Abstract
Objectives:
Determine if patient satisfaction is greater after delivering postoperative care via telemedicine following minimally invasive gynecologic surgery.
Materials and Methods:
University-based outpatient clinic; Randomized controlled trial (Canadian Task Force classification I). Females between 18 and 60 years of age scheduled to undergo laparoscopic hysterectomy or laparoscopic excision of endometriosis were invited to participate. Eligible patients were randomized to receive postoperative care either through a traditional office visit or via telemedicine. PSQ-18 satisfaction surveys were performed by phone after the visit.
Results:
Forty-one patients were analyzed out of which 25 were in the office group and 16 in the telemedicine group. Groups were homogenous to age (41.4 vs. 43.3 p. 48), body mass index (31.9 vs. 30.6 P = 0.52), distance in miles from home (12.7 vs. 12.4 P = 0.92), and parity (P = 0.51). PSQ-18 questionnaire was scored and each category was compared between the office and telemedicine groups. When comparing medians (interquartile range), the general satisfaction and time spent with doctor categories were significantly higher in the telemedicine group (4.0 [4.0, 4.5] vs. 4.5 [4.5, 5.0] P = 0.05), (4.0 [4.0, 4.5] vs. 4.5 [4.0, 5.0] P = 0.05). The remainder of the categories analyzed were not different between groups Technical Quality (4.0 [3.8, 4.5] vs. 4.5 [3.9, 5.0] P = 0.13), Interpersonal Manner (4.0 [4.0, 4.5] vs. 4.5 [4.0, 5.0] P = 0.34), Communication (4.5 [4.0, 4.5] vs. 4.5 [4.3, 5.0] P = 0.21), Accessibility and Convenience (4.0 [3.5, 4.5] v 4.0 [3.6, 4.5] P = 0.84). A chart review was performed, examining the first 30 days after surgery. One (4%) patient in the office group went to the ER after postoperative visit, and 0 in the telemedicine group (P = 0.42).
Conclusion:
Postoperative care via telemedicine after gynecologic surgery results in higher patient satisfaction.
Keywords: Gynecologic, hysterectomy, laparoscopic, postoperative, robotic, surgery, telemedicine, virtual
INTRODUCTION
The wide-spread use of minimally invasive surgical techniques in Gynecology has brought several tangible benefits to patients including faster-recovery times, shorter hospital stays, and decreased risk of long-term complications, to name a few.[1,2,3] Technological advances such as the development of robotic assistance have allowed to further expand the variety of cases that can be performed via a minimally invasive approach.[4] The shift has been of such magnitude that the landscape regarding operative routes in gynecologic surgery has completely reversed, with now the majority of cases being performed laparoscopically.[5] Although much has changed intraoperatively, care during the postoperative period has, for the most part, remained static.
The current logistics of the postoperative visit involves blocking a time-slot for the patient during office hours, frequently 2 weeks after the operation. The patient is required to transport herself to the clinic site. Once checked-in, there may be a waiting period before being placed in a room for the practitioner to conduct the visit. The main components of a postoperative visit include inquiring about how the patient has been progressing, examining the incision site(s), and reviewing the pathology results if any specimens were extracted. Despite these visits being short and with a predefined structure, the invested time required by patients is substantially greater than the actual interaction with the clinician. Furthermore, because of the advantages of minimally invasive surgery, many patients have already returned to work by the time of the postoperative visit, which may result in disruption of their daily schedule.[6]
Delivery of postoperative care via telemedicine has been successfully incorporated into other fields such as urology and pediatrics with promising results.[7,8,9,10,11,12] Although this modality of care in gynecology only recently gained traction due social distancing guidelines implemented to mitigate the SARS-COV2 pandemic, there is a current lack of data regarding the safety of this practice.[13] In addition, information regarding patient perception and satisfaction is also lacking.[14]
We present data from a randomized control trial evaluating the use of telemedicine to deliver postoperative care in patients who underwent laparoscopic surgery. Recruitment for this study occurred before the COVID-19 contingency. Our primary objective was to determine if there was a difference in patient satisfaction between traditional postoperative visits and telemedicine postoperative visits. We also evaluated the safety of the practice by analyzing hospital re-admissions, visits to the emergency department, further visits to the clinic, or the development of postoperative complications.
MATERIALS AND METHODS
We began enrollment after obtaining approval from the Institutional Review Board (IRB# E19110, approval date 6/21/2019). The trial was registered in clinicaltrials.gov (NCT04348357). We included patients between the ages of 18 and 60 who had access to a smart-phone with internet and audio/video capabilities and who were scheduled to undergo either a total laparoscopic hysterectomy with or without removal of adnexal structures or excision of endometriosis. We chose these procedures given that they are the most common benign operations in our practice that are considered major gynecologic surgery. Patients were excluded if they had concomitant pelvic floor repair procedures scheduled (utero-sacral ligament suspension, sacro-colpopexy, and/or mid-urethral slings). It was also established that patients would be dropped from the study if they suffered from a complication during surgery that required repair (bowel, bladder, or major vascular injury), if they were converted to an open procedure, or if they requested to physically come in.
Our primary outcome was to detect a difference in patient satisfaction. Expecting a 20% relative increase in the experimental arm, assuming two-tailed testing with an alpha of 0.05, and power of 80%, it was established that a sample of 64 patients was required.
The consent process occurred during their preoperative visit. After agreeing to participate, patients were randomly assigned to either traditional office visit group or telemedicine group via a pregenerated masked sequential list with block sizes 4:6. Patients and providers were blinded to allocation. Every patient was given oral and written instructions at this time regarding the logistics of a telemedicine visit in case they were assigned to that group. We used Webex Teams (Cisco, San Jose, CA, USA) to establish real-time audio/video telemedicine visits, so assistance with downloading the phone application was provided by a member of the research staff. Along with printed instructions, patients were given a sealed envelope that contained their group assignment and appointment date and time. They were instructed to not open the envelope until after the operation.
To standardize the structure of all postoperative visits regardless of modality, we established the following sequence of components: (1) Inquire about any concerns the patient has regarding recovery. (2) Review findings and procedures done during surgery and pathology results. (3) Visually examine abdominal laparoscopic port-sites. (4) The opportunity for the patient to ask any additional questions.
Data collected included age, ethnicity, body mass index (BMI), parity, distance from home address to the clinic in miles calculated using Google maps (Google, Mountain View, CA, USA), and operating time. We also collected the duration of the postoperative visit. In the case of telemedicine, this was from when the connection was established until disconnection. In the case of the traditional visit, it was collected by a member of the research team using a stop-watch from the time the provider first entered the room until the visit concluded.
All patients were then contacted by phone between 7 and 14 days after the encounter and were subjected to a PSQ-18 (Patient satisfaction questionnaire) regarding their post-operative visit. Results scale from 1 to 5 in 7 different categories, with 5 reflecting the highest satisfaction. The survey was conducted by a member of the research team blinded to allocation. They were also asked the question: “If you had the opportunity to have switched groups, would you have?” Finally, they were asked to give an estimate of how much time they utilized to complete the postoperative visit including transportation and waiting time (in 15 min increments).
A chart review was performed to investigate the first 30 postoperative days to determine if there were any phone calls to the clinic, hospital admissions, or visits to the emergency department following the postoperative encounter, which was scheduled at 2 weeks after surgery.
Quantitative variables were compared using mean and standard deviation. For skewed data, the median and inter-quartile range were used. Categorical variables were described using frequency and proportions. To assess the differences across the two randomized groups, the Student's t-test, and the Chi-squared test were used. In the case of violation of normality, the Wilcoxon sum rank test was used. Linear regression models were used to estimate the adjusted effects of the outcomes of the PSQ 18 scores for patients' satisfaction between the two groups. P < 5% were considered statistically significant. All analyses were performed using STATA V.15 (StataCorp LLC, College Station, Texas, USA).
RESULTS
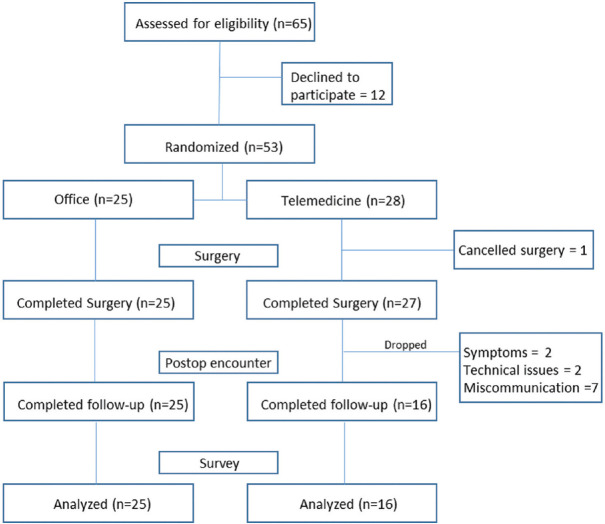
Recruitment for the study was halted early given that all postoperative visits were converted to telemedicine during the COVID-19 contingency. A total of 65 patients were invited to enroll, out of which 53 accepted to participate. After randomization, 1 patient in the telemedicine group cancelled her surgery due to financial reasons. After surgery, 2 patients in the telemedicine group came for a physical appointment due to being symptomatic, 2 patients lost internet access, and 7 patients came in due to miscommunication (thought they were supposed to show up in clinic). We ended with 25 patients in the office group and 16 in the telemedicine group for analysis [Figure 1]. Groups were homogenous to age (41.4 vs. 43.3 p. 48), BMI (31.9 vs. 30.6 P = 0.52), distance in miles from home (12.7 vs. 12.4 P = 0.92), parity (P = 0.51) and nights in the hospital after surgery (P = 0.43) [Table 1]. 22 (88%) of patients had a hysterectomy in the office group and 14 (88%) in the telemedicine group (P = 0.43).
Figure 1.
Consort diagram
Table 1.
Baseline characteristics between randomized groups
| Factor | Cohort (%) | Office (%) | Telemedicine (%) | P |
|---|---|---|---|---|
| n | 41 | 25 | 16 | |
| Age, mean (SD) | 42.1 (7.9) | 41.4 (7.6) | 43.3 (8.3) | 0.48 |
| BMI, mean (SD) | 31.4 (6.0) | 31.9 (6.1) | 30.6 (6.1) | 0.52 |
| Distance, mean (SD) | 12.6 (6.8) | 12.7 (7.3) | 12.5 (6.2) | 0.92 |
| Distance, median (IQR) | 12.1 (8.7, 15.2) | 12.6 (8.1, 17.3) | 11.8 (8.8, 13.9) | 0.71 |
| Parity | 0.51 | |||
| 0 | 6 (15) | 3 (12) | 3 (19) | |
| 1 | 1 (2) | 1 (4) | 0 (0) | |
| 2 | 12 (29) | 9 (36) | 3 (19) | |
| 3 | 17 (41) | 8 (32) | 9 (56) | |
| 4 | 4 (10) | 3 (12) | 1 (6) | |
| 5 | 1 (2) | 1 (4) | 0 (0) | |
| Surgery | 0.96 | |||
| 0 | 36 (88) | 22 (88) | 14 (88) | |
| 1 | 5 (12) | 3 (12) | 2 (13) | |
| Nights in hospital after surgery | 0.43 | |||
| 0 | 31 (76) | 20 (80) | 11 (69) | |
| 1 | 8 (20) | 4 (16) | 4 (25) | |
| 2 | 1 (2) | 1 (4) | 0 (0) | |
| 3 | 1 (2) | 0 (0) | 1 (6) |
SD: Standard deviation; IQR: Interquartile range, BMI: Body mass index
PSQ-18 questionnaires were scored and each category was compared between the office and telemedicine groups [Table 2]. When comparing medians (interquartile range), the general satisfaction category was significantly higher in the telemedicine group (4.0 [4.0, 4.5] vs. 4.5 [4.5, 5.0] P = 0.05). Although mean visit time was similar between groups (9.2 min vs. 9.1 min P = 0.95), the PSQ-18 category for “time spent with doctor” was significantly higher in the telemedicine group (4.0 [4.0, 4.5] vs. 4.5 [4.0, 5.0] P = 0.05). The remainder of the categories analyzed were not different between groups Technical Quality (4.0 [3.8, 4.5] vs. 4.5 [3.9, 5.0] P = 0.13), Interpersonal manner (4.0 [4.0, 4.5] vs. 4.5 [4.0, 5.0] P = 0.34), Communication (4.5 [4.0, 4.5] vs. 4.5 [4.3, 5.0] P = 0.21), Accessibility and Convenience (4.0 [3.5, 4.5] vs. 4.0 [3.6, 4.5] P = 0.84). Results were similar after regression analysis when adjusting for distance from home in miles, demonstrating higher scores in general satisfaction (P 0.03) and time spent with doctor (P = 0.04).
Table 2.
Comparison of patients’ satisfaction (using patient satisfaction questionnaire 18) across groups
| Factor | Cohort | Office | Telemedicine | P |
|---|---|---|---|---|
| n | 41 | 25 | 16 | |
| General satisfaction, mean (SD) | 4.3 (0.6) | 4.1 (0.6) | 4.5 (0.6) | 0.11 |
| Technical quality, mean (SD) | 4.2 (0.6) | 4.1 (0.6) | 4.4 (0.6) | 0.15 |
| Interpersonal manner, mean (SD) | 4.3 (0.5) | 4.3 (0.4) | 4.3 (0.8) | 0.85 |
| Communication, mean (SD) | 4.4 (0.5) | 4.3 (0.5) | 4.5 (0.5) | 0.34 |
| Accessibility and convenience, mean (SD) | 4.0 (0.6) | 4.0 (0.6) | 4.0 (0.7) | 0.83 |
| Time spent with doctor, mean (SD) | 4.2 (0.7) | 4.0 (0.7) | 4.4 (0.6) | 0.08 |
| General satisfaction, median (IQR) | 4.5 (4.0, 5.0) | 4.0 (4.0, 4.5) | 4.5 (4.5, 5.0) | 0.05 |
| Technical quality, median (IQR) | 4.3 (3.8, 4.8) | 4.0 (3.8, 4.5) | 4.5 (3.9, 5.0) | 0.13 |
| Interpersonal manner, median (IQR) | 4.5 (4.0, 4.5) | 4.0 (4.0, 4.5) | 4.5 (4.0, 5.0) | 0.34 |
| Communication, median (IQR) | 4.5 (4.0, 5.0) | 4.5 (4.0, 4.5) | 4.5 (4.3, 5.0) | 0.21 |
| Accessibility and convenience, median (IQR) | 4.0 (3.5, 4.5) | 4.0 (3.5, 4.5) | 4.0 (3.6, 4.5) | 0.84 |
SD: Standard deviation; IQR: Interquartile range
As expected, when inquiring about total time invested to complete the visit, time was greater in the office group (60.8 min vs. 14.7 min P < 0.01). When asked the question whether they would have switched groups if possible, 2 (8%) said yes in the office group, and 0 in the telemedicine group P = 0.25).
A chart review was performed, examining the first 30 days after surgery. 1 (4%) patient in the office group went to the ER after postoperative visit, and 0 in the telemedicine group (P = 0.42). Regarding phone calls to the clinic 5 (20%) of patients incurred in at least one call in the office group, and 4 (25%) in the telemedicine group (P = 0.92) [Table 3].
Table 3.
Comparison of other cofactors across groups
| Factor | Cohort | Office | Telemedicine | P |
|---|---|---|---|---|
| n | 41 | 25 | 16 | |
| Actual visit time, mean (SD) | 9.2 (3.5) | 9.2 (4.0) | 9.1 (2.6) | 0.95 |
| Total time by patient, mean (SD) | 42.8 (42.8) | 60.8 (45.8) | 14.7 (11.9) | <0.001 |
| Total time by patient, median (IQR) | 30.0 (10.0, 60.0) | 50.0 (30.0, 70.0) | 10.0 (10.0, 15.0) | <0.001 |
| Would you switch groups? | 0.25 | |||
| No | 39 (95) | 23 (92) | 16 (100) | |
| Yes | 2 (5) | 2 (8) | 0 (0) | |
| ER visits after postop encounter | 0.42 | |||
| No | 40 (98) | 24 (96) | 16 (100) | |
| Yes | 1 (2) | 1 (4) | 0 (0) | |
| Office calls after postop encounter | 0.92 | |||
| 0 | 32 (78) | 20 (80) | 12 (75) | |
| 1 | 7 (17) | 4 (16) | 3 (19) | |
| 2 | 2 (5) | 1 (4) | 1 (6) |
SD: Standard deviation; IQR: Interquartile range
DISCUSSION
A significant shift towards virtual visits has occurred secondary to the SARS-COV 2 pandemic. However, there is a lack of literature to assess the implications of this practice, particularly in the field of Gynecology. In this study, we shed some light on patient acceptance and outcomes pertaining to postoperative care via telemedicine. The results are encouraging, and support a continuation of the modality postpandemic. General satisfaction and the subjective appreciation of “time spent with doctor” appear to be greater with postoperative care via telemedicine, and although the study was not designed to assess noninferiority, the scores in the remaining categories do not appear to be decreased. Furthermore, we did not observe significant increases in office phone calls or ER visits after receiving postoperative care via telemedicine, although the study may have not been sufficiently powered for this. The data also sheds light on the time invested by patients to complete an in-person visit, which are usually brief. Since many patients are back to routine activities, this extra time can be disruptive. Strengths of the study include the randomized nature of the analysis and the use of a widely validated instrument to assess patient satisfaction.[15] In addition, standardizing the structure of the postoperative visit and limiting inclusion to laparoscopy contributes towards reducing confounding factors. The data presented does have limitations. The population we serve is predominantly Hispanic and uninsured, which may not be generalizable to other geographic areas. It is also important to note that the inherent design of the study makes it subject to selection bias, as the patients that are not technologically inclined would tend to refuse participation or change their mind after consenting to participate once they realized they were allocated to the telemedicine group, resulting in uneven drop-out rate. This improved as the study was implemented by assisting all participants with installing the teleconference application during the preoperative visit. Another limitation is that recruitment stopped early. This was driven by an institutional halt in enrollment on all non-COVID related studies, and our department's decision to switch all postoperative visits to telemedicine. Lastly, logistic issues during early implementation resulted in some patients in the telemedicine group to drop out. These factors may limit the population towards which this data are applicable, as only patients that were able to navigate the hurdles of the technology were ultimately studied in the telemedicine group.
Overall, the data presented support the use of telemedicine to deliver postoperative care after gynecologic surgery. General satisfaction is greater, as well as the subjective perception of time spent with the provider, and there does not appear to be an increase in readmissions or complications. This modality of care should become widely available to willing patients undergoing minimally invasive gynecologic surgery in the future.
CONCLUSION
Postoperative care via telemedicine after gynecologic surgery results in higher patient satisfaction when compared to a traditional office visit.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Bijen CB, Vermeulen KM, Mourits MJ, de Bock GH. Costs and effects of abdominal versus laparoscopic hysterectomy: Systematic review of controlled trials. PLoS One. 2009;4:e7340. doi: 10.1371/journal.pone.0007340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.ACOG Committee Opinion No. 444: Choosing the route of hysterectomy for benign disease. Obstet Gynecol. 2009;114:1156–8. doi: 10.1097/AOG.0b013e3181c33c72. [DOI] [PubMed] [Google Scholar]
- 3.Schindlbeck C, Klauser K, Dian D, Janni W, Friese K. Comparison of total laparoscopic, vaginal and abdominal hysterectomy. Arch Gynecol Obstet. 2008;277:331–7. doi: 10.1007/s00404-007-0481-7. [DOI] [PubMed] [Google Scholar]
- 4.Silasi DA, Gallo T, Silasi M, Menderes G, Azodi M. Robotic versus abdominal hysterectomy for very large uteri. JSLS. 2013;17:400–6. doi: 10.4293/108680813X13693422521755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Turner LC, Shepherd JP, Wang L, Bunker CH, Lowder JL. Hysterectomy surgery trends: A more accurate depiction of the last decade? Am J Obstet Gynecol. 2013;208:277 e271–7. doi: 10.1016/j.ajog.2013.01.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vonk Noordegraaf A, Anema JR, Louwerse MD, Heymans MW, van Mechelen W, Brölmann HA, et al. Prediction of time to return to work after gynaecological surgery: A prospective cohort study in the Netherlands. BJOG. 2014;121:487–97. doi: 10.1111/1471-0528.12494. [DOI] [PubMed] [Google Scholar]
- 7.Finkelstein JB, Cahill D, Kurtz MP, Campbell J, Schumann C, Varda BK, et al. The use of telemedicine for the postoperative urologic care of children: Results of a pilot program. J Urol. 2019;202:159–63. doi: 10.1097/JU.0000000000000109. [DOI] [PubMed] [Google Scholar]
- 8.DeAntonio JH, Kang HS, Cockrell HC, Rothstein W, Oiticica C, Lanning DA. Utilization of a handheld telemedicine device in postoperative pediatric surgical care. J Pediatr Surg. 2019;54:1005–8. doi: 10.1016/j.jpedsurg.2019.01.032. [DOI] [PubMed] [Google Scholar]
- 9.Barnett ML, Ray KN, Souza J, Mehrotra A. Trends in telemedicine use in a large commercially insured population, 2005-2017. JAMA. 2018;320:2147–9. doi: 10.1001/jama.2018.12354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gutierrez G. Medicare, the Internet, and the future of telemedicine. Crit Care Med. 2001;29:N144–50. doi: 10.1097/00003246-200108001-00002. [DOI] [PubMed] [Google Scholar]
- 11.Viers BR, Lightner DJ, Rivera ME, Tollefson MK, Boorjian SA, Karnes RJ, et al. Efficiency, satisfaction, and costs for remote video visits following radical prostatectomy: A randomized controlled trial. Eur Urol. 2015;68:729–35. doi: 10.1016/j.eururo.2015.04.002. [DOI] [PubMed] [Google Scholar]
- 12.Canon S, Shera A, Patel A, Zamilpa I, Paddack J, Fisher PL, et al. A pilot study of telemedicine for post-operative urological care in children. J Telemed Telecare. 2014;20:427–30. doi: 10.1177/1357633X14555610. [DOI] [PubMed] [Google Scholar]
- 13.Lewnard JA, Lo NC. Scientific and ethical basis for social-distancing interventions against COVID-19. Lancet Infect Dis. 2020;20:631–3. doi: 10.1016/S1473-3099(20)30190-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gunter RL, Chouinard S, Fernandes-Taylor S, Wiseman JT, Clarkson S, Bennett K, et al. Current use of telemedicine for post-discharge surgical care: A systematic review. J Am Coll Surg. 2016;222:915–27. doi: 10.1016/j.jamcollsurg.2016.01.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Thayaparan AJ, Mahdi E. The patient satisfaction questionnaire short form (PSQ-18) as an adaptable, reliable, and validated tool for use in various settings. Med Educ Online. 2013;18:21747. doi: 10.3402/meo.v18i0.21747. [DOI] [PMC free article] [PubMed] [Google Scholar]