Abstract
Background:
Migraine patients often have painful trigger points, especially in the area of head and neck. Thus, we aimed to investigate the effect of myofascial release and stretching techniques in the management of migraine headache.
Materials and Methods:
This was a randomized controlled trial study on 40 migraine patients. The subjects in the experimental group received three sessions with a duration of 20 min per session techniques. Databases were analyzed using 2 × 3 repeated-measures analyses of variance (P < 0.05).
Results:
Experimental group showed a significant reduction in pain intensity (P < 0.001) and the neck disability index score (P < 0.001) and an increase in cervical range of motion (P < 0.001) in all time points after the intervention as compared with baseline and control group (P < 0.001).
Conclusion:
Myofascial release and stretching techniques were effective in improving symptoms in patients with migraine headache.
Keywords: Disability evaluation, migraine disorders, musculoskeletal manipulations, trigger points
INTRODUCTION
Primary headaches as classified according to the criteria of the International Headache Society (IHS) have a high percentage among adolescents. Migraine is a common and often debilitating neurologic condition, which is associated with physical and emotional dysfunctions.[1] One of the most problems that have an important role in the progression of headaches is the referral of muscle pain.[2] A bidirectional effect reflecting convergence of muscle afferents from the trigeminal and upper cervical neural systems has been shown. Therefore, the dysfunction of any structure receiving nociceptive information from the trigeminocervical nucleus caudalis can refer pain to the head.[3] The migraine patients revealed the presence of active trigger points (TrPs) in neck muscles such as the upper trapezius (UT), suboccipital, and sternocleidomastoid (SCM) muscles with increased tenderness to palpation of these muscles due to the presence of myofascial TrPs. This expedites the onset of migraine. Hence, evidence showed inactivation of active TrPs in patients with migraine, which can reduce the number of migraine attacks.[4]
There are a number of approaches for the treatment of migraine headaches, including drug therapy and nondrug therapy interventions. Nondrug approaches are often focused on musculoskeletal disorders.[5] In this study, we hypothesized that MTrP therapy and muscle stretching would provide relief of symptoms in patients with migraine. Hence, the present study aimed to analyze the effects of myofascial release and stretching techniques on the clinical outcomes of patients with migraine headache.
MATERIALS AND METHODS
In our randomized controlled trial study (Registration number: 20171219037956N1), neurologists referred 40 migraine patients between April and September 2018. They were invited to participate in this study according to the consolidated standards of reporting trials guideline [Figure 1].
Figure 1.
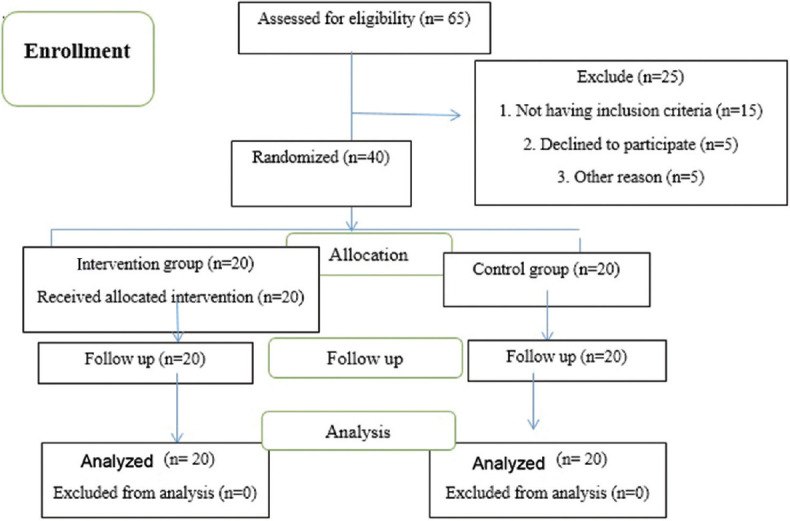
CONSORT flow diagram of the study
All subjects signed an informed consent form which was approved by the Ethics Committee of Social Welfare and Rehabilitation Sciences University (Ethics code no: IR.USWR.REC.1395.192).
They were included if presented a diagnosis of migraine headache according to the IHS criteria by a neurologist. In addition, participants showed active TrPs in the UT, suboccipital, and SCM muscles reproducing their headache. Participants were excluded if they had a history of neck trauma; cervical radiculopathy; previously had surgery in the neck or shoulder area; a history of diagnosed other headaches; and trigger point therapy in the neck within the previous 6 months.
Study design
Subjects were randomly divided into experimental and placebo-control groups by using block randomization method. The treatment was carried out over 2 weeks and included six sessions (3 sessions every week) with a duration of 20 min per session. Both the groups were assessed at baseline, immediately after the end of treatment, and after 1-month follow-up.
All interventions were performed with the patient placed in the supine position.
Sternocleidomastoid and upper trapezius muscles
To apply for the myofascial release, the active TrP was grasped between the physiotherapist's thumb and index fingers. The sustained and constant pressure was applied. For stretching of the SCM muscle, the therapist performed contralateral lateral flexion and ipsilateral rotation of the head to achieve stretching, separating the origin, and the insertion of the SCM muscle.[6]
Suboccipital muscle
To apply myofascial release technique, therapist's fingertips of each hand contacted the bony attachment of the sub-occipital region. Then, the therapist put sustained deep pressure over the musculature attachment to the occipital bone. For stretching technique, therapist put long-axis traction in a cephalic direction with the index finger and thumb in contact with the occiput and chin.[7]
Patients in this group received a soft and superficial massage on the attachment of the relevant muscles while participants were in the supine position.
Outcome measures
The pain intensity, neck disability index (NDI), and cervical range of motion (CROM) were evaluated at baseline, immediately after the treatment, and after 1-month follow-up.
The pain intensity was recorded on a reliable visual analog scale (VAS). Pain level on the VAS was recorded on a 10 cm line that subjects were asked to state their pain level by placing a mark along with this horizontal line[8]
The NDI is a widely used questionnaire that was designed to assess disability due to neck pain. Neck disability is classified as follows, as a function of NDI score: 0–4 = absence of disability; 5–14 = mild; 15–24 = moderate; 25–34 = severe; and 35 or higher = complete[9]
The CROM was measured by a reliable clinical goniometer. The subject sat in a chair with a backrest, with the straight column resting on it. Then, it was requested to perform the active cervical movements of flexion, extension, left and right rotation, and left and right lateral flexion with the goniometer on their head, to the point of pain.[10]
Statistical analysis
Normality of variables was evaluated by Kolmogorov–Smirnov test (P > 0.05). Two-way mixed-design ANOVA was used to determine changes of variables between the two groups. The level of significance was considered at P < 0.05. Statistical analysis was done by SPSS version 23 [Statistical Package for the Social Sciences (SPSS)].
RESULTS
In the experimental group, the mean age was 40.4 ± 11.2 years and in the control group, it was 37.45 ± 8.9. There was no statistically significant difference in gender distribution, age, weight, and body mass index between the two groups [Table 1].
Table 1.
Demographic data of the subjects (mean standard deviation)
| Variables | Control group (n=20) | Soft tissue group (n=20) | Pa, t |
|---|---|---|---|
| Age (years) | 37.45±8.9 | 40.40±11.27 | 0.36, 0.91 |
| Weight (kg) | 70.25±6.71 | 70.20±9.15 | 0.98, 0.02 |
| Height (m) | 1.70±0.1 | 1.68±0.09 | 0.60, 0.52 |
| BMIb | 24.37±2.46 | 25.07±3.40 | 0.46, 0.73 |
| Female/male | 12/8 | 12/8 | - |
aP-value for independent t-test. BMI=Body mass index
The pain intensity and NDI scores in the experimental group significantly decreased after intervention and 1-month follow-up (P < 0.001), but mean changes in pain intensity and NDI in the control group were the same and increased, respectively (P > 0.001). In addition, the difference between both the groups was significant [P < 0.001; Table 2].
Table 2.
Comparison of pain intensity, neck disability index, and cervical range of motion between subjects of the two experimental groups in different phases
| Variable | Control | Soft tissue | P1 | P2 Control | P2 Soft tissue | P3 | |||
|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|||||||
| Before-after | Before-follow | Before-after | Before-after | After | Follow | ||||
| Pain intensity | |||||||||
| Before | 7.70±0.92 | 7.21±0.85 | <0.001 | t=0.76 0.45 | t=1.78 0.09 | t=13.79 <0.001 | t=20.26 <0.001 | t=20.65 <0.001 | t=23.39 <0.001 |
| Immediately | 7.85±0.67 | 3.36±0.68 | |||||||
| Follow up | 8.05±0.88 | 1.57±0.83 | |||||||
| Neck disability index | |||||||||
| Before | 21.10±3.86 | 22.73±7.12 | <0.001 | t=7.99 0.45 | t=7.13 0.35 | t=10.31 <0.001 | t=13.15 <0.001 | t=13.74 <0.001 | t=23.38 <0.001 |
| Immediately | 24.50±3.13 | 9.42±3.70 | |||||||
| Follow up | 24.70±3.19 | 4.05±2.19 | |||||||
| Flexion (Degree) | |||||||||
| Before | 35.35±1.84 | 35.00±3.87 | <0.001 | t=17.94 <0.001 | t=14.18 <0.001 | t=12.82 <0.001 | t=13.24 <0.001 | t=6.32 0.001 | t=12.98 <0.001 |
| Immediately | 32.95±1.73 | 38.57±3.56 | |||||||
| Follow up | 31.20±1.39 | 41.21±3.13 | |||||||
| Extension (Degree) | |||||||||
| Before | 25.15±1.84 | 23.15±2.91 | <0.001 | t=15.02 <0.001 | t=21.08 <0.001 | t=9.80 <0.001 | t=18.11 <0.001 | t=4.98 <0.001 | t=12.06<0.001 |
| Immediately | 22.60±1.78 | 26.15±2.60 | |||||||
| Follow up | 20.20±1.73 | 28.57±2.54 | |||||||
| Right rotation (Degree) | |||||||||
| Before | 42.05±3.01 | 41.26±2.05 | <0.001 | t=11.89 <0.001 | t=12.95 <0.001 | t=12.15 <0.001 | t=15.84 <0.001 | t=9.12 <0.001 | t=15.69 <0.001 |
| Immediately | 38.95±3.11 | 46.78±2.12 | |||||||
| Follow up | 36.85±3.03 | 50.15±2.16 | |||||||
| Center rotation (Degree) | |||||||||
| Before | 40.85±3.01 | 39.36±3.26 | <0.001 | t=13.50 <0.001 | t=15.14 <0.001 | t=14.84 <0.001 | t=13.32 <0.001 | t=5.03 0.006 | t=10.65 <0.001 |
| Immediately | 38.10±2.78 | 42.84±3.09 | |||||||
| Follow-up | 35.95±2.96 | 46.31±3.11 | |||||||
| Right lateral flexion (Degree) | |||||||||
| Before | 37.35±3.01 | 35.05±3.71 | <0.001 | t=12.45 <0.001 | t=15.46 <0.001 | t=12.38 <0.001 | t=14.91 <0.001 | t=4.74 <0.001 | t=9.28 <0.001 |
| Immediately | 34.55±2.92 | 39.84±3.98 | |||||||
| Follow up | 32.40±2.50 | 42.94±4.39 | |||||||
| Center lateral flexion (Degree) | |||||||||
| Before | 36.70±2.38 | 34.47±3.83 | <0.001 | t=13.17 <0.001 | t=14.10 <0.001 | t=14.26 <0.001 | t=27.94 <0.001 | t=5.68 <0.001 | t=11.53 <0.001 |
| Immediately | 34.10±2.10 | 39.57±3.73 | |||||||
| Follow up | 32.00±1.97 | 43.68±4.05 | |||||||
P1=P-value for repeated measurement; P2=P-value for paired t-test, P3=P-value for independent t-test
Finally, the mean score of CROM in all directions showed that these trends increased in the intervention group (P < 0.001), but it was decreased in the control group (P < 0.001). The difference between the two groups was significant [P < 0.001; Table 2].
DISCUSSION
This study showed that myofascial release and stretching techniques used in this study were effective in improvement of clinical outcomes in the migraine patients, such as the pain intensity, CROM, and functional disability. These findings support previous studies that determined the myofascial release techniques as the best option to manage patients with migraine headache.[6,11] In line with the current study, Espí-López et al.[12] found that the suboccipital soft-tissue inhibition caused significant improvement of headache frequency, disability, and increased CROM in the tension-type patients. Furthermore, Ferragut- Garcías et al.[13] indicated the same results in the tension-type headache. Phadke et al.[14] stated that manual techniques on neck muscles were found to be effective to improve the pain and disability.
According to Simons,[15] the application of passive stretching with a gradual increase in range of motion during, as used in the present study, appears to inhibit alpha motor neuron response and inhibition of shortened muscle fibers when stretched. Thus, sarcomeres return to normal length. On the other hand, the use of myofascial release and stretching techniques may alter the sensitization of the trigeminocervical nucleus, since these techniques may have the potential to change neck muscle tone through alteration of the trigeminoreticular pathway.[3] In agreement with the above hypothesis, our results indicated that symptoms of migraine patients improved after treatment of TrPs of cervical muscles.
Study limitations
The short duration of therapy was one of the limitations of this study. Furthermore, the outcomes were subject to the misclassification bias related to the self-reported data. Further studies are recommended with further variable evaluation.
CONCLUSION
Myofascial release and stretching techniques were effective in improving symptoms in patients with migraine headache. Hence, these techniques can be used as a therapeutic option in migraine patients.
Financial support and sponsorship
This study was financially supported by the Social Welfare and Rehabilitation Sciences University.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders. (beta version). Cephalalgia. (3rd) 2013;33:629–808. doi: 10.1177/0333102413485658. [DOI] [PubMed] [Google Scholar]
- 2.Merikangas KR. Contributions of epidemiology to our understanding of migraine. Headache. 2013;53:230–46. doi: 10.1111/head.12038. [DOI] [PubMed] [Google Scholar]
- 3.Piovesan EJ, Di Stani F, Kowacs PA, Mulinari RA, Radunz VH, Utiumi M, et al. Massaging over the greater occipital nerve reduces the intensity of migraine attacks: Evidence for inhibitory trigemino-cervical convergence mechanisms. Arq Neuropsiquiatr. 2007;65:599–604. doi: 10.1590/s0004-282x2007000400010. [DOI] [PubMed] [Google Scholar]
- 4.Tali D, Menahem I, Vered E, Kalichman L. Upper cervical mobility, posture and myofascial trigger points in subjects with episodic migraine: Case-control study. J Bodyw Mov Ther. 2014;18:569–75. doi: 10.1016/j.jbmt.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 5.Rezaeian T, Mosallanezhad Z, Nourbakhsh MR, Noroozi M, Sajedi F. Effects of Dry Needling Technique Into Trigger Points of the Sternocleidomastoid Muscle in Migraine Headache: A Randomized Controlled Trial. American journal of physical medicine & rehabilitation. 2020;99:1129–37. doi: 10.1097/PHM.0000000000001504. [DOI] [PubMed] [Google Scholar]
- 6.Espí-López GV, Ruescas-Nicolau MA, Nova-Redondo C, Benítez-Martínez JC, Dugailly PM, Falla D. Effect of soft tissue techniques on headache impact, disability, and quality of life in migraine sufferers: A pilot study. J Altern Complement Med. 2018;24:1099–107. doi: 10.1089/acm.2018.0048. [DOI] [PubMed] [Google Scholar]
- 7.Rezaeian T, Mosallanezhad Z, Nourbakhsh MR, Ahmadi M, Nourozi M. The Impact of Soft Tissue Techniques in the Management of Migraine Headache: A Randomized Controlled Trial. Journal of Chiropractic Medicine. 2019;18:243–52. doi: 10.1016/j.jcm.2019.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hsieh YL, Kao MJ, Kuan TS, Chen SM, Chen JT, Hong CZ. Dry needling to a key myofascial trigger point may reduce the irritability of satellite MTrPs. Am J Phys Med Rehabil. 2007;86:397–403. doi: 10.1097/PHM.0b013e31804a554d. [DOI] [PubMed] [Google Scholar]
- 9.Vernon H. The neck disability index: State-of-the-art, 1991-2008. J Manipulative Physiol Ther. 2008;31:491–502. doi: 10.1016/j.jmpt.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Fletcher JP, Bandy WD. Intrarater reliability of CROM measurement of cervical spine active range of motion in persons with and without neck pain. J Orthop Sports Phys Ther. 2008;38:640–5. doi: 10.2519/jospt.2008.2680. [DOI] [PubMed] [Google Scholar]
- 11.Bevilaqua-Grossi D, Gonçalves MC, Carvalho GF, Florencio LL, Dach F, Speciali JG, et al. Additional effects of a physical therapy protocol on headache frequency, pressure pain threshold, and improvement perception in patients with migraine and associated neck pain: A randomized controlled trial. Arch Phys Med Rehabil. 2016;97:866–74. doi: 10.1016/j.apmr.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 12.Espí-López GV, Gómez-Conesa A, Gómez AA, Martínez JB, Pascual-Vaca AO, Blanco CR. Treatment of tension-type headache with articulatory and suboccipital soft tissue therapy: A double-blind, randomized, placebo-controlled clinical trial. J Bodyw Mov Ther. 2014;18:576–85. doi: 10.1016/j.jbmt.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 13.Ferragut-Garcías A, Plaza-Manzano G, Rodríguez-Blanco C, Velasco-Roldán O, Pecos-Martín D, Oliva-Pascual-Vaca J, et al. Effectiveness of a treatment involving soft tissue techniques and/or neural mobilization techniques in the management of tension-type headache: A randomized controlled trial. Arch Phys Med Rehabil. 2017;98:211–900. doi: 10.1016/j.apmr.2016.08.466. [DOI] [PubMed] [Google Scholar]
- 14.Phadke A, Bedekar N, Shyam A, Sancheti P. Effect of muscle energy technique and static stretching on pain and functional disability in patients with mechanical neck pain: A randomized controlled trial. Hong Kong Physiother J. 2016;35:5–11. doi: 10.1016/j.hkpj.2015.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simons DG. New views of myofascial trigger points: Etiology and diagnosis. Arch Phys Med Rehabil. 2008;89:157–9. doi: 10.1016/j.apmr.2007.11.016. [DOI] [PubMed] [Google Scholar]


