Abstract
In the absence of adequate social security, out-of-pocket health expenditure compels households to adopt coping strategies, such as utilizing savings, selling assets, or acquiring external financial support (EFS) by borrowing with interest. Households' probability of acquiring EFS and its amount (intensity) depends on its social capital – the nature of social relationships and resources embedded within social networks. This study examines the effect of social capital on the probability and intensity of EFS during health events in Uttar Pradesh (UP), India. The analysis used data from a cross-sectional survey of 6218 households, reporting 3066 healthcare events, from two districts of UP. Household heads (HH) reported demographic, socioeconomic, and health-related information, including EFS, for each household member. Self-reported data from Shortened and Adapted Social Capital Assessment Tool in India (SASCAT-I) was used to generate four unique social capital measures (organizational participation, social support, trust, and social cohesion) at HH and community-level, using multilevel confirmatory factor analysis. After descriptive analysis, two-part mixed-effect models were implemented to estimate the probability and intensity of EFS as a function of social capital measures, where multilevel mixed-effects probit regression was used as the first-part and multilevel mixed-effects linear model with log link and gamma distribution as the second-part. Controlling for all covariates, the probability of acquiring EFS significantly increased (p = 0.04) with higher social support of the HH and significantly decreased (p = 0.02) with higher community social cohesion. Conditional to receiving any EFS, higher social trust of the HH resulted in higher intensity of EFS (p = 0.09). Social support and trust may enable households to cope up with financial stress. However, controlling for the other dimensions of social capital, high cohesiveness with the community might restrict a household's access to external resources demonstrating the unintended effect of social capital exerted by formal or informal social control.
Keywords: Out-of-pocket health expenditure, social capital, coping strategies, mixed-effect model, SASCAT-I, India
Highlights
-
•
Social support assists household head to acquire external financing for healthcare payment.
-
•
But higher social support may not secure higher intensity of receiving external financing.
-
•
However, trust is a catalyst to acquire more financing conditional of any external financing was acquire in the first place.
-
•
Living in a cohesive community may restrict access to external financial resources.
1. Introduction
In seven decades since independence, the Indian health sector has made significant progress in improving access and availability of health services, infrastructure, human resources, and availability of vaccines and medicines (Patel et al., 2015). At a broader contextual level, income has risen, millions have been lifted out of poverty, the country is urbanizing rapidly, and the population is aging (Desai et al., 2010). While continuing to grapple with the prevention and control of communicable diseases, staggered reduction of maternal and child mortality, and the burden of non-communicable illnesses and substance abuse (Al Kibria, Swasey, Hasan, Sharmeen, & Day, 2019; Hasan, Cohen, et al., 2020; Zodpey & Farooqui, 2018), the Indian health sector is facing a growing challenge of rising healthcare expenditure (Sangar, Dutt, & Thakur, 2019). At the national level, 59% of the total healthcare expenditure is financed by households’ out-of-pocket contributions (National Health Accounts Technical Secretariat National Health Systems Resource Centre & Ministry of Health and Family Welfare, 2019). The burden of healthcare expenditure is surprisingly high for the rural region of northern India – more specifically in Uttar Pradesh. The latest Sample Survey (2019) reported that a household in Uttar Pradesh spends around International.$ [Int.$]1 1264 for each hospital stay episode and Int.$ 41 per non-hospitalization events (1 Int.$ = 20.65 Indian Rupee, TheWorld Bank, 2017).
High out-of-pocket payment while seeking healthcare often leads to financial catastrophe (World Health Organization, 2017). An analysis of the 75th round of the National Sample Survey reported four out of five (81%) household of India faces catastrophic expenditure (10% of household's total consumption expenditure) and 40% households fall into poverty when paying for healthcare (Yadav, Menon, & John, 2021). The impact of catastrophic health expenditure reduces healthcare utilization, leading to a pervasive cycle of ill health and poverty (Russell, Fox-Rushby, & Arhin, 1995).
The high burden of healthcare costs results from the absence of an effective formal financial risk-sharing mechanism. At the national level, only 14% of the rural and 19% of the urban population are covered by any health insurance in India (National Sample Survey Office, 2019). Moreover, in Uttar Pradesh, only 6.1% of the households have at least one member insured by any health insurance package (International Institute for Population Sciences & ICF, 2017). Thus, the financial burden of healthcare has to be coped with using various informal risk-sharing mechanisms, such as using the savings, selling or mortgaging assets, borrowing, or reducing consumption expenditures (Quintussi, Van de Poel, Panda, & Rutten, 2015). According to the most recent estimates, household income and savings together are the most significant sources for healthcare payment (80% and 84% for rural and urban areas accordingly). In comparison, around 17% of the rural and 12% of the urban households use external financial support (EFS) – such as borrowed money or contribution/gift/help from friends and family – to pay for the cost of hospitalization (National Sample Survey Office, 2019).
Relying on one's associational network for this type of informal borrowing and gift-giving largely depends on social capital (Kanbur et al., 2000). Bourdieu (1986) and Lin (2001) defined social capital mainly focusing on the economic value of the expected return for one's investment in the social relationships. According to them, social capital is defined as the characteristics of social relationships and the actual or potential resources embedded within the social network of a person that can be accessed and utilized in the time of need (Bourdieu, 1986; Lin, 2001).
Social capital is often used as an alternative form of social insurance for “tapping resources” from neighbors, friends, and social groups to cushion the shocks of healthcare costs (Ravallion, 2016; Townsend, 1995; World Bank, 2014). Acquiring EFS as borrowed money or a gift from friends and relatives to pay for healthcare is identified as an “Idiosyncratic Risk Sharing” (Dercon, 2002). However, there are limitations to this type of risk-sharing strategy. The type, frequency, and severity of the disease can drastically change the coping strategies (Morduch, 1999). Moreover, socioeconomic status and health-related behaviors also affect the ability of the household to implement these informal risk-sharing strategies, such as drawing on social support from the community. De Weerdt (2004) reported that poor households often struggle to mitigate financial stress because of fewer social contacts or limited resources within their networks. Nevertheless, these coping strategies may have far-reaching consequences in the future as they continue the “inequity and patronage lined with the risk sharing agreement” (Fafchamps, 2003).
Previous literature anecdotally reported social capital as a coping strategy to mitigate the financial stress of healthcare (Fang, Shia, & Ma, 2012; Hoque, Dasgupta, Naznin, & Al Mamun, 2015; Nguyen et al., 2012; Quintussi et al., 2015). According to Chou (2006), there are three possible ways a household can use social capital as an economic tool: (a) using the information from the social network to obtain instrumental support (Valente, Hoffman, Ritt-Olson, Lichtman, & Johnson, 2003), (b) being cohesive with social groups to acquire social support (Kawachi et al., 2013), and (c) transforming the credit of social capital into human capital (Bourdieu, 1986). However, to date, no study has quantitatively explored if the stock of social capital within a household has any empirical association with the probability of acquiring EFS and its intensity (amount of EFS acquired).
Addressing this gap in evidence, this is the first study that had explored the first two mechanisms whereby being a part of social groups or deeply embedding yourself with the social norms could allow you to access financial resources within the social networks. This study aims to statistically examine the association between household head's social capital and the probability and intensity of acquiring EFS while paying for healthcare, using two-part mixed-effects models in a sample from rural Uttar Pradesh, India.
2. Methods
2.1. Conceptualizing social capital and healthcare payment using two-part mixed-effects models
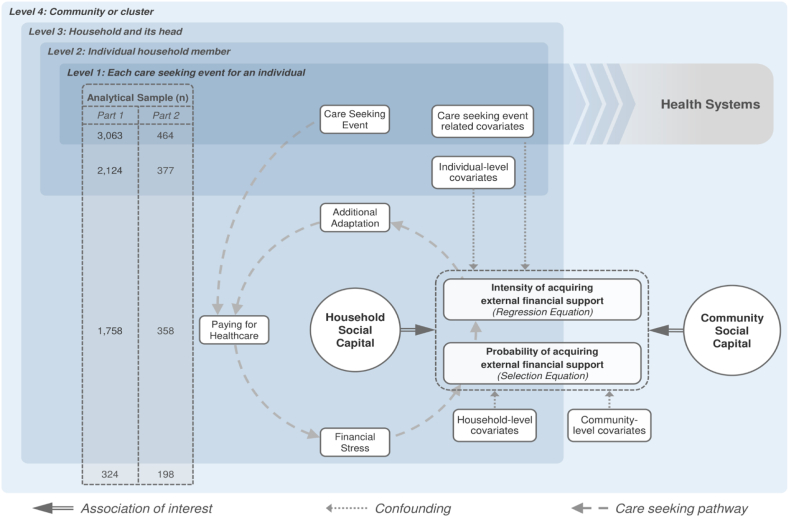
Fig. 1 presented our framework, which conceptualized how social capital – along with other social determinants – influences the acquisition of EFS for healthcare expenditure during the care-seeking event using a conceptual framework (Fig. 1). During a healthcare-seeking event for its member, a household engages with the health system embedded within the community. A household has to finance for the care-seeking events – if any expenditure is incurred – via a wide range of strategies such as using their saving, selling or mortgaging assets, or borrowing (Quintussi et al., 2015; Russell, 2001). Without the presence of a robust social safety net, a household with overwhelming financial stress may try to draw supports from its community as financial gifts or borrowed credit (Dhanaraj, 2016). However, the stress-buffering effect of EFS largely depends on two critical elements – (a) the probability of acquiring any EFS and (b) the amount of EFS acquired (its intensity) if any EFS was received.
Fig. 1.
Conceptual framework to explore the role of social capital as a determinant of DPT3 immunization among 12-59-month-old children in UP, India.
This phenomenon splits up the analytical sample into two groups – (1) receivers vs. non-receivers of EFS – presenting a binary distribution, and (2) who received any amount of EFS – presenting a continuous distribution. The nature of the relationship between covariates (such as social capital) and EFS will be considerably different for these two underlying analytical samples (Sauzet, Razum, Widera, & Brzoska, 2019). Furthermore, while exploring this relationship, the statistical analysis must account for the hierarchical nature of the data (health-seeking events nested in individuals nested in households nested in communities) using multilevel regression models (Hasan, Dean, et al., 2020; Rice & Jones, 1997). Thus, our study had implemented two-part mixed-effects models by fitting the binary and continuous components of EFS separately as a function of the covariates (Aitchison, 1955; J.; Zhao et al., 2020; T.; Zhao et al., 2016).
2.1.1. Part 1 – selection equation: multilevel mixed-effects probit regression
The first part, the selection equation, of the two-part mixed-effect model considers a binomial distribution – whether any EFS was received (y > 0) for paying for a healthcare event or not (y = 0) – and implements a mixed-effects probit regression to estimate the probability of acquiring any EFS. Let us consider M number of household members, each of whom had multiple healthcare events for which EFS can be acquired. These events can be influenced by a set of fixed effects xij and random effects uij. The probability function of acquiring EFS can be defined as:
| (1) |
Here, j = 1, …, M individuals, with the j individual having i = 1, …, nj healthcare-seeking events. The outcome (yij) is a binary response, where yij > 0 if any EFS is acquired and yij = 0 otherwise, xij is the 1 × p row vector of fixed effects, and βp1 are their associated regression coefficients for the Part 1 model. Considering no random slope, uj is the random intercept for each individual, which follows a multivariate normal distribution with the mean of 0 and a variance of σ2u. Lastly, H(•) presented a standard normal cumulative distribution function. For the probit regression, this function estimates the probability of (yij > 0). While equation (1) presents a simplified two-level model, the mixed-effects probit regression can be extended into three or four levels with nested random intercepts for households and communities as higher-level clusters.
2.1.2. Part 2 – regression equation: multilevel mixed-effects linear model with log link and gamma distribution
Conditional to any EFS acquired (yij > 0), the intensity of EFS can be fitted with a multilevel mixed-effects linear model. This is called the “regression equation”. If we consider n number of healthcare-seeking events, for which EFS is received, are clustered within each of M individuals, the estimated intensity of EFS can be defined as:
| (2) |
Here, j = 1, …, M individuals, with the j individual having i = 1, …, nj healthcare-seeking events with yij > 0. Also, yij|yij > 0 is the n × 1 vector for the EFS intensity reported by the household, which takes the form of the F distribution. The model also includes the 1 × p row vector of xij covariates as fixed effects, for each of them, βp2 are the associated regression coefficients for the Part 2 model. Without considering any random slopes, vj indicates the random intercept for each individual having a multivariate normal distribution with the mean of 0 and a variance of σ2v. Here, g(•) is identified as an invertible link function. Specific distribution (F) and link function (g) must be specified for the linear mixed-effect model during the estimation process. Much like healthcare expenditure data, the positive values of EFS tends to be right-skewed (O’Donnell, van Doorslaer, Wagstaff, & Lindelow, 2007). In this case, log link and gamma distribution perform exceptionally well (Malehi, Pourmotahari, & Angali, 2015), and equation (2) can be re-specified as:
| (3) |
| (4) |
The β0 + xijβp2 presents the overall regression line for all individuals, vj indicates the random intercept, representing the variability of each individual from the mean, and εij is the normally distributed random error. Due to the natural log transformation of yij|yij > 0 response, β0 and βp2 estimates need to be exponentiated for interpretation. This retransformation changes the β0 as the geometric mean of EFS of all individuals and βp2 as the multiplicative coefficient (rate ratio) in reference to the β0. If the data present additional higher levels of clustering, this two-level model can be naturally extended into three or four levels by including additional random intercepts.
2.2. Study design and analytical sample
The analytical sample of this study came from a cross-sectional household survey conducted in six census blocks of two rural districts of Uttar Pradesh, India. The survey was conducted from June to August 2017 in 6218 randomly selected households from 346 rural communities (averaging 17–18 households per cluster). The ethical approval for the survey was obtained from the Institutional Review Board Office of the author's institute and locally from the Center for Media Studies, New Delhi, India.
After receiving oral informed consent, trained data collectors interviewed the household heads (≥18 years) using a multi-topic structured questionnaire. Each household head reported a wide range of information, including demographic information, socioeconomic and consumption data of the household, and the social capital of the household head. The respondents also provided detailed information on the illness, care-seeking events, healthcare expenditure, the source, and the amount for healthcare payment strategies for each household member within the last six months of the survey.
The unit of analysis of this study was “healthcare-seeking events” of the individual household members. The analytical sample consisted of 3066 healthcare events sought by 2127 members of 1761 households within 324 communities. The response rate was 99%, with only three observations missing the age of the respondents. The effective sample size for Part 1 (selection equation) was 3063 healthcare events from 2124 members living in 1758 households nested within 324 communities. And the effective sample size for the Part 2 (regression equation) was 464 healthcare events – for which any EFS was received – from 377 members living in 358 households nested within 198 communities (Fig. 1).
2.3. Outcome variable
The response variable of the study was the total amount of money (in Indian Rupees) the household has acquired as EFS. Household heads separately reported the amount of EFS acquired as help/gift and borrowed money for each healthcare-seeking event within the last six months preceding the survey. We considered the cumulative amount from the two sources as the EFS values. In this analysis, the selection equation considered a binary EFS indicator using the zero vs. non-zero EFS values as the outcome, and for the regression equation, the outcome was the positive values of EFS (see supplement 1 in Additional File 1). For ease of interpretation, EFS values were converted into Int.$ using the 2017 Purchasing Power Parity (PPP) conversion factor for India (The World Bank, 2017).
2.4. Explanatory variables
2.4.1. Household head and community social capital measure
The measure of social capital of the household heads and the communities were the primary explanatory variables of this study. During the survey, each household head responded to the Shortened and Adapted Social Capital Assessment Tool in India (SASCAT-I) (Hasan et al., 2019), where they reported their community participation (2 questions), collective action (2 questions), social support (3 questions), social cohesion (3 questions), and trust (3 questions). These responses were categorized into 12 categorical indicators and used as the input for a multilevel confirmatory factor analytical model (MCFA), considering each household head as level one (n = 6218) and community as level two (n = 346) (Heck & Thomas, 2015).
Four unique latent constructs of social capital emerged from the MCFA – both at the household and community level – classified as organizational participation, social support, trust, and social cohesion. Standardized factor scores were obtained from the MCFA model as the composite measure for the social capital constructs and included in the analysis (see supplement 2 and 3 in Additional File 1 for details).
2.5. Other covariates
The association between the social capital and acquisition of EFS and its intensity could be confounded by several factors, such as the attributes of each healthcare event – the type of illness, type of healthcare providers, and the frequency of healthcare-seeking episodes by an individual within the six months preceding the survey. Similarly, characteristics of the individual household members for whom healthcare was sought (e.g., age, gender, education, disability, etc.), traits of the household heads (gender, education, occupation, etc.), and features of the household itself (religion, caste, wealth, financial stability, monthly health expenditure, etc.) can influence the relationship between social capital measures and EFS.
As each household is embedded within the community, the community's organization, its environment, and the socio-cultural factors would also affect the ability of a household head to draw in EFS (Nyswander, 1956). Thus, considering the hierarchical nature of the data and the confounding effect of the social determinants from various levels of the community, a wide range of covariates were included in the analysis (Table 1).
Table 1.
Covariates included in the two-part mixed-effects models according to the level of analysis.
| Variables | Type | Description |
|---|---|---|
| Level 1 covariates: Characteristics of the care-seeking events | ||
| Cause of health-seeking | Categorical | Health condition for which care has been sought |
| Sequence of health visits | Categorical | A dummy variable indicating the first, second, or the third episode of the healthcare-seeking event for a household member in the last six months |
| Healthcare provider | Categorical | Type of providers from whom healthcare was sought after |
| Level 2 covariates: Characteristics of the individual household members for whom healthcare was sought | ||
| Gender | Binary | Gender of an individual household member |
| Age categories | Categorical | Age of the household member as a category |
| Relationship with household head | Categorical | Relationship of the household member with the household head |
| Education | Categorical | Educational attainment of the household member |
| Employment status | Binary | Employment status of the household member |
| Disability | Binary | Presence of any disability of the household member |
| Level 3 covariates: Characteristics of the household heads and the household | ||
| Gender | Binary | Gender of the household head |
| Age categories | Categorical | Age categories of the household heads |
| Education | Categorical | Educational attainment of the household head |
| Occupation | Categorical | Occupation of the household heads |
| Freedom of decision making | Binary | Perceived level of freedom of decision making of the household heads |
| Household head's social capital measures | Continuous | Four standardized factor scores of household head's social capital constructs derived from the MCFA measured by Adapted Social Capital Assessment Tool-India (SASCAT-I) |
| Religion | Binary | Religion of the household |
| Caste | Categorical | Social caste of the household |
| Caste concordance | Binary | An indicator which reflects if the household caste was the same as the dominant caste of the community |
| Wealth | Categorical | Asset index was developed by principal component analysis using 27 household asset-related binary variables. The standardized score of the first component was used to create five asset quintile groups, where Quintile 1 was assigned to the least wealthy household, and Quintile 5 was assigned to the wealthiest household |
| Financial stability | Categorical | Response of the household heads to the question “In the last 12 months, how has your financial situation changed overall?” |
| Household member number | Continuous | Number of members living in the household for the last six months |
| Monthly health expenditure | Continuous | Reported total monthly healthcare expenditure converted into the International.$ using Purchasing Power Parity (PPP) 2017 of India*. This is considered as the proxy of the severity of illness. |
| Level 4 covariates: Characteristics of the community | ||
| Census block | Categorical | The administrative boundary which serves as the enumeration block of the census in each district |
| Community wealth | Continuous | Standardized average scores of the first component of principal component analysis from the households of each cluster |
| Community reciprocity | Continuous | The community-level average response of household heads of two questions: (1) “Do you think people in your village generally are willing to help each other out?” and (2) “Do you think if you help someone in your village, they will help you in return when you need it?” (response: Yes = 2, Sometime = 1, No = 0) |
| Community social capital | Continuous | Community-level standardized factor scores of four social capital constructs derived from the MCFA |
Note: * = 1 International Doller = 20.648 Rupee (https://data.worldbank.org/indicator/PA.NUS.PPP?locations=IN).
2.6. Analytical strategy for implementing the two-part mixed-effects model
Before implementing the regression models, we performed descriptive analysis and explored the Intraclass Correlation Coefficient (ICC) of EFS for the underlying two sub-samples. This is particularly necessary to understand the proportion of the overall variance of EFS explained by the members, household, and community-level, which informed the number of random intercepts needed to be included in the regression models (Rice & Jones, 1997).
The ICC for the analytical sample of Part 1 (selection equation, n = 3063) indicated 45%, 38%, and 10% of the total variance of the binary EFS outcome was attributed to individual members (level 2, n = 2124), household (level 3, n = 1758) and community (level 4, n = 324), respectively. Thus, we implemented four-level mixed-effect probit models as Part 1 of the two-part model. We did not observe a similar pattern of ICC for the EFS intensity in the analytical sample of Part 2 (regression equation, n = 464). Only 18 out of 358 households (5%) – which had acquired EFS – had more than one member for whom the EFS was acquired. Including individual members as a separate random intercept in the mixed-effect model would not provide any additional benefit. Thus, we implemented three-level mixed-effect models with log link and gamma distribution as Part 2, where 72% and 5% of the total variance of EFS intensity was attributed to the households (level 2, n = 358) and community (level 3, n = 198).
To understand the explanatory power of the covariates, first, bivariate regression models were implemented. Covariates with a p-value ≤ 0.2 in the bivariate regressions were included in the multiple regression model (Maldonado & Greenland, 1993). Before developing the multivariate models, the multicollinearity of the eligible covariates was assessed using the variance inflation factor (VIF). Next, we separately implemented the adjusted regression models with the appropriate number of random intercepts (identified from the ICC values) with no random slopes.
For estimating the adjusted effect of social capital measures, we have implemented six alternative specifications of Part 1 and 2 regression models, starting with a null model with no covariate (Model 1) and incrementally including fixed effects associated with social capital (Model 2), healthcare events (Model 3), household members (Model 4), households and its heads (Model 5), and the community (Model 6). For the ease of interpretation of the final model (Model 6), we calculated the marginal effects of the estimated coefficients of the multilevel mixed-effects probit model, which indicated the marginal probability of acquiring EFS as a function of the covariates. For the multilevel mixed-effects linear model, we exponentiated the estimated coefficients, which represented the ratio of the acquired EFS amount in reference to the baseline (constant or β0) as a function of the covariates.
To assess the overall significance of the categorical variables, Wald tests were used after each regression. The goodness of fit of all adjusted models was evaluated using Log-Likelihood (LL) and Akaike information criterion (AIC). In addition, to assess the robustness of our final model, sensitivity analysis was conducted considering only borrowed money, and gifted money as the outcome variable, separately, instead of the cumulative EFS value.
3. Results
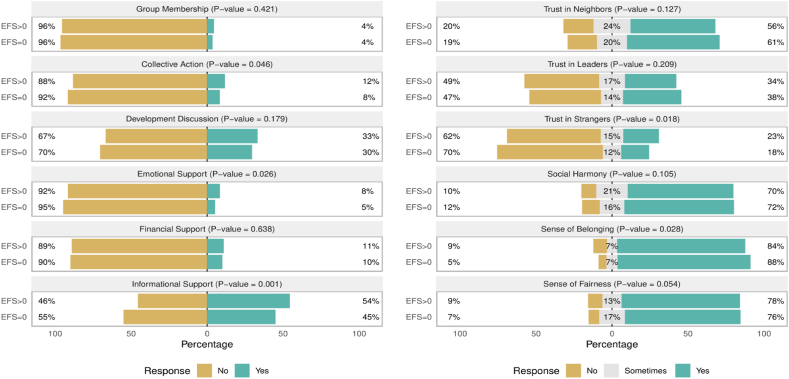
Overall, for 15.13% (n = 464) of healthcare-seeking events, the household heads received some amount of EFS within the last six months preceding the survey. Conditional on any EFS received, a household acquired an average of Int.$ 386.10 (range Int.$ 0.05–4794.65) as EFS, which indicated the data was skewed to the right, and application of log link is an appropriate decision (see supplement 4 in Additional File 1). Table 2 presents the descriptive statistics of the care-seeking events (n = 3066) and any care-seeking for which EFS was acquired (n = 464). Fig. 2 shows the distribution of the 12 social capital indicators reported by 1761 household heads disaggregated by the respondents who reported not acquiring (n = 1403) vs. acquiring some EFS (n = 358). A statistically significant difference (p < 0.05) was observed for their collective action, emotional support, informational support, trust in strangers, and sense of belonging.
Table 2.
Characteristics of study participants and their associated healthcare events in two rural districts of Uttar Pradesh, India.
| All care-seeking events (n = 3066) |
Care seeking events for which external financial support received (n = 464) |
|||||
|---|---|---|---|---|---|---|
| N | Col% | N | Col% | |||
| Characteristics of Healthcare Event | ||||||
| Cause of health-seeking | ||||||
| Pregnancy or delivery | 201 | 6.56 | 52 | 11.21 | ||
| Acute Illness | 1331 | 43.41 | 188 | 40.52 | ||
| Chronic illness | 726 | 23.68 | 106 | 22.84 | ||
| Accident or injury | 213 | 6.95 | 56 | 12.07 | ||
| Others | 595 | 19.41 | 62 | 13.36 | ||
| Sequence of health visits | ||||||
| First | 2191 | 71.46 | 365 | 78.66 | ||
| Second | 580 | 18.92 | 75 | 16.16 | ||
| Third | 295 | 9.62 | 24 | 5.17 | ||
| Healthcare provider | ||||||
| Public | 641 | 20.91 | 105 | 22.63 | ||
| Private | 2005 | 65.39 | 333 | 71.77 | ||
| Informal |
420 |
13.70 |
26 |
5.60 |
||
|
Mean |
Min |
Max |
||||
| Acquired financial support (Int.$)* | 386.1 | 0.05 | 4794.65 | |||
| Member's Characteristics | ||||||
| Gender | ||||||
| Male | 1411 | 46.02 | 201 | 43.32 | ||
| Female | 1655 | 53.98 | 263 | 56.68 | ||
| Age categories | ||||||
| 0–15 years | 773 | 25.21 | 98 | 21.12 | ||
| 16–49 years | 1581 | 51.57 | 260 | 56.03 | ||
| 50 yeas or above | 709 | 23.12 | 106 | 22.84 | ||
| Relationship with household head | ||||||
| Self | 820 | 26.74 | 120 | 25.86 | ||
| Spouse | 830 | 27.07 | 139 | 29.96 | ||
| Child/Parents | 1140 | 37.18 | 175 | 37.72 | ||
| Others | 276 | 9.00 | 30 | 6.47 | ||
| Education | ||||||
| No Education | 1037 | 33.82 | 155 | 33.41 | ||
| Up to primary | 823 | 26.84 | 146 | 31.47 | ||
| Up to secondary | 581 | 18.95 | 88 | 18.97 | ||
| Above secondary | 242 | 7.89 | 34 | 7.33 | ||
| Child | 383 | 12.49 | 41 | 8.84 | ||
| Employment | ||||||
| Unemployed | 2113 | 68.92 | 332 | 71.55 | ||
| Employed | 953 | 31.08 | 132 | 28.45 | ||
| Disability | ||||||
| No | 2929 | 95.53 | 431 | 92.89 | ||
| Yes | 137 | 4.47 | 33 | 7.11 | ||
| Household Head's Characteristics | ||||||
| Gender | ||||||
| Male | 2674 | 87.21 | 399 | 85.99 | ||
| Female | 392 | 12.79 | 65 | 14.01 | ||
| Age Categories | ||||||
| Less than 30 years | 646 | 21.07 | 129 | 27.80 | ||
| 31–40 | 859 | 28.02 | 118 | 25.43 | ||
| 41–50 | 663 | 21.62 | 93 | 20.04 | ||
| 51–60 | 536 | 17.48 | 84 | 18.10 | ||
| 61 and above | 362 | 11.81 | 40 | 8.62 | ||
| Education | ||||||
| No Education | 924 | 30.14 | 157 | 33.84 | ||
| Up to primary | 835 | 27.23 | 136 | 29.31 | ||
| Up to secondary | 951 | 31.02 | 137 | 29.53 | ||
| Above secondary | 356 | 11.61 | 34 | 7.33 | ||
| Occupation | ||||||
| Agriculture | 1539 | 50.20 | 197 | 42.46 | ||
| Wage laborer | 769 | 25.08 | 149 | 32.11 | ||
| Self-employed & Salaried | 345 | 11.25 | 44 | 9.48 | ||
| Unemployed | 413 | 13.47 | 74 | 15.95 | ||
| Freedom of decision making | ||||||
| Low | 284 | 9.26 | 56 | 12.07 | ||
| High | 2782 | 90.74 | 408 | 87.93 | ||
| Household's Characteristics | ||||||
| Religion | ||||||
| Hindu | 2678 | 87.35 | 410 | 88.36 | ||
| Muslim and Others | 388 | 12.65 | 54 | 11.64 | ||
| Caste | ||||||
| General | 618 | 20.16 | 87 | 18.75 | ||
| ST/SC | 1291 | 42.11 | 193 | 41.59 | ||
| OBC and Others | 1157 | 37.74 | 184 | 39.66 | ||
| Caste concordanceb | ||||||
| No | 1173 | 38.26 | 188 | 40.52 | ||
| Yes | 1893 | 61.74 | 276 | 59.48 | ||
| Wealth | ||||||
| Poorest | 511 | 16.67 | 91 | 19.61 | ||
| Poorer | 570 | 18.59 | 104 | 22.41 | ||
| Medium | 633 | 20.65 | 90 | 19.40 | ||
| Richer | 630 | 20.55 | 93 | 20.04 | ||
| Richest | 722 | 23.55 | 86 | 18.53 | ||
| Financial stability | ||||||
| Worsen | 966 | 31.51 | 227 | 48.92 | ||
| Stable | 1716 | 55.97 | 200 | 43.10 | ||
| Improved |
384 |
12.52 |
37 |
7.97 |
||
|
Mean |
Min |
Max |
Mean |
Min |
Max |
|
| Household member number (Count) | 5.36 | 1 | 18 | 5.23 | 1 | 17 |
| Monthly health expenditure (Int.$)* | 434.99 | 0.05 | 22297.56 | |||
| Community's Characteristics | ||||||
| Census block | ||||||
| Behadar | 722 | 23.55 | 86 | 18.53 | ||
| Kachhauna | 303 | 9.88 | 43 | 9.27 | ||
| Kothwan | 525 | 17.12 | 83 | 17.89 | ||
| Kasmanda | 379 | 12.36 | 55 | 11.85 | ||
| Machhrehta | 488 | 15.92 | 104 | 22.41 | ||
| Sidhauli |
649 |
21.17 |
93 |
20.04 |
||
|
Mean |
Min |
Max |
Mean |
Min |
Max |
|
| Community wealthc | 0.09 | −2.00 | 3.63 | −0.01 | −2.00 | 3.63 |
| Community reciprocity | 0.87 | 0.00 | 2.29 | 0.87 | 0.00 | 2.29 |
Note: a = Social capital scores were measured as the standardized factor score generated by multilevel confirmatory factor analysis of social capital indicators of Shortened Adapted Social Capital Assessment Tool in India (SASCAT-I) b = Caste concordance: Household caste is the same as the caste of the majority of the population in the community.
c = Community wealth is measured by the average of the individual household wealth index generated by PCA.
* International.$ is calculated using Purchasing Power Parity (PPP) 2017 of India: 1 International Doller = 20.648 Rupee (https://data.worldbank.org/indicator/PA.NUS.PPP?locations=IN).
Fig. 2.
Distribution of social capital indicators of household heads (n = 1749) and mothers (n = 1779) of 12–59-month-old children in UP, India.
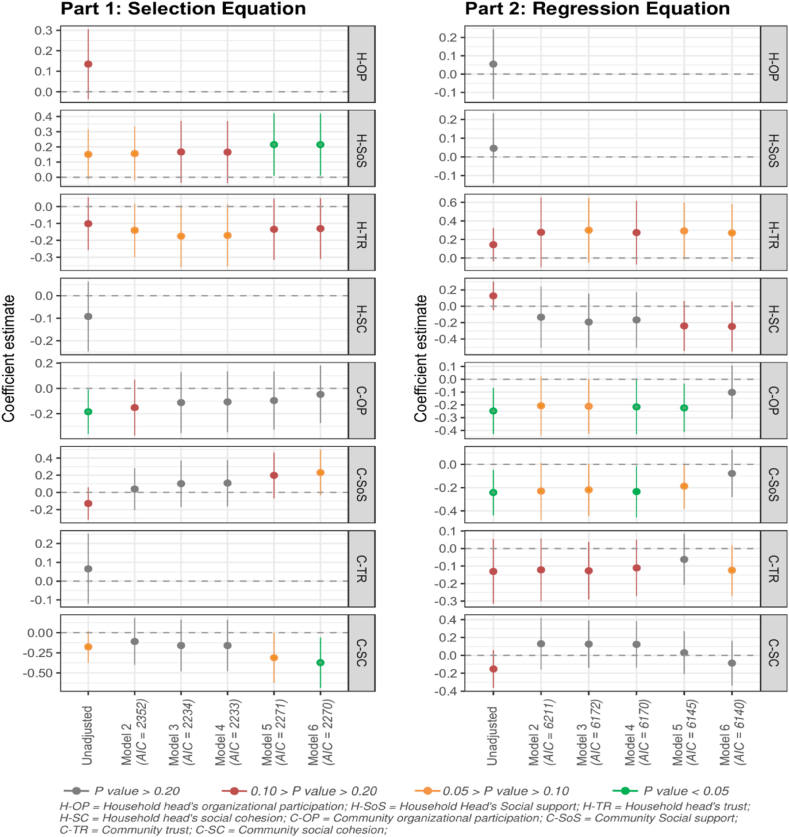
The effect estimates of social capital measures were robust and stable across all alternative specification models with different sets of covariates (Fig. 3) (see supplement 5, 7, and 8 in Additional File 1 for more details). Moreover, the sensitivity analysis indicated that the final model estimates were valid. The models developed using borrowed and gifted money as separate outcome variables also presented a similar pattern of association with social capital measures (see supplement 9 and 10 in Additional File 1). Table 3 presents the adjusted marginal probability of acquiring EFS estimated using four-level mixed-effect probit model (Part 1: Selection Equation) and adjusted exponentiated estimates (or rate ratio) of the intensity of EFS estimated using from three-level mixed-effect linear models with log link and gamma distribution (Part 2: Regression Equation) from Model 6.
Fig. 3.
Effect estimates of the social capital measures derived from four-level mixed-effect probit model (Part 1: selection equation) and three-level mixed-effects linear model with log link and gamma distribution (Part 2: regression equation) in rural Uttar Pradesh, India.
Table 3.
Multivariate fixed and random-effect estimates derived from Model 6 of four-level mixed-effect probit model (Part 1: selection equation) and three-level mixed-effects linear model with log link and gamma distribution (Part 2: regression equation) in rural Uttar Pradesh, India.
| Four-level mixed-effect probit model (Part 1: selection equation) |
Three-level mixed-effect linear model with log link and gamma distribution (Part 2: regression equation) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Adjusted Marginal Probability |
[95% CI] | P Value | Adjusted Rate Ratio | [95% CI] | P Value | |||
| Fixed Effects | ||||||||
| Household head's social capitala | ||||||||
| H-SoS | 0.02 | * | [0.001, 0.03] | 0.04 | Not included in adjusted modele | |||
| H-TR | −0.01 | [-0.03, 0.004] | 0.20 | 1.31 | # | [0.96, 1.79] | 0.09 | |
| H-SC | Not included in adjusted modele | 0.78 | # | [0.58, 1.06] | 0.11 | |||
| Community social capitala | ||||||||
| C-OP | −0.004 | [-0.02, 0.02] | 0.69 | 0.90 | [0.73, 1.11] | 0.34 | ||
| C-SoS | 0.02 | # | [-0.002, 0.04] | 0.09 | 0.93 | [0.75, 1.13] | 0.45 | |
| C-TR | Not included in adjusted modele | 0.90 | # | [0.78, 1.04] | 0.14 | |||
| C-SC | −0.03 | * | [-0.06, −0.01] | 0.02 | 0.92 | [0.71, 1.18] | 0.49 | |
| Characteristics of Healthcare Event | ||||||||
| Cause of health-seeking (Ref: Acute Illness) | ||||||||
| Pregnancy or delivery | 0.08 | * | [0.02, 0.15] | 0.00 | 1.18 | [0.71, 1.96] | 0.00 | |
| Chronic illness | 0.02 | # | [-0.01, 0.06] | 0.88 | [0.61, 1.28] | |||
| Accident or injury | 0.08 | ** | [0.02, 0.15] | 1.30 | [0.83, 2.04] | |||
| Others | −0.04 | * | [-0.07, −0.01] | 0.45 | *** | [0.29, 0.69] | ||
| Sequence of health visits (Ref: First) | ||||||||
| Second | −0.03 | ** | [-0.06, −0.01] | 0.00 | 0.65 | * | [0.47, 0.91] | 0.02 |
| Third | −0.05 | *** | [-0.08, −0.02] | 0.61 | # | [0.35, 1.05] | ||
| Healthcare provider (Ref: Public) | ||||||||
| Private | 0.04 | ** | [0.01, 0.07] | 0.00 | 0.94 | [0.67, 1.32] | 0.00 | |
| Informal | −0.07 | ** | [-0.10, −0.03] | 0.25 | *** | [0.12, 0.49] | ||
| Member's Characteristics | ||||||||
| Patient's age categories (Ref: 0–15 years) | ||||||||
| 16–49 years | 0.03 | # | [-0.001, 0.07] | 0.12 | 1.77 | * | [1.10, 2.84] | 0.06 |
| 50 yeas or above | 0.05 | # | [-0.001, 0.10] | 1.59 | # | [0.94, 2.68] | ||
| Relationship with household head (Ref: Self) | ||||||||
| Spouse | Not included in adjusted modele | 1.07 | [0.73, 1.57] | 0.92 | ||||
| Child/Parents | 1.17 | [0.75, 1.83] | ||||||
| Others | 1.12 | [0.59, 2.13] | ||||||
| Employment (Ref: Unemployed) | ||||||||
| Employed | −0.03 | # | [-0.06, 0.004] | 0.11 | Not included in adjusted modele | |||
| Disability (Ref: No) | ||||||||
| Yes | 0.07 | # | [-0.01, 0.14] | 0.06 | Not included in adjusted modele | |||
| Household Head's Characteristics | ||||||||
| Age categories (Ref: less than 30 years) | ||||||||
| 31-40 | −0.04 | # | [-0.09, 0.003] | 0.03 | Not included in adjusted modele | |||
| 41-50 | −0.06 | * | [-0.10, −0.01] | |||||
| 51-60 | −0.03 | [-0.09, 0.02] | ||||||
| 61 and above | −0.09 | ** | [-0.15, −0.04] | |||||
| Education (Ref: No Education) | ||||||||
| Up to primary | −0.002 | [-0.04, 0.04] | 0.19 | Not included in adjusted modele | ||||
| Up to secondary | −0.01 | [-0.05, 0.03] | ||||||
| Above secondary | −0.06 | * | [-0.11, −0.01] | |||||
| Household head's occupation (Ref: Agriculture) | ||||||||
| Wage laborer | 0.03 | [-0.01, 0.07] | 0.33 | Not included in adjusted modele | ||||
| Self-employed & Salaried | 0.02 | [-0.03, 0.07] | ||||||
| Unemployed | 0.03 | [-0.02, 0.08] | ||||||
| Freedom of decision making (Ref; Low) | ||||||||
| High | −0.03 | [-0.08, 0.02] | 0.22 | 1.06 | [0.69, 1.62] | 0.80 | ||
| Household's Characteristics | ||||||||
| Household caste (Ref: General) | ||||||||
| ST/SC | Not included in adjusted modele | 0.82 | [0.55, 1.23] | 0.58 | ||||
| OBC and Others | 0.82 | [0.54, 1.23] | ||||||
| Caste concordanceb (Ref: No) | ||||||||
| Yes | Not included in adjusted modele | 0.86 | [0.64, 1.16] | 0.32 | ||||
| Household wealth (Ref: Poorest) | ||||||||
| Poorer | 0.02 | [-0.03, 0.07] | 0.51 | 1.46 | # | [0.96, 2.24] | 0.35 | |
| Medium | −0.001 | [-0.05, 0.05] | 1.34 | [0.85, 2.11] | ||||
| Richer | −0.01 | [-0.06, 0.04] | 1.51 | # | [0.94, 2.41] | |||
| Richest | −0.02 | [-0.07, 0.02] | 1.55 | # | [0.93, 2.59] | |||
| Financial stability of the household (Ref: Worsen) | ||||||||
| Stable | −0.10 | *** | [-0.13, −0.06] | 0.00 | Not included in adjusted modele | |||
| Improved | −0.15 | *** | [-0.20, −0.11] | |||||
| Household member number (Count) | Not included in adjusted modele | 1.02 | [0.95, 1.10] | 0.57 | ||||
| Monthly health expenditure (per Int.$100)c | 0.006 | *** | [0.004, 0.007] | 0.00 | 1.04 | *** | [1.02, 1.06] | 0.00 |
| Community's Characteristics | ||||||||
| Census block (Ref: Behadar) | ||||||||
| Kachhauna | 0.03 | [-0.02, 0.09] | 0.10 | 1.83 | # | [1.00, 3.33] | 0.40 | |
| Kothwan | 0.04 | # | [-0.01, 0.09] | 1.25 | [0.76, 2.07] | |||
| Kasmanda | 0.01 | [-0.03, 0.06] | 1.27 | [0.73, 2.21] | ||||
| Machhrehta | 0.08 | ** | [0.03, 0.13] | 1.12 | [0.68, 1.83] | |||
| Sidhauli | 0.02 | [-0.02, 0.07] | 1.04 | [0.65, 1.68] | ||||
| Community wealthd | Not included in adjusted modele | 0.98 | [0.83, 1.15] | 0.77 | ||||
| Community reciprocity | Not included in adjusted modele | 0.65 | * | [0.44, 0.95] | 0.03 | |||
| Random Effects | ||||||||
| Level 4: Community variance | 0.18 | |||||||
| Level 4: ICC | 0.03 | |||||||
| Level 3: Household variance | 2.48 | ~0.001 | ||||||
| Level 3: ICC | 0.35 | ~0.001 | ||||||
| Level 2: Household members variance | 2.26 | 0.57 | ||||||
| Level 2: ICC | 0.47 | 0.69 | ||||||
| Fit Statistics | ||||||||
| Log-likelihood (LL) | −1041 | −3032 | ||||||
| Akaike information criterion (AIC) | 2170 | 6140 | ||||||
| Observations | 3063 | 464 | ||||||
Note: The adjusted regressions include data from 3063 health events of 2124 individual household members from 1758 households within 324 communities or sampling clusters, *** = p < 0.001, ** = p < 0.01, * = p < 0.05, # = p < 0.20.
a = Social capital scores were measured as the standardized factor score generated by multi-level confirmatory factor analysis of social capital indicators of Shortened Adapted Social Capital Assessment Tool in India (SASCAT-I).
b = Caste concordance: Household caste is the same as the caste of the majority of the population in the community.
c = Int.$ is calculated using Purchasing Power Parity (PPP) 2017 of India: 1 Int..$ = 20.648 Rup (https://data.worldbank.org/indicator/PA.NUS.PPP?locations=IN).
d = Community wealth is measured by the average of the individual household wealth index generated by PCA.
H-SoS = Household head's social support, H-TR = Household head's trust, H-SC = Household head's social cohesion.
C-OP = Community organizational participation, C-SoS = Community social support, C-TR = Community trust.
C-SC = Community social cohesion.
e = Variable was not included in the adjusted model as it did not present a significant association in the unadjusted model. Please, see the supplement 5 in the Additional File 1 for more information.
After adjusting for all fixed and random effects in the model, the probability of acquiring EFS during a health-seeking event significantly increased with a higher level of social support of the household head. In contrast, the intensity of EFS did not have any association with the household head's social support (Table 3). Within the same community, comparing two household heads with the difference of one standard deviation (SD) of social support, the household head with higher social support had a 2% higher probability of acquiring EFS (marginal probability = 0.02; 95% Confidence Intervals [CI] = 0.001, 0.03; p = 0.04), compared to a household head with the lower social support. On the other hand, the probability of acquiring EFS significantly decreased (p = 0.02) with increasing community-level social cohesion, while the intensity of EFS did not have any significant association (p = 0.49) with the community's cohesiveness. The result suggested, between two communities that differed by 1 SD of social cohesion, a household head living in the community with higher social cohesion had a 3% lower probability of acquiring EFS (marginal probability = −0.03; 95% CI = −0.06, −0.01; p = 0.02), compared to a household head from a community with lower social cohesion.
None of the social capital measures presented any significant association with the intensity of EFS (at the level of p < 0.05). However, considering a significance level of p < 0.10, the intensity of EFS – conditional on any EFS received – increased with a higher level of trust of the household head. Household heads living in the same community, who acquired at least Int.$ 1 as EFS during a care-seeking event for any household member, was able to acquire a higher amount of EFS as a factor of 1.31 (95% CI = 0.96, 1.79, p = 0.09) with every 1 SD increase of their level of trust, after adjusting all fixed and random effects in the model.
4. Discussion
4.1. Discussion of the result
We found that for around 15% of healthcare-seeking events, EFS was acquired to pay for healthcare expenditures in Uttar Pradesh, a finding similar to the latest national estimate. According to the National Sample Survey (2019), around 16.8% of rural households of India financed hospitalization events either by borrowing or acquiring financial contributions from friends or relatives. The role of social capital in acquiring EFS was very much nuanced. We found that social capital constructs were both negatively (i.e., social cohesion) and positively (i.e., social support, trust) associated with EFS. Social capital also appeared to be a contextual feature of the community. Several studies also identified the contextual nature of social capital by reporting its influence on self-rated health (Mohnen, Groenewegen, Völker, & Flap, 2011), care-seeking behavior (Hasan, Dean, et al., 2020; Story, 2014), and mental health (De Silva, Huttly, Harpham, & Kenward, 2007).
The first set of results was rather intuitive, indicating a higher likelihood of a household head acquiring any EFS for a health event if he/she had higher social support. Bourdieusian perspective of social capital theorized that actual or potential neighborhood resources could support the health and wellbeing of an individual or community, “either in the absence of or in conjunction with, their own economic and cultural capital” (Carpiano, 2008). Our study – along with several previous investigations (Domínguez & Watkins, 2003; Hoque et al., 2015; Nguyen et al., 2012; Quintussi et al., 2015) – support the theory that households can draw upon the resources embedded within their social connections to cope with the financial burden of healthcare.
Still, there are limitations to EFS as a type of informal health insurance. The social, cultural, and political fabric of the community can drastically change the effectiveness of using EFS as a risk-sharing strategy (Morduch, 1999). Our results showed that living in a highly cohesive community reduced the probability of receiving EFS. Such a negative impact is postulated as the “dark side” of social capital by Alejandro Portes (2014). Within a highly cohesive community, over-reliance on social capital could exert a coercive effect, especially during financial stress (Lakon, Godette, & Hipp, 2008). Though household heads may readily avail EFS if their social network includes individuals or groups with power and authority, a tightly-knit community can impose informal social control, which results in the social exclusion of those who deviate from the norm (e.g., those with chronic or disabling health conditions) (Portes, 1998).
Thus, households facing impoverishment due to high healthcare expenditure may not be able to mitigate their financial stress while living in a community with stronger social cohesion, as they have been ostracized, leading to fewer social contacts (De Weerdt, 2004). Being closely-knitted members of a cohesive but impoverished neighborhood, such as a rural community of Uttar Pradesh, individuals often face excessive demands to share their limited resources supporting other members (Villalonga-Olives & Kawachi, 2017), leading to a strategic share of resources based on their social position and network.
An alternative explanation is postulated by Kondo and Shirai (2013). While investigating the role of social cohesion on the microfinance program, they have found that highly cohesive communities with limited financial resources support themselves by non-financial means or by developing informal financial support systems. Such informal arrangement can be leveraged when rural households receive consultation or medications as a credited service without immediate point-of-care payments, for which payments are made later (Kruk, Goldmann, & Galea, 2009; Morduch, 1999). Information on such credited service was not collected during the survey, which can potentially underestimate the probability and intensity of EFS within the sample.
We did not observe any association between the trust of a household head and the probability of acquiring EFS. According to Carpiano (2008), on its own, trust may not be sufficient to achieve a specific aim – such as acquiring EFS for healthcare expenditure – by a person or group, but the critical determinant is the stock of resources that can be accessed using social networks (Carpiano, 2008). Glanville and Story (2018) suggested that trust can strengthen norms of reciprocity and enable collective action to benefit the wellbeing of the community. Specifically, their findings suggested that trust activates resources within one's social network to support better health (Glanville & Story, 2018). Supporting their hypothesis, we found that if the stock of resources was accessed, the trust might have played a role in tapping more significant amounts of resources (Anderson & Mellor, 2008), which was observed in the positive association between individualized trust and the intensity of EFS (at the level of p < 0.10). Although other economic concepts such as “altruism” (Michalski, 2003) or “warm glow” – the selfish pleasure or emotional reward of performing a selfless act (Andreoni, 1989) – may explain cooperative behavior such as transaction of EFS, within the scope of this study, we were not able to explore these concepts.
4.2. Strengths and limitations
This study broke new ground in the economic sociology research on social capital by implementing two-part mixed-effects models within a multilevel semi-continuous data structure. Implementation of this advanced econometric model allowed us to explore the relationship between social capital and the probability of acquiring EFS and the intensity of EFS, simultaneously, to understand the contextual nature of social capital in the rural communities of Uttar Pradesh, India. Using a validated social capital assessment tool (Hasan et al., 2019) and implementing the MCFA model to develop social capital measures – devoid of any measurement error (Heck & Thomas, 2015) – further strengthen our study. Furthermore, including a wide range of confounders in the analysis using a comprehensive conceptual framework made our analysis robust.
We also acknowledge a few limitations of the study. Due to the limitation of the data collection process, we could not include the severity of the illness associated with the health-seeking events, which could influence the healthcare expenditure vis-a-vis the amount of EFS acquired. We have included each household's total monthly health expenditure as a proxy variable to account for this confounding factor. The study collected data on the current level of the household head's social capital, while the health-seeking event could be sought up to six months preceding the date of the survey. However, we assume that the social capital of the household heads may not drastically change within the last six months (Claridge, 2018).
While it would be ideal for estimating the effect of social capital by modeling the financial gifts and borrowed money as separate outcomes in the regressions, we aggregated these two sources of EFS for retaining the adequate sample size for analysis. The sensitivity analysis has supported the validity of this decision by demonstrating the stability of the effect estimates of the social capital measures across the different outcome variables (see supplement 9 and 10 in Additional File 1). And lastly, we cannot make any causal inference because of the study's cross-sectional design.
5. Conclusion
This paper concludes that external financing sources are a significant contributor to healthcare payment in rural northern India. Social support plays a pivotal role while households of Uttar Pradesh acquired EFS to cope with the financial stress of healthcare costs. The individualized social trust of the household head also acts as a catalyst for acquiring more EFS, only if the household heads can access external financing first. Furthermore, being highly cohesive with the community may limit household heads from accessing external financial resources. These results provide critical insights into how social relationships were leveraged – almost like a transactional good (Kawachi & Subramanian, 2018) – within India's rural community, where social relationships are heavily influenced by gender, religion, caste, and class hierarchies (Goli, Maurya, & Sharma, 2015; Kowal & Afshar, 2015; Srivatsan, 2015).
However, to appropriately contextualized our result, we have also carried out a follow-up qualitative study by exploring the role of social capital as a coping strategy for healthcare payment among a subsample of the study participants. The result of that study will provide further insights into the lived experience of rural households when drawing on community resources for healthcare payment and how social capital affects their attitude, perceived social norm, self-efficacy, and agency when they rely on such an informal system.
Currently, less than 20% of the population of India is covered by any health insurance. It is not surprising that households still bear 59% of the total healthcare cost (National Health Accounts Technical Secretariat National Health Systems Resource Centre & Ministry of Health and Family Welfare, 2019) and continue to rely upon pervasive coping strategies. Therefore, the government of India must not undermine the strength of the communal society and the resources embedded in social networks in rural India (Serra, 1999). In this regard, using the resources within the community can bridge the gap between the ability to pay and utilization of healthcare (Donfouet & Mahieu, 2012) and break the insidious cycle of poverty and ill-health (Russell et al., 1995). India has a long history of developing and implementing grassroots-level programs (such as community-based health insurance), which are tailor-made according to the community's need and best suited for rural India's unique social and cultural milieu (Bhageerathy, Nair, & Bhaskaran, 2017; Ranson, 2003). Mainstreaming such initiatives and developing a clear pathway to integrate them within formal health insurance structures should be considered a practical step forward. Moreover, future research should explore the value of social capital as a resource for paying for healthcare to understand the interplay among healthcare financing, social support, and community cohesiveness. The findings of such a study will be immensely valuable as India strives to expand its social safety nets for its 1.36 billion population.
Authors contribution
The study was conceptualized by MZH and KDR with the support of SG. MZH supervised the household survey and the data collection process along with the supportive supervision of AA. MZH led data management and performed all statistical analyses. WTS, DMB, KDR, AA, and SG contributed to interpreting the result of the study. The first draft of the manuscript was developed by MZH under the supervision of KDR, DMB, and WTS. All authors contributed to the manuscript revision process, and they read and approved the final version before the submission.
Funding
This work was supported by the HCL Foundation, India (Grant Number- JHU: 124005). The funding organization did not have any participation in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the article for publication.
Declaration of competing interest
None.
Footnotes
AIC = Akaike information criterion; CI = Confidence intervals; EFS = External financial support; ICC = Intraclass correlation coefficient; Int.$ = International.$; MCFA = Multilevel confirmatory factor analysis; LL = Log-Likelihood; PPP = Purchasing power parity; SASCAT-I = Shortened and adapted social capital assessment tool in India; SD = Standard deviation; VIF = Variance inflation factor.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2021.100901.
Contributor Information
Md Zabir Hasan, Email: zabir.hasan@gmail.com.
William T. Story, Email: william-story@uiowa.edu.
David M. Bishai, Email: dbishai1@jhu.edu.
Akshay Ahuja, Email: akshay-a@hcl.com.
Krishna D. Rao, Email: kdrao@jhu.edu.
Shivam Gupta, Email: sgupta23@jhu.edu.
Ethical approval
Ethical approval for the study was received from the Institutional Review Board Office of Johns Hopkins Bloomberg School of Public Health, Maryland, USA (IRB No: 00007469) and locally from the Center for Media Studies, New Delhi, India (IRB No: IRB00006230).
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Aitchison J. On the distribution of a positive random variable having a discrete probability mass at the origin. Journal of the American Statistical Association. 1955;50(271):901–908. [Google Scholar]
- Al Kibria G.M., Swasey K., Hasan M.Z., Sharmeen A., Day B. Prevalence and factors associated with underweight, overweight and obesity among women of reproductive age in India. Global Health Research and Policy. 2019;4 doi: 10.1186/s41256-019-0117-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson L.R., Mellor J.M. Social capital and health. Springer; 2008. The economic approach to cooperation and trust; pp. 117–136. [Google Scholar]
- Andreoni J. Giving with impure altruism: Applications to charity and Ricardian equivalence. Journal of Political Economy. 1989;97(6):1447–1458. doi: 10.1086/261662. [DOI] [Google Scholar]
- Bhageerathy R., Nair S., Bhaskaran U. A systematic review of community-based health insurance programs in South Asia. The International Journal of Health Planning and Management. 2017;32(2):e218–e231. doi: 10.1002/hpm.2371. [DOI] [PubMed] [Google Scholar]
- Bourdieu P. In: Handbook of theory and research for the sociology of education. Richardson J., editor. 1986. The forms of capital; pp. 241–258.http://architecturalnetworks.research.mcgill.ca/assets/w06_bourdieu.pdf Greenwood. [Google Scholar]
- Carpiano R.M. In: Social capital and health. Kawachi I., Subramanian S.V., Kim D., editors. Springer New York; 2008. Actual or potential neighborhood resources for health; pp. 83–93. [DOI] [Google Scholar]
- Chou Y.K. Three simple models of social capital and economic growth. The Journal of Socio-Economics. 2006;35(5):889–912. doi: 10.1016/j.socec.2005.11.053. psyh. [DOI] [Google Scholar]
- Claridge T. Explanation of different levels of social capital. Social Capital Research & Training. 2018 https://www.socialcapitalresearch.com/levels-of-social-capital/ January 28. [Google Scholar]
- De Silva M.J., Huttly S.R., Harpham T., Kenward M.G. Social capital and mental health: A comparative analysis of four low income countries. Social Science & Medicine. 2007;64(1):5–20. doi: 10.1016/j.socscimed.2006.08.044. [DOI] [PubMed] [Google Scholar]
- De Weerdt J. Insurance Against; 2004. Risk sharing and endogenous group formation. [Google Scholar]
- Dercon S. Vol. 2002. 2002. (Income risk, coping strategies and safety nets). 27. [Google Scholar]
- Desai S.B., Dubey A., Joshi B.L., Sen M., Shariff A., Vanneman R. Oxford University; New York: 2010. Human development in India. [Google Scholar]
- Dhanaraj S. Economic vulnerability to health shocks and coping strategies: Evidence from Andhra Pradesh, India. Health Policy and Planning. 2016;31(6):749–758. doi: 10.1093/heapol/czv127. [DOI] [PubMed] [Google Scholar]
- Domínguez S., Watkins C. Creating networks for survival and mobility: Social capital among african-American and Latin-American low-income mothers. Social Problems. 2003;50(1):111–135. doi: 10.1525/sp.2003.50.1.111. [DOI] [Google Scholar]
- Donfouet H.P.P., Mahieu P.-A. Community-based health insurance and social capital: A review. Health Economics Review. 2012;2(1):5. doi: 10.1186/2191-1991-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fafchamps M. Edward Elgar Publishing; 2003. Rural poverty, risk and development. [Google Scholar]
- Fang K., Shia B.-C., Ma S. Health insurance coverage, medical expenditure and coping strategy: Evidence from Taiwan. BMC Health Services Research. 2012;12:442. doi: 10.1186/1472-6963-12-442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanville J.L., Story W.T. Social capital and self-rated health: Clarifying the role of trust. Social Science Research. 2018;71:98–108. doi: 10.1016/j.ssresearch.2018.01.002. [DOI] [PubMed] [Google Scholar]
- Goli S., Maurya N.K., Sharma M.K. Continuing caste inequalities in rural Uttar Pradesh. International Journal of Sociology & Social Policy. 2015;35(3/4):252–272. doi: 10.1108/IJSSP-07-2014-0051. [DOI] [Google Scholar]
- Hasan M.Z., Cohen J.E., Bishai D., Kennedy C.E., Rao K.D., Ahuja A. Social capital and peer influence of tobacco consumption: A cross-sectional study among household heads in rural Uttar Pradesh, India. BMJ Open. 2020;10(6) doi: 10.1136/bmjopen-2020-037202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan M.Z., Dean L.T., Kennedy C.E., Ahuja A., Rao K.D., Gupta S. Social capital and utilization of immunization service: A multilevel analysis in rural Uttar Pradesh, India. SSM - Population Health. 2020;10:100545. doi: 10.1016/j.ssmph.2020.100545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan M.Z., Leoutsakos J.-M., Story W.T., Dean L.T., Rao K.D., Gupta S. Exploration of factor structure and measurement invariance by gender for a modified shortened adapted social capital assessment tool in India. Frontiers in Psychology. 2019;10:2641. doi: 10.3389/fpsyg.2019.02641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heck R.H., Thomas S.L. Routledge; 2015. An introduction to multilevel modeling techniques: MLM and SEM approaches using Mplus. [Google Scholar]
- Hoque M.E., Dasgupta S.K., Naznin E., Al Mamun A. Household coping strategies for delivery and related healthcare cost: Findings from rural Bangladesh. Tropical Medicine and International Health. 2015;20(10):1368–1375. doi: 10.1111/tmi.12546. [DOI] [PubMed] [Google Scholar]
- International Institute for Population Sciences & Icf . 2017. India national family health survey NFHS-4 2015-16. IIPS and ICF.http://dhsprogram.com/pubs/pdf/FR339/FR339.pdf [Google Scholar]
- World Bank . In: Attacking poverty. Kanbur S.M.R., Lustig N., editors. Oxford University Press; 2000. Helping poor people manage risk; pp. 135–159. (Published for the World Bank). [Google Scholar]
- Kawachi I., Subramanian S.V. Social epidemiology for the 21st century. Social Science & Medicine. 2018;196:240–245. doi: 10.1016/j.socscimed.2017.10.034. [DOI] [PubMed] [Google Scholar]
- Kawachi I., Takao S., Subramanian S.V., editors. Global perspectives on social capital and health. Springer; New York: 2013. [DOI] [Google Scholar]
- Kondo N., Shirai K. In: Global perspectives on social capital and health. Kawachi I., Takao S., Subramanian S.V., editors. Springer; 2013. Microfinance and health; pp. 239–275. [DOI] [Google Scholar]
- Kowal P., Afshar S. Health and the Indian caste system. The Lancet. 2015;385(9966):415–416. doi: 10.1016/S0140-6736(15)60147-7. [DOI] [PubMed] [Google Scholar]
- Kruk M.E., Goldmann E., Galea S. Borrowing and selling to pay for health care in low- and middle-income countries. Health Affairs. 2009;28(4):1056–1066. doi: 10.1377/hlthaff.28.4.1056. [DOI] [PubMed] [Google Scholar]
- Lakon C.M., Godette D.C., Hipp J.R. In: Social capital and health. Kawachi I., Subramanian S.V., Kim D., editors. Springer New York; 2008. Network-based approaches for measuring social capital; pp. 63–81. [DOI] [Google Scholar]
- Lin N. Cambridge University Press; 2001. Social capital: A theory of social structure and action. [DOI] [Google Scholar]
- Maldonado G., Greenland S. Simulation study of confounder-selection strategies. American Journal of Epidemiology. 1993;138(11):923–936. doi: 10.1093/oxfordjournals.aje.a116813. [DOI] [PubMed] [Google Scholar]
- Malehi A.S., Pourmotahari F., Angali K.A. Statistical models for the analysis of skewed healthcare cost data: A simulation study. Health Economics Review. 2015;5 doi: 10.1186/s13561-015-0045-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Michalski J.H. Financial altruism or unilateral resource exchanges? Toward a pure sociology of welfare. Sociological Theory. 2003;21(4):341–358. [Google Scholar]
- Mohnen S.M., Groenewegen P.P., Völker B., Flap H. Neighborhood social capital and individual health. Social Science & Medicine. 2011;72(5):660–667. doi: 10.1016/j.socscimed.2010.12.004. [DOI] [PubMed] [Google Scholar]
- Morduch J. Between the state and the market: Can informal insurance patch the safety net? The World Bank Research Observer. 1999;14(2):187–207. [Google Scholar]
- National Health Accounts Technical Secretariat, National Health Systems Resource Centre, & Ministry of Health and Family Welfare . 2019. National health accounts estimates for India 2016-17.http://nhsrcindia.org/sites/default/files/FINAL%20National%20Health%20Accounts%202016-17%20Nov%202019-for%20Web.pdf [Google Scholar]
- National Sample Survey Office . 2019. Key indicators of social consumptionin India: Health (NSS KI (75/25.0)). Ministry of statistics and prosramme implementation.http://www.mospi.gov.in/sites/default/files/publication_reports/KI_Health_75th_Final.pdf [Google Scholar]
- Nguyen K.T., Khuat O.T.H., Ma S., Pham D.C., Khuat G.T.H., Ruger J.P. Coping with health care expenses among poor households: Evidence from a rural commune in Vietnam. Social Science & Medicine. 2012;74(5):724–733. doi: 10.1016/j.socscimed.2011.10.027. 1982. [DOI] [PubMed] [Google Scholar]
- Nyswander D.B. Education for health: Some principles and their application. Health Education Monographs. 1956;14:65–70. [Google Scholar]
- O'Donnell O., van Doorslaer E., Wagstaff A., Lindelow M. The World Bank; 2007. Analyzing health Equity using household survey data: A Guide to techniques and their Implementation. [DOI] [Google Scholar]
- Patel V., Parikh R., Nandraj S., Balasubramaniam P., Narayan K., Paul V.K. Assuring health coverage for all in India. Lancet (London, England) 2015;386(10011):2422–2435. doi: 10.1016/S0140-6736(15)00955-1. [DOI] [PubMed] [Google Scholar]
- Portes A. Social capital: Its origins and applications in modern sociology. Annual Review of Sociology. 1998;24(1):1–24. doi: 10.1146/annurev.soc.24.1.1. [DOI] [Google Scholar]
- Portes A. Downsides of social capital. Proceedings of the National Academy of Sciences of the United States of America. 2014;111(52):18407–18408. doi: 10.1073/pnas.1421888112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quintussi M., Van de Poel E., Panda P., Rutten F. Economic consequences of ill-health for households in northern rural India. BMC Health Services Research. 2015;15 doi: 10.1186/s12913-015-0833-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ranson M.K. Community-based health insurance schemes in India: A review. The National Medical Journal of India. 2003;16(2):79–89. [PubMed] [Google Scholar]
- Ravallion M. 2016. The economics of poverty: History, measurement, and policy./z-wcorg/ [Google Scholar]
- Rice N., Jones A. Multilevel models and health economics. Health Economics. 1997;6(6):561–575. doi: 10.1002/(sici)1099-1050(199711)6:6<561::aid-hec288>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- Russell S.J. 2001. Can households afford to be ill? : The role of the health system, material resources and social networks in Sri Lanka.http://researchonline.lshtm.ac.uk/682239/ [Google Scholar]
- Russell S.J., Fox-Rushby J., Arhin D. Willingness and ability to pay for health care: A selection of methods and issues. Health Policy and Planning. 1995;10(1):94–101. doi: 10.1093/heapol/10.1.94. [DOI] [PubMed] [Google Scholar]
- Sangar S., Dutt V., Thakur R. Economic burden, impoverishment, and coping mechanisms associated with out-of-pocket health expenditure in India: A disaggregated analysis at the state level. The International Journal of Health Planning and Management. 2019;34(1):e301–e313. doi: 10.1002/hpm.2649. [DOI] [PubMed] [Google Scholar]
- Sauzet O., Razum O., Widera T., Brzoska P. Two-Part Models and quantile regression for the analysis of survey data with a spike. The example of satisfaction with health care. Frontiers in Public Health. 2019;7 doi: 10.3389/fpubh.2019.00146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serra R. Institute of Development Studies (IDS); 1999. Putnam in India: Is social capital a Meaningful and measurable concept at Indian state level?https://opendocs.ids.ac.uk/opendocs/handle/20.500.12413/3413 [Google Scholar]
- Srivatsan R. Reflections on discrimination and health in India. Indian Journal of Medical Ethics. 2015;12(1):13–17. doi: 10.20529/IJME.2015.004. [DOI] [PubMed] [Google Scholar]
- Story W.T. Social capital and the utilization of maternal and child health services in India: A multilevel analysis. Health & Place. 2014;28:73–84. doi: 10.1016/j.healthplace.2014.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The World Bank . 2017. PPP conversion factor for India, GDP (LCU per international $)https://data.worldbank.org/indicator/PA.NUS.PPP?locations=IN [Google Scholar]
- Townsend R.M. Consumption insurance: An evaluation of risk-bearing systems in low-income economies. The Journal of Economic Perspectives. 1995;9(3):83–102. [Google Scholar]
- Valente T.W., Hoffman B.R., Ritt-Olson A., Lichtman K., Johnson C.A. Effects of a social-network method for group Assignment strategies on peer-led tobacco prevention programs in schools. American Journal of Public Health. 2003;93(11):1837–1843. doi: 10.2105/ajph.93.11.1837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villalonga-Olives E., Kawachi I. The dark side of social capital: A systematic review of the negative health effects of social capital. Social Science & Medicine. 2017;1982(194):105–127. doi: 10.1016/j.socscimed.2017.10.020. [DOI] [PubMed] [Google Scholar]
- World Bank . The World Bank; 2014. World development report 2015: Mind, society, and behavior. [DOI] [Google Scholar]
- World Health Organization . WHO; 2017. Out-of-pocket payments, user fees and catastrophic expenditure.http://www.who.int/health_financing/topics/financial-protection/out-of-pocket-payments/en/ [Google Scholar]
- Yadav J., Menon G.R., John D. Catastrophic health expenditure and impoverishment effects in India: An analysis of national health survey data. Applied health economics and health policy. 2021. Disease-specific out-of-pocket payments. [DOI] [PubMed] [Google Scholar]
- Zhao T., Luo X., Chu H., Le C.T., Epstein L.H., Thomas J.L. A two-part mixed effects model for cigarette purchase task data. Journal of the Experimental Analysis of Behavior. 2016;106(3):242–253. doi: 10.1002/jeab.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao J., Zhao Y., Xiang L., Khanal V., Binns C.W., Lee A.H. A two-part mixed-effects model for analyzing clustered time-to-event data with clumping at zero. Computer Methods and Programs in Biomedicine. 2020;187:105196. doi: 10.1016/j.cmpb.2019.105196. [DOI] [PubMed] [Google Scholar]
- Zodpey S., Farooqui H.H. Universal health coverage in India: Progress achieved & the way forward. Indian Journal of Medical Research. 2018;147(4):327–329. doi: 10.4103/ijmr.IJMR_616_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.