health 2015;21:622–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nelson EL, Duncan AB, Peacock G, Bui T. Telemedicine and adherence to national guidelines for ADHD evaluation: a case study. Psychol Serv 2012;9:293–297. [DOI] [PubMed] [Google Scholar]
- 20.Wilcock AD, Rose S, Busch AB, et al. Association between broadband internet availability and telemedicine use. JAMA Intern Med 2019;179:1580–1582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Drake C, Zhang Y, Chaiyachati KH, Polsky D. The limitations of poor broadband internet access for telemedicine use in rural America: an observational study. Ann Intern Med 2019;171:382–384. [DOI] [PubMed] [Google Scholar]
- 22.Wang Y, Hunt K, Nazareth I, Freemantle N, Petersen I. Do men consult less than women? An analysis of routinely collected UK general practice data. BMJ Open 2013;3:e003320. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Anonymized data will be shared by request from any qualified investigator.