Abstract
Objective
To update data for diagnostic accuracy of a clinical diagnosis of Parkinson disease (PD) using neuropathologic diagnosis as the gold standard.
Methods
Data from the Arizona Study of Aging and Neurodegenerative Disorders (AZSAND) were used to determine the predictive value of a clinical PD diagnosis. Two clinical diagnostic confidence levels were used, possible PD (PossPD, never treated or not responsive) and probable PD (ProbPD, 2/3 cardinal clinical signs and responsive to dopaminergic medications). Neuropathologic diagnosis was the gold standard.
Results
Based on the first visit to AZSAND, 15/54 (27.8%) PossPD participants and 138/163 (84.7%) ProbPD participants had confirmed PD. PD was confirmed in 24/34 (70.6%) ProbPD with <5 years and 114/128 (89.1%) with ≥5 years disease duration. Using the consensus final clinical diagnosis following death, 161/187 (86.1%) ProbPD had neuropathologically confirmed PD. Diagnostic accuracy for ProbPD improved if included motor fluctuations, dyskinesias, and hyposmia, and hyposmia for PossPD.
Conclusions
This updated study confirmed lower clinical diagnostic accuracy for elderly, untreated or poorly responsive PossPD participants and for ProbPD with <5 years of disease duration, even when medication responsive. Caution continues to be needed when interpreting clinical studies of PD, especially studies of early disease, that do not have autopsy confirmation.
Classification of Evidence
This study provides Class II evidence that a clinical diagnosis of ProbPD at the first visit identifies participants who will have pathologically confirmed PD with a sensitivity of 82.6% and a specificity of 86.0%.
An accurate clinical diagnosis of Parkinson disease (PD) is critical for patient care and research. Given the lack of a definitive biomarker, the gold standard remains neuropathologic confirmation. Numerous studies report that neuropathologic confirmation of a clinical diagnosis of PD may range from 65% to 93% depending on the criteria used and the stage of disease.1–6 A review of this topic and its importance was recently published.7
Previous analysis of the Arizona Study of Aging and Neurodegenerative Disorders (AZSAND) data set revealed that at the first AZSAND visit, there was a diagnostic accuracy of 26% for participants with clinically possible PD (PossPD, 2/3 clinical signs but either never treated or not clearly responsive to dopaminergic treatment), 53% for probable PD (ProbPD) of <5 years of duration (ProbPD, 2/3 clinical signs and responsive to dopaminergic treatment), and 88% for ProbPD with ≥5 years of duration.8 Even using the final consensus clinical diagnosis of ProbPD following death, combining all previous examination data and chart review, the diagnostic accuracy was only 85%.8 The objective of the current study was to update the previous AZSAND results8 with a larger cohort of participants.
Methods
Participants
Participants enrolled from 1997 to 2019, an additional 6 years of data, in an ongoing longitudinal clinical-neuropathologic study, AZSAND,9 with autopsies performed by the Banner Sun Health Research Institute Brain and Body Donation Program (brainandbodydonationprogram.org), were included.
Standard Protocol Approvals, Registrations, and Patient Consents
All participants signed written informed consent approved by the Banner Health Institutional Review Board (IRB) or Western IRB.
Clinical Assessments
Participants received annual standardized movement disorder examinations by a fellowship-trained movement disorders specialist as previously described.10,11 Examinations included a full Unified Parkinson Disease Rating Scale (UPDRS) (performed in the practically defined off state whenever possible),12 medication history, and neuropsychological test battery.11 Olfactory testing, using the University of Pennsylvania Smell Identification Test (UPSIT), began in 2005, and data were used if they could be linked to the first visit within 2 years.13,14
At each assessment, participants were evaluated for one or more of the cardinal signs of PD: rest tremor, a UPDRS motor score of ≥1 for the lower lip or any limb; bradykinesia, a UPDRS motor score of ≥1 in 2 motor tests on the same side of the body (arm/leg) or a score of ≥2 in 1 motor test of a limb; and cogwheel rigidity, a UPDRS motor score of ≥1 of any limb. Following each evaluation, participants were given a movement disorders diagnosis: (1) ProbPD: 2 of 3 cardinal signs, no symptomatic cause, improvement when treated with dopaminergic medications and continued response if still being treated, or if lack of current response, an explanation for why treatment was no longer working (i.e., inadequate dose due to side effects); (2) PossPD: 2 of 3 cardinal signs, no symptomatic cause, symptoms or signs present for ≤5 years, dopaminergic treatment had not been tried, or an adequate trial had not clearly occurred (i.e., too low a dose and side effects that limited therapeutic dose); (3) progressive supranuclear palsy (PSP): meeting the National Institute of Neurological Disorders and Stroke-PSP clinical criteria15 for diagnosis; (4) parkinsonism nonspecific (ParkNOS): parkinsonism without response to an adequate dose of dopaminergic medication or disease duration of >5 years and had not been treated or been given an adequate trial of dopaminergic treatment or appeared to have another etiology including an unclear neurodegenerative condition, dementia with parkinsonian features, or secondary parkinsonism; and (5) multiple system atrophy (MSA): autonomic dysfunction with or without parkinsonism poorly responsive to medication and/or cerebellar findings. At the time of death, all available medical records were reviewed, and a final consensus clinical diagnosis was given. Although newer Movement Disorders Society clinical diagnostic criteria for PD were published in 2015, the present study was begun in 1997, and the database does not have sufficient data for many of the variables to use the new criteria.16 Participants with a clear secondary cause for clinical findings, such as stroke, arthritis, and other joint disease, were not included as they would not be diagnosed as having parkinsonism.
Neuropathologic Assessments
The postmortem diagnosis of PD was made based on previously reported neuropathologic criteria together with a clinical diagnosis of parkinsonism.17–20 This included participants with a clinical diagnosis of ProbPD, PossPD, or any other forms of parkinsonism with neuropathologic evidence of substantia nigra pigmented neuron loss and Lewy bodies. Gross and microscopic neuropathologic assessments were made by a single observer (T.G.B.) initially blinded to clinical history or clinical diagnosis and then able to review clinical information to make an appropriate clinical-neuropathologic diagnosis. Paraffin sections of multiple brain regions were stained with H&E and an immunohistochemical method for pathologic α-synuclein deposits using a polyclonal antibody raised against an α-synuclein peptide fragment phosphorylated at serine 129, after epitope exposure with proteinase K, to identify Lewy bodies and related neurite pathology.18,21–24 Histologic evaluation of substantia nigra pigmented neuron loss was graded using H&E-stained microscopic sections.18
Statistical Analysis
Diagnostic accuracy was assessed for the clinical diagnosis at the first visit and for the final clinical diagnosis at the time of death. The sample included all participants with ProbPD, PossPD, or other types of parkinsonism at the given time point. Positive predictive value (PPV) was the percentage of participants with neuropathologically confirmed PD among those with the given clinical diagnosis. Negative predictive value (NPV) was the percentage of participants with other clinical findings of parkinsonism, not PossPD or ProbPD, who did not have neuropathologically confirmed PD. Sensitivity was the percentage of participants with a clinical diagnosis of PD among those with neuropathologically confirmed PD, and specificity was the percentage of participants without a clinical diagnosis of PD among those without neuropathologically confirmed PD. Mean UPSIT scores were compared between groups by using the 2-sample t test. UPSIT cutoff scores were chosen to maximize the Youden index (sensitivity + specificity − 1). Proportions were compared among groups by using the Pearson χ2 test. The Fisher exact test was used instead of the Pearson χ2 test if the minimum expected cell count was less than 5. The primary research question was to determine the diagnostic accuracy of a clinical diagnosis of PossPD or ProbPD using neuropathologic assessment as the reference standard, and the level of evidence was Class II.
Data Availability
Data are available at brainandbodydonationprogram.org.
Results
Demographics
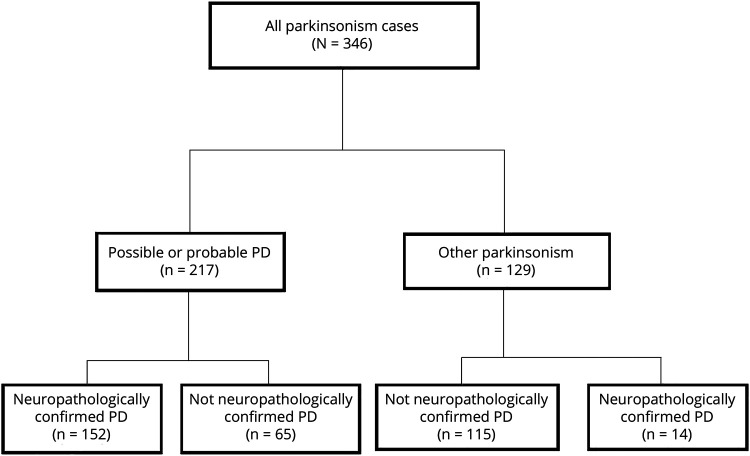
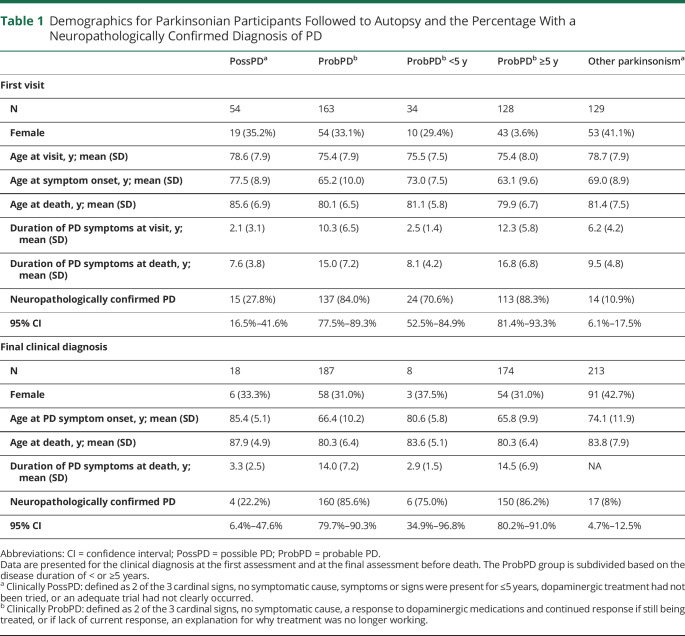
At the time of the first visit, there were 346 participants of parkinsonism, 163 participants had ProbPD, 54 had PossPD, and 129 had other types of parkinsonism (figure). Age, sex, and disease duration at the first visit and time of death are presented in table 1. When ProbPD was subdivided by disease duration, those with disease duration <5 years had an older age at disease onset (mean 73.0 years) than those with a disease duration of ≥5 years (mean 63.1 years), although age at death was no different (table 1). The PossPD participants had shorter disease duration (mean 2.1 years) than the ProbPD group at the first visit and an older age at onset (77.5 years) and age at death (85.6 years) (table 1).
Figure. Flowchart of the Clinical Categorization and Then the Neuropathologic Diagnostic Category for All the Parkinsonian Participants Included in This Study.
Table 1.
Demographics for Parkinsonian Participants Followed to Autopsy and the Percentage With a Neuropathologically Confirmed Diagnosis of PD
Predictive Value for a Diagnosis of PossPD
For the PossPD participants (most of whom had never received treatment) at the first visit, only 15/54 (27.8%) had neuropathologically confirmed PD (table 1). Of the 18 with PossPD as the final consensus diagnosis at the time of death, 4 (22.2%) had PD.
Predictive Value for ProbPD
For those with ProbPD at the first visit, 138/163 (84.7%) had neuropathologically confirmed PD. For the ProbPD participants with disease duration <5 years at the first visit, and 24/34 (PPV 70.6%) had neuropathologically confirmed PD (table 1). For ProbPD with disease duration ≥5 years, 114/128 (PPV 89.1%) had neuropathologically confirmed PD. Using the final clinical diagnosis of ProbPD at the time of death, there were only 6/8 (75%) participants with disease duration <5 years and 86.8% (151/174) for disease duration ≥5 years.
Using a disease duration at the first visit of <3 years, 14/21 (66.7%) had neuropathologically confirmed PD, and for disease duration of <2 years, 10/14 (71.4%) had neuropathologically confirmed PD.
Predictive Value Based on Clinical Signs
For those with ProbPD at the first visit, rest tremor, asymmetric onset, persistent asymmetry, and having all 3 cardinal features of PD did not improve diagnostic accuracy (data not shown). Diagnostic accuracy was improved in those having motor fluctuations (74/79, 93.7% with vs 62/80, 77.5% without) and dyskinesias (45/47, 95.7% with vs 90/111, 81.1% without). None of the clinical signs improved diagnostic accuracy for the PossPD group (data not shown).
Olfactory Testing and Diagnostic Accuracy
Of the 17 PossPD participants that had an UPSIT within the first 2 years of the first visit, the mean UPSIT score for the 6 participants with autopsy-confirmed PD was 14.0, and it was 27.7 for the 11 that did not have PD (p < 0 .001) (table 2). Based on the Youden index using a cutoff score of 22, 5/6 (83.3%) PossPD participants below the cutoff had path confirmed PD compared with 2/11 (18.2%) that did not have PD (p = 0.035). One of the 2 had a neuropathologic diagnosis of PSP and the other MSA.
Table 2.
UPSIT Scores for Participants Who Did and Those Who Did Not Have Neuropathologically Confirmed PD
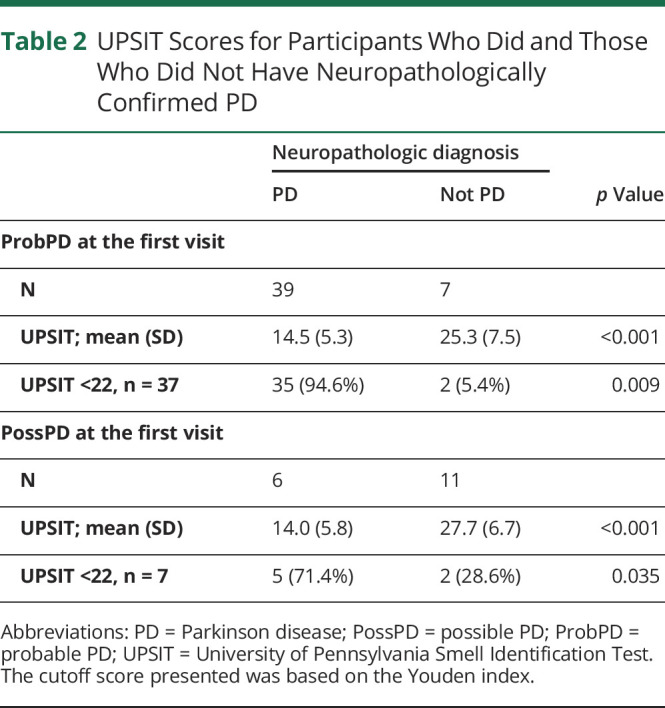
Of ProbPD participants at the first visit with UPSIT testing, those with neuropathologically confirmed PD had significantly lower UPSIT scores (14.5 vs 25.3) (p < 0.001) (table 2). Using an UPSIT cutoff of <22, 35/39 (89.7%) with UPSIT below the cutoff had pathologically confirmed PD, whereas 2/7 (28.6%) (p = 0.002) below the cutoff did not have PD (table 2). Both participants that did not have PD had Alzheimer disease (AD).
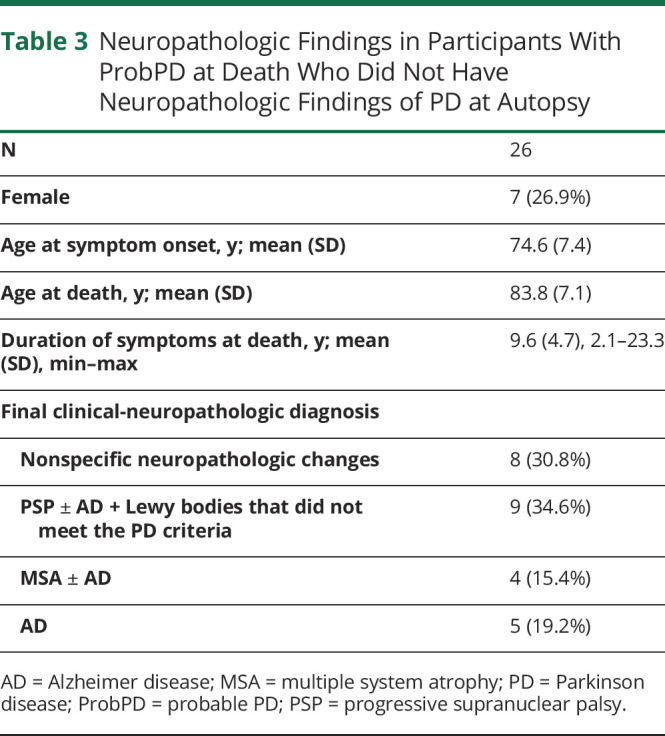
ProbPD Participants Without Neuropathologically Confirmed PD
There were 26/187 (13.9%) ProbPD participants at the time of death that did not have neuropathologically confirmed PD (table 3). The mean age at symptom onset and the mean age at death were higher for those cases that did not have neuropathologically confirmed PD (tables 1 and 3). Nine had PSP (with or without other neuropathologic findings), 4 had MSA, 3 had just AD, and 10 had no clear neuropathologic/neurodegenerative findings to explain the parkinsonism.
Table 3.
Neuropathologic Findings in Participants With ProbPD at Death Who Did Not Have Neuropathologic Findings of PD at Autopsy
Sensitivity and Specificity: Clinical Diagnosis in Pathologically Proven PD
There were 182 participants with a final clinical-neuropathologic diagnosis of PD (table 4). The sensitivity for the clinical diagnosis of ProbPD was 161/182 (88.5%). There were 22 participants with a final clinical diagnosis with PSP, and 6 actually had a neuropathologic diagnosis of PD. A final clinical diagnosis of ParkNOS (most of whom had dementia) was given to 165 participants, of whom 11 met the neuropathologic criteria for PD.
Table 4.
Demographics and Clinical Diagnoses for Participants With and Without Neuropathologically Confirmed PD
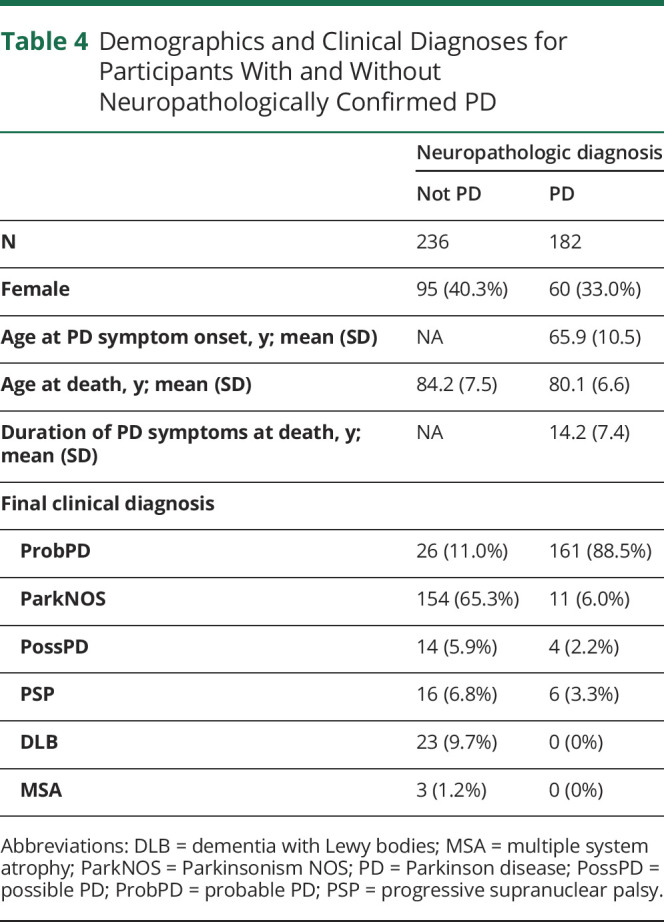
Therefore, the specificity for a final clinical diagnosis of ProbPD was 89.0% as 26/236 participants who did not have a clinical diagnosis of ProbPD had neuropathologically confirmed PD (table 4).
Negative Predictive Value of a Clinical Diagnosis of Other Parkinsonism
Of the 129 participants with other types of parkinsonism (i.e., PSP, MSA, and ParkNOS) at the first visit, 115 did not have neuropathologically confirmed PD (NPV 89.1%, table 1). Similar NPV was found for a final clinical diagnosis of parkinsonism (196/213, 92.0%).
Discussion
These updated data continue to show that early in the course of a parkinsonian disorder, clinical diagnosis of PossPD and ProbPD, even if the participant is responsive to dopaminergic medication, is not very accurate. These data build on our own previously published data8 and now represent the largest neuropathologically confirmed series of prospectively evaluated participants having had both movement disorder and cognitive assessments. These data also improve on previously published clinical-neuropathologic correlation studies showing that appreciable numbers of participants diagnosed with PD during life, especially those for whom signs and symptoms have been present for less than 5 years, do not have neuropathologically confirmed PD.1–6,25 These data are critical as many biomarker and disease-modifying treatment studies, especially in early PD, do not have pathologic confirmation.
The diagnostic inaccuracy has the potential of severely compromising the likelihood of observing an adequate effect size in a trial. This inaccuracy was present despite a strength of this study being that all participants had been examined by a small group of movement disorder specialists, as opposed to many neurologists and geriatricians that examined the participants in other studies.2 For ProbPD participants who had ≥5 years of disease duration, diagnostic accuracy improved to 88.3%. A disease duration of >5 years was also found to be key to making the correct clinical diagnosis in an earlier study.1 In that study of 43 patients initially diagnosed as PD, only 28 (65%) had neuropathologically confirmed PD.1 After a mean follow-up period of 12 years, 41 had a clinical diagnosis of PD at the final visit before death, and 31 (76%) had PD pathologically.1
In a study of 100 clinically diagnosed PD participants,2 76 had neuropathologically confirmed PD. Accuracy improved to 82% (73/89) with retrospective application of diagnostic criteria5 that included response to levodopa and >10 years of disease course.26
The present data clearly showed that as expected, the presence of motor fluctuations (92.4% PPV at the first visit) or dyskinesia (93.6% PPV at the first visit) improved diagnostic accuracy. That is not surprising as fluctuations and dyskinesia help determine responsiveness to dopaminergic medication. However, in participants responsive to dopaminergic medications yet having disease duration <5 years, the PPV was only 70.6%. Although the sample size was small (n = 34), this finding supports a previous report that participants with other forms of parkinsonism may respond to dopaminergic medications early in the disease course.27
Hyposmia has been linked to PD,13,14 and although the study sample was small, this study demonstrates that low UPSIT scores significantly improve the PPV. The value of the UPSIT may be greatest in early disease duration patients especially in patients with PossPD as 5/6 PossPD participants with an UPSIT <22 had PD, whereas only 2/11 participants without neuropathologically confirmed PD had a score of <22.
A major limitation to this study, and the previous study,8 was the age of the PossPD participants. The mean age at disease onset for the ProbPD group was 65.2 years, and mean age at death was 80.1 years, suggesting the ProbPD participants in AZSAND are similar to what has been reported in other studies28,29 including 1 previously discussed above26 (PD onset 64.5 years, age at death 76.5 years). However, when looking at both the ProbPD with disease duration <5 years or the PossPD groups, their mean ages at disease onset were older (ProbPD <5 years was 75.5, and PossPD was 77.5) than the ProbPD ≥5 years (63.1). These participants are clearly older than would be expected in research studies of early PD. Whether a diagnosis of PossPD or early ProbPD in a younger cohort would have a similarly lower diagnostic accuracy cannot be determined from AZSAND data, this despite adding 20 PossPD and 19 ProbPD having <5 years disease duration since the data were previously published.8 It is possible that some of these participants had bradykinesia related to other medical issues, such as arthritis (although the examining physicians all take this into account) or that the research diagnosis of PossPD was too lenient. Unfortunately, recruiting younger PossPD and ProbPD with <5 years of disease duration to enter into the AZSAND program has been difficult and would require more decades to follow-up to autopsy. Another limitation is the lack of neuroimaging as part of AZSAND. Although this might improve diagnostic accuracy slightly, most of the participants that did not have neuropathologically confirmed PD did have another neurodegenerative disorder that likely would have had abnormal neuroimaging and thus not have improved accuracy significantly.
In summary, diagnostic accuracy of a first visit clinical diagnosis of PD (both PossPD and ProbPD) varies between 27.8% and 88.3%, with shorter duration of disease and participants who have never been treated or do not have a clear response to dopaminergic medication having lower diagnostic accuracy. Overall, the sensitivity for an initial diagnosis of ProbPD was 82.5%, and the specificity was 85.6% at first visit and 85.6% and 88.6% at death. As clinical research studies attempt to find the earliest possible biomarkers for PD and early, disease-modifying treatments for PD, the low diagnostic accuracy at this stage needs to be addressed and will continue to be a critical impediment until autopsy-verified or diagnostic biomarkers are developed.
Acknowledgment
The authors are grateful to the participants who have volunteered to participate in the Banner Sun Health Research Institute Brain and Body Donation Program. They thank Mr. Bruce Peterson for developing and maintaining the database.
Appendix. Authors
Footnotes
Class of Evidence: NPub.org/coe
Study Funding
This study was funded by the National Institute of Neurological Disorders and Stroke (U24 NS072026 National Brain and Tissue Resource for Parkinson's Disease and Related Disorders), the National Institute on Aging (P30 AG19610 Arizona Alzheimer's Disease Core Center), the Arizona Department of Health Services (contract 211002, Arizona Alzheimer's Research Center), the Arizona Biomedical Research Commission (contracts 4001, 0011, 05-901, and 1001 to the Arizona Parkinson's Disease Consortium), the Michael J. Fox Foundation for Parkinson's Research, and the Mayo Clinic Foundation.
Disclosure
The authors report no disclosures relevant to the manuscript. Full disclosure form information provided by the authors is available with the full text of this article at Neurology.org/cp.
References
- 1.Rajput AH, Rozdilsky B, Rajput A. Accuracy of clinical diagnosis in parkinsonism: a prospective study. Can J Neurol Sci 1991;18:275–278. [DOI] [PubMed] [Google Scholar]
- 2.Hughes AJ, Daniel SE, Kilford L, Lees AJ. The accuracy of the clinical diagnosis of Parkinson's disease: a clinicopathological study of 100 cases. J Neurol Neurosurg Psychiatry 1992;55:181–184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hughes AJ, Daniel SE, Blankson S, Lees AJ. A clinicopathologic study of 100 cases of Parkinson's disease. Arch Neurol 1993;50:140–148. [DOI] [PubMed] [Google Scholar]
- 4.Hughes AJ, Daniel SE, Lees AJ. Improved accuracy of clinical diagnosis of Lewy body Parkinson's disease. Neurology 2001;57:1497–1499. [DOI] [PubMed] [Google Scholar]
- 5.Gibb WR, Lees AJ. The relevance of the Lewy body to the pathogenesis of idiopathic Parkinson's disease. J Neurol Neurosurg Psychiatry 1988;51:745–752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jellinger KA. Morphological substrates of parkinsonism with and without dementia: a retrospective clinico-pathological study. J Neural Transm Suppl 2007:91–104. [DOI] [PubMed] [Google Scholar]
- 7.Beach TG, Adler CH. Importance of low diagnostic accuracy for early Parkinson's disease. Mov Disord 2018;33:1551–1554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Adler CH, Beach TG, Hentz JG, et al. Low clinical diagnostic accuracy of early vs advanced Parkinson disease: clinicopathologic study. Neurology 2014;83:406–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Beach TG, Adler CH, Sue LI, et al. Arizona study of aging and neurodegenerative disorders and brain and body donation program. Neuropathology 2015;35:354–389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Adler CH, Hentz JG, Shill HA, et al. Probable RBD is increased in Parkinson's disease but not in essential tremor or restless legs syndrome. Parkinsonism Relat Disord 2011;17:456–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Adler CH, Hentz JG, Joyce JN, Beach T, Caviness JN. Motor impairment in normal aging, clinically possible Parkinson's disease, and clinically probable Parkinson's disease: longitudinal evaluation of a cohort of prospective brain donors. Parkinsonism Relat Disord 2002;9:103–110. [DOI] [PubMed] [Google Scholar]
- 12.Fahn S, Elton RL, Committee amotUD. Unified Parkinson's disease rating scale. In: Fahn S, Marsden CD, Goldstein M, Calne CD, editors. Recent Developments in Parkinson's Disease Volume II. Florham Park: Macmillan; 1987:153–163. [Google Scholar]
- 13.Stern MB, Doty RL, Dotti M, et al. Olfactory function in Parkinson's disease subtypes. Neurology 1994;44:266–268. [DOI] [PubMed] [Google Scholar]
- 14.McKinnon J, Evidente V, Driver-Dunckley E, et al. Olfaction in the elderly: a cross-sectional analysis comparing Parkinson's disease with controls and other disorders. Int J Neurosci 2010;120:36–39. [DOI] [PubMed] [Google Scholar]
- 15.Litvan I, Agid Y, Calne D, et al. Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome): report of the NINDS-SPSP International Workshop. Neurology 1996;47:1–9. [DOI] [PubMed] [Google Scholar]
- 16.Postuma RB, Berg D, Stern M, et al. MDS clinical diagnostic criteria for Parkinson's disease. Mov Disord 2015;30:1591–1601. [DOI] [PubMed] [Google Scholar]
- 17.Beach TG, Sue LI, Walker DG, et al. The Sun Health Research Institute Brain Donation Program: description and experience, 1987–2007. Cell Tissue Bank 2008;9:229–245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Beach TG, Adler CH, Lue L, et al. Unified staging system for Lewy body disorders: correlation with nigrostriatal degeneration, cognitive impairment and motor dysfunction. Acta Neuropathol 2009;117:613–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dickson DW, Braak H, Duda JE, et al. Neuropathological assessment of Parkinson's disease: refining the diagnostic criteria. Lancet Neurol 2009;8:1150–1157. [DOI] [PubMed] [Google Scholar]
- 20.Gelb DJ, Oliver E, Gilman S. Diagnostic criteria for Parkinson disease. Arch Neurol 1999;56:33–39. [DOI] [PubMed] [Google Scholar]
- 21.Beach TG, Adler CH, Dugger BN, et al. Submandibular gland biopsy for the diagnosis of Parkinson's disease. J Neuropath Exp Neurol 2013;72:130–136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Adler CH, Caviness JN, Sabbagh MN, et al. Heterogeneous neuropathological findings in Parkinson's disease with mild cognitive impairment. Acta Neuropathologica 2010;120:829–830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Beach TG, White CL, Hamilton RL, et al. Evaluation of alpha-synuclein immunohistochemical methods used by invited experts. Acta Neuropathol 2008;116:277–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walker DG, Lue LF, Adler CH, et al. Changes in properties of serine 129 phosphorylated alpha-synuclein with progression of Lewy-type histopathology in human brains. Exp Neurol 2013;240:190–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Uitti RJ, Calne DB, Dickson DW, Wszolek ZK. Is the neuropathological ‘gold standard' diagnosis dead? Implications of clinicopathological findings in an autosomal dominant neurodegenerative disorder. Parkinsonism Relat Disord 2004;10:461–463. [DOI] [PubMed] [Google Scholar]
- 26.Hughes AJ, Ben-Shlomo Y, Daniel SE, Lees AJ. What features improve the accuracy of clinical diagnosis in Parkinson's disease: a clinicopathologic study. Neurology 1992;42:1142–1146. [DOI] [PubMed] [Google Scholar]
- 27.Rajput AH, Rozdilsky B, Rajput A, Ang L. Levodopa efficacy and pathological basis of Parkinson syndrome. Clin Neuropharmacol 1990;13:553–558. [DOI] [PubMed] [Google Scholar]
- 28.Abbott RD, Ross GW, White LR, et al. Environmental, life-style, and physical precursors of clinical Parkinson's disease: recent findings from the Honolulu-Asia Aging Study. J Neurol 2003;250(suppl 3):30–39. [DOI] [PubMed] [Google Scholar]
- 29.Aarsland D, Brønnick K, Larsen JP, Tysnes OB, Alves G. Cognitive impairment in incident, untreated Parkinson disease: the Norwegian ParkWest study. Neurology 2009;72:1121–1126. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available at brainandbodydonationprogram.org.