Abstract
Coronavirus disease 2019 (COVID-19) has become a significant global public health issue resulting from SARS-CoV-2 (Severe Acute Respiratory Syndrome Coronavirus 2). COVID-19 outbreak approaches an unprecedented challenge for human health, the economy, and societies. The transmission of the COVID-19 is influenced by many factors, including climatic, environmental, socioeconomic, and demographic. This study aimed to investigate the influences of climatic and sociodemographic determinants on COVID-19 transmission. The climatic variables considered herein were air temperature, relative humidity, wind speed, air pollution, and cumulative precipitation. Sociodemographic variables included population density, socioeconomic conditions, misinformation, and personal hygiene practices towards the pandemic. Review results indicated that lower temperatures and greater incidence of COVID-19 are reported in a more significant number of studies. Another factor linked to COVID-19 occurrence was the humidity. However, the results were varied; some research reported positive, and others reported negative relationships. In addition, poor air quality, along with strong winds, makes the virus more vulnerable to spreading, leading to a spike in COVID-19 cases. PM2.5, O3, and NO2 also showed a strong correlation with the recent epidemic. The findings on rainfall were inconsistent between studies. Among the non-climatic factors, population density, education, and income were credited as potential determinants for the coronavirus outbreak. Climatic and sociodemographic factors showed a significant correlation on the COVID-19 outbreak. Thus, our review emphasizes the critical importance of considering climatic and non-climatic factors while developing intervention measures. This study's core findings will support the decision-makers in identifying climatic and socioeconomic elements that influence the risks of future pandemics.
Keywords: COVID-19 outbreak, Climatic factors, Non-climatic factors and transmission
1. Introduction
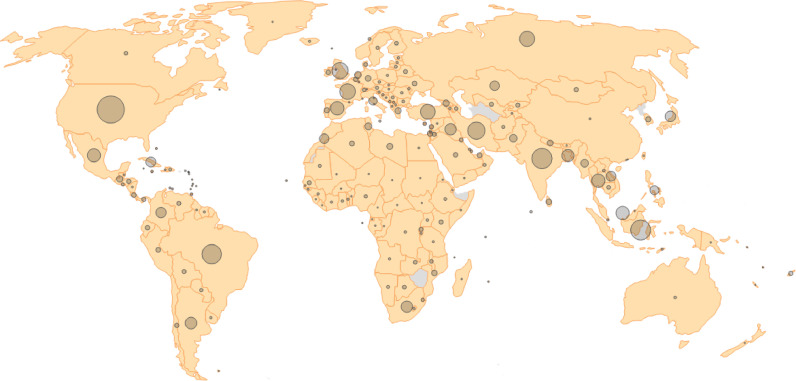
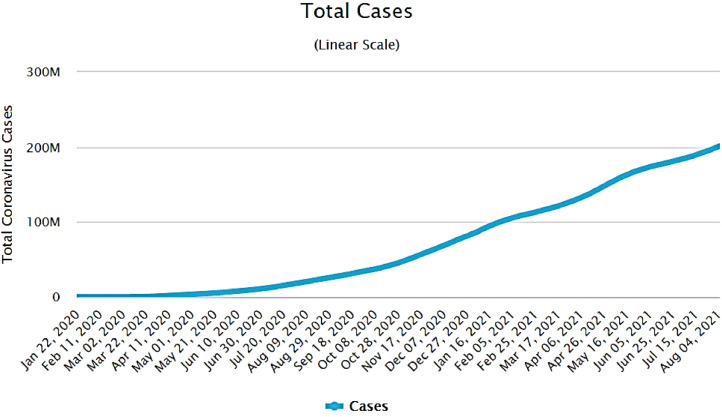
The Coronavirus disease 2019 (COVID-19), caused by the Severe Acute Respiratory Syndrome (SARS), was first reported in Wuhan in December 2019, the capital of Hubei Province of China (Zhou et al., 2020). Shortly after that, COVID-19 expanded rapidly throughout Asia, Europe, North America, South America, and Oceania from China (McClymont and Hu, 2021). Due to the high concurrent characteristics of the COVID-19 and rapidity of the spread, the World Health Organization (WHO) was formally proclaimed a global pandemic on 11 March 2020 (WHO, 2020a). Since the first discovery of COVID-19, it has affected over 214 countries and territories worldwide (Fig. 1 ), with 200,816,440 confirmed cases and 4266,677 deaths as of 29 July 2021 (Fig. 2 ).
Fig. 1.
The spread of the coronavirus globally. Data as of 04 August 2021 (JHU, 2021).
Fig. 2.
Total coronavirus cases from 22 January 2020 to 04 Aug 2021.
COVID-19 is a coronavirus-induced respiratory infection caused by SARS-CoV-2. Two primary methods in which COVID-19 can be transmitted are through the air, either by droplets or by aerosols and surface contact (e.g., fomites or direct contact with a contaminated person) (Doremalen et al., 2020; Setti et al., 2020). It spreads fast via aerosolized droplets and virus-infected hands and surfaces (Sohrabi et al., 2020). Some common signs and symptoms linked explicitly to COVID-19 infection are fever, coughing, myalgia or fatigue, and shortness of breath. However, trouble breathing, pneumonia, acute respiratory syndrome, kidney failure, and even death can happen in severe cases (Holshue et al., 2020.) Individuals aged 65 and older and those with a medical history of cardiovascular disease or diabetes, specifically coronary artery disease, are the most vulnerable to severe COVID-19 manifestations (Clark et al., 2020).
Recently, a field of investigation involving the impact of climate variability on COVID-19 transmission has emerged. In light of past SARS-COV-2 findings, it is projected that the same transmission patterns will be observed for seasonal influenza and possibly other respiratory viruses as well (Sobral et al., 2020). Climate variability can contribute to novel viruses transmission, accelerated illness, and mortality. Thus, to prevent future outbreaks, understanding the worldwide spatial-temporal patterns and trends of COVID-19 transmission is necessary. (Xu et al., 2020; McClymont and Hu, 2021).
COVID-19 initially expanded slowly in South Asian nations such as India, Bangladesh, and Nepal. This slow emergence maybe because of this region's tropical and subtropical climate (Haque and Rahman,2020). Numerous climatic and non-climatic factors contribute significantly to the spread of COVID-19 (Bilal et al., 2021). Environmental and social variables, in addition to climatic variables, cause significant distress worldwide (Bashir et al., 2020). Climate factors include air temperature, relative humidity, precipitation, air pollution, and non-climate factor comprises several factors like population density, socioeconomic condition, personal health hygiene, social behavior, migratory flow, and host immunity reported to influence the transmission of COVID-19 (Oliveiros et al., 2020; Lakshmi and Suresh, 2020).
The global pandemic induced by COVID-19 has compelled the scientific community to expend enormous effort identifying significant factors and their correlations with virus transmission. Extensive research must comprehend the disease in different countries under varied socioeconomic and climatic conditions (Marson and Ortega, 2020; Wilder-Smith et al., 2020). Sociodemographic and climatic factors may be linked to confirmed cases. Early investigations suggested that the COVID-19 virus transmission was linked to population size and temperature ((Jahangiri et al., 2020; Rahman et al., 2021). These investigations clarify that socioeconomic and environmental factors must be considered while analyzing how climatic factors influence the COVID-19 outbreak.
Numerous studies have been conducted to examine the effect of climate on the spread of COVID-19. These studies have concentrated on specific locations and nations like China, Brazil, Indonesia, the United States of America, Russia, Iran, and Europe (Ahmadi et al., 2020; Auler et al., 2020; Lasisi and Eluwole, 2021; Liu et al., 2020; (Tosepu et al., 2020); Xie and Zhu,2020). A minimal study has also been conducted on climatic factors influencing COVID-19 transmission in the South Asian region (Awasthi et al., 2021; Gupta et al., 2020; Mofijur et al., 2020; Sasikumar et al., 2020). In transboundary infection, the effect of shared cultural and behavioral practices on the temporal and spatial spread of COVID-19 in south Asia remains unknown (Islam et al., 2021). However, studies considering climatic and non-climatic factors while understanding this pandemic outbreak in South Asia are limited (exceptions Jha et al., 2021; Mehmood et al., 2021; Tandukar et al., 2021; Islam et al., 2021). Therefore, it is justifiable to explore the effect of climatic and non-climatic determinants on transmitting this novel coronavirus in the South Asian region to provide practical implications for researchers, policymakers, and the general people. Thus, the study aims to find out the influences of climatic and non-climatic factors on COVID-19 transmission. To attain this objective, two questions were answered. First, how do climatic factors influence coronavirus transmission? Second, what is the role of sociodemographic determinants on the COVID-19 outbreak? Table 1
Table 1.
The influencing Climatic factors and their impacts on transmission of COVID-19.
| Influencing factors | Impacts on transmission | References |
|---|---|---|
| Air temperature | Air temperature was substantially linked with COVID-19 transmission at the community level, and oppositely, a few investigations discovered no significant correlation between temperature and transmission with COVID-19. In addition, arid and tropical climate conditions are less conducive to the virus spreading. | (Tosepu et al., 2020; Liu et al., 2020; Xie and Zhu 2020; Sajadi et al., 2020; Araujo and Naimi, 2020; Bashir et al., 2020; Şahin, 2020; Mehmood et al., 2021; Rahman et al., 2021 |
| Humidity | High absolute humidity performs a slowdown in transmissions. In contrast to this finding, many studies reported that low relative humidity likely favored the transmission of COVID-19 and showed an interactive effect between daily temperature and relative humidity on COVID-19 incidence. | Bukhari and Jameel, 2020; Liu et al., 2020; Qi et al., 2020; Sajadi et al., 2020; Mecenas et al., 2020 |
| Rainfall | Rainfall is not significantly correlated with COVID-19 transmission. One hypothesis is that rain (in comparison to sunny weather) strengthens the 'stay-at-home' order. On the contrary, one research finding showed that the higher attack rate of COVID-19 was significantly associated with moderate cumulative precipitation. | (Tosepu et al., 2020; Menebo, 2020; Chien and Chen, 2020; Wei et al., 2020 |
| wind speed | Poor air quality, along with strong winds, makes the virus more vulnerable to spreading, leading to an increase in the number of COVID-19 cases. On the other hand, a new study discovered that low wind speeds are linked to increased COVID-19 infection and association with the wind blows. | Bashir et al., 2020a, Coskun et al., 2021; Rendana, 2020; Coccia, 2021, 2021a; Şahin, 2020 |
| Air pollution | Atmospheric pollution can be regarded as a contributing factor to COVID-19 transmission being so high. Long-term exposure to air pollution induces a chronic inflammatory response, even in young and healthy individuals. PM2.5, O3, and NO2 have a strong correlation with the recent COVID-19 outbreak. | Bilal et al., 2021; Glencross et al., 2020; Conticini et al., 2020; Contini and Costabile, 2020; Coccia, 2021 |
2. Methodology
This study performed a scoping review of existing literature to address how climatic and non-climatic factors influence the transmission of COVID-19. Several potential climatic factors like temperature, rainfall, humidity, and verities of non-climatic factors, i.e., population density, physical distancing & quarantine, socioeconomic conditions, migratory flow, host immunity, personal hygiene practice, and public misinformation, were considered and recognized to understand the transmission mode of COVID-19. We provide a crystal clear scenario of virus transmission based on a comprehensive literature review that includes academic papers, policy reports, state papers, documents from foreign bodies, news articles, and numerous public websites with tone links. The scholarly article was collected with an endless search on PubMed, Scopus, and Google Scholar using COVID-19, Coronavirus, environment and COVID-19, Climate and COVID-19, transmission, health hygiene practice, awareness, and social behavior and South Asia.
3. Modes of transmission
The study of Gralinski and Menachery (2020) clarified that the novel coronavirus causing epidemics matches with the CoV isolated in bats. This finding can be linked with the appearance of the first case in Huanan Seafood Market in Wuhan city of China as wild animals were present on that market for trading purposes. Secondary cases started to be identified roughly ten days from the first outbreak. These patients, however, had no market contact. They had a history of contacting people who are either work at or visited that marketplace. A recent study on healthcare workers has explored that infected workers in Wuhan are human to human transmission (Sahin et al., 2020).
The first infection outside China was reported in Thailand on 13 January 2020. It reflects how the infection was spreading from Chinese provinces to Asian continents. This case was of Chinese tourists who traveled to Thailand and had no epidemiologic link to the Huanan Seafood Market (Hui et al., 2020). Human-to-human transmission usually happens with close contact. Mainly, the transmission occurs when an infected person produces respiratory droplets through sneezing and coughing. This process is similar to influenza and other respiratory pathogen spreading (Martins et al., 2020). The nature of the droplet is observed in individuals who inhale contaminated air through the mouth, nose, and lungs. However, it is still unclear if a person can get COVID-19 infected by touching an infected object or surface and then touching their nose, mouth, or likely eyes (Sedik et al., 2021; WHO, 2020b). It is considered that, like other respiratory viruses, coronavirus is the most contagious in symptomatic patients (Li et al., 2020). Cases have been reported where coronaviruses have been transmitted by airborne particles, further bolstering the idea that coronaviruses can spread through the air (Mehmood et al., 2021). During coughing, talking, and exhaling, viruses are spread into microdroplets that are small enough to remain suspended in the air for some time long enough to expose others from more than one to two meters away (Morawska and Milton, 2020).
The weather in winter, cold and dry, is directly correlated with annual peaks in influenza outbreaks (Park et al., 2020). One possible explanation for this different pattern of seasonal outbreaks in subtropical and tropical climates is that they frequently exhibit lower cases in the community, with numerous outbreaks occurring over a year, with Autumn through Spring being the primary shoulder seasons (Tamerius et al., 2011). The seasonality of outbreaks is impacted by various factors, with changes in weather fostering higher spread (Liu et al., 2020). According to previous studies, COVID-19 transmission may be influenced by environmental variations that occur with the seasons. SARS-CoV-2 is much more infectious and more lethal in colder climates. The result of the simulation reveals that 40–60% of COVID-19 cases are related to seasonality. Besides, in higher latitudes, COVID-19 seasonality is more apparent (Altamimi and Ahmed, 2020; Liu et al., 2021).
At least 80 countries in all climate zones, from cold, dry, and hot to wet regions across the WHO territory, reported local transmission from 20 June 2020. In particular, reports on local transmissions are made in South Africa, United States, Brazil, Mexico, Canada, Iran, Pakistan, India, Bangladesh, Russia, United Kingdom, Spain, Italy, and Germany (WHO 2020a). Burkina Faso, Panama, the Democratic Republic of the Congo, and Paraguay local communications have been notified with a mean ambient temperature of over 25 °C between 1 January 2020 and 31 March 2020. (O'Reilly et al., 2020).
4. Influencing factors on transmission
There are various driving factors on COVID-19 transmission at the community level: climatic, social, economic, and environmental. Climate variables such as temperature, wind speed, and rainfall may act as biological catalysts in this particular case of COVID-19, facilitating interaction between COVID-19 and humans. Behavioral characteristics of the host, host defensive mechanisms, virus infectivity, and population density are all important variables in determining how quickly a virus spreads (Cory, 2015; Menebo, 2020).
In this study, we attempted to explore possible climatic and non-climatic factors and their interconnectedness. Minimal studies were conducted on influencing determinants of COVID-19 transmission. Based on the recent literature, possible climatic and non-climatic factors have been identified (Table-1 and Table-2).
4.1. Climatic factor
The previous study reported that SARS was slowly blanched with warmer weather, and temperature changes, including climate change, could lead to the outbreak of COVID-19 (Liu et al., 2020). For example, Wu et al. (2020) found that increasing temperature and humidity may partially reduce the COVID 19 pandemic. Korean scientists also explored that low daily temperatures and low/high relative humidity have been associated with increased influenza cases (Park et al., 2020). Liu et al. (2020) clarified that in COVID- 19 transmission, weather factors play a role independently. The transmission is favored by low humidity and moderate diurnal temperatures. In contrast to this finding, one recent study did not find any evidence to support that warmer weather could decline the COVID-19 infection cases (Xie and Zhu, 2020).
However, it is noticeable that maximum COVID-19 infected countries are primarily located in the low-temperature region. Positive linear relation with the number of confirmed cases COVID-19 is shown below the 3 °C mean temperature (Xie and Zhu, 2020). Sajadi et al. (2020) observed that areas with known community outbreaks had lower mean temperatures and specific humidity than regions where significant community transmission was not recorded. Ecological niche models and climate and transmission intensity comparisons have also been used to observe similar results (Wang et al., 2020; Araujo and Naimi, 2020).
Considering only the temperature variable, an increasing amount of COVID-19 decreases every 1 °C increase in temperature. However, the temperature rise cannot lead to substantial declines in reported cases of COVID-19 without comprehensive public health assistance (Wang et al., 2020; Luo et al., 2020). Therefore, the pandemic spread may be attributed to environmental conditions such as ambient temperature, humidity, air pollution, and wind speed.
Significant relations have been explored of wind speed and air quality on COVID-19 transmission from recent studies. Average wind speed is positively correlated with confirmed cases; an increase of 1% in average wind speed (m/s) results in 11.21 percent in confirmed cases (Adekunle et al., 2020). Poor air quality, along with strong winds, makes the virus more vulnerable to spreading, leading to a spike in COVID-19 cases (Bashir et al., 2020, Coskun et al., 2021; Coccia, 2021; Şahin, 2020). Oppositely, Rendana (2020) found low wind speeds linked to increased COVID-19 infection in Indonesia. Atmospheric pollution can be considered a co-factor in the extremely high level of COVID-19 transmission. PM2.5, O3, and NO2 strongly correlate with the recent COVID-19 outbreak (Conticini et al., 2020; Bilal et al., 2021; Glencross et al., 2020; Contini and Costabile, 2020; Coccia, 2021). However, most studies found a substantial negative connection between precipitation and COVID-19 instances. (Menebo, 2020; (Tosepu et al., 2020); Ward et al., 2020). Menebo (2020) drawn a hypothesis, rain strengthens the 'stay-at-home' order, decreasing the spread of virus transmission. On the contrary, Wei et al. (2020) showed that the higher attack rate of COVID-19 was significantly associated with moderate cumulative precipitation.
4.2. Non-climatic factor
There are several socioeconomic and demographic factors why this pandemic affects various social groups. According to socioeconomic and demographic characteristics, it appears that COVID-19 is having varying effects on different populations (Ahmad et al., 2020; Bashir et al., 2020). These include population density, urban and rural environments, education level, lifestyle, and household size. Non-climatic factors contribute to the COVID-19 infection, but the different socioeconomic groups probably feel differently. COVID-19 would spread in the specific socioeconomic group with increased people proximity, more large networks of communication, and lower hygiene levels (Lipsitch et al., 2020). There is evidence from a study done in New York City that communities with a lower average income were more at risk of being infected than higher-income areas (Bashir et al., 2020). Thus, in contrast to other groups, certain socioeconomic groups are more vulnerable. Therefore, logically, more virus infections from certain parts of society can be predicted (Saadat et al., 2020).
Table 2 shows essential influencing non-climatic factors for being infected by COVID-19.
Table 2.
The influencing non-climatic factors and their impacts on transmission of COVID-19.
| Influencing non-climatic factors | Impacts on transmission | References |
|---|---|---|
| Population density | Population density is highly associated with more significant infection and fatality rates in the Covid-19 pandemic. Chronic respiratory disorders are prevalent in people who live in densely populated areas, making them ideal targets for any infectious pathogen. | Conticini et al., 2020; Jha et al., 2021; Bashir et al., 2020; Sahin, 2020; Bhadra et al., 2021 |
| Household size | A large household has more potential to bring the virus home compared to a small household. | Bashir et al., 2020; Jha et al., 2021 |
| social/physical distancing and isolation/quarantine | social/physical distancing and isolation/quarantine can limit the rate of infection and reduce the peak incidence of covid-19. close interaction between people is robust in urban areas rather than in a rural environment. so, social distancing is made more difficult in metropolitan areas because of higher population density. in addition, it is challenging to apply appropriately in densely south asia because big gatherings characterize social practices. | sen-crowe et al., 2020; suppawittaya et al., 2020; MacIntyre, 2020; sjödin et al., 2020; kaur et al., 2021; seale et al., 2020; davey et al., 2020; bashir et al., 2020,smith et al., 2021, kaur et al., 2021 |
| socioeconomic conditions | several social and economic criteria like education, sanitation, income and clean water availability were credited as potential determinants for the outbreak of coronavirus. | jha et al., 2021, bashir et al., 2020; hawkins et al., 2020; mena et al., 2021 |
| Awareness level | Educated people are more aware of COVID- 19 infections than illiterate people. Lower educational attainment is highly connected with the increased incidence of COVID-19 cases and mortality. | Abboah-Offei et al., 2021; Hawkins et al., 2020; Sultana and Alam, 2020 |
| Lifestyles | Lifestyle change, i.e., staying at home more, avoiding public places and transport, canceling plans with family or friends, and colleagues, may decrease the risk of being infected by COVID-19. | (Cancello et al., 2020, Huang et al., 2020 |
| Host immunity | The healthy immune system can fight against the COVID-19 | Taghizadeh-Hesary and Akbari, 2020; Calder, 2020, Wang et al., 2020; Randolph and Barreiro, 2020; Bajaj et al., 2021 |
| Personal hygiene practice | One of the essential steps for preventing infections with COVID-19 is the WHO recommended standard and appropriate hand washing and wearing a mask. Personal hygiene practice can reduce the spread of coronavirus disease . | Seale et al., 2020; Arai et al., 2021; Humphreys, 2020; Liao et al., 2021; Abboah-Offei et al., 2021; WHO, 2020c |
| Healthcare facilities | The same level of healthcare services is not available to various socioeconomic groups. Residents in areas with a lower socioeconomic status, such as India, Pakistan, and Bangladesh, are at greater risk due to a lack of healthcare services . | Islam et al., 2021; Singh and Chauhan, 2020 |
| Public misinformation | Misinformation on reported diseases, medications, and vaccines; methods of prevention and mitigation; nutritional guidelines; and methods of COVID-19 disease transmission impact the pandemic. Such misinformation is hiding good habits and encouraging harmful practices that transmit the virus. | Bastani and Bahrami 2020; Tasnim et al., 2020; Enders et al., 2020; Siddiqui et al., 2020; Lee et al., 2020; Mian and Khan, 2020 |
| Migratory flow | Migrants are the responsible factor as a reliable host source of COVID-19. | Fernández-Niño et al., 2020; Guadagno, 2020; Suresh et al., 2020; Alahmad et al., 2020; Zhang et al., 2021 |
Non-climatic factors, such as socioeconomic and political ones, also play a significant role in spreading COVID-19 (Wu et al., 2020). Researchers have concluded that 18 percent of the variability in disease replication duration is apparent from environmental factors, and the remaining 82 percent could be linked to prevention steps, public health strategies, population density, migration, and social and cultural aspects (Oliveiros et al., 2020). Among the non-climatic factor, inadequate health care facilities, low health literacy, migrants, people's unconsciousness, and social behavior also play a significant role in the fast transmission of COVID-19 (Hawkins et al., 2020; Jha et al., 2021; Singh and Chauhan, 2020; Sultana and Alam, 2020). It is challenging to decline the transmission of COVID-19 cases considering all non-climatic determinants in the resource-limited densely populated countries, like South Asian nations (Singh and Chauhan 2020; Bashir et al., 2020).
Another worrisome factor behind COVID-19 transmission is the return of migrants such as foreign workers. Though foreign worker remittance is one of the significant factors for the growing economy of developing countries, especially in the South Asian region (Takenaka et al., 2020) Unfortunately, these remittance fighters who return from Europe and the Middle East to South Asia during this pandemic are worrisome for their effete health awareness and social behavior (Islam et al., 2021; Jamil and Dutta, 2021). Migration data of Bangladesh, India, and Pakistan explored that returnee foreign migrants rapidly spread the virus in South Asia (Lee et al., 2021). After returning home, most migrants met relatives, friends, and neighbors without following quarantine rules (Suresh et al., 2020). Notably, one of the first patients infected with COVID-19 in Bangladesh returned from Italy during the pandemic (IEDCR, 2021). Besides, a healthy lifestyle, self-quarantine, and social distancing are challenging in developing countries because most people live in large families. They are financially constrained and hence cannot afford separate residences (Islam et al., 2021). On average, four members sharing a single room; all members use a single toilet, towel, and comb World Bank (2020).
While the extent of the COVID-19 pandemic is unknown, it is well recognized that beneficial individual and collective public positive behavior can help minimize virus spread and eventually save lives (Anderson et al., 2020). Throughout south Asian countries, traditional customs and values might be the primary components in community transmission since people of different religions traditionally celebrated their cultural events, such as weddings and funeral rites, with large gatherings (Sultana et al., 2020). South Asians have a very distinct way of greeting one another culturally. People enjoy exchanging handshakes and then hugging friends and relatives. Visiting someone who is sick is often considered a good gesture among south Asians. Those greetings manners can rapidly spread the virus (Islam et al., 2021; Lee et al., 2021). Most males, especially the young, spend their leisure time talking with friends in the street side tea stall. It is reported that males are loitering here and there, violating lockdown without a valid reason in South Asian countries (Islam et al., 2021). This scenario can also be linked with the higher death rate of male patients and the affected rate of young people (WHO, 2020b). A higher possibility is that females are getting affected by male family members. The level of personal health hygiene among the mass population is deficient in South Asia. Most people do not follow WHO-recommended proper handwashing methods and wear masks to kill and stop spreading viruses, respectively, due to their poor health literacy and unconsciousness (Rahman et al., 2019; Unicef, 2020).
The misconception through misinformation is one of the vital factors among the South Asian nations for the transmission of COVID-19 cases at community levels. Culturally South Asian people are religious. Amid the pandemic, religions can serve beneficial and destructive functions (Djalante et al., 2020). Religious fundamentalists propagate misinformation by claiming that godly people will not be affected by Sars-Cov2. Praying to God will protect them from being affected by the COVID-19 virus (Barua et al., 2020). For example, more than a hundred thousand people of Bangladesh attended funeral rites in the third week of April 2020 without maintaining physical distancing, violating government rules (CNN, 2020).
By avoiding groups and maintaining a safe distance of 1–2 m, social/physical distancing was encouraged (de Bruin et al. 2020). Studies indicated that social distancing in combination with isolation/restrictions reduces the probability of the disease within 13 to 14 weeks, and its peak incidence falls by 40 to 60 percent (Chang et al., 2020; Zhang et al., 2020). In addition, Isolation measures can be beneficial in controlling secondary viral transmission (Basile et al., 2020).
As procedures for preventing the spread of germs, practice good personal hygiene, such as using a tissue to cover the nose or mouth when coughing or sneezing or placing elbows on surfaces, were recommended (de Bruin et al. 2020). Efforts to prevent the spread of disease by regularly using hand sanitizer or washing hands thoroughly after contacting contaminated surfaces (de Bruin et al. 2020; Kaur et al., 2021). In order to limit the transmission of the contagious covid-19 virus, face masks became a vital tool. In addition, the significance of the facial mask can be inferred from the fact that one patient who did not wear the mask transmitted the virus to five others while traveling in a vehicle (Liu and Zhang, 2020; Liu et al., 2020). Thus, we may reasonably conclude that socioeconomic and demographic factors are at the heart of the COVID-19 outbreak, which explains why densely populated places have the more significant infection and mortality rates.
5. Conclusions
In this study, we assessed the influences of climatic and socioeconomic factors on COVID-19 transmission. According to the studies included in this review, climatic factors, notably temperature and humidity, contribute significantly to COVID-19 transmission. The relationship between temperature and humidity received much greater attention than wind speed and rainfall from the scientific community. Poor air quality, along with strong winds, makes the virus more vulnerable to spreading, leading to a spike in COVID-19 cases. PM2.5, O3, and NO2 showed a strong correlation with the recent outbreak.
There may be a link between rainfall and COVID-19 transmission, but it was not demonstrated consistently across all research studies due to limited available data and research examining these factors. In addition, the COVID-19 outbreak is also driven by socioeconomic and demographic factors, which explains why densely populated areas have higher infection and mortality rates. Population density is highly associated with more significant infection. Besides, Lower educational attainment is highly connected with increased incidence of COVID-19 cases and mortality.
The pandemic outbreak is generally controlled by many biological, health, political, social, economic, and climatic determinants and complex interrelationships among the determinants. The lack of available potential vaccines or effective medicines is the thumb limitation to control the pandemic. However, since 2020, the first generation of COVID-19 vaccines are available to the public, while research is ongoing to determine their efficacy against the new variants. Considering the issue, urgent short and long measures should be implicated to mitigate the risk of the epidemic, emphasizing both climatic and non-climatic factors. The majority of previous findings have not examined the independent effects on COVID-19 transmission of non-climatic factors such as population migration, health hygiene, and social behavior.
Further studies on the influences of climatic variables on COVID-19 transmission will be needed to consider population movements from increasing areas of occurrence and social circumstances. Caution should also be exercised in making any COVID-19 risk forecasts based on both climatic and non-climatic determinants. Further research is needed to clearly understand the association between sociodemographic and climatic factors with COVID 19 transmission for improved risk assessment, preparedness, and prevention and provide functional implications for scientists, policymakers, and the public .
Declaration of Competing Interest
The authors declare no conflict of interest.
Acknowledgments
Research funding
No funding.
Author contributions
Conceptualization, Alam, M.S.; methodology, Sultana, R.; writing, Alam, M.S.; review and editing, Sultana, R. All authors have read and agreed to the published version of the manuscript.
Ethical approval
The conducted research is not related to either human or animal use.
References
- Abboah-Offei M., Salifu Y., Adewale B., Bayuo J., Ofosu-Poku R., Opare-Lokko E.B.A. A rapid review of the use of face mask in preventing the spread of COVID-19. Int. J. Nurs. Studies Adv. 2021;3 doi: 10.1016/j.ijnsa.2020.100013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adekunle I.A., Tella S.A., Oyesiku K.O., Oseni I.O. Spatio-temporal analysis of meteorological factors in abating the spread of COVID-19 in Africa. Heliyon. 2020;6(8):e04749. doi: 10.1016/j.heliyon.2020.e04749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmadi M., Sharifi A., Dorosti S., Ghoushchi S.J., Ghanbari N. Investigation of effective climatology parameters on COVID-19 outbreak in Iran. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad S., Shoaib A., Ali M.S., Alam M.S., Alam N., Ali M., Mujtaba M.A., Ahmad A., Ansari M.S., Ali M.D. Epidemiology, risk, myths, pharmacotherapeutic management and socio economic burden due to novel COVID-19: a recent update. Res. J. Pharm. Technol. 2020;13(9):4435–4442. [Google Scholar]
- Alahmad B., Kurdi H., Colonna K., Gasana J., Agnew J., Fox M.A. COVID-19 stressors on migrant workers in Kuwait: cumulative risk considerations. BMJ Global Health. 2020;5(7) doi: 10.1136/bmjgh-2020-002995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altamimi A., Ahmed A.E. Climate factors and incidence of Middle East respiratory syndrome coronavirus. J. Infect. Public Health. 2020;13(5):704–708. doi: 10.1016/j.jiph.2019.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson R.M., Heesterbeek H., Klinkenberg D., Hollingsworth T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet North Am. Ed. 2020;395(10228):931–934. doi: 10.1016/S0140-6736(20)30567-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arai Y., Oguma Y., Abe Y., Takayama M., Hara A., Urushihara H., Takebayashi T. Behavioral changes and hygiene practices of older adults in Japan during the first wave of COVID-19 emergency. BMC Geriatr. 2021;21(1):1–9. doi: 10.1186/s12877-021-02085-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Araujo M.B., Naimi B. Spread of SARS-CoV-2 Coronavirus likely to be constrained by climate. MedRxiv. 2020 doi: 10.1101/2020.03.12.20034728. http://dx.doi.org/ [DOI] [Google Scholar]
- Awasthi A., Sharma A., Kaur P., Gugamsetty B., Kumar A. Statistical interpretation of environmental influencing parameters on COVID-19 during the lockdown in Delhi, India. Environ. Develop. Sustain. 2021;23(6):8147–8160. doi: 10.1007/s10668-020-01000-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Auler A.C., Cássaro F.A.M., Da Silva V.O., Pires L.F. Evidence that high temperatures and intermediate relative humidity might favor the spread of COVID-19 in tropical climate: a case study for the most affected Brazilian cities. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.139090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bajaj V., Gadi N., Spielman A.P., Wu S.C., Choi C.H., Moulton V.R. Aging, immunity, and COVID-19: how age influences the host immune response to coronavirus infections? Front. Physiol. 2021;11:1793. doi: 10.3389/fphys.2020.571416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barua Z., Barua S., Aktar S., Kabir N., Li M. Effects of misinformation on COVID-19 individual responses and recommendations for resilience of disastrous consequences of misinformation. Progr. Dis. Sci. 2020;8 doi: 10.1016/j.pdisas.2020.100119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., Benjiang M.A., Shahzad L. A brief review of socio-economic and environmental impact of Covid-19. Air Qual. Atmos. Health, 2020;13(12):1403–1409. doi: 10.1007/s11869-020-00894-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashir M.F., Ma B., Komal B., Bashir M.A., Tan D., Bashir M. Correlation between climate indicators and COVID-19 pandemic in New York, USA. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basile C., Combe C., Pizzarelli F., Covic A., Davenport A., Kanbay M., Kirmizis D., Schneditz D., Van Der Sande F., Mitra S. Recommendations for the prevention, mitigation and containment of the emerging SARS-CoV-2 (COVID-19) pandemic in haemodialysis centres. Nephrol. Dialysis Transplant. 2020;35(5):737–741. doi: 10.1093/ndt/gfaa069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bastani P., Bahrami M.A. COVID-19 related misinformation on social media: a qualitative study from Iran. J. Med. Internet Res. 2020 doi: 10.2196/18932. [DOI] [PubMed] [Google Scholar]
- Bhadra A., Mukherjee A., Sarkar K. Impact of population density on Covid-19 infected and mortality rate in India. Model. Earth Syst. Environ. 2021;7(1):623–629. doi: 10.1007/s40808-020-00984-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilal M.F.B., Komal B., Benghoul M., Bashir M.A., Tan D. Nexus between the COVID-19 dynamics and environmental pollution indicators in South America. Risk Manag. Healthc Policy. 2021;14:67. doi: 10.2147/RMHP.S290153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukhari, Q., Jameel, Y., 2020. Will coronavirus pandemic diminish by summer? SSRN. https://ssrn.com/abstract=3556998 or doi:https://doi.org/10.2139/ssrn.3556998
- Calder P.C. Nutrition, immunity and COVID-19. BMJ Nutr. Prevent. Health. 2020;3(1):74. doi: 10.1136/bmjnph-2020-000085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cancello R., Soranna D., Zambra G., Zambon A., Invitti C. Determinants of the lifestyle changes during COVID-19 pandemic in the residents of Northern Italy. Int. J. Environ. Res. Public Health. 2020;17(17):6287. doi: 10.3390/ijerph17176287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang L., Yan Y., Wang L. Coronavirus disease 2019: coronaviruses and blood safety. Transfus. Med. Rev. 2020;34(2):75–80. doi: 10.1016/j.tmrv.2020.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chien L.C., Chen L.W. Meteorological impacts on the incidence of COVID-19 in the US. Stochastic Environ. Res. Risk Assess. 2020;34(10):1675–1680. doi: 10.1007/s00477-020-01835-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark A., Jit M., Warren-Gash C., Guthrie B., Wang H.H., Mercer S.W., Sanderson C., McKee M., Troeger C., Ong K.L., Checchi F. Global, regional, and national estimates of the population at increased risk of severe COVID-19 due to underlying health conditions in 2020: a modelling study. Lancet Global Health. 2020;8(8):e1003–e1017. doi: 10.1016/S2214-109X(20)30264-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contini D., Costabile F. Does air pollution influence COVID-19 outbreaks? Atmosphere (Basel) 2020;377 doi: 10.3390/atmos11040377. [DOI] [Google Scholar]
- Cory J.S. Insect virus transmission: different routes to persistence. Curr. Opin. Insect. Sci. 2015;8:130–135. doi: 10.1016/j.cois.2015.01.007. [DOI] [PubMed] [Google Scholar]
- Coskun H., Yıldırım N., Gündüz S. The spread of COVID-19 virus through population density and wind in Turkey cities. Sci. Total Environ. 2021;751 doi: 10.1016/j.scitotenv.2020.141663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. The effects of atmospheric stability with low wind speed and of air pollution on the accelerated transmission dynamics of COVID-19. Int. J. Environ. Stud. 2021;78(1):1–27. doi: 10.1080/00207233.2020.1802937. [DOI] [Google Scholar]
- Coccia M. How do low wind speeds and high levels of air pollution support the spread of COVID-19? Atmos. Pollut. Res. 2021;12(1):437–445. doi: 10.1016/j.apr.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in Northern Italy? Environ. Pollut. 2020 doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davey S., Davey A., Jain R. Impact of social distancing on curtailing COVID 2019 epidemic in India: a systematic review by SWOT analysis approach. Epidemiol. Int. 2020;5(1):44–49. doi: 10.24321/2455.7048.202009. [DOI] [Google Scholar]
- de Bruin Y.B., Lequarre A.S., McCourt J., Clevestig P., Pigazzani F., Jeddi M.Z., Colosio C., Goulart M. Initial impacts of global risk mitigation measures taken during the combatting of the COVID-19 pandemic. Saf. Sci. 2020;128 doi: 10.1016/j.ssci.2020.104773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djalante R., Lassa J., Setiamarga D., Sudjatma A., Indrawan M., Haryanto B., Mahfud C., Sinapoy M.S., Djalante S., Rafliana I., Gunawan L.A. Review and analysis of current responses to COVID-19 in Indonesia: period of January to March 2020. Prog. Dis. Sci. 2020;6 doi: 10.1016/j.pdisas.2020.100091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doremalen N.van, Bushmaker T., Morris D.H., Holbrook M.G., Gamble A., Williamson B.N., Tamin A., Harcourt J.L., Thornburg N.J., Gerber S.I., Lloyd-Smith J.O., Wit E., Munster V.J. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020;382(16) doi: 10.1056/NEJMc2004973. 0-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CNN, 2020. 100,000 gather for funeral in Bangladesh, defying lockdown and sparking outbreak fears. https://edition.cnn.com/2020/04/19/world/bangladesh-funeral-cornavirus/index.html (Accessed on 02 July 2021)
- Enders, A.M., Uscinski, J.E., Klofstad, C., Stoler, J., 2020. The different forms of COVID-19 misinformation and their consequences. The Harvard Kennedy School (HKS) Misinformation Review, 1(8).
- Fernández-Niño J.A., Cubillos-Novella A., Bojórquez L., Rodríguez M. Recommendations for the response against COVID-19 in migratory contexts under a closed border: the case of Colombia. Biomédica. 2020;40:68–72. doi: 10.7705/biomedica.5512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glencross D.A., Ho T.-.R., Cami˜na N., Hawrylowicz C.M., Pfeffer P.E. Air pollution and its effects on the immune system. Free Radic. Biol. Med. 2020;151:56–68. doi: 10.1016/j.freeradbiomed.2020.01.179. [DOI] [PubMed] [Google Scholar]
- Guadagno, L., 2020. Migrants and the COVID-19 pandemic: an initial analysis.
- Gralinski L.E., Menachery V.D. Return of the Coronavirus: 2019-nCoV. Viruses. 2020;12(2):135. doi: 10.3390/v12020135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta A., Banerjee S., Das S. Significance of geographical factors to the COVID-19 outbreak in India. Model. Earth Syst. Environ. 2020;6(4):2645–2653. doi: 10.1007/s40808-020-00838-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haque S.E., Rahman M. Association between temperature, humidity, and COVID-19 outbreaks in Bangladesh. Environ. Sci. Policy. 2020;114:253–255. doi: 10.1016/j.envsci.2020.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins R.B., Charles E.J., Mehaffey J.H. Socio-economic status and COVID-19–related cases and fatalities. Public Health. 2020;189:129–134. doi: 10.1016/j.puhe.2020.09.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holshue M.L., DeBolt C., Lindquist S., Lofy K.H., Wiesman J., Bruce H., Spitters C., Ericson K., Wilkerson S., Tural A., Diaz G. First case of 2019 novel coronavirus in the United States. N. Engl. J. Med. 2020;382:929–936. doi: 10.1056/NEJMoa2001191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Wu Q., Wang P., Xu Y., Wang L., Zhao Y., Yao D., Xu Y., Lv Q., Xu S. Measures undertaken in China to avoid COVID-19 infection: internet-based, cross-sectional survey study. J. Med. Internet Res. 2020;22(5):e18718. doi: 10.2196/18718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hui D.S., Azhar E.I., Madani T.A., Ntoumi F., Kock R., Dar O., Ippolito G., Mchugh T.D., Memish Z.A., Drosten C., Zumla A. The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health—The latest 2019 novel coronavirus outbreak in Wuhan. China. International journal of infectious diseases. 2020;91:264–266. doi: 10.1016/j.ijid.2020.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphreys J. The importance of wearing masks in curtailing the COVID-19 pandemic. J. Family Med. Prim. Care. 2020;9(6):2606. doi: 10.4103/jfmpc.jfmpc_578_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- IEDCR(Institute of Epidemiology, Disease Control and Research) IEDCR; 2021. COVID-19 Status Bangladesh. Retrieved from https://www.iedcr.gov.bd (Accessed 4 August 2021) [Google Scholar]
- Islam A., Sayeed M.A., Rahman M.K., Ferdous J., Shano S., Choudhury S.D., Hassan M.M. Spatiotemporal patterns and trends of community transmission of the pandemic COVID-19 in South Asia: Bangladesh as a case study. Biosafe. Health. 2021;3(1):39–49. doi: 10.1016/j.bsheal.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jahangiri M., Jahangiri M., Najafgholipour M. The sensitivity and specificity analyses of ambient temperature and population size on the transmission rate of the novel coronavirus (COVID-19) in different provinces of Iran. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamil R., Dutta U. Centering the margins: the precarity of Bangladeshi low-income migrant workers during the time of COVID-19. Am. Behav. Sci. 2021 doi: 10.1177/00027642211000397. p. 00027642211000397. https://doi.org/10.1177%2F00027642211000397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jha S., Goyal M.K., Gupta B., Gupta A.K. A novel analysis of COVID 19 risk in India incorporating climatic and socio-economic factors. Technol. Forecast. Soc. Change. 2021;167 doi: 10.1016/j.techfore.2021.120679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaur S., Bherwani H., Gulia S., Vijay R., Kumar R. Understanding COVID-19 transmission, health impacts and mitigation: timely social distancing is the key. Environ. Develop. Sustain. 2021;23(5):6681–6697. doi: 10.1007/s10668-020-00884-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakshmi P.S., Suresh M. Factors influencing the epidemiological characteristics of pandemic COVID 19: a TISM approach. Int. J. Healthc Manag. 2020;13(2):89–98. doi: 10.1080/20479700.2020.1755804. [DOI] [Google Scholar]
- Lasisi T.T., Eluwole K.K. Is the weather-induced COVID-19 spread hypothesis a myth or reality? Evidence from the Russian Federation. Environ. Sci. Pollut. Res. 2021;28(4):4840–4844. doi: 10.1007/s11356-020-10808-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.J., Kang K.A., Wang M.P., Zhao S.Z., Wong J.Y.H., O'Connor S., Yang S.C., Shin S. Associations between COVID-19 misinformation exposure and belief with COVID-19 knowledge and preventive behaviors: cross-sectional online study. J. Med. Internet Res. 2020;22(11):e22205. doi: 10.2196/22205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.N., Mahmud M., Morduch J., Ravindran S., Shonchoy A.S. Migration, externalities, and the diffusion of COVID-19 in South Asia☆. J. Public Econ. 2021;193 doi: 10.1016/j.jpubeco.2020.104312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Q., Guan X., Wu P., Wang X., Zhou L., Tong Y., Ren R., Leung K.S., Lau E.H., Wong J.Y., Xing X. Early transmission dynamics in Wuhan, China, of novel coronavirus–infected pneumonia. N. Engl. J. Med. 2020 doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liao M., Liu H., Wang X., Hu X., Huang Y., Liu X., Brenan K., Mecha J., Nirmalan M., Lu J.R. A technical review of face mask wearing in preventing respiratory COVID-19 transmission. Curr. Opin. Colloid Interface Sci. 2021 doi: 10.1016/j.cocis.2021.101417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lipsitch M., Swerdlow D.L., Finelli L. Defining the epidemiology of Covid-19—Studies needed. N. Engl. J. Med. 2020;382(13):1194–1196. doi: 10.1056/NEJMp2002125. [DOI] [PubMed] [Google Scholar]
- Liu J., Zhou J., Yao J., Zhang X., Li L., Xu X., He X., Wang B., Fu S., Niu T., Yan J. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci. Total Environ. 2020;726 doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Zhang S. COVID-19: face masks and human-to-human transmission. Influenza Other Respir. Viruses. 2020;14(4):472. doi: 10.1111/irv.12740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Huang J., Li C., Zhao Y., Wang D., Huang Z., Yang K. The role of seasonality in the spread of COVID-19 pandemic. Environ. Res. 2021;195 doi: 10.1016/j.envres.2021.110874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu R., Gunawan J., Effendy D.S., Lestari H., Bahar H., Asfian P. Correlation between weather and Covid-19 pandemic in Jakarta, Indonesia. Sci. Total Environ. 2020;725 doi: 10.1016/j.scitotenv.2020.138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JHU, 2021. Center for Systems Science and Engineering at Johns Hopkins University. Available from https://github.com/CSSEGISandData/COVID-19. Accessed on 03 August 2021.
- Luo, W., Majumder, M.S., Liu, D., Poirier, C., Mandl, K., D, Lipsitch, M., Santillana, M., 2020. The role of absolute humidity on transmission rates of the COVID-19 outbreak. MedRxiv. DOI: https://doi.org/10.1101/2020.02.12.20022467 [DOI] [PMC free article] [PubMed]
- MacIntyre C.R. Case isolation, contact tracing, and physical distancing are pillars of COVID-19 pandemic control, not optional choices. Lancet Infect. Dis. 2020;20(10):1105–1106. doi: 10.1016/S1473-3099(20)30512-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marson F.A.L., Ortega M.M. COVID-19 in Brazil. Pulmonology. 2020;26(4):241–256. doi: 10.1016/j.pulmoe.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martins L.D., da Silva I., Batista W.V., de Fátima Andrade M., de Freitas E.D., Martins J.A. How socio-economic and atmospheric variables impact COVID-19 and influenza outbreaks in tropical and subtropical regions of Brazil. Environ. Res. 2020;191 doi: 10.1016/j.envres.2020.110184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McClymont H., Hu W. Weather variability and COVID-19 transmission: a review of recent research. Int. J. Environ. Res. Public Health. 2021;18(2):396. doi: 10.3390/ijerph18020396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehmood K., Bao Y., Abrar M.M., Petropoulos G.P., Soban A., Saud S., Khan Z.A., Khan S.M., Fahad S. Spatiotemporal variability of COVID-19 pandemic in relation to air pollution, climate and socio-economic factors in Pakistan. Chemosphere. 2021;271 doi: 10.1016/j.chemosphere.2021.129584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mena G.E., Martinez P.P., Mahmud A.S., Marquet P.A., Buckee C.O., Santillana M. Socio-economic status determines COVID-19 incidence and related mortality in Santiago, Chile. Science. 2021;372(6545) doi: 10.1126/science.abg5298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Menebo M.M. Temperature and precipitation associate with Covid-19 new daily cases: a correlation study between weather and Covid-19 pandemic in Oslo, Norway. Sci. Total Environ. 2020;737 doi: 10.1016/j.scitotenv.2020.139659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mecenas P., Bastos R.T.D.R.M., Vallinoto A.C.R., Normando D. Effects of temperature and humidity on the spread of COVID-19: a systematic review. PLoS ONE. 2020;15(9) doi: 10.1371/journal.pone.0238339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mian A., Khan S. Coronavirus: the spread of misinformation. BMC Med. 2020:1–2. doi: 10.1186/s12916-020-01556-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mofijur M., Rizwanul Fattah I.M., Saiful Islam A.B.M., Uddin M.N., Ashrafur Rahman S.M., Chowdhury M.A., Alam M.A., Uddin M. Relationship between weather variables and new daily COVID-19 cases in Dhaka, Bangladesh. Sustainability. 2020;12(20):8319. [Google Scholar]
- Morawska L., Milton D.K. It is time to address airborne transmission of coronavirus disease 2019 (COVID-19) Clin. Infect. Dis. 2020;71(9):2311–2313. doi: 10.1093/cid/ciaa939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Reilly K.M., Auzenbergs M., Jafari Y., Liu Y., Flasche S., Lowe R. Effective transmission across the globe: the role of climate in COVID-19 mitigation strategies. Lancet Planetary Health. 2020;4(5):e172. doi: 10.1016/S2542-5196(20)30106-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oliveiros, B., Caramelo, L., Ferreira, N.C.,Caramelo, F., 2020. Role of temperature and humidity in the modulation of the doubling time of COVID-19 cases. MedRxiv. DOI: https://doi.org/10.1101/2020.03.05.20031872
- Park J.E., Son W.S., Ryu Y., Choi S.B., Kwon O., Ahn I. Effects of temperature, humidity, and diurnal temperature range on influenza incidence in a temperate region. Influenza Other Respir. Viruses. 2020;14(1):11–18. doi: 10.1111/irv.12682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi H., Xiao S., Shi R., Ward M.P., Chen Y., Tu W., Su Q., Wang W., Wang X., Zhang Z. COVID-19 transmission in Mainland China is associated with temperature and humidity: a time-series analysis. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman, M., Islam, M., Shimanto, M.H., Ferdous, J., Rahman, A.A.N.S., Sagor, P.S., Chowdhury, T., 2021. A global analysis on the effect of temperature, socio-economic and environmental factors on the spread and mortality rate of the COVID-19 pandemic. Environ. Develop. Sustain., 23(6), pp.9352–9366. doi:10.1007/s10668-020-01028-x [DOI] [PMC free article] [PubMed]
- Rahman M.M., Ali M.A., Parvez A., Shahriar M., Rahman T., Shameem D. Knowledge and practice of personal hygiene among primary school students in Dhaka, Bangladesh. J. Pharm. Sci. Res. 2019;11(9):3140–3144. [Google Scholar]
- Randolph H.E., Barreiro L.B. Herd immunity: understanding COVID-19. Immunity. 2020;52(5):737–741. doi: 10.1016/j.immuni.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rendana M. Impact of the wind conditions on COVID-19 pandemic: a new insight for direction of the spread of the virus. Urban Clim. 2020 doi: 10.1016/j.uclim.2020.100680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sultana R., Alam M.S. Disaster Medicine and Public Health Preparedness; 2020. Natural Disasters and the Dengue Epidemic During the COVID-19 Outbreak: Deadly Combination For Public Health Threats in Bangladesh; pp. 1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saadat S., Rawtani D., Hussain C.M. Environmental perspective of COVID-19. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahin Ahmet-Riza, Aysegul Erdogan, Mutlu Agaoglu P., Dineri Yeliz, Cakirci Ahmet-Yusuf, Senel Mahmut-Egemen, Okyay Ramazan-Azim, Tasdogan Ali-Muhittin. 2019 novel coronavirus (COVID-19) outbreak: a review of the current literature. EJMO. 2020;4(1):1–7. doi: 10.14744/ejmo.2020.12220. [DOI] [Google Scholar]
- Şahin M. Impact of weather on COVID-19 pandemic in Turkey. Sci. Total Environ. 2020;728 doi: 10.1016/j.scitotenv.2020.138810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sajadi, M.M., Habibzadeh, P., Vintzileos, A., Shokouhi, S., Miralles-Wilhelm, F., Amoroso, A., 2020. Temperature, Humidity and Latitude Analysis to Predict Potential Spread and Seasonality for COVID-19. SSRN. https://dx.doi.org/ 10.2139/ssrn.3550308 [DOI] [PMC free article] [PubMed]
- Sasikumar K., Nath D., Nath R., Chen W. Impact of extreme hot climate on COVID-19 outbreak in India. GeoHealth. 2020;4(12) doi: 10.1029/2020GH000305. p.e2020GH000305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seale H., Dyer C.E., Abdi I., Rahman K.M., Sun Y., Qureshi M.O., Dowell-Day A., Sward J., Islam M.S. Improving the impact of non-pharmaceutical interventions during COVID-19: examining the factors that influence engagement and the impact on individuals. BMC Infect. Dis. 2020;20(1):1–13. doi: 10.1186/s12879-020-05340-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sedik A., Hammad M., Abd El-Samie F.E., Gupta B.B., Abd El-Latif A.A. Efficient deep learning approach for augmented detection of Coronavirus disease. Neural Comput. Appl. 2021:1–18. doi: 10.1007/s00521-020-05410-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sen-Crowe B., McKenney M., Elkbuli A. Social distancing during the COVID-19 pandemic: staying home save lives. Am. J. Emerg. Med. 2020;38(7):1519–1520. doi: 10.1016/j.ajem.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setti L., Passarini F., De Gennaro G., Barbieri P., Perrone M.G., Borelli M., Palmisani J., Di Gilio A., Torboli V., Fontana F., Clemente L., Pallavicini A., Ruscio M., Piscitelli P., Miani A. SARS-Cov-2RNA found on particulate matter of Bergamo in Northern Italy: first evidence. Environ. Res. 2020;188 doi: 10.1016/j.envres.2020.109754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siddiqui M.Y.A., Mushtaq K., Mohamed M.F., Al Soub H., Mohamedali M.G.H., Yousaf Z. Social media misinformation"—An epidemic within the COVID-19 pandemic. Am. J. Trop. Med. Hyg. 2020;103(2):920. doi: 10.4269/ajtmh.20-0592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh R.P., Chauhan A. Impact of lockdown on air quality in India during COVID-19 pandemic. Air Qual. Atmos. Health, 2020;13(8):921–928. doi: 10.1007/s11869-020-00863-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sjödin H., Wilder-Smith A., Osman S., Farooq Z., Rocklöv J. Only strict quarantine measures can curb the coronavirus disease (COVID-19) outbreak in Italy, 2020. Eurosurveillance. 2020;25(13) doi: 10.2807/1560-7917.ES.2020.25.13.2000280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobral M.F.F., Duarte G.B., da Penha Sobral A.I.G., Marinho M.L.M., de Souza Melo A. Association between climate variables and global transmission oF SARS-CoV-2. Sci. Total Environ. 2020;729 doi: 10.1016/j.scitotenv.2020.138997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sohrabi C., Alsafi Z., O'Neill N., Khan M., Kerwan A., Al-Jabir A., Iosifidis C., Agha R. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19) Int. J. Surg. 2020;76:71–76. doi: 10.1016/j.ijsu.2020.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith T.P., Flaxman S., Gallinat A.S., Kinosian S.P., Stemkovski M., Unwin H.J.T., Watson O.J., Whittaker C., Cattarino L., Dorigatti I., Tristem M. Temperature and population density influence SARS-CoV-2 transmission in the absence of nonpharmaceutical interventions. Proc. Natl. Acad. Sci. 2021;118(25) doi: 10.1073/pnas.2019284118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sultana, R., Fuad, N. and Ferdous, J., 2020. Containment Strategy during COVID-19 Outbreak-Analysis of Hospitals Hotspots in Dhaka to Prevent Community Transmission. Available at SSRN 3581666. https://dx.doi.org/ 10.2139/ssrn.3581666
- Suresh R., James J., RSJ B. Migrant Workers at Crossroads–The COVID-19 Pandemic and the Migrant Experience in India. Soc. Work Public Health. 2020;35(7):633–643. doi: 10.1080/19371918.2020.1808552. [DOI] [PubMed] [Google Scholar]
- Suppawittaya P., Yiemphat P., Yasri P. Effects of social distancing, self-quarantine and self-isolation during the COVID-19 pandemic on people's well-being, and how to cope with it. Int. J. Sci. Healthcare Res. 2020;5(2):12–20. doi: 10.1007/s40808-020-00984-7. [DOI] [Google Scholar]
- Taghizadeh-Hesary F., Akbari H. The powerful immune system against powerful COVID-19: a hypothesis. Med. Hypotheses. 2020;140 doi: 10.1016/j.mehy.2020.109762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takenaka, A.K., Gaspar, R., Villafuerte, J. and Narayanan, B., 2020. COVID-19 impact on International migration, remittances, and recipient households in developing Asia.
- Tamerius J., Nelson M.I., Zhou S.Z., Viboud C., Miller M.A., Alonso W.J. Global influenza seasonality: reconciling patterns across temperate and tropical regions. Environ. Health Perspect. 2011;119(4):439–445. doi: 10.1289/ehp.1002383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tandukar S., Bhandari D., Shrestha R.G., Sherchan S.P., Aryal A. Association between climatic and nonclimatic parameters and transmission of SARS-CoV-2 infection in Nepal. Environ. Dis. 2021;6(2):38. [Google Scholar]
- Tasnim S., Hossain M.M., Mazumder H. Impact of rumors and misinformation on COVID-19 in social media. J. Prevent. Med. Public Health. 2020;53(3):171–174. doi: 10.3961/jpmph.20.094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unicef, 2020. Water, sanitation, and hygiene (WASH).2020, Available from https://www.unicef.org/rosa/water-sanitation-and-hygiene-wash (Accessed on 10 June 2021)
- Wang, M., Jiang, A., Gong, L., Lu,L., Guo,W., Li, C., Zheng, J., Li, C., Yang B., Zeng, J., Chen, Y., Zheng, K., Li h.,2020. Temperature significant change COVID-19 transmission in 429 cities. MedRxiv. doi: https://doi.org/10.1101/2020.02.22.20025791
- Tosepu R, Gunawan J, Effendy D.S, Lestari H, Bahar H, Asfian P. Correlation between weather and Covid-19 pandemic in Jakarta, Indonesia. Science of the total environment. 2020;725 doi: 10.1016/j.scitotenv.2020.138436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward M.P., Xiao S., Zhang Z. The role of climate during the COVID-19 epidemic in New SouthWales, Australia. Transbound Emerg. Dis. 2020;67:2313–2317. doi: 10.1111/tbed.13631. https://onlinelibrary.wiley.com/journal/18651682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei J.T., Liu Y.X., Zhu Y.C., Qian J., Ye R.Z., Li C.Y., Ji X.K., Li H.K., Qi C., Wang Y., Yang F. Impacts of transportation and meteorological factors on the transmission of COVID-19. Int. J. Hyg. Environ. Health. 2020;230 doi: 10.1016/j.ijheh.2020.113610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- WHO(World Health Organization), 2020a. Coronavirus disease (COVID-19) outbreak situation. available from https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020
- WHO(World Health Organization), 2020b. Pneumonia of unknown origin – China. Disease outbreak news. Emergencies preparedness, response. Available from http://www.who.int/csr/don/12-january-2020-novel-coronavirus-china/en/csr/don/12-january-2020-novel-coronavirus-china/en, accessed on 07 July 2021.
- WHO(World Health Organization),2020c. Technical brief on Water, sanitation, hygiene, and waste management for the COVID-19 virus. https://apps.who.int/iris/bitstream/handle/10665/331305/WHO-2019-NcOV-IPC_WASH-2020.1-eng.pdf. Accessed on 06 June 2021.
- Wilder-Smith A., Chiew C.J., Lee V.J. Can we contain the COVID-19 outbreak with the same measures as for SARS? Lancet Infect. Dis. 2020;20:e102–e107. doi: 10.1016/S1473-3099(20)30129-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Bank, 2020. Press release on health impact. Available from: https://www.worldbank.org/en/news/press-release/2020/04/12/south-asia-must-act-now-to-lessen-covid-19-health-impacts. Accessed on 05 July 2021.
- Wu J.T., Leung K., Leung G.M. Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet North Am. Ed. 2020;395(10225):689–697. doi: 10.1016/S0140-6736(20)30260-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci. Total Environ. 2020;724 doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Z.W., Li Z.J., Hu W.B. Global dynamic spatiotemporal pattern of seasonal influenza since 2009 influenza pandemic. Infect. Dis. Poverty. 2020;9(1):1–9. doi: 10.1186/s40249-019-0618-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Chen C., Zhu S., Shu C., Wang D., Song J., Song Y., Zhen W., Feng Z., Wu G., Xu J. Isolation of 2019-nCoV from a stool specimen of a laboratory-confirmed case of the coronavirus disease 2019 (COVID-19). China. CDC Weekly. 2020;2(8):123–124. doi: 10.46234/ccdcw2020.033. http://dx.doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang M., Zhou J., Jia S., Zhao X., Chen Y., Sun Y., Liu Z., Zhou X., Li D., Luo C., Zhang Y. Undocumented Migrants Reintroducing COVID-19, Yunnan Province, China. Emerging Infect. Dis. 2021;27(5):1543. doi: 10.3201/eid2705.204944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., Xiang J., Wang Y., Song B., Gu X., Guan L. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet North Am. Ed. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]