Abstract
Atypical fibroxanthoma (AFX) is a rare cutaneous ulcerative lesion with a good prognosis. Diagnosis is difficult and is usually made by exclusion from pleomorphic dermal sarcoma and squamous cell carcinoma. Definitive treatment varies from Mohs micrographic surgery to wide local excision. We present a case of 76-year-old woman with AFX over the dorsum of her left hand. The tumour was excised and the resulting defect was reconstructed with a local second dorsal metacarpal artery perforator flap.
Keywords: plastic and reconstructive surgery, dermatology
Background
The term atypical fibroxanthoma (AFX) was coined by Helwig in 1963.1 It represents a reactive process. AFX is a rare low-grade soft tissue sarcoma. The exact aetiology is not known. It is believed to arise from fibroblast-like cells and myofibroblasts. Exposure to ultraviolet light is believed to cause its development. Other risk factors include trauma, radiation therapy and immunosuppression (diabetes, organ transplant, AIDS).2–4 It is seen most commonly in elderly people in the head and neck region. Other locations include the trunk, upper extremities and dorsum of hands. In middle-aged patients, it is most commonly seen on extremities and the trunk. It is usually presented as an ulcerated red nodule. It gives an impression of pyogenic granuloma or carcinoma. Definitive treatment varies from Mohs micrographic surgery to wide local excision with 1 cm margin.5
Case presentation
A 76-year-old female patient presented with 18-month history of nodular plaque over the dorsum of the middle finger extending into the third web space. The patient was a known case of undifferentiated connective tissue disorder. She was neither hypertensive nor diabetic. The lesion was approximately 4×1.5 cm in size with mild tenderness (figure 1A). She denied any history of trauma. There were no similar lesions anywhere on the body.
Figure 1.
(A) Atypical fibroxanthoma over the dorsum of the middle finger. (B) Wide local excision with 1 cm margin done; metacarpal artery flap has been planned. (C) Transfer of the second dorsal metacarpal artery flap to the defect. (D) Transferred flap; the donor area has been closed primarily.
Investigations
Preoperative punch biopsy findings were suggestive of AFX. The X-ray of the hand showed no signs of bony erosion.
Differential diagnosis
The differential diagnosis includes squamous cell carcinoma (SCC), malignant melanoma, dermatofibrosarcoma and pleomorphic dermal sarcoma (PDS). The absence of immunostaining for HMB45 and S100 differentiates from SCC and malignant melanoma. The absence of storiform pattern and CD34 positivity rules out dermatofibrosarcoma. A PDS can be differentiated by the absence of epithelial hyperplasia, grenz zone, collagen trapping.
Treatment
The lesion was excised with a resection margin of 1 cm all around the tumour (figure 1B) and sent for histopathological examination. The residual defect exposing the extensor tendon was covered with a second dorsal metacarpal artery perforator–based flap (figure 1C). The donor defect was closed primarily (figure 1D).
Outcome and follow-up
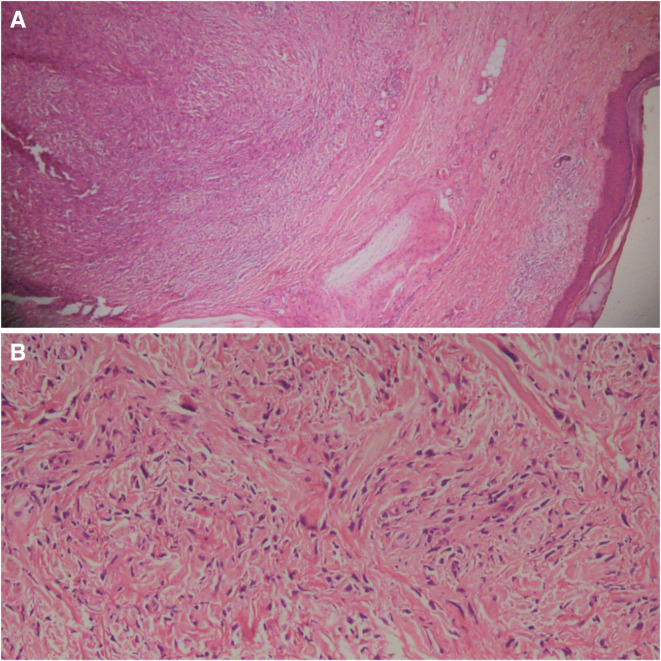
The histopathology report was consistent with AFX with resected margins free of tumour. Tumour cells were spindle to round in shape, arranged in short fascicles. Tumour cells showed marked pleomorphic nuclei, coarse chromatin and pale eosinophilic cytoplasm (figure 2A, B). AFX was concluded after the immunostains were positive for CD68 and being negative for SMA, CD34, S100. After a follow-up of 15 months, the patient did not complain of any recurrence (figure 3).
Figure 2.
(A) Dermis is occupied by atypical spindle cell lesion arranged short fascicles and ill-defined nodules (H&E ×10). (B) Presence of atypical spindle cells in a background of fibromyxoid stroma (H&E ×20).
Figure 3.

Well settled flap.
Discussion
AFX is rare. It is a pleomorphic spindle cell cutaneous neoplasm. Common presentation is a red or pink papule or nodular growth. Sakamoto et al reported the accumulation of DNA photoproducts which plays a key role in its pathogenesis.6 A skin biopsy confirms the diagnosis. Differential diagnoses include basal cell carcinoma, SCC, Merkel cell carcinoma, amelanotic melanoma, pyogenic granuloma and adnexal tumours. The term malignant fibrous histiocytoma is no longer used and the deep and more aggressive variant of AFX is called PDS.
AFX and PDS tumours share many clinical, aetiological and histological features and likely represent components of a tumour spectrum. In dermatologic oncology, differentiating between both soft tissue sarcomas, AFX and PDS, is pivotal as tumours with histological features consistent with PDS are more likely to behave in a clinically aggressive manner. Surgery remains the gold standard for treatment. In the setting of AFX, excision with the Mohs micrographic technique appears to offer superior tumour control rates while maintaining greater tissue preservation over wide local excision and should be considered first line in aesthetically important areas such as face, eyelids and canthus of the eye where tissue preservation is important. In our case, as the tumour was involving the dorsum of finger, we planned for wide local excision for better tumour control and as there was excessive skin laxity over dorsum of hand in the elderly woman, covering the resultant defect was easier with no donor site morbidity. The diagnosis of AFX is by exclusion. MRI may be of help when the lesion is situated in a poorly accessible location or metastasised. It rarely metastasises. It has a local recurrence of 6%–10%.7 Risk factors for metastasis include tumour necrosis, perineural or vascular invasion, deep lesion and immunocompromised state. The most common location of metastases includes subcutaneous tissue, parotid gland and lymph nodes.
Adjuvant radiotherapy is given in cases where the tumour cannot be excised completely. Brachytherapy can be given to those who are poor candidates for surgery. For a small lesion, less than 1 cm in size and slow-growing electrodesiccation and curettage has been tried. The prognosis of this tumour is good. There is no definitive consensus for follow-up. Every 6 monthly examination to look for recurrence and additional malignancies is recommended.
With this case report, we would like to share our reconstruction experience of a rare hand disease. With tumour-free resection and reconstruction with like tissue, we offered the best possible reconstruction without hampering hand function.
Learning points.
Diagnosis of atypical fibroxanthoma (AFX) is challenging.
AFX is believed to be a benign lesion and needs to be differentiated from other malignant skin lesions with its characteristic histological and immunostaining properties.
Wide local excision or Mohs micrographic surgery is the treatment of choice.
Regular follow-up is recommended to look for recurrence.
Footnotes
Contributors: GK, ST and SN have conceived the idea of writing the paper and have contributed equally to prepare the manuscript. RKS has guided intellectually and corrected the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.HELWIG EB. Tumor seminar. Tex State J Med 1963;59:652–89. [PubMed] [Google Scholar]
- 2.Tolkachjov SN, Kelley BF, Alahdab F, et al. Atypical fibroxanthoma: systematic review and meta-analysis of treatment with Mohs micrographic surgery or excision. J Am Acad Dermatol 2018;79:929–34. 10.1016/j.jaad.2018.06.048 [DOI] [PubMed] [Google Scholar]
- 3.Worley B, Nemechek AJ, Stoler S, et al. Naturopathic self-treatment of an atypical Fibroxanthoma: lessons for dermatologic surgery. J Drugs Dermatol 2018;17:683–5. [PubMed] [Google Scholar]
- 4.Winchester D, Lehman J, Tello T, et al. Undifferentiated pleomorphic sarcoma: factors predictive of adverse outcomes. J Am Acad Dermatol 2018;79:853–9. 10.1016/j.jaad.2018.05.022 [DOI] [PubMed] [Google Scholar]
- 5.Davis JL, Randle HW, Zalla MJ, et al. A comparison of Mohs micrographic surgery and wide excision for the treatment of atypical fibroxanthoma. Dermatol Surg 1997;23:105–10. 10.1111/j.1524-4725.1997.tb00670.x [DOI] [PubMed] [Google Scholar]
- 6.Sakamoto A, Oda Y, Itakura E, et al. Immunoexpression of ultraviolet photoproducts and p53 mutation analysis in atypical fibroxanthoma and superficial malignant fibrous histiocytoma. Mod Pathol 2001;14:581–8. 10.1038/modpathol.3880354 [DOI] [PubMed] [Google Scholar]
- 7.Mirza B, Weedon D. Atypical fibroxanthoma: a clinicopathological study of 89 cases. Australas J Dermatol 2005;46:235–8. 10.1111/j.1440-0960.2005.00190.x [DOI] [PubMed] [Google Scholar]