Abstract
When youth in the emergency department become acutely agitated, it can be dangerous and distressing to patients, families, and clinicians. Timely, effective, and patient-centered management is key to reducing the potential for patient and staff injury while preserving patient dignity. We review the definition of agitation and pharmacologic management for youth with acute agitation, including common classes of medications, indications for use, and adverse effects. We also discuss the need to integrate the use of medications into a comprehensive strategy for agitation management that begins with proactive prevention of aggressive behavior, creation of a therapeutic treatment environment, and verbal de-escalation strategies.
Keywords: Agitation, Aggression, Youth, Mental Health, Emergency Psychiatry, Antipsychotics, Benzodiazepines
Target Audience:
This CME activity is intended for health care clinicians who care for youth at risk for agitation, such as youth with mental health conditions, substance use, developmental delay, or autism spectrum disorder. The target audience includes emergency medicine physicians, pediatricians, psychiatrists, physician assistants, and nurse practitioners.
Learning Objectives:
After completion of this article, the reader should be able to:
Recognize and differentiate mild, moderate, and severe agitation in youth.
Describe considerations in the choice of medication for the management of agitation in youth, including common and severe medication adverse effects.
Understand how medications fit into a comprehensive strategy for the management of agitation in youth in the emergency department.
Acute agitation of youth in the emergency department (ED) can be dangerous and distressing to patients, families, and clinicians.1 ED visits for mental health conditions among children are rising in the U.S., with the use of pharmacologic restraint increasing more than threefold from 2009–2019.2,3 Among children seen in the ED for a mental health condition, 2–12% require intramuscular medication for agitation management and 5–10% require physical restraints.3,4 Agitation is a frequent cause of injuries to patients and medical staff, with at least 30 reported pediatric deaths in the U.S. due to restraint-related incidents.5,6 Agitation care must be proactive, timely, effective, and patient-centered in order to ensure safety and preserve patient dignity. Here, we review the pharmacologic management of agitation in youth in the ED and discuss the role of medications as part of a comprehensive strategy for agitation management.
Initial Assessment and Management of the Child or Adolescent with Agitation
The first step to the management of agitation in the ED is to ensure the safety of the patient and staff. Patient belongings should be removed, and, when safe to do so, the patient should be changed into a gown to ensure there are no items or substances on the patient that might cause harm to the patient or staff. The patient should be placed in a specialized safe room if available. If the patient is placed in a standard ED room, potentially dangerous items should be removed. A facility-specific checklist may assist in ensuring the removal of items such as the contents of sharps containers, oxygen tanks, poles used to hang intravenous fluids, trash cans, glove boxes, and chairs. The appropriate level of observation of the patient should be initiated, including one-to-one nursing or security if needed. If available, a behavioral rapid response team may be activated. A behavioral rapid response is an emerging strategy to ensure that all relevant staff members arrive to the bedside of a patient with acute agitation in a coordinated and timely fashion.7
Next, the clinician should perform a focused history and physical examination to assess the etiology of the patient’s agitation and identify underlying medical conditions that could be life-threatening. Although patients who are acutely agitated may not be able to cooperate with portions of the physical examination, the use of de-escalation strategies may enhance cooperation.1 If the clinician is unable to perform a comprehensive physical examination initially, a more thorough examination should be pursued as soon as agitation improves.
Several potential etiologies for acute agitation deserve consideration. First, agitation may be due to delirium, which is characterized by waxing and waning mental status associated with an underlying medical problem such as a metabolic, neurologic, traumatic, hypoxic, or infectious condition. Second, agitation may be due to substance intoxication, poisoning, or withdrawal. In particular, opioid withdrawal and ethanol intoxication and withdrawal must be considered. Additional classes of drugs that may cause agitation include sympathomimetics, hallucinogens, immunomodulatory drugs, antiepileptics, and anticholinergics. For patients with prescribed psychotropic medications, serotonin syndrome and neuroleptic malignant syndrome should also be considered as they may be life-threatening. Drug-related agitation may be suspected by history, due to the presence of a specific toxidrome, or based on laboratory testing such as a positive urine toxicology panel or serum ethanol level. Third, acute psychiatric presentations of psychosis or bipolar disorder may result in acute agitation. Fourth, conditions that cause pain may lead to agitation, particularly among patients with communication disorders, intellectual disability, developmental delay, or autism spectrum disorder. For these patients, the clinician should carefully assess for potential causes of pain such as acute otitis media, dental abscess, urinary tract infection, or constipation.
In tandem with the assessment of the etiology of agitation, an accurate determination of the severity of agitation is necessary to guide management. Mild agitation includes behaviors such as fidgeting, pulling at clothes or hair, hand writing, nail biting, difficulty sitting still, and irritability. Moderate agitation involves raising the voice or yelling, making threatening statements, pacing, rocking, throwing small objects without aiming at others, lightly scratching without breaking skin, hitting lightly, or brief head banging. Severe agitation is defined by behaviors that place the patient or others at imminent risk of harm. This includes attempts to assault others, moving or throwing large objects, destroying property, strangulation attempts, attempts to cut or deep scratching of skin, or forceful or prolonged head banging.
All levels of agitation share several management strategies. Verbal de-escalation techniques should be attempted first, and can be an effective means of achieving quick resolution of agitation (Table 1). The clinician should respect the patient’s personal space and maintain a calm demeanor, facial expression, and posture. Stimulation should be minimized by dimming lights, reducing noise, and minimizing staff when safe to do so. It is essential for the clinician to consider a child’s developmental level and preferred means of communication. Instructions should be given one step at a time, allowing the patient adequate time to process the information and respond. The patient should be offered choices (e.g. “Would you prefer that I take your temperature first or measure your heart rate first?”), and cooperation should be positively rewarded. Children with autism spectrum disorder may particularly benefit from soothing sensory items and visuals for communication, such as storyboards that visually depict upcoming tasks. It is always best to ask the parent or guardian what works best for their child. If the patient has an existing scheduled home medication that can target the presenting behavior, the clinician may consider administering it earlier than scheduled. Multidisciplinary collaboration with child life, social work, and/or psychiatry may be helpful to ensure a complete evaluation that addresses the patient’s individual needs.
Table 1.
Verbal de-escalation techniques for youth with acute agitation
| De-escalation Technique | Example |
|---|---|
| Respect personal space | 2 arm length distance |
| Body language | Calm demeanor, facial expression, posture |
| Minimize stimulation | Dim lights, reduce noise, minimize staff |
| Simple instructions | Single step, with adequate time to respond |
| Ask patient what helps | “What helps you at times like this?” |
| Active listening | “Tell me if I have this right,” “What I heard is…” |
| Build empathy | “What you’re experiencing is difficult” |
| Set expectations and consequences | “If you’re having a hard time staying safe or controlling your behavior, we will…” |
| Choices, redirection, distraction | “What else could you do? Would (activity) help?” |
| Reward cooperation | Snacks, crayons, toys, stickers |
| Soothing sensory tools | Vibration tube, fidget toys, sunglasses, headphones, vibrating teether, chewy tubes, rainstick, pop tubes, bells |
| Enhance communication | Visuals such as storyboards, demonstration, have caregiver give instructions |
Pharmacologic Treatment of Acute Agitation in Children and Adolescents
Pharmacologic treatment is indicated to treat moderate or severe agitation when verbal de-escalation techniques fail or when needed to promote safety. Few rigorously designed studies have assessed the effectiveness and safety of medications for acute agitation in children. The current body of evidence includes one randomized controlled trial and a handful of observational studies conducted in the emergency department, pre-hospital setting, and inpatient psychiatric units. Current practice is based on these studies in combination with clinical experience, extrapolation from the adult literature, and the consensus of experts.1,8 Notable references include Project BETA (Best Practices for the Evaluation and Treatment of Agitation) consensus guidelines by child and adolescent psychiatrists and the American Academy of Pediatrics Clinical Report on the management of children and adolescents with psychiatric emergencies.1,9
Several medication classes are available for treatment of agitation in youth, including antihistamines, benzodiazepines, and antipsychotics (Table 2).10,11 The primary consideration when choosing a medication should be the etiology and severity of the patient’s agitation. Additional considerations may include prior successful response to a particular medication, interaction with medications received at home or in the ED, pharmacologic properties of the medication such as its onset and duration of action, availability of particular routes of administration (such as an orally dissolving formulation), and patient or family preference.
Table 2.
Medications commonly used for treatment of acute agitation in youth
| Medication | Route and Initial Dose | Onset of Action | Peak Effect | Duration of Action | Maximum Daily Dose1 | Adverse Effects | Additional Notes |
|---|---|---|---|---|---|---|---|
| Diphenhydramine | PO/IM: 1 mg/kg/dose Max: 50 mg/dose |
PO: 1 hour IM: 5–15 min |
PO: 2–4 hours IM: 2 hours |
4–6 hours | Child: 50–100 mg Adolescent: 100–200 mg |
Paradoxical reactions, disinhibition, anticholinergic effects | Avoid in delirium. Co-administered along with haloperidol to prevent EPS. |
| Lorazepam | PO/IM/IV: 0.05–0.1 mg/kg/dose Max: 2 mg/dose |
PO: 20–30 min IM/IV: 15–30 min |
PO: 2 hours IM: 2 hours IV: 15–30 min |
6–8 hours | Child: 4 mg Adolescent: 6 mg |
Paradoxical reactions, disinhibition, respiratory depression | Preferred for agitation due to intoxication. Do not give IM olanzapine within 1 hour of IM/IV benzodiazepine. |
| Haloperidol | PO/IM: 0.05–0.1 mg/kg/dose Child: 2 mg/dose Adolescent: 5 mg/dose |
PO: 1 hour IM: 15–30 min |
PO: 2–3 hours IM: 20 min |
3–8 hours | Child: 5 mg/day Adolescent: 15 mg/day |
QTc prolongation, EPS risk, NMS, hypotension | Co-administer with diphenhydramine to prevent EPS. |
| Chlorpromazine | PO/IM: 0.55 mg/kg/dose Max: 50 mg/dose |
PO: 30–60 min IM:15 min |
PO: 30–60 min IM: 15 min |
4–6 hours | Child: 75–100 mg/day Adolescent: 200 mg/day |
QTc prolongation EPS, NMS, hypotension |
|
| Olanzapine | PO/IM: 0.1 mg/kg/dose Child: 2.5 mg/dose Adolescent: 5 mg/dose |
PO: 20–30 min IM: 15 min |
PO: 5–6 hours IM:15–45 min |
24 hours | 10–20 mg/day | EPS, NMS, hypotension, anticholinergic effects | Do not give IM olanzapine within 1 hour of IM/IV benzodiazepine. |
EPS: Extrapyramidal symptoms; NMS: Neuroleptic malignant syndrome; PO: by mouth; IM: intramuscular: IV: intravenous
Maximum total daily doses may differ in patients with prior exposure to the medication.
Antihistamines
Diphenhydramine works by competing with histamine at H1–1 receptors to provide antihistamine effects. A double-blind, placebo-controlled trial of 21 children 5–13 years old hospitalized in an inpatient psychiatric unit compared oral and intramuscular (IM) diphenhydramine to oral and IM placebo. Patient behavior, as measured on two standardized scales, did not differ between diphenhydramine and placebo groups. The intramuscular route was more effective than the oral route, regardless of whether active drug or placebo was given.12 Despite limited available evidence for its efficacy, diphenhydramine is widely used in practice; for instance, in a retrospective study of psychotropic pro re nata (PRN) medications in an inpatient adolescent psychiatric unit, diphenhydramine was the most commonly prescribed medication.8 Diphenhydramine should be avoided when delirium is the etiology of agitation, as it may cause increased confusion. It is often considered for younger children due to its favorable safety profile with few adverse effects. Clinicians who do not commonly prescribe psychotropic medications may feel more comfortable with its use, given its other indications such as treatment of allergic reactions. Adverse effects may include paradoxical reactions or disinhibition. If multiple doses are administered in a short time frame, an anticholinergic toxidrome could result, consisting of hallucinations, confusion, flushing, dry mouth, diminished bowel sounds, tachycardia, dilated pupils, and urinary retention.
Benzodiazepines
Benzodiazepines are a class of medications used to treat moderate or severe agitation that work through enhancement of GABA transmission. Benzodiazepines used for the management of agitation include lorazepam, midazolam, and diazepam. They are the preferred class of medications for agitation due to substance intoxication (except for alcohol intoxication, due to the increased risk of respiratory depression), substance withdrawal, catatonia, and severe anxiety. For agitation due to delirium, benzodiazepines should generally be avoided as they may cause increased confusion.1 Benzodiazepines may occasionally cause paradoxical agitation or disinhibition. In a retrospective study of youth less than 20 years of age treated for agitation at a single pediatric emergency department, only 2 (2%) of 85 youth who received lorazepam had a paradoxical reaction, with one requiring additional medication as treatment.13 Patients who receive benzodiazepines should also be monitored for respiratory depression or hypotension.
Antipsychotic Medications
Antipsychotic medications, also known as neuroleptics, are used to treat severe agitation. There are two major classes of antipsychotic medications: first-generation antipsychotics (also known as typical antipsychotics), first available in the 1950s, and second-generation antipsychotics (also known as atypical antipsychotics), introduced in the 1990s. First-generation antipsychotics have strong post-synaptic blockade of dopamine D2 receptors in the brain. Drug activity in the meso-limbo-cortical system is thought to explain the antipsychotic activity of these medications, whereas neurological side effects such as extrapyramidal symptoms (EPS) result from activity in the nigrostriatal system. Relative to second-generation antipsychotics, most first-generation antipsychotics have stronger D2 receptor affinity, which leads to increased risk of EPS. In contrast, most second-generation antipsychotics (besides risperidone) have lower D2 receptor affinity, can be partial agonists at dopamine receptors, and have serotonin 5HT2 receptor binding properties.14 Because they do not rely on dopamine receptors as their sole mechanism of action, the risk of EPS is lower.
Clinicians should be aware of several potential adverse effects of antipsychotic medications. One of the most common extrapyramidal symptoms is an acute dystonic reaction, which consists of involuntary, slow, sustained contractions of muscle groups, resulting in twisting, repetitive movements and abnormal posturing. Types of dystonic reactions include rigid contraction of back muscles with arching (opisthotonos), neck extension (retrocollis), torticollis, sustained eye deviation (oculogyric crisis), tongue protrusions which can lead to choking, and rarely laryngeal or pharyngeal spasms which can be fatal. While some dystonic reactions occur within hours of medication administration, the majority of dystonic reactions occur within a few days of initiation of a standing antipsychotic medication regimen. They may be treated with diphenhydramine or benztropine. Another common extrapyramidal symptom is akathisia, which is a subjective feeling of inner restlessness manifested by a need to be in constant movement. Stopping the offending antipsychotic agent, lowing the dose, or treating with propranolol or benztropine may be beneficial.15
Additionally, antipsychotics may cause cardiovascular side effects such as QTc prolongation and orthostatic hypotension. Although rare, QTc prolongation has been associated with ventricular arrhythmias (torsade de pointes), which in turn may progress to ventricular fibrillation and can be fatal. Thus, it is important to obtain a cardiac history prior to administration, and the potential for interaction with home medications and other medications given in the ED must be carefully considered. When multiple doses of antipsychotic medications are administered, the clinician may consider ordering an electrocardiogram to monitor the QTc interval. While orthostatic hypotension has been described as a side effect of antipsychotic medications, it is typically self-limited without requiring intervention.
A rare but potentially fatal adverse reaction of antipsychotics is neuroleptic malignant syndrome, which is characterized by fever, altered mental status, severe muscle rigidity, and autonomic dysfunction. Laboratory analysis may demonstrate elevated levels of creatine phosphokinase. Early detection and treatment can be lifesaving. Treatment includes cessation of the causative agent, supportive care such as correction of fluid and electrolyte imbalances, and the addition of bromocriptine or dantrolene for severe cases.16
First Generation Antipsychotic Medications
Haloperidol is a first-generation antipsychotic used for severe agitation. It is a potent D2 receptor antagonist with minimal anticholinergic and autonomic effects. It is often administered in combination with lorazepam for patients with severe agitation. Intramuscular administration is recommended, as intravenous administration may be associated with an increased risk of QTc prolongation and torsades de pointes.17 To prevent extrapyramidal reactions, coadministration with diphenhydramine or benztropine may also be considered. Haloperidol is a preferred agent for the treatment of alcohol intoxication.1
Chlorpromazine is a first-generation antipsychotic medication with a long history of use in the treatment of agitation. In a retrospective study of children and adolescents admitted to a residential treatment program in Canada, chlorpromazine was the most frequently used PRN medication for aggressive behavior (with 665 administrations, representing 40% of all PRN medications used) with no reported side effects other than drowsiness, including no cases of extrapyramidal side effects.18
Droperidol is a first-generation antipsychotic medication used to treat agitation that belongs to the same subclass of antipsychotics as haloperidol. In 2007, the Food and Drug Administration placed a black-box warning on droperidol related to its potential for QTc prolongation and case reports of torsades de pointes. Subsequent reviews of the data suggest that this warning based on a very limited number of adverse events, mostly involving doses of droperidol much higher than those typically used to treat agitation in the United States.19 Droperidol has been widely used for agitation management in adults with few adverse effects reported in practice, including in a study of 12,000 adults with no occurrence of dysrhythmias.20 Recent studies have demonstrated reasonable safety and effectiveness in children and adolescents. For instance, a prospective observational study of droperidol for prehospital acute behavioral disturbance in children demonstrated a median time to sedation of 14 minutes and 8 cases (8%) of adverse events among 102 administrations: 5 with hypotension (1 of which required treatment with intravenous fluids), 2 dystonic reactions, and 1 with respiratory depression.21
Second-Generation Antipsychotic Medications
Olanzapine is a second-generation antipsychotic that is available in an orally dissolving tablet, in addition to an intramuscular formulation and standard tablet. Several studies have supported its effectiveness in the treatment of agitation among youth. In a retrospective study of 338 children and adolescents admitted to a residential treatment program in Canada, olanzapine was more likely than lorazepam or chlorpromazine to produce adequate sedation within 30 minutes.18 Among 166 children and adolescents who received olanzapine for agitation in a pediatric ED, most were adequately sedated, with 17% requiring another sedative within 1 hour.22 Olanzapine appears to have less of a QTc prolonging effect than other commonly used antipsychotic medications.23 Based on current effectiveness and safety data, along with the availability of multiple formulations (such as the orally dissolving tablet), olanzapine is the favored antipsychotic of the authors of this review for the management of severe agitation in youth. Due to case reports of cardiorespiratory suppression, olanzapine should not be given parenterally within 1 hour of a parenteral benzodiazepine.24
Ziprasidone is a second-generation antipsychotic medication that may be used to treat severe agitation. In a retrospective study of 100 youth in an inpatient psychiatric unit who received either IM ziprasidone or IM olanzapine, no differences were found in medication efficacy, the number of patients who required restraints, or duration of restraint use. However, the mean number of doses of emergency medication received for acute agitation or aggression during the hospitalization was significantly higher in the ziprasidone group.25 In a retrospective case-control study of 52 adolescents in a psychiatric ED who received either IM ziprasidone or IM haloperidol/lorazepam, no differences were found between the two groups in the duration of restraint use or the need for additional medication within 60 minutes.26
Physical Restraints
Due to their restrictive nature, physical restraints are used only as a measure of last resort when needed to ensure the safety of the patient or staff. Physical restraints include manual holding of the patient or the use of devices such as wrist or ankle straps. In a survey conducted to study restraint practices, most emergency medicine clinicians reported that 5% or fewer youth undergoing emergency psychiatric evaluation at their institution receive physical restraints.27 In support of this estimate, a retrospective study of physical restraint use in a pediatric ED demonstrated a 6.8% frequency of physical restraint use among children undergoing emergency psychiatric evaluation.4 The preferred position for physical restraint is supine without pressure placed on the patient’s head or neck.27 Frequent reassessments should be performed to monitor the patient’s alertness, respiratory status, circulation, and level of agitation. Changes in position may aid in preventing rhabdomyolysis, pressures sores, and paresthesias. Physical restraints should be removed as soon as it is safe to do so. Clinicians should familiarize themselves with regulatory requirements associated with the application of physical restraints.27
Care Following an Episode of Agitation
After medication is administered for agitation, monitoring for potential adverse effects should be initiated, including observation of the patient’s level of alertness, respiratory status, and blood pressure. Prior to administering a second dose of medication, the clinician must allow sufficient time for the initial medication to take effect, in order to avoid dose stacking, oversedation, and increased risk of other adverse medication effects. It is important to remember to continue to use verbal de-escalation techniques throughout the agitation episodes. Most youth with agitation in the ED setting do not require a second dose of medication. In a retrospective study of 128 youth who presented to a pediatric ED with agitation who received a benzodiazepine or antipsychotic, 13% received 2 doses of medication and 5% received 3 or more doses.13 Generally, a second dose of the same medication is preferable to adding multiple different medications to avoid drug interaction adverse effects. If multiple doses of antipsychotics are administered, the clinician may consider obtaining an electrocardiogram to monitor the QTc interval.
To facilitate treatment of subsequent episodes of agitation, a medication contingency plan should be developed that includes the frequencies and maximum total daily dose for each medication. Triggers for agitation and successful de-escalation strategies should be recorded and communicated between team members during care transitions through handoff tools or a longitudinal care plan. Figure 1 provides a suggested algorithm to guide comprehensive care for youth with agitation in the ED.
Figure 1.
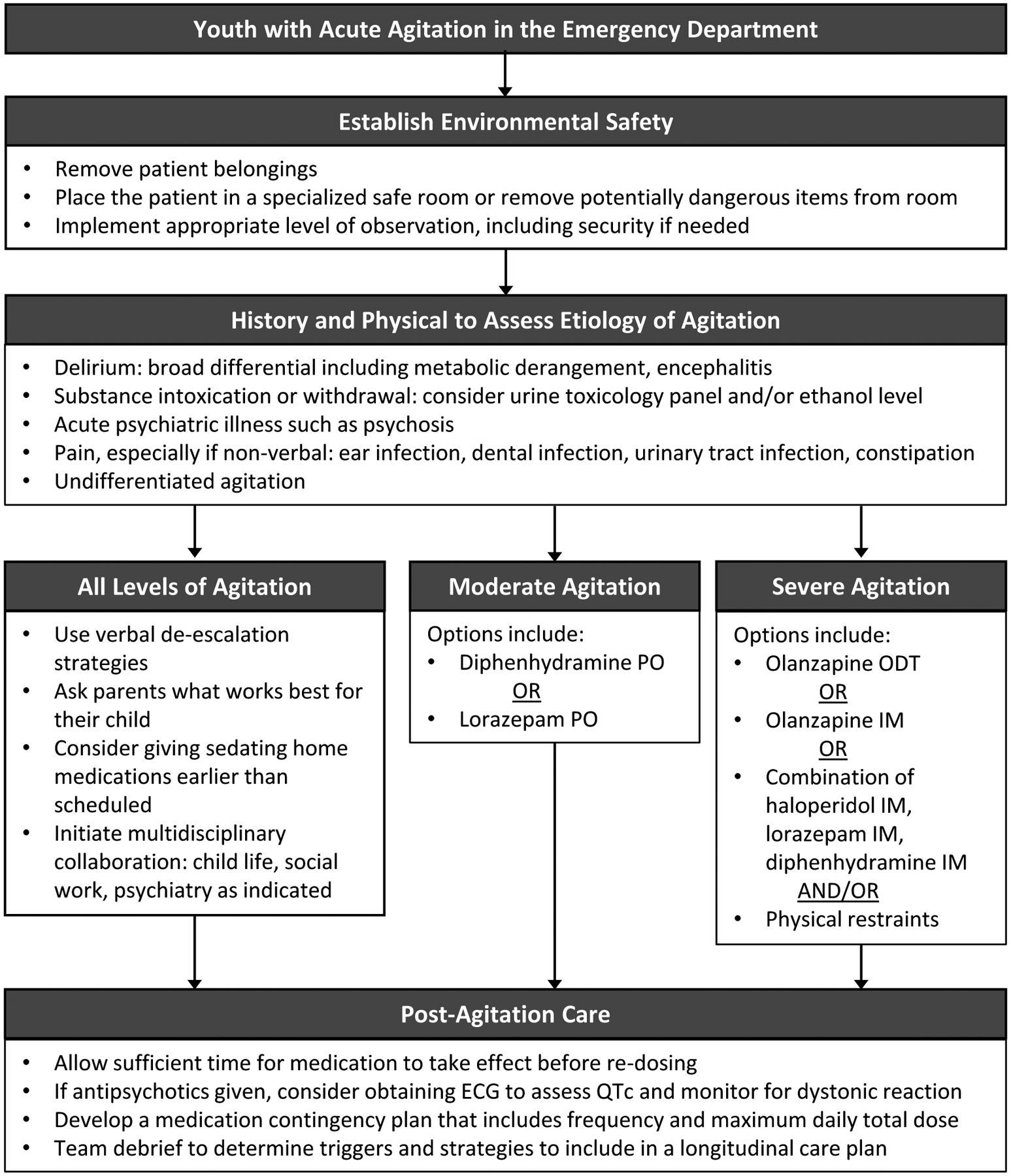
Algorithm for comprehensive care of agitation in youth in the emergency department
This algorithm may be used to guide comprehensive care for youth with agitation in the emergency department. PO: per os; ODT: orally dissolving tablet; IM: intramuscular; ECG: electrocardiogram.
Conclusion
In summary, a comprehensive strategy is required to address agitation among youth in the ED. Priorities for care include the establishment of safety, assessment of the etiology and severity of agitation, utilization of effective verbal de-escalation techniques, selection of medication, and monitoring after an episode of agitation. As there is currently limited available evidence to guide management, further research is needed to rigorously compare the effectiveness and safety of medications for agitation in children.
Multiple Choice Questions.
- Which of the following are well-described adverse effects of antipsychotic medications given for acute agitation?
- QTc prolongation
- Dystonic reaction
- Akathisia
- Neuroleptic malignant syndrome
- All of the above
- Which of the following is recommended for treatment of a dystonic reaction caused by an antipsychotic medication such as haloperidol?
- Diphenhydramine
- Lorazepam
- Chlorpromazine
- Clonidine
- Which class of medications is considered first-line for agitation due to substance intoxication or withdrawal (except for alcohol intoxication)?
- Antihistamines
- Benzodiazepines
- First-generation antipsychotics
- Second-generation antipsychotics
- Which of the following non-pharmacologic de-escalation techniques may be particularly beneficial for children with autism spectrum disorder?
- Use a calm demeanor, facial expression, and posture
- Reward patient cooperation
- Enhance communication by using visuals or demonstration
- Ask the patient what usually helps and build empathy
- Which combination of medications is NOT considered safe to give together due to the risk of cardiopulmonary depression?
- Haloperidol IM and lorazepam IM
- Olanzapine IM and lorazepam IM
- Haloperidol IM, lorazepam IM, and diphenhydramine IM
- Haloperidol IM and midazolam IM
Funding:
Dr. Jennifer Hoffmann receives grant support from the U.S. Agency for Healthcare Research and Quality (Grant 5K12HS026385-03).
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to disclose.
References
- 1.Gerson R, Malas N, Feuer V, et al. Best Practices for Evaluation and Treatment of Agitated Children and Adolescents (BETA) in the Emergency Department: Consensus Statement of the American Association for Emergency Psychiatry. West J Emerg Med. 2019;20(2):409–418. doi: 10.5811/westjem.2019.1.41344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cutler GJ, Rodean J, Zima BT, et al. Trends in Pediatric Emergency Department Visits for Mental Health Conditions and Disposition by Presence of a Psychiatric Unit. Acad Pediatr. 2019;19(8):948–955. doi: 10.1016/j.acap.2019.05.132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Foster AA, Porter JJ, Monuteaux MC, Hoffmann JA, Hudgins JD. Pharmacologic Restraint Use During Mental Health Visits in Pediatric Emergency Departments. J Pediatr. 2021;0(0). doi: 10.1016/j.jpeds.2021.03.027 [DOI] [PubMed] [Google Scholar]
- 4.Dorfman DH, Mehta SD. Restraint use for psychiatric patients in the pediatric emergency department. Pediatr Emerg Care. 2006;22(1):7–12. doi: 10.1097/01.pec.0000195758.12447.69 [DOI] [PubMed] [Google Scholar]
- 5.Chun TH, Katz ER, Duffy SJ, Gerson RS. Challenges of Managing Pediatric Mental Health Crises in the Emergency Department. Child Adolesc Psychiatr Clin N Am. 2015;24(1):21–40. doi: 10.1016/j.chc.2014.09.003 [DOI] [PubMed] [Google Scholar]
- 6.Weiss EM. Deadly restraint: A Hartford Courant Investigative Report. Hartford Courant. 1998:October11–15. [Google Scholar]
- 7.Choi KR, Omery AK, Watkins AM. An Integrative Literature Review of Psychiatric Rapid Response Teams and Their Implementation for De-escalating Behavioral Crises in Nonpsychiatric Hospital Settings. J Nurs Adm. 2019;49(6):297–302. doi: 10.1097/NNA.0000000000000756 [DOI] [PubMed] [Google Scholar]
- 8.Saito E, Eng S, Grosso C, Ozinci Z, Van Meter A. Pro Re Nata Medication Use in Acute Care Adolescent Psychiatric Unit. J Child Adolesc Psychopharmacol. 2020;30(4):250–260. doi: 10.1089/cap.2019.0131 [DOI] [PubMed] [Google Scholar]
- 9.Chun TH, Mace SE, Katz ER, et al. Evaluation and Management of Children and Adolescents With Acute Mental Health or Behavioral Problems. Part I: Common Clinical Challenges of Patients With Mental Health and/or Behavioral Emergencies. Pediatrics. 2016;138(3):e20161570. doi: 10.1542/peds.2016-1570 [DOI] [PubMed] [Google Scholar]
- 10.Lexi-Drugs.; 2015. AccessedApril 15, 2021. http://online.lexi.com/
- 11.IBM Micromedex Solutions. AccessedApril 15, 2021. http://www.micromedexsolutions.com/
- 12.Vitiello B, Hill JL, Elia J, Cunningham E, McLeer SV., Behar D. P.R.N. medications in child psychiatric patients: A pilot placebo-controlled study. J Clin Psychiatry. 1991;52(12):499–501. [PubMed] [Google Scholar]
- 13.Kendrick JG, Goldman RD, Carr RR. Pharmacologic Management of Agitation and Aggression in a Pediatric Emergency Department – A Retrospective Cohort Study. J Pediatr Pharmacol Ther. 2018;23(6):455–459. doi: 10.5863/1551-6776-23.6.455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sadock BJ, Sadock VA, Ruiz P, Kaplan HI. Kaplan and Sadock’s Comprehensive Textbook of Psychiatry. 10th ed.Wolters Kluwer; 2017. [Google Scholar]
- 15.Pringsheim T, Gardner D, Addington D, et al. The Assessment and Treatment of Antipsychotic-Induced Akathisia. Can J Psychiatry. 2018;63(11):719–729. doi: 10.1177/0706743718760288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Berman B. Neuroleptic Malignant Syndrome: A Review for Neurohospitalists. The Neurohospitalist. 2011;1(1):41–417. doi: 10.1177/1941875210386491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Meyer-Massetti C, Cheng CM, Sharpe BA, Meier CR, Guglielmo BJ. The FDA extended warning for intravenous haloperidol and torsades de pointes: How should institutions respond? J Hosp Med. 2010;5(4). doi: 10.1002/jhm.691 [DOI] [PubMed] [Google Scholar]
- 18.Swart GT, Siman E, Stewart SL. The use of pro re nata or statim medications for behavioral control: A summary of experience at a tertiary care children’s mental health center. J Child Adolesc Psychopharmacol. 2011;21(1):67–77. doi: 10.1089/cap.2010.0010 [DOI] [PubMed] [Google Scholar]
- 19.Jackson CW, Sheehan AH, Reddan JG. Evidence-based review of the black-box warning for droperidol. Am J Heal Pharm. 2007;64(11):1174–1186. doi: 10.2146/ajhp060505 [DOI] [PubMed] [Google Scholar]
- 20.Shale JH, Shale CM, Mastin WD. A review of the safety and efficacy of droperidol for the rapid sedation of severely agitated and violent patients. J Clin Psychiatry. 2003;64(5):500–505. doi: 10.4088/JCP.v64n0502 [DOI] [PubMed] [Google Scholar]
- 21.Page CB, Parker LE, Rashford SJ, Isoardi KZ, Isbister GK. A Prospective Study of the Safety and Effectiveness of Droperidol in Children for Prehospital Acute Behavioral Disturbance. Prehospital Emerg Care. 2019;23(4):519–526. doi: 10.1080/10903127.2018.1542473 [DOI] [PubMed] [Google Scholar]
- 22.Cole JB, Klein LR, Strobel AM, Blanchard SR, Nahum R, Martel ML. The Use, Safety, and Efficacy of Olanzapine in a Level i Pediatric Trauma Center Emergency Department over a 10-Year Period. Pediatr Emerg Care. 2020;36(2):70–76. doi: 10.1097/PEC.0000000000001231 [DOI] [PubMed] [Google Scholar]
- 23.Harrigan EP, Miceli JJ, Anziano R, et al. A Randomized Evaluation of the Effects of Six Antipsychotic Agents on QTc, In the Absence and Presence of Metabolic Inhibition. J Clin Psychopharmacol. 2004;24(1):62–69. doi: 10.1097/01.jcp.0000104913.75206.62 [DOI] [PubMed] [Google Scholar]
- 24.Marder SR, Sorsaburu S, Dunayevich E, et al. Case reports of postmarketing adverse event experiences with olanzapine intramuscular treatment in patients with agitation. J Clin Psychiatry. 2010;71(4):433–441. doi: 10.4088/JCP.08m04411gry [DOI] [PubMed] [Google Scholar]
- 25.Khan SS, Mican LM. A naturalistic evaluation of intramuscular ziprasidone versus intramuscular olanzapine for the management of acute agitation and aggression in children and adolescents. J Child Adolesc Psychopharmacol. 2006;16(6):671–677. doi: 10.1089/cap.2006.16.671 [DOI] [PubMed] [Google Scholar]
- 26.Jangro WC, Preval H, Southard R, Klotz SG, Francis A. Conventional intramuscular sedatives versus ziprasidone for severe agitation in adolescents: Case-control study. Child Adolesc Psychiatry Ment Health. 2009;3:1–6. doi: 10.1186/1753-2000-3-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dorfman DH, Kastner B. The Use of Restraint for Pediatric Psychiatric Patients in Emergency Departments. Pediatr Emerg Care. 2004;20(3):151–156. doi: 10.1097/01.pec.0000117921.65522.fd [DOI] [PubMed] [Google Scholar]


