Abstract
Background
The prevalence of childhood morbidity remains high in low-and middle-income countries, including sub-Saharan Africa (SSA). In this study, the association between maternal age at first childbirth and under-five morbidity in SSA was examined.
Methods
This was a cross-sectional study involving nationally-representative data from the most recent Demographic and Health Surveys conducted in 32 countries in SSA from 2010 to 2019. A sample size of 311,603 mothers of children under-five was considered. The outcome variable for this study was under-five morbidity. This variable was derived from the experience of fever, cough, and diarrhoea among children under-five. Both multilevel and binary logistic regression models were used to test the hypothesis that adolescent childbirth is associated with under-five morbidity. The results were presented as crude odds ratios (cORs) and adjusted odds ratios (aORs), with 95 % confidence intervals (CIs).
Results
Children born to mothers whose first childbirth occurred at < 20 years were 16 % times more likely to suffer from under-five morbidity, compared to those whose mothers’ first childbirth occurred at age ≥ 20 years [cOR = 1.16; CI = 1.13–1.19], and this persisted but with reduced odds after controlling for covariates [aOR = 1.10; CI = 1.07–1.12]. At the country level, children born to mothers whose first childbirth occurred at < 20 years were more likely to suffer from under-five morbidity, compared to those whose mothers’ first childbirth occurred at age ≥ 20 years in Angola, Burundi, Congo DR, Guinea, Kenya, and Uganda.
Conclusions
In this study, an association between adolescent childbirth and morbidity in children under five in SSA has been established. The study concludes that under-five morbidity is higher among children born to mothers whose first childbirth occurred before 20 years compared to those whose mothers’ first childbirth occurred at 20 years and above. The findings indicate that in order to reduce under-five morbidity, there is the need to deal with adolescent childbearing through cultural and social change, coupled with engagement of adolescents and stakeholders in adolescent sexual and reproductive health programmes.
Keywords: Age at first childbirth, Under-five morbidity, Sub-Saharan Africa, Global Health
Background
Globally, morbidity in children has been considered as the major cause of death in children under five [1]. According to the World Health Organisation (WHO), infectious diseases, including pneumonia, diarrhoea and malaria, along with pre-term birth, birth asphyxia and trauma, and congenital anomalies remain the leading causes of death for children under five [2]. The prevalence of childhood morbidity remains high in low-and middle-income countries (LMICs), including sub-Saharan Africa (SSA) [3]. For instance, studies have shown that diarrhea and fever are among the major diseases that contribute to the burden of childhood morbidity and mortality in SSA [3–5]. Across LMICs, 10 % of deaths in under-five children is attributable to diarrhoea [6]. A recent study in 31 countries in SSA also found that about 22 % of children in SSA suffered from fever, 23 % suffered from cough and 16 % suffered from diarrhea between 2010 and 2018 [3].
In SSA, numerous studies have established significant associations between several demographic and socio-economic characteristics of women as well as child characteristics and morbidity among children under five. For instance, a number of studies have found associations between maternal age, education, wealth index, employment status, marital status, birth order, child’s age, child’s size at birth and child’s sex as predictors of morbidity among children under five [3, 5, 7]. Specifically, these studies found higher odds of under-five morbidity among older women, women with low level of education, those with poor wealth index, unemployed women, women with higher birth order, younger children, female children and children with small size at birth [3, 5, 7]. One key factor that these studies failed to examine is the role maternal age at first childbirth plays in morbidity among children under five.
Studies that have examined the association between maternal age at first childbirth and morbidity among children have found that children born to mothers whose first childbirth occurred when they were adolescents are the most vulnerable to poor child health outcomes [8, 9]. The possible reasons that have been linked to this association are the low socio-economic status and weak immune systems of adolescent mothers [10, 11]. Moreover, women who give birth as adolescents are less likely to use antenatal, delivery and postnatal care services compared to those who give birth as adults [12, 13]. Furthermore, the fact that such births are more likely to be their first birth, may account for increased risks of under-five morbidity [14].
Studies in SSA have established that the negative consequences of adolescent childbearing on child health may not only be short and medium-term but long term as well [15, 16]. For instance, adolescents who have had a child are more likely to be disadvantaged socio-economically even after several years due to dropping out of school, unemployment and abandonment by parents [16, 17]. Others may also go through long-term psychological problems such as anxiety and depression due to stigmatisation [18–20]. All these may have negative consequences on the health status of their subsequent children who may be born when they are adults.
Despite the established association between maternal age at first childbirth and under-five morbidity, there are few studies on the association between these phenomena in SSA and these were only single country studies [21–23]. In this study, the association between maternal age at first childbirth and under-five morbidity in 32 countries in SSA was examined. Findings from the study can raise awareness and show the need to have adequate policies and programmes to deal with adolescent childbearing and child morbidity in SSA.
Methods
Study design
This study was based on a cross-sectional survey from the Demographic and Health Surveys (DHS) of 32 countries in SSA. In this study, the children’s files, which contain data on children under-five of women aged 15–49 were used. The DHS data is often gathered every 5 years, with longer periods in some countries due to contextual factors.
Sampling and data collection procedure
A two-stage sampling procedure is followed in gathering data for the DHS. The two stages involve the selection of clusters usually called enumeration areas (EAs) at the first stage and the selection of households for the survey at the second stage. Detailed description of the sampling methodology and data collection processes are published elsewhere [24]. The inclusion criteria for considering a DHS in this study is that it has to be published between 2010 and 2019, should have information on age at first childbirth, under-five morbidity and all other important variables considered in this study. Using these criteria, the DHS datasets of 32 countries in SSA with a sample size of 311,603 were considered. The countries included in this study and their samples are shown in Table 1. The manuscript was prepared in line with the Strengthening Reporting of Observational studies in Epidemiology (STROBE) reporting guidelines [25].
Table 1.
Distribution of study sample by country
| Survey Countries | Survey Year | Weighted Sample | Weighted Percentage |
|---|---|---|---|
| Angola | 2016 | 12,539 | 4.02 |
| Benin | 2018 | 12,507 | 4.01 |
| Burkina Faso | 2010 | 13,994 | 4.49 |
| Burundi | 2017 | 12,405 | 3.98 |
| Cameroon | 2018 | 9441 | 3.03 |
| Chad | 2015 | 16,499 | 5.30 |
| Comoros | 2012 | 2968 | 0.95 |
| Congo | 2011-12 | 7680 | 2.46 |
| Congo DR | 2013-14 | 16,780 | 5.38 |
| Cote D’lvoire | 2011-12 | 6588 | 2.11 |
| Ethiopia | 2016 | 10,340 | 3.32 |
| Gabon | 2012 | 4536 | 1.46 |
| Gambia | 2013 | 7436 | 2.39 |
| Ghana | 2014 | 5421 | 1.74 |
| Guinea | 2018 | 7232 | 2.32 |
| Kenya | 2014 | 8855 | 2.84 |
| Lesotho | 2014 | 2812 | 0.91 |
| Liberia | 2013 | 5869 | 1.88 |
| Malawi | 2016 | 16,284 | 5.23 |
| Mali | 2018 | 9549 | 3.06 |
| Namibia | 2013 | 4140 | 1.33 |
| Niger | 2012 | 12,057 | 3.87 |
| Nigeria | 2018 | 30,677 | 9.84 |
| Rwanda | 2015 | 7589 | 2.44 |
| Senegal | 2010-11 | 10,724 | 3.44 |
| Sierra Leone | 2019 | 8809 | 2.83 |
| South Africa | 2016 | 3248 | 1.04 |
| Tanzania | 2016 | 9217 | 2.96 |
| Togo | 2013-14 | 6261 | 2.01 |
| Uganda | 2016 | 14,111 | 4.53 |
| Zambia | 2018 | 9199 | 2.95 |
| Zimbabwe | 2015 | 5836 | 1.87 |
Study variables
Outcome variable
The outcome variable for this study was under-five morbidity. This variable was derived from the experience of fever, cough and diarrhoea among children under-five. For each of these morbid conditions, women were asked if their children had suffered from them at any time in the 2 weeks preceding the survey. The responses for each of the questions were “Yes” and “No”. Children who suffered from at least one of these morbid conditions were considered as those who had under-five morbidity and those who did not suffer from any of these conditions were considered as those who had never experienced under-five morbidity.
Explanatory variables
Age at first childbirth categorised into < 20 years (adolescent childbirth) and ≥ 20 years (adult childbirth) was the key explanatory variable in this study. This variable was derived from the question, “how old were you when you first gave birth to [name]?” The responses to this question were in single years. Based on the findings of previous studies on under-five morbidity [3, 21, 26, 27], mother’s age, marital status, pregnancy intention, place of residence, mother’s education level, wealth quintile, sex of child, child’s weight, number of antenatal care [ANC] visits, place of delivery, and assistant during delivery were considered as covariates.
Statistical analysis
In testing the hypothesis that children under-five born to women whose first childbirth occurred before 20 years are more likely to suffer from either fever, cough or diarrhea, several statistical analyses were carried out using Stata version 14.0. First, bar charts were used to show the prevalence of adolescent childbirth, under-five morbidity and the distribution of under-five morbidity across age at first childbirth of women. Next, using chi-square test, the association between age at first childbirth and fever, cough and diarrhea for each of the 32 countries in SSA were presented using a table. Thirdly, to account for the hierarchical structure and the clustering effect of the datasets, multilevel binary logistic regression models were used to show the association between age at first childbirth and under-five morbidity while controlling for the covariates. Model 0 showed the variance in under-five morbidity attributed to the clustering of the primary sampling units (PSUs) without any explanatory variable. Model I contained the age at first childbirth and under-five morbidity. Model II had age at first childbirth and under-five morbidity while controlling for all the covariates. The Stata command “melogit” was used in fitting these models. The log-likelihood and Akaike’s Information Criterion (AIC) tests were used to check for model fitness. Finally, both bivariate and multivariable binary logistic regression models were used to test the hypothesis that adolescent childbirth is associated with under-five morbidity in each of the countries. The results were presented as crude odds ratios (cORs) and adjusted odds ratios (aORs), at 95 % confidence intervals (CIs). Sample weights were applied using the variable v005 and the survey command in Stata was used to adjust for the complex sampling structure of the data in the regression analyses.
Results
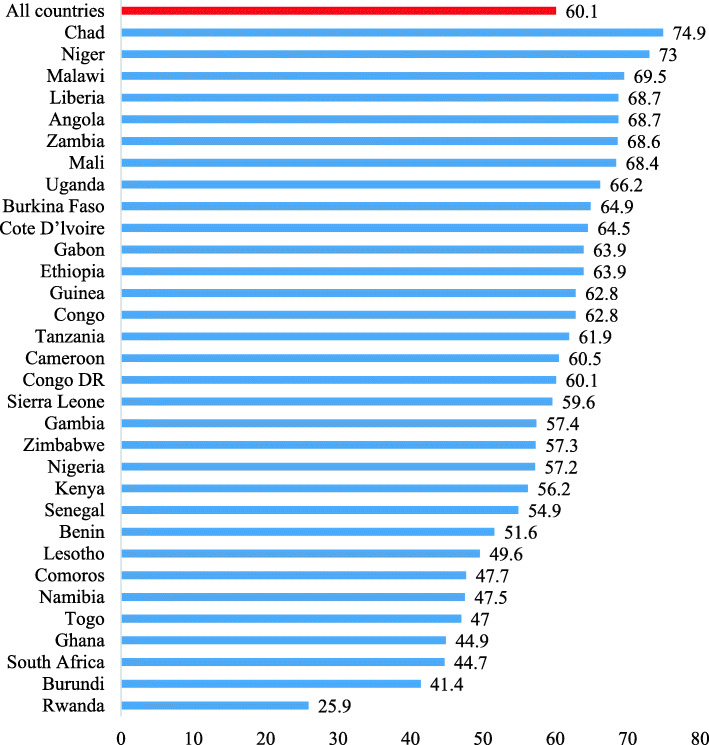
Proportion of mothers whose first childbirth occurred when they were adolescents in sub-Saharan Africa
In the 32 countries in SSA, the proportion of mothers whose first childbirth occurred when they were adolescents was 60.1%. The highest prevalence was found in Chad (74.9%) and the lowest prevalence was in Rwanda (25.9%) (Fig. 1).
Fig. 1.
Bar chart showing the proportion of mothers whose first childbirth occurred when they were adolescents in sub-Saharan Africa
Prevalence of under-five morbidity in sub-Saharan Africa
The prevalence of morbidity among children under five in the 32 countries in SSA was 30.9%. Children under-five born to women in Burundi had the highest prevalence of 49.1% while the lowest prevalence of under-five morbidity was found in Sierra Leone (21.0%) (Fig. 2).
Fig. 2.
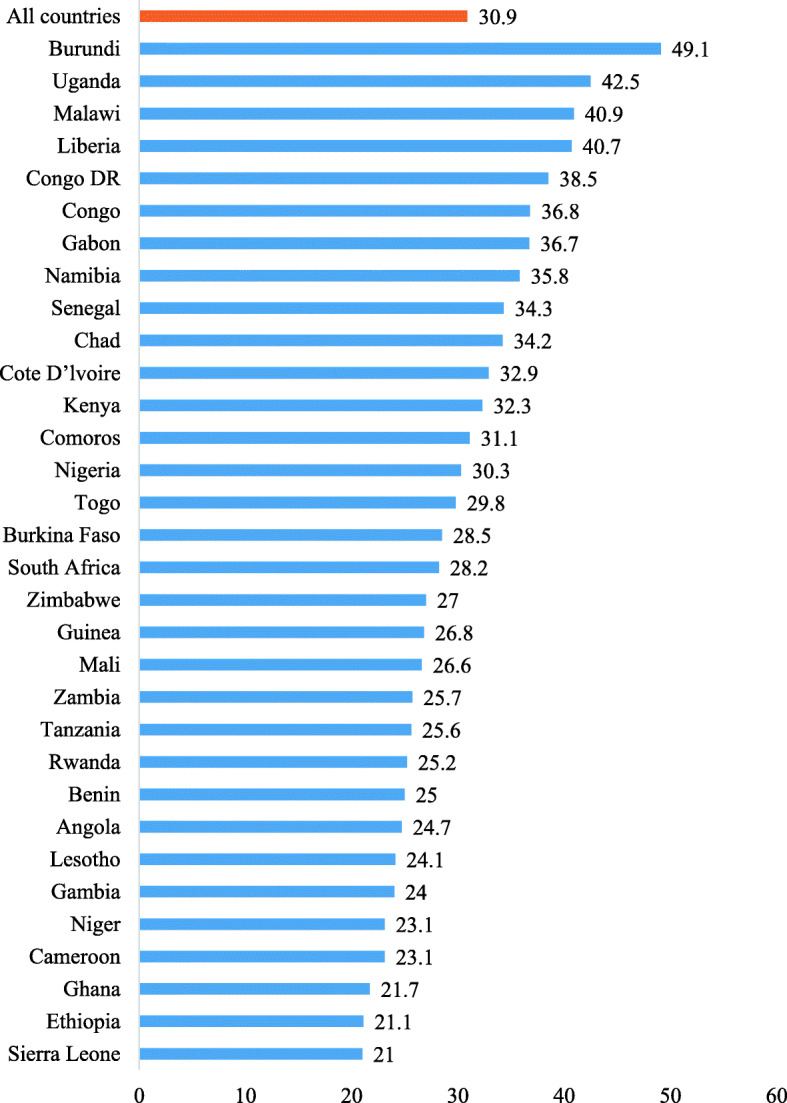
Bar chart showing prevalence of under-five morbidity in sub-Saharan Africa by country
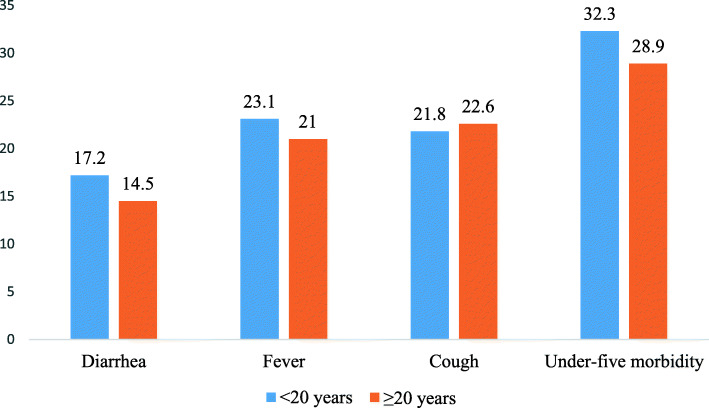
Distribution of the experience of diarrhea, fever, cough, and under-five morbidity accross age at first childbirth
Compared to children born to women whose first childbirth occurred when they were adults (14.5%), those born to women whose first childbirth occurred when they were adolescents had the highest prevalence of diarrhea (17.2%). The experience of fever was also higher among children whose mothers’ first childbirth occurred when they were adolescents (23.1%), compared to adults (21%). This was also true of children’s experience of under-five morbidity (32.3% versus 28.9%). On the contrary, the prevalence of cough among children under-five was higher among children whose mothers’ first childbirth occurred when they were adults (22.6%) than adolescents (21.8%) (Fig. 3).
Fig. 3.
Bar chart showing the distribution of under-five morbidity accross age at first childbirth
Age at first childbirth and under-five morbidity by country
Table 2 shows the distribution of under-five morbidity by country. In general, under-five morbidity was significantly higher among children born to mothers whose first childbirth occurred before 20 years compared to 20 years or more in Angola, Burundi, Cameroon, Congo DR, Gabon, Guinea, Kenya, Malawi, Mali, Namibia, Nigeria, Sierra Leone, Togo, Uganda, and Zimbabwe at p < 0.05.
Table 2.
Distribution of under-five morbidity across age at first childbirth by country
| Countries | Diarrhea | Fever | Cough | Under-five morbidity | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 20 years | ≥ 20 years | p-values | < 20 years | ≥ 20 years | p-values | < 20 years | ≥ 20 years | p-values | < 20 years | ≥ 20 years | p-values | |
| Angola | 16.7 | 13.5 | 0.002 | 16.1 | 11.9 | < 0.001 | 12.8 | 11.6 | 0.210 | 26.4 | 21.0 | < 0.001 |
| Benin | 11.2 | 9.8 | 0.015 | 20.0 | 18.8 | 0.186 | 16.2 | 16.5 | 0.709 | 25.9 | 24.1 | 0.056 |
| Burkina Faso | 14.9 | 14.9 | 0.920 | 20.1 | 21.9 | 0.029 | 9.8 | 11.2 | 0.021 | 28.1 | 29.4 | 0.147 |
| Burundi | 24.5 | 21.0 | < 0.001 | 42.2 | 37.5 | < 0.001 | 38.1 | 38.2 | 0.941 | 52.3 | 46.8 | < 0.001 |
| Cameroon | 13.0 | 10.7 | 0.012 | 16.9 | 13.6 | 0.002 | 17.8 | 19.1 | 0.239 | 24.8 | 20.4 | < 0.001 |
| Chad | 22.7 | 21.6 | 0.352 | 24.4 | 23.7 | 0.553 | 20.4 | 19.7 | 0.529 | 34.3 | 33.7 | 0.653 |
| Comoros | 18.1 | 16.4 | 0.323 | 22.0 | 22.1 | 0.954 | 19.1 | 18.3 | 0.665 | 31.4 | 30.9 | 0.803 |
| Congo | 20.0 | 18.2 | 0.122 | 26.0 | 24.1 | 0.130 | 28.0 | 27.8 | 0.683 | 37.8 | 35.1 | 0.104 |
| Congo DR | 18.2 | 15.3 | 0.001 | 31.1 | 28.2 | 0.003 | 32.6 | 29.9 | 0.018 | 40.4 | 35.8 | < 0.001 |
| Cote D’lvoire | 18.7 | 18.4 | 0.822 | 23.4 | 25.8 | 0.141 | 21.1 | 24.2 | 0.049 | 32.3 | 33.9 | 0.363 |
| Ethiopia | 11.9 | 11.6 | 0.773 | 14.3 | 14.7 | 0.747 | 20.3 | 19.3 | 0.419 | 21.0 | 21.1 | 0.965 |
| Gabon | 18.3 | 14.1 | 0.003 | 26.0 | 23.6 | 0.273 | 42.1 | 38.9 | 0.080 | 36.6 | 31.3 | 0.006 |
| Gambia | 18.3 | 17.0 | 0.347 | 12.4 | 11.5 | 0.862 | 13.3 | 14.4 | 0.028 | 24.8 | 23.0 | 0.295 |
| Ghana | 12.2 | 11.7 | 0.654 | 14.3 | 13.7 | 0.589 | 14.5 | 13.7 | 0.517 | 22.3 | 21.2 | 0.479 |
| Guinea | 15.4 | 13.2 | 0.046 | 17.9 | 16.1 | 0.089 | 11.6 | 11.0 | 0.511 | 28.3 | 24.2 | 0.003 |
| Kenya | 16.6 | 13.4 | 0.003 | 25.9 | 21.5 | < 0.001 | 37.8 | 35.9 | 0.167 | 35.2 | 28.6 | < 0.001 |
| Lesotho | 13.0 | 11.4 | 0.361 | 16.0 | 15.0 | 0.548 | 30.8 | 28.7 | 0.325 | 25.1 | 23.2 | 0.378 |
| Liberia | 23.9 | 20.4 | 0.040 | 30.0 | 28.4 | 0.417 | 27.6 | 22.0 | 0.002 | 41.8 | 38.3 | 0.099 |
| Malawi | 22.5 | 20.7 | 0.062 | 30.1 | 27.2 | 0.001 | 25.2 | 24.3 | 0.426 | 42.0 | 38.3 | < 0.001 |
| Mali | 18.0 | 15.5 | 0.020 | 16.2 | 15.7 | 0.567 | 10.3 | 10.0 | 0.740 | 27.3 | 24.9 | 0.042 |
| Namibia | 22.1 | 16.9 | < 0.001 | 28.7 | 24.4 | 0.016 | 36.4 | 29.8 | < 0.001 | 39.1 | 32.9 | 0.001 |
| Niger | 14.5 | 13.9 | 0.524 | 14.3 | 15.1 | 0.472 | 14.1 | 15.2 | 0.313 | 22.9 | 23.5 | 0.613 |
| Nigeria | 15.8 | 9.0 | < 0.001 | 28.2 | 19.3 | < 0.001 | 14.5 | 15.2 | < 0.001 | 35.0 | 24.0 | < 0.001 |
| Rwanda | 13.1 | 12.0 | 0.239 | 19.9 | 18.6 | 0.284 | 26.0 | 26.8 | 0.539 | 26.1 | 24.9 | 0.350 |
| Senegal | 21.3 | 21.0 | 0.485 | 21.6 | 25.1 | 0.010 | 19.4 | 23.4 | 0.001 | 33.0 | 36.0 | 0.106 |
| Sierra Leone | 7.97 | 6.16 | 0.020 | 7.8 | 15.5 | 0.018 | 14.1 | 13.8 | 0.702 | 22.5 | 18.8 | < 0.001 |
| South Africa | 11.9 | 10.0 | 0.162 | 21.9 | 20.2 | 0.358 | 27.0 | 25.5 | 0.472 | 29.7 | 27.0 | 0.196 |
| Tanzania | 12.4 | 11.7 | 0.437 | 19.1 | 17.2 | 0.076 | 15.9 | 17.2 | 0.197 | 26.2 | 24.8 | 0.239 |
| Togo | 16.7 | 14.0 | 0.014 | 23.9 | 20.1 | 0.002 | 27.5 | 28.2 | 0.630 | 31.8 | 22.0 | 0.007 |
| Uganda | 20.7 | 18.7 | 0.016 | 36.6 | 28.7 | < 0.001 | 41.2 | 41.9 | 0.599 | 44.8 | 38.1 | < 0.001 |
| Zambia | 16.1 | 14.0 | 0.057 | 16.5 | 15.1 | 0.172 | 22.1 | 20.4 | 0.278 | 26.5 | 24.1 | 0.091 |
| Zimbabwe | 18.6 | 14.8 | 0.002 | 14.2 | 13.8 | 0.763 | 40.0 | 38.2 | 0.231 | 28.7 | 24.8 | 0.018 |
Association between adolescent childbirth and under-five morbidity
As shown in Table 3, there was a significant independent association between age at first childbirth and under-five morbidity, with children born to mothers whose first childbirth occurred at < 20 years, 16 % times more likely to suffer from under-five morbidity, compared to those whose mothers’ first childbirth occurred at age ≥ 20 years [cOR = 1.16; CI = 1.13–1.19], and this persisted but with reduced odds after controlling for the covariates [aOR = 1.10; CI = 1.07–1.12] (Model I and Model II of Table 3). At the country level, children born to mothers whose first childbirth occurred at < 20 years, were more likely to suffer from under-five morbidity, compared to those whose mothers’ first childbirth occurred at age ≥ 20 years in Angola, Burundi, Congo DR, Guinea, Kenya, and Uganda (Model II of Table 4).
Table 3.
Multilevel logistic regression on the association between adolescent childbirth and under-five morbidity in sub-Saharan Africa
| Variables | Model 0 | Model I cOR (95 % CI) | Model II aOR (95 % CI) |
|---|---|---|---|
| Fixed effects | |||
| Age at first childbirth | |||
| < 20 years | 1.16***[1.13–1.19] | 1.10** (1.07–1.12) | |
| ≥ 20 years | Reference | Reference | |
| Random effects | |||
| Primary sampling unit variance (95 % CI) | 0.11 (0.09–0.15) | 0.11 (0.08–0.14) | 0.06 (0.05–0.08) |
| Intraclass correlation coefficient | 0.03 | 0.03 | 0.02 |
| Wald chi-square | Reference | 170.27*** | 1430.54*** |
| Model fitness | |||
| Log-likelihood | -189072.57 | -188907.15 | -137588.17 |
| Akaike’s Information Criterion | 378149.1 | 377820.3 | 275226.3 |
| Sample size | 311,603 | 311,603 | 311,603 |
| Number of clusters | 1610 | 1610 | 1610 |
NB: Model II adjusted for mother’s age, marital status, pregnancy intention, place of residence, mother’s education level, wealth quintile, sex of child, child’s weight, number of ANC visits, place of delivery, and assistant during delivery; cOR=crude odds ratio; aOR=adjusted odds ratio
*p < 0.05; **p < 0.01; ***p < 0.001
Table 4.
Binary logistic regression on the association between adolescent childbirth and under-five morbidity disaggregated by country
| Countries | Model I cOR (95 % CI) | Model II aOR (95 % CI) |
|---|---|---|
| Angola | 1.43***(1.31–1.57) | 1.23*** (1.10–1.39) |
| Benin | 1.09* (1.01–1.18) | 1.01 (0.92–1.13) |
| Burkina Faso | 0.95 (0.88–1.03) | 0.97 (0.89–1.07) |
| Burundi | 1.25***(1.16–1.35) | 1.13* (1.02–1.25) |
| Cameroon | 1.27*** (1.15–1.41) | 1.28 (1.12–1.46) |
| Chad | 1.05 (0.97–1.13) | 1.03 (0.93–1.14) |
| Comoros | 1.05 (0.90–1.23) | 0.89 (0.72–1.11) |
| Congo | 1.08 (0.94–1.19) | 1.02 (0.91–1.15) |
| Congo DR | 1.22*** (1.14–1.30) | 1.19***(1.09–1.29) |
| Cote D’lvoire | 1.03 (0.93–1.15) | 0.98 (0.68–1.46) |
| Ethiopia | 1.07 (0.97–1.19) | 1.05 (0.93–1.19) |
| Gabon | 1.20**(1.05–1.36) | 1.07 (0.91–1.25) |
| Gambia | 1.06 (0.95–1.18) | 1.10 (0.96–1.26) |
| Ghana | 1.05 (0.92–1.19) | 0.99 (0.85–1.16) |
| Guinea | 1.19**(1.06–1.33) | 1.17* (1.03–1.35) |
| Kenya | 1.26*** (1.15–1.38) | 1.13* (1.01–1.26) |
| Lesotho | 1.05 (0.88–1.25) | 0.97 (0.78–1.20) |
| Liberia | 1.07 (0.96–1.19) | 1.07 (0.94–1.22) |
| Malawi | 1.17***(1.09–1.26) | 1.01 (0.93–1.10) |
| Mali | 1.10 (1.00-1.22) | 1.04 (0.92–1.18) |
| Namibia | 1.25***(1.11–1.42) | 1.05 (0.90–1.23) |
| Niger | 0.97 (0.88–1.06) | 0.95 (0.84–1.08) |
| Nigeria | 1.62***(1.54–1.71) | 0.97 (0.84–1.13) |
| Rwanda | 1.07 (0.95–1.21) | 1.01 (0.58–1.74) |
| Senegal | 0.94 (0.86–1.01) | 1.14 (0.77–1.69) |
| Sierra Leone | 1.32***(1.19–1.47) | 1.33 (1.17–1.51) |
| South Africa | 1.13 (0.97–1.33) | 1.09 (0.91–1.31) |
| Tanzania | 1.06 (0.97–1.17) | 1.02 (0.90–1.15) |
| Togo | 1.22***(1.10–1.36) | 1.03 (0.90–1.17) |
| Uganda | 1.31***(1.22–1.41) | 1.14** (1.04–1.25) |
| Zambia | 1.12*(1.01–1.24) | 1.02 (0.90–1.15) |
| Zimbabwe | 1.21**(1.07–1.37) | 1.10 (0.95–1.27) |
NB: Model II adjusted for mother’s age, marital status, pregnancy intention, place of residence, mother’s education level, wealth quintile, sex of child, child’s weight, number of ANC visits, place of delivery, and assistant during delivery; cOR=crude odds ratio; aOR=adjusted odds ratio
*p < 0.05
**p < 0.01
***p < 0.001
Discussion
In this study, the hypothesis that children born to mothers whose first childbirth birth occurred before 20 years were more likely to experience under-five morbidity (diarrhea, fever and cough), compared to those whose mothers’ first childbirth occurred at 20 years and above was tested. Findings from the study showed that the risk of under-five morbidity is high among children born to mothers whose first childbirth occurred before 20 years, compared to those whose mothers’ first childbirth occurred at 20 years and above. This finding is consistent with the findings of previous studies in Ethiopia [21, 22] and 55 low-and middle-income countries [8]. Several reasons may account for this finding including poor living conditions among adolescent mothers, no formal education, and low utilization of maternal and child health services [10–13]. These factors explain the overall low socio-economic status and healthcare seeking behaviours of adolescent mothers and determine the likelihood of under-five morbidity [28–32].
Considering that some of the women whose first childbirth occurred when they were adolescents were not adolescents at the time of the survey, the results of the current study on the association between adolescent childbearing and under-five morbidity suggest that the negative effects of adolescent childbearing on under-five morbidity may extend over several years. Hence, the problem is even more profound than we imagine and is not only short or medium-term but long term as well. For instance, adolescents who have had a child are more likely to have low socio-economic status even after several years due to dropping out of school, unemployment and abandonment by parents [16, 17] while others may also go through long-term psychological problems such as anxiety and depression due to stigmatisation [18–20], which may result in under-five morbidity among their subsequent children.
In this study, Angola, Burundi, Congo DR, Guinea, Kenya, and Uganda were the countries where under-five morbidity was higher among children born to mothers whose first childbirth occurred before 20 years compared to those whose mothers’ first childbirth occurred at 20 years and above. This finding is expected because all of these countries have gone through some years of political or civil crises which consequently affected the living conditions in the countries. For instance, the finding that under-five morbidity is higher in children born to mothers whose first childbirth occurred before 20 years, compared to those whose mothers’ first childbirth occurred at 20 years and above in Burundi has been found to be attributed to poor living conditions in the country such as overcrowding and poor housing conditions, inadequate sanitation and unsafe water, where less than 50 % of the population have access to potable water [33]. Other studies have attributed the high childhood morbidity among adolescent mothers in the country to political instability and violent conflict, weakened delivery systems, lower coverage of interventions, disempowering policies and gaps in the continuum of care [23, 34, 35]. Children born to adolescent mothers in Angola, Congo DR, Guinea, Kenya, and Uganda are more likely to experience under-five morbidity due to similar conditions that exist in Burundi since these conditions are more prevalent in countries that have gone through political or civil crisis. These findings imply that in order to reduce under-five morbidity, there is the need to improve the living conditions of mothers as well as children through the implementation of effective sanitation conditions and enhanced access to healthcare for adolescent mothers. In countries where significant associations were not found between adolescent childbearing and under-five morbidity, other maternal characteristics such as mother’s age, marital status, pregnancy intention, place of residence, mother’s education level, and wealth quintile; child characteristics such as sex of child, and child’s weight; and access and use of maternal healthcare services such as number of ANC visits, place of delivery, and assistant during delivery may be responsible for the under-five morbidity [3, 21, 26, 27]. Another possible reason for the lack of association between adolescent childbearing and under-five morbidity could be the existence of protecting factors such as better access to health care in general, a better system of educational and professional rehabilitation for adolescent mothers in those countries [36, 37].
Strengths and limitations
The major strength of this study is the use of nationally-representative datasets of 32 countries in SSA and the large sample size that made it possible to use high level statistical analyses. Despite this strength, there are some limitations that need to be mentioned. First, the design employed in the DHS is cross-sectional and hence, causal interpretations of the findings cannot be established. Second, age at first childbirth was self-reported, and as a result, there is the possibility of under-and over-reporting of data [38–40].
Conclusions
In this study, an association between adolescent childbirth and morbidity in children under five in SSA has been established. However, this association was statistically significant in Angola, Burundi, Congo DR, Guinea, Kenya, and Uganda. The study concludes that under-five morbidity is higher among children born to mothers whose first childbirth birth occurred before 20 years compared to those whose mothers’ first childbirth occurred at 20 years and above. The findings indicate that in order to reduce under-five morbidity there is the need to deal with adolescent childbearing through cultural and social change, coupled with engagement of adolescents and stakeholders in adolescent sexual and reproductive health programmes. There is the need for future research to examine the healthcare seeking behaviour for childhood illness among women whose first birth occurred when they were adolescents.
Acknowledgements
The author thanks the MEASURE DHS for granting free access to the original data.
Abbreviations
- aOR
Adjusted odds ratio
- cOR
Crude odds ratio
- DHS
Demographic and Health Survey
- LMICs
Low-and middle-income countries
- SSA
Sub-Saharan Africa
- WHO
World Health Organisation
Author’s contributions
BOA conceived the study, reviewed literature, carried out the analysis, wrote the entire manuscript and submitted it to the journal. BOA was responsible for revising and amending the drafts of the paper until it was published. The author read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data for this study is available at: http://dhsprogram.com/data/available-datasets.cfm.
Declarations
Ethics approval and consent to participate
Ethics approval was not a requirement in this study since secondary data which is available in the public domain was used. More details regarding DHS data and ethical standards are available can be found at: http://goo.gl/ny8T6X.
Consent for publication
Not Applicable.
Competing interests
The author declares no competing interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.WHO: World health statistics 2016: monitoring health for the SDGs sustainable development goals. Geneva: WHO; 2016. Retrieved from https://apps.who.int/iris/handle/10665/206498 on 11 Feb 2021.
- 2.WHO: Children: improving survival and well-being. Geneva: WHO; 2020. Retrieved from https://www.who.int/news-room/fact-sheets/detail/children-reducing-mortality on 11 Feb 2021.
- 3.Adedokun ST, Yaya S. Childhood morbidity and its determinants: evidence from 31 countries in sub-Saharan Africa. BMJ Global Health. 2020;5(10):e003109. doi: 10.1136/bmjgh-2020-003109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Khatab K, Fahrmeir L. Analysis of childhood morbidity with geoadditive probit and latent variable model: a case study for Egypt. Am J Trop Med Hyg. 2009;81(1):116–28. [PubMed] [Google Scholar]
- 5.Takele K, Zewotir T, Ndanguza D. Risk factors of morbidity among children under age five in Ethiopia. BMC Public Health. 2019;19(1):1–9. doi: 10.1186/s12889-019-7273-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Reiner RC, Jr, Wiens KE, Deshpande A, Baumann MM, Lindstedt PA, Blacker BF, Troeger CE, Earl L, Munro SB, Abate D. Mapping geographical inequalities in childhood diarrhoeal morbidity and mortality in low-income and middle-income countries, 2000–17: analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395(10239):1779–1801. doi: 10.1016/S0140-6736(20)30114-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Adedokun ST. Correlates of childhood morbidity in Nigeria: Evidence from ordinal analysis of cross-sectional data. Plos one. 2020;15(5):e0233259. doi: 10.1371/journal.pone.0233259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Finlay JE, Özaltin E, Canning D. The association of maternal age with infant mortality, child anthropometric failure, diarrhoea and anaemia for first births: evidence from 55 low-and middle-income countries. BMJ Open. 2011:1(2);1–24. [DOI] [PMC free article] [PubMed]
- 9.Gibbs CM, Wendt A, Peters S, Hogue CJ. The impact of early age at first childbirth on maternal and infant health. Paediatr Perinat Epidemiol. 2012;26:259–84. doi: 10.1111/j.1365-3016.2012.01290.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rani M, Lule E. Exploring the socioeconomic dimension of adolescent reproductive health: a multicountry analysis. Int Fam Plan Perspect. 2004:30(4);110–7. [DOI] [PubMed]
- 11.Chirwa GC, Mazalale J, Likupe G, Nkhoma D, Chiwaula L, Chintsanya J. An evolution of socioeconomic related inequality in teenage pregnancy and childbearing in Malawi. PloS one. 2019;14(11):e0225374. doi: 10.1371/journal.pone.0225374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reynolds HW, Wong EL, Tucker H. Adolescents’ use of maternal and child health services in developing countries. Int Fam Plan Perspect. 2006:32(1);6–16. [DOI] [PubMed]
- 13.Atuyambe L, Mirembe F, Tumwesigye NM, Annika J, Kirumira EK, Faxelid E. Adolescent and adult first time mothers’ health seeking practices during pregnancy and early motherhood in Wakiso district, central Uganda. Reprod Health. 2008;5(1):13. doi: 10.1186/1742-4755-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mahy M: Childhood mortality in the developing world: a review of evidence from the Demographic and Health Surveys, vol. 4: MEASURE DHS+, ORC Macro; 2003. Retrived from https://www.dhsprogram.com/publications/publication-cr4-comparative-reports.cfm on 11 Feb 2021.
- 15.Psaki SR, Soler-Hampejsek E, Saha J, Mensch BS, Amin S. The effects of adolescent childbearing on literacy and numeracy in Bangladesh, Malawi, and Zambia. Demography. 2019;56(5):1899–929. doi: 10.1007/s13524-019-00816-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Assini-Meytin LC, Green KM. Long-term consequences of adolescent parenthood among African-American urban youth: A propensity score matching approach. J Adolesc Health. 2015;56(5):529–35. doi: 10.1016/j.jadohealth.2015.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grant MJ, Hallman KK. Pregnancy-related school dropout and prior school performance in KwaZulu‐Natal, South Africa. Stud Fam Plann. 2008;39(4):369–82. doi: 10.1111/j.1728-4465.2008.00181.x. [DOI] [PubMed] [Google Scholar]
- 18.Osok J, Kigamwa P, Vander Stoep A, Huang K-Y, Kumar M. Depression and its psychosocial risk factors in pregnant Kenyan adolescents: a cross-sectional study in a community health Centre of Nairobi. BMC Psychiatry. 2018;18(1):1–10. doi: 10.1186/s12888-018-1706-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Govender D, Naidoo S, Taylor M. Antenatal and postpartum depression: prevalence and associated risk factors among adolescents’ in KwaZulu-Natal, South Africa. Depress Res Treat. 2020:1–13. [DOI] [PMC free article] [PubMed]
- 20.Ayamolowo SJ, Olajubu AO, Akintola FE. Perceived social support and depression among pregnant and child-rearing teenagers in Ile-Ife, Southwest Nigeria. Afr J Midwifery Women’s Health. 2019;13(4):1–9. [Google Scholar]
- 21.Gashaw TA, Walie YM. Prevalence and determinate factors of diarrhea morbidity among under five children in shake zone, Southwest Ethiopia, a community based cross-sectional study. Arch Commun Med Public Health. 2019;5(1):008–14. [Google Scholar]
- 22.Workicho A, Belachew T, Argaw A, Ghosh S, Kershaw M, Lachat C, Kolsteren P. Adolescent pregnancy and linear growth of infants: a birth cohort study in rural Ethiopia. Nutr J. 2019;18(1):22. doi: 10.1186/s12937-019-0448-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Moise IK. Causes of morbidity and mortality among neonates and children in post-conflict Burundi: a cross-sectional retrospective study. Children. 2018;5(9):125. doi: 10.3390/children5090125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Corsi DJ, Neuman M, Finlay JE, Subramanian S. Demographic and health surveys: a profile. Int J Epidemiol. 2012;41(6):1602–13. doi: 10.1093/ije/dys184. [DOI] [PubMed] [Google Scholar]
- 25.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, Strobe I. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9. doi: 10.1016/j.ijsu.2014.07.013. [DOI] [PubMed] [Google Scholar]
- 26.Nworie KM, Oyine Aluh D, Aluh DO. Determinants of diarrhea and optimal childcare among Under-Five children in Nigeria: insights from the 2013 demographic and health survey. Fam Med Med Sci Res. 2018;7(10.4172):2327–4972. [Google Scholar]
- 27.Alebel A, Tesema C, Temesgen B, Gebrie A, Petrucka P, Kibret GD. Prevalence and determinants of diarrhea among under-five children in Ethiopia: a systematic review and meta-analysis. PloS one. 2018;13(6):e0199684. doi: 10.1371/journal.pone.0199684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Van Malderen C, Amouzou A, Barros AJD, Masquelier B, Van Oyen H, Speybroeck N. Socioeconomic factors contributing to under-five mortality in sub-Saharan Africa: a decomposition analysis. BMC Public Health. 2019;19(1):760. doi: 10.1186/s12889-019-7111-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yaya S, Ahinkorah BO, Ameyaw EK, Seidu A-A, Darteh EKM, Adjei NK. Proximate and socio-economic determinants of under-five mortality in Benin, 2017/2018. BMJ Global Health. 2020;5(8):e002761. doi: 10.1136/bmjgh-2020-002761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ahinkorah BO, Seidu A-A, Budu E, Armah-Ansah EK, Agbaglo E, Adu C, Hagan JE, Yaya S. Proximate, intermediate, and distal predictors of under-five mortality in Chad: analysis of the 2014–15 Chad demographic and health survey data. BMC Public Health. 2020;20(1):1–12. doi: 10.1186/s12889-020-09869-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nattey C, Masanja H, Klipstein-Grobusch K. Relationship between household socio-economic status and under-five mortality in Rufiji DSS, Tanzania. Global Health Act. 2013;6(1):19278. doi: 10.3402/gha.v6i0.19278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chowdhury AH, Hanifi SMA, Mia MN, Bhuiya A. Socioeconomic inequalities in under-five mortality in rural Bangladesh: evidence from seven national surveys spreading over 20 years. Int J Equity Health. 2017;16(1):197. doi: 10.1186/s12939-017-0693-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.WHO: Health Action in Crises: Burundi. In. New York: WHO; 2005. Retrieved from https://www.who.int/hac/crises/bdi/background/Burundi_Dec05.pdf on 11 Feb 2021.
- 34.Moise IK, Verity JF, Kangmennaang J. Identifying youth-friendly service practices associated with adolescents’ use of reproductive healthcare services in post-conflict Burundi: a cross-sectional study. Int J Health Geogr. 2017;16(1):1–15. doi: 10.1186/s12942-016-0075-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chi PC, Urdal H, Umeora OU, Sundby J, Spiegel P, Devane D. Improving maternal, newborn and women’s reproductive health in crisis settings: a cochrane systematic review. Prehospital Disaster Med. 2017;32(S1):198–8. [Google Scholar]
- 36.Mekonnen T, Dune T, Perz J. Maternal health service utilisation of adolescent women in sub-Saharan Africa: a systematic scoping review. BMC Pregnancy Childbirth. 2019;19(1):1–16. doi: 10.1186/s12884-019-2501-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Harding JF, Knab J, Zief S, Kelly K, McCallum D. A systematic review of programs to promote aspects of teen parents’ self-sufficiency: Supporting educational outcomes and healthy birth spacing. Matern Child Health J. 2020:24;1–21. [DOI] [PMC free article] [PubMed]
- 38.Ahinkorah BO. Individual and contextual factors associated with mistimed and unwanted pregnancies among adolescent girls and young women in selected high fertility countries in sub-Saharan Africa: a multilevel mixed effects analysis. Plos one. 2020;15(10):e0241050. doi: 10.1371/journal.pone.0241050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ahinkorah BO. Predictors of unmet need for contraception among adolescent girls and young women in selected high fertility countries in sub-Saharan Africa: a multilevel mixed effects analysis. PloS one. 2020;15(8):e0236352. doi: 10.1371/journal.pone.0236352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ahinkorah BO. Predictors of modern contraceptive use among adolescent girls and young women in sub-Saharan Africa: a mixed effects multilevel analysis of data from 29 demographic and health surveys. Contracept Reprod Med. 2020;5(1):1–12. doi: 10.1186/s40834-020-00138-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data for this study is available at: http://dhsprogram.com/data/available-datasets.cfm.